Abstract
BACKGROUND
The COVID-19 pandemic has had wide-ranging impacts across international healthcare systems and direct impacts on rehabilitation professionals. Few outcome data for cardiac patients undergoing rehabilitation programs during the COVID-19 pandemic are available.
AIM
We conducted a study to compare the effect of modified rehabilitation therapies mainly performed in wards versus conventional therapies mainly performed in rehabilitation units in which exercise on a treadmill and cardiopulmonary exercise testing were available.
DESIGN
Observational study.
SETTING
University hospital.
POPULATION
Fifty-five consecutive inpatients admitted to a university hospital and underwent a cardiac rehabilitation program from August 2019 to June 2020.
METHODS
The patients were divided into two groups: those admitted during the COVID-19 outbreak (Group A, N.=28) and those admitted before the COVID-19 outbreak (Group B, N.=27). The evaluation included age, sex, duration of the rehabilitation intervention program, days before initiation of the rehabilitation program, functional status, and Functional Independence Measure (FIM) Score.
RESULTS
A higher proportion of patients in Group A than B underwent a cardiac rehabilitation program provided in wards (88.5% vs. 48.8%, respectively). Group A showed a significantly lower 6-minute walking distance and walking speed than Group B at discharge (P=0.031 and 0.014, respectively). Group A showed a significantly shorter exercise time using an ergometer than Group B (P=0.028).
CONCLUSIONS
The difference in the cardiac rehabilitation location during the COVID-19 pandemic may affect the rehabilitation contents and lead to less improvement in physical function.
CLINICAL REHABILITATION IMPACT
A cardiac rehabilitation program was performed mainly in wards instead of in rehabilitation units during the COVID-19 pandemic. Walking abilities were adversely affected by the modified cardiac rehabilitation program.
Key words: Rehabilitation, Exercise, Heart failure
The COVID-19 pandemic has had wide-ranging impacts across international healthcare systems and direct impacts on rehabilitation professionals. Most patients with disabilities, regardless of COVID-19 infection, suffer because of restrictions imposed on rehabilitation service delivery. The COVID-19 outbreak is having a profound impact on cardiac rehabilitation organization and provision of cardiac rehabilitation programs, and this impact will likely continue for a long period of time.1 Regular rehabilitation has been disrupted by quarantine requirements, social isolation, and movement restriction. Efforts are urgently needed to avoid minimizing patients’ activity while simultaneously avoiding the spread of infection in the COVID-19 pandemic. Thus, partially modified rehabilitation approaches that differ from conventional therapies have been under development in regions strongly affected by the COVID-19 pandemic.2-6 However, the lack of available high-quality comparative studies regarding modified rehabilitation approaches is problematic. In emergency situations under the COVID-19 pandemic, implementation of cardiac rehabilitation programs mainly in wards instead of in rehabilitation units may be an alternative strategy; this may help to avoid the “three Cs”—crowded places, close-contact settings, and confined and enclosed spaces.7 To the best of our knowledge, no outcome data for cardiac patients undergoing rehabilitation programs during the COVID-19 pandemic have been reported. In this study, we compared the effect of modified rehabilitation therapy mainly performed in wards versus conventional therapies mainly performed in rehabilitation units in which exercise on a treadmill and cardiopulmonary exercise testing were available.
Materials and methods
Patients
This retrospective, observational, single-center registry study involved consecutive patients who were admitted to the Department of Cardiology, Fujita Health University Bantane Hospital and underwent a cardiac rehabilitation program from August 2019 to June 2020. Patients were excluded if they could not walk 10 m independently, had acute coronary syndrome, had severe dementia, had a history of psychiatric disorders, and/or did not wish to participate. After applying the exclusion criteria, 55 patients were enrolled in the study. The Research Ethics Committee of Fujita Health University approved the study (Approval No: CI20-748), informed consent was obtained using the opt-out method approved by the Committee.
Study design and protocol
The enrolled patients were divided into two groups: those admitted during the COVID-19 outbreak (Group A, March 2020-June 2020) and those admitted before the COVID-19 outbreak (Group B, August 2019-February 2020) (Figure 1).
