Abstract
Employing an ecological approach, we sought to identify social determinants of obesity among Hispanics/Latinos and non-Hispanic whites living in the Southeast US. Data on social determinants of obesity (individual, family, community and cultural/contextual) were collected from 217 participants [106 Hispanics/Latinos; 111 non-Hispanic whites]; height and weight were objectively measured. We compared prevalence of overweight and obese between ethnic groups and BMI values within each group by social determinants. Hispanics had a 1.9-fold increase (OR 1.93, 95% CI: 1.05–3.55) in overweight prevalence compared to non-Hispanic whites after adjusting for age and gender. We found positive estimates between unfavorable family-level determinants and BMI among Hispanic/Latinos. In contrast, non-Hispanic whites who reported unfavorable neighborhood characteristics had higher BMI’s. Findings highlight the need for targeted approaches for the prevention and control of obesity.
Keywords: Hispanic/Latino, Obesity, Social determinants of health, Obesogenic environment, Health disparity
Introduction
U.S. Hispanics/Latinos experience a high burden of obesity, a risk factor for multiple chronic health conditions and increased medical expenditures [1]. For adults living in the U.S., the prevalence of obesity is 47% among Hispanics/Latinos compared with 38% among non-Hispanic whites [2]. Hispanic/Latino immigrants often arrive in the U.S. at a healthy weight; however, time in the U.S. and changes in lifestyle behaviors are associated with weight gain [3–5]. Growing evidence suggests that social and environmental factors also influence obesity [6], including social support for healthy behaviors [7], access to safe physical activity opportunities [8] and healthy food options [9]. Geographical differences in rates of obesity, such as the high rates observed in the Southern U.S., may be attributable to sub-optimal social and environmental factors (e.g. obesogenic environments) [10]. Thus, Hispanic/Latinos who live in obesogenic environments may be more prone to weight gain.
Social determinants of health (SDoH), defined as the economic, environmental, political and social conditions in which people live, are responsible for a major part of health inequity worldwide [11]. Multiple SDoH have been associated with obesity, with the effects of the built/structural environment well established in the literature [6]. Similarly, socioeconomic status has consistently been linked to higher obesity rates [12], driven largely by limited access to education and material resources [13]. Social networks (e.g. the people in one’s life), [14] as well as social capital and collective efficacy at the interpersonal and neighborhood levels, are correlated with obesity [15]. These determinants are multi-systemic; thus, studies that employ an ecological approach to understand SDoH provide valuable insights into factors that contribute to risk for obesity, especially among U.S. Hispanic/Latino immigrants [16].
This is important because the U.S. Hispanic/Latino population is increasing [17], particularly in the proportion of Hispanics/Latinos living in emerging Hispanic/Latino communities. Historically, immigrants from Mexico and Central and South America have settled in states such as California, Florida, Illinois and Texas however, individuals are increasingly immigrating to emerging communities. Emerging communities are defined as those where Hispanic/Latino populations are growing but have not achieved institutional power or recognition [18]. Seven states with the largest percent increase in their Hispanic/Latino populations are found in a band across the southeastern U.S. that are considered emerging communities [19]. A growing body of research demonstrates that Hispanic/Latino immigrants living in these emerging communities face distinct barriers when it comes to healthy lifestyles. This includes underdeveloped social networks, isolation and discrimination, and limited access to health education programs and quality health services [20–23], all factors that have been linked to obesity. Hispanic/Latino immigrants who find themselves in emerging communities, such as Alabama where rates of obesity are high [24], may be at risk for accelerated weight gain and heightened diabetes risk.
Recognizing the need to conduct ecological studies to identify social determinants of obesity, researchers developed the Community Energy Balance (CEB) framework [25]. This framework was developed to guide research on the social determinants of health and obesity that specifically incorporates cultural and contextual factors relevant to racial/ethnic minority communities and immigrants to the U.S (Fig. 1). Using the CEB as a guide, we developed a survey to identify social determinants of obesity among Hispanics/Latinos and non-Hispanic whites living in a rural, Alabama community. The city of Albertville was selected based on its sizable Hispanic population relative to other areas of Alabama [26].
Fig. 1.
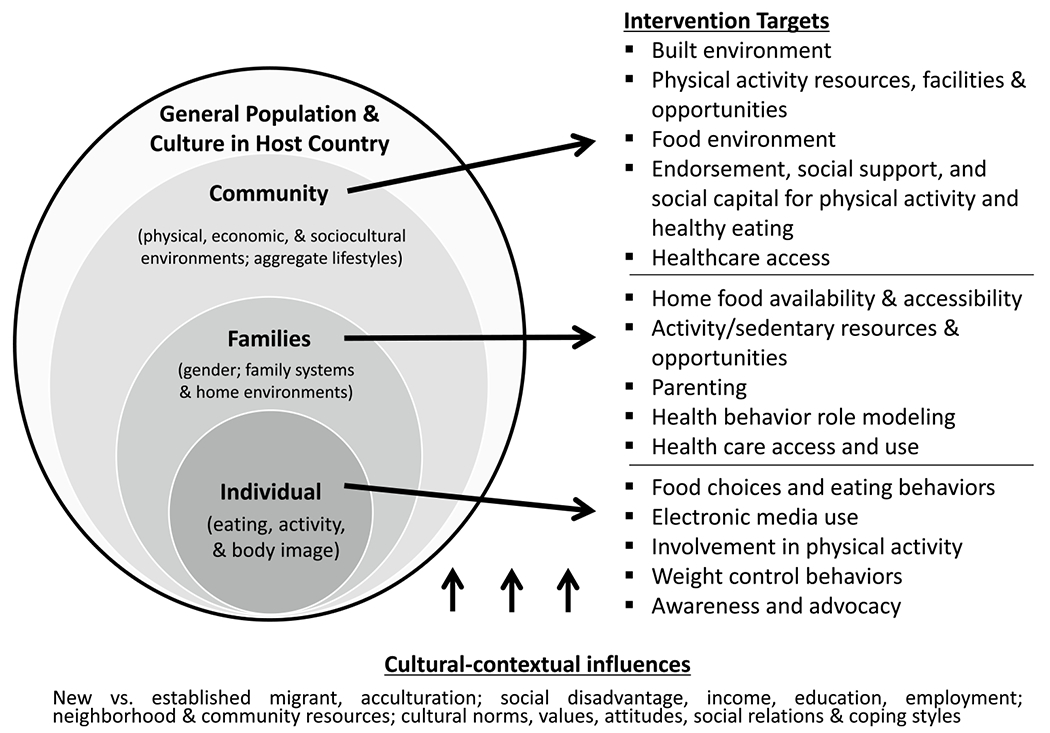
Community Energy Balance Framework, adapted from Kumanyika et al. [25]
Methods
Study Design
A population-based cross-sectional survey was administered to residents in Albertville, Alabama identified using a cluster sampling approach. The study was reviewed and approved by the institution’s review board.
