ABSTRACT
Most COVID-19 studies aim to assess factors influencing willingness to pay for vaccines between the public and medical staff. However, few studies focus on parents’ willingness to pay for their children’s COVID-19 vaccine. The current study aimed to assess parents’ willingness to pay for their children’s vaccination against COVID-19 and its influencing factors. This population-based cross-sectional study used a self-administered questionnaire. The inclusion criterion was parents with at least one child younger than 18 years. The final analysis included 384 valid data points. A total of 89.1% of the parents indicated that they are willing to pay for their children’s vaccination against COVID-19. Among them, both fathers’ and mothers’ willingness to pay for their children’s COVID-19 vaccine was 89.6%. The mean and median willingness to pay were% would pay for their children. Excluding other confounding factors, willingness to pay for the COVID-19 vaccine for themselves and hesitation to vaccinate their children were significantly associated with parents’ willingness to pay for their children’s COVID-19 vaccine. We found that 89.1% of the parents in Taiwan would pay for their children’s COVID-19 vaccine. Parents’ willingness to pay for themselves and hesitation to vaccinate their children were associated with willingness to pay. Reducing hesitation about vaccines and developing policies for vaccine payment may have a positive impact on willingness to pay for vaccines and promoting COVID-19 vaccination.
KEYWORDS: Willingness to pay, COVID-19 vaccine, parents, children, China, Taiwan
Introduction
Willingness to pay (WTP) for a vaccine is an assessment of the maximum amount people are willing to spend on vaccination.1,2 Previous studies found that WTP is influenced by many factors, such as an individual’s health status, socioeconomic characteristics, previous vaccination history, knowledge, attitudes and practices regarding vaccination, and peer or physician recommendations.3 The factors influencing WTP may also vary across different regions or populations.4 Therefore, identifying the determinants associated with WTP is crucial for reducing the risk of recurrent widespread outbreaks.5
An outbreak of severe acute respiratory syndrome was caused by the coronavirus disease in 2019 (COVID-19). People had no resistance to this emerging virus.6 Vaccination helps to achieve herd immunity and is considered as one of the most effective methods of combating the COVID-19 pandemic. Most significantly, it lowers the prevalence of COVID-19 in children.7 However, the SARS-CoV-19 virus is subject to constant mutation, and commercially available vaccines provide only limited immunity; therefore, regular vaccinations are required to achieve successful herd immunity.8 To enhance the availability of the COVID-19 vaccine, it has been made available for children aged 3–17 years since July 2021.9
Parents are key decision-makers in determining children’s WTP for COVID-19 vaccination, and measuring parental attitudes plays an important role in achieving full childhood immunization.10,11 There are limited studies assessing parents’ WTP and its influencing factors on their children’s COVID-19 vaccination. A study in the United States showed that men, African Americans, and Africans had a higher WTP for their offspring, and that this WTP increased with income.12 A cross-sectional study in the Taizhou region of China showed that lower literacy levels, one-child families, knowledge of vaccine use, and parents’ WTP for themselves are four aspects that can influence parents’ WTP for their children.9
Few studies have examined parents’ WTP for their children’s COVID-19 vaccine. The current study, conducted in Taiwan, China, was designed to assess parents’ WTP for their children’s COVID-19 vaccine and its influencing factors.
Materials and methods
Study design and population
This population-based cross-sectional study was based on an online survey that was conducted among parents in Taiwan between July 14, 2021, and September 23, 2021. Participants completed a questionnaire survey using the WeChat platform. The inclusion criterion was being a parent with at least one child younger than 18 years. Exclusion criteria: Taiwan residents who are unwilling to participate in the survey, unmarried or whose children’s age is higher than 18 years old. The study procedure was approved by the Ethics Committee of Taizhou Hospital, Zhejiang Province, and was performed in accordance with the ethical guidelines of the World Medical Association (Declaration of Helsinki) and the CHERRIES statement. Participants’ personal information was fully anonymized.
Questionnaire frame
An online questionnaire comprising multiple sections was developed, based on previous relevant research and a framework for estimating WTP for the COVID-19 vaccine.9,13 The formal questionnaire was determined by a panel of two experts in the relevant field to ensure that the content was comprehensive, valid and scientific. The initial questionnaire was first tested, then revised based on feedback from the test population, and finally the formal questionnaire was finalized. The sections are as follows:
Basic demographic information (gender, age, place of residence, education level, previous vaccination history).
Parental knowledge related to the COVID-19 vaccine, including the following questions: “How much do you know about the COVID-19 vaccine,” “how effective do you think the COVID-19 vaccine is in preventing COVID-19 pneumonia,” and “how safe do you feel the current COVID-19 vaccine is?”
