Abstract
Objective
To assess the risk of transmission of SARS-CoV-2 in schools in Norway mainly kept open during the covid-19 pandemic in the academic year 2020-21.
Design
Population wide, register based cohort study.
Setting
Primary and lower secondary schools in Norway open during the academic year 2020-21, with strict infection prevention and control measures in place, such as organisation of students into smaller cohorts. Contact tracing, quarantine, and isolation were also implemented, and testing of students and staff identified as close contacts.
Participants
All students and educational staff in primary and lower secondary schools in Norway, from August 2020 to June 2021.
Main outcome measures
Overall attack rate of SARS-CoV-2 transmission (AR14) was defined as the number of individuals (among students, staff, or both) in the school with covid-19, detected within 14 days of the index case, divided by the number of students and staff members in the school. AR14 to students (attack rates from all index cases to students only) and AR14 to school staff (attack rates from all index cases to staff members only) were also calculated. These measures for student and school staff index cases were also calculated separately to explore variation in AR14 based on the characteristics of the index case.
Results
From August 2020 to June 2021, 4078 index cases were identified; 3220 (79%) students and 858 (21%) school staff. In most (2230 (55%)) schools with an index case, no subsequent individuals with covid-19 were found within 14 days; in 631 (16%) schools, only one more individual with covid-19 within 14 days was found. Overall, AR14 was 0.33% (95% confidence interval 0.32% to 0.33%). When restricting index cases and subsequent individuals with covid-19 to students born in the same year, AR14 to students (0.56-0.78%) was slightly higher.
Conclusions
Regarding the number of people infected with SARS-CoV-2 among students and staff, these results suggest that schools were not an important setting for transmission of the virus in Norway during the covid-19 pandemic in the academic year 2020-21.
Keywords: COVID-19, Public health, Epidemiology, Pediatrics
What is already known on this topic
Many countries kept schools closed for extended periods during the pandemic and thus limited information on transmission of SARS-CoV-2 in schools is available
Previous studies were limited to one school district or municipality, or to a short time frame around the time of reopening of schools, providing little information at a national level of keeping schools open
What this study adds
This register based cohort study considers subsequent transmission of SARS-CoV-2 among students and staff in Norwegian primary and lower secondary schools during the academic year 2020-21, when schools were mostly kept open
No subsequent cases were observed by 14 days in most cases (55%) when the virus was introduced into schools
Only 0.33% of students and staff tested positive for covid-19 within 14 days of the school index case in primary and lower secondary schools
How this study might affect research, practice, or policy
The findings suggest that schools were not an important setting for transmission of SARS-CoV-2 in Norway during the academic year 2020-21
While these results were valid for the alpha variant, future studies should looks at how vaccination coverage and more transmissible virus variants affects school transmission patterns in schools kept open
Introduction
The role of schools in transmitting SARS-CoV-2, the virus that causes covid-19, has had considerable attention during the pandemic. The evidence indicates that the risk of transmission between students and staff in schools is low when infection prevention and control measures are implemented and adhered to.1 Most studies on transmission in schools have been conducted when schools have reopened after a period of closure, however, when community transmission is decreasing. The risk of introducing the virus into schools by students and staff increases with a higher incidence of the virus in the community.1 Thus many countries closed schools during periods of rising infection rates in the community.2 3 Information on transmission in schools during periods of high infection rates in the community is sparse, especially in the context of more transmissible variants of the virus.1
In Norway, schools were closed for six weeks during the first infection wave in spring 2020. School closures have been associated with a range of negative consequences for learning, wellbeing, and the mental health of students.4–9 Schools in Norway were therefore largely kept open during the academic year 2020-21 (ie, from August 2020 to June 2021), when the more transmissible alpha variant of the SARS-CoV-2 virus became dominant in Norway (February 2021).10 Instead of school closures, infection prevention and control measures specifically for schools were carefully implemented and adapted to the local epidemiological situation with a traffic light model of three levels (green, yellow, and red, figure 1). The model included organising students into smaller cohorts and limiting the mixing of cohorts. The main difference between the levels was the physical distancing measures. Green level was a near normal situation, yellow level had intermediate measures with cohorts similar to normal classes, whereas the red level had strict measures. If a student or staff member with covid-19 had been present at school during the infectious period, the cohort was normally placed in quarantine, and mostly offered online teaching.
Figure 1.