Identification and Recruitment of Participants
Participants were recruited from Albertville, a rural community located in Marshall County in Northeastern Alabama. As of the 2010 U.S. Census, Albertville had a population of 21,160 with Hispanics/Latinos comprising roughly 28% of the population [26]. To be included, potential participants had to be a resident living in an Albertville Census block group selected for participation, self-identify as Hispanic or non-Hispanic white, be 19 years of age or older at time of survey, and able to speak English or Spanish.
Based on power calculations, the goal was to recruit 200 participants, with roughly 50% Hispanic/Latino respondents. To ensure ethnic representativeness, participants were recruited using an area-based stratified random sampling approach [27]. First, we divided Albertville into four non-overlapping strata based on Census block group by Hispanic household proportion: blocks with < 10% Hispanic households, 10–30%, 30–50%, and ≥ 50%. We then randomly selected block groups within each stratum, oversampling the two strata with higher proportions of Hispanic households. Interviewers were given a block map and a starting address. Using a systematic random sampling interval based on the CASPER toolkit [28], interviewers approached Nth house until the proposed number of surveys per block were completed (N varied as a function of block population and proposed surveys per block). Door-to-door recruitment was conducted between June and December 2013. Data were collected on weekdays and weekends to avoid bias toward individuals who did not have full-time employment or non-traditional work schedules. Trained bilingual staff obtained written informed consent, assessed eligibility, collected physiologic measures, and administered the survey.
Measures
Body Mass Index, kg/m2 (BMI)
Height and weight were measured at the in-person survey using standard procedures and equipment. Weight was collected using the Homedics SC-540 LCD Scale and recorded in kilograms. Height was measured using the Seca 214 Portable Stadiometer and recorded to the nearest millimeter. Weight in kilograms was divided by height in meters squared to derive BMI.
Social Determinants of Health
Using the CEB framework as a guide, we selected measures representing social determinants of health related to obesity (see Table 1), including individual, family, community and cultural/contextual determinants. Domains are listed in Table 1, along with sources of the scales used and how responses to scale items were categorized for analysis purposes [29–39]. Cut-points for the Perceived Stress Scale (PSS) and Centers for Epidemiologic Studies Depression Scale (CES-D) were based on previous recommendations in the literature [37, 38]. Note that many measures, particularly interpersonal and community level measures, did not have validated cut-points documented. Since our intent was to compare within and between Hispanics/Latinos and non-Hispanic whites, we employed a median split approach to classify these measures into low vs high for comparisons (see Table 1 for specific measures and cut-points utilized).
Table 1.