Parental hesitation and WTP for their own COVID-19 vaccination was addressed using these questions: “Have you ever hesitated to get the COVID-19 vaccine, whether you received it or not,” “would you get it if you had to pay for the COVID-19 vaccine,” and “what price would you accept for the COVID-19 vaccine?”
With regard to parents’ hesitation and WTP for their child’s COVID-19 vaccination, we asked the following questions: “Do you hesitate to have your children receive the COVID-19 vaccine,” “are you likely to vaccinate your children if there is a fee for the COVID-19 vaccine,” and “what is the price you are willing to pay for the COVID-19 vaccine for your child?”
For simplicity, parents’ WTP for themselves, parents’ WTP for their children, and parents’ hesitance about vaccines were re-recorded in the final analysis. “Very willing” and “willing” to be marked “yes;” “Very reluctant” and “reluctant” to be marked “no.”
Statistical analysis
This study used chi-squared tests and a binary logistic regression analysis to identify the factors associated with parents’ WTP for children in two steps. In the first step, the variables in our study were all enumeration data, so a χ2 (chi-square) test was applied to compare the discrepancies between the WTP group and the reluctant to pay (RTP) group, which initially assessed possible factors associated with parents’ WTP for their children’s vaccines; these include gender, place of residence, education level, knowledge and attitude toward the COVID-19 vaccine, and hesitation to vaccinate their children. Second, in the variables with statistical significance in the chi-square test, binary logistic regression was performed to identify the factors associated with parents’ WTP for the vaccine for their children. All inferential tests were performed under the following assumptions: corrected advantage ratios with 95% CI and p-values (p < .05). The mean and median of the estimated WTP are shown in dollars. Data were analyzed using IBM SPSS statistics 26.0 software (SPSS Inc, Chicago, IL, USA). A p-value <.05 was established to represent statistical significance among the test populations.
Results
Sociodemographic characteristics of the parents
A total of 384 parents completed the online questionnaire. Table 1 presents the sociodemographic characteristics of the parents. Of the 384 parents, 80.2% (308/384) were female, 84.6% (325/384) lived in urban areas, 90.1% (346/384) had a university or higher education, and 43.0% (165/384) were medical workers.
Table 1.
Sociodemographic characteristics of the parents (N = 384).
| Characteristics | N (%) |
|---|---|
| Gender | |
| Male | 76 (19.8) |
| female | 308 (80.2) |
| Education level | |
| Senior Secondary and below | 38 (9.9) |
| Undergraduate and above | 346 (90.1) |
| Number of children (<18 years) | |
| One | 145 (37.8) |
| Two | 203 (52.9) |
| Three and above | 36 (9.3) |
| Occupation | |
| Worker | 111 (28.9) |
| Medical worker | 165 (43.0) |
| Education | 37 (9.6) |
| Civil servant | 18 (4.7) |
| Other | 53 (13.8) |
| Residence | |
| Urban | 325 (84.6) |
| Towns & Rural | 59 (15.4) |
| Parents’ WTP for COVID-19 vaccine for their children | |
| Yes | 342 (89.1) |
| No | 42 (10.9) |
| Parents’ WTP for COVID-19 vaccine for their themselves | |
| Yes | 322 (83.9) |
| No | 62 (16.1) |
| Price paid by parents for their children’s COVID-19 vaccine(NT) | |
| <1000 | 278 (72.4) |
| 1000 ~ 1499 | 72 (18.6) |
| 1500 ~ 1999 | 19 (5.0) |
| >2000 | 15 (4.0) |
Relationship between parents’ WTP for their children and for themselves
Parents willing to pay for their children’s vaccines comprised 89.1% (342/384). Among them, both fathers’ and mothers’ WTP for their children’s COVID-19 vaccines was 89.6%. As shown in Table 1, a total of 72.4% (278/384) of parents were willing to pay less than NT 1,000 ($33.20) for their children’s vaccinations; 83.9% (322/384) of parents would pay for the vaccine for themselves, and 73.4% (282/384) of parents were willing to pay the same amount, NT 1,000 (US$ 33.20), for themselves. The mean and median amounts parents were willing to pay for themselves or their children were <NT 1,000 (US$ 33.20). From Figure 1, we can see an interesting finding that of the parents who were not willing to pay for the COVID-19 vaccine for themselves, 56.5% (35/62) would pay for their child and of those who would pay for themselves, 95.3% (307/322) were willing to pay for their child. The relationships between parents’ WTP for themselves and parents’ WTP for their children were significant (p-value <.001) both in fathers and mothers.
Figure 1.
