Abstract
Background
In addition to the role of vitamin D in bone mineralization, calcium and phosphate homeostasis, and skeletal health, evidence suggests an association between vitamin D deficiency and a wide range of chronic conditions. This is of clinical concern given the substantial global prevalence of vitamin D deficiency. Vitamin D deficiency has traditionally been treated with vitamin D3 (cholecalciferol) or vitamin D2 (ergocalciferol). Calcifediol (25-hydroxyvitamin D3) has recently become available more widely.
Methods
By means of targeted literature searches of PubMed, this narrative review overviews the physiological functions and metabolic pathways of vitamin D, examines the differences between calcifediol and vitamin D3, and highlights clinical trials conducted with calcifediol in patients with bone disease or other conditions.
Results
For supplemental use in the healthy population, calcifediol can be used at doses of up to 10 µg per day for children ≥ 11 years and adults and up to 5 µg/day in children 3−10 years. For therapeutic use of calcifediol under medical supervision, the dose, frequency and duration of treatment is determined according to serum 25(OH)D concentrations, condition, type of patient and comorbidities. Calcifediol differs pharmacokinetically from vitamin D3 in several ways. It is independent of hepatic 25-hydroxylation and thus is one step closer in the metabolic pathway to active vitamin D. At comparable doses to vitamin D3, calcifediol achieves target serum 25(OH)D concentrations more rapidly and in contrast to vitamin D3, it has a predictable and linear dose–response curve irrespective of baseline serum 25(OH)D concentrations. The intestinal absorption of calcifediol is relatively preserved in patients with fat malabsorption and it is more hydrophilic than vitamin D3 and thus is less prone to sequestration in adipose tissue.
Conclusion
Calcifediol is suitable for use in all patients with vitamin D deficiency and may be preferable to vitamin D3 for patients with obesity, liver disease, malabsorption and those who require a rapid increase in 25(OH)D concentrations.
Keywords: Vitamin D deficiency; Calcifediol; Cholecalciferol; Immunomodulatory; 25-Hydroxyvitamin D3; 1,25-Dihydroxyvitamin D3
Introduction
Vitamin D is known to play an important role in bone mineralization, calcium and phosphate homeostasis, and skeletal health. The link between vitamin D deficiency and rickets, osteomalacia and osteoporosis is well established [1–3]. Nowadays, there is growing interest in the potential role of vitamin D in multiple other body functions. Evidence suggests an association between vitamin D deficiency and cardiovascular disease, selected cancers, autoimmune diseases (e.g., multiple sclerosis, type 1 diabetes and rheumatoid arthritis), pulmonary disorders (e.g., asthma and chronic obstructive pulmonary disease), and upper respiratory infections (e.g., influenza, COVID-19), including potential causal relationships with some of these outcomes [4–8].
The two commonly available forms of vitamin D supplement for maintaining vitamin D status or treating vitamin D deficiency or insufficiency are ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3) [1]. In Spain, calcifediol (a vitamin D3 metabolite) has been used for these same purposes for more than 40 years and recently became available in several other European countries (e.g., Poland, The Netherlands, Belgium) and in Latin America (e.g., Chile, Colombia, Ecuador, Peru, Mexico).
This narrative review provides an overview of the physiological functions and metabolic pathways of vitamin D, examines the differences between calcifediol and vitamin D3, and highlights clinical trials conducted with calcifediol in patients with bone disease or other conditions. To identify relevant published data, targeted literature searches of PubMed were conducted using the terms ‘vitamin D deficiency’ and ‘calcifediol’ and ‘cholecalciferol’; as well as ‘calcifediol’ and specific disease conditions of interest using the key words ‘bone disease’, ‘Paget’s ‘osteoporosis’, ‘osteomalacia’, ‘osteopenia’, ‘falls’, ‘muscle’, ‘immune system’, ‘asthma’, ‘COVID-19’ and ‘secondary hyperparathyroidism’, applying the ‘Clinical Trials’ filter to individual searches. Additional articles were identified from the reference lists of published articles or were known to the authors. Searches were last updated 24 January 2022.
Physiology of vitamin D
Characterized initially as a vitamin, vitamin D is now also recognized as a prohormone [9]. Vitamin D consists of two forms, vitamin D2 and vitamin D3, both of which contribute to overall vitamin D status [10, 11]. Sunlight accounts for more than 90% of the body’s daily requirement of vitamin D under normal physiological conditions. Exposure to ultraviolet B radiation converts 7-dehydrocholesterol in the skin to previtamin D3 which undergoes thermal conversion to form vitamin D3. Other sources of vitamin D3 are foods such as oily fish (e.g., wild salmon, mackerel etc.), cod liver oil and egg yolks [1, 2]. Vitamin D2 is present in UV-exposed mushrooms (e.g., oyster, shiitake mushrooms) [12] and is produced from irradiation of yeast. Vitamins D2 and D3 are both used to fortify foods (e.g., milk, margarine, yogurts, breakfast cereals, cooking oil) and as dietary supplements [1, 10, 13–15]. In 2021, calcifediol received a positive evaluation by EFSA for use in the European Union as an additive in food supplements targeting the healthy population at doses of up to 10 µg per day for children ≥ 11 years and adults, including pregnant and lactating women, and up to 5 µg/day in children 3−10 years. European Commission approval is pending [16].
Irrespective of source, vitamin D2 and vitamin D3 must undergo a two-step enzymatic process to become biologically active (Fig. 1). First, liver 25-hydroxylases (of the cytochrome P450 group) convert these inert prohormones to 25-hydroxyvitamin D2 [25(OH)D2] and 25-hydroxyvitamin D3 [25(OH)D3, calcifediol], respectively. The composite of 25(OH)D2 and 25(OH)D3 is reported for clinical purposes as the total serum 25-hydroxyvitamin D [25(OH)D] concentration and is the biomarker of vitamin D status. Next, 1α-hydroxylases in the kidneys covert the 25-hydroxylated vitamin D2 and vitamin D3 to 1,25-dihydroxyvitamin D2 [1,25(OH)2D2] and 1,25-dihydroxyvitamin D3 [1,25(OH)2D3, calcitriol], respectively [1, 10, 13–15], which are collectively referred to as 1,25-dihydroxyvitamin D [1,25(OH)2D].
Fig. 1.
Vitamin D activation pathway
1,25(OH)2D is the biologically active form of vitamin D. 1,25(OH)2D regulates calcium homeostasis by acting on its intestinal absorption, renal reabsorption, and bone mobilization [1, 9]. A reduction in serum calcium concentrations stimulates secretion of parathyroid hormone (PTH), which activates synthesis of 1,25(OH)2D. Conversely, an increase in serum calcium concentrations reduces PTH secretion and decreases the synthesis of 1,25(OH)2D. Phosphate homeostasis is maintained through intestinal phosphate absorption, renal phosphate reabsorption or excretion and/or bone metabolism. The processes are regulated by PTH, 1,25(OH)2D, and bone-derived fibroblast growth factor 23 (FGF23) via several negative feedback loops [17, 18]. In response to hyperphosphatemia, FGF23 suppresses phosphate reabsorption and 1,25(OH)2D synthesis in the kidneys [19]. FGF23 excess is associated with phosphate-wasting disorders (e.g., hypophosphatemic rickets and tumor-induced osteomalacia) and chronic kidney disease, although the hormone also has a role in normal physiological processes in bone and kidney [19].
1,25(OH)2D activity is mediated by the vitamin D specific receptor (VDR), a ligand-dependent transcription regulator molecule belonging to the nuclear receptor superfamily. The presence of VDR in most cells may explain the activity of vitamin D at different tissue sites, including its immunomodulatory effects [1, 4, 6, 9, 20, 21]. In this regard, VDR expression and activity play an important role in T-cell development, differentiation, and function [21]. Acting via the VDR, 1,25(OH)2D suppresses parathyroid gene expression and blocks chief cell proliferation to facilitate the maintenance of optimal serum calcium concentrations [9]. 1,25(OH)2D also increases the intestinal absorption of calcium by interacting with the VDR to enhance expression of the epithelial calcium channel and calcium binding protein [1]. 25(OH)D has also been shown to bind to and activate the VDR, although not as strongly as 1,25(OH)2D [22, 23]. Regulation of renal 1,25(OH)2D production may also directly or indirectly influence the activity of other hormones (PTH, glucocorticoids, growth hormone, estrogens, thyroid hormones, prolactin) on intestinal calcium absorption [24].
Vitamin D deficiency
Although consensus is lacking about an ‘optimal’ serum 25(OH)D concentration, a 25(OH)D level above 75 nmol/L (to convert nmol/L to ng/mL, divide by 2.5) can be regarded as the target level based on recommendations by the Endocrine Society Guidelines on vitamin D [25]. Other organizations including the Institute of Medicine [26] regard a 25(OH)D concentration above 50 nmol/L as sufficient, a 25(OH)D concentration between 30−50 nmol/L as insufficient, and a 25(OH)D concentration below 25−30 nmol/L as deficient. It is worth noting that vitamin D thresholds are not always intended to be diagnostic but are indicative of increased risk of disease. Based on these definitions, the prevalence of vitamin D deficiency/insufficiency worldwide is substantial irrespective of geographical region, ethnicity, latitude or altitude [3, 5, 27–35]. Indeed, a large systematic review found that 88% of the worldwide population had serum 25(OH)D concentrations < 75 nmol/L, 37% had concentrations < 50 nmol/L and 7% had concentrations < 25 nmol/L [3].
With some variation, serum 25(OH)D concentrations below 25−30 nmol/L are generally regarded as inadequate and concentrations above 50 nmol/L as adequate for maintaining bone health [36, 37]. A target serum 25(OH)D concentration of > 75 nmol/L may be recommended for individuals with various conditions who are at risk of vitamin D deficiency, or when focusing on the potential multiple/pleiotropic effects of vitamin D [25, 26, 38–41]. In this regard, there is evidence to suggest a role for vitamin D in modulating immune function [6, 42], although clinical data are not yet sufficiently robust to support recommendations for therapeutic vitamin D supplementation in patients with infections or autoimmune diseases [42]. The situation may change, however, as more evidence accumulates. An ancillary study to the randomized, double-blind vitamin D and omega-3 trial (VITAL; n = 25,871 participants) showed that improved vitamin D status over 5 years significantly reduced by 22% new incident autoimmune disease [43]. Observational data have suggested that maintaining adequate serum 25(OH)D concentrations may protect against COVID-19 infectivity and severity [44, 45], although a randomized controlled trial has since shown no reduction in the risk of all-cause acute respiratory infection or COVID-19 with vitamin D3 supplementation in a large group of adults with vitamin D insufficiency [46].