Social determinant of health measures assessed based on the Community Energy Balance (CEB) framework
| CEB Level | Domain | Measure (# of items) | Categorization of measure |
|---|---|---|---|
| Individual | |||
| Demographic | |||
| Age | Self-reported age at time of survey (1 item) | Continuous years | |
| Gender | Self-reported gender (1 item) | Male/Female | |
| Health behaviors | |||
| Diet | Rapid food screener, fruit and vegetable consumption section. [29] (7 items) | < 5 servings/day; ≥ 5 servings/day | |
| Physical activity | Global physical activity questionnaire [30] (15 items) | < 150 min/day; ≥ 150 min/day | |
| Sedentary behavior | Global physical activity questionnaire [30] (1 items) | Total minutes sedentary per day; low vs high based on median split | |
| Families | |||
| Family cohesion | Family Adaptability and Cohesion Evaluation Scale (FACES III), Family cohesion subscale [31] (10 items) | Scale of 10–50; low vs high based on median split with higher scores indicating more cohesion | |
| Social support for physical activity and healthy eating | |||
| Family encouragement | Sallis Social Support and Eating Habits/Exercise surveys, family encouragement items [32] (5 items) | Scale of 1–5; low vs high based on median split with higher scores indicating more encouragement | |
| Family participation | Sallis Social Support and Eating Habits/Exercise surveys, family participation items [32] (5 items) | Scale of 1–5; low vs high based on median split with higher scores indicating more participation | |
| Social network size | Name generator of up to 5 people with close relationship to participant, count of names [33] (1 item) | Scale of 0–5; low vs high based on median split with higher scores indicating more people in social network | |
| Food insecurity | USDA Food security short form [34] (6 items) | Scale of 0–6; 0 to 1 = food secure; 2–6 = food insecure | |
| Community | |||
| Neighborhood cohesion | Project on Human Development in Chicago Neighborhoods Community Survey [35] (5 items) | Scale of 1–5; low vs high based on median split with higher scores indicating more neighborhood cohesion | |
| Neighborhood disorder | Ross-Mirowsky Perceived Neighborhood Disorder Scale [36] (15 items) | Scale of 10–45; low vs high based on median split with higher scores indicating more disorder | |
| Civic trust | Project on Human Development in Chicago Neighborhoods Community Survey [35] (5 items) | Scale of 1–5; low vs high based on median split with higher scores indicating more civic trust | |
| Physical activity opportunities | Awareness of Resources in the Community for Physical Activity (1 item – list resources) [33] Used local park in last year (1 item) | Variable number; low vs high based on median split with higher scores indicating more awareness Yes/No | |
| Cultural/contextual | |||
| SES | |||
| Education | Highest education obtained (1 item) | < High School, High School, > High School | |
| Employment | Currently working (1 item) | Yes/No | |
| Insurance status | |||
| Participant has health insurance (includes VA benefits, Medicaid or Medicare) (1 item) | Yes/No | ||
| Mental health | |||
| Stress | Perceived Stress Scale (PSS) [37] (10 items) | ≥ score of 10; < score of 10 higher scores indicate more frequent report of perceived stress | |
| Depressive Symptoms | Centers for Epidemiologic Studies Depression Scale (CES-D) [38] (10 items) | ≥ score of 10; < score of 10; higher scores indicate more frequent report of depressive symptoms | |
| Perceived discrimination | Perceived Discrimination Scale, Daily Discrimination Subscale [39] (9 items) | Scale of 0–45; low vs high based on median split with higher scores indicating more perceived discrimination |
Statistical approach
Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). All analyses took into account stratified recruitment and controlled for clustering by block using the survey procedures in SAS 9.4. We characterized the population using descriptive statistics and compared Hispanics/Latinos to non-Hispanic whites using chi-square tests for categorical measures. Means and standard deviations are reported for continuous measures (e.g. BMI, individual, family, community level and cultural/contextual determinants). Since these measures were not normally distributed in our sample, we report p-values where we log transformed values and tested for differences between ethnic groups using generalized linear regression. Logistic regression was used to compare the prevalence of overweight (BMI 25–29.9 kg/m2) and obesity (BMI ≥ 30 kg/m2) between Hispanic and non-Hispanic whites, adjusting for age and gender. Mean log BMI values within each ethnic group were compared by individual, family, community, and cultural/contextual factors using generalized linear models. To examine social determinant risk factors of obesity (BMI ≥ 30 kg/m2), we compared determinants among individuals with obesity to those without obesity, stratified by ethnic group and adjusted for age and gender. Estimates are reported as odds ratios (OR) with 95% confidence intervals (95% CI).