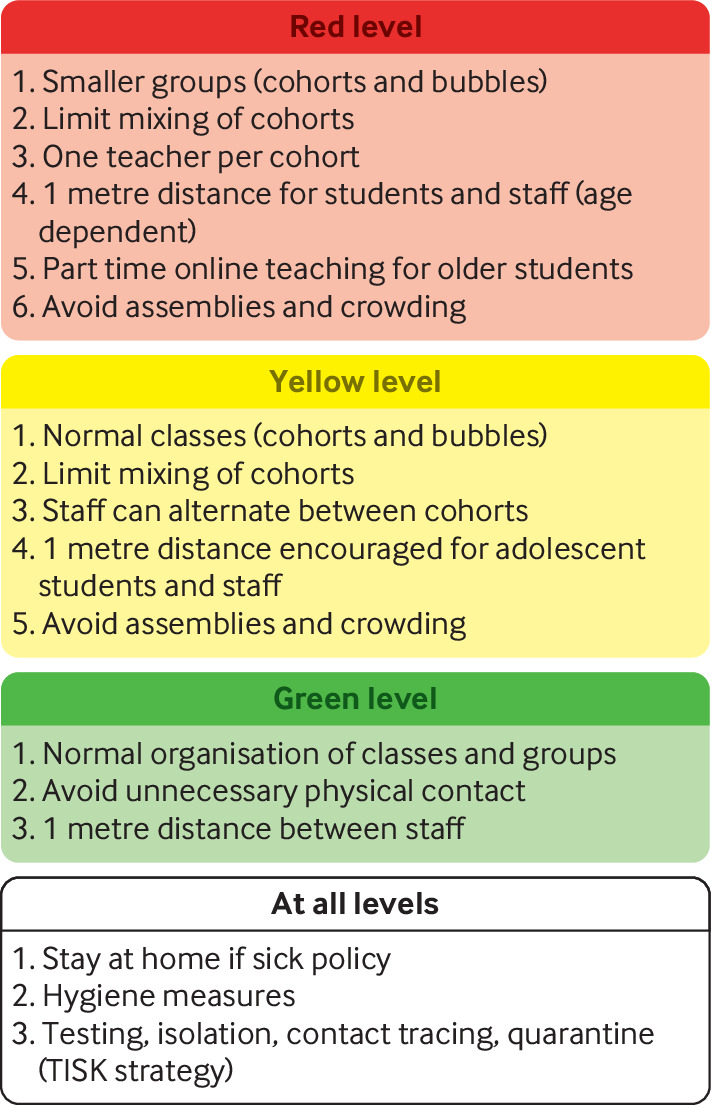
Traffic light model relating to infection prevention and control measures for schools
The red level was recommended nationally in lower secondary schools in the first weeks of January 2021 as a response to the introduction of the alpha variant of the virus. Except for these weeks, the yellow level was recommended nationally for primary and lower secondary schools throughout the study period. The red level was implemented in municipalities during periods when the infection rate in the local community was high, however. Face masks were not part of measures for students in primary schools, and had only a minor role in secondary schools when implemented in March 2021. As well as the measures in schools, the pandemic in Norway was managed mainly by the widespread use of testing, isolation, contact tracing, and quarantine11–13 (table 1).
Table 1.
Description of elements of the TISK (testing, isolation, contact tracing, and quarantine) strategy in relation to SARS-CoV-2 transmission
| Testing | Isolation | Contract tracing | Quarantine |
| People with symptoms of respiratory infection, people defined as close contacts* | Isolation of individuals who tested positive for covid-19 for 10 days after onset of symptoms or test date if asymptomatic† | Identification of close contacts | 10 days' quarantine required for close contacts after exposure |
Isolation and quarantine was mandatory, wheras testing was recommended.
*People who had been in close contact (<2 metre distance for ≥15 minutes, in direct physical contact, or in contact with secretions) with an individual who tested positive for covid-19 within 48 hours before the onset of symptoms or a positive test if asymptomatic.
†Before 2 November 2020, patients with symptoms had to isolate for at least eight days after the start of symptoms and for three days after the end of symptoms.
Studies of transmission into and within schools are important to improve our understanding of whether school closures prevent transmission of the virus in schools. Norway had limited school closures in primary and secondary schools during the academic year 2020-21 and therefore was a useful setting for studying transmission rates among students and staff after introduction of an individual with covid-19 into schools. Based on individual level data from nationwide administrative registers, we identified index cases and subsequent individuals with covid-19 in all primary and lower secondary schools in Norway in the academic year 2020-21.
Methods
Data sources
In this register based cohort study, we used data from Beredt C19, an emergency preparedness register developed to provide rapid information on the covid-19 pandemic in Norway.14 From the Beredt C19 register, we compiled individual level information from other administrative registers: personal information from the National Population Register; date of positive nasopharyngeal polymerase chain reaction (PCR) tests for SARS-CoV-2 from the Norwegian Surveillance System for Communicable Diseases (MSIS); date of PCR test regardless of the test result from the MSIS Laboratory Database; employment contracts for school staff members from the employer register and employee register; and encrypted school organisational numbers to identify school attendance and employment from the National Education Database from Statistics Norway.
In the 2020-21 academic year, 2776 primary and lower secondary schools were registered in Norway.15 We had data on 2641 schools and their respective geographical school catchment areas. We linked each student to a school based on their place of residence and birth year to determine student school affiliation (appendix).
bmjmed-2021-000026supp001.pdf (213.3KB, pdf)
Study population
The study period was the academic year 2020-21 (ie, 17 August 2020 to 15 June 2021). Our study population consisted of all students of primary and lower secondary school age (primary school students born 2008-14; lower secondary school students born 2005-07) and all employees aged 20-70 years in the 2641 schools who were registered as Norwegian residents in August 2020. We included only employees in occupations that usually have frequent contact with students (teachers, child care workers, and teaching assistants, online supplemental table A-1). The register data are of high quality and include information on the population over time, allowing complete follow-up with no loss of data (except for emigration and death).
Index cases, subsequent infections, and infection clusters
Within each school, the index case was defined as the first student or staff member with a positive PCR test for the SARS-CoV-2 virus. Subsequent individuals with covid-19 included all non-index students or staff at the same school as the index case with a positive PCR test within 14 days of the positive test date of the index case. Index cases and subsequent individuals with covid-19 were clustered together if they occurred at the same school within a period of ≤14 days. Based on the total number of individuals with covid-19, we categorised the clusters into single case clusters, two case clusters, and multiple case clusters (>2 cases). All cluster types were considered ended after 14 days if no new individuals with covid-19 were found at the same school, and schools were then re-entered if new individuals with covid-19 were detected. No index cases or subsequent individuals with covid-19 were included after 31 May 2021 to ensure complete follow-up.
Outcome
Our main outcome measure was incidence percentage of SARS-CoV-2 infection within 14 days of the index case, termed the attack rate (AR14). We calculated AR14 as the number of subsequent individuals with covid-19 divided by the total number of students and staff members in every school with an index case, multiplied by 100.16 Index cases were excluded in both the numerator and denominator. Clusters with two or more co-index cases (ie, index cases with identical test dates) were excluded from the main analysis.
