Abstract
Antimicrobial resistance is a global health threat. Among Gram-negative bacteria, resistance to carbapenems, a class of β-lactam antibiotics, is usually a proxy for difficult-to-treat resistance, since carbapenem-resistant organisms are often resistant to many classes of antibiotics. Carbapenem resistance in the Gram-negative pathogen Klebsiella pneumoniae is mostly due to the production of carbapenemases, enzymes able to hydrolyze carbapenems, and K. pneumoniae carbapenemase (KPC)-type enzymes are overall the most prevalent carbapenemases in K. pneumoniae. In the last decade, the management of severe infections due to KPC-producing K. pneumoniae (KPC-Kp) in humans has presented many peculiar challenges to clinicians worldwide. In this perspective, we discuss how the treatment of severe KPC-Kp infections has evolved over the last decades, guided by the accumulating evidence from clinical studies, and how recent advances in diagnostics have allowed to anticipate identification of KPC-Kp in infected patients.
KEY MESSAGES
In the last decade, the management of severe infections due to KPC-Kp has presented many peculiar challenges to clinicians worldwide
Following the introduction in clinical practice of novel β-lactam/β-lactamase inhibitor combinations and novel β-lactams active against KPC-producing bacteria, the management of severe KPC-Kp infections has witnessed a remarkable evolution
Treatment of severe KPC-Kp infections is a highly dynamic process, in which the wise use of novel antimicrobials should be accompanied by a continuous refinement based on evolving clinical evidence and laboratory diagnostics
Keywords: BL-BLI, KPC, cefiderocol, ceftazidime-avibactam, imipenem-relebactam, meropenem-vaborbactam, rapid tests, early diagnosis
Introduction
Antimicrobial resistance has been estimated to cause at least 700,000 people deaths worldwide each year, possibly rising to 10 million by 2050 [1]. Since early 1990s, resistance to carbapenems, a class of β-lactam antibiotics, has been reported with increasing frequency among Gram-negative bacteria [2], usually as a proxy for difficult-to-treat resistance. Indeed, carbapenem-resistant organisms are often resistant to many classes of antibiotics, thereby complicating the treatment of infections caused by these bacteria in humans [3].
Among major Gram-negative pathogens, Klebsiella pneumoniae is one of the most affected by carbapenem resistance. In this species, carbapenem resistance is mostly due to the production of β-lactamases able to hydrolyze carbapenems (i.e. carbapenemases), although combinations of other different mechanisms may also occur [4,5]. K. pneumoniae carbapenemase (KPC)-type enzymes are overall the most prevalent acquired carbapenemases in K. pneumoniae and became of major relevance after their emergence and global spread during the first decade of the 21st century [6]. KPC enzymes belong to molecular class A of β-lactamases (Ambler classification), whose active site contains a serine residue, are usually plasmid-encoded, and are able to hydrolyze a very broad spectrum of β-lactam substrates, including penicillins, cephalosporins, monobactams and carbapenems. They are weakly inhibited by traditional β-lactam inhibitors (i.e. clavulanic acid and tazobactam), but efficiently inhibited by the novel β-lactamase inhibitors (i.e. diazabicyclooctanes and boronates) [7,8].
In the last decade, following the introduction in clinical practice of novel β-lactam/β-lactamase inhibitor combinations and novel β-lactams active against KPC-producing bacteria, the management of severe infections due to KPC-producing K. pneumoniae (KPC-Kp) in humans has witnessed a remarkable evolution. In this perspective, we discuss how the treatment of severe KPC-Kp infections has evolved over the last decades, guided by the accumulating evidence from clinical studies, and how recent advances in diagnostics have allowed to anticipate identification of KPC-Kp in infected patients.
Evolution of treatment algorithms and clinical studies
The old era (2013–2018)
Back to the early 2010s, the treatment of severe infections due to KPC-Kp mostly relied on combinations of two or even three antibacterial agents, almost invariably including a polymyxin or an aminoglycoside, that belong to two classes of antibiotics potentially associated with significant nephrotoxicity [9,10]. To understand such a peculiar prescribing pattern, it should be first reminded that, besides being resistant to carbapenems, KPC-Kp are very often resistant to other classes of commonly used antibiotics, such as penicillins, third and fourth-generation cephalosporins, and fluoroquinolones (owing both to the broad spectrum of activity of KPC-type enzymes against β-lactams other than carbapenems and to the genetic linkage of blaKPC to other resistance determinants located on the same plasmid, commonly including genes conferring resistance to aminoglycosides, quinolones, trimethoprim, sulphonamides, and tetracyclines) [11,12]. It was thus not uncommon for aminoglycosides or, more frequently, polymyxins, to remain the only class/classes of antibiotics showing in vitro activity against KPC-Kp isolates from infected patients, and polymyxins were thus frequently selected as first-line treatment.
The fact that polymyxins retained activity against KPC-Kp on most occasions was no surprise. Polymyxins, of which those currently available for use in humans are polymyxin B and polymyxin E (the latter also known as colistin), are bactericidal lipopeptides mainly exerting their antimicrobial activity through interaction with the lipopolysaccharide of Gram-negative bacteria and permeabilization of their outer membrane [13]. They became available in the 1950s, but their use in humans was soon abandoned, with few exceptions, because of concerns about their nephrotoxicity and the concomitant availability of other less toxic classes of antibiotics. The lack of widespread use of polymyxins for several decades is thought to have massively relieved the selective pressure for polymyxin resistance in human pathogens, thereby justifying the very high frequency of susceptibility even among KPC-Kp isolates when, at the beginning of the current century, polymyxins started to be used again and conspicuously, for the treatment of severe infections due carbapenem-resistant Gram-negative bacteria. However, crude mortality rates of severe KPC-Kp infections treated with polymyxins were generally higher than those registered in patients with severe infections due to carbapenem-susceptible Kp (CS-Kp) infections treated with carbapenems [14]. The reasons for such worse mortality rates are still not completely clear even today. The principal suspected culprits are a suboptimal efficacy of polymyxins and an increased frequency of inappropriate empirical therapy in KPC-Kp infections than in CS-Kp infections. Other reasons such as increased KPC-Kp virulence are overall far less likely, although still remaining to be definitely ruled out [14,15]. Suboptimal efficacy of polymyxins is a plausible argument. Certainly, polymyxins have been tremendously useful for treating severe KPC-Kp infections in the last 20 years (in the presence of scant alternatives), but several shortcomings could have played a role in unfavorably influencing their efficacy. The first is that also studies on the pharmacokinetic/pharmacodynamic (PK/PD) properties of polymyxins were largely abandoned starting from the middle of the past century, therefore, around twenty years ago, the available PK/PD data guiding administration of polymyxins were not updated according to current standards. For example, it is now known that intravenous polymyxins have a reduced lung penetration and that, for colistin, there could be an interpatient variability in the conversion of the prodrug (colistimethate) into the active moiety (colistin) [16]. In addition, some other factors likely and unfavorably influenced efficacy of polymyxins before the availability of updated PK/PD guidance (the international guidelines for optimizing the use of polymyxins in clinical practice, that represented the sum of all the crucial efforts of different research groups worldwide, were released only at the beginning of 2019) [15]. In the early 2010s, colistin maintenance dosages were usually of 6 million international units (MIU), and without a loading dose, whereas it is now well recognized that maintenance doses in patients with normal kidney function should be of 9 MIU daily (and possibly even >9 MIU in critically ill patients with augmented renal clearance), after an initial loading dose of 9 MIU [17]. In addition, gradient tests were widely used for colistin susceptibility testing at the time, but it was lately recognized that false susceptibility results could arise in a non-negligible proportion of cases [18].