Results
Characteristics of the study sample overall and by ethnic group are presented in Table 2. Hispanics/Latinos were roughly 10 years younger at the time of assessment compared to non-Hispanic whites, were less likely to hold a high school education, and were less likely to have health insurance. In terms of health behaviors and other determinants, Hispanics/Latinos engaged in fewer minutes of sedentary behavior and reported stronger family cohesion than non-Hispanics whites. Hispanics/Latinos had smaller social networks, reported lower neighborhood cohesion, and less civic trust than non-Hispanic whites. Hispanics/Latinos were more likely to be overweight compared to non-Hispanic whites (OR 1.93, 95% CI: 1.05–3.55) after adjusting for age and gender (Fig. 2).
Table 2.
Characteristics of the study sample overall and by ethnic group
| All participants, N = 217 | Latino, n = 106 | White, n = 111 | P-value | |
|---|---|---|---|---|
|
| ||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age at assessment | 40.9 (21.4) | 34.6 (11.8) | 46.9 (18.9) | <0.001 |
| BMI, kg/m2 | 30.5 (8.3) | 30.8 (6.3) | 30.3 (8.3) | 0.67 |
| Length time in US | – | 14.18 (6.8) | – | – |
| N (%) | N (%) | N (%) | ||
| Sex | 0.25 | |||
| Male | 80 (36.9) | 43 (40.6) | 37 (33.3) | |
| Female | 137 (63.1) | 63 (59.4) | 74 (66.7) | |
| Education | <0.001 | |||
| Less than HS | 95 (44.0) | 74 (69.8) | 22 (19.8) | |
| HS | 98 (45.4) | 28 (26.4) | 70 (63.1) | |
| College degree | 23 (10.6) | 4 (3.8) | 19 (17.1) | |
| Employment | 0.03 | |||
| Employed | 123 (56.7) | 68 (64.2) | 55 (49.5) | |
| Unemployed | 94 (43.3) | 38 (35.8) | 56 (50.5) | |
| Insurance status | 0.001 | |||
| Yes | 107 (49.3) | 26 (24.5) | 84 (75.7) | |
| No | 110 (50.7) | 80 (75.5) | 27 (24.3) | |
| Marital status | 0.85 | |||
| Single/divorced | 106 (48.8) | 51 (48.1) | 55 (49.5) | |
| Married/live together | 111 (51.2) | 55 (51.9) | 56 (50.5) | |
| BMI category | 0.01 | |||
| Normal | 35 (16.1) | 9 (8.5) | 26 (23.4) | |
| Overweight | 87 (40.1) | 49 (46.2) | 38 (34.2) | |
| Obese | 95 (43.8) | 48 (45.3) | 47 (42.3) | |
| Mean (SD) | Mean (SD) | Mean (SD) | p-value | |
| Individual * | ||||
| Servings fruits and vegetables/day | 2.3 (2.2) | 2.2 (2.3) | 2.4 (1.9) | 0.12 |
| Physical activity, min/day | 124.9 (136.7) | 112.4 (119.4) | 137.0 (146.6) | 0.10 |
| Sedentary time, min/day | 209.1 (203.7) | 158.0 (183.5) | 258.0 (185.8) | <0.001 |
| Family * | ||||
| Family cohesion | 38.5 (9.0) | 41.3 (8.6) | 35.8 (7.9) | <0.001 |
| Family encouragement | 2.2 (1.0) | 2.3 (1.0) | 2.1 (0.9) | 0.26 |
| Family participation | 1.9 (0.7) | 2.0 (0.8) | 1.8 (0.8) | 0.13 |
| Social network size | 3.2 (2.1) | 2.6 (1.4) | 3.7 (1.8) | <0.001 |
| Food insecurity | 1.6 (0.6) | 1.6 (0.6) | 1.5 (0.8) | 0.75 |
| Community * | ||||
| Neighborhood cohesion | 3.4 (1.0) | 3.2 (0.7) | 3.5 (1.1) | 0.03 |
| Neighborhood disorder | 24.9 (8.7) | 25.4 (6.7) | 24.3 (9.6) | 0.29 |
| Civic trust | 24.0 (5.3) | 22.8 (3.5) | 25.2 (5.6) | <0.001 |
| Physical Activity resources | 7.9 (2.7) | 7.8 (2.4) | 8.1 (2.6) | 0.39 |
| Cultural/contextual * | ||||
| Perceived Stress Scale | 14.9 (9.0) | 15.0 (6.7) | 14.9 (9.9) | 0.94 |
| CES-D | 5.5 (4.2) | 5.3 (3.1) | 5.8 (4.7) | 0.37 |
| Perceived Discrimination | 7.9 (8.4) | 8.1 (8.9) | 7.8 (8.1) | 0.80 |
Bold values represent significance of p < 0.05
SD Standard deviation;
based on the Community Energy Balance (CEB) framework
Fig. 2.
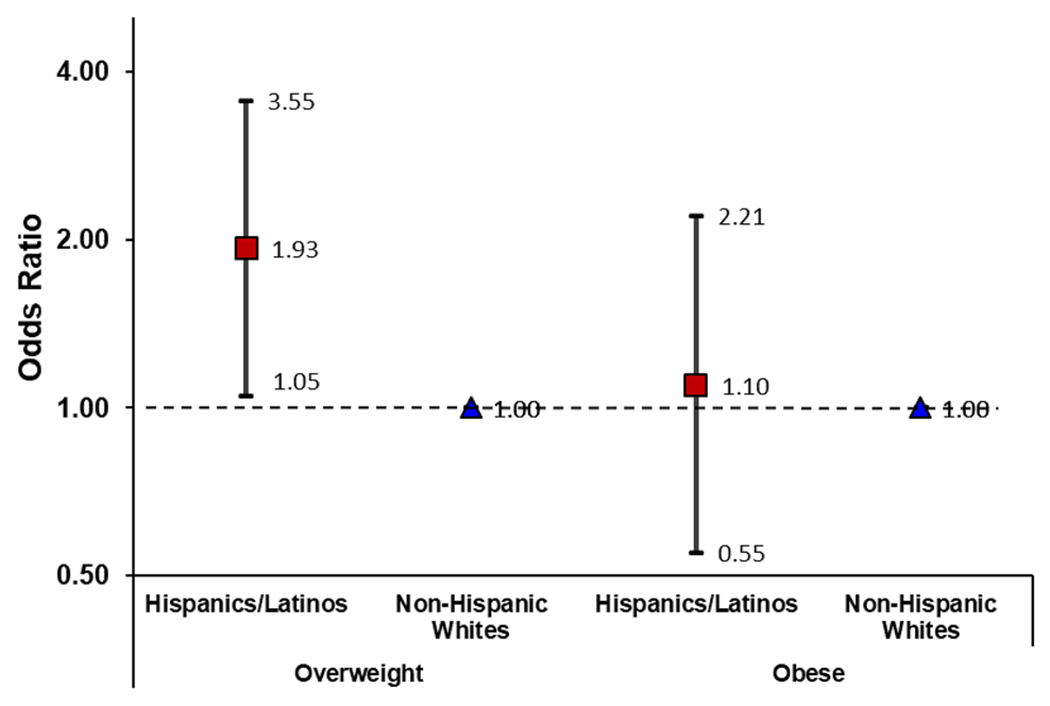
Prevalence of overweight and obesity among Hispanics/Latinos compared to non-Hispanic whites, adjusted for age and gender
Figure 3 shows mean BMI values by social determinants within ethnic groups. BMI did not differ across levels of most determinants within each respective ethnic group. However, Hispanics/Latinos who were less aware of physical activity resources in their community had higher log BMI values (p’s < 0.05) than Hispanics/Latinos who reported more awareness of resources. Non-Hispanic whites who reported consuming less than 5 servings of fruits and vegetables per day, more frequent depressive symptoms, and more family encouragement had significantly higher BMI’s (p’s < 0.05).
Fig. 3.
