Abstract
BACKGROUND
Hip and knee strengthening exercises are implemented in rehabilitation of patellofemoral pain patients, but typically use high loads (70% of 1 repetition maximum). This may lead to increased patellofemoral joint stress. Low load training (20-30% of 1 repetition maximum) with blood flow restriction could allow for exercise strength benefits to proximal and distal muscles with reduced joint stress and by promoting hypoalgesia.
AIM
The aim of this study was to compare hip and knee focused exercises with and without blood flow restriction in adults with patellofemoral pain for short term effectiveness.
DESIGN
A randomized observed-blind controlled trial.
SETTING
Musculoskeletal laboratories of the European University Cyprus, Nicosia, Cyprus.
POPULATION
60 volunteer patients, 18-40 years of age with patellofemoral pain.
METHODS
Participants were randomly assigned to (1 reference group) hip and knee strengthening at (70% of 1 repetition maximum) or (2 experimental group) Strengthening with blood flow restriction at (30% of 1 repetition maximum at 70% of limb occlution pressure). Treatments took place 3 times per week for 4weeks and outcomes were assessed at baseline, end of treatment and at 2-month follow-up. The primary outcome was the Kujala Anterior Knee Pain Scale and secondary outcomes were worst and usual pain, pain with Single leg Squats, the maximum pain free flexion angle, the Tampa Scale of kinesiophobia, the Pain Catastrophizing Scale and isometric strength of knee extensors, hip extensors and hip abductors.
RESULTS
No difference were found for the main outcome of this study between groups. There was a significant effect of time for all outcome measures in both groups. Between group differences showed a significant difference for isometric strength of Knee extensor values at 2 month follow-up F(1,58)=5.56, P=0.02, partial η2=0.09, 459.4 (412.13, 506.64) vs. 380.68 (333.42, 427.93) and in worst pain post-treatment F(1,58)=5.27, P=0.02, partial η2=0.08, 0.76 (0.48, 1.04) vs. reference group 1.30 (0.91, 1.68) with significantly better scores in the blood flow restriction group.
CONCLUSIONS
Blood flow restriction exercises of the hip and knee musculature used in this study were as effective as usual exercises of Hip and knee musculature in reducing symptoms in the short term. They also indicated greater increases in strength and reduction of worst pain post-treatment.
CLINICAL REHABILITATION IMPACT
Further research is needed to investigate the dose response relationship with longer follow-ups.
Key words: Patellofemoral pain syndrome, Exercise, Rehabilitation
Patellofemoral pain is one of the most common musculoskeletal knee joint problems in young adults.1 It is defined as peri or retro patellar pain aggravated by at least one of the following activities that increase stress on the patellofemoral joint (squatting, running, jumping, kneeling, stair ascent/descent and prolonged sitting).2
According to the 2018 consensus statement,3 on patellofemoral pain, exercise is considered to be the treatment of choice. Exercises consist mainly of quadriceps strengthening and in recent years strengthening the hip muscles in combination have been proved appropriate.3 Exercises use relatively high loads (70% of one repetition maximum)4-10 and can increase patellofemoral joint stress, potentially aggravating patients symptoms. This may lead therapists to reduce the exercise load in order to avoid pain during exercise and thus loads may not be sufficient for increasing strenght.11
Blood flow restriction training is a method of exercise where the limbs blood flow is restricted by a pneumatic cuff reducing arterial blood flow and venous return. This technique forces the musculature to exercise in an oxygen deprived environment leading to early fatigue.12 While exercising with low loads of 20-30% of one repetition maximum, muscle hypertrophy is promoted,13, 14 not only muscles distal to the cuff but proximal muscles above the cuff as well.15 It is thought that these changes occur due to a greater accumulation of metabolites as a result of increased production and the prolonged stasis from blood pooling.16 It has been shown that it could possibly induce hypoalgesia in patients with anterior knee pain17, 18 although mechanisms are still unclear. It seems that blood flow restriction training could facilitate patellofemoral pain rehabilitation, by allowing exercise benefits with reduced joint stress, possibly with faster increases in strength and by promoting hypoalgesia. However, only one study has been conducted on patellofemoral pain patients but it did not include hip exercises.19
The purpose of this study was to compare hip and knee focused exercises with and without blood flow restriction training in adults with patellofemoral pain.
Materials and methods
This was an observer blinded randomized trial with the first primary end point at 4 weeks (end of treatment) and final endpoint at 2-month follow-up which took place between November 2019 and February 2020. Ethical approval was granted by the European University Cyprus of Cyprus as part of the main authors PhD thesis and by the Cyprus National Bioethics Committee, ΕΕΒΚ/ΕΠ/2019/86. The study was registered after completion at ClinicalTrials.gov data base NCT04340453. It was designed and reported in accordance with the CONSORT (Consolidated Standards of Reporting Trials) guidelines for reporting of randomized controlled trials20 (Figure 1). All assessments and treatments took place at the European University Cyprus.
Figure 1.