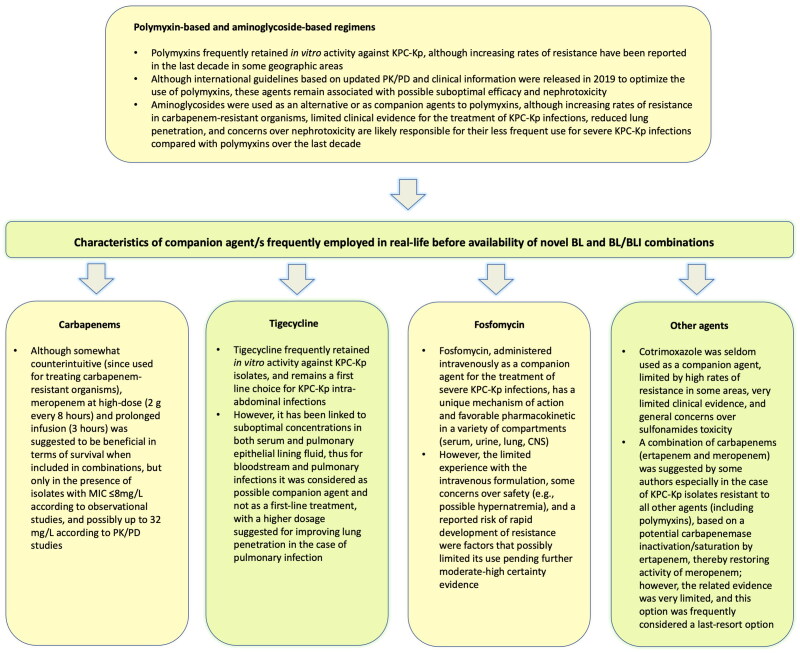
The suspicion of reduced polymyxins efficacy eventually led clinicians to consider the addition of other agents to polymyxins, in turn leading to the administration of polymyxin-based combination regimens (see Figure 1 for a summary of the most frequently used companion agents and of their characteristics). Polymyxin-based combination regimens have been used for many years between 2010 and 2018. During the same period, many observational studies were conducted to compare clinical outcomes (mainly short-term mortality) between patients with severe KPC-Kp infections treated with polymyxin monotherapy and patients with severe KPC-Kp infections treated with polymyxin-based combinations. However, although some large Italian and Greek studies suggested an advantage of combinations over monotherapy in terms of mortality, this topic remained debated for several years, partly due to many inherent weaknesses of observational, nonrandomized studies in evaluating this topic [19,20]. In 2017, the results of the large, multinational INCREMENT study seemed to tip the balance more solidly in favor of combinations, although certainty of evidence still remained low due to the observational, retrospective nature of the study [35]. Furthermore, as shown in Figure 1, the employed combinations were highly heterogeneous (they were mostly colistin-based regimens, but with heterogeneous companion agent/s). Such a large heterogeneity in the type of selected companion agent/s possibly reflected the lack of high-level evidence (and, in turn, solid guidelines) dictating which combinations to use in the different clinical scenarios.
Figure 1.
Combination therapies frequently employed before availability of novel β-lactam/β-lactam inhibitor (BL/BLI) combinations and β-lactams (BL) for the treatment of severe infections caused by KPC-producing Klebsiella pneumoniae. CNS: central nervous system; KPC-Kp: Klebsiella pneumoniae carbapenemase-producing Klebsiella pneumoniae; MIC: minimum inhibitory concentration; PK/PD: pharmacokinetic/pharmacodynamic. Information included in the table is from Refs. [9,15,19–34].
Overall, while certainly having been useful for improving our ability to treat severe KPC-Kp infections with the few available agents from 2010 to 2018, observational studies conducted in those years eventually led to sufficient consensus only after 2017. This is not a criticism, but rather a consideration reminding us about the importance of the following: (i) pursuing high certainty evidence from randomized controlled trials; (ii) improving national and multinational efforts to conduct large and well-designed observational studies (to provide lower but still acceptable evidence whenever randomized studies are unfeasible). Indeed, although we now have novel agents that have revolutionized the treatment of severe KPC-Kp infections (see next section), we cannot exclude that we will face again a similar situation in the future, since antimicrobial resistance has proved to be highly dynamic and disseminate very rapidly. We should not remain unprepared.
The era of novel β-lactam/β-lactamase inhibitor combinations and β-lactams active against KPC-Kp (2019–onward)
Novel β-lactam/β-lactamase inhibitor (BL/BLI) combinations showing in vitro activity against KPC-Kp and currently approved for use in humans are ceftazidime-avibactam, meropenem-vaborbactam, and imipenem-cilastatin-relebactam [8]. The first that became available is ceftazidime/avibactam (first approved by the Food and Drug Administration [FDA] and the European Medicines Agency [EMA] in 2015 and 2016 in the US and Europe, respectively), followed by meropenem/vaborbactam (first approved by the FDA and the EMA in 2017 and 2018, respectively) and imipenem/relebactam (first approved by the FDA and the EMA in 2019 and 2020, respectively). In addition, the recently approved siderophore cephalosporin cefiderocol (first approved by the FDA and the EMA in 2019 and 2020, respectively) also shows activity against KPC-Kp [36,37]. Two important considerations should be made regarding these novel agents. The first is that they made KPC-Kp treatable again with β-lactams, thereby removing the label of ‘difficult-to-treat resistance’ (i.e. resistance to all β-lactams and fluoroquinolones) [21]. The second is that, for some of these novel agents, besides classical indication-based randomized trials (e.g. patients with complicated urinary infection, nosocomial pneumonia), also pathogen-directed randomized trials (i.e. patients with carbapenem-resistant Gram-negative bacteria infections) were conducted [38,39]. Nonetheless, while these pathogen-directed studies are certainly a crucial innovation, it still remains difficult to enroll a high number of patients with infections due to resistant organisms (KPC-Kp included) in randomized trials, thus their populations are frequently small. This inherently reduces the potential to generalize their results, as well as possibly precluding adequate mitigation of both measured and unmeasured confounding. The solution to this issue is still debated. Indeed, it is also true that pragmatically widening the classically strict inclusion criteria of randomized trials (for allowing enrollment of larger samples of patients with infection due to resistant organisms) could confound results by leading to inclusion of several patients with other factors contributing to their prognosis (e.g. too severe acute conditions or high burden of baseline comorbidities). Novel designs and methods for randomized trials are in development or under evaluation for improving our ability to deal with this issue [40]. In the meantime, high certainty evidence guiding the use of novel agents for KPC-Kp infections remains mostly indirect, drawn from large, randomized trials conducted predominantly in patients with infection due to carbapenem-susceptible bacteria, and thus with some inherent uncertainty about the legitimacy of extrapolating results also to KPC-Kp infections.