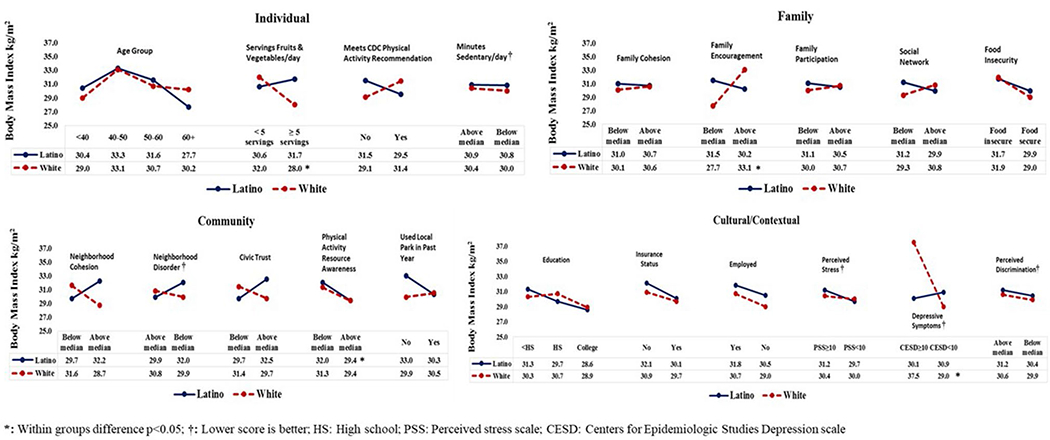
Mean BMI values by social determinants within each Community Energy Balance level, stratified by ethnicity
Outside of these few significant findings, there were no statistical differences in BMI across other determinants within each ethnic group. However, visual inspection of the plots in Fig. 3 indicate that effects of determinants on BMI vary strikingly depending on ethnicity. For instance, unfavorable family/interpersonal determinants were indicative of a higher BMI for Hispanics/Latinos with the opposite effect seen in non-Hispanic whites. Conversely, favorable neighborhood determinants (e.g. cohesion, trust) were indicative of a higher BMI among Hispanics/Latinos and the opposite effect among non-Hispanic whites.
Determinants for increased risk of obesity (BMI ≥ 30 kg/m2) by ethnic group are presented in Table 3. Hispanics/Latinos who reported more frequent perceived discrimination were three times as likely to be obese compared to those who reported less perceived discrimination (OR 3.01, 95% CI: 1.25–7.22). No other significant factors emerged.
Table 3.
Social determinants of obesity risk (BMI ≥ 30 kg/m2), stratified by ethnicity and adjusted for age and gender
| Determinant | Hispanics/Latinos | P-value | Non-Hispanic Whites | P-value |
|---|---|---|---|---|
|
| ||||
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |||
| Interpersonal/family | ||||
| Family cohesion | ||||
| Above median | 1.00 | 1.00 | ||
| Below median | 1.66 (0.67–4.10) | 0.27 | 0.65 (0.33–1.26) | 0.20 |
| Family encouragement | ||||
| Above median | 1.00 | 1.00 | ||
| Below median | 1.83 (0.87–3.85) | 0.11 | 0.19 (0.08–0.44) | <0.001 |
| Family participation | ||||
| Above median | 1.00 | 1.00 | ||
| Below median | 0.99 (0.49–2.00) | 0.98 | 0.57 (0.28–1.16) | 0.12 |
| Social Network size | ||||
| Above median | 1.00 | 1.00 | ||
| Below median | 1.31 (0.52–3.28) | 0.56 | 0.60 (0.28–1.31) | 0.20 |
| Food insecurity | ||||
| Food insecure | 1.17 (0.53–2.60) | 0.69 | 1.06 (0.47–2.41) | 0.89 |
| Food secure | 1.00 | 1.00 | ||
| Community/contextual | ||||
| Neighborhood cohesion | ||||
| Above median | 1.00 | 1.00 | ||
| Below median | 0.84 (0.36–1.96) | 0.68 | 1.49 (0.74–2.98) | 0.26 |
| Discrimination | ||||
| Above median | 3.01 (1.25–7.22) | 0.01 | 0.83 (0.35–1.99) | 0.68 |
| Below median | 1.00 | 1.00 | ||
| Neighborhood disorder | ||||
| Above median | 0.59 (0.29–1.21) | 0.15 | 0.91 (0.40–2.10) | 0.83 |
| Below median | 1.00 | 1.00 | ||
| Civic trust | ||||
| Above median | 1.00 | 1.00 | ||
| Below median | 0.77 (0.33–1.80) | 0.54 | 0.72 (0.30–1.72) | 0.45 |
| Physical activity resources | ||||
| Above median | 1.00 | 1.00 | ||
| Below median | 1.20 (0.45–1.03) | 0.71 | 0.98 (0.49–1.99) | 0.96 |
| Used park in last year | ||||
| Yes | 1.00 | 1.00 | ||
| No | 0.87 (0.28–2.68) | 0.80 | 0.80 (0.32–1.99) | 0.63 |
Discussion
In this examination of the social determinants of obesity among Hispanics/Latinos and non-Hispanic whites living in a rural community, we found that the prevalence of obesity was similar, the prevalence of overweight was higher, and the determinants of obesity varied by ethnic groups. More frequent reporting of perceived discrimination was associated with obesity among Hispanics/Latinos. We also found positive associations, albeit not statistically significant, between unfavorable family determinants and BMI/obesity among Hispanic/Latinos. In contrast, non-Hispanic whites who reported unfavorable neighborhood characteristics had higher BMI’s and were more at risk for obesity. Findings highlight that social determinants of obesity vary based on ethnicity and sometimes in unexpected ways. Preliminary findings should be validated in a larger sample moving forward, but they suggest potentially targeted approaches to the prevention and control of obesity.
