Abstract
Secondary infection with Streptococcus pneumoniae has contributed significantly to morbidity and mortality during multiple influenza virus pandemics and remains a common threat today. During a concurrent infection, both pathogens can influence the transmission of each other, but the mechanisms behind this are unclear. In this study, condensation air sampling and cyclone bioaerosol sampling were performed using ferrets first infected with the 2009 H1N1 pandemic influenza virus (H1N1pdm09) and secondarily infected with S. pneumoniae strain D39 (Spn). We detected viable pathogens and microbial nucleic acid in expelled aerosols from co-infected ferrets, suggesting that these microbes could be present in the same respiratory expulsions. To assess whether microbial communities impact pathogen stability within an expelled droplet, we performed experiments measuring viral and bacterial persistence in 1 µL droplets. We observed that H1N1pdm09 stability was unchanged in the presence of Spn. Further, Spn stability was moderately increased in the presence of H1N1pdm09, although the degree of stabilization differed between airways surface liquid collected from individual patient cultures. These findings are the first to collect both pathogens from the air and in doing so, they provide insight into the interplay between these pathogens and their hosts.
Keywords: influenza, Streptococcus pneumoniae, aerosols, stability, survival, persistence
Observation and Discussion
Environmental stability of respiratory pathogens expelled from an infected host is a key factor impacting transmission (1). Previous work has shown that several factors (eg. humidity, temperature, and solute concentration) influence microbial stability in droplets (2–5). Our understanding of how microbes within the same droplets affect persistence is insufficient, as studies often only examine one microbe at a time. The limited work investigating how bacteria alter viral stability have primarily focused on enteric pathogen stability in feces and found that binding of poliovirus to bacteria increased virus stability (6–9). However, these studies did not examine how viruses alter bacterial stability. So, it remains unclear whether multiple microbes exist within the same aerosols, and if so, whether they influence each other to impact environmental persistence.
Bacterial co-infection is a common occurrence for viral respiratory pathogens: bacterial co-infection rates during influenza virus infection in humans range from 4.2–32.7% and cause significant illness in critically ill patients (10–12). Studies of influenza virus and S. pneumoniae secondary infection in animals have shown that influenza virus facilitates transmission of S. pneumoniae (13–15), while S. pneumoniae may decrease viral transmission (14, 15). Other groups have found that S. pneumoniae can increase influenza transmission after antibiotic administration (16). A study on the interaction of nasopharyngeal bacteria on influenza virus observed that influenza virus binds S. pneumoniae (17), suggesting that these pathogens may travel in the same aerosols. These observations indicate a complex interplay between these pathogens that requires further investigation to understand how their interactions affect environmental persistence and transmission.
Co-infected ferrets shed H1N1pdm09 and Spn into expelled aerosols.
Co-infections can lead to high titers of virus and bacteria in infected hosts (14, 15, 18), suggesting that multiple microbes could be present within expelled respiratory droplets. To characterize environmental shedding of H1N1pdm09 and Spn, ferrets were first infected with H1N1pdm09 and then infected with Spn 2 days later. Nasal washes were collected, and air sampling was performed for 3 days after co-infection.