Nonetheless, two important considerations can be firmly made: (i) differently from efficacy, safety can be more directly extrapolated to patients with KPC-Kp infections, with novel BL and BL/BLI combinations being less nephrotoxic than previously polymyxin-based or aminoglycoside-based regimens; (ii) initial observational evidence on the use of novel agents for treating severe KPC-Kp infections is suggesting lower mortality than previously registered with the use of previous standard of care [41,42]. Although with lower certainty of evidence than randomized trials, this observational evidence has guided the development of two much awaited guidance document/guidelines for the treatment of resistant organisms of concerns, including also KPC-Kp, from the infectious Diseases Society of America (IDSA) and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) [36,37]. A summary of current recommendations for the treatment of KPC-Kp infections, as well as of the evidence underlying their development, is available in Table 1. Certainly, there are still some important unanswered questions that will need to be addressed in the forthcoming years (e.g. to optimize the use of novel agents in patients with impaired renal function, renal replacement therapy, and/or pneumonia [43–46]), but it cannot be denied that we are entering a completely new era in the treatment of severe KPC-Kp infections. This also considering that other BL or BL/BLI showing in vitro activity against KPC-Kp such as ARX-1796, aztreonam/avibactam, cefepime/taniborbactam, cefepime/zidebactam, ceftaroline/avibactam, meropenem/nacubactam, ETX1317, QPX7728, and VNRX-7145 are under clinical development and may become available in the future [47].
Table 1.
Current IDSA and ESCMID recommendations for the treatment of severe infections caused by KPC-producing Klebsiella pneumoniae.
| Guidelines/Guidance document | Recommended treatment for severe KPC-Kp infections | Comments |
|---|---|---|
| ESCMID guidelines [36] |
|
|
| IDSA guidance document [37] (No strength of recommendation and level of evidence provided) |
|
|
CRE: carbapenem-resistant Enterobacterales; ESCMID: European Society of Clinical Microbiology and Infectious Diseases; GRADE: Grading of Recommendations Assessment, Development, and Evaluation; IDSA: Infectious Diseases Society of America; KPC-Kp: Klebsiella pneumoniae carbapenemase-producing Klebsiella pneumoniae.
The availability of novel agents is a true revolution and may help reducing the high mortality of KPC-Kp infections we frequently witnessed in the past decade. However, we should not let our guard down and allow indiscriminate use of these novel agents, in line with antimicrobial stewardship principles. Notably, this does not mean that we should not use novel agents, but that they will need to be used wisely and appropriately. Indeed, reports of resistance to novel agents are increasing worldwide. More in detail, resistance to ceftazidime/avibactam has been increasingly documented among KPC-Kp over the last few years, mostly owing to the emergence of mutated KPC variants [49], although other mechanisms (e.g. increased production of KPC, permeability defects, overexpression of efflux pumps, and production of other transferable – mutated – class A or class C and class D β-lactamases) may also contribute [49–53]. In addition, cases of KPC-Kp resistant also to meropenem/vaborbactam have been recently reported. To this regard, it should be noted that a marked overproduction of KPC associated with impairment of major porins may led to development of cross-resistance to ceftazidime/avibactam, meropenem/vaborbactam, and imipenem/relebactam in KPC-Kp [53–58]. Finally, some KPC variants have also been associated with reduced susceptibility to cefiderocol [59,60]. Concerted efforts aimed at slowing down the development of resistance to these novel agents are therefore needed to minimize this problem and its potential unfavorable impact on patients’ outcome in the forthcoming future.
The key role of the laboratory for the rapid diagnosis of KPC-Kp infections: what has changed over the years?
Until the first decade of the new century, from the diagnostic laboratory perspective, the principal strategies for the diagnosis of KPC-Kp infections were based on phenotypic screening followed by confirmatory tests. The screening relied upon the detection of a reduced susceptibility to carbapenems, since carbapenemase production does not necessarily confer resistance to carbapenems and may cause an increase in minimum inhibitory concentration (MIC) that remains below the clinical breakpoints for resistance. Nonsusceptibility to ertapenem was considered by the Clinical and Laboratory Standards Institute (CLSI) as the most sensitive indicator of carbapenemase production [61], while a meropenem MIC ≥ 0.125 mg/L (i.e. above the epidemiological cut-off value [ECOFF]) was considered the best compromise of sensitivity and specificity for screening of carbapenemase producers by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [62]. The phenotypic screening could be performed with standard antimicrobial susceptibility testing (AST), provided that the adopted system measured MIC values low enough to intercept the screening breakpoints, or disk diffusion was used.
Since a reduced carbapenem susceptibility could also be due to different mechanisms (e.g. outer membrane permeability defects coupled with production of extended-spectrum β-lactamases [ESBL]) [63], and since several different carbapenemases can be found in K. pneumoniae in addition to KPC (e.g. class B [IMP, VIM, NDM] or class D [OXA-48-like] β-lactamases), confirmatory tests were needed to confirm\rule out a carbapenemase activity and to identify the carbapenemase type [64]. The modified Hodge test (MHT) was initially recommended by CLSI to confirm carbapenemase production in isolates positive to the phenotypic screening [61]. However, this test proved difficult to interpret in some cases and suffered from several limitations (Table 2), which led the CLSI to abandon its endorsement in 2018. Easier and faster phenotypic tests for the detection of carbapenemase production were developed, such as the modified carbapenem inactivation method (mCIM) and the carba NP test. However, also these tests (like MHT) did not inform about the carbapenemase type [65], except for subsequent updates of carba NP which allow discrimination between the different classes of carbapenemases (i.e. classes A, B, and D) and identification of KPC producers [66]. Other phenotypic assays were developed based on the inhibitory properties that several molecules retain against KPC enzymes, such as boronic acid and its derivatives (i.e. phenylboronic [PBA] and 3-aminophenylboronic acid [APBA]), a feature exploited by combined-disk tests (CDTs), also known as disc-inhibitors synergy tests. CDTs, which are performed by comparing the diameter of the growth-inhibitory zone around an indicator β-lactam disk (containing cefepime or imipenem, meropenem and/or ertapenem) plus the inhibitor to that around the corresponding β-lactam disk alone, exhibit high sensitivities and specificities for the detection of KPC, and can also provide accurate information about isolates expressing KPC plus ESBL or class B carbapenemases (i.e. metallo-β-lactamases [MBL]) when coupled with inhibitors of these enzyme types (i.e. clavulanic acid for ESBL, and ethylenediaminetetraacetic acid [EDTA] for MBL) [65]. Following a similar approach, addition of PBA to gradient MIC strip susceptibility tests (e.g. E-test) has also been used as confirmation assay for recognition of KPC producers (or MBL using EDTA) [66,67]. Although these tests are simple, unexpensive, and relatively efficient in detecting specific carbapenemases, all require prior bacterial culture from the clinical specimen, so that the long time to results represents the main drawback for most of them (Table 2). Moreover, as with all phenotypic tests, potential false negative results can be achieved in the case of unexpressed or minimally expressed carbapenemase genes [68].
