Abstract
Objective
To determine changes in industry marketing payments to physicians due to the covid-19 pandemic.
Design
Quasi experimental, difference-in-difference study.
Data source
US nationwide database of licensed physicians, the National Plan and Provider Enumeration System, which was linked to a database of industry marketing payments made to physicians, Open Payments.
Population
All licensed US physicians from 2018 to 2020 and those who received payments from industry.
Main outcome measures
Changes in the value and the number of monthly industry payments physician received before (January-February 2020) and during the pandemic (April-December 2020) were assessed, adjusting for physicians’ characteristics (gender and specialty). As the control, data for the same months in 2019 were used. Industry payments by type of payments (eg, meals, travel, consulting fees, speaker compensation, honorariums), were also examined.
Results
Among 880 589 US physicians included in this study, 267 463 (30.4%) physicians received a total of 4 117 482 non-research payments with $626 million ($710 per physician; £610; €708) in 2020 (40-44% decrease from $1047m in 2018 and $1115m in 2019). Industry payments decreased significantly in the months of the covid-19 pandemic (adjusted change in the value of −48.4%; 95% confidence interval −50.6 to −46.2; P<0.001; and adjusted change in the number of −47.4%, 95% confidence interval −47.7 to −47.1; P<0.001), particularly for meals and travel fees. No evidence was seen of a decrease in the number of industry payments for consulting and honorariums. A similar pattern was observed across physicians’ gender and specialty.
Conclusions
Industry payments to physicians, particularly those involving physical interactions such as meals and travel, substantially decreased during the pandemic. How such changes affect prescription practices and the quality of clinical practice in the long term should be investigated.
Keywords: Health policy
What is already known on this topic.
Financial relations between industry and physicians can influence clinical practice and physician prescription patterns
Some industry marketing involves physical interactions with physicians, the covid-19 pandemic might have altered the patterns of industry payments to physicians
What remains unknown, however, is whether and how the financial relations between industry and physicians have changed during the covid-19 pandemic
What this study adds
Across 880 589 physicians from a nationally representative database of industry marketing payments to physicians, the value and the number of industry payments to US physicians decreased substantially during the pandemic across all specialties, particularly those involving physical interactions, such as meals and travel fees
These results indicate that the pandemic affected the financial association between physicians and the pharmaceutical industry
How this study might affect research, practice, or policy
These difference-in-difference analyses highlight the importance to assess how the decline in industry payments during the pandemic could have influenced subsequent prescription patterns and patient outcomes, which should be the subject of future research
Close monitoring of whether the financial relations between industry and physician will return to the prepandemic state or whether some of these changes become permanent
Introduction
The covid-19 pandemic has brought unprecedented challenges to the world. In addition to the direct effect of covid-19 infection on people’s health, the pandemic has had numerous spillover effects mediated through changes in lifestyle, economic burden, and disruptions of the healthcare delivery system.1 In 2020 in the US, decreases of 12% in overall prescription volume and 37% in new prescription volume were reported, compared with those in 2019.2 Although the reduction in prescriptions could be influenced by multiple factors (eg, decreased office visits,3 4 initiation and proliferation of telemedicine,3 4 decreased prevalence of other communicable diseases,5 and restrained health seeking behavior6 during the pandemic), the underlying reasons for the change in physicians’ prescription behavior during the pandemic have not been fully elucidated.
One potential mechanism might be related to disruptions in the direct relations between the pharmaceutical industry and individual physicians. Since the establishment of the Open Payments program in 2013 under the Physician Payment Sunshine Act,7 ample evidence has shown that receipt of industry marketing payments influences physicians’ medication prescribing practices and increases the associated healthcare costs.8–12 This financial competing interest has been scrutinized heavily worldwide by policy makers and public health leaders alike, given the possibility of inappropriately influencing clinical decision making among physicians for monetary gain.13 14 Despite widespread concern and criticism, one study has shown that the amount of marketing payments related to the industry has remained stable between 2014 and 2018,15 indicating that increased transparency might not be sufficient to change physicians’ financial relations with the industry.
The covid-19 pandemic, however, substantially altered the healthcare delivery system and the associated activities that physicians normally engage in, such as local and national medical conferences, continuing medical education activities, and academic detailing events. To date, how this disruption might have influenced the interaction between the pharmaceutical industry and individual physicians is unclear. Physician and industry financial relations could have been drastically affected during the covid-19 pandemic, which could have led to a number of potential consequences, including the reduction of both appropriate and inappropriate medication prescriptions by individual physicians. This possible influence of industry payments on physician practicing behavior means that understanding how these financial associations have (or have not) changed during the covid-19 pandemic is critically important.
Therefore, using a national database of US physicians, we examined changes in the value and the number of industry payments made to physicians associated with the covid-19 pandemic compared with the prepandemic baseline using a quasi experimental, difference-in-difference study design. Given the heterogeneous role of each type of payment (eg, meals, travel, consulting fees, speaker compensation, honorariums), we also examined changes in industry payments by the type of payments. Furthermore, because the financial relations between physician and industry might vary by physicians’ gender and specialties,16–18 we investigated whether changes in industry payments due to the pandemic vary by physicians’ gender and specialty.