Causes of vitamin D deficiency are myriad and include limited exposure to sunlight, use of sun blockers, dark skin pigmentation, inadequate intake of vitamin D-containing foods, malabsorption, genetic diseases of vitamin D metabolizing enzymes and the VDR, hepatic disease, renal disease, aging, obesity, and drugs that may affect the absorption or metabolism of vitamin D [1, 29, 41]. Depending on dietary preferences and latitude of residence in the general population, natural sources of vitamin D may be inadequate to maintain serum concentrations above 50 nmol/L throughout the year [39]. Strategies to improve vitamin D status include increased sun exposure, although this carries an increased risk of skin cancer; increased dietary intake of vitamin D-containing and vitamin D-fortified foods [47]; and vitamin D supplementation. Options for vitamin D supplementation vary by country. The most widely used supplement for vitamin D deficiency globally is vitamin D3. Vitamin D2 is used primarily in the USA and India [1, 10, 48]. Calcifediol is the primary supplement used in Spain and recently has been introduced to other markets.
An important and challenging issue regarding dosage recommendations for vitamin D supplementation is the continued use of international units (IU), which were defined several decades ago. In 1949, the Expert Committee on Biological Standardization defined 1 IU of vitamin D as 0.025 µg of crystalline vitamin D3. The antirachitic activity of vitamin D was determined by administering various known concentrations of vitamin D to vitamin D deficient rachitic rats for 8 days. The proximal radii and ulnas were harvested and placed in a solution of silver nitrate where the line of new mineralization in the growth plate would turn black. The thickness of the line was determined and related to the amount of vitamin D administered. A higher vitamin D intake resulted in a thicker line and hence a higher visual score as described in the United States Pharmacopeia. This was known as the line test which was used to determine the number of IUs of vitamin D present in food or other substances. Subsequent experiments showed that the effect of 1.5 µg of vitamin D3 with respect to calcium deposits in the line test was similar to that of approximately 1 µg of calcifediol [49]. As such, it is inappropriate to refer to calcifediol in IU since it is more effective per µg than vitamin D3 in inducing antirachitic activity in a rat. Calcifediol doses should be expressed in micrograms or milligrams.
Differences between supplemental vitamin D3 and calcifediol
A key molecular difference between calcifediol and vitamin D3 is that calcifediol is one step closer in the metabolic pathway to biologically active vitamin D (see Fig. 1) [50]. The additional hydroxyl group on carbon 25 of calcifediol confers pharmacokinetic properties that can be pharmacologically advantageous in certain clinical situations such as malabsorption, liver impairment and obesity (Fig. 2).
Fig. 2.
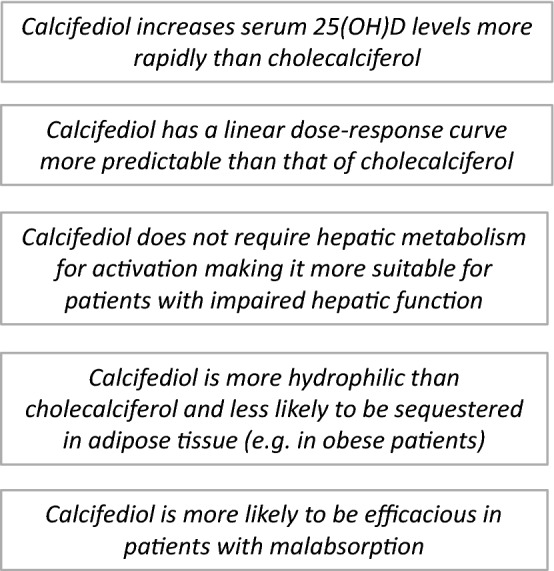
Pharmacological advantages of calcifediol as a vitamin D supplement
Pharmacokinetic differences and their clinical implications
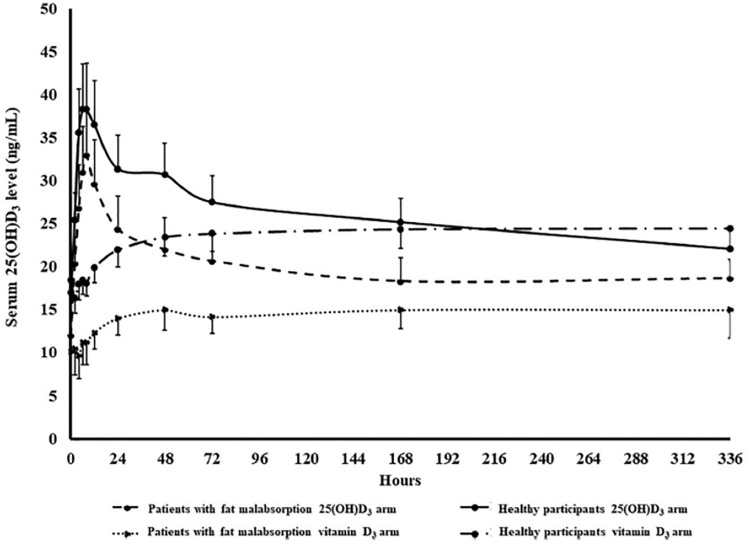
The intestinal absorption of vitamin D3, but not calcifediol, depends on the presence of bile acids and micelle formation [51]. In patients with fat malabsorption (e.g., celiac disease, pancreatic insufficiency, biliary cirrhosis), intestinal absorption of vitamin D3 is markedly compromised [52–54], whereas that of calcifediol is relatively preserved (Fig. 3) [55]. Some European consensus statements recommend calcifediol as the vitamin D supplement of choice for patients with malabsorption syndromes (e.g., short bowel syndrome), and those undergoing bariatric surgery [56–58]. Calcifediol may also be preferable for use in patients receiving concomitant drugs that interfere with fat absorption, such as orlistat [59].
Fig. 3.
Mean ± SEM serum 25-hydroxyvitamin D3 (25(OH)D3) concentration versus time curve after a single oral 900 µg dose of vitamin D3 (cholecalciferol) or 25-hydroxyvitamin D3 (25(OH)D3, calcifediol) in healthy participants (n = 10) and patients with intestinal malabsorption of vitamin D (n = 6). The AUC of 25(OH)D3 was statistically significantly higher with calcifediol than vitamin D3 in both patient groups (both p < 0.001; Wilcoxon signed-rank test).
Reproduced with permission from [55]. Copyright Holick 2021. AUC area under the curve, SEM standard error of the mean
Calcifediol has a linear dose–response curve irrespective of baseline serum 25(OH)D concentrations [51]. In contrast, with vitamin D3, the higher the basal 25(OH)D concentration, the smaller the increase during supplementation and vice versa [51]. The less predictable dose response to vitamin D3 may arise from factors affecting its absorption (as discussed above) and metabolic conversion (e.g., age- and disease-related decreases in hepatic 25-hydroxylase activity). The more linear dose–response curve of calcifediol may be advantageous in situations where higher serum 25(OH)D concentrations are desirable [51]. For example, the requirement for higher doses of vitamin D supplements in patients receiving drugs that interfere with hepatic 25-hydroxylases (e.g., antiepileptic and antiretroviral drugs) [56, 58] suggests a possible advantage for calcifediol over vitamin D3. Calcifediol is recommended as the preferred vitamin D supplement in patients with advanced liver disease [56].
Numerous comparative clinical trials have demonstrated that, at comparable doses to vitamin D3, calcifediol induces a more rapid and larger increase in serum 25(OH)D concentrations (Table 1) [55, 60–72]. On a weight basis, calcifediol is considered to be between 3- to sixfold more potent than vitamin D3, with the range reflecting the non-linear efficacy of vitamin D3 for vitamin D repletion in comparative studies. The higher potency of calcifediol may be beneficial in clinical situations where a rapid increase in vitamin D status is required, such as patients with symptoms of osteomalacia due to vitamin D deficiency or before initiation of antiresorptive treatment or anabolic bone therapy in patients at risk of fracture [73, 74].
Table 1.
Studies comparing calcifediol and vitamin D3 for improving vitamin D status
| Study [reference number] design | Patient population | Treatment (no. of pts) | Results (calcifediol vs vitamin D3) |
|---|---|---|---|
| Double-blind | |||
|
Bischoff-Ferrari et al. 2012 [60] r, db, sc |
Healthy Caucasian post-menopausal women 50‒70 years of age with serum 25(OH)D concentrations of 20‒60 nmol/L | Calcifediol 20 µg/day (n = 5) or 140 µg/wk (n = 5) vs vitamin D3 800 IU/day (20 µg/day) [n = 5] or 5600 IU/wk (140 µg/wk) [n = 5] |
At 4 months, mean serum 25(OH)D concentrations were 174 nmol/L (69.5 ng/mL) in the calcifediol group and 79 nmol/L (31.0 ng/mL) in the vitamin D3 group (p < 0.0001) Serum 25(OH)D concentrations shifted to > 75 nmol/L in all calcifediol-treated women at 35 days of follow-up, whereas ≈ 50% of those receiving vitamin D3 had concentrations below the target threshold throughout the 4-month follow-up |
|
Cashman et al. 2012 [61] r, db |
Healthy Caucasian men and women ≥ 50 years of age | Calcifediol 7 µg/day (n = 14) or 20 µg/day (n = 12) vs vitamin D3 800 IU/day (20 µg/day) [n = 13] vs placebo (n = 16) | Mean increases (per microgram of vitamin D compound) from baseline in serum 25(OH)D concentrations after 10 wks of supplementation were 0.96 ± 0.62 nmol/L with vitamin D3, 4.02 ± 1.27 nmol/L with calcifediol 7 µg/day, and 4.77 ± 1.04 nmol with calcifediol 20 µg/day |
|
Jetter et al. 2014 [62] r, db, sc |
Healthy women 50‒75 years of age with serum 25(OH)D concentrations of 20‒60 nmol/L | Calcifediol 20 µg/day (n = 5), 140 µg/wk (n = 5) or 140 µg single dose (n = 5) vs vitamin D3 800 IU/day (20 µg/day) [n = 5], 5600 IU/wk (140 µg/wk) [n = 5] or 5600 IU/wk (140 µg/wk) single dose (n = 5) vs combination of calcifediol 140 µg plus vitamin D3 5600 IU as single doses | Serum 25(OH)D concentrations of > 75 nmol/L were achieved in 100% of women treated with calcifediol (daily or weekly) after a mean of 16.8 days, versus 70% of women treated with vitamin D3 (daily or weekly) after a mean of 68.4 days |
|
Catalano et al. 2015 [63] r, sc |
Post-menopausal women (mean age 59 years) at low risk of fracture with serum 25(OH)D concentrations < 75 nmol/L | Calcifediol 140 µg/wk (n = 29) or vitamin D3 140 µg/wk [n = 28] | After 24 wks, a significant increase from baseline in mean 25(OH)D levels was observed in both groups (p < 0.001), although the level was higher with calcifediol than vitamin D3 (50.3 ± 15.5 vs 24.3 ± 7.8; p < 0.001) |
|
Jakobsen et al. 2018 [64] r, db, co |
Healthy male volunteers 20−30 years of age with mean baseline serum 25(OH)D concentration of 56.1 ± 8.5 nmol/L | Run-in with 10 µg/day vitamin D3 for 4 wks, followed by 3 × 6-wk treatment periods with 10 µg/day of vitamin D2, 25(OH)D3 (calcifediol) and vitamin D3 (cholecalciferol) | Based on the assumption that 1 µg vitamin D3/day will show an increase in vitamin D status of 1.96 nmol/L, 10 µg vitamin D3 was similar to 6.8 µg 25(OH)D3 and 23 µg vitamin D2 |
|
Vaes et al. 2018 [65] r, db |