Table 2.
Overview of established laboratory methods for detection of KPC-type carbapenemases in patients with severe infections caused by KPC-producing Klebsiella pneumoniae.
| Time to results | Specimen | Information provided | Limitation(s) | Note | Commercial assay(s) | Ref. | ||
|---|---|---|---|---|---|---|---|---|
| Phenotypic tests | Modified Hodge test (MHT) | 18–24 h | Pure culture | Carbapenemase activity | • False-positive results for high-level AmpC producers or CTX-M-type ESBL producers • Weak detection of NDM producers |
Early CLSI-endorsed method | – | [64,65,69] |
| Modified carbapenemase inactivation method (mCIM) | 18–24 h | Pure culture | Carbapenemase activity | – | Laboratory developed test | – | [64,65,68] | |
| Gradient MIC strip | 18–24 h | Pure culture | Production of KPC or MBL | • Poor specificity with AmpC | – | ETEST® KPC | [66–68] | |
| (Multidisc) combined-disk tests (CDT) | 18–24 h | Pure culture | Production of KPC, MBL or OXA-48 | • Identification of carbapenemase Producers among AmpC-positive species (e.g. Enterobacter spp.) |
Laboratory developed test | – | [64,65,68] | |
| Carba NP test II | 30 min–2 h | Pure culture | Production of class A, B or D β-lactamases | • Weak detection of OXA-48 producers | CLSI-endorsed method | RAPIDEC® CARBA NP | [64,68,69] | |
| Genotypic tests | MALDI-TOF MS | 30 min | Pure culture | Identification of a gene product (often) accompanying KPC | • Alternate MALDI-TOF instrument Settings (on the usual instrument) • Identification limited by the presence of blaKPC aboard of pKpQIL-like plasmids |
– | – | [68,70] |
| Lateral flow immunoassay (LFIA) | 20 min | Pure culture, positive blood culture, rectal swab | Production of KPC, MBL (VIM, IMP, NDM), OXA-48-like | • Possible false-negative results with new enzyme variants • Non high throughput • False-negative results may occur with some KPC variants (e.g. KPC-31) • Unable to detect novel carbapenemases |
– | NG Test Carba 5® RESIST-4 O.K.N.V.® KPC K-SeT |
[68,71] | |
| PCR, real time-PCR | 50 min–4 h | Pure culture rectal swab | Detection of specific carbapenemase genes (e.g. blaKPC, blaNDM, blaIMP, blaVIM, blaOXA 48-like) | • Unable to detect novel carbapenemases | Include laboratory developed test | Hyperplex SuperBug ID Check-Direct CPE assay CRE ELITe MGB® kit Revogene® Carba C Novodiag® CarbaR+ AllPlexTM Entero-DR assay Xpert Carba-R test CARBAPLEX® |
[72,73] | |
| Loop-mediated isothermal amplification (LAMP) | 25 min | Pure culture | Detection of specific carbapenemase genes (e.g. blaKPC, blaNDM, blaIMP, blaVIM, blaOXA 48-like) | • Unable to detect novel carbapenemases | – | eazyplex® superBug | [72] | |
| Syndromic assay | 40 min–6 h | Positive blood culture, whole blood, respiratory sample, synovial fluid | Detection of specific carbapenemase genes (e.g. blaKPC, blaNDM, blaIMP, blaVIM, blaOXA 48-like) and pathogens | • Limited spectrum of target carbapenemases • Unable to detect novel carbapenemases • Multiple positive results or targets may complicate test interpretation • Higher cost than confirmatory molecular tests based on PCR\RT-PCR • False-positive results may occur • No detection of off-target pathogens |
Minimal hands-on time, highly automated | Biofire® FilmArray panels (Blood Culture Identification 2, Pneumonia Panel plus, Bone and Joint Infection) Unyvero® ePlex® BCID-GN panel Verigene® (BC-GN) T2Resistance Panel \ T2Bacteria Panel |
[74,75] | |
| Whole-genome sequencing (WGS) | 2 h–3 days | Pure culture | Detection of all resistance genes | • Need of trained microbiologists • Need of dedicated instrumentation, infrastructures • Longer time to results than other molecular assays |
Not yet FDA- / CE- IVD cleared | – | [76] | |
CE: Conformite Europeenne; CLSI: Clinical and Laboratory Standards Institute; CTX-M: active on cefotaxime, first isolated in Munich; ESBL: extended-spectrum β-lactamases; FDA: Food and Drug Administration; IMP: active on imipenem; IVD: in vitro diagnostic; KPC: Klebsiella pneumoniae carbapenemase; MALDI-TOF: matrix assisted laser desorption/ionization - time of flight; MBL: metallo-β-lactamases; MIC: minimum inhibitory concentration; NDM: New Delhi MBL; OXA: oxacillinase; PCR: polymerase chain reaction; TAT: turnaround time from pure culture of isolate; VIM: Verona integron-encoded.
The recent development of rapid multiplex lateral-flow immunochromatographic assays (LFIAs), based on immunological detection of epitopes of carbapenemase enzymes, has partially overcome the above limitations. LFIAs represent easy, rapid, and reliable confirmatory tests for the detection of the most widespread and clinically important carbapenemases found in Enterobacterales (i.e. NDM-, KPC-, IMP-, VIM-and OXA-48-like enzymes) from bacterial cultures on solid media and were also proven useful for the detection of carbapenemases directly from positive blood cultures with high sensitivities and specificities (>96%) [71,77]. It should be noted, however, that some recently emerged KPC variants showing reduced susceptibility to ceftazidime-avibactam (e.g. KPC-31) can be associated with relevant detection issues with LFIAs [78]. The possible use of matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) for the detection of a gene product encoded by the pKpQIL plasmid, the most successful genetic support driving the global spread of blaKPC, has also been investigated. This approach relies on the detection of a ∼11,109-Da mass peak corresponding to the cleavage product of a hypothetical protein (designated p019 or pKpQIL_019) that is fairly closely linked to pKpQIL-like plasmids, and could be of help for the rapid and unexpensive tracking of KPC-producing strains [70,79], although suffering from some limitations (Table 2).