Methods
Data sources
We matched the Centres for Medicare and Medicaid Services' Open Payments databases in 2018-202019 to its National Plan and Provider Enumeration System (NPPES) database20 and collated physicians’ full name and the zip code for the primary practice location, as previous studies have done.16 18
Physician characteristics
We extracted information on physicians’ gender(male and female), specialty (taxonomy code), and practice location (US state) from the NPPES database. Physician specialty was classified into 32 categories; four in primary care physicians (internal medicine, family medicine, pediatrics, and hospitalist), nine in surgeons (obstetrics and gynecology, general, orthopedic, otolaryngology, urology, neurosurgery, plastic, thoracic and vascular, and colorectal), 18 in specialists (emergency medicine, psychiatry, anesthesiology, radiology, cardiology, ophthalmology, pediatric specialty, neurology, rehabilitation, dermatology, gastroenterology, hematology and oncology, nephrology, pulmonology, infectious diseases, endocrinology, rheumatology, and allergy and immunology), and one called others (eg, surgical oncology, oral surgery, radio oncology, pathology, and nuclear medicine). As a result of the variation of stay-at-home orders across states during the pandemic,21 information about practice location by state was also extracted from the NPPES database.
Payment data
We identified all non-research payments to physicians, which included non-research forms of payment such as meals, travel, consulting fees, speaker compensation, honorariums, and others (education, grant, gifts, entertainment, and space rental or facility fees). Research payments, royalty or license payments, and ownership interests, such as stocks and partnership shares, were not included in this analysis because these payments were not likely to be targeted to specific drugs at a specific time point. Payments are presented in nominal US dollars.
Statistical analysis
First, we examined the trends in the value and the number of industry payments between 2018 and 2020, according to the type of payments (ie, meals, travel, consulting, speaking fee, honorariums, and others). We then used a quasi experimental, difference-in-difference method22 23 to investigate changes in monthly industry payments due to the covid-19 pandemic. We compared before the pandemic (January-February 2020) to after (April-December 2020; March 2020 was excluded as the transition period) in 2020, using the same period in 2019 as the control, adjusting for physician characteristics (ie, gender, specialty, and US state). The changes in outcomes attributable to the covid-19 pandemic were represented by regression coefficients of the interaction terms between the year indicator (ie, 2019 v 2020) and the month indicator (ie, January-February v April-December) in the multivariable negative binomial models (to account for the distribution skewed to the right of the value and the number of industry payments). In all models, we adjusted for physicians’ gender, specialty, and the state in which the practice is located. We report difference-in-difference estimates in relative percentage changes as well as absolute changes in outcomes using average marginal effects. We found the average marginal effects by calculating the differences in predicted outcomes at each level of the interaction terms for each observation and averaging over the entire sample.24 The parallel trend assumption of the difference-in-difference model was formally tested.
Each type of industry marketing payment requires different resources and might have different influences on clinical practice,25 26 therefore, we stratified analyses by the type of payments (meals, travel, consulting fees, speaker compensation, honorariums, and others). Because the receipt of industry marketing payments also varies depending on physicians’ characteristics,16–18 we also stratified our analyses by physicians’ gender and specialties. Additionally, to assess whether the trends in industry payments during the pandemic vary by geographical regions, we stratified analyses by the four main areas (northeastern, midwestern, southern, and western regions) in the US according to the Census Bureau.27 P values were adjusted for multiple comparisons using the Benjamini-Hochberg method.28 Statistical analyses were done with Stata software version 16.0 (StataCorp, TX).
Sensitivity analysis
To evaluate the robustness of our findings, we carried out three main sensitivity analyses. We used the mean value and number of payments in 2018 and 2019 (instead of 2019 only) as the control group. We reanalyzed the data using ordinary least squares regression models with Huber-White robust standard errors adjusting for physicians’ characteristics. We also used the event study design23 29 to compare the change in the value and the number of industry marketing payments in the event year with the previous year as the control year. In the event study design, we used the multivariable negative binomial models, including indicator variables for time (reference category was defined as February—ie, a month before the event), a binary variable for the intervention year group (2018-19 v 2019-20), the interaction term between these two regressors, and physicians’ characteristics.
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. No patients were asked to advise on interpretation or writing up of results. We have no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
Physician characteristics
Across 1 029 149 physicians in the merged database, we excluded 148 541 physicians without information about practice location in the US. Of 785 237 physicians were unmatched in the Open Payments Profile database. We also excluded 19 physicians who received industry payments of more than $1 million (£850 000; €1 005 000) within a month (as outliers), resulting in the final analytical sample of 880 589 physicians. The flow of sample selection for the study is provided in online supplemental figure A. Among 880 589 physicians included in our study, 63.7% were men, 38.2% were primary care physicians, 16.8% were surgeons, and 39.5% were specialists (table 1). Surgeons and most of the specialists (except emergency medicine, psychiatry, anesthesiology, radiology, pediatric specialty, and rehabilitation) were likely to receive industry payments across 2018-20 (ie, they showed a larger proportion among physicians who received industry payments than the proportion among physicians in each specialty in the NPPES database). The distribution of physicians’ gender and specialty among physicians who received industry payments was similar across the study period.