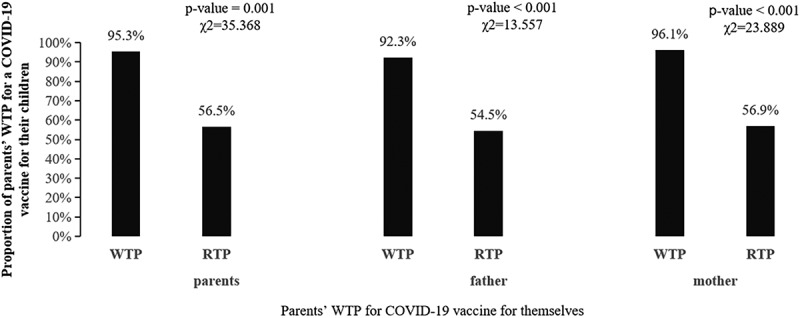
Relationship between parents’ WTP for their children and for themselves.
Factors affecting parents’ WTP for the COVID-19 vaccine for their children
As shown in Table 2, the χ2 (chi-square) test showed an inconsistency between the WTP group and the RTP group. We assessed the potential factors of WTP for several univariate variables: education level (χ2 = 2.425, p = .119), degree of knowledge of the COVID-19 vaccine (χ2 = 4.638, p = .031), preventive effect of the COVID-19 vaccine (χ2 = 6.332, p = .012), safety of the COVID-19 vaccine (χ2 = 7.871, p = .005), parents’ hesitation to vaccinate themselves (χ2 = 0.459, p = .498), parents’ WTP for their own COVID-19 vaccine (χ2 = 80.720, p < .001), and parents’ hesitation to vaccinate their children (χ2 = 9.603, p = .002). Mothers had the same potential factors of WTP for their children’s vaccine as parents overall (mothers and fathers). However, the WTP for their COVID-19 vaccination among fathers (χ2 = 11.741, p = .001) differed between the RTP and WTP group. However, there were no statistical differences in parents’ WTP in terms of gender, place of residence, education level, and previous vaccination history with the COVID-19 vaccine.
Table 2.
Differences in parents’ WTP for their children’s COVID-19 vaccination between WTP group and RTP group (N = 384).
| Parents (n = 384) |
Fathers (n = 76) |
Mothers (n = 308) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WTP | RTP | WTP | RTP | WTP | RTP | |||||
| Variables | Categories | (n = 342) | (n = 42) | p-value | (n = 66) | (n = 10) | p-value | (n = 276) | (n = 32) | p-value |
| Gender | men | 66 (19.3) | 10 (23.8) | .489 | 66 (100) | 10 (100) | / | / | / | / |
| women | 276 (80.7) | 32 (76.2) | / | / | 276 (100) | 32 (100) | ||||
| Residence | urban | 291 (85.1) | 34 (81.0) | .483 | 58 (87.9) | 7 (70.0) | .134 | 233 (84.4) | 27 (84.4) | .995 |
| Towns & Rural | 51 (14.9) | 8 (19.0) | 8 (12.1) | 3 (30.0) | 43 (15.6) | 5 (15.6) | ||||
| Education level | Senior Secondary and below | 31(9.1) | 7(16.7) | .119 | 4(6.1) | 2(20.0) | .128 | 27(9.8) | 5(15.6) | .305 |
| Undergraduate and above | 311(90.9) | 35(83.3) | 62(93.9) | 8(80.0) | 249(90.2) | 27(84.4) | ||||
| Allergic reactions to previous vaccinations | ||||||||||
| yes | 53(15.5) | 7(16.7) | .844 | 6(9.1) | 0(0) | .320 | 47(17.0) | 7(21.9) | .495 | |
| no | 289(84.5) | 35(83.3) | 60(90.9) | 10(100) | 229(83) | 25(78.1) | ||||
| Preventive effect of COVID-19 | ||||||||||
| yes | 340 (99.4) | 40 (95.2) | .012 | 65 (98.5) | 9 (90.0) | .118 | 275 (99.6) | 31 (96.8) | .065 | |
| no | 2 (0.6) | 2 (4.8) | 1 (1.5) | 1 (10.0) | 1 (0.4) | 1 (3.2) | ||||
| Degree of knowledge on COVID-19 vaccine | ||||||||||
| high | 332 (97.1) | 38 (90.5) | .031 | 64 (97.0) | 10 (100.0) | .577 | 268 (97.1) | 28 (87.5) | .008 | |
| low | 10 (2.9) | 4 (9.5) | 2 (3.0) | 0 (0.0) | 8 (2.9) | 4 (12.5) | ||||
| Perception of safety of COVID-19 vaccine | ||||||||||
| high | 328 (95.9) | 36 (85.7) | .005 | 63 (95.5) | 8 (80.0) | .066 | 265 (99.3) | 28 (87.5) | .034 | |