The association observed such that Hispanics/Latinos in our sample who frequently reported perceived discrimination were more likely to be obese than Hispanics/Latinos that did not report frequent discrimination; are in line with other investigations. A recent study found that more frequent perceived discrimination was associated with BMI and central adiposity in a group of Hispanic adults [40]; similar findings have been reported among other minorities [41, 42]. Our positive estimates here suggested that, while not significant, Hispanics who reported unfavorable family determinants were more likely to be obese. While the traditional value of familism (dedication to family) is a characteristic of the Hispanic culture, associations with weight loss and obesity have been mixed [43–45], in part, due to varied measurement approaches. Further, Hispanics/Latinos who had fewer social networks and less knowledge about physical activity resources were more likely to be obese. Social networks have been associated with weight loss among Hispanics/Latinos, although the size and composition of networks can have either positive or negative effects [46, 47]. Social capital (a concept that includes social network size and quality among other factors) has also been linked to obesity risk [48]. Acknowledging perceived discrimination, harnessing the protective mechanisms of family support, and bolstering social networks and capital may be potential intervention targets for Hispanics/Latinos with obesity.
Interestingly, Hispanics/Latinos who reported more neighborhood cohesion and civic trust had higher BMI’s and were more at risk for obesity than those who reported less cohesion/trust and more disorder, which seems counter-intuitive. In fact, one recent study found an association between cohesion and lower BMI in Hispanics [49]. Our findings may represent the clustering of Hispanics/Latinos in communities (such as Albertville) where cultural factors of cohesion and trust are fostered, along with other cultural factors such as food choices, cooking styles, and family sedentary behaviors that may promote obesity [50]. Cultural factors have been speculated to contribute to the Hispanic paradox, a well-documented phenomenon where Hispanics/Latinos with high risk factors exhibit lower rates of poor health outcomes [51].
Our results highlight the importance of examining how family factors and social networks are associated with obesity risk among Hispanics/Latinos to inform intervention targets to reduce disparities in health. As seen in our study, there were different findings based on ethnic group, providing insight into how to culturally adapt or develop targeted interventions [52] to mitigate obesity. The CEB framework emphasizes the need to address cultural-contextual interactions that influence an individual’s energy balance [25]. The framework provides researchers with information and strategies to design interventions that acknowledge the role of contextual facilitators and barriers to shaping obesity-related health behaviors. Suggestions for fostering social capital include developing community physical activities (e.g. walking clubs) and encouraging advocacy for healthier environments [53]. Family targets include promoting effective parenting strategies and structural aspects of the home environment to influence food choices, food availability, and physical activity [54, 55].
Reported findings should be interpreted within the context of several limitations. Our sample size was small for risk factor analysis, and findings should be validated in a larger cohort. Our Hispanic/Latino sample was considerably younger than the non-Hispanic whites in our study, introducing age bias. While we controlled for age in most analyses, interpretations of estimates should be viewed with caution. Further, we limited our study to Hispanic/Latino and non-Hispanic whites; including other races would have allowed for additional comparisons across other at-risk groups [2]. Another limitation, common in studies that survey community level attributes, is the lack of standardized and validated measures of social and neighborhood level determinants making direct comparisons between studies difficult. Many of the scales used in this study do not report psychometric properties and have not been used across multiple studies or populations. Our small sample was limited to a specific community in a rural, Southeastern state, making widespread generalizability problematic. Lastly, our counter-intuitive findings may be unique to our sample, context, or measures; validation of our results are needed.
Despite these limitations, our study has several strengths that should be emphasized. Our study provides much needed data regarding social determinants and obesity risk among Hispanic/Latino adults living in the U.S. and in emerging communities more specifically, regardless of power or direction of estimates. Our approach was effective in identifying potential differences in determinants of obesity risk between Hispanics/Latinos and non-Hispanic whites in the Southeastern U.S. Consistent with calls to use both an etic and emic approach, reporting these types of data will help move the field towards standardization of social determinant measures that are sensitive to context and racial/ethnic group. Additionally, our sampling method allowed us to successful recruit a balanced sample in a community study and therefore minimized selection bias. Lastly our study utilized the CEB framework to systematically assess determinants across multiple systems that contribute to obesogenic environments.
Conclusion
Overall, we find that associations between social determinants of health and obesity varied by ethnic group in our study. Perceived discrimination, unfavorable family factors and small social networks were determinants for Hispanics/Latinos obesity but not for non-Hispanic whites, warranting further exploration. Nonetheless, it is important to stress that these findings are a preliminary step. Future work should query a larger, more representative sample of Hispanics and explore concepts using standardized measures.
Acknowledgements
We especially thank Matthew Carle, Morgan Griesemer Lepard, Ynhi Thai, Meghan Meehan, Amancia Carrera, Sylvia Alavarez Mancinas, Susan Henry Barber, and Chris Caudill for their tireless efforts to canvas neighborhoods and interviews participants. We would also like to thank all our participants, the office of the Mayor of Albertville, the Albertville Police Department, support staff, and others who helped make this study possible.
Funding
This work was supported by the National Institute on Minority Health and Health Disparities under grant U54MD008176; and the National Institute of Diabetes and Digestive and Kidney Diseases, UAB Diabetes Research Center under grant 1P60DK079626-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Minority Health and Health Disparities or National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health or others supporting this work.
Conflict of Interest
All authors have no conflicts of interest or financial relationships relevant to this article to disclose. All sources of funding had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Footnotes
Ethical Approval The study was reviewed and approved by the institution’s review board.