Table 1.
Physician characteristics in the NPPES database and who received payments shown from the Open Payments database. Data are number (%) of physicians (%) unless stated otherwise
| Physician characteristics and specialty | Total No of physicians in NPPES | No of physicians who received industry payments between 2018 and 2020 | ||
| 2018 | 2019 | 2020 | ||
| No of physicians | 880 589 | 350 718 | 345 989 | 267 805 |
| Gender: | ||||
| Male | 560 707 (63.7) | 239 835 (68.4) | 235 633 (68.1) | 185 879 (69.4) |
| Female | 319 882 (36.3) | 110 883 (31.6) | 110 356 (31.9) | 81 926 (30.6) |
| Primary care: | ||||
| Internal medicine | 140 202 (15.9) | 54 336 (15.5) | 53 590 (15.5) | 41 719 (15.6) |
| Family medicine | 123 661 (14.0) | 46 804 (13.4) | 45 110 (13.0) | 34 870 (13.0) |
| Pediatrics | 62 959 (7.2) | 21 030 (6.0) | 20 362 (5.9) | 14 642 (5.5) |
| Hospitalist | 9307 (1.1) | 2780 (0.8) | 2925 (0.9) | 2119 (0.8) |
| Surgery: | ||||
| Obstetrics/gynecology | 44 310 (5.0) | 21 629 (6.2) | 21 107 (6.1) | 16 375 (6.1) |
| General | 36 635 (4.2) | 17 934 (5.1) | 17 966 (5.2) | 14 187 (5.3) |
| Orthopedic | 28 274 (3.2) | 17 362 (5.0) | 17 453 (5.0) | 14 675 (5.5) |
| Otolaryngology | 11 138 (1.3) | 6056 (1.7) | 6105 (1.8) | 4707 (1.8) |
| Urology | 10 941 (1.2) | 6780 (1.9) | 6693 (1.9) | 5699 (2.1) |
| Neurosurgery | 5921 (0.7) | 3455 (1.0) | 3434 (1.0) | 2882 (1.1) |
| Plastic | 4855 (0.6) | 2945 (0.8) | 2932 (0.9) | 2376 (0.9) |
| Thoracic and vascular | 3920 (0.5) | 2292 (0.7) | 2246 (0.7) | 1892 (0.7) |
| Colorectal | 1251 (0.1) | 781 (0.2) | 776 (0.2) | 620 (0.2) |
| Specialists: | ||||
| Emergency medicine | 53 637 (6.1) | 11 340 (3.2) | 11 380 (3.3) | 7867 (2.9) |
| Psychiatry | 52 469 (6.0) | 15 270 (4.4) | 15 084 (4.4) | 10 793 (4.0) |
| Anesthesiology | 42 482 (4.8) | 13 379 (3.8) | 13 391 (3.9) | 8918 (3.3) |
| Radiology | 30 373 (3.5) | 7325 (2.1) | 7303 (2.1) | 4857 (1.8) |
| Cardiology | 22 362 (2.5) | 14 716 (4.2) | 14 402 (4.2) | 12 438 (4.6) |
| Ophthalmology | 20 781 (2.4) | 11 969 (3.4) | 12 013 (3.5) | 10 388 (3.9) |
| Pediatric specialty | 19 239 (2.2) | 5617 (1.6) | 5523 (1.6) | 3637 (1.4) |
| Neurology | 15 677 (1.8) | 7948 (2.3) | 7979 (2.3) | 6334 (2.4) |
| Rehabilitation | 14 016 (1.6) | 3945 (1.1) | 3842 (1.1) | 2833 (1.1) |
| Dermatology | 13 669 (1.6) | 7791 (2.2) | 7805 (2.3) | 6682 (2.5) |
| Gastroenterology | 12 906 (1.5) | 8262 (2.4) | 7926 (2.3) | 6635 (2.5) |
| Hematology and oncology | 11 527 (1.3) | 6732 (1.9) | 6472 (1.9) | 5368 (2.0) |
| Nephrology | 8457 (1.0) | 4786 (1.4) | 4833 (1.4) | 3828 (1.4) |
| Pulmonology | 7289 (0.8) | 4041 (1.2) | 3977 (1.2) | 3386 (1.3) |
| Infectious diseases | 6065 (0.7) | 2512 (0.7) | 2491 (0.7) | 1957 (0.7) |
| Endocrinology | 5910 (0.7) | 3359 (1.0) | 3275 (1.0) | 2679 (1.0) |
| Rheumatology | 4794 (0.5) | 2749 (0.8) | 2651 (0.8) | 2249 (0.8) |
| Allergy and immunology | 4240 (0.5) | 2407 (0.7) | 2335 (0.7) | 1975 (0.7) |
| Others* | 51 322 (5.8) | 12 386 (3.5) | 12 608 (3.6) | 8218 (3.1) |
NPPES=National Plan and Provider Enumeration System.