| low | 14 (4.1) | 6 (14.3) | 3 (4.5) | 2 (20.0) | 11 (0.7) | 4 (12.5) | ||||
| Parents’ hesitance to receive COVID-19 vaccine themselves | ||||||||||
| yes | 218 (63.7) | 29(69.0) | .498 | 30 (45.5) | 3 (30.0) | .358 | 188 (68.1) | 26 (81.3) | .127 | |
| no | 124 (32.3) | 13(31.0) | 36 (54.5) | 7 (70.0) | 88 (31.9) | 6 (18.7) | ||||
| Willingness to get vaccinated if the vaccine is paid for | ||||||||||
| yes | 307 (89.8) | 15 (35.7) | <.001 | 60 (91.0) | 5 (50.0) | .001 | 247 (89.5) | 10 (31.3) | <.001 | |
| no | 35 (10.2) | 27 (64.3) | 6 (9.0) | 5 (50.0) | 29 (10.5) | 22 (68.7) | ||||
| Parents’ hesitance for children to receive vaccine | ||||||||||
| yes | 210 (61.4) | 36 (85.7) | .002 | 31 (47.0) | 7 (70.0) | .175 | 179 (64.9) | 29 (90.6) | .003 | |
| no | 132 (39.2) | 6 (14.3) | 35 (53.0) | 3 (30.0) | 97 (35.1) | 3 (9.4) | ||||
*p-value < .05; n (%), count (percentage). WTP = willingness to pay; RTP = Reluctant to pay.
Independent factors affecting parents’ WTP for their children’s COVID-19 vaccine were further analyzed using a binary logistic regression model. As shown in Table 3, excluding possible confounding factors and after stratification by gender, parents’ WTP for their own COVID-19 vaccination (yes or no, odds ratio [OR] = 13.77, 95% confidence interval [CI]: 6.51–29.11), parents’ hesitation to vaccinate their children (yes or no, OR = 3.50, 95% CI: 1.25–9.79), and parents’ willingness to vaccinate their children with WTP for the COVID-19 vaccine were significantly associated with the same influencing factors as for mothers. However, fathers’ WTP for their children’s vaccination was significantly associated only with their WTP for their own vaccination (yes or no, OR = 6.12, 95% CI: 1.21–31.10).
Table 3.
Independent factors affecting parents’ WTP for children’s COVID-19 vaccine after binary logistic regression model (N = 384).
| Parents |
Fathers |
Mothers |
|||||
|---|---|---|---|---|---|---|---|
| Variables | Categories | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) |
| Degree of knowledge of COVID-19 vaccine | |||||||
| High vs low | .845 | 0.87 (0.21–3.60) | / | / | .530 | 0.61 (0.13–2.85) | |
| Preventive effect of COVID-19 | |||||||
| Yes vs No | .091 | 0.15 (0.02–1.35) | / | / | .132 | 0.10 (0.00–2.04) | |
| Perception of safety of COVID-19 vaccine | |||||||
| High vs low | .717 | 0.80 (0.23–2.78) | / | / | .868 | 1.13 (0.26–4.92) | |
| willingness to get vaccinated if the vaccine is paid for | |||||||
| Yes vs No | <.001 | 13.77 (6.51–29.11) | .029 | 6.12 (1.21–31.10) | <.001 | 16.62 (6.90–40.00) | |
| Parents’ hesitancy with children to receive against COVID-19 | |||||||
| No vs Yes | .017 | 3.50 (1.25–9.79) | .171 | 3.31 (0.60–18.35) | .025 | 5.00 (1.23–20.42) | |
OR = odds ratio; CI = confidence interval.
The main reason parents were hesitant to vaccinate their children against COVID-19 was that they were concerned about the side effects of the vaccine. Second, they preferred to wait and first find out what happened to others; very few parents considered it unnecessary to vaccinate their children against COVID-19.