Figure 1.
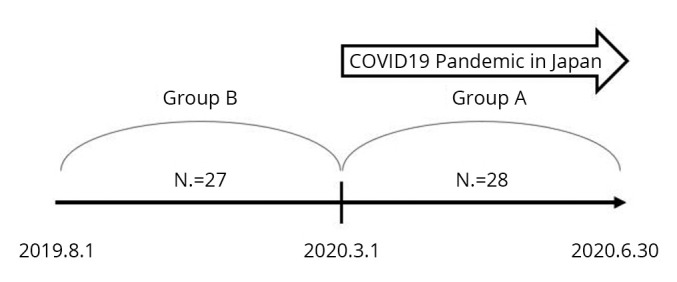
—Patients flow for group classification. Group A: During the COVID-19 outbreak (March 2020–June 2020), Group B: Before the COVID-19 outbreak (August 2019–February 2020).
None of the patients enrolled in this study had COVID-19. The patients’ diagnosis requiring hospitalization, age, sex, and systolic blood pressure were registered at admission. Their body mass index was registered at discharge. We obtained each patient’s geriatric nutritional risk index, serum hemoglobin concentration, serum albumin concentration, serum sodium concentration, N-terminal pro B-type natriuretic peptide concentration, and estimated glomerular filtration rate from the results of a blood investigation. Echocardiography was also performed to obtain the left ventricular ejection fraction at admission. Physical function was assessed at discharge using the 6-minute walking distance (6MWD), grip strength, waist circumference, isometric knee extensor muscle strength (KEMS), walking speed, and functional reach test. Cognitive function and mental function were assessed with the Mini-Mental State Examination and five-item Geriatric Depression Scale, respectively. We evaluated the functional independence measure (FIM)8 as an index of activities of daily living (ADL) at admission and at discharge. FIM gain (FIM Score at discharge minus FIM Score at admission), which is commonly used to assess the degree of improvement, was also evaluated.
Finally, we evaluated the contents and duration of the rehabilitation program, including assessment, range of motion exercise, sitting up exercise, sitting exercise, standing exercise, walking exercise, ergometer exercise, resistance training, ADL training, and other parameters as recorded in the medical records.
Parameter measurements
The 6MWD was conducted in accordance with the guidelines of the American Thoracic Society.9 Grip strength was measured using a digital grip strength dynamometer (T.K.K.5401; Takei Scientific Instruments, Niigata, Japan). The patient exerted maximum effort twice with the left and right hands with the upper limb lowered parallel to the trunk in the sitting position, and the highest value was used for the analysis. KEMS was measured using a digital handheld dynamometer (m-Tas F1; Anima, Tokyo, Japan). During testing, the patients adopted a sitting position with the arms held on the edge of the table and were fitted with the handheld dynamometer on the anterior aspect of the lower extremity just proximal to the malleoli, which was fixed to the table leg by a vinyl strap. The patients were asked to extend their legs and push twice on the left and right, and the highest value was used for the analysis. KEMS was transformed into Newtons adjusted by weight (N/kg). Walking speed was measured by the usual 10-m walk test; the patients were requested to walk at their usual pace for 14 m, the middle 10 m of which was timed. The test was completed twice, and the speed in the faster trial was used for analysis. Functional reach was measured as the length of the shortened rod after reaching forward as far as possible using the expandable rod.10
COVID-19 preventive measures
The difference in rehabilitation programs during and before the COVID-19 outbreak are shown in Table I. Patients in Group B underwent rehabilitation in the ward until their general condition became stable; they later performed exercise therapy at the rehabilitation center if they could walk steadily. However, to avoid the “three Cs,” exercise therapy in Group A was provided in a medical ward as a rule.
Table I. —Differences in rehabilitation programs during and before COVID-19 outbreak.
| Under COVID-19 outbreak (Group A) |
Before COVID-19 outbreak (Group B) |
|
|---|---|---|
| Rehabilitation place | In a medical ward | In a rehabilitation center (590 m2) as long as the general condition is stable and the patient can walk steadily |
| Ergometer exercise | Not performed | Performed as needed |
COVID-19: Coronavirus disease 2019.