*Others include surgical oncology, oral surgery, radio oncology, pathology, and nuclear medicine.
bmjmed-2022-000219supp001.pdf (1.4MB, pdf)
Industry payments between 2018 and 2020
In 2020, 267 463 physicians in the US received 4 117 482 non-research payments (except royalty, license, and ownership interests) to the value of $626m, which was a 40-44% reduction from $1115m in 2019 and $1047m in 2018 (table 2). From 2018 to 2020, meals constituted 90% of the total number of industry payments, and speaking fees constituted the largest value of payments (35-38%). The proportion of travel fees decreased in 2020 compared with previous years for both the number (5.1% in 2018, 5.6% in 2019, and 2.7% in 2020) and the value (12.1% in 2018, 12.4% in 2019, and 5.0% in 2020) of payments.
Table 2.
Changes in industry payments to physicians between 2018 and 2020
| Types of industry payments | 2018 | 2019 | 2020 |
| Total* | |||
| No of physicians | 350 520 | 345 789 | 267 463 |
| No of payments | 7 761 986 | 7 492 724 | 4 117 482 |
| Total payment value | $1047 million | $1115 million | $626 million |
| Type of non-research payments | |||
| Meals: | |||
| No of physicians | 342 178 | 337 595 | 254 448 |
| No (%) of payments | 6 915 047 (89.1) | 6 642 500 (88.7) | 3 710 716 (90.1) |
| Total payment value (% of main total) | $162 million (15.5) | $163 million (14.6) | $78 million (12.5) |
| Travel: | |||
| No of physicians | 44 709 | 45 458 | 20 204 |
| No (%) of payments | 396 793 (5.1) | 422 708 (5.6) | 112 314 (2.7) |
| Total payment value (% of main total) | $127 million (12.1) | $138 million (12.4) | $31 million (5.0) |
| Consulting: | |||
| No of physicians | 21 242 | 23 435 | 19 054 |
| No (%) of payments | 96 215 (1.2) | 99 859 (1.3) | 93 460 (2.3) |
| Total payment value (% of main total) | $290 million (27.7) | $305 million (27.4) | $240 million (38.3) |
| Speaking fee | |||
| No of physicians | 21 947 | 20 172 | 16 317 |
| No (%) of payments | 174 745 (2.3) | 179 202 (2.4) | 128 550 (3.1) |
| Total payment value (% of main total) | $393 million (37.5) | $421 million (37.8) | $217 million (34.7) |
| Honorariums | |||
| No of physicians | 3812 | 4331 | 3548 |
| No (%) of payments | 10 733 (0.1) | 12 782 (0.2) | 10 367 (0.3) |
| Total payment value (% of main total) | $27 million (2.6) | $31 million (2.8) | $19 million (3.0) |
| Others† | |||
| No of physicians | 79 718 | 76 435 | 43 983 |
| No (%) of payments | 168 453 (2.2) | 135 673 (1.8) | 62 075 (1.5) |
| Total payment value (% of main total) | $47 million (4.5) | $57 million (5.1) | $40 million (6.4) |
$1.00=£0.86; €1.00.
*Research payments, royalty, or license, and ownership interests such as stocks and partnership shares were not included in this analysis.
†Others include education, grant, gifts, entertainment, and space rental or facility fees.
Change in the value of industry payments
The unadjusted monthly trends in the value of industry payments between 2018 and 2020 are shown in figure 1 (top panel). The results of the tests for the parallel trend assumption can be found in online supplemental table A. We found a significant decline in the monthly value of payments due to the covid-19 pandemic (adjusted percentage change of −48.4%; 95% confidence interval −50.6% to −46.2%; P<0.001; and adjusted absolute change of −$75.7, 95% confidence interval −81.2 to −70.3; P<0.001; table 3). We also found a significant reduction in the value of payments during the pandemic across any types of payments except others (table 3, online supplemental figure B). We found no evidence that changes in the value of payments due to the pandemic varied by gender (online supplemental table B). When we stratified by physicians’ specialty, the change was noted across all specialties, with the largest reduction among neurologists and rheumatologists on both the relative and the absolute scales compared with internal medicine physicians. The decline in the value of industry payments was consistently found across all regions in the US (online supplemental table C).
Figure 1.
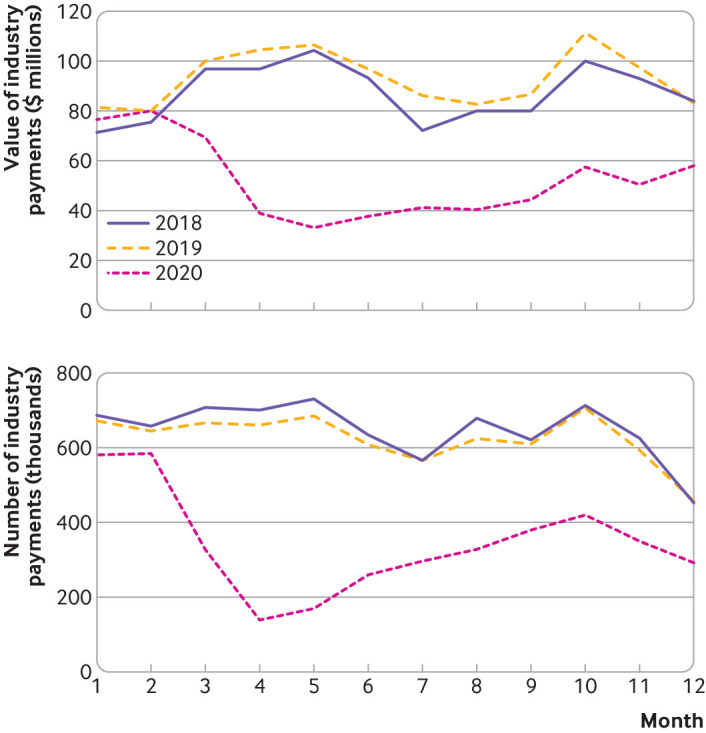
Overall monthly trends in the value and number of industry payments to physicians between 2018 and 2020. $1.00=£0.86; €1.00
Table 3.