Elderly men and women ≥ 65 years of age with serum 25(OH)D concentrations of 25‒50 nmol/L | Calcifediol 5.1 µg/day (n = 14), 10.3 µg/day (n = 15) or 15.3 µg/day (n = 16) vs vitamin D3 800 IU/day (22.3 µg/day) [n = 14] |
Calcifediol 10 µg/day and 15 µg/day increased serum 25(OH)D concentrations to > 75 nmol/L in 8 and 4 wks, respectively Vitamin D3 increased serum 25(OH)D concentrations toward 70 nmol/L within 16 wks |
|
Graeff-Armas et al. 2020 [66] r, db, sc |
Healthy Caucasian men and women > 50 years of age | Calcifediol 10 µg/day (n = 22), 15 µg/day (n = 23), 20 µg/day (n = 24) vs vitamin D3 800 IU/day (20 µg/day) [n = 22] |
At 6 months, mean increases from baseline in serum 25(OH)D concentrations were 50.1, 72.5, and 97.4 nmol/L with calcifediol 10 (p = 0.0173), 15 (p < 0.0001), and 20 (p < 0.0001) µg/day, respectively, versus 38.7 nmol/L with vitamin D3 Time to reach serum 25(OH)D concentrations of 75 nmol/L were 7 and 10 days with calcifediol 15 and 20 µg/day, versus 40 days with vitamin D3 (both p < 0.0001) |
|
Pérez-Castrillón et al. 2021 [67] r, db, mc |
Post-menopausal women with serum 25(OH)D concentrations < 50 nmol/L | Calcifediol 266 µg/month (n = 200) vs vitamin D3 25,000 IU/month (n = 98) | At month 4, 35.0% of women treated with calcifediol reached serum 25(OH)D concentrations > 75 nmol/L versus 8.2% treated with vitamin D3 (p < 0.0001) [primary end point]; 13.5 vs 0% after 1 month (p < 0.0001) |
|
Charoenngam et al. 2021 [55] r, db, co, sc |
Healthy adults (n = 10) Patients with intestinal malabsorption of vitamin D (n = 6) |
Vitamin D3 900 μg (36,000 IU) or calcifediol 900 μg for 14 days, then 14 days’ washout and crossover |
AUCs of vitamin D3 were 64% lower in patients with malabsorption than in healthy participants (1177 ± 425 vs. 3258 ± 496 ng∙h/mL; p < 0.05); AUCs of calcifediol were not significantly different between groups (p = 0.540) In healthy participants, AUCs of vitamin D3 were 53% lower in the higher vs lower BMI group (2089 ± 490 vs 4427 ± 313 ng∙h/mL; p < 0.05); AUCs of calcifediol were not significantly different between groups (p = 0.500) Cmax and Tmax in the vitamin D3 arm were 53.5 ± 6.0 vs 24.3 ± 8.4 ng/mL and 10.4 ± 0.7 vs 11.3 ± 0.7 h in healthy participants and malabsorptive patients, respectively Cmax and Tmax in the calcifediol arm were 23.1 ± 4.6 vs 23.2 ± 6.8 ng/mL and 11.2 ± 4.1 vs 5.3 ± 0.7 h in healthy participants and malabsorptive patients, respectively |
|
Shieh et al. 2021 [68] r, pg |
Healthy adults with serum 25(OH)D concentrations < 50 nmol/L | Calcifediol 20 µg/day vs vitamin D3 60 µg/day | At 8 wks, there was a significant increase from baseline in serum 25(OH)D concentrations with calcifediol (p < 0.001) and vitamin D3 (p = 0.002), but the increase was greater with calcifediol than vitamin D3 (127 vs 75 nmol/L) |
| Non-blinded | |||
|
Shieh et al. 2017 [69] r, nb, sc |
Adults ≥ 18 years of age with serum 25(OH)D concentrations < 50 nmol/L | Calcifediol 20 µg/day (n = 19) vs vitamin D3 2400 IU/day (60 µg/day) [n = 16] |
At 16-wk follow-up, there was a significant increase in total serum 25(OH)D concentrations with calcifediol versus vitamin D3 (64 vs 34.5 nmol/L; p = 0.008) By 4 wks, 87.5% of calcifediol-treated participants versus 23.1% of vitamin D3-treated participants had achieved total serum 25(OH)D concentrations ≥ 75 nmol/L (p = 0.001) |
|
Ruggiero et al. 2019 [70] r, nb, sc |
Elderly men and women > 75 years of age admitted to geriatric acute care ward | Calcifediol 150 µg/wk vs vitamin D3 6000 IU/wk (150 µg/wk) [n = 67 total for both groups] |
After 7 months, serum 25(OH)D increased on average by 47.5 nmol/L (19 ng/mL) in calcifediol-treated participants and by 40.0 nmol/L in vitamin D3-treated participants (p = 0.5) Increase in serum 25(OH)D concentrations was steeper (i.e., more rapid) with calcifediol (p = 0.01 for group*time interaction) |
|
Corrado et al. 2021 [71] r, nb, sc |
Post-menopausal Caucasian women with serum 25(OH)D concentrations of 20‒60 nmol/L | Calcifediol (dose equivalent to 7000 IU)/wk (n = 26); vitamin D3 300,000 IU single dose (n = 28), 100,000 IU/q2mo (n = 26) or 7000 IU/wk (n = 27) | Target serum 25(OH)D concentrations of > 75 nmol/L were reached at 2 months in calcifediol-treated participants versus 3 and 5 months, respectively, in participants treated with vitamin D3 weekly and q2mo |
| Non-randomized, non-blinded | |||
|
Navarro-Valverde et al. 2016 [72] nr, nb, sc |
Post-menopausal osteopenic women with serum 25(OH)D concentrations < 50 nmol/L | Calcifediol 20 µg/day (n = 10), 266 µg/wk (n = 10) or 266 µg q2wk (n = 10) vs vitamin D3 800 IU/day (20 µg/day) [n = 10] |
At 6 and 12 months, serum 25(OH)D concentrations were 161 ± 21.7 and 188.0 ± 24.0 with calcifediol 20 µg/day, 213.5 ± 80.0 and 233.0 ± 81.2 with calcifediol 266 µg/wk, 164.5 ± 41.7 and 210.5 ± 22.2 with calcifediol 266 µg q2wk, and 80.0 ± 2 and 86.2 ± 23.7 with vitamin D3 20 µg/day Increases with calcifediol were more rapid and significantly greater than with vitamin D3 (p < 0.001) |
Conversion factors for serum 25(OH) D concentrations: for ng/mL to nmol/L, × by 2.5; for nmol/L to ng/mL, ÷ by 2.5
AUC area under the curve, BMI body mass index, Cmax maximum concentration, co crossover, db double-blind, mc multicenter, nb nonblind, nr nonrandomized, pg parallel group, q2mo every 2 months, q2wk every 2 weeks, r randomized, sc single-center, Tmax time to maximum serum concentration, wk week
Vitamin D3 is more lipophilic than calcifediol and can be sequestered in adipose tissue [75, 76]. By virtue of its additional hydroxy (OH) group, calcifediol is more hydrophilic, and thus less prone to sequestration [50, 55, 77]. This difference in lipophilicity results in a much-prolonged elimination half-life for vitamin D3 compared with calcifediol (≈ 2 months versus ≈ 10‒15 days) [77]. A long and short half-life each may have clinical advantages. A short half-life can be clinically useful as it allows for a more rapid response to dose adjustments [66]. In general, higher doses of any type of vitamin D supplement are required in individuals with obesity to achieve optimal serum concentrations of 25(OH)D [78]. Preclinical data suggesting that hepatic 25-hydroxylation is altered in obesity may account at least in part for the reduction in circulating 25(OH)D concentrations [79, 80]. Some guidelines recommend calcifediol as the vitamin D supplement of choice in patients with obesity [56–58].
Lastly, as discussed above, vitamin D3 but not calcifediol requires 25-hydroxylation, which has implications for the conversion efficacy of vitamin D3 to 25(OH)D depending on the functioning of metabolizing enzymes. Studies have shown severe impairment in the expression and activity of hepatic CYP2R1 in obesity [79, 80], during fasting and in type 1 and type 2 diabetes mouse models, with involvement of at least two molecular pathways: the peroxisome proliferator-activated-gamma-coactivator-1α/estrogen-related receptor α axis and the glucocorticoid receptor [81].
Safety and dosage issues
The reference range for vitamin D sufficiency is 50−250 nmol/L. Available data indicate that serum 25(OH)D concentrations associated with vitamin D toxicity (hypervitaminosis D) are in excess of 375 nmol/L [26]. As such, the safety margin is broad irrespective of which supplement is used. Vitamin D toxicity and its associated manifestations (e.g., hypercalcemia, hypercalciuria, nephrocalcinosis) are rare, typically arising from patients self-administering extremely high doses of a vitamin D supplement for prolonged periods of time [25, 39]. Nevertheless, in view of the higher potency of calcifediol relative to vitamin D3, and greater risk of excessive serum 25(OH)D concentrations in case of overdose, it is important that clinicians are aware of the optimal dosing per condition of each vitamin D supplement and prescribe accordingly. The calcifediol dose, and the frequency and duration of treatment are determined according to the serum 25(OH)D concentration, type of patient, condition being treated and presence of comorbidities such as obesity, malabsorption syndrome, and treatment with corticosteroids [82]. As with all medicines used for therapeutic purposes, patients receiving calcifediol should be advised to adhere to the prescribed dose.
During widespread use of calcifediol for more than 40 years in Spain, there have been few reports to the Spanish Pharmacovigilance System of hypercalcemia and/or hypervitaminosis D [83]. In studies which investigated weekly or biweekly doses of calcifediol 266 µg (i.e., in excess of the recommended dose) for 6–12 months in patients with osteoporosis or asthma, serum 25(OH)D concentrations remained below the 250 nmol/L threshold considered to be a risk for hypercalcemia [84, 85]. In general, monthly administration of calcifediol 266 µg is regarded as adequate to achieve effective vitamin D status and avoid risks associated with excessive concentrations [82, 84]. A pharmacokinetic study in healthy older adults found that calcifediol at doses of 15 and 20 µg/day significantly reduced the time to reach 25(OH)D concentrations of 75 nmol/L compared with vitamin D3 (20 µg/day); upon discontinuation, calcifediol was eliminated faster than vitamin D3 [66]. The superior efficacy of calcifediol in repleting serum 25(OH)D concentrations has important implications for clinical practice and should be considered in therapeutic guidelines.