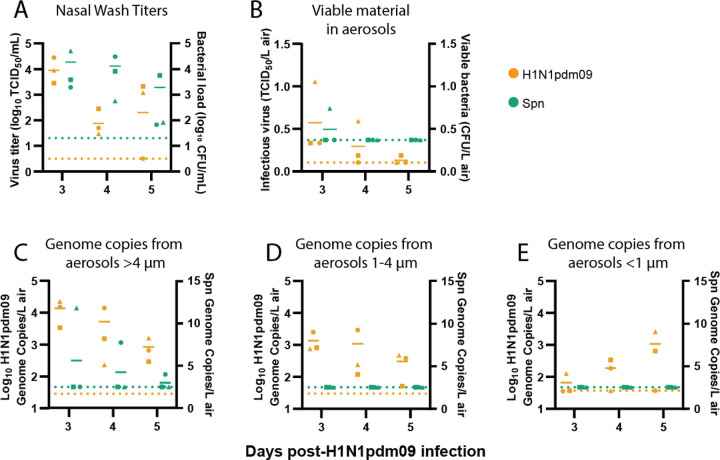
Nasal wash titers from co-infected ferrets showed that all three animals shed H1N1pdm09 on days 3 and 4 post-H1N1pdm09 infection, but only two animals shed virus on day 5, while all animals shed Spn throughout the time course (Figure 1A). We next assessed whether infectious microbes were released from co-infected ferrets by air sampling with a condensation sampler (Supplemental Figure 1). Aerosolized infectious H1N1pdm09 was detected from all ferrets on day 3, but from fewer animals on days 4 and 5 (Figure 1B). Despite measurable levels of Spn in nasal washes, only one animal had viable Spn collected from the condensation sampler (Figure 1B). This may be underrepresenting expelled bacteria in the air, as previous work has shown that not all viable bacteria form colonies after aerosolization (19). Cyclone bioaerosol sampling, used to collect microbial genomic material, detected H1N1pdm09 in air samples from all co-infected ferrets for both the >4 µm and 1–4 µm fractions on all days (Figure 1C-D). The small <1 µm fraction had measurable H1N1pdm09 from two of three co-infected ferrets on any day (Figure 1E). Spn was only detectable in the >4 µm fraction in two animals (Figure 1C), which is unsurprising given that S. pneumoniae ranges from 5–10x greater in diameter than influenza and is, therefore, less likely to be found in smaller aerosols. This result may also underrepresent the amount of aerosolized Spn, since sample processing was not optimized for encapsulated bacterial DNA. Our results are the first to detect infectious H1N1pdm09 and viable Spn in expelled aerosols from co-infected animals.
Figure 1. Co-infected ferrets shed H1N1pdm09 and Spn.
Ferrets were infected with 106 TCID50 of H1N1pdm09 and subsequently infected 2 days later with 107 CFU S. pneumoniae D39. (A) Nasal wash loads of H1N1pdm09 and Spn are shown for the days following initial H1N1pdm09 infection. (B) Condensation sampling with a Liquid Spot Sampler was used to collect infectious virus and bacteria shed by co-infected animals. Viral and bacterial loads were measured by TCID50 and CFU assays, respectively. (C-E) Cyclone based air samplers were used to fractionate and collect microbial genomic material shed from co-infected ferrets in (C) >4 µm droplets, (D) 1–4 µm droplets, and (E) <1 µm droplets. Quantitative PCR was used to measure genome copies for each microbe. For all graphs, orange symbols represent H1N1pdm09 (N=3) and green symbols represent Spn (N=3), with each animal indicated by a unique shape and the mean indicated by short, solid lines. Dotted lines denote the limit of detection for H1N1pdm09 (orange) and Spn (green).
Environmental stability of H1N1pdm09 is not impacted by the presence of Spn.