During the past two decades, following the technological advances in diagnostics and the need to increase rapidity of microbiologic diagnosis, several molecular tools based on different nucleic acid amplification tests (NAATs) (e.g. real-time PCR and loop-mediated isothermal amplification), possibly in combination with microarrays, have rapidly taken a prominent place in the clinical laboratory [72,73]. Overall, NAATs are advantageous over phenotypic methods due to faster turnaround times, higher sensitivity, possible use directly with clinical samples, and ability to give direct information about the nature of the carbapenemase genes (Table 2), that nowadays has relevant therapeutic implications. In fact, while knowledge of the carbapenemase type was initially relevant only for epidemiological and infection control purposes, the exact and rapid identification of carbapenemase genes has become of the utmost importance following the advent of novel BL and BL/BLI combinations, which differentially cover class A, B and D carbapenemases [7,80]. Although in early stages NAATs mainly consisted of laboratory-developed assays, typically employed by diagnostic laboratories with advanced technical expertise, at present, several FDA-cleared and CE-cleared in vitro diagnostic (IVD) commercial assays are available in automated formats, of which some are also suitable for point-of-care testing. These assays allow for confirmation of blaKPC, as well as of other carbapenemase-encoding genes (i.e. blaNDM, blaIMP, blaVIM and blaOXA 48-like) from bacterial isolates exhibiting a reduced susceptibility to carbapenems or even directly from clinical specimens, with a short time to results (Table 2).
In the last decade, molecular testing of carbapenemase genes has also been incorporated into syndromic panels, providing a marked reduction of the time to diagnosis and significant benefits for antimicrobial stewardship for bloodstream infections, starting from positive blood cultures, for lower respiratory tract infections, starting from bronchoalveolar lavage or bronchial aspirate specimens, and for bone and joint infections, starting from synovial fluid [74] (Table 2); similar platforms can provide identification of the most common pathogens, and of the most clinically-relevant associated resistance genes, in a timeframe of 1–5 h directly from blood or deep respiratory samples [75,81], and invariably include the blaKPC target. However, although syndromic panels are powerful tools that may assist in a timely manner diagnosis of infections, it should also be noted that these assays only detect a predefined range of carbapenemases and/or pathogens, proving of major value only when they render a positive result. Moreover, in some cases, potential interpretation issues may occur upon detection of the KPC-encoding gene, since this does not always correlate with the susceptibility phenotype against certain β-lactamase inhibitors (i.e. the inhibitory activity of avibactam and vaborbactam can be hindered by the presence of overexpressed enzymes or mutated KPC variants) [82–84].
In recent years, identification of KPC-producing organisms has been increasingly centered on molecular testing, also including whole genome sequencing (WGS). Although WGS can potentially provide untapped information regarding novel KPC enzymes as well as the whole resistance genes’ content, not suffering from the major limitations of other molecular assays (i.e. off-target pathogens and/or carbapenemases), the long time to results, costs and infrastructure limitations actually make its implementation in the routine laboratory workflow a big challenge [76], so that its use is primarily demanded for epidemiological purposes.
Conclusion
As with other β-lactamases, a notable diversification has been observed with KPC enzymes, following their emergence in the clinical setting. Currently, at least 136 different allelic variants have been assigned (https://www.ncbi.nlm.nih.gov/pathogens/refgene/#KPC; last access on 30 November 2022), of which some already exhibit modification of the functional properties that may provide resistance also to the novel agents [85]. This should further remind us that the treatment of severe KPC-Kp infections is a highly dynamic process, in which the wise use of novel antimicrobials should be accompanied by a continuous refinement based on evolving clinical evidence and laboratory diagnostics. We should not waste all the tremendous steps forward made in the last decade.
Author contributions
DRG: conceptualization, supervision, writing of original draft, review, and editing; VDP, TG, and IK: writing of original draft, review and editing; AM, GMR, and MB: review and editing, supervision.
Disclosure statement
Outside the submitted work, DRG reports investigator-initiated grants from Pfizer, Shionogi, and Gilead Italia, and advisor/consultant and/or speaker’s bureau from Pfizer and Tillotts Pharma. Outside the submitted work, AM reports investigator-initiated grants from Gilead Italia. Outside the submitted work, VDP reports research grants from Seegene. Outside the submitted work, TG reports advisor/consultant and/or speaker’s bureau and/or research grants and/or personal fees from Alifax, bioMérieux, Thermo Fisher Scientific, Seegene, Accelerate Diagnostics, Merlin, VenatorX, and AstraZeneca. Outside the submitted work, GMR reports advisor/consultant and/or speaker’s bureau and/or research grants and/or personal fees from Accelerate, Angelini, Arrow, Becton Dickinson, Biomedical Service, bioMérieux, Cepheid, DID, Hain Lifescience GmbH, Menarini, Meridian, MSD, Nordic Pharma, Pfizer, Qiagen, Qlinea, Qpex, Quidel, Qvella, Roche, SD Biosensor, Seegene, Setlance, Shionogi, Symcel, Thermo Fisher, VenatorX, Zambon. Outside the submitted work, MB reports research grants and/or personal fees for advisor/consultant and/or speaker/chairman from Bayer, BioMérieux, Cidara, Cipla, Gilead, Menarini, MSD, Pfizer, and Shionogi.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
- 1.Shallcross LJ, Howard SJ, Fowler T, et al. Tackling the threat of antimicrobial resistance: from policy to sustainable action. Philos Trans R Soc Lond B Biol Sci. 2015;370(1670):20140082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta N, Limbago BM, Patel JB, et al. Carbapenem-resistant enterobacteriaceae: epidemiology and prevention. Clin Infect Dis. 2011;53(1):60–67. [DOI] [PubMed] [Google Scholar]
- 3.Giacobbe DR, Mikulska M, Viscoli C.. Recent advances in the pharmacological management of infections due to multidrug-resistant gram-negative bacteria. Expert Rev Clin Pharmacol. 2018;11(12):1219–1236. [DOI] [PubMed] [Google Scholar]
- 4.Munoz-Price LS, Poirel L, Bonomo RA, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13(9):785–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tzouvelekis LS, Markogiannakis A, Psichogiou M, et al. Carbapenemases in Klebsiella pneumoniae and other enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev. 2012;25(4):682–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bush K, Bradford PA.. Epidemiology of beta-lactamase-producing pathogens. Clin Microbiol Rev. 2020;33(2):e00047-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karaiskos I, Galani I, Papoutsaki V, et al. Carbapenemase producing Klebsiella pneumoniae: implication on future therapeutic strategies. Expert Rev Anti Infect Ther. 2022;20(1):53–69. [DOI] [PubMed] [Google Scholar]