Statistical analysis
The data are presented as median (interquartile range) for continuous variables and as percentages for categorical data. In the comparisons of the two groups, categorical variables were analyzed using the chi-square test and continuous variables were analyzed using the Mann-Whitney U Test. All analyses were performed with the SPSS 25.0 software package (SPSS Inc., Tokyo, Japan), and a P-value of <0.05 was considered statistically significant.
Results
This study involved 24 men and 31 women (mean age, 79.6±12.6 years). Group A and B comprised 28 and 27 patients, respectively. Table II shows a comparison of the patients’ characteristics between Groups A and B.
Table II. —Demographic and clinical characteristics of patients during and before COVID-19 outbreak.
| Under COVID-19 outbreak (Group A) (N.=28) | Before COVID-19 outbreak (Group B) (N.=27) | P | |
|---|---|---|---|
| Age | 83.0 (75.8-90.8) | 79.0 (71.0-87.0) | 0.363 |
| Gender (male/female) | 9/19 | 15/12 | 0.080 |
| Days before the initiation of rehabilitation program | 2.0 (2.0-3.0) | 2.0 (2.0-3.0) | 0.696 |
| Hypertension | 13 (46.4%) | 16 (59.3%) | 0.341 |
| Old myocardial infarction | 3 (10.7%) | 1 (3.7%) | 0.317 |
| Diabetes mellitus | 11 (39.3%) | 7 (25.9%) | 0.291 |
| Stroke | 5 (17.9%) | 1 (3.7%) | 0.092 |
| Cancer | 3 (10.7%) | 6 (22.2%) | 0.249 |
| Dyslipidemia | 11 (39.3%) | 7 (25.9%) | 0.291 |
| Length of hospitalization (days) | 15.0 (12.0-26.3) | 20.0 (16.0-31.0) | 0.076 |
| Rehabilitation duration per week (minutes) | 461.8 (414.8-547.6) | 442.1 (285.5-503.0) | 0.083 |
| Place (ward/rehabilitation center) | 564/73 (88.5/11.5) | 319/335 (48.8/51.2) | <0.001 |
| MMSE | 25.0 (23.0-28.0) | 26.0 (23.0-29.0) | 0.385 |
| SBP at admission (mmHg) | 142.0 (117.0-175.0) | 127.0 (115.0-157.0) | 0.235 |
| GNRI | 98.7 (80.3-101.2) | 94.2 (78.9-107.5) | 0.643 |
| Serum hemoglobin (g/dL) | 11.4 (9.9-13.3) | 11.8 (10.4-14.8) | 0.474 |
| Serum albumin (g/dL) | 3.6 (3.3-3.9) | 3.6 (3.0-4.1) | 0.972 |
| Serum sodium (mEq/L) | 139.5 (135.0-142.5) | 139.0 (136.0-142.0) | 0.447 |
| eGFR | 49.8 (38.3-60.5) | 43.6 (30.7-66.4) | 0.414 |
| NT-proBNP (pg/mL) | 3388.0 (1032.5-8349.0) | 4386.0 (1577.3-9336.3) | 0.598 |
| LVEF (%) | 57.6 (48.7-63.4) | 54.0 (36.4-63.0) | 0.360 |
| Grip strength (kg) | 15.2 (11.0-19.5) | 17.5 (11.9-28.5) | 0.195 |
| Waist circumference (cm) | 79.6 (70.0-87.2) | 79.4 (72.3-91.5) | 0.539 |
| KEMS (N/kg) | 3.2 (2.2-4.4) | 3.5 (2.9-4.0) | 0.309 |
| 6MWD (m) | 210.0 (122.5-285.0) | 290.0 (193.0-382.0) | 0.031 |
| Walking speed (m/s) | 0.7 (0.5 – 0.9) | 0.9 (0.7 – 1.1) | 0.014 |
| FRT(cm) | 25.0 (20.0-31.9) | 29.0 (19.8-32.5) | 0.388 |
| FIM Score at admission total | 107.0 (73.3-115.5) | 96.0 (60.0-114.0) | 0.572 |