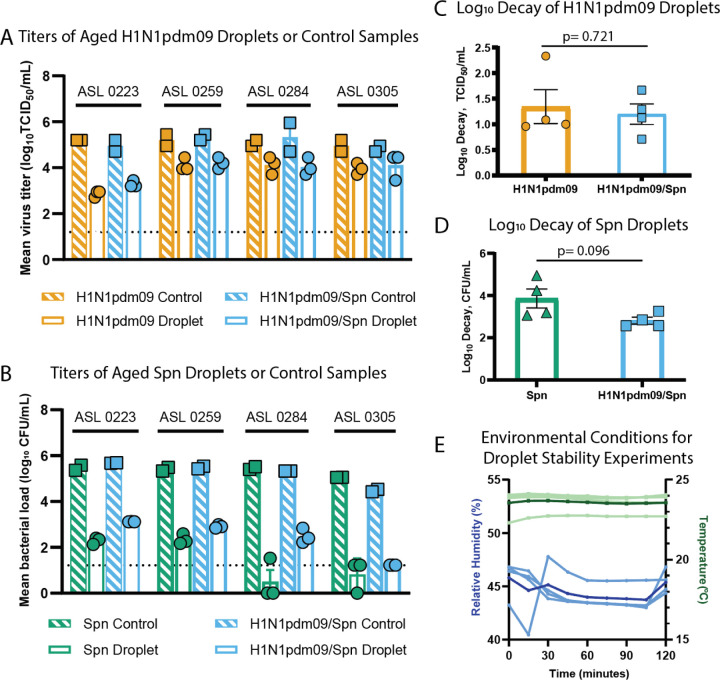
Given the observation that H1N1pdm09 and Spn are shed from co-infected ferrets, we questioned whether these microbes might influence each other’s environmental stability in respiratory droplets. Spn has been shown to potentially alter influenza A transmission (14, 15), suggesting that Spn might decrease H1N1pdm09 environmental stability. H1N1pdm09, on the other hand, has been shown to increase transmission of Spn (13–15), which might indicate enhanced Spn stability with H1N1pdm09. To test this, we measured microbial persistence in droplets containing H1N1pdm09, Spn, or a 1:1 ratio of both pathogens in the presence of airway surface liquid (ASL) collected from four different human bronchial epithelial (HBE) cell donors (Figure 2). ASL is an important component of the respiratory tract and has been shown to increase stability of influenza viruses in the environment (3). After aging 1 µL droplets of each solution in a humidified chamber for 2 hours, infectious H1N1pdm09 or Spn was measured and compared to bulk solution controls (Figure 2A-B). Experiments were performed at 43% relative humidity (Figure 2E), as viruses and Gram-positive bacteria are more susceptible to decay at intermediate relative humidity (20). After 2 hours, there was no significant difference (p= 0.721) in H1N1pdm09 stability with or without Spn (average decay of 1.19 log10 TCID50/mL versus 1.34 log10 TCID50/mL, respectively) (Figure 2C). In contrast, there was a trend of increased stability for Spn in the presence of H1N1pdm09. Improved Spn stability was clearly observed in ASL from one patient culture (0284), as Spn alone decayed an average of 3.86 log10 CFU/mL and H1N1pdm09/Spn decayed an average of 2.81 log10 CFU/mL (p=0.096, Figure 2D, Supplemental Table 1). More modest stabilization for Spn was observed in 2 other cultures (0223 and 0259) and no difference was observed in ASL from one patient (0305) (Supplemental Table 1). Together, these results suggest that H1N1pdm09 infectivity is not impacted by Spn at the environmental conditions tested. There may be a modest impact of Spn stability in the presence of H1N1pdm09, although this may be more sensitive to variations in the ASL (or mucus composition) per individual. Further research should explore the impact of mucus and lung disease states on the relationship between influenza viruses and S. pneumoniae.
Figure 2. Stability of S. pneumoniae and influenza viruses in droplets.
(A-D) Viral and bacterial loads of H1N1pdm09 and Spn were assessed after exposure of 10x1 µL droplets to 43% relative humidity (RH) at room temperature for 2 hours. Microbes were suspended in ASL from four different HBE cell donors as indicated in A and B. Control titers were determined using 10 µL of bulk solutions in closed tubes at room temperature. (A) The stability of H1N1pdm09 in droplets containing H1N1pdm09 or H1N1pdm09/Spn measured by TCID50 assay, and (C) log10 decay for each individual ASL culture were determined. (B) The stability of Spn in droplets containing Spn or H1N1pdm09/Spn measured by CFU assay, and (D) log10 decay for each individual ASL culture were determined. Differences were assessed using Welch’s unpaired t-test. (E) The RH and temperature were recorded every 15 minutes during stability experiments. Temperature (light green) and RH (light blue) for each ASL replicate are shown. The average temperature (dark green) and RH (dark blue) for all experiments are also included.