Difference-in-difference estimates of adjusted change in value and number of industry payments per physician during the covid-19 pandemic (ie, January-February v April-December in 2020) compared with 2019 according to the type of payments
| Type of payment | Value of industry payments per physician (95% CI) | No of industry payments per 100 physicians (95% CI) | ||||
| Relative % change | Absolute $ change | Adjusted P value | Relative % change | Absolute change | Adjusted P value | |
| Total | −48.4 (−50.6 to −46.2) | −75.7 (−81.2 to −70.3) | <0.001 | −47.4 (−47.7 to −47.1) | −43.6 (−44.2 to −43.0) | <0.001 |
| Meal | −63.9 (−64.3 to −63.5) | −14.9 (−15.1 to −14.7) | <0.001 | −46.0 (−46.3 to −45.7) | −37.0 (−37.5 to −36.5) | <0.001 |
| Travel | −93.8 (−94.3 to −93.3) | −19.3 (−20.4 to −18.2) | <0.001 | −91.5 (−91.9 to −91.0) | −5.9 (−6.1 to −5.7) | <0.001 |
| Consulting | −15.7 (−23.5 to −6.9) | −6.7 (−10.8 to −2.7) | <0.001 | 6.6 (1.8 to 11.6) | 0.1 (0.0 to 0.1) | 0.01 |
| Speaking fee | −36.3 (−41.4 to −30.7) | −13.1 (−15.7 to −10.5) | <0.001 | −34.4 (−36.8 to −31.8) | −0.9 (−0.9 to −0.8) | <0.001 |
| Honorariums | −48.5 (−55.9 to −39.9) | −2.3 (−2.9 to −1.7) | <0.001 | 7.9 (−28.8 to 63.5) | 0.0 (−0.1 to 0.1) | 0.72 |
| Others | −12.0 (−29.8 to 10.4) | −1.1 (−2.8 to 0.6) | 0.27 | −25.7 (−28.7 to −22.6) | −0.1 (−0.1 to 0.0) | <0.001 |
Difference-in-difference estimates in relative percentage changes were calculated by regression coefficients of the interaction terms between the year indicator (ie, 2019 v 2020) and the month indicator (ie, January-February v April-December) in the multivariable negative binomial models adjusting for physicians’ gender, specialty, and practice location. The adjusted absolute changes in outcomes were estimated by calculating the differences in predicted outcomes at each level of the interaction terms for each observation and averaging over the entire sample. P value was adjusted for multiple comparisons using the Benjamini-Hochberg method.
CI=confidence interval.
Changes in the number of industry payments
The unadjusted monthly trends in the number of industry payments between 2018 and 2020 are shown in figure 1 (bottom panel). We found a significant decline in the monthly number of payments per 100 physicians due to the covid-19 pandemic (adjusted percentage change of −47.4%; 95% confidence interval −47.7 to −47.1; P<0.001; and adjusted absolute change of −43.6, 95% confidence interval −44.2 to −43.0; P<0.001; table 3). Although we found a significant reduction in the number of payments, particularly for meals, travel fees, and speaking fees, the reduction was not observed for consulting and honorariums (table 3, online supplemental figure C). We found no evidence that changes in the number of payments due to the pandemic varied by gender (online supplemental table D). When we stratified by physicians’ specialty, most surgeons and specialists, except rehabilitation physicians and pulmonologists, showed a larger reduction on the relative scale during the pandemic compared with physicians in internal medicine (a specialty with the highest proportion among US physicians). The reduction in the number of industry payments was consistently noted across all regions in the US (online supplemental table C).
Sensitivity analyses
The results did not qualitatively change when we used the average value and number of payments in 2018 and 2019 instead of 2019 only (online supplemental table E) and when we reanalyzed the data using ordinary least squares instead of the negative binomial model (online supplemental table F). Our findings were also supported by the event study design, which provided visual evidence to show that the industry marketing payments dropped at the event month (ie, pandemic in March 2020; figure 2).
Figure 2.