Consent to Participate Informed consent was obtained from all individual participants included in the study.
References
- 1.World Health Organization. Obesity and Overweight Fact Sheet No. 311. 2013. [cited 2020 October 27]. http://www.who.int/mediacentre/factsheets/fs311/en/index.html.
- 2.Hales CM CM, Fryar CD, Ogden CL Prevalence of obesity among adults and youth: United States, 2015–2016. Hyattsville, MD: National Center for Health Statistics; 2017. Report No.: 288. [Google Scholar]
- 3.Benavides-Vaello S Cultural influences on the dietary practices of Mexican Americans: a review of the literature. Hispanic Health Care Int. 2005;3:27–35. [Google Scholar]
- 4.Kaplan MS, Huguet N, Newsom JT, McFarland BH The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med. 2004;27(4):323–6. [DOI] [PubMed] [Google Scholar]
- 5.Perez-Escamilla R, Putnik P The role of acculturation in nutrition, lifestyle, and incidence of type 2 diabetes among Latinos. J Nutr. 2007;137(4):860–70. [DOI] [PubMed] [Google Scholar]
- 6.Sallis JF, Floyd MF, Rodriguez DA, Saelens BE Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pachucki MA, Jacques PF, Christakis NA Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101(11):2170–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallis JF, Cerin E, Conway TL, Adams MA, Frank LD, Pratt M, et al. Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. Lancet. 2016;387(10034):2207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larson N, Story M A review of environmental influences on food choices. Ann Behav Med. 2009;38(Suppl 1):S56–73. [DOI] [PubMed] [Google Scholar]
- 10.Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16(2):175–90. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Closing the gap in a generation: Health equity through action on the social determinants of health. 2008. [cited 2020 October 27]. http://www.who.int/social_determinants/thecommission/finalreport/en/index.html.
- 12.Monteiro CA, Moura EC, Conde WL, Popkin BM Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ. 2004;82(12):940–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–9. [DOI] [PubMed] [Google Scholar]
- 14.Powell K, Wilcox J, Clonan A, Bissell P, Preston L, Peacock M, et al. The role of social networks in the development of overweight and obesity among adults: a scoping review. BMC Public Health. 2015;15:996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glonti K, Mackenbach JD, Ng J, Lakerveld J, Oppert JM, Bardos H, et al. Psychosocial environment: definitions, measures and associations with weight status–a systematic review. Obes Rev. 2016;17(Suppl 1):81–95. [DOI] [PubMed] [Google Scholar]
- 16.Baquero B, Molina M, Elder JP, Norman GJ, Ayala GX Neighborhoods, social and cultural correlates of obesity risk among Latinos living on the US-Mexico border in Southern California. J Health Care Poor Underserved. 2016;27(4):1934–55. [DOI] [PubMed] [Google Scholar]
- 17.Pew Hispanic Center. Statistical Portrait of Hispanics in the United States. 2009. [cited 2020 October 27]. http://pewhispanic.org/factsheets/factsheet.php?FactsheetID=70.
- 18.Institute for Latinx Health Equity. Emerging Populations Defined. [cited 2020 October 27]. https://ilhe.org/emerging-population-defined/.
- 19.Passel J, Cohen D, Hugo-Lopez M Hispanics Account for More than Half of Nation’s Growth in Past Decade. Washington, DC: Pew Hispanic Center; 2011. http://www.pewhispanic.org/2011/03/24/hispanics-account-for-more-than-half-of-nations-growth-in-past-decade/. [Google Scholar]
- 20.Amirehsani K Mexican Americans with type 2 diabetes in an emerging Latino community: evaluation of health disparity factors and interventions. Home Health Care Manag Pract. 2010;22(7):470–8. [Google Scholar]
- 21.Kochlar R, Suro R, Tafoya S The New Latino South: the context and consequences of rapid population growth. Washington, DC: Pew Hispanic Center; 2005. http://pewhispanic.org/reports/report.php?ReportID=50. [Google Scholar]
- 22.Shattell M, Villalba J, Stokes N, Hamilton D, Foster J, Petrini H, et al. Depression in Latinas residing in emerging Latino immigrant communities in the United States. Hispanic Health Care Int. 2009;7(4):190–202. [Google Scholar]
- 23.Martinez J, Powell J, Agne A, Scarinci I, Cherrington A A focus group study of Mexican immigrant men’s perceptions of weight and lifestyle. Public Health Nurs. 2012;29(6):490–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levi J, Segal L, Laurent R, Kohn D F as in Fat: How Obesity Threatens America’s Future. Washington, D.C.: Trust for America’s Health and the Robert Wood Johnson Foundation; 2011. http://www.healthyamericans.org/assets/files/TFAH2011FasInFat10.pdf. [Google Scholar]
- 25.Kumanyika S, Taylor WC, Grier SA, Lassiter V, Lancaster KJ, Morssink CB, et al. Community energy balance: a framework for contextualizing cultural influences on high risk of obesity in ethnic minority populations. Prev Med. 2012;55(5):371–81. [DOI] [PubMed] [Google Scholar]
- 26.US Census Bureau. QuickFacts: Albertville, AL. https://www.census.gov/quickfacts/fact/table/albertvillecityalabama/PST045218.
- 27.Howell CR, Su W, Nassel AF, Agne AA, Cherrington AL Area based stratified random sampling using geospatial technology in a community-based survey. BMC Public Health. 2020;20(1):1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Community Assessment for Public Health Emergency Response (CASPER), Sampling Methodology. https://www.cdc.gov/nceh/casper/sampling-methodology.htm.