Co-infection with pathogens can impact the transmissibility to subsequent hosts. Concurrent infections of influenza virus and S. pneumoniae result in increased morbidity and a greater risk of bacterial transmission (13, 14). The work here shows that co-infected animals expel both influenza virus and S. pneumoniae into air and can be collected using a condensation air-sampler or cyclone bioaerosol sampler. No impact was observed for influenza virus in the presence of S. pneumoniae, but a trend towards increased S. pneumoniae stability in the presence of influenza virus may help explain augmented S. pneumoniae transmission in addition to the increased bacterial shedding observed during co-infection (13, 14). Investigation of microbial stability using polymicrobial populations is not widely performed and could help elucidate the complexity of pathogen transmission seen in the human population. In addition, identifying host specific factors underlying microbial stability in the environment could increase our understanding of individual transmission risks and strategies mitigating the spread of pathogens in the population.
Methods
Methods can be found in the supplemental materials.
Supplementary Material
Importance.
The impact of microbial communities on transmission fitness and environmental persistence is under-studied. Environmental stability of microbes is crucial to identifying transmission risks and mitigation strategies, such as removal of contaminated aerosols and decontamination of surfaces. Co-infection with S. pneumoniae is very common during influenza virus infection, but little work has been done to understand whether S. pneumoniae alters stability of influenza virus, or vice versa, in a relevant system. Here, we demonstrate that influenza virus and S. pneumoniae are expelled by co-infected hosts. Our stability assays did not reveal any impact of S. pneumoniae on influenza virus stability, and a trend towards increased stability of S. pneumoniae in the presence of influenza viruses. Future work characterizing environmental persistence of viruses and bacteria should include microbially-complex solutions to better mimic physiologically relevant conditions.
Acknowledgements
We thank members of the Lakdawala and Hiller lab for providing constructive feedback of this manuscript and Dr. Rachel Duron for editorial comments. This work was supported in part with Federal funds from NIAID, NIH, and DHHS (75N93021C00015, SSL). Additional funding was provided by Flu Lab (SSL and LCM) and NIAID (R01 AI158484). JF was supported by the University of Pittsburgh Training Program in Antimicrobial Resistance (T32AI138954). We would also like to acknowledge the Research Development Program from the Cystic Fibrosis Foundation to the University of Pittsburgh (MM and SF).
References
- 1.Leung NHL. 2021. Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol 19:528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marr LC, Tang JW, van Mullekom J, Lakdawala SS. 2019. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J R Soc Interface 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kormuth KA, Lin K, Prussin AJ, Vejerano EP, Tiwari AJ, Cox SS, Myerburg MM, Lakdawala SS, Marr LC. 2018. Influenza virus infectivity is retained in aerosols and droplets independent of relative humidity. Journal of Infectious Diseases 218:739–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin K, Schulte CR, Marr LC. 2020. Survival of MS2 and Φ6 viruses in droplets as a function of relative humidity, pH, and salt, protein, and surfactant concentrations. PLoS One 15:e0243505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang CC, Prather KA, Sznitman J, Jimenez JL, Lakdawala SS, Tufekci Z, Marr LC. 2021. Airborne transmission of respiratory viruses. Science (1979) 373. [DOI] [PMC free article] [PubMed]