Recommended dosages of vitamin D3 or calcifediol to correct deficiency may take into account the vitamin D status of the recipient and other factors [86]. As an example, Italian guidelines recommend using different doses of vitamin D3 or calcifediol depending on basal serum 25(OH)D concentrations [87]. In patients with serum 25(OH)D concentrations below 30 nmol/L, the recommended cumulative dose of vitamin D3 is 300,000 IU over a maximum period of 12 weeks, divided into daily, weekly, or monthly administration (with no dose to exceed 100,000 IU for safety reasons). The recommended regimen of calcifediol is one capsule (266 µg) twice per month. At serum concentrations of 30‒50 nmol/L, vitamin D3 750‒1000 IU/day or corresponding weekly or monthly administration is recommended, or calcifediol can be administered at a dose of one capsule (266 µg) per month. At serum concentrations of > 50 nmol/L, vitamin D supplementation is generally not recommended. Recent guidelines from the Spanish Society for Bone Research and Mineral Metabolism (SEIOMM) also recommend different dosage regimens for calcifediol and vitamin D3 depending on the patient population (general or at-risk populations) [58]. Recommendations for calcifediol are provided in Table 2. Conversely, Dutch guidelines for vitamin D deficiency do not factor baseline serum 25(OH)D concentrations into dosage recommendations for the general population since lower baseline 25(OH)D concentrations result in larger increases during vitamin D3 supplementation [88].
Table 2.
Spanish Society for Bone Research and Mineral Metabolism (SEIOMM)-recommended dosage regimens for calcifediol in different patient populations with vitamin D deficiency [58]
| Population | Recommendations |
|---|---|
| General population with severe deficiency (serum 25(OH)D concentrations < 25 nmol/L) | Calcifediol 266 µg/week for 5 weeks then 266 µg/month |
| General population with insufficiency (serum 25(OH)D concentrations 25‒62.5 nmol/L) | Calcifediol 266 µg/month |
| Osteoporosis and other populations at risk of deficiency (and with serum 25(OH)D concentrations < 25 nmol/L) | Calcifediol 266 µg/week for 5 weeks then 266 µg every 3–4 weeks |
| Osteoporosis and other populations at risk of deficiency (and with serum 25(OH)D concentrations of 25‒75 nmol/L) | Calcifediol 266 µg every 3–4 weeks |
Studies of supplemental calcifediol in disease
Since calcifediol only recently became available outside of Spain, most literature evaluating vitamin D supplementation for bone diseases and other conditions refers to vitamin D3. Studies of calcifediol have frequently used serum 25(OH)D concentrations as the end point (see Table 1), rather than hard clinical end points such as fracture numbers or hospitalization rates. In recent years, however, several studies conducted with calcifediol have reported non-laboratory clinical end points. The design features and outcomes of these studies are summarized in Table 3 [60, 70, 71, 85, 89–100].
Table 3.
Studies of supplemental calcifediol in disease
| Study [reference number] design | Patient population | Treatment (no. of pts) | Results |
|---|---|---|---|
| Physical performance and muscle strength parameters | |||
|
Bischoff-Ferrari et al. 2012 [60] r, db, sc |
Healthy Caucasian post-menopausal women 50‒70 years of age with serum 25(OH)D concentrations of 20‒60 nmol/L | Calcifediol 20 µg/day (n = 5) or 140 µg/wk (n = 5) vs vitamin D3 800 IU/day (20 µg/day) [n = 5] or 5600 IU/wk (140 µg/wk) [n = 5] |
At 4 months, significant (p = 0.03) improvement in knee extension strength with calcifediol vs vitamin D3 At 4 months, non-significant improvement in knee flexion strength, Timed Up-and-Go test, and repeated Sit-to-Stand test with calcifediol vs vitamin D3 |
|
Vaes et al. 2018 [89] r, db, pc |
Prefrail or frail men and women ≥ 65 years of age with serum 25(OH)D concentrations of 20‒50 nmol/L | Calcifediol 10 µg/day (n = 26), vitamin D3 800 IU/day (20 µg/day) [n = 26], or placebo (n = 26) |
After 6 months, no significant change from baseline in knee-extension strength with calcifediol, vitamin D3, or placebo After 6 months, mean changes in physical performance tests, muscle mass, and muscle fiber type and size did not differ between groups |
|
Ruggiero et al. 2019 [70] r, nb, sc |
Elderly men and women > 75 years of age admitted to geriatric acute care ward | Calcifediol 150 µg/wk vs vitamin D3 6000 IU/wk (150 µg/wk) [n = 67 total for both groups] | At 7 months after discharge, polypharmacy and low handgrip strength at baseline were predictors of failure of intervention, independent of supplement (calcifediol or vitamin D3) |
|
Corrado et al. 2021 [71] r, ol, sc |
Post-menopausal women with serum 25(OH)D concentrations of 20‒60 nmol/L | Group 1: vitamin D3 300,000 IU, single oral dose (n = 32); group 2: vitamin D3 100,000 IU every two months (n = 31); group 3: vitamin D3 7000 IU weekly (n = 31); group 4: calcifediol 7000 IU weekly (n = 30) |
At 6 months, all vitamin D regimens induced significant improvement in muscular function (Timed-Up-and-Go test and 30 s repeated Sit-to-Stand test) Significantly greater improvement in lower extremity muscular strength and function with calcifediol 7000 IU weekly vs vitamin D3 treatment regimens (p < 0.05) |
|
Gonnelli et al. 2021 [90] r, ol, pg |
Post-menopausal osteopenic/osteoporotic women aged 55 to 70 years with serum 25(OH)D concentrations of 25‒50 nmol/L | Calcifediol 20 µg/day (n = 25) or calcifediol 30 µg/day (n = 25) | At 3 and 6 months, significant improvement from baseline in values for hand grip strength with calcifediol 30 µg (p < 0.05), but not calcifediol 20 µg |
|
Iolascon et al. 2017 [91] Prospective cohort |
Post-menopausal women aged ≥ 50 years with osteoporosis and/or serum 25(OH)D concentrations < 75 nmol/L | Calcifediol 20 µg/day (n = 113) |
After 6 months’ treatment, significant increase from baseline in appendicular muscle strength (p < 0.001) using Isometric Hand Grip Strength Test and Knee Isometric Extension Strength Test; and in physical performance (p = 0.002 at Short Physical Performance Battery and p = 0.010 at 4 m gain speed) At 6 months, significant reduction in percentage of recurrent fallers (p < 0.001) and mean number of falls (p = 0.020) |
| Asthma control | |||
|
Andújar-Espinosa et al. 2021 [85]; Andújar-Espinosa et al. 2021 [92] r, tb, pc, pg |
Patients with asthma and serum 25(OH)D concentrations < 75 nmol/L | Calcifediol 266 µg/wk (16,000 IU) [n = 56] or placebo (n = 56) |
At 6 months, significant improvement from baseline in asthma control (Asthma Control Test scores) with calcifediol vs placebo (difference 3.66; 95% CI 0.89–5.43; p < 0.001) At 6 months, significant improvement in quality of life (Mini Asthma Quality of Life Questionnaire) with calcifediol vs placebo (difference 0.7; 95% CI 0.15–1.25; p = 0.01) |
| COVID-19 | |||
|
Entrenas Castillo et al. 2020 [93] r, ol, pg |
Hospitalized patients (mean age 53 years) with COVID-19 | Calcifediol 0.532 mg on day of admission, then 0.266 mg on day 3 and 7, then weekly until discharge or ICU admission (n = 50) vs no calcifediol treatment (n = 26) | One of 50 patients (2%) treated with calcifediol vs 13 of 26 patients (50%) not treated with calcifediol required ICU admission |
|
Maghbooli et al. 2021 [94] r, mc, db, pc |
Hospitalized patients (mean age 49 years) with COVID-19 and serum 25(OH)D concentrations < 75 nmol/L | Calcifediol 25 µg/day (n = 53) vs placebo (n = 53) | Trend for lower hospitalization duration (median 5 vs 6 days), intensive care unit duration (7 vs 11 days), need for ventilator assistance (4 vs 9%), and mortality (6 vs 9%) with calcifediol, but differences vs placebo were not statistically significant |
|
Alcala-Diaz et al. 2021 [95] ret, mc, ol, nr |
Hospitalized patients (mean age 53 years) with COVID-19 | Calcifediol (n = 79) vs no calcifediol treatment (n = 458) | Patients supplemented with calcifediol had lower risk of death during hospitalization (5 vs 20%; OR 0.22; 95% CI 0.08–0.61; p < 0.01) vs patients not receiving calcifediol supplementation |
|
Nogues et al. 2021 [96] obs, cohort |
Hospitalized patients ≥ 18 years of age with COVID-19 | Calcifediol 0.532 mg on day 1, then 0.266 mg on day 3, 7, 15, and 30 (n = 447) vs no calcifediol treatment (n = 391) |
ICU admission rate was significantly lower in patients treated vs not treated with calcifediol at admission (4.5 vs 21%; p < 0.0001) Mortality rate was significantly lower in patients treated vs not treated with calcifediol at admission (4.7% vs 15.9%; OR 0.21; 95% CI: 0.10 − 0.43; p < 0.001) |
|
Loucera et al. 2021 [97] ret, cohort |
Hospitalized patients with COVID-19 (n = 15, 968) | Prior prescription of vitamin D3, calcifediol or calcitriol |
Association between prescription of vitamin D3 or metabolites stronger for calcifediol (HR 0.75; 95% CI 0.61–0.91) than for vitamin D3 (HR 0.67; 95% CI 0.50–0.91) when prescribed 15 days prior to hospitalization The relation was maintained but weaker when prescribed 30 days prior to hospitalization: calcifediol (HR = 0.73; 95% CI 0.57–0.95) and vitamin D3 (HR 0.88; 95% CI 0.75–1.03) |
|
Oristrell et al. 2022 [98] ret, cohort |
Individuals ≥ 18 years old living in Barcelona-Central Catalonia supplemented with vitamin D3 (n = 108,343) or calcifediol (n = 134, 703) from April 2019 to February 2020 vs propensity score-matched untreated controls | Vitamin D3 or calcifediol supplementation |
Patients on vitamin D3 achieving 25(OH)D levels ≥ 75 nmol/L had lower risk of SARS-CoV2 infection, lower risk of severe COVID-19, and lower COVID-19 mortality compared to unsupplemented 25(OH)D-deficient patients (0.6 vs 1.3%; HR 0.66; 95% CI 0.46–0.93; p = 0.018) Patients on calcifediol achieving serum 25(OH)D levels ≥ 75 nmol/L had lower risk of SARS-CoV2 infection, lower risk of severe COVID-19, and lower COVID-19 mortality compared to unsupplemented 25(OH)D-deficient patients (0.5 vs 1.3%; HR 0.56; 95% CI 0.42–0.76; p < 0.001 |
| Secondary hyperparathyroidism | |||
|
Sprague et al. 2014 [99] r, db, pc |
Patients with CKD, iPTH > 70 pg/ml and serum total 25(OH)D < 75 nmol/L | Extended-release (ER) calcifediol 30 µg/day (n = 13) vs placebo (n = 14) and ER calcifediol 60 (n = 17) or 90 (n = 17) µg/day vs placebo (n = 17) |