Discussion
Clinical implications
As COVID-19 continues to mutate and vaccine efficacy naturally decays, frequent vaccinations are required to achieve herd immunity.9 The COVID-19 vaccine may require out-of-pocket payments in the future, and assessing individuals’ WTP not only allows for the development of a payment scheme that balances costs and benefits, it also identifies potential market demand.4 Assessing the optimal WTP value depends on parental acceptance of the COVID-19 vaccine and how much they are willing to pay for the vaccine.14
We also summarized the WTP for the COVID-19 vaccine of the general population in other countries and found a large variation, ranging from 18.4% to 84.3%, with a minimum WTP of $1.15 to a maximum of $159.2 (Table 4). Among them, the WTP in Nigeria and Pakistan (ranging from 18.4% to 33.9%) is significantly lower than the WTP summarized in other countries in Africa and Asia (ranging from 56% to 84.3%).17–19,21 The factors that may influence this difference are gender, place of residence, education level, age, religious beliefs (whether the vaccine is halal or not), previous vaccination history with the COVID-19 vaccine, the perceived safety of the vaccine, perceived risk, and time of survey. In addition, income and whether someone close to them contracted COVID-19 (experience related to COVID-19) are related to WTP for vaccination.2,25-27 However, these factors were not adequately investigated and our study found that gender, place of residence, education level, and previous vaccination history did not significantly affect parents’ WTP for their children. It is necessary to further explore whether parental income and experience related to COVID-19 influence WTP.
Table 4.
The estimates of adults’ WTP for the COVID-19 vaccine in Asia and Africa.
| WTP |
|||||||
|---|---|---|---|---|---|---|---|
| Author | Study period | Sample size | Sample range | Country | Percentage | Mean/Median | Reference |
| Wang et al. | March 3–18, 2020 | 2,058 | adults | China | 84.3% | RMB 254 (US$ 36.80) | 3 |
| Harapan et al. | March 25 – April 6, 2020 | 1,359 | public | Indonesia | 78.3% | US$ 57.20 | 4 |
| Zhang et al. | March – May, 2020 | 1,179 | public | China | 81.1% | US$ 73.40–146.50 | 15 |
| Karam et al. | June – July, 2020 | 352 | public | Lebanon | 78.1% | US$ 63.70 | 16 |
| Ilesanmi et al. | September 21–25, 2020 | 232 | 15 years and older | Nigeria | 18.4% | US$ 13.16 | 17 |
| Tahir et al. | September 27 – October 11, 2020 | 883 | public | Pakistan | 33.9% | US$ 7 | 18 |
| Okafor et al. | October 18–30, 2020 | 689 | adults | Nigeria | 22.8% | US$ 1.20–2.50 | 19 |
| Kiran et al. | October – December, 2020 | 3,371 | adults | India | 68% | NA | 20 |
| Banik et al. | December 10, 2020 – January 10, 2021 | 894 | adults | Bangladesh | 72.9% | US$ 4.72 | 14 |
| Adigwe et al. | January, 2021 | 1,767 | public | Nigeria | 26% | US$ 1.15 | 21 |
| Kabir et al. | January 20–27, 2021 | 697 | adults | Bangladesh | 68.4% | US$ 7.08 | 1 |
| Xiao et al. | January 28 – February 5, 2021 | 2,450 | adults | China | 77.7% | US$ 127.60–159.20 | 22 |
| Seboka et al. | February – March, 2021 | 1,160 | public | Ethiopia | 56% | NA | 23 |
| Tung et al. | June 9–17, 2021 | 1,788 | parents | China | 66.1% | < RMB 200 (US$ 29.70) | 9 |
| Mueangpoon et al. | September 13, 2021 – January 14, 2022 | 705 | adults | Thailand | 77.2% | US$ 14.30–28.50 | 24 |
NA = Not available; relevant studies were searched in the Cochrane Library, PubMed, and EMBASE databases, from inception to August 21, 2022. The search included key concepts such as WTP and the COVID-19 vaccine. Titles and abstracts were scanned, irrelevant literature was filtered out, and duplicates were removed, resulting in 15 relevant papers.
Interestingly, we also summarized the WTP for COVID-19 vaccination of the general population in mainland China. In the four cross-sectional studies conducted in China, the surveys occurred in the first six months after the emergence of COVID-19, and the prolonged global outbreak and seriousness of the situation increased the sense of urgency and awareness of the seriousness of COVID-19 among individuals.3,15,25,28 Therefore, the WTP for the COVID-19 vaccine was also relatively high, which is consistent with two studies conducted in Chile at different times.29,30 In May 2021, the first large outbreak of COVID-19 hit Taiwan;31 although the survey period of our study was not at the time of the outbreak, a high percentage (89.1%) of parents were still happy to pay for their children’s vaccination, considering that the first large outbreak in Taiwan only happened two years after the global COVID-19 pandemic. After two years, there has been a significant increase in COVID-19 awareness and the COVID-19 vaccine in Taiwan. Previous studies show that knowledge of COVID-19 vaccines is associated with a significantly higher WTP.7,9 In the same way, two study in Malaysia showed that the more knowledgeable parents were about vaccines, the more positive their attitudes and perceptions about vaccination were.32,33
Clinical practices
In our findings, 89.1% of parents wanted to pay for their children, indicating a high level of parental acceptance of the COVID-19 vaccine for children in Taiwan, higher than that of Bangladesh (56%) and India (68%). Interestingly, among the parents who were reluctant to receive the COVID-19 vaccine, 56.5% were still happy to pay for their children. The reason for the difference in parents’ WTP for themselves and their children may be that parents in China believe that the COVID-19 vaccine is of high value in preventing COVID-19 infection. Moreover, they were more pleased to pay for their children to be immunized.