- 29.Block G, Gillespie C, Rosenbaum EH, Jenson C A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med. 2000;18(4):284–8. [DOI] [PubMed] [Google Scholar]
- 30.Armstrong T, Bull F Development of the world health organization global physical activity questionnaire (GPAQ). J Public Health. 2006;14(2):66–70. [Google Scholar]
- 31.Olson DH, Portner J, Lavee Y “Faces III”: family adaptability & cohesion evaluation scales. St. Paul: University of Minnesota; 1985. [Google Scholar]
- 32.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–36. [DOI] [PubMed] [Google Scholar]
- 33.Marquez B, Elder JP, Arredondo EM, Madanat H, Ji M, Ayala GX. Social network characteristics associated with health promoting behaviors among Latinos. Health Psychol. 2014;33(6):544–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.US Department of Agriculture. Six-Item Short Form of the Food Security Survey Module. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools/
- 35.Community Surveys: Resource Guide, Project on Human Development in Chicago Neighborhoods. https://www.icpsr.umich.edu/web/pages/NACJD/guides/phdcn/community-survey.html#csInstrumentsMeasures. Accessed 1 May 2020
- 36.Ross CE, Mirowsky J Disorder and decay: the concept and measurement of perceived neighborhood disorder. Urban Aff Rev. 1999;34(3):412–32. [Google Scholar]
- 37.Cohen S, Kamarck T, Mermelstein R A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 38.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 39.Williams DR, Yan Y, Jackson JS, Anderson NB Racial differences in physical and mental health: socio-economic Status. Stress Discrimination J Health Psychol. 1997;2(3):335–51. [DOI] [PubMed] [Google Scholar]
- 40.Molina KM, Estrella ML, Rivera-Olmedo N, Frisard C, Lemon S, Rosal MC. It weigh(t)s on you: everyday discrimination and adiposity among Latinos. Obesity (Silver Spring). 2018;26(9):1474–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gee GC, Ro A, Gavin A, Takeuchi DT Disentangling the effects of racial and weight discrimination on body mass index and obesity among Asian Americans. Am J Public Health. 2008;98(3):493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thorpe RJ Jr, Parker LJ, Cobb RJ, Dillard F, Bowie J. Association between discrimination and obesity in African-American men. Biodemography Soc Biol. 2017;63(3):253–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arevalo Avalos MR, Ayers SL, Patrick DL, Jager J, Castro FG, Konopken YP, et al. Familism, self-esteem, and weight-specific quality of life among latinx adolescents with obesity. J Pediatr Psychol. 2020;45(8):848–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McLaughlin EA, Campos-Melady M, Smith JE, Serier KN, Belon KE, Simmons JD, et al. The role of familism in weight loss treatment for Mexican American women. J Health Psychol. 2017;22(12):1510–23. [DOI] [PubMed] [Google Scholar]
- 45.Salvy SJ, Miles JN, Shih RA, Tucker JS, D’Amico EJ. Neighborhood, family and peer-level predictors of obesity-related health behaviors among young adolescents. J Pediatr Psychol. 2017;42(2):153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wieland ML, Njeru JW, Okamoto JM, Novotny PJ, Breen-Lyles MK, Goodson M, et al. Association of social network factors with weight status and weight loss intentions among hispanic adults. J Behav Med. 2020;43(2):155–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Winston GJ, Phillips EG, Wethington E, Devine C, Wells M, Peterson JC, et al. Social network characteristics associated with weight loss among black and hispanic adults. Obesity (Silver Spring). 2015;23(8):1570–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim D, Subramanian SV, Gortmaker SL, Kawachi I. US state- and county-level social capital in relation to obesity and physical inactivity: a multilevel, multivariable analysis. Soc Sci Med. 2006;63(4):1045–59. [DOI] [PubMed] [Google Scholar]
- 49.Wong MS, Chan KS, Jones-Smith JC, Colantuoni E, Thorpe RJ Jr, Bleich SN. The neighborhood environment and obesity: understanding variation by race/ethnicity. Prev Med. 2018;111:371–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hernandez R, Carnethon M, Giachello AL, Penedo FJ, Wu D, Birnbaum-Weitzman O, et al. Structural social support and cardiovascular disease risk factors in Hispanic/Latino adults with diabetes: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Ethn Health. 2018;23(7):737–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis 2001;11(3):496–518. [PubMed] [Google Scholar]
- 52.Kreuter MW, Thompson T, McQueen A, Garg R. Addressing social needs in health care settings: evidence, challenges, and opportunities for public health. Annu Rev Public Health. 2020;42:epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Elder JP, Ayala GX, Arredondo EM, Talavera GA, McKenzie TL, Hoffman L, et al. Community health partnerships for chronic disease prevention among Latinos: the San Diego Prevention Research Center. J Prim Prev. 2013;34(1–2):17–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arredondo EM, Ayala GX, Soto S, Slymen DJ, Horton LA, Parada H, et al. Latina mothers as agents of change in children’s eating habits: findings from the randomized controlled trial Entre Familia: Reflejos de Salud. Int J Behav Nutr Phys Act. 2018;15(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Crespo NC, Elder JP, Ayala GX, Slymen DJ, Campbell NR, Sallis JF, et al. Results of a multi-level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Ninos Study. Ann Behav Med. 2012;43(1):84–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cheung FM, van de Vijver FJ, Leong FT. Toward a new approach to the study of personality in culture. Am Psychol. 2011;66(7):593–603. [DOI] [PubMed] [Google Scholar]