| Motor | 72.0 (43.8-80.5) | 61.0 (32.0-79.0) | 0.704 |
| Cognitive | 35.0 (26.0-35.0) | 35.0 (30.0-35.0) | 0.458 |
| FIM Score at discharge total | 114.0 (85.3-125.8) | 120.0 (104.0-126.0) | 0.329 |
| Motor | 80.5 (61.8-90.8) | 85.0 (74.0-91.0) | 0.320 |
| Cognitive | 35.0 (29.0-35.0) | 35.0 (35.0-35.0) | 0.233 |
| FIM gain total | 4.0 (0-17.0) | 16.0 (0-32.0) | 0.078 |
| Motor | 4.0 (0-17.0) | 16.0 (0-32.0) | 0.107 |
| Cognitive | 0 (0-0) | 0 (0-0) | 0.663 |
Data are presented as median (interquartile range), N., or N. (%). COVID-19: Coronavirus disease 2019; MMSE: Mini-Mental State Examination; SBP: systolic blood pressure; GNRI: geriatric nutritional risk index; eGFR: estimated glomerular filtration rate; NT-proBNP: N-terminal pro-brain natriuretic peptide; LVEF: left ventricular ejection fraction; KEMS: knee extensor muscle strength; 6MWD: 6-minute walking distance; FRT: functional reach test; FIM: functional independence measure.
A higher proportion of patients in Group A than B underwent a cardiac rehabilitation program provided in wards (88.5% vs. 48.8%, respectively). Group A showed a significantly lower 6MWD and walking speed than Group B at discharge (6MWD: P=0.031, walking speed: P=0.014). Total FIM gain was likely to be higher in Group B than A (P=0.078). However, there was no significant difference in The Body Mass Index, blood parameters, left ventricular ejection fraction, or FIM score between the two groups.
Table III shows a comparison of treatment times for each cardiac rehabilitation program. Group A showed a significantly shorter exercise time using an ergometer than Group B (P=0.028). There was no significant difference in other exercise times between the groups.
Table III. —Duration (minutes) of rehabilitation program during hospitalization.
| Under COVID-19 (Group A) (N.=28) |
Before COVID-19 (Group B) (N.=27) |
P | |
|---|---|---|---|
| Assessment | 205 (181.3-250.0) | 215 (145.0-265.0) | 0.860 |
| Range of motion exercise | 20.0 (0-97.5) | 30.0 (0-75.0) | 0.946 |
| Sitting up exercise | 0 (0-0) | 0 (0-0) | 0.972 |
| Sitting exercise | 0 (0-28.8) | 0 (0-15.0) | 0.984 |
| Standing exercise | 5 (0-52.5) | 0 (0-35.0) | 0.738 |
| Walking exercise | 140.0 (61.3-287.5) | 160.0 (65.0-245.0) | 0.827 |
| Ergometer exercise | 0 (0-0) | 10.0 (0-90.0) | 0.028 |
| Resistance training | 127.5 (55.0-303.8) | 220.0 (100.0-445.0) | 0.316 |
| ADL training | 0 (0-21.3) | 0 (0-20.0) | 0.538 |
| Others | 5.0 (0-30.0) | 10.0 (0-35.0) | 0.813 |
| Total | 640.0 (425.0-1150.0) | 900.0 (560.0-1200.0) | 0.337 |
Data are presented as median (interquartile range). COVID-19: Coronavirus disease 2019; ADL: activities of daily living.