Parents’ reluctance to pay for the COVID-19 vaccine for themselves influenced their decision to pay for their children. Parents who agreed to pay for COVID-19 vaccines were mostly willing to pay for their children. However, the possibility of side effects due to the COVID-19 vaccine may also contribute to reluctance among parents who were willing to pay for their children’s vaccines. The main factor contributing to parents’ hesitation to vaccinate their children is the possible side effects of the vaccines. Previous studies have shown that hesitation about vaccines can strongly influence people’s WTP.5,8According to our findings, increasing parents’ WTP and reducing their hesitancy to vaccinate their children could help achieve full vaccination of children.
It has been shown that improved vaccination rates among children and developing herd immunity can be achieved through public pressure and private funding, as was evident for the influenza vaccine in Chile.34 The government in Chile provides an influenza vaccine free of charge to high-risk groups (children under six years of age, pregnant women, chronically ill patients, and older adults), while others must pay their own way.35 Thus, government provision of the vaccine to vulnerable groups (including low-income and severely co-morbid groups) can greatly increase vaccination rates. In addition, occasional dissemination of information about the COVID-19 vaccine can reduce parents’ hesitation to vaccinate their children and increase their WTP for their children.
Our study provides insight into parents’ WTP for COVID-19 vaccine for their children and for themselves. By increasing parents’ WTP for their own vaccinations, they further promote their WTP for their children, thereby increasing child vaccination rates.
Methodological considerations
The current study had some limitations. First, the use of an online anonymous survey may produce multiple sampling biases; we collected a sample of predominantly urban residents, households with high education levels, and stable economic resources, and the results of data analysis are not generalizable. Such sampling errors may alter the observed WTP. Second, 43% of the participants were HCWs. Given that this population has greater knowledge and acceptance of the vaccine, this may bias the study data and its results may not be fully extrapolated to the general population. Third, this was a cross-sectional study, which can only reflect the situation at a specific point in time. During the questionnaire period, the number of newly confirmed cases in Taiwan increased daily, but not during the pandemic. Our estimates were made at only one point in time, and it is uncertain how people’s attitudes changed as the epidemic changed. Furthermore, vaccines are currently available free of charge in most countries, the perception of paying for vaccines is insufficient, and the WTP survey will differ from the actual WTP.
Conclusion
Our survey results showed that a high percentage (89.1%) of parents in Taiwan were happy to pay for their children’s COVID-19 vaccine. Parents’ WTP for themselves and their hesitation to vaccinate their children are both related to their WTP. Enhancing vaccine knowledge, reducing hesitation about vaccines, and the development of vaccine payment policies have positive implications for increasing WTP for vaccines and promoting vaccination.
Funding Statement
This study was supported in part by the Medical and Health Science and Technology Project of Zhejiang Province (2020385612) and Science and Technology Administration Public Interest Technology Research Project of Zhejiang Province (LGF19H030013).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Author contributions
J.S.Z. and T.H.T. conceived the study and designed the questionnaire. J.Y.C collected the data. C.L.H. was responsible for analyzing and writing the first draft of the paper. C.L.H, C.Q.Y, and J.S.D searched, sorted, and interpreted the relevant literature. All authors edited and approved the final manuscript.
Data availability statement
The data used for this study, although not available in a public repository, will be made available to other researchers upon reasonable request.
Ethics approval and consent to participate
We did not require a separate written informed consent because of anonymity. Parental participation in the survey was treated as informed consent. This study was approved by the Ethics Committee of Taizhou Hospital of Zhejiang Province (approval number: K20210520) in China.