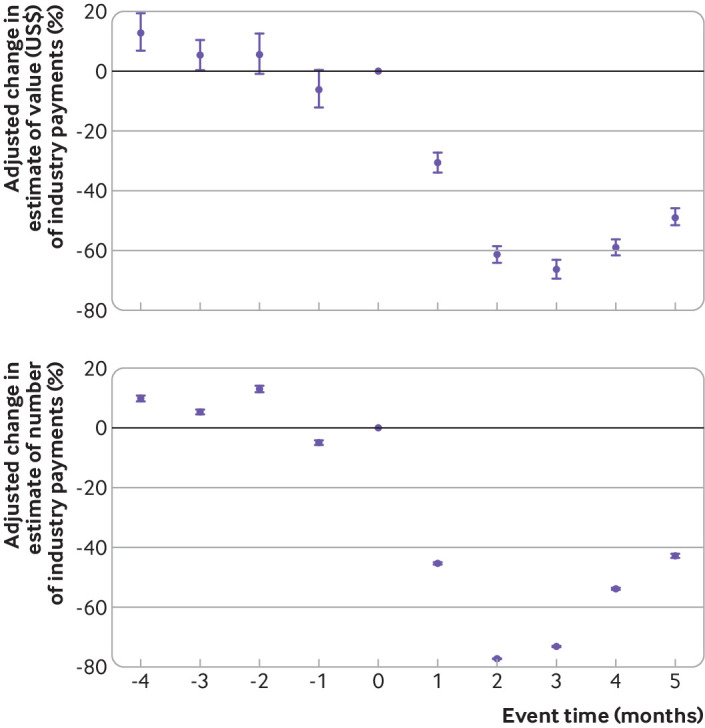
Adjusted change (%) in estimates of the value and the number of industry payments per physician between 2018-19 and 2019-20 before and after the pandemic. The intervention year was 2019-20, and the control period included 2018-19. Reference of event time was set to February (a month before the pandemic in 2020). Multivariable negative binomial regression models were used to calculate percentage change in the estimate (ie, (coefficient−1)×100) adjusting for physicians’ gender, specialty, and practice location
Discussion
Principal findings
Using national data for industry marketing payments to US physicians, we found that the value and the number of the payments significantly declined by almost half during the covid-19 pandemic. A similar pattern was observed across physicians’ gender, all specialties, and regions in the US. To our knowledge, this study is the first to elucidate how the covid-19 pandemic has changed the relations between industry and physicians. Given that the reduction in these payments was the largest among those related to meals and travel fees, this effect was observed partially due to restricted in-person interactions during the pandemic. Our findings should be informative for policy makers interested in understanding the financial association between industry and physicians, and how these changes might eventually affect individual physicians’ prescription practice and patient outcomes, which should be the subject of future research.
The possible influence of the financial association between the pharmaceutical industry and physicians has received great concern,30 mainly because inappropriate prescriptions could have been introduced through misguided information and potential financial competing interests. For example, a previous study showed that physicians who received meals sponsored by the pharmaceutical industry were more likely to prescribe brand name drug than generic alternatives.31 Additionally, the receipt of the industry payments related to opioids was associated with increased prescription of opioids and opioid overdose deaths, indicating the possible over prescription of opioids related to the industry marketing.32–34 However, industry marketing to physicians might also have positive aspects related to continuing medical education activities. Across the US, the pharmaceutical industry often engages and supports the provision of educational opportunities for physicians to obtain the latest evidence on old and new drugs. For example, a previous work focusing on a new cardiovascular drug that was under strict prior-authorization requirements indicated that industry marketing to physicians might have contributed to facilitating the judicious and early adoption of the high-cost but effective drugs as a key driver of their prescribing behavior.26
Of note, we found the largest reduction in the value and the number of industry payments in the form of meals and travel fees during the pandemic. Previous studies have consistently shown that meals constituted more than 90% of the total number of industry payments.11 26 These studies suggested that encounters with industry marketing, even in the inexpensive form of meals, drive prescriptions, possibly through educational opportunities, drive sharing updated information on the drug, and improve physicians’ familiarity with the drug.11 26 31 Our findings indicate that these educational opportunities have been reduced due to the physical restrictions enforced during the pandemic and cancellations of local and national medical conferences. Although a decrease in revenues could also be a reason for decreased marketing, the average profit margin of pharmaceutical industries did not decrease during the pandemic.35 Because this trend might be affected by profits related to covid-19 for some specific pharmaceutical organizations, future research is needed to assess whether and to what extent the change in revenues of each organization influences their financial relations with physicians.
We did not find a reduction in the number of payments for consulting and honorariums. These payments do not necessarily require physical interactions between the pharmaceutical industry and physicians. Because consulting and honorariums are likely to be targeted to key opinion leaders (whereas meals are generally targeted to a broad type of physicians), the possible influence of the pandemic on prescription patterns through reduced industry marketing payments needs to be carefully assessed and monitored according to physicians’ role in academia or clinical practice.
The reduction in industry payments during the pandemic was consistently observed, even when categorized by physician gender and across all physician specialties and geographical regions in the US. Although the absolute reductions in the value and the number of payments were larger in male physicians than in female physicians, this amount is probably because male physicians are generally more likely to receive industry payments than female physicians at baseline (ie, before the pandemic),16–18 and the relative reduction was similar between physicians’ gender. Our consistent findings of the stratified analyses by physician specialties indicate that the pandemic has influenced the interaction between the pharmaceutical industry and individual physicians regardless of their specialties.