Discussion
As the number of patients with both confirmed and suspected COVID-19 increases, overwhelmed medical systems are becoming a social problem because both human and medical resources have become limited. In May 2020, the Japanese Association of Rehabilitation Medicine published a statement to support management of rehabilitation during the COVID-19 pandemic (https://www.jarm.or.jp/topics/member/7676.html). Strict curbs in daily life cannot continue for a long period of time, but new lifestyles should be explored with respect to social and economic activities during the COVID-19 pandemic. Typically, it is important to avoid the “three Cs”—confined spaces, crowded places, and close contact. In rehabilitation therapy, avoidance of the three Cs among patients and therapists is also necessary. Degeneration of rehabilitation might occur if such trade-off is implemented. In contrast, continuous support is more useful for patients. Therefore, we modified our rehabilitation program from conventional therapy during the COVID-19 pandemic; i.e., the cardiac rehabilitation program was performed mainly in wards instead of in rehabilitation units for patients who had not been diagnosed with COVID-19. Additionally, cardiopulmonary exercise testing, which is considered an aerosol-generating procedure,11 was performed only in patients with high need during the pandemic. We hypothesized that some functional outcomes are adversely affected by the modified rehabilitation program performed mainly in the wards after the COVID-19 pandemic. The present study demonstrated that cardiac rehabilitation provided in the ward might reduce physical function at discharge if the rehabilitation location had been changed during the outbreak (Group A). Thus, an important finding of this study was that physical function (6MWD and walking speed) was better when exercise therapy was performed in the cardiac rehabilitation center than in the ward.
In general, rehabilitation in a unit is considered better than that in wards because we can use many tools such as parallel bars or machines in a wider space. However, to the best of our knowledge, no reports have compared cardiac rehabilitation performed mainly in wards with that performed mainly in rehabilitation units. Group A underwent cardiac rehabilitation program in wards, and their physical function at discharge (6MWD and walking speed) was low. There was no difference in the quality of resistance training between the two groups; however, the low amount of aerobic exercise using equipment such as ergometers might have had less effect on improving physical function in Group A.
Patients with heart disease who have low 6MWD and walking speed reportedly have a poor prognosis in terms of death and readmission.12 Considering the prognosis, exercise therapy in the ward should be devised to maintain the same quality as performed in the rehabilitation center. In general, exercise intensity tailored to individual exercise capacity should be used for optimal exercise prescriptions that are safe and efficacious. It should be useful to unify the setting of exercise load according to the Karvonen coefficient and rating of perceived exertion (Borg scale) in a ward without exercise equipment. Further investigations are needed in this regard.
There is a certain need to deliver as much cardiac rehabilitation as possible under the given circumstances of the ongoing COVID-19 pandemic.13, 14 Alternative person-tailored, remotely guided, home-based programs may be suboptimal choices for preventing disuse syndrome and maintaining or improving ADL.
Limitations of the study
Some limitations of this study should be discussed. First, this was a single-center study with a small number of participating patients. Second, the generalizability of the study results is limited because of the different circumstances surrounding the healthcare systems between Japan and other countries. Third, we had no data on the patients’ baseline physical function. Therefore, we could not compare the changes in physical function during hospitalization in both groups. Finally, we had no data on the patients’ prognosis because of the short survey period. A recent study suggested that patients with a slow walking speed are at high risk for severe COVID-19 and mortality.15 The patients enrolled in this study were not positive for COVID-19; further investigations are needed for COVID-19-positive patients undergoing cardiac rehabilitation.
Conclusions
The present study suggests that the difference in the cardiac rehabilitation location during the COVID-19 pandemic may affect the rehabilitation contents and the patient’s physical function at discharge. As of April 2021, there were concerns about the re-spread of infection. To avoid the three Cs, rehabilitation programs in wards may be needed for some time. From this point of view, our findings seem of significance.