References
- 1.Kabir R, Mahmud I, Chowdhury MTH, Vinnakota D, Jahan SS, Siddika N, Isha SN, Nath SK, Hoque Apu E.. COVID-19 vaccination intent and willingness to pay in Bangladesh: a cross-sectional study. Vaccines (Basel). 2021. Apr 21;9(5):416. doi: 10.3390/vaccines9050416. PMID: 33919254; PMCID: PMC8143282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vo NX, Huyen Nguyen TT, Van Nguyen P, Tran QV, Vo TQ.. Using contingent valuation method to estimate adults’ willingness to pay for a future coronavirus 2019 vaccination. Value Health Reg Issues. 2021;24:240–7. doi: 10.1016/j.vhri.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang J, Lyu Y, Zhang H, Jing R, Lai X, Feng H, Knoll MD, Fang H. Willingness to pay and financing preferences for COVID-19 vaccination in China. Vaccine. 2021;39(14):1968–76. doi: 10.1016/j.vaccine.2021.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Setiawan AM, Rajamoorthy Y, Sofyan H, Vo TQ, et al. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Hum Vaccin Immunother. 2020;16:(12):3074–80. doi: 10.1080/21645515.2020.1819741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alhassan RK, Nketiah-Amponsah E, Immurana M, Abuosi AA. Financing COVID-19 vaccination in sub-Saharan Africa: lessons from a nation-wide willingness to pay (WTP) survey in Ghana. BMC Public Health. 2022;22(1):1273. Published 2022 Jun 30. doi: 10.1186/s12889-022-13602-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adhikari SP, Meng S, Wu YJ, Mao Y-P, Ye R-X, Wang Q-Z, Sun C, Sylvia S, Rozelle S, Raat H, et al., Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review, Infect Dis Poverty. 2020;9(1):29. Published 2020 Mar 17. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–14. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.García LY, Cerda AA. Authors’ reply to Sprengholz and Betsch: “Willingness to pay for a COVID-19 vaccine”. Appl Health Econ Health Policy. 2021;19(4):623–24. doi: 10.1007/s40258-021-00657-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tung TH, Lin XQ, Chen Y, Wu H, Zhang MX, Zhu JS. Why do parents willingness-to-pay to vaccinate their children against COVID-19? A real-world evidence in Taizhou, China. Hum Vaccin Immunother. 2022;18(1):1–9. doi: 10.1080/21645515.2021.2014731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Kaitelidou D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. 2022;157:106994. doi: 10.1016/j.ypmed.2022.106994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yılmaz M, Sahin MK. Parents’ willingness and attitudes concerning the COVID-19 vaccine: a cross-sectional study. Int J Clin Pract. 2021;75(9):e14364. doi: 10.1111/ijcp.14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Catma S, Reindl D. Parents’ willingness to pay for a COVID-19 vaccine for themselves and their children in the United States. Hum Vaccin Immunother. 2021 Sep 2;17(9):2919–25. doi: 10.1080/21645515.2021.1919453. Epub 2021 Apr 30. PMID: 33929290; PMCID: PMC8428178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang MX, Lin XQ, Chen Y, Tung TH, Zhu JS. Determinants of parental hesitancy to vaccinate their children against COVID-19 in China. Expert Rev Vaccines. 2021;20(10):1339–49. doi: 10.1080/14760584.2021.1967147. [DOI] [PubMed] [Google Scholar]
- 14.Banik R, Islam MS, Pranta MUR, Rahman QM, Rahman M, Pardhan S, Driscoll R, Hossain S, Sikder MT. Understanding the determinants of COVID-19 vaccination intention and willingness to pay: findings from a population-based survey in Bangladesh. BMC Infect Dis. 2021;21(1):892. Published 2021 Aug 31. doi: 10.1186/s12879-021-06406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Luo X, Ma ZF. Willingness of the general population to accept and pay for COVID-19 vaccination during the early stages of COVID-19 pandemic: a nationally representative survey in mainland China. Hum Vaccin Immunother. 2021;17(6):1622–27. doi: 10.1080/21645515.2020.1847585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karam MM, Baki JA, Al-Hajje A, Sraj M, Awada S, Salameh P, Ajrouche R. Willingness to pay for a coronavirus vaccine and its associated determinants in Lebanon. Value Health Reg Issues. 2022;30:18–25. doi: 10.1016/j.vhri.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ilesanmi O, Afolabi A, Uchendu O. The prospective COVID-19 vaccine: willingness to pay and perception of community members in Ibadan, Nigeria. PeerJ. 2021;9:e11153. Published 2021 Mar 26. doi: 10.7717/peerj.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tahir MJ, Saqlain M, Tariq W, Waheed S, Tan SHS, Nasir SI, Ullah I, Ahmed A. Population preferences and attitudes towards COVID-19 vaccination: a cross-sectional study from Pakistan. BMC Public Health. 