- 8.Yahav D, Giske CG, Grāmatniece A, et al. New beta-lactam-beta-lactamase inhibitor combinations. Clin Microbiol Rev. 2020;34(1):e00115-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bassetti M, Giacobbe DR, Giamarellou H, et al. Management of KPC-producing Klebsiella pneumoniae infections. Clin Microbiol Infect. 2018;24(2):133–144. [DOI] [PubMed] [Google Scholar]
- 10.Tumbarello M, Viale P, Viscoli C, et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis. 2012;55(7):943–950. [DOI] [PubMed] [Google Scholar]
- 11.Papagiannitsis CC, Di Pilato V, Giani T, et al. Characterization of KPC-encoding plasmids from two endemic settings, Greece and Italy. J Antimicrob Chemother. 2016;71(10):2824–2830. [DOI] [PubMed] [Google Scholar]
- 12.Chen L, Mathema B, Chavda KD, et al. Carbapenemase-producing Klebsiella pneumoniae: molecular and genetic decoding. Trends Microbiol. 2014;22(12):686–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Z, Velkov T.. Polymyxins: mode of action. Adv Exp Med Biol. 2019;1145:37–54. [DOI] [PubMed] [Google Scholar]
- 14.Maraolo AE, Corcione S, Grossi A, et al. The impact of carbapenem resistance on mortality in patients With Klebsiella Pneumoniae bloodstream infection: an individual patient data meta-analysis of 1952 patients. Infect Dis Ther. 2021;10(1):541–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsuji BT, Pogue JM, Zavascki AP, et al. International consensus guidelines for the optimal use of the polymyxins: endorsed by the American College of Clinical Pharmacy (ACCP), european society of clinical microbiology and infectious diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-Infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. 2019;39(1):10–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nation RL, Forrest A.. Clinical pharmacokinetics, pharmacodynamics and toxicodynamics of polymyxins: implications for therapeutic use. Adv Exp Med Biol. 2019;1145:219–249. [DOI] [PubMed] [Google Scholar]
- 17.Giacobbe DR, Karaiskos I, Bassetti M.. How do we optimize the prescribing of intravenous polymyxins to increase their longevity and efficacy in critically ill patients? Expert Opin Pharmacother. 2022;23(1):5–8. [DOI] [PubMed] [Google Scholar]
- 18.Matuschek E, Ahman J, Webster C, et al. Antimicrobial susceptibility testing of colistin – evaluation of seven commercial MIC products against standard broth microdilution for Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter spp. Clin Microbiol Infect. 2018;24(8):865–870. [DOI] [PubMed] [Google Scholar]
- 19.Daikos GL, Tsaousi S, Tzouvelekis LS, et al. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections: lowering mortality by antibiotic combination schemes and the role of carbapenems. Antimicrob Agents Chemother. 2014;58(4):2322–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tumbarello M, Trecarichi EM, Rosa D, et al. Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrob Chemother. 2015;70(7):2133–2143. [DOI] [PubMed] [Google Scholar]
- 21.Kadri SS, Adjemian J, Lai YL, et al. Difficult-to-Treat resistance in gram-negative bacteremia at 173 US hospitals: retrospective cohort analysis of prevalence, predictors, and outcome of resistance to all first-line agents. Clin Infect Dis. 2018;67(12):1803–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Antonello RM, Di Bella S, Maraolo AE, et al. Fosfomycin in continuous or prolonged infusion for systemic bacterial infections: a systematic review of its dosing regimen proposal from in vitro, in vivo and clinical studies. Eur J Clin Microbiol Infect Dis. 2021;40(6):1117–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cojutti P, Sartor A, Righi E, et al. Population pharmacokinetics of high-dose continuous-infusion meropenem and considerations for use in the treatment of infections due to KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2017;61(10):e00794-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Del Bono V, Giacobbe DR, Marchese A, et al. Meropenem for treating KPC-producing Klebsiella pneumoniae bloodstream infections: should we get to the PK/PD root of the paradox? Virulence. 2017;8(1):66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duong A, Simard C, Wang YL, et al. Aminoglycosides in the intensive care unit: what Is new in population PK modeling? Antibiotics. 2021;10(5):507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giacobbe DR, Bono D, Trecarichi V, et al. Risk factors for bloodstream infections due to colistin-resistant KPC-producing Klebsiella pneumoniae: results from a multicenter case-control-control study. Clin Microbiol Infect. 2015;21(12):1106–1108. [DOI] [PubMed] [Google Scholar]
- 27.Giamarellou H, Poulakou G.. Pharmacokinetic and pharmacodynamic evaluation of tigecycline. Expert Opin Drug Metab Toxicol. 2011;7(11):1459–1470. [DOI] [PubMed] [Google Scholar]
- 28.Karaiskos I, Friberg LE, Pontikis K, et al. Colistin population pharmacokinetics after application of a loading dose of 9 MU colistin methanesulfonate in critically ill patients. Antimicrob Agents Chemother. 2015;59(12):7240–7248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monaco M, Giani T, Raffone M, et al. Colistin resistance superimposed to endemic carbapenem-resistant Klebsiella pneumoniae: a rapidly evolving problem in Italy. Euro Surveill. 2014;19(42):20939. [DOI] [PubMed] [Google Scholar]
- 30.Nation RL, Garonzik SM, Li J, et al. Updated US and european dose recommendations for intravenous colistin: how do they perform? Clin Infect Dis. 2016;62(5):552–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ni W, Han Y, Liu J, et al. Tigecycline treatment for carbapenem-resistant enterobacteriaceae infections: a systematic review and meta-analysis. Medicine. 2016;95(11):e3126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Panidis D, Markantonis SL, Boutzouka E, et al. Penetration of gentamicin into the alveolar lining fluid of critically ill patients with ventilator-associated pneumonia. Chest. 2005;128(2):545–552. [DOI] [PubMed] [Google Scholar]
- 33.Wang G, Yu W, Cui Y, et al. Optimal empiric treatment for KPC-2-producing Klebsiella pneumoniae infections in critically ill patients with normal or decreased renal function using monte carlo simulation. BMC Infect Dis. 2021;21(1):307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zha L, Pan L, Guo J, et al. Effectiveness and safety of high dose tigecycline for the treatment of severe infections: a systematic review and meta-analysis. Adv Ther. 2020;37(3):1049–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gutierrez-Gutierrez B, Salamanca E, de Cueto M, et al. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing enterobacteriaceae (INCREMENT): a retrospective cohort study. Lancet Infect Dis. 2017;17(7):726–734. [DOI] [PubMed] [Google Scholar]
- 36.Paul M, Carrara E, Retamar P, et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant gram-negative bacilli (endorsed by European Society of Intensive Care Medicine). Clin Microbiol Infect. 2021. [DOI] [PubMed] [Google Scholar]