Statistical analyses
Firstly, we plotted the weekly number of school clusters and the weekly number of new individuals with covid-19 per 100 000 residents between week 34, 2020 and week 21, 2021, in Norway, to provide an overview of the national infection rates during the study period. We also calculated the proportion of individuals with covid-19 detected among students and staff in the study population. Secondly, we grouped index cases by cluster type to study differences in distribution and characteristics. Thirdly, we used the number of subsequent individuals with covid-19 within 14 days of the index case to calculate overall AR14 (percentage of individuals who tested positive for covid-19 among students and staff members); AR14 to students (percentage of individuals who tested positive for covid-19 among students only); and AR14 to school staff (percentage of individuals who tested positive for covid-19 among staff members only). We also calculated these measures for student index cases and school staff index cases separately, and separately for index cases by occupational group (teachers, teaching assistants, and child care workers). To study changes in trends from before to after the alpha variant of the virus became dominant (February 2021), we visualised the overall AR14 by month of positive test date for student and school staff index cases. We also calculated the percentage of students and staff at schools who were tested within 14 days of the index case to assess the relation between attack rates and testing behaviour.
We conducted a subgroup analysis by calculating AR14 to students for each student birth cohort because students were likely to have closer contacts with other students of the same age (eg, infection prevention and control measures involved restriction of close contact between students and staff across school grades, and all close contacts, usually the whole cohort or class, were urged to get tested if an individual with covid-19 was identified at school).17 We conducted a sensitivity analysis by including clusters with two or more co-index cases and calculating AR14. To assess the robustness of the results when heterogeneity across schools was taken into account, we fitted a random effects regression model with random intercept for each school with at least one infection cluster. In this sensitivity analysis, we presented the mean AR14, interpreted as the mean intercept across schools, multiplied by 100.
In all analyses (except for the final sensitivity analysis), 95% confidence intervals were calculated with the Wilson method for binomial proportions, multiplied by 100. All statistical analyses were performed with R Statistical Software (version 3.6.2).
Patient and public involvement
This study was conducted without patient and public involvement, owing to both the urgency and the register based design. Thus no patients were involved in the design, execution, or interpretation of the study. As this study used anonymous data, dissemination to research participants is not possible. Results will be disseminated to public communities through the websites of the Norwegian Institute of Public Health.
Results
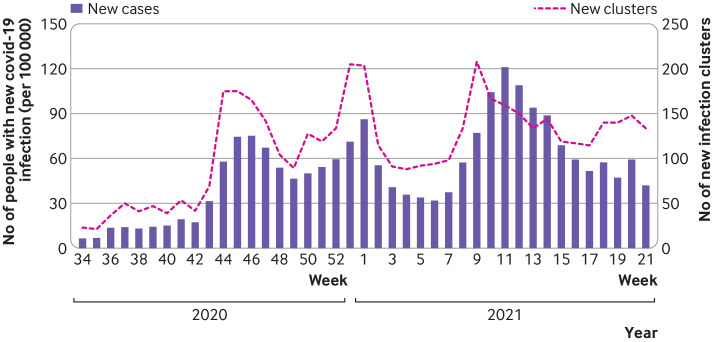
A total of 1 18 629 patients with a confirmed diagnosis of covid-19 were registered in MSIS between 17 August 2020 and 15 June 2021. The incidence of covid-19 peaked in week 46, 2020, and in week 1 and week 11, 2021 (figure 2). The highest number of new infection clusters in schools was in week 9, 2021 (209 clusters).
Figure 2.
Number of new school clusters of covid-19 and individuals with new infections of covid-19 per 100 000 people, per week in Norway, between week 34, 2020 and week 21, 2021. Infection clusters with co-index cases (ie, those with identical test dates) are included
The study population included 640 295 students and 102 574 staff members in 2641 different schools; 15 390 (2.4%) students and 2419 (2.4%) staff members tested positive for covid-19. We found large geographical variations, and the Oslo region had the highest number of individuals with covid-19 in the academic year 2020-21 among students (6.2%) and staff members (7.3%; online supplemental figure A-1). The corresponding value for the Norwegian population during the study period was 2.2%.
Characteristics of index cases
We excluded 586 infection clusters, involving 3609 patients with two or more co-index cases, from further analysis, leaving 12 217 students and 2073 school staff members who tested positive for covid-19. We identified 4078 index cases in 1573 different schools; 79.0% (n=3220) were students and 21.0% (n=858) were staff members (online supplemental table A-2). No subsequent individuals with covid-19 were seen by 14 days in most (54.7%, n=2230) clusters, and only one more individual with covid-19 was detected in 15.5% (n=631) of clusters. Multiple case clusters were detected in 29.8% (n=1217) of clusters. Multiple case clusters were more common in larger schools (<100 students, 10.0% (n=20/201); 100-299 students, 21.2% (n=236/1115); ≥300 students, 34.8% (n=961/2762)), whereas single case clusters were more common in smaller schools (<100 students, 75.6% (n=152/201); 100-299 students, 64.1% (n=715/1115); ≥300 students, 49.3% (n=1363/2762)). A higher proportion of single case clusters were found in teachers compared with students (60.8% (n=522/858) v 53.0% (n=1708/3220)), and a higher proportion of multiple case clusters were seen in lower secondary schools than in primary schools (32.1% (n=379/1181) v 28.4% (n=664/2341)).