At 6 wks, 90% of calcifediol-treated patients achieved 25(OH)D levels > 75 nmol/L vs 3% of placebo-treated patients (p < 0.0001) At 6 wks, mean PTH decreased from baseline by 20.9, 32.8 and 39.3% in the 30, 60 and 90 μg dose groups, respectively, and increased from baseline by 17.2% in the pooled placebo group (p < 0.005) |
|
Sprague et al. 2014 [100] r, mc, db, pc |
Patients with CKD stage 3 or 4, SHPT and vitamin D insufficiency |
Study A: extended-release (ER) calcifediol 30 µg/day (n = 141) vs placebo (n = 72) Study B: extended-release (ER) calcifediol 30 µg/day (n = 144) vs placebo (n = 72) |
At 12 wks in studies A and B, 80 and 83% of calcifediol-treated patients achieved 25(OH)D levels > 75 nmol/L vs 3 and 7% of placebo-treated patients (p < 0.001), respectively At 12 wks in studies A and B, 33% and 34% of calcifediol-treated patients achieved ≥ 30% reduction in plasma iPTH vs 8 and 7% of placebo-treated patients (p < 0.001), respectively |
Conversion factors for serum 25(OH)D concentrations: for ng/mL to nmol/L, × by 2.5; for nmol/L to ng/mL, ÷ by 2.5
CI confidence interval, CKD chronic kidney disease, db double-blind, HR hazard ratio, ICU intensive care unit, iPTH intact parathyroid hormone, mc multicenter, nb nonblind, nr nonrandomized, obs observational, ol open-label, OR odds ratio, pc placebo-controlled, pg parallel group, r randomized, ret retrospective, sc single-center, SHPT secondary parahyperthyroidism, tb triple-blind, wk week
Physical performance and muscle strength parameters in post-menopausal or frail patients
Several studies have examined the effects of calcifediol supplementation on physical performance and muscle strength parameters in post-menopausal women or frail and elderly patients with vitamin D insufficiency [60, 70, 71, 89–91]. Two small comparative RCTs of calcifediol and vitamin D3 reported modest benefits with calcifediol [60] or no change from baseline with either supplement [89]. In a monocentric open-label randomized trial comparing weekly calcifediol (dosage reported as 7000 IU/week) with vitamin D3 (at dosages of 7000 IU/week, 100,000 IU every 2 months or 300,000 IU as a single dose) in 107 post-menopausal women, calcifediol achieved target serum 25(OH)D concentrations more rapidly than vitamin D3 and, at 6 months, was associated with significantly (p < 0.05) greater improvement than vitamin D3 in lower extremity muscle strength/function assessed using the 30-s Sit-to-Stand test and Timed-Up-and-Go test [71]. A prospective, open-label study randomized 50 post-menopausal women with osteopenia/osteoporosis and baseline serum 25(OH)D concentrations of 25−50 nmol/L to receive calcifediol at doses of 20 or 30 µg/day. Serum 25(OH)D concentrations were normalized to above > 75 nmol/L within 30 days in 87% (20 of 23) and 100% (23 of 23) of patients, respectively. At 6 months, the group treated with calcifediol 30 µg/day showed a modest but statistically significant increase in upper limb (handgrip) strength [90]. In an nonblinded, nonrandomized, uncontrolled, prospective cohort study, calcifediol 20 µg/day was administered to 113 post-menopausal women with osteoporosis and/or serum 25(OH)D concentrations < 75 nmol/L. After 6 months’ treatment, statistically significant improvements from baseline were measured in serum 25(OH)D concentrations (p < 0.001), as well as in appendicular muscle strength (p < 0.001) assessed by Isometric Hand Grip Strength Test and Knee Isometric Extension Strength Test, and physical performance assessed by the Short Physical Performance Battery (p = 0.002) and 4-m Gait Speed (p = 0.01). There were also statistically significant reductions in the percentage of patients who were recurrent fallers (p < 0.001) and in the mean number of falls (p = 0.020) [91]. A systematic review and meta-analysis of seven RCTs (n = 269 participants), including those reported herein, concluded that, over a median follow-up of 24 weeks, calcifediol may have a positive effect on muscle strength parameters, with less evidence of an effect on physical performance [101].
Asthma control
Calcifediol was associated with improved asthma control in a randomized, placebo-controlled trial involving 112 adults with asthma who had serum 25(OH)D concentrations < 75 nmol/L. In addition to their asthma therapy, patients received calcifediol (dose reported as 16,000 IU/week equivalent to 266 µg/week) or placebo for 6 months. Change/improvement from baseline in Asthma Control Test scores at the end of the study period (primary end point) significantly favored calcifediol over placebo (+ 3.09 vs − 0.57; difference 3.66; 95% confidence interval [CI] 0.89−5.43; p < 0.001) [85]. Calcifediol was also associated with a statistically significant improvement compared with placebo in scores on the Mini Asthma Quality of Life Questionnaire [92].
COVID-19
Studies evaluating calcifediol supplementation for COVID-19 have reported favorable clinical outcomes [93–98].
A randomized, non-blinded non-controlled pilot study in 76 patients hospitalized with COVID-19 infection showed a marked reduction in intensive care unit (ICU) admissions among those treated versus not treated with calcifediol (2 vs 50%) [93]. A double-blind placebo-controlled trial identified trends for lower hospitalization and ICU durations, need for ventilator assistance and mortality among 106 hospitalized patients with vitamin D insufficiency (serum 25(OH)D concentrations < 75 nmol/L) treated with calcifediol than placebo, although the differences were not statistically significant. Improved outcomes in calcifediol-treated patients were associated with a higher percent lymphocyte count and lower neutrophil–lymphocyte ratio, which is a surrogate marker for decreased inflammatory activity [94]. A retrospective study of 537 patients hospitalized because of COVID-19 infection reported a statistically significant reduction in in-hospital mortality during the first 30 days (5 vs 20%; p < 0.01) among 79 patients who had been treated with calcifediol after admission [95]. Another retrospective study showed statistically significant reductions in the risk of mortality and ICU admission among patients admitted to COVID-19 hospital wards who had versus had not received calcifediol during the first 30 days [96]. A retrospective cohort study involving nearly 16,000 patients hospitalized with COVID in Andalusia found a stronger association between patient survival and prior use of calcifediol (HR 0.67; 95% CI 0.50−0.91) than prior use of vitamin D3 (HR 0.75, 95% CI 0.61−0.91) [97]. Finally, a large (n > 240,000) population-based observational study conducted in Spain showed that adults receiving calcifediol supplementation who achieved serum 25(OH)D concentrations ≥ 75 nmol/L had a lower risk of COVID-19 infection (3.3 vs 5.6%; hazard ratio [HR] 0.69; 95% CI 0.61−0.79; p < 0.001), severe COVID-19 infection (0.6 vs 1.3%; HR 0.61; 95% CI 0.46−0.81; p = 0.001) and COVID-19-related mortality (0.5 vs 1.3%; HR 0.56; 95% CI 0.42−0.76; p < 0.001) compared with those not receiving vitamin D supplementation [98]. Similar findings were observed with vitamin D3 supplementation in the same study [98]. In contrast, in a recent randomized controlled trial in adults with suboptimal vitamin D status (86.8% with a 25(OH)D concentration < 75 nmol/L), implementation of a test-and-treat approach to vitamin D replacement with vitamin D3 (3200 IU/day, n = 1550; 800 IU/day, n = 1550; no testing or supplementation, n = 3100) for 6 months did not reduce the risk of acute respiratory tract or COVID-19 infection [45]. As regards calcifediol, the paucity of high-quality prospective trials precludes drawing definitive conclusions about its effect on the incidence and outcome of COVID-19 infections. Nevertheless, based on observational evidence of a reduction in COVID-19 severity, it is proposed that calcifediol may be considered for use in all patients in the early stages of COVID-19 infection to correct vitamin D deficiency [102].
Secondary hyperparathyroidism
As a treatment option for secondary hyperparathyroidism in non-dialysis patients with chronic kidney disease and vitamin D insufficiency [99, 100], extended-release calcifediol was shown to gradually improve serum 25(OH)D concentrations, leading to physiologically regulated increases in serum 1,25(OH)2D concentration and sustained reductions in PTH, without any clinically relevant increases in serum phosphorus, calcium and FGF23 [103].
Conclusions
Vitamin D deficiency is a common problem worldwide. Achieving and maintaining a sufficient serum 25(OH)D concentration is important, since vitamin D has beneficial effects not only on musculoskeletal health, but potentially also on other aspects of health through its immunomodulatory effects specifically in individuals with a vitamin D deficiency. Calcifediol and vitamin D3 are both effective at achieving and maintaining optimal 25(OH)D concentrations in the general population. From a pharmacokinetic perspective, when administered at similar doses, calcifediol achieves target serum 25(OH)D concentrations more rapidly than vitamin D3 and has a more predictable and linear dose–response curve. This may be an advantage if rapid correction of vitamin D status is warranted, for example, in symptomatic osteomalacia. Overall, calcifediol is a suitable option for all patients with vitamin D deficiency and is preferable to vitamin D3 for patients with obesity, severe liver disease, or malabsorption, and those who require a rapid increase in 25(OH)D concentrations.
Acknowledgements
Writing assistance for this article was provided by Greg Plosker and Kerry Dechant on behalf of Content Ed Net (Madrid, Spain) with funding from Faes Farma S.A. (Madrid, Spain).
Author contributions
EJG, CCM, MFH, RTdeJ: conceptualization. EJG, CCM, MFH, RTdeJ: review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This review was funded by FAES FARMA. The views and opinions expressed in this publication are those of the authors and do not necessarily reflect the official policy or position of FAES FARMA or any of its officers.
Data availability
Not applicable.
Code availability
Not applicable.