- 37.Tamma PD, Aitken SL, Bonomo RA, et al. Infectious diseases society of america 2022 guidance on the treatment of extended-spectrum beta-lactamase producing enterobacterales (ESBL-E), carbapenem-resistant enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis. 2022;75(2):187–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bassetti M, Echols R, Matsunaga Y, et al. Efficacy and safety of cefiderocol or best available therapy for the treatment of serious infections caused by carbapenem-resistant gram-negative bacteria (CREDIBLE-CR): a randomised, open-label, multicentre, pathogen-focused, descriptive, phase 3 trial. Lancet Infect Dis. 2021;21(2):226–240. [DOI] [PubMed] [Google Scholar]
- 39.Wunderink RG, Giamarellos-Bourboulis EJ, Rahav G, et al. Effect and safety of meropenem-vaborbactam versus best-available therapy in patients with carbapenem-resistant enterobacteriaceae infections: the TANGO II randomized clinical trial. Infect Dis Ther. 2018;7(4):439–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Kraker MEA, Sommer H, de Velde F, et al. Optimizing the design and analysis of clinical trials for antibacterials against multidrug-resistant organisms: a white paper from COMBACTE's STAT-Net. Clin Infect Dis. 2018;67(12):1922–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tumbarello M, Trecarichi EM, Corona A, et al. Efficacy of ceftazidime-avibactam salvage therapy in patients with infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Clin Infect Dis. 2019;68(3):355–364. [DOI] [PubMed] [Google Scholar]
- 42.van Duin D, Lok JJ, Earley M, et al. Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant enterobacteriaceae. Clin Infect Dis. 2018;66(2):163–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kang Y, Zhou Q, Cui J.. Pharmacokinetic/pharmacodynamic modelling to evaluate the efficacy of various dosing regimens of ceftazidime/avibactam in patients with pneumonia caused by Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae: a multicentre study in Northern China. J Glob Antimicrob Resist. 2021;27:67–71. [DOI] [PubMed] [Google Scholar]
- 44.Karaiskos I, Daikos GL, Gkoufa A, et al. Ceftazidime/avibactam in the era of carbapenemase-producing Klebsiella pneumoniae: experience from a national registry study. J Antimicrob Chemother. 2021;76(3):775–783. [DOI] [PubMed] [Google Scholar]
- 45.Shields RK, Nguyen MH, Chen L, et al. Pneumonia and renal replacement therapy are risk factors for ceftazidime-avibactam treatment failures and resistance among patients with carbapenem-resistant enterobacteriaceae infections. Antimicrob Agents Chemother. 2018;62(5):e02497–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tumbarello M, Raffaelli F, Giannella M, et al. Ceftazidime-avibactam use for Klebsiella pneumoniae carbapenemase-producing K. pneumoniae infections: a retrospective observational multicenter study. Clin Infect Dis. 2021;73(9):1664–1676. [DOI] [PubMed] [Google Scholar]
- 47.Giacobbe DR, Bassetti M.. Innovative beta-lactam/beta-lactamase inhibitor combinations for carbapenem-resistant gram-negative bacteria. Future Microbiol. 2022;17:393–396. [DOI] [PubMed] [Google Scholar]
- 48.Lawandi A, Yek C, Kadri SS.. IDSA guidance and ESCMID guidelines: complementary approaches toward a care standard for MDR gram-negative infections. Clin Microbiol Infect. 2022;28(4):465–469. [DOI] [PubMed] [Google Scholar]
- 49.Xu M, Zhao, J, Xu L, et al. Emergence of transferable ceftazidime-avibactam resistance in KPC-producing Klebsiella pneumoniae due to a novel CMY AmpC beta-lactamase in China. Clin Microbiol Infect. 2022;28(1)e1-136–e6.136. [DOI] [PubMed] [Google Scholar]
- 50.Venditti C, Butera O, Meledandri M, et al. Molecular analysis of clinical isolates of ceftazidime-avibactam-resistant Klebsiella pneumoniae. Clin Microbiol Infect. 2021;27(7)e6.1040:e1-1040. [DOI] [PubMed] [Google Scholar]
- 51.Nelson K, Hemarajata P, Sun D, et al. Resistance to ceftazidime-avibactam is due to transposition of KPC in a porin-deficient strain of Klebsiella pneumoniae with increased efflux activity. Antimicrob Agents Chemother. 2017;61(10):e00989–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Di Bella S, Giacobbe DR, Maraolo AE, et al. Resistance to ceftazidime/avibactam in infections and colonisations by KPC-producing enterobacterales: a systematic review of observational clinical studies. J Glob Antimicrob Resist. 2021;25:268–281. [DOI] [PubMed] [Google Scholar]
- 53.Gaibani P, Giani T, Bovo F, et al. Resistance to ceftazidime/avibactam, meropenem/vaborbactam and imipenem/relebactam in gram-negative MDR bacilli: molecular mechanisms and susceptibility testing. Antibiotics. 2022;11(5):628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jorgensen SCJ, Rybak MJ.. Meropenem and vaborbactam: stepping up the battle against carbapenem-resistant enterobacteriaceae. Pharmacotherapy. 2018;38(4):444–461. [DOI] [PubMed] [Google Scholar]
- 55.Dulyayangkul P, Douglas EJA, Lastovka F, et al. Resistance to ceftazidime/avibactam plus meropenem/vaborbactam when both are used together is achieved in four steps in metallo-beta-lactamase-negative Klebsiella pneumoniae. Antimicrob Agents Chemother. 2020;64(10):e00409–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lapuebla A, Abdallah M, Olafisoye O, et al. Activity of imipenem with relebactam against gram-negative pathogens from New York city. Antimicrob Agents Chemother. 2015;59(8):5029–5031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Balabanian G, Rose M, Manning N, et al. Effect of porins and blaKPC expression on activity of imipenem with relebactam in Klebsiella pneumoniae: can antibiotic combinations overcome resistance? Microb Drug Resist. 2018;24(7):877–881. [DOI] [PubMed] [Google Scholar]
- 58.Di Pilato V, Principe L, Andriani L, et al. Deciphering variable resistance to novel carbapenem-based β-lactamase-inhibitor combinations in a multiclonal outbreak by KPC carbapenemase-producing Klebsiella pneumoniae resistant to ceftazidime/avibactam. Clin Microbiol Infect. 2022. doi: 10.1016/j.cmi.2022.11.011 [DOI] [PubMed] [Google Scholar]
- 59.Kazmierczak KM, Tsuji M, Wise MG, et al. In vitro activity of cefiderocol, a siderophore cephalosporin, against a recent collection of clinically relevant carbapenem-non-susceptible gram-negative bacilli, including serine carbapenemase- and metallo-beta-lactamase-producing isolates (SIDERO-WT-2014 study). Int J Antimicrob Agents. 2019;53(2):177–184. [DOI] [PubMed] [Google Scholar]
- 60.Hobson CA, Cointe A, Jacquier H, et al. Cross-resistance to cefiderocol and ceftazidime-avibactam in KPC beta-lactamase mutants and the inoculum effect. Clin Microbiol Infect. 2021;27(8):1172:e7–1172:e10. [DOI] [PubMed] [Google Scholar]
- 61.Centers for Disease Control Prevention . Guidance for control of infections with carbapenem-resistant or carbapenemase-producing enterobacteriaceae in acute care facilities. MMWR Morb Mortal Wkly Rep. 2009;58(10):256–260. [PubMed] [Google Scholar]
- 62.EUCAST . EUCAST guidelines for detection of resistance mechanisms and specific resistances of clinical and/or epidemiological importance. Available from: https://eucast.org/. 2017.