Attack rates of SARS-CoV-2 infection in Norwegian schools
Among all 4078 index cases, the overall AR14 was 0.33% (95% confidence interval 0.32% to 0.33%), meaning that an average of 0.33% of other students and staff had confirmed covid-19 within 14 days of the index case (table 2 and table A-3; or about three subsequent people with covid-19 per 1000 index cases). Overall, we found small absolute differences across the main results. For example, AR14 was similarly low when considering subsequent cases only among students and only among staff, respectively. Small schools with <100 students had a slightly higher overall AR14 (0.60%, 95% confidence interval 0.49% to 0.74%) than schools of medium size (0.36%, 0.34% to 0.39%) and large size (0.32%, 0.31% to 0.32%). The same pattern was seen for AR14 to students, whereas school size did not affect AR14 to staff.
Table 2.
Attack rates of SARS-CoV-2 infection within 14 days after index test date (AR14), grouped by personal characteristics of the index case
| Characteristics of index case | Overall AR14 (%) (95% CI) | AR14 to students (%) (95% CI) | AR14 to staff (%) (95% CI) |
| All index cases, all school levels | 0.33 (0.32 to 0.33) | 0.33 (0.32 to 0.34) | 0.31 (0.29 to 0.34) |
| School size (all index cases): | |||
| <100 | 0.60 (0.49 to 0.74) | 0.69 (0.56 to 0.87) | 0.35 (0.21 to 0.58) |
| 100–299 | 0.36 (0.34 to 0.39) | 0.38 (0.35 to 0.40) | 0.30 (0.25 to 0.35) |
| ≥300 | 0.32 (0.31 to 0.32) | 0.32 (0.31 to 0.33) | 0.32 (0.29 to 0.35) |
| Students: | 0.32 (0.31 to 0.33) | 0.33 (0.32 to 0.34) | 0.28 (0.25 to 0.30) |
| Primary school age | 0.31 (0.30 to 0.32) | 0.31 (0.30 to 0.32) | 0.30 (0.27 to 0.34) |
| Lower secondary school age | 0.34 (0.32 to 0.36) | 0.36 (0.34 to 0.37) | 0.23 (0.20 to 0.27) |
| School staff: | 0.34 (0.32 to 0.36) | 0.32 (0.30 to 0.34) | 0.45 (0.40 to 0.52) |
| Primary school | 0.37 (0.35 to 0.40) | 0.35 (0.32 to 0.38) | 0.50 (0.43 to 0.59) |
| Combined schools* | 0.25 (0.22 to 0.29) | 0.23 (0.20 to 0.27) | 0.36 (0.27 to 0.49) |
| Lower secondary school | 0.34 (0.30 to 0.39) | 0.34 (0.29 to 0.38) | 0.40 (0.29 to 0.54) |
| Teacher | 0.37 (0.35 to 0.39) | 0.35 (0.33 to 0.37) | 0.49 (0.43 to 0.57) |
| Teaching assistants | 0.25 (0.21 to 0.29) | 0.24 (0.19 to 0.29) | 0.31 (0.21 to 0.47) |
| Child care workers | 0.23 (0.18 to 0.29) | 0.21 (0.16 to 0.27) | 0.35 (0.21 to 0.57) |
95% confidence intervals (CI) were calculated with the Wilson method for binomial proportions, multiplied by 100 to obtain percentages. AR14 was calculated as a percentage, with the number of subsequent individuals with covid-19 (infected non-index students and staff members within 14 days of the index case) in the numerator and the total number of non-index students and staff members in all schools with an index case in the denominator, multiplied by 100.
*Primary and lower secondary schools combined.
When the index case was a student, 0.33% (95% confidence interval 0.32% to 0.34%) of other students and 0.28% (0.25% to 0.30%) of staff members had confirmed covid-19 within 14 days. When the index case was a student in a primary school, we found no difference in AR14 to students or AR14 to staff. When the index case was a student in a lower secondary school, however, AR14 was higher in students (0.36%, 0.34% to 0.37%) than in staff members (0.23%, 0.20% to 0.27%). When the index case was a staff member, 0.45% (0.40% to 0.52%) of staff members and 0.32% (0.30% to 0.34%) of students were found to have confirmed covid-19 within 14 days. The highest attack rate was found for staff to other staff in primary schools (0.50%, 0.43% to 0.59%).
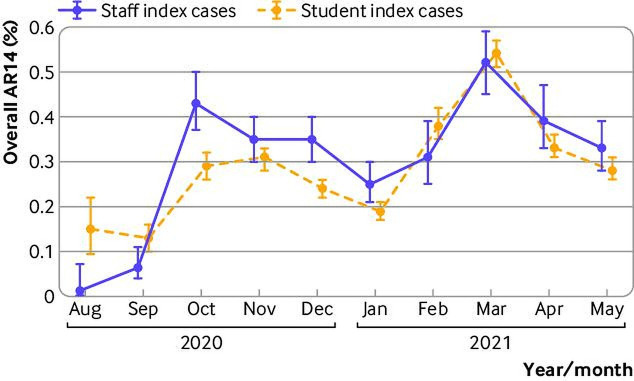
AR14 from staff index cases to staff or students who subsequently had covid-19 was slightly higher than from student index cases during the second wave of covid-19 in Norway, starting in October 2020 (figure 3). AR14 peaked in October for staff index cases and in November 2020 for student index cases. From January 2021, around the beginning of the third wave, we found a relatively steep increase in AR14 for student and staff index cases, followed by a second peak in both groups in March 2021. From February 2021 onwards, when the alpha variant of the virus became dominant, no significant difference in AR14 between student and staff index cases was seen. The temporal trend in testing rates generally followed the trend in attack rates (online supplemental figure A-2), and about 10% of all students and 15% of all staff at a school were tested within 14 days after the index case tested positive (online supplemental table A-4).
Figure 3.