Declarations
Conflict of interest
Esteban Jodar reports grants from Amgen, AstraZeneca, Boehringer Ingelheim, FAES, Janssen, Lilly, MSD, Novo Nordisk, Pfizer, Sanofi, Shire, and UCB; personal fees from Adium, Amgen, Asofarma, AstraZeneca, FAES, Helios-Fresenius, Italfármaco, Lilly, MSD, Mundipharma, Novo Nordisk, UCB, and Viatris. Claudia Campusano Montaño has received honoraria from Amgen, FAES, Novartis, Sanofi, and Tecnofarma. Renata T de Jongh has received a grant from the Dutch Lung Foundation (project number 5113033), an investigator fee from Shire for a pharmacy-initiated study (SHP634-401), and personal fees from Kyowa Kirin, Lilly and UCB. Michael F. Holick has served as consultant for Biogena Inc., Ontometrics Inc. and Solius Inc.; has received grants from Carbogen Amcis BV and Solius Inc. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
References
- 1.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 2.Tsiaras WG, Weinstock MA. Factors influencing vitamin D status. Acta Derm Venereol. 2011;91(2):115–124. doi: 10.2340/00015555-0980. [DOI] [PubMed] [Google Scholar]
- 3.Hilger J, Friedel A, Herr R, Rausch T, Roos F, Wahl DA, Pierroz DD, Weber P, Hoffmann K. A systematic review of vitamin D status in populations worldwide. Br J Nutr. 2014;111(1):23–45. doi: 10.1017/S0007114513001840. [DOI] [PubMed] [Google Scholar]
- 4.Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, Bilezikian J. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr Rev. 2019;40(4):1109–1151. doi: 10.1210/er.2018-00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A, Martucci G, Pilz S, Malle O. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74(11):1498–1513. doi: 10.1038/s41430-020-0558-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charoenngam N, Holick MF. Immunologic effects of vitamin D on human health and disease. Nutrients. 2020;12(7):2097. doi: 10.3390/nu12072097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmad S, Arora S, Khan S, Mohsin M, Mohan A, Manda K, Syed MA. Vitamin D and its therapeutic relevance in pulmonary diseases. J Nutr Biochem. 2021;90:108571. doi: 10.1016/j.jnutbio.2020.108571. [DOI] [PubMed] [Google Scholar]
- 8.Dawson-Hughes B. Role of vitamin D in COVID-19: active or passive? J Clin Endocrinol Metab. 2021;106:e5260–e5261. doi: 10.1210/clinem/dgab505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gil Á, Plaza-Diaz J, Mesa MD. Vitamin D: classic and novel actions. Ann Nutr Metab. 2018;72(2):87–95. doi: 10.1159/000486536. [DOI] [PubMed] [Google Scholar]
- 10.Tripkovic L, Lambert H, Hart K, Smith CP, Bucca G, Penson S, Chope G, Hyppönen E, Berry J, Vieth R, Lanham-New S. Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. Am J Clin Nutr. 2012;95(6):1357–1364. doi: 10.3945/ajcn.111.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biancuzzo RM, Clarke N, Reitz RE, Travison TG, Holick MF. Serum concentrations of 1,25-dihydroxyvitamin D2 and 1,25-dihydroxyvitamin D3 in response to vitamin D2 and vitamin D3 supplementation. J Clin Endocrinol Metab. 2013;98(3):973–979. doi: 10.1210/jc.2012-2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cardwell G, Bornman JF, James AP, Black LJ. A review of mushrooms as a potential source of dietary vitamin D. Nutrients. 2018;10(10):1498. doi: 10.3390/nu10101498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc. 2010;85(8):752–757. doi: 10.4065/mcp.2010.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christakos S, Ajibade DV, Dhawan P, Fechner AJ, Mady LJ. Vitamin D: metabolism. Endocrinol Metab Clin North Am. 2010;39(2):243–253. doi: 10.1016/j.ecl.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wacker M, Holick MF. Sunlight and Vitamin D: A global perspective for health. Dermatoendocrinol. 2013;5(1):51–108. doi: 10.4161/derm.24494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA) Turck D, Castenmiller J, De Henauw S, Hirsch-Ernst KI, Kearney J, Maciuk A, Mangelsdorf I, McArdle HJ, Naska A, Peláez C, Pentieva K, Siani A, Thies F, Tsabouri S, Vinceti M, Cubadda F, Frenzel T, Heinonen M, Marchelli R, Neuhauser-Berthold M, Poulsen M, Maradona MP, Schlatter JR, van Loveren H, Dumas C, Roldán-Torres R, Steinkellner H, Knutsen HK. Safety of calcidiol monohydrate produced by chemical synthesis as a novel food pursuant to Regulation (EU) 2015/2283. EFSA J. 2021;19(7):e06660. doi: 10.2903/j.efsa.2021.6660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergwitz C, Jüppner H. Regulation of phosphate homeostasis by PTH, vitamin D, and FGF23. Annu Rev Med. 2010;61:91–104. doi: 10.1146/annurev.med.051308.111339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fukumoto S. Phosphate metabolism and vitamin D. Bonekey Rep. 2014;3:497. doi: 10.1038/bonekey.2013.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Erben RG. Physiological actions of fibroblast growth factor-23. Front Endocrinol (Lausanne) 2018;9:267. doi: 10.3389/fendo.2018.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bouillon R, Carmeliet G, Verlinden L, van Etten E, Verstuyf A, Luderer HF, Lieben L, Mathieu C, Demay M. Vitamin D and human health: lessons from vitamin D receptor null mice. Endocr Rev. 2008;29(6):726–776. doi: 10.1210/er.2008-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kongsbak M, Levring TB, Geisler C, von Essen MR. The vitamin D receptor and T cell function. Front Immunol. 2013;4:148. doi: 10.3389/fimmu.2013.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lou YR, Molnár F, Peräkylä M, Qiao S, Kalueff AV, St-Arnaud R, Carlberg C, Tuohimaa P. 25-hydroxyvitamin D(3) is an agonistic vitamin D receptor ligand. J Steroid Biochem Mol Biol. 2010;118(3):162–170. doi: 10.1016/j.jsbmb.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 23.Donati S, Palmini G, Romagnoli C, Aurilia C, Miglietta F, Falsetti I, Marini F, Zonefrati R, Galli G, Marcucci G, Iantomasi T, Brandi ML. In vitro non-genomic effects of calcifediol on human preosteoblastic cells. Nutrients. 2021;13(12):4227. doi: 10.3390/nu13124227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diaz de Barboza G, Guizzardi S, Tolosa de Talamoni N. Molecular aspects of intestinal calcium absorption. World J Gastroenterol. 2015;21(23):7142–7154. doi: 10.3748/wjg.v21.i23.7142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine Society Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 26.Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Mayne ST, Rosen CJ, Shapses SA. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–58. doi: 10.1210/jc.2010-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Schoor NM, Lips P. Worldwide vitamin D status. Best Pract Res Clin Endocrinol Metab. 2011;25(4):671–680. doi: 10.1016/j.beem.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 28.Cashman KD, Dowling KG, Škrabáková Z, Gonzalez-Gross M, Valtueña J, De Henauw S, Moreno L, Damsgaard CT, Michaelsen KF, Mølgaard C, Jorde R, Grimnes G, Moschonis G, Mavrogianni C, Manios Y, Thamm M, Mensink GB, Rabenberg M, Busch MA, Cox L, Meadows S, Goldberg G, Prentice A, Dekker JM, Nijpels G, Pilz S, Swart KM, van Schoor NM, Lips P, Eiriksdottir G, Gudnason V, Cotch MF, Koskinen S, Lamberg-Allardt C, Durazo-Arvizu RA, Sempos CT, Kiely M. Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr. 2016;103(4):1033–1044. doi: 10.3945/ajcn.115.120873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Schoor N, Lips P. Global overview of vitamin D status. Endocrinol Metab Clin North Am. 2017;46(4):845–870. doi: 10.1016/j.ecl.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 30.Herrick KA, Storandt RJ, Afful J, Pfeiffer CM, Schleicher RL, Gahche JJ, Potischman N. Vitamin D status in the United States, 2011–2014. Am J Clin Nutr. 2019;110(1):150–157. doi: 10.1093/ajcn/nqz037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sarafin K, Durazo-Arvizu R, Tian L, Phinney KW, Tai S, Camara JE, Merkel J, Green E, Sempos CT, Brooks SP. Standardizing 25-hydroxyvitamin D values from the Canadian health measures survey. Am J Clin Nutr. 2015;102(5):1044–1050. doi: 10.3945/ajcn.114.103689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Asakura K, Etoh N, Imamura H, Michikawa T, Nakamura T, Takeda Y, Mori S, Nishiwaki Y. Vitamin D status in Japanese adults: relationship of serum 25-hydroxyvitamin D with simultaneously measured dietary vitamin D intake and ultraviolet ray exposure. Nutrients. 2020;12(3):743. doi: 10.3390/nu12030743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brito A, Cori H, Olivares M, Fernanda Mujica M, Cediel G, López de Romaña D. Less than adequate vitamin D status and intake in Latin America and the Caribbean: a problem of unknown magnitude. Food Nutr Bull. 2013;34(1):52–64. doi: 10.1177/156482651303400107. [DOI] [PubMed] [Google Scholar]
- 34.González G. Vitamin D status among healthy postmenopausal women in South America. Dermatoendocrinol. 2013;5(1):117–120. doi: 10.4161/derm.24807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palacios S, Cerdas S, Da Silva R, Paradas A, Vargas J, Mostajo D, Tserotas K, Danckers L, Moreno M, Navas M, Muñoz-Louis R, Maida T, Rosero O, Rueda C, Vasquez D, Melo L, Córdoba S, Rasec-Morales L, de Melo NR. Vitamin D supplementation: position statement of the iberoamerican society of osteoporosis and mineral metabolism (SIBOMM) Gynecol Endocrinol. 2021;37(1):10–14. doi: 10.1080/09513590.2020.1858781. [DOI] [PubMed] [Google Scholar]
- 36.Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GE, Josse RG, Lips P, Morales-Torres J, Yoshimura N. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int. 2010;21(7):1151–1154. doi: 10.1007/s00198-010-1285-3. [DOI] [PubMed] [Google Scholar]
- 37.Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, Michigami T, Tiosano D, Mughal MZ, Mäkitie O, Ramos-Abad L, Ward L, DiMeglio LA, Atapattu N, Cassinelli H, Braegger C, Pettifor JM, Seth A, Idris HW, Bhatia V, Fu J, Goldberg G, Sävendahl L, Khadgawat R, Pludowski P, Maddock J, Hyppönen E, Oduwole A, Frew E, Aguiar M, Tulchinsky T, Butler G, Högler W. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101(2):394–415. doi: 10.1210/jc.2015-2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giustina A, Adler RA, Binkley N, Bouillon R, Ebeling PR, Lazaretti-Castro M, Marcocci C, Rizzoli R, Sempos CT, Bilezikian JP. Controversies in vitamin D: summary statement from an international conference. J Clin Endocrinol Metab. 2019;104(2):234–240. doi: 10.1210/jc.2018-01414. [DOI] [PubMed] [Google Scholar]