- 63.Nordmann P, Cuzon G, Naas T.. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009;9(4):228–236. [DOI] [PubMed] [Google Scholar]
- 64.Lutgring JD, Limbago BM.. The problem of carbapenemase-producing-carbapenem-resistant-enterobacteriaceae detection. J Clin Microbiol. 2016;54(3):529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pournaras S, Poulou A, Tsakris A.. Inhibitor-based methods for the detection of KPC carbapenemase-producing enterobacteriaceae in clinical practice by using boronic acid compounds. J Antimicrob Chemother. 2010;65(7):1319–1321. [DOI] [PubMed] [Google Scholar]
- 66.Dortet L, Poirel L, Nordmann P.. Rapid identification of carbapenemase types in enterobacteriaceae and Pseudomonas spp. by using a biochemical test. Antimicrob Agents Chemother. 2012;56(12):6437–6440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Girlich D, Halimi D, Zambardi G, et al. Evaluation of etest(R) strips for detection of KPC and metallo-carbapenemases in enterobacteriaceae. Diagn Microbiol Infect Dis. 2013;77(3):200–201. [DOI] [PubMed] [Google Scholar]
- 68.Tamma PD, Simner PJ.. Phenotypic detection of carbapenemase-producing organisms from clinical isolates. J Clin Microbiol. 2018;56(11):e01140-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hrabak J, Chudackova E, Papagiannitsis CC.. Detection of carbapenemases in enterobacteriaceae: a challenge for diagnostic microbiological laboratories. Clin Microbiol Infect. 2014;20(9):839–853. [DOI] [PubMed] [Google Scholar]
- 70.Hleba L, Hlebova M, Kovacik A, et al. Carbapenemase producing Klebsiella pneumoniae (KPC): what is the best MALDI-TOF MS detection method. Antibiotics. 2021;10(12):1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vasilakopoulou A, Karakosta P, Vourli S, et al. Detection of KPC, NDM and VIM-producing organisms directly from rectal swabs by a multiplex lateral flow immunoassay. Microorganisms. 2021;9(5):942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Buchan BW, Ledeboer NA.. Emerging technologies for the clinical microbiology laboratory. Clin Microbiol Rev. 2014;27(4):783–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rentschler S, Kaiser L, Deigner HP.. Emerging options for the diagnosis of bacterial infections and the characterization of antimicrobial resistance. Int J Mol Sci. 2021;22(1):456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dumkow LE, Worden LJ, Rao SN.. Syndromic diagnostic testing: a new way to approach patient care in the treatment of infectious diseases. J Antimicrob Chemother. 2021;76(Suppl 3):iii4–iii11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ramanan P, Bryson AL, Binnicker MJ, et al. Syndromic panel-based testing in clinical microbiology. Clin Microbiol Rev. 2018;31(1):e00024-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Balloux F, Bronstad Brynildsrud O, van Dorp L, et al. From theory to practice: translating whole-genome sequencing (WGS) into the clinic. Trends Microbiol. 2018;26(12):1035–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Giordano L, Fiori B, D’Inzeo T, et al. Simplified testing method for direct detection of carbapenemase-producing organisms from positive blood cultures using the NG-test carba 5 assay. Antimicrob Agents Chemother. 2019;63(7):e00550-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Antonelli A, Giani T, Di Pilato V, et al. KPC-31 expressed in a ceftazidime/avibactam-resistant Klebsiella pneumoniae is associated with relevant detection issues. J Antimicrob Chemother. 2019;74(8):2464–2466. [DOI] [PubMed] [Google Scholar]
- 79.Figueroa-Espinosa R, Costa A, Cejas D, et al. MALDI-TOF MS based procedure to detect KPC-2 directly from positive blood culture bottles and colonies. J Microbiol Methods. 2019;159:120–127. [DOI] [PubMed] [Google Scholar]
- 80.Giacobbe DR, Giani T, Bassetti M, et al. Rapid microbiological tests for bloodstream infections due to multidrug resistant gram-negative bacteria: therapeutic implications. Clin Microbiol Infect. 2020;26(6):713–722. [DOI] [PubMed] [Google Scholar]
- 81.Liotti FM, Posteraro B, Mannu F, et al. Development of a multiplex PCR platform for the rapid detection of bacteria, antibiotic resistance, and candida in human blood samples. Front Cell Infect Microbiol. 2019;9:389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Coppi M, Di Pilato V, Monaco F, et al. Ceftazidime-avibactam resistance associated with increased bla KPC-3 gene copy number mediated by pKpQIL plasmid derivatives in sequence type 258 Klebsiella pneumoniae. Antimicrob Agents Chemother. 2020;64(4):e01816-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Findlay J, Poirel L, Juhas M, et al. KPC-mediated resistance to ceftazidime-avibactam and collateral effects in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2021;65(9):e0089021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sun D, Rubio-Aparicio D, Nelson K, et al. Meropenem-vaborbactam resistance selection, resistance prevention, and molecular mechanisms in mutants of KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2017;61(12):e01694-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hobson CA, Pierrat G, Tenaillon O, Bonacorsi S, Bercot B, Jaouen E, Jacquier H, Birgy A. Klebsiella pneumoniae Carbapenemase Variants Resistant to Ceftazidime-Avibactam: an Evolutionary Overview. Antimicrob Agents Chemother. 2022. Sep 20;66(9):e0044722. doi: 10.1128/aac.00447-22. Epub 2022 Aug 18. PMID: 35980232; PMCID: PMC9487638. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.