Attack rates (95% confidence interval; AR14), calculated by including both students and staff subsequently infected with SARS-CoV-2 within 14 days of the index case in the numerator and all non-index student and staff members in the denominator, grouped by type of index case and month of the positive SARS-CoV-2 test of the index case
Subgroup analysis
The results from our subgroup analysis, where we calculated AR14 to students within each student birth cohort, showed slightly higher AR14 values than our main results for AR14 to students (table 3). AR14 ranged from 0.56% (95% confidence interval 0.52% to 0.61%) in students born in 2007 (grade 8) to 0.78% (0.70% to 0.87%) in students born in 2013 (grade 2).
Table 3.
Attack rates of SARS-CoV-2 infection within 14 days after index test date (AR14) in study population, by birth year
| Characteristics of index case | AR14 to students (%) (95% CI) | Numerator/denominator |
| School grade (birth year): | ||
| 1 (2014) | 0.65 (0.62 to 0.72) | 283/43 351 |
| 2 (2013) | 0.78 (0.70 to 0.87) | 349/44 685 |
| 3 (2012) | 0.65 (0.59 to 0.73) | 313/47 827 |
| 4 (2011) | 0.69 (0.62 to 0.76) | 358/51 955 |
| 5 (2010) | 0.66 (0.59 to 0.73) | 337/51 435 |
| 6 (2009) | 0.68 (0.62 to 0.75) | 397/58 043 |
| 7 (2008) | 0.73 (0.66 to 0.80) | 413/56 964 |
| 8 (2007) | 0.56 (0.52 to 0.61) | 568/101 337 |
| 9 (2006) | 0.57 (0.53 to 0.62) | 615/107 805 |
| 10 (2005) | 0.67 (0.62 to 0.72) | 701/104 650 |
95% confidence intervals (CI) were calculated with the Wilson method for binomial proportions, multiplied by 100 to obtain percentages. AR14 was calculated as a percentage, with the number of subsequent individuals with covid-19 (infected non-index students within 14 days of the index case) in the numerator and the total number of non-index students in the denominator, stratified by birth year of the index case, multiplied by 100. Only students born in the same year and attending the same school as the index case were included in the equation.
Sensitivity analyses
When we included the infection clusters with two or more co-index cases in our main analysis, we found a slightly higher overall AR14 of 0.38% (95% confidence interval 0.37% to 0.39%), whereas AR14 to students and AR14 to staff were unchanged (0.32%, 0.31% to 0.33% and 0.31%, 0.29% to 0.33%, respectively) (online supplemental table A-5). AR14 estimated with the random effects regression model, allowing for heterogeneity across schools, did not substantially alter the estimates for AR14 (results in table 2 compared with results in online supplemental table A-6).
Discussion
Principal findings
Population wide register data showed minimal transmission of SARS-CoV-2 between students and staff in primary and lower secondary schools in Norway during the academic year 2020-21. For most index cases, we found no (55%) or only one (16%) subsequent individual with covid-19. We found a low risk of transmission of covid-19 in schools, measured by AR14. Less than 0.5% of students and staff tested positive within 14 days of the index case, regardless of the characteristics of the index case.
Overall attack rates in schools were low throughout the whole study period, varying from just above 0% to 0.5%, even after the alpha variant of the virus became dominant in Norway in February 2021. We saw a steady reduction in AR14 for student and staff index cases after the first peak in October 2020, which might be explained by stricter infection prevention and control measures implemented as a response to high infection rates in the community. A similar reduction in AR14 was seen after the peak in March 2021, which was dominated by the alpha variant of the virus. This finding supports the effectiveness of implementing targeted infection prevention and control measures to reduce transmission of the virus in schools when infection rates are high in the community, especially when the alpha variant was the dominant form of the virus. Caution is needed, however, in generalising the effectiveness of these measures in reducing transmission of other variants of the SARS-CoV-2 virus, such as the delta and omicron variants.
Comparison with related studies
Previous studies have shown substantial variation in transmission of SARS-CoV-2 in different contact settings. Households have been the most important source of transmission; meta-analyses have reported pooled secondary attack rates of 16.4-20.0%.18–20 A nationwide study in Norway, involving all families with at least one parent and one child (comprising most students included in our study) found an overall secondary attack rate of 24%, with even higher transmission rates when a parent rather than a child was the index case.21 The school transmission rates in this nationwide study were exceptionally low, implying that transmission of covid-19 is more common in households and other social settings than in schools.
In contrast with our study, most studies on transmission of covid-19 in schools have been conducted in selected schools or regions and over a shorter time frame, typically around the time when schools reopened for in-person learning after a period of school closure.1 22–26 Our results support and extend these studies, concluding that the importance of schools as a source of transmission of SARS-CoV-2 is marginal when relevant infection prevention and control measures are in place.1 27
Transmission from students to staff was higher in primary schools than in lower secondary schools. A possible explanation for this finding is the closer contact between staff and younger children required for a secure and healthy psychosocial environment.28 Although the differences were small, the main results of our study showed that transmission between students was slightly higher in lower secondary schools than in primary schools, supporting the literature.29 30
Limitations of the study
In this study, we examined attack rates of covid-19 in schools based on data representative of a whole country, covering a full academic year. Our analysis had some limitations, however. Firstly, lack of data on whether subsequent individuals with covid-19 were infected in school or elsewhere might have led to overestimation of the attack rates. Because transmission is more likely to occur within the family than in schools or other public areas,19 21 31 transmission between siblings attending the same school might have added to this overestimation. Overestimating attack rates would strengthen our finding that primary and lower secondary schools in Norway have not been important settings for transmission of SARS-CoV-2, however.