- 6.Berger AK, Yi H, Kearns DB, Mainou BA. 2017. Bacteria and bacterial envelope components enhance mammalian reovirus thermostability. PLoS Pathog 13:e1006768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aguilera ER, Nguyen Y, Sasaki J, Pfeiffer JK. 2019. Bacterial Stabilization of a Panel of Picornaviruses. mSphere 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson CM, Jesudhasan PR, Pfeiffer JK. 2014. Bacterial Lipopolysaccharide Binding Enhances Virion Stability and Promotes Environmental Fitness of an Enteric Virus. Cell Host Microbe 15:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olive M, Gan C, Carratalà A, Kohn T. 2020. Control of Waterborne Human Viruses by Indigenous Bacteria and Protists Is Influenced by Temperature, Virus Type, and Microbial Species. Appl Environ Microbiol 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Louie JK, Acosta M, Winter K, Jean C, Gavali S, Schechter R, Vugia D, Harriman K, Matyas B, Glaser CA, Samuel MC, Rosenberg J, Talarico J, Hatch D. 2009. Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA - Journal of the American Medical Association 302:1896–1902. [DOI] [PubMed] [Google Scholar]
- 11.Randolph AG, Vaughn F, Sullivan R, Rubinson L, Thompson BT, Yoon G, Smoot E, Rice TW, Loftis LL, Helfaer M, Doctor A, Paden M, Flori H, Babbitt C, Graciano AL, Gedeit R, Sanders RC, Giuliano JS, Zimmerman J, Uyeki TM. 2011. Critically Ill Children During the 2009–2010 Influenza Pandemic in the United States. Pediatrics 128:e1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin-Loeches I, Schultz MJ, Vincent J-L, Alvarez-Lerma F, Bos LD, Solé-Violán J, Torres A, Rodriguez A. 2016. Increased incidence of co-infection in critically ill patients with influenza. Intensive Care Medicine 2016 43:1 43:48–58. [DOI] [PubMed] [Google Scholar]
- 13.McCullers JA, McAuley JL, Browall S, Iverson AR, Boyd KL, Henriques Normark B. 2010. Influenza Enhances Susceptibility to Natural Acquisition of and Disease due to Streptococcus pneumoniae in Ferrets. J Infect Dis 202:1287–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mueller-Brown K, le Sage V, French AJ, Jones JE, Padovani GH, Avery AJ, Schultz-Cherry S, Rosch JW, Hiller NL, Lakdawala SS. 2022. Secondary infection with Streptococcus pneumoniae decreases influenza virus replication and is linked to severe disease. FEMS Microbes 10.1093/FEMSMC/XTAC007. [DOI] [PMC free article] [PubMed]
- 15.Diavatopoulos DA, Short KR, Price JT, Wilksch JJ, Brown LE, Briles DE, Strugnell RA, Wijburg OL. 2010. Influenza A virus facilitates Streptococcus pneumoniae transmission and disease. The FASEB Journal 24:1789–1798. [DOI] [PubMed] [Google Scholar]
- 16.Rowe HM, Livingston B, Margolis E, Davis A, Meliopoulos VA, Echlin H, Schultz-Cherry S, Rosch JW. 2020. Respiratory Bacteria Stabilize and Promote Airborne Transmission of Influenza A Virus. mSystems 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rowe HM, Meliopoulos VA, Iverson A, Bomme P, Schultz-Cherry S, Rosch JW. 2019. Direct interactions with influenza promote bacterial adherence during respiratory infections. Nat Microbiol 4:1328–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mifsud EJ, Farrukee R, Hurt AC, Reading PC, Barr IG. 2022. Infection with different human influenza A subtypes affects the period of susceptibility to secondary bacterial infections in ferrets. FEMS Microbes 3:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heidelberg JF, Shahamat M, Levin M, Rahman I, Stelma G, Grim C, Colwell RR. 1997. Effect of aerosolization on culturability and viability of gram-negative bacteria. Appl Environ Microbiol 63:3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin K, Marr LC. 2020. Humidity-Dependent Decay of Viruses, but Not Bacteria, in Aerosols and Droplets Follows Disinfection Kinetics. Cite This: Environ Sci Technol 2020:1024–1032. [DOI] [PubMed] [Google Scholar]
- 21.Kormuth KA, Lin K, Qian Z, Myerburg MM, Marr LC, Lakdawala SS. 2019. Environmental Persistence of Influenza Viruses Is Dependent upon Virus Type and Host Origin. mSphere 4:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myerburg MM, Harvey PR, Heidrich EM, Pilewski JM, Butterworth MB. 2010. Acute regulation of the epithelial sodium channel in airway epithelia by proteases and trafficking. Am J Respir Cell Mol Biol 43:712–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.