Limitations of the study
Our study has limitations. First, although we used the nationwide database of licensed US physicians (NPPES), the matching rate of physicians in the Open Payments database to the NPPES database was 88%; thus, we might not be able to capture all physicians who received industry marketing payments in the US. Second, measurement error is a possibility due to misreporting or under-reporting of payments. However, this bias would be small given the effort by the Centres for Medicare and Medicaid Services to improve the accuracy of the Open Payments data (eg, encouraging all physicians to review the information, facilitating education activities to increase awareness of the program), making the database comprehensive and reliable.7 Third, because the present study focused on non-research payments, our findings might not be generalizable to other forms of payments such as ownership interests, royalty, and license payments. These types of payments are targeted to a small number of physicians18 and not specific to a drug at a specific time,19 thus beyond the scope of this study. Finally, because data for physicians’ prescription and patients’ outcomes during the covid-19 pandemic are not publicly available yet, we could not evaluate these outcomes via the decreased industry marketing payments, which should be the subject of future research.
Conclusions
Using a nationally representative database of US physicians, we found that the pharmaceutical industry marketing payments to physicians, particularly those involving physical interactions such as meals and travel fees, substantially decreased during the covid-19 pandemic. Our findings highlight the need to closely monitor how this might have influenced subsequent prescription patterns, physicians’ medical education on drug related evidence to date, and, importantly, patient outcomes. Policy makers and public health leaders must continue to monitor whether the financial relations between industry and physician will return to the prepandemic state as the covid-19 pandemic eases or whether some of these changes will become permanent.
Footnotes
Twitter: @ki_endoepi, @ytsugawa1
Contributors: KI and YT conceived the concept and design. KI, JFF, NK, and YT were responsible for acquisition, analysis, or interpretation of data. KI and YT drafted the manuscript. KI, JFF, NK, and YT critically revised the manuscript for important intellectual content. KI is the guarantor and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors assume full responsibility for the accuracy and completeness of the ideas presented. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. Transparency: The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Funding: KI was supported by the Japan Society for the Promotion of Science (JSPS; 21K20900 and 22K17392). NK was supported by JSPS (18H04071) and the Ministry of Health, Labour and Welfare, Japan (19FA1012, 19FA2001). YT was supported by the National Institutes of Health (NIH)/National Institute on Minority Health and Health Disparities grant R01MD013913 and NIH/National Institute on Aging grant R01AG068633 for other work not related to this study. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Disclaimer: This article does not necessarily represent the views and policies of the NIH. Study sponsors were not involved in study design, data interpretation, writing, or the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. No additional data available.
Ethics approval
The study was exempted by the institutional review board at the University of California, Los Angeles (IRB#18–0 01 960) and Kyoto University (IRB#R3067).
References
- 1. Banerjee A, Pasea L, Harris S, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet 2020;395:1715–25. 10.1016/S0140-6736(20)30854-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Monitoring the impact of COVID-19 on the pharmaceutical market. Available: https://www.iqvia.com/library/white-papers/monitoring-the-impact-of-covid-19-on-the-pharmaceutical-market [Accessed 18 Jul 2021].
- 3. Hollander JE, Carr BG. Virtually perfect? telemedicine for Covid-19. N Engl J Med 2020;382:1679–81. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 4. Baum A, Kaboli PJ, Schwartz MD. Reduced In-Person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med 2021;174:129-131. 10.7326/M20-3026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rubin R. Influenza's unprecedented low profile during COVID-19 pandemic leaves experts Wondering what this flu season has in store. JAMA 2021;326:899–900. 10.1001/jama.2021.14131 [DOI] [PubMed] [Google Scholar]
- 6. Tan HMJ, Tan MS, Chang ZY, et al. The impact of COVID-19 pandemic on the health-seeking behaviour of an Asian population with acute respiratory infections in a densely populated community. BMC Public Health 2021;21:1196. 10.1186/s12889-021-11200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agrawal S, Brown D. The Physician Payments Sunshine Act--Two Years of the Open Payments Program. N Engl J Med 2016;374:906–9. 10.1056/NEJMp1509103 [DOI] [PubMed] [Google Scholar]
- 8. Mitchell AP, Trivedi NU, Gennarelli RL, et al. Are Financial Payments From the Pharmaceutical Industry Associated With Physician Prescribing? : A Systematic Review. Ann Intern Med 2021;174:353–61. 10.7326/M20-5665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fleischman W, Agrawal S, King M, et al. Association between payments from manufacturers of pharmaceuticals to physicians and regional prescribing: cross sectional ecological study. BMJ 2016;354:i4189. 10.1136/bmj.i4189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hadland SE, Cerdá M, Li Y, et al. Association of pharmaceutical industry marketing of opioid products to physicians with subsequent opioid prescribing. JAMA Intern Med 2018;178:861–3. 10.1001/jamainternmed.2018.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Inoue K, Tsugawa Y, Mangione CM, et al. Association between industry payments and prescriptions of long-acting insulin: an observational study with propensity score matching. PLoS Med 2021;18:e1003645. 10.1371/journal.pmed.1003645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mejia J, Mejia A, Pestilli F. Open data on industry payments to healthcare providers reveal potential hidden costs to the public. Nat Commun 2019;10:1–8. 10.1038/s41467-019-12317-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Campbell EG, Doctors CEG. Doctors and drug companies--scrutinizing influential relationships. N Engl J Med 2007;357:1796–7. 10.1056/NEJMp078141 [DOI] [PubMed] [Google Scholar]
- 14. Schwartz LM, Woloshin S. Medical marketing in the United States, 1997-2016. JAMA 2019;321:80–96. 10.1001/jama.2018.19320 [DOI] [PubMed] [Google Scholar]
- 15. Marshall DC, Tarras ES, Rosenzweig K, et al. Trends in industry payments to physicians in the United States from 2014 to 2018. JAMA 2020;324:1785. 10.1001/jama.2020.11413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tringale KR, Marshall D, Mackey TK, et al. Types and distribution of payments from industry to physicians in 2015. JAMA 2017;317:1774–84. 10.1001/jama.2017.3091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brunt CS. Physician characteristics, industry transfers, and pharmaceutical prescribing: empirical evidence from Medicare and the physician payment sunshine act. Health Serv Res 2019;54:636–49. 10.1111/1475-6773.13064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Inoue K, Blumenthal DM, Elashoff D, et al. Association between physician characteristics and payments from industry in 2015-2017: observational study. BMJ Open 2019;9:e031010. 10.1136/bmjopen-2019-031010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Centers for Medicare & Medicaid Services . Open payments. Available: https://www.cms.gov/OpenPayments [Accessed 17 Dec 2019].