Secondly, the register data did not include information on who were defined as close contacts of students and school staff (ie, were in the same class or in the same cohort). Thus we did not have the data necessary to estimate secondary attack rates among close contacts. The aim of our study was not to estimate the rate of transmission between close contacts or describe the general transmissibility of the virus, but rather to provide information on how keeping primary and lower secondary schools open (with infection prevention and control measures in place) affected the risk of transmission of the virus among students and school staff. The relatively high testing rates compared with attack rates after the detection of an index case indicate that most true subsequent individuals with covid-19 were captured in our data.
Modelling studies have shown that the Norwegian testing system has been functioning well since summer 2020, with an estimated detection rate of >60% of all real infections with SARS-CoV-2.32 Students in the same grade at the same school are more likely to be close contacts than students at the same school in general, and all close contacts were routinely recommended to test for the virus as part of the standard infection prevention and control measures. Although many close contacts chose to be tested, testing was only a recommendation and we did not have information on who among the close contacts was tested. Furthermore, testing capacity varied throughout the academic year and across municipalities. The closest proxy to close contacts available in our data was the subgroup analysis on attack rates in students in the same age cohorts. In relative terms, results from the subgroup analysis were two times greater than the main results. The absolute differences between the results from the main analysis and the subgroup analysis were small, however, and we believe had no practical implications, supporting the robustness of the main results.
Thirdly, we did not have data on whether the index case attended school or work during the infectious period. The lack of these data does not affect our main result, however, of a low risk of transmission in open schools with appropriate infection prevention and control measures in place. The policy in Norway of rapid testing, quarantine, and isolation of individuals infected with SARS-CoV-2 and their close contacts suggests that many index cases were, in reality, not attending school. Clearly, attack rates would likely have been much higher if the infection prevention and control measures had not succeeded in quarantining suspected individuals with covid-19 and keeping infected patients in isolation.
Lastly, indirect identification of school affiliation based on small geographical districts might have resulted in some misclassifications of students to schools, although previous research suggests that this assumption is not a great concern.33 Overall, the external validity of our results might be limited to countries and contexts comparable with Norway, and the findings might not be applicable to subsequent waves of infection caused by other variants of the virus or when widespread vaccination became available.
Clinical implications and future directions
The findings of this study indicate that primary and lower secondary schools in Norway have not been important settings for transmission of SARS-CoV-2 during the 2020-21 academic year, despite being kept open. Our results are similar to other studies.1 8 In Norway, test, isolate, trace, and quarantine has been the main infection prevention and control strategy for limiting spread of SARS-CoV-2.11 Infection prevention and control measures were imposed nationally throughout the study period, with further restrictions in areas with high community transmission. Also, targeted and flexible infection prevention and control guidelines for schools were developed and implemented to reduce transmission and avoid school closures,12 13 especially because of the negative consequences of school closures for student learning and wellbeing.4–8
The low attack rates reported in this study indicate that these strategies were appropriate in reducing transmission of the virus in schools in communities with high infection rates after the alpha variant of the virus became dominant. A policy on the use of face masks for was not in place for students for most of the study period, questioning the need for extensive use of face masks for children, given that other infection prevention and control measures were effectively implemented. The effect of face masks on reducing the risk of SARS-CoV-2 infection in the community is uncertain, however.34 35
The measures implemented in schools that were open could have been more effective than school closure and online education in reducing overall transmission of the virus. Schools allow students to meet and socialise in a controlled environment with infection prevention and control measures in place. As well as the negative consequences for student learning and wellbeing, closing schools might result in less efficient contact tracing and delayed testing.36 Also, students who are not socialising in school might over time find other areas to socialise, possibly with a higher risk of transmission of the virus.19 21 31 Transmission of the virus in schools cannot be separated from community transmission, and therefore combining school targeted strategies with general infection prevention and control measures for the whole community is crucial to limit transmission into, within, and outside schools.
Our overall results showed low attack rates in schools, but variation based on the characteristics of the index case was seen. Transmission rates were higher when a staff member, particularly a teacher, was the index case. After the alpha variant of the virus appeared and eventually dominated, we found no significant difference between these groups, however. This finding might be explained by increased transmissibility of the alpha variant of the virus across all age groups, including children.8 At the same time, vaccination of adults in high risk groups (ie, elderly people and people with underlying medical conditions at risk of severe covid-19, as well as healthcare staff) was started, which could have affected transmission rates in staff members or from adult family members to students. General first-dose vaccination of the working age population started at the end of our study period.37 Also, no covid-19 vaccines were approved for students or administered to students in our study population (aged ≤15 years) at that time. Hence we believe that vaccination rates had little effect on our results. The success of vaccination strategies will most likely be important for effective targeting of infection prevention and control measures in schools in the future.
Our study included data for primary and lower secondary schools only. Higher infection rates of SARS-CoV-2 were seen in older than in younger students during this period.38 Whether this finding translates into higher transmission rates in students and staff in upper secondary schools is unclear. Models made by the European Centre for Disease Prevention and Control showed that closing secondary schools had a larger effect on community transmission than closing primary schools or nurseries.8 School closures should be avoided as much as possible for all age groups, however, and more information on transmission of the virus in upper secondary schools is needed to help identify effective alternatives. Also, future studies should look at how vaccination coverage and more transmissible variants of the virus (such as the delta and omicron variants) affect transmission patterns in schools and households. Future topics for research include the potential wider implications of school transmission, such as the risk of introducing the virus to vulnerable family members.
Conclusion
During the academic year of 2020-21 in Norway, no subsequent individuals with covid-19 were found in most situations where SARS-CoV-2 was introduced into schools. Only a small proportion of all index cases led to clusters of three or more subsequent individuals with covid-19, and attack rates were generally low. These results suggest that primary and lower secondary schools, which were mainly kept open in Norway, were not important settings for transmission of SARS-CoV-2, when appropriate infection prevention and control measures were in place.