- 39.Pludowski P, Holick MF, Grant WB, Konstantynowicz J, Mascarenhas MR, Haq A, Povoroznyuk V, Balatska N, Barbosa AP, Karonova T, Rudenka E, Misiorowski W, Zakharova I, Rudenka A, Łukaszkiewicz J, Marcinowska-Suchowierska E, Łaszcz N, Abramowicz P, Bhattoa HP, Wimalawansa SJ. Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018;175:125–135. doi: 10.1016/j.jsbmb.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 40.EFSA Nda Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) Scientific opinion on dietary reference values for vitamin D. EFSA J. 2016;14:4547. doi: 10.2903/j.efsa.2016.4547. [DOI] [Google Scholar]
- 41.Lips P, Cashman KD, Lamberg-Allardt C, Bischoff-Ferrari HA, Obermayer-Pietsch B, Bianchi ML, Stepan J, El-Hajj Fuleihan G, Bouillon R. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society. Eur J Endocrinol. 2019;180(4):P23–P54. doi: 10.1530/EJE-18-0736. [DOI] [PubMed] [Google Scholar]
- 42.Sassi F, Tamone C, D’Amelio P. Vitamin D: nutrient, hormone, and immunomodulator. Nutrients. 2018;10(11):1656. doi: 10.3390/nu10111656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hahn J, Cook NR, Alexander EK, Friedman S, Walter J, Bubes V, Kotler G, Lee IM, Manson JE, Costenbader KH. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ. 2022;376:e066452. doi: 10.1136/bmj-2021-066452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Charoenngam N, Shirvani A, Holick MF. Vitamin D and its potential benefit for the COVID-19 pandemic. Endocr Pract. 2021;27(5):484–493. doi: 10.1016/j.eprac.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seal KH, Bertenthal D, Carey E, Grunfeld C, Bikle DD, Lu CM. Association of vitamin D status and COVID-19-related hospitalization and mortality. J Gen Intern Med. 2022;37(4):853–861. doi: 10.1007/s11606-021-07170-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jolliffe DA, Holt H, Greenig M, Talaei M, Perdek N, Pfeffer P, Maltby S, Symons J, Barlow NL, Normandale A, Garcha R, Richter AG, Faustini SE, Orton C, Ford D, Lyons RA, Davies GA, Kee F, Griffiths CJ, Norrie J, Sheikh A, Shaheen SO, Relton C, Martineau AR. Vitamin D supplements for prevention of COVID-19 or other acute respiratory infections: a phase 3 randomized controlled trial (CORONAVIT) BMJ. 2022;378:e071230. doi: 10.1136/bmj-2022-071230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dunlop E, Kiely M, James AP, Singh T, Black LJ. Efficacy of vitamin D food fortification and biofortification in children and adults: a systematic review protocol. JBI Evid Synth. 2020;18(12):2694–2703. doi: 10.11124/JBISRIR-D-19-00373. [DOI] [PubMed] [Google Scholar]
- 48.Jan Y, Malik M, Yaseen M, Ahmad S, Imran M, Rasool S, Haq A. Vitamin D fortification of foods in India: present and past scenario. J Steroid Biochem Mol Biol. 2019;193:105417. doi: 10.1016/j.jsbmb.2019.105417. [DOI] [PubMed] [Google Scholar]
- 49.Blunt JW, Tanaka Y, DeLuca HF. Biological activity of 25-hydroxycholecalciferol, a metabolite of vitamin D3. Proc Natl Acad Sci USA. 1968;61(4):1503–1506. doi: 10.1073/pnas.61.4.1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cesareo R, Falchetti A, Attanasio R, Tabacco G, Naciu AM, Palermo A. Hypovitaminosis D: is it time to consider the use of calcifediol? Nutrients. 2019;11(5):1016. doi: 10.3390/nu11051016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Quesada-Gomez JM, Bouillon R. Is calcifediol better than cholecalciferol for vitamin D supplementation? Osteoporos Int. 2018;29(8):1697–1711. doi: 10.1007/s00198-018-4520-y. [DOI] [PubMed] [Google Scholar]
- 52.Thompson GR, Lewis B, Booth CC. Absorption of vitamin D3–3H in control subjects and patients with intestinal malabsorption. J Clin Invest. 1966;45(1):94–102. doi: 10.1172/JCI105327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davies M, Mawer EB, Krawitt EL. Comparative absorption of vitamin D3 and 25-hydroxyvitamin D3 in intestinal disease. Gut. 1980;21(4):287–292. doi: 10.1136/gut.21.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sitrin MD, Bengoa JM. Intestinal absorption of cholecalciferol and 25-hydroxycholecalciferol in chronic cholestatic liver disease. Am J Clin Nutr. 1987;46(6):1011–1015. doi: 10.1093/ajcn/46.6.1011. [DOI] [PubMed] [Google Scholar]
- 55.Charoenngam N, Kalajian TA, Shirvani A, Yoon GH, Desai S, McCarthy A, Apovian CM, Holick MF. A pilot-randomized, double-blind crossover trial to evaluate the pharmacokinetics of orally administered 25-hydroxyvitamin D3 and vitamin D3 in healthy adults with differing BMI and in adults with intestinal malabsorption. Am J Clin Nutr. 2021;114(3):1189–1199. doi: 10.1093/ajcn/nqab123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cianferotti L, Cricelli C, Kanis JA, Nuti R, Reginster JY, Ringe JD, Rizzoli R, Brandi ML. The clinical use of vitamin D metabolites and their potential developments: a position statement from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Osteoporosis Foundation (IOF) Endocrine. 2015;50(1):12–26. doi: 10.1007/s12020-015-0606-x. [DOI] [PubMed] [Google Scholar]
- 57.Cesareo R, Attanasio R, Caputo M, Castello R, Chiodini I, Falchetti A, Guglielmi R, Papini E, Santonati A, Scillitani A, Toscano V, Triggiani V, Vescini F, Zini M, AME and Italian AACE Chapter Italian Association of Clinical Endocrinologists (AME) and Italian Chapter of the American Association of Clinical Endocrinologists (AACE) position statement: clinical management of vitamin D deficiency in adults. Nutrients. 2018;10(5):546. doi: 10.3390/nu10050546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Casado E, Quesada JM, Naves M, Peris P, Jódar E, Giner M, Neyro JL, Del Pino J, Sosa M, De Paz HD, Blanch-Rubió J. SEIOMM recommendations on the prevention and treatment of vitamin D deficiency. Rev Osteoporos Metab Miner. 2021;13:84–97. doi: 10.4321/S1889-836X2021000200007. [DOI] [Google Scholar]
- 59.Robien K, Oppeneer SJ, Kelly JA, Hamilton-Reeves JM. Drug-vitamin D interactions: a systematic review of the literature. Nutr Clin Pract. 2013;28(2):194–208. doi: 10.1177/0884533612467824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bischoff-Ferrari HA, Dawson-Hughes B, Stöcklin E, Sidelnikov E, Willett WC, Edel JO, Stähelin HB, Wolfram S, Jetter A, Schwager J, Henschkowski J, von Eckardstein A, Egli A. Oral supplementation with 25(OH)D3 versus vitamin D3: effects on 25(OH)D levels, lower extremity function, blood pressure, and markers of innate immunity. J Bone Miner Res. 2012;27(1):160–169. doi: 10.1002/jbmr.551. [DOI] [PubMed] [Google Scholar]
- 61.Cashman KD, Seamans KM, Lucey AJ, Stöcklin E, Weber P, Kiely M, Hill TR. Relative effectiveness of oral 25-hydroxyvitamin D3 and vitamin D3 in raising wintertime serum 25-hydroxyvitamin D in older adults. Am J Clin Nutr. 2012;95(6):1350–1356. doi: 10.3945/ajcn.111.031427. [DOI] [PubMed] [Google Scholar]
- 62.Jetter A, Egli A, Dawson-Hughes B, Staehelin HB, Stoecklin E, Goessl R, Henschkowski J, Bischoff-Ferrari HA. Pharmacokinetics of oral vitamin D(3) and calcifediol. Bone. 2014;59:14–19. doi: 10.1016/j.bone.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 63.Catalano A, Morabito N, Basile G, Cucinotta D, Lasco A. Calcifediol improves lipid profile in osteopenic atorvastatin-treated postmenopausal women. Eur J Clin Invest. 2015;45(2):144–149. doi: 10.1111/eci.12390. [DOI] [PubMed] [Google Scholar]
- 64.Jakobsen J, Andersen EAW, Christensen T, Andersen R, Bügel S. Vitamin D vitamers affect vitamin d status differently in young healthy males. Nutrients. 2017;10(1):12. doi: 10.3390/nu10010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vaes AMM, Tieland M, de Regt MF, Wittwer J, van Loon LJC, de Groot LCPGM. Dose-response effects of supplementation with calcifediol on serum 25-hydroxyvitamin D status and its metabolites: a randomized controlled trial in older adults. Clin Nutr. 2018;37(3):808–814. doi: 10.1016/j.clnu.2017.03.029. [DOI] [PubMed] [Google Scholar]
- 66.Graeff-Armas LA, Bendik I, Kunz I, Schoop R, Hull S, Beck M. Supplemental 25-hydroxycholecalciferol is more effective than cholecalciferol in raising serum 25-hydroxyvitamin D concentrations in older adults. J Nutr. 2020;150(1):73–81. doi: 10.1093/jn/nxz209. [DOI] [PubMed] [Google Scholar]
- 67.Pérez-Castrillón JL, Dueñas-Laita A, Brandi ML, Jódar E, Del Pino-Montes J, Quesada-Gómez JM, Cereto Castro F, Gómez-Alonso C, Gallego López L, Olmos Martínez JM, Alhambra Expósito MR, Galarraga B, González-Macías J, Bouillon R, Hernández-Herrero G, Fernández-Hernando N, Arranz-Gutiérrez P, Chinchilla SP. Calcifediol is superior to cholecalciferol in improving vitamin D status in postmenopausal women: a randomized trial. J Bone Miner Res. 2021;36(10):1967–1978. doi: 10.1002/jbmr.4387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shieh A, Lee SM, Lagishetty V, Gottleib C, Jacobs JP, Adams JS. Pilot trial of vitamin D3 and calcifediol in healthy vitamin D deficient adults: does it change the fecal microbiome? J Clin Endocrinol Metab. 2021;106(12):3464–3476. doi: 10.1210/clinem/dgab573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shieh A, Ma C, Chun RF, Witzel S, Rafison B, Contreras HTM, Wittwer-Schegg J, Swinkels L, Huijs T, Hewison M, Adams JS. Effects of cholecalciferol vs calcifediol on total and free 25-hydroxyvitamin D and parathyroid hormone. J Clin Endocrinol Metab. 2017;102(4):1133–1140. doi: 10.1210/jc.2016-3919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ruggiero C, Baroni M, Bini V, Brozzetti A, Parretti L, Zengarini E, Lapenna M, Antinolfi P, Falorni A, Mecocci P, Boccardi V. Effects of weekly supplementation of cholecalciferol and calcifediol among the oldest-old people: findings from a randomized pragmatic clinical trial. Nutrients. 2019;11(11):2778. doi: 10.3390/nu11112778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Corrado A, Rotondo C, Cici D, Berardi S, Cantatore FP. Effects of different vitamin D supplementation schemes in post-menopausal women: a monocentric open-label randomized study. Nutrients. 2021;13(2):380. doi: 10.3390/nu13020380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Navarro-Valverde C, Sosa-Henríquez M, Alhambra-Expósito MR, Quesada-Gómez JM. Vitamin D3 and calcidiol are not equipotent. J Steroid Biochem Mol Biol. 2016;164:205–208. doi: 10.1016/j.jsbmb.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 73.Carmel AS, Shieh A, Bang H, Bockman RS. The 25(OH)D level needed to maintain a favorable bisphosphonate response is ≥33 ng/ml. Osteoporos Int. 2012;23(10):2479–2487. doi: 10.1007/s00198-011-1868-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.da Rocha VM, Faria MBB, Júnior FADR, Lima COGX, Fiorelli RKA, Cassiano KM. Use of bisphosphonates, calcium and vitamin D for bone demineralization in patients with human immunodeficiency virus/acquired immune deficiency syndrome: a systematic review and meta-analysis of clinical trials. J Bone Metab. 2020;27(3):175–186. doi: 10.1100/jbm.2020.27.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Need AG, Morris HA, Horowitz M, Nordin C. Effects of skin thickness, age, body fat, and sunlight on serum 25-hydroxyvitamin D. Am J Clin Nutr. 1993;58(6):882–885. doi: 10.1093/ajcn/58.6.882. [DOI] [PubMed] [Google Scholar]