- 20. Centers for Medicare & Medicaid Services . National Plan and Provider Enumeration System (NPPES) National Provider Identifier registry. Available: https://npiregistry.cms.hhs.gov/ [Accessed 17 Dec 2019].
- 21. Moreland A. Timing of state and territorial COVID-19 Stay-at-Home orders and changes in population movement — United States, March 1–May 31, 2020. MMWR Morb Mortal Wkly Rep 2020:69. 10.15585/mmwr.mm6935a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA 2014;312:2401–2. 10.1001/jama.2014.16153 [DOI] [PubMed] [Google Scholar]
- 23. Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health 2018;39:453–69. 10.1146/annurev-publhealth-040617-013507 [DOI] [PubMed] [Google Scholar]
- 24. Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J 2012;12:308–31. 10.1177/1536867X1201200209 [DOI] [Google Scholar]
- 25. Yeh JS, Franklin JM, Avorn J, et al. Association of industry payments to physicians with the prescribing of brand-name statins in Massachusetts. JAMA Intern Med 2016;176:763–8. 10.1001/jamainternmed.2016.1709 [DOI] [PubMed] [Google Scholar]
- 26. Inoue K, Figueroa JF, DeJong C, et al. Association between industry marketing payments and prescriptions for PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitors in the United States. Circ Cardiovasc Qual Outcomes 2021;14:e007521. 10.1161/CIRCOUTCOMES.120.007521 [DOI] [PubMed] [Google Scholar]
- 27. Bureau UC . Geographic levels. Census.gov. Available: https://www.census.gov/programs-surveys/economic-census/guidance-geographies/levels.html [Accessed 31 May 2022].
- 28. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B 1995;57:289–300. 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- 29. Campbell JY, AW L, MacKinlay AC. 4. Event-Study Analysis in “The Econometrics of Financial Markets.” Princeton University Press; 2012:149-180. Available: https://www.degruyter.com/document/doi/10.1515/9781400830213-008/html [Accessed 18 Jul 2021].
- 30. Bekelman JE, Li Y, Gross CP. Scope and impact of financial conflicts of interest in biomedical research: a systematic review. JAMA 2003;289:454–65. 10.1001/jama.289.4.454 [DOI] [PubMed] [Google Scholar]
- 31. DeJong C, Aguilar T, Tseng C-W, et al. Pharmaceutical industry-sponsored meals and physician prescribing patterns for Medicare beneficiaries. JAMA Intern Med 2016;176:1114–22. 10.1001/jamainternmed.2016.2765 [DOI] [PubMed] [Google Scholar]
- 32. Hadland SE, Rivera-Aguirre A, Marshall BDL, et al. Association of pharmaceutical industry marketing of opioid products with mortality from Opioid-Related overdoses. JAMA Netw Open 2019;2:e186007. 10.1001/jamanetworkopen.2018.6007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nguyen TD, Bradford WD, Simon KI. Pharmaceutical payments to physicians may increase prescribing for opioids. Addiction 2019;114:1051–9. 10.1111/add.14509 [DOI] [PubMed] [Google Scholar]
- 34. Inoue K, Figueroa JF, Orav EJ, et al. Association between industry payments for opioid products and physicians' prescription of opioids: observational study with propensity-score matching. J Epidemiol Community Health 2020;74:jech-2020-214021–654. 10.1136/jech-2020-214021 [DOI] [PubMed] [Google Scholar]
- 35. Hawksbee L, McKee M, King L. Don't worry about the drug industry's profits when considering a waiver on covid-19 intellectual property rights. BMJ 2022;376:e067367. 10.1136/bmj-2021-067367 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjmed-2022-000219supp001.pdf (1.4MB, pdf)
Data Availability Statement
No data are available. No additional data available.