Acknowledgments
We thank our colleagues, especially Petter Elstrøm at the Norwegian Institute of Public Health, who have been part of the team handling the covid-19 situation at educational institutions, for valuable discussion on the topic.
Footnotes
Contributors: TAR, VBL, and KET conceptualised and developed the methodology of the study. TAR and VBL prepared the data and conducted the statistical analyses. TAR, VBL, and KET wrote the first draft of the manuscript, and EA and TBJ described infection prevention and control measures in schools. All authors contributed to the interpretation of results, as well as commenting on drafts and approving the final manuscript. The corresponding author (TAR) attests that all listed authors meet the authorship criteria. TAR is the guarantor. Transparency: The lead author (the guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Funding: The study was funded by the Norwegian Institute of Public Health, where the study was conducted. The institute had no direct role in the design and conduct of the study; compilation, analysis, and interpretation of data, writing of the manuscript, and decision to submit the manuscript for publication. No external funding was received.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from the Norwegian Institute for Public Health for the submitted work; PS has received a grant from the OAK Fellowships Programme in Molecular and Environmental Epidemiology (grant No OCAY-12-356) and has acted as an expert witness in court cases for the National Office for Health Service Appeals. No other author had financial relationships with any organisations that might have an interest in the submitted work in the previous three years or report other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. No additional data available. The datasets that support the findings of this study contain sensitive information and cannot be shared by the authors because of privacy laws. Individual level data for research are generally available within Norway on application, conforming with strict regulations and procedures.
Ethics approval
Institutional board review was conducted and the project was approved by the ethics committee of South-East Norway (9 March 2021, #198964). The emergency preparedness register, BEREDT C19, was established according to the Norwegian Health Preparedness Act sections 2-4.
References
- 1. National Collaborating Centre for Methods and Tools . Living rapid review update 17: what is the specific role of daycares and schools in COVID-19 transmission? Canada: McMaster University, 2021. [Google Scholar]
- 2. UNESCO . Global monitoring of school closures: UNESCO, 2020. Available: https://en.unesco.org/covid19/educationresponse#schoolclosures
- 3. UNICEF . COVID 19 and school closures; 2021. https://data.unicef.org/wp-content/uploads/2021/03/COVID19-and-school-closures-report.pdf
- 4. Viner RM, Bonell C, Drake L, et al. Reopening schools during the COVID-19 pandemic: governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Arch Dis Child 2021;106:111–3. 10.1136/archdischild-2020-319963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Viner RM, Russell S, Saulle R. Impacts of school closures on physical and mental health of children and young people: a systematic review. MedRxiv 2021. 10.1101/2021.02.10.21251526 [DOI] [Google Scholar]
- 6. Lewis SJ, Munro APS, Smith GD, et al. Closing schools is not evidence based and harms children. BMJ 2021;372:n521. 10.1136/bmj.n521 [DOI] [PubMed] [Google Scholar]
- 7. Engzell P, Frey A, Verhagen MD. Learning loss due to school closures during the COVID-19 pandemic. Proc Natl Acad Sci U S A 2021;118. 10.1073/pnas.2022376118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ECDC . COVID-19 in children and the role of school settings in transmission - second update. Stockholm: ECDC, 2021. [Google Scholar]
- 9. Buonsenso D, Roland D, De Rose C, et al. Schools closures during the COVID-19 pandemic: a catastrophic global situation. Pediatr Infect Dis J 2021;40:e146–50. 10.1097/INF.0000000000003052 [DOI] [PubMed] [Google Scholar]
- 10. Norwegian Institute of Public Health . Ukesrapport - uke 25 [Weekly report - week 25]. Oslo: Norwegian Institute of Public Health, 2021. [Google Scholar]
- 11. The Norwegian Directorate of Health . Operasjonalisering av testing, isolering, smittesporing og karantene (TISK) ved covid-19 i kommunene [Operationalization of testing, isolation, infection detection and quarantine (TISK) in cases of covid-19 in the municipalities]. Oslo: The Norwegian Directorate of Health, 2020. [Google Scholar]
- 12. The Norwegian Directorate of Health . Nivåinndeling av smitteverntiltak – trafikklysmodellen (barneskoler) [Levels of infection control measures - The traffic light model (primary schools)] Oslo: The Norwegian Directorate of Health, 2021. Available: https://www.helsedirektoratet.no/veiledere/smittevern-for-skoletrinn-1-7-covid-19/smitteforebyggende-tiltak/nivainndeling-av-smitteverntiltak-trafikklysmodell
- 13. The Norwegian Directorate of Health . Nivåinndeling av smitteverntiltak – trafikklysmodellen (ungdomsskoler) [Levels of infection control measures - The traffic light model (lower secondary schools)] Oslo: The Norwegian Directorate of Health, 2021. Available: https://www.helsedirektoratet.no/veiledere/smittevern-i-ungdomsskole-covid-19/smitteforebyggende-tiltak/nivainndeling-av-smitteverntiltak-trafikklysmodell
- 14. Norwegian Institute of Public Health . Emergency preparedness register for COVID-19 (Beredt C19) Oslo: Norwegian Institute of public health, 2020. Available: https://www.fhi.no/en/id/infectious-diseases/coronavirus/emergency-preparedness-register-for-covid-19/
- 15. The Norwegian Directorate for Education and Training . Fakta om grunnskolen 2020–21 [Facts about primary school 2020-21]: The Norwegian Directorate for Education and Training, 2021. Available: https://www.udir.no/tall-og-forskning/finn-forskning/tema/tall-om-grunnskolen-skolearet-202021/fakta-om-grunnskolen/#stabilt-elevtall-og-farre-og-storre-skoler