2021;21(1):1759. Published 2021 Sep 26. doi: 10.1186/s12889-021-11814-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okafor UG, Isah A, Onuh JC, Mgbemena CB, Ubaka CM. Community acceptance and willingness to pay for hypothetical COVID-19 vaccines in a developing country: a web-based nationwide study in Nigeria. Pan Afr Med J. 2021;40:112. Published 2021 Oct 21. doi: 10.11604/pamj.2021.40.112.27780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kiran T, Junaid KP, Sharma D, Jain L, Vij J, Satapathy P, Chakrapani V, Patro BK, Kar SS, Singh R, et al. Sociodemographic determinants of willingness and extent to pay for COVID-19 vaccine in India. Front Public Health. 2022;10:870880. Published 2022 Jun 6. doi: 10.3389/fpubh.2022.870880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adigwe OP. COVID-19 vaccine hesitancy and willingness to pay: emergent factors from a cross-sectional study in Nigeria. Vaccine X. 2021. Dec;9:100112. doi: 10.1016/j.jvacx.2021.100112. Epub 2021 Sep 3. PMID: 34494000; PMCID: PMC8413098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiao J, Wu Y, Wang M, Ma Z. Scope issue in contingent valuation studies of the COVID-19 vaccine: the case of China. Appl Health Econ Health Policy. 2022;20(3):417–29. doi: 10.1007/s40258-021-00706-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seboka BT, Yehualashet DE, Belay MM, Kabthymer RH, Ali H, Hailegebreal S, Demeke AD, Amede ES, Tesfa GA. Factors influencing COVID-19 vaccination demand and intent in resource-limited settings: based on health belief model. Risk Manag Healthc Policy. 2021;14:2743–56. Published 2021 Jun 28. doi: 10.2147/RMHP.S315043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mueangpoon K, Inchan C, Kaewmuneechoke P, Rattana P, Budsratid S, Japakiya S, Ngamchaliew P, Vichitkunakorn P. Self-Reported COVID-19 vaccine hesitancy and willingness to pay: a cross-sectional survey in Thailand. Vaccines (Basel). 2022;10(4):627. Published 2022 Apr 16. doi: 10.3390/vaccines10040627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qin W, Wang E, Ni Z, Gao Z. Chinese consumers’ willingness to get a COVID-19 vaccine and willingness to pay for it. PLoS One. 2021;16(5):e0250112. Published 2021 May 4. doi: 10.1371/journal.pone.0250112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Das U, Rathore U, Pal R. On willingness to pay for Covid-19 vaccines: a case study from India. Hum Vaccin Immunother. 2021 Dec 2;17(12):4904–13. doi: 10.1080/21645515.2021.1989918. Epub 2021 Nov 10. PMID: 34757868; PMCID: PMC8903962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Echazu L, Nocetti DC. Willingness to pay for morbidity and mortality risk reductions during an epidemic. Theory and preliminary evidence from COVID-19. Geneva Risk Insur Rev. 2020;45(2):114–33. doi: 10.1057/s10713-020-00053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP, Marques ETA. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020;14(12):e0008961. Published 2020 Dec 17. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cerda AA, García LY. Willingness to pay for a COVID-19 vaccine. Appl Health Econ Health Policy. 2021;19(3):343–51. doi: 10.1007/s40258-021-00644-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Willingness to pay for a COVID-19 vaccine high in Chile. PharmacoEcon Outcomes News. 2020;858(1):35. doi: 10.1007/s40274-020-7008-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang VY. Systemic resilience and COVID-19: lessons from Taiwan. Int J Qual Health Care. 2022;34(2):mzac029. doi: 10.1093/intqhc/mzac029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ansari MT, Jamaluddin NN, Ramlan TA, Zamri N, Majeed S, Badgujar V, Sami F, Hasnain MS, Balbir Singh HK. Knowledge, attitude, perception of Muslim parents towards vaccination in Malaysia. Hum Vaccin Immunother. 2021;17(3):785–90. doi: 10.1080/21645515.2020.1800325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Balbir Singh HK, Badgujar VB, Yahaya RS, Abd Rahman S, Sami FM, Badgujar S, Govindan SN, Ansari MT. Assessment of knowledge and attitude among postnatal mothers towards childhood vaccination in Malaysia. Hum Vaccin Immunother. 2019;15(11):2544–51. doi: 10.1080/21645515.2019.1612666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Organization for Economic Co-operation and Development (OECD) . Influenza vaccination rates. [accessed 2020 Mar 30]. https://data.oecd.org/healthcare/influenza-vaccination-rates.htm.
- 35.Sprengholz P, Betsch C. Comment on: “willingness to pay for a COVID-19 vaccine. Appl Health Econ Health Policy. 2021;19(4):619–21. doi: 10.1007/s40258-021-00656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used for this study, although not available in a public repository, will be made available to other researchers upon reasonable request.