- 76.Carrelli A, Bucovsky M, Horst R, Cremers S, Zhang C, Bessler M, Schrope B, Evanko J, Blanco J, Silverberg SJ, Stein EM. Vitamin D storage in adipose tissue of obese and normal weight women. J Bone Miner Res. 2017;32(2):237–242. doi: 10.1002/jbmr.2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr. 2008;88:582S–586S. doi: 10.1093/ajcn/88.2.582S. [DOI] [PubMed] [Google Scholar]
- 78.Migliaccio S, Di Nisio A, Mele C, Scappaticcio L, Savastano S, Colao A, Obesity Programs of nutrition, Education, Research and Assessment (OPERA) Group Obesity and hypovitaminosis D: causality or casualty? Int J Obes Suppl. 2019;9(1):20–31. doi: 10.1038/s41367-019-0010-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Elkhwanky MS, Kummu O, Piltonen TT, Laru J, Morin-Papunen L, Mutikainen M, Tavi P, Hakkola J. Obesity represses CYP2R1, the vitamin D 25-hydroxylase, in the liver and extrahepatic tissues. JBMR Plus. 2020;4(11):e10397. doi: 10.1002/jbm4.10397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Roizen JD, Long C, Casella A, O’Lear L, Caplan I, Lai M, Sasson I, Singh R, Makowski AJ, Simmons R, Levine MA. Obesity decreases hepatic 25-hydroxylase activity causing low serum 25-hydroxyvitamin D. Bone Miner Res. 2019;34(6):1068–1073. doi: 10.1002/jbmr.3686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Aatsinki SM, Elkhwanky MS, Kummu O, Karpale M, Buler M, Viitala P, Rinne V, Mutikainen M, Tavi P, Franko A, Wiesner RJ, Chambers KT, Finck BN, Hakkola J. Fasting-induced transcription factors repress vitamin D bioactivation, a mechanism for vitamin D deficiency in diabetes. Diabetes. 2019;68(5):918–931. doi: 10.2337/db18-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.EU Union Register of Medicinal Products. Calcifediol. Summary of Product Characteristics. https://mri.cts-mrp.eu/Human/Downloads/ES_H_0412_001_FinalSPC.pdf
- 83.García Doladé N, Cereza García G, Madurga Sanz M, Montero Corominas D. Riesgo de hipercalcemia e hipervitaminosis D por calcifediol. Revisión de casos notificados al Sistema Español de Farmacovigilancia [Risk of hypercalcemia and hipervitaminosis D induced by calcifediol. Review of cases reported to the Spanish Pharmacovigilance System] Med Clin (Barc) 2013;141(2):88–89. doi: 10.1016/j.medcli.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 84.Olmos JM, Arnaiz F, Hernández JL, Olmos-Martínez JM, González-Macías J. Calcifediol mensual frente a calcifediol quincenal en el tratamiento de pacientes osteoporóticos. Estudio en la vida real [Monthly versus biweekley calcifediol in the treatment of osteoporotic patients. Study in real life] Rev Osteoporos Metab Miner. 2018;10:89–95. doi: 10.4321/s1889-836x2018000200005. [DOI] [Google Scholar]
- 85.Andújar-Espinosa R, Salinero-González L, Illán-Gómez F, Castilla-Martínez M, Hu-Yang C, Ruiz-López FJ. Effect of vitamin D supplementation on asthma control in patients with vitamin D deficiency: the ACVID randomised clinical trial. Thorax. 2021;76(2):126–133. doi: 10.1136/thoraxjnl-2019-213936. [DOI] [PubMed] [Google Scholar]
- 86.Varsavsky M, Rozas Moreno P, Becerra Fernández A, Luque Fernández I, Quesada Gómez JM, Ávila Rubio V, García Martín A, Cortés Berdonces M, Naf Cortés S, Romero Muñoz M, Reyes García R, Jódar Gimeno E, Muñoz Torres M, en representación del Grupo de Trabajo de Osteoporosis y Metabolismo Mineral de la Sociedad Española de Endocrinología y Nutrición Recommended vitamin D levels in the general population. Endocrinol Diabetes Nutr. 2017;64(Suppl 1):7–14. doi: 10.1016/j.endinu.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 87.AIFA (Italian Medicines Agency). Gazzetta Ufficiale Della Repubblica Italiana, Serie generale–n 252. https://www.aifa.gov.it/documents/20142/1030827/Determina_n.1533_2019_Nota96.pdf
- 88.Balvers MG, Brouwer-Brolsma EM, Endenburg S, de Groot LC, Kok FJ, Gunnewiek JK. Recommended intakes of vitamin D to optimise health, associated circulating 25-hydroxyvitamin D concentrations, and dosing regimens to treat deficiency: workshop report and overview of current literature. J Nutr Sci. 2015;4:e23. doi: 10.1017/jns.2015.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Vaes AMM, Tieland M, Toussaint N, Nilwik R, Verdijk LB, van Loon LJC, de Groot LCPGM. Cholecalciferol or 25-hydroxycholecalciferol supplementation does not affect muscle strength and physical performance in prefrail and frail older adults. J Nutr. 2018;148(5):712–720. doi: 10.1093/jn/nxy024. [DOI] [PubMed] [Google Scholar]
- 90.Gonnelli S, Tomai Pitinca MD, Camarri S, Lucani B, Franci B, Nuti R, Caffarelli C. Pharmacokinetic profile and effect on bone markers and muscle strength of two daily dosage regimens of calcifediol in osteopenic/osteoporotic postmenopausal women. Aging Clin Exp Res. 2021;33(9):2539–2547. doi: 10.1007/s40520-020-01779-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Iolascon G, Moretti A, de Sire A, Calafiore D, Gimigliano F. Effectiveness of calcifediol in improving muscle function in post-menopausal women: a prospective cohort study. Adv Ther. 2017;34(3):744–752. doi: 10.1007/s12325-017-0492-0. [DOI] [PubMed] [Google Scholar]
- 92.Andújar-Espinosa R, Aparicio-Vicente M, Ruiz-López FJ, Salinero-González L. Influence of vitamin D supplementation on the quality of life of asthma patients: findings from ACVID randomised clinical trial. Respir Med. 2021;185:106484. doi: 10.1016/j.rmed.2021.106484. [DOI] [PubMed] [Google Scholar]
- 93.Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, Alcalá Díaz JF, López Miranda J, Bouillon R, Quesada Gomez JM. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study. J Steroid Biochem Mol Biol. 2020;203:105751. doi: 10.1016/j.jsbmb.2020.105751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Maghbooli Z, Sahraian MA, Jamalimoghadamsiahkali S, Asadi A, Zarei A, Zendehdel A, Varzandi T, Mohammadnabi S, Alijani N, Karimi M, Shirvani A, Holick MF. Treatment with 25-hydroxyvitamin D3 (calcifediol) is associated with a reduction in the blood neutrophil-to-lymphocyte ratio marker of disease severity in hospitalized patients with COVID-19: a pilot multicenter, randomized, placebo-controlled, double-blinded clinical trial. Endocr Pract. 2021;27(12):1242–1251. doi: 10.1016/j.eprac.2021.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Alcala-Diaz JF, Limia-Perez L, Gomez-Huelgas R, Martin-Escalante MD, Cortes-Rodriguez B, Zambrana-Garcia JL, Entrenas-Castillo M, Perez-Caballero AI, López-Carmona MD, Garcia-Alegria J, Lozano Rodríguez-Mancheño A, Arenas-de Larriva MDS, Pérez-Belmonte LM, Jungreis I, Bouillon R, Quesada-Gomez JM, Lopez-Miranda J. Calcifediol treatment and hospital mortality due to COVID-19: a cohort study. Nutrients. 2021;13(6):1760. doi: 10.3390/nu13061760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nogues X, Ovejero D, Pineda-Moncusí M, Bouillon R, Arenas D, Pascual J, Ribes A, Guerri-Fernandez R, Villar-Garcia J, Rial A, Gimenez-Argente C, Cos ML, Rodriguez-Morera J, Campodarve I, Quesada-Gomez JM, Garcia-Giralt N. Calcifediol treatment and COVID-19-related outcomes. J Clin Endocrinol Metab. 2021;106(10):e4017–e4027. doi: 10.1210/clinem/dgab405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Loucera C, Peña-Chilet M, Esteban-Medina M, Muñoyerro-Muñiz D, Villegas R, Lopez-Miranda J, Rodriguez-Baño J, Túnez I, Bouillon R, Dopazo J, Quesada Gomez JM. Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients. Sci Rep. 2021;11(1):23380. doi: 10.1038/s41598-021-02701-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Oristrell J, Oliva JC, Casado E, Subirana I, Domínguez D, Toloba A, Balado A, Grau M. Vitamin D supplementation and COVID-19 risk: a population-based, cohort study. J Endocrinol Invest. 2022;45(1):167–179. doi: 10.1007/s40618-021-01639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sprague SM, Silva AL, Al-Saghir F, Damle R, Tabash SP, Petkovich M, Messner EJ, White JA, Melnick JZ, Bishop CW. Modified-release calcifediol effectively controls secondary hyperparathyroidism associated with vitamin D insufficiency in chronic kidney disease. Am J Nephrol. 2014;40(6):535–545. doi: 10.1159/000369939. [DOI] [PubMed] [Google Scholar]
- 100.Sprague SM, Crawford PW, Melnick JZ, Strugnell SA, Ali S, Mangoo-Karim R, Lee S, Petkovich PM, Bishop CW. Use of extended-release calcifediol to treat secondary hyperparathyroidism in stages 3 and 4 chronic kidney disease. Am J Nephrol. 2016;44(4):316–325. doi: 10.1159/000450766. [DOI] [PubMed] [Google Scholar]
- 101.Barbagallo M, Veronese N, Di Prazza A, Pollicino F, Carruba L, La Carrubba A, Dominguez LJ. Effect of calcifediol on physical performance and muscle strength parameters: a systematic review and meta-analysis. Nutrients. 2022;14(9):1860. doi: 10.3390/nu14091860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Quesada-Gomez JM, Lopez-Miranda J, Entrenas-Castillo M, Casado-Díaz A, Nogues Y, Solans X, Mansur JL, Bouillon R. Vitamin D endocrine system and COVID-19: treatment with calcifediol. Nutrients. 2022;14(13):2716. doi: 10.3390/nu14132716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cozzolino M, Ketteler M. Evaluating extended-release calcifediol as a treatment option for chronic kidney disease-mineral and bone disorder (CKD-MBD) Expert Opin Pharmacother. 2019;20(17):2081–2093. doi: 10.1080/14656566.2019.1663826. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.