References
- 1.Vigorito C, Faggiano P, Mureddu GF. COVID-19 pandemic: what consequences for cardiac rehabilitation? Monaldi Arch Chest Dis 2020;90. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32297490&dopt=Abstract 10.4081/monaldi.2020.1315 [DOI] [PubMed]
- 2.Aoyagi Y, Ohashi M, Funahashi R, Otaka Y, Saitoh E. Oropharyngeal Dysphagia and Aspiration Pneumonia Following Coronavirus Disease 2019: A Case Report. Dysphagia 2020;35:545–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32533346&dopt=Abstract 10.1007/s00455-020-10140-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aoyagi Y, Inamoto Y, Shibata S, Kagaya H, Otaka Y, Saitoh E. Clinical manifestation, evaluation, and eehabilitative strategy of dysphagia associated with COVID-19. Am J Phys Med Rehabil 2021;100:424–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33657028&dopt=Abstract 10.1097/PHM.0000000000001735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mukaino M, Tatemoto T, Kumazawa N, Tanabe S, Kato M, Saitoh E, et al. Staying active in isolation: telerehabilitation for individuals with the SARS-CoV-2 infection. Am J Phys Med Rehabil 2020;99:478–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32282339&dopt=Abstract 10.1097/PHM.0000000000001441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spielmanns M, Pekacka-Egli AM, Cecon M, Witassek F, Schoendorf S, Lutz D, et al. COVID-19 Outbreak During Inpatient Rehabilitation: Impact on Settings and Clinical Course of Neuromusculoskeletal Rehabilitation Patients. Am J Phys Med Rehabil 2021;100:203–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33443857&dopt=Abstract 10.1097/PHM.0000000000001686 [DOI] [PubMed] [Google Scholar]
- 6.Van Iterson EH, Laffin LJ, Crawford M, Mc Mahan D, Cho L, Khot U. Cardiac Rehabilitation Is Essential in the COVID-19 Era: delivering uninterrupted heart care based on the Cleveland clinic experience. J Cardiopulm Rehabil Prev 2021;41:88–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33591062&dopt=Abstract 10.1097/HCR.0000000000000585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Avoid the Three Cs [Internet]. Available from: https://www.who.int/brunei/news/infographics [cited 2021, Mar 5]
- 8.Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD. Performance profiles of the functional independence measure. Am J Phys Med Rehabil 1993;72:84–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=8476548&dopt=Abstract 10.1097/00002060-199304000-00005 [DOI] [PubMed] [Google Scholar]
- 9.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories . ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12091180&dopt=Abstract 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 10.Morio Y, Omori Y, Izawa K, Tanaka A, Watanabe S, Beppu M, et al. The development of Functional Reach Test using the telescoping rod. Sogo Rehabilitation 2007;35:487–93. [Japanese] [Google Scholar]
- 11.Faghy MA, Sylvester KP, Cooper BG, Hull JH. Cardiopulmonary exercise testing in the COVID-19 endemic phase. Br J Anaesth 2020;125:447–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32571569&dopt=Abstract 10.1016/j.bja.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tanaka S, Kamiya K, Hamazaki N, Matsuzawa R, Nozaki K, Nakamura T, et al. Short-Term Change in Gait Speed and Clinical Outcomes in Older Patients With Acute Heart Failure. Circ J 2019;83:1860–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31281168&dopt=Abstract 10.1253/circj.CJ-19-0136 [DOI] [PubMed] [Google Scholar]
- 13.Cardiology ESo. Recommendations on how to provide cardiac rehabilitation activities during the COVID-19 pandemic 2020 [Internet]. Available from: https://www.escardio.org/Education/Practice-Tools/CVD-prevention-toolbox/recommendations-on-how-to-provide-cardiac-rehabilitation-activities-during-the-c [cited 2020, Sep 5].
- 14.Ambrosetti M, Abreu A, Cornelissen V, Hansen D, Iliou MC, Kemps H, et al. Delphi consensus recommendations on how to provide cardiovascular rehabilitation in the COVID-19 era. Eur J Prev Cardiol 2021;28:541–57. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33624042&dopt=Abstract 10.1093/eurjpc/zwaa080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yates T, Razieh C, Zaccardi F, Rowlands AV, Seidu S, Davies MJ, et al. Obesity, walking pace and risk of severe COVID-19 and mortality: analysis of UK Biobank. Int J Obes 2021;45:1155–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33637952&dopt=Abstract 10.1038/s41366-021-00771-z [DOI] [PMC free article] [PubMed] [Google Scholar]