- 16. Centers for Disease Control and Prevention . Lesson 3: measures of risk: centers for disease control and prevention, 2012. Available: https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section2.html
- 17. Norwegian Institute of Public Health . Test criteria for coronavirus: Norwegian Institute of Public Health, 2020. Available: https://www.fhi.no/en/op/novel-coronavirus-facts-advice/testing-and-follow-up/test-criteria-for-coronavirus/
- 18. Madewell ZJ, Yang Y, Longini IM, et al. Household transmission of SARS-CoV-2: a systematic review and meta-analysis. JAMA Netw Open 2020;3:e2031756. 10.1001/jamanetworkopen.2020.31756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tian T, Huo X. Secondary attack rates of COVID-19 in diverse contact settings, a meta-analysis. J Infect Dev Ctries 2020;14:1361–7. 10.3855/jidc.13256 [DOI] [PubMed] [Google Scholar]
- 20. Koh WC, Naing L, Chaw L, et al. What do we know about SARS-CoV-2 transmission? A systematic review and meta-analysis of the secondary attack rate and associated risk factors. PLoS One 2020;15:e0240205. 10.1371/journal.pone.0240205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Telle K, Jørgensen SB, Hart R. Secondary attack rates of COVID-19 in Norwegian families: a nation-wide register-based study. Eur J Epidemiol 2021:1–8. 10.1007/s10654-021-00760-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gandini S, Rainisio M, Iannuzzo ML. No evidence of association between schools and SARS-CoV-2 second wave in Italy. MedRxiv 2020. 10.1101/2020.12.16.20248134 [DOI] [Google Scholar]
- 23. Zimmerman KO, Akinboyo IC, Brookhart MA, et al. Incidence and secondary transmission of SARS-CoV-2 infections in schools. Pediatrics 2021;147:e2020048090. 10.1542/peds.2020-048090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Macartney K, Quinn HE, Pillsbury AJ, et al. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child Adolesc Health 2020;4:807–16. 10.1016/S2352-4642(20)30251-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ehrhardt J, Ekinci A, Krehl H, et al. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in may 2020, Baden-Württemberg, Germany. Eurosurveillance 2020;25:2001587. 10.2807/1560-7917.ES.2020.25.36.2001587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schoeps A, Hoffmann D, Tamm C, et al. COVID-19 transmission in educational institutions August to December 2020, Rhineland-Palatinate, Germany: a study of index cases and close contact cohorts. medRxiv 2021. 10.2139/ssrn.3774830 [DOI] [Google Scholar]
- 27. Buonsenso D, De Rose C, Moroni R, et al. SARS-CoV-2 infections in Italian schools: preliminary findings after 1 month of school opening during the second wave of the pandemic. Front Pediatr 2020;8:615894. 10.3389/fped.2020.615894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. The Norwegian Directorate of Health . Smitteforebyggende tiltak [Infection prevention measures]: The Norwegian Directorate of Health, 2021. Available: https://www.helsedirektoratet.no/veiledere/smittevern-for-skoletrinn-1-7-covid-19/smitteforebyggende-tiltak
- 29. Aiano F, Mensah AA, McOwat K, et al. COVID-19 outbreaks following full reopening of primary and secondary schools in England: cross-sectional national surveillance, November 2020. The Lancet Regional Health - Europe 2021;6:100120. 10.1016/j.lanepe.2021.100120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alonso S, Alvarez-Lacalle E, Català M, et al. Age-dependency of the propagation rate of coronavirus disease 2019 inside school bubble groups in Catalonia, Spain. Pediatr Infect Dis J 2021;40:955. 10.1097/INF.0000000000003279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Thompson HA, Mousa A, Dighe A, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) setting-specific transmission rates: a systematic review and meta-analysis. Clin Infect Dis 2021;73:e754–64. 10.1093/cid/ciab100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Norwegian Institute of Public Health . Situational awareness and forecasting for Norway, week 35. Oslo: Norwegian Institute of Public Health, 2021. [Google Scholar]
- 33. Borgen NT, Raaum O, Kirkebøen LJ, et al. Heterogeneity in short- and long-term impacts of school-wide positive behavior support (SWPBS) on academic outcomes, behavioral outcomes, and criminal activity. J Res Educ Eff 2021;14:379–409. 10.1080/19345747.2020.1862375 [DOI] [Google Scholar]
- 34. World Health Organization . Infection prevention and control in the context of coronavirus disease (COVID-19): a living guideline, 25 April 2022: updated chapter: mask use, part 1: health care settings. World Health Organization, 2022. [Google Scholar]
- 35. Ford N, Holmer HK, Chou R, et al. Mask use in community settings in the context of COVID-19: a systematic review of ecological data. EClinicalMedicine 2021;38:101024. 10.1016/j.eclinm.2021.101024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Perramon A, Soriano-Arandes A, Pino D, et al. Schools as a framework for COVID-19 epidemiological surveillance of children in Catalonia, Spain: a population-based study. Front Pediatr 2021;9:754744. 10.3389/fped.2021.754744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Norwegian Institute of Public Health . Ukesrapport - uke 23 [Weekly report - week 23]. Oslo: Norwgian Institute of Public Health, 2021. [Google Scholar]
- 38. Leidman E, Duca LM, Omura JD, et al. COVID-19 trends among persons aged 0-24 years—united - United States, March 1-December 12, 2020. MMWR Morb Mortal Wkly Rep 2021;70:88. 10.15585/mmwr.mm7003e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjmed-2021-000026supp001.pdf (213.3KB, pdf)
Data Availability Statement
No data are available. No additional data available. The datasets that support the findings of this study contain sensitive information and cannot be shared by the authors because of privacy laws. Individual level data for research are generally available within Norway on application, conforming with strict regulations and procedures.