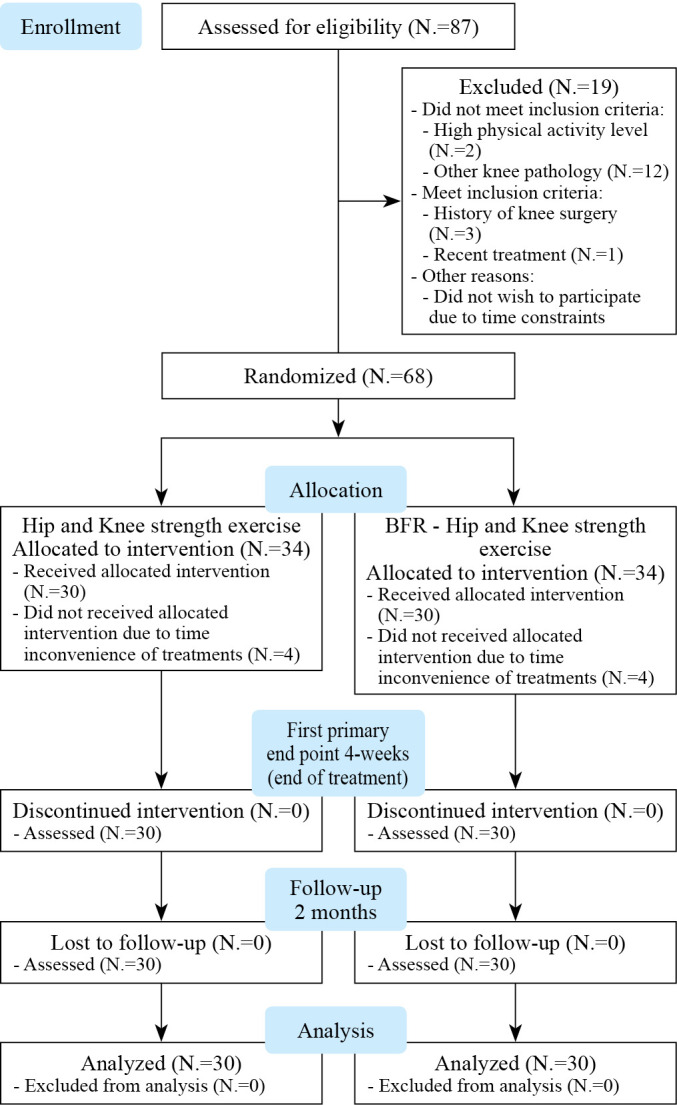
—CONSORT Diagram of patient flow through the study.
Sample size was determined through power analysis using the GPower 3.0.10 software. The minimal clinical significant difference of the main outcome measure (Kujala Anterior Knee Pain Scale) was used for the estimation. For a minimal clinical significant difference of 10 points21 with an estimated standard deviation of 13.5 points22 and 0.80 power with level of significance a=0.05 and considering a two tailed t-test, sample size was calculated to be 60 participants. By estimating a possible 20% drop out we concluded to a sample size of 75. To include an equal number of participants in the two groups we concluded to 38 participants per group.
Participants volunteered for inclusion after being informed of the study by printed posters at the European University Cyprus campus and local social media. Screening was carried out by an orthopedic surgeon to determine eligibility at the University’s musculoskeletal laboratory. All participants signed consent forms. Assessment involved patient history and clinical examination based on the inclusion and exclusion criteria are listed below.
Patellofemoral pain patients who voluntarily agreed to participate in this study were included for screening. The following inclusion criteria were used: either male or female, between 18-40 years of age with at least a 4 week23 history of peri or retro-patella non traumatic pain (≥3 cm Visual Analogue Scale [VAS]). Pain had to be reproduced by at least two of the following functional tasks: squatting, kneeling, prolonged sitting, stair ascending or descending, hopping or running.2 In addition, during physical examination pain had to be present with either palpation of the patella facets or with the patella compression test. For volunteers with bilateral symptoms the limb with the worst pain was used for analysis.
Participants were excluded if they were athletes or had a high level of physical activity based on assessment of the International Physical Activity Questionnaire in Greek.24 Other exclusion criteria included history or current meniscus ligament or other knee injury and/or surgery. Other knee pathology such as knee osteoarthritis, Osgood-Schlatter or Sinding-Larsen-Johanssen Syndrome or tendinopathy of muscles surrounding the knee.25 Knee instability, feeling of “giving way,” history of subluxation or dislocation of the knee joint or joint edema. Extended use (≥3 months) of nonsteroidal anti-inflammatory drugs or corticosteroids. Referred pain from lumbar spine or another region. Patella dysplasia, rheumatoid arthritis or neurological syndromes or diseases.2, 10 Pain located on the patella tendon eliminated with isometric contraction, the pes anserinus, the iliotibial band, or with a positive medial or lateral patella apprehension test.26 Previous treatment in the past 6 months. Unexplained chest pains, cardiovascular disease, renal disease, vascular surgery or disease, high risk or history of deep venous thrombosis, resent surgery ≤6 months, high blood pressure (≥140/90 mmHg), dizzy spells, history of fainting or dizziness with exercise, pregnancy and any contraindication to exercise.19
Randomization was carried out using a block sequence of 4, generated at https://www.sealedenvelope.com27 by an external statistician and assigned participants into one of two treatment groups; group 1 ‘hip and knee exercise’ (reference group) and group 2 ‘blood flow restriction, hip and κnee exercise’ (experimental group).
Outcomes assessor was blinded to patient allocation. Physiotherapists providing treatment were blind to the other groups treatment. Data analysis and writing of the manuscript were performed blinded until consensus about the interpretation was reached. Patient blinding was impossible.
Group 1 (reference group) followed hip and knee strengthening exercises with a combination of stretching, 3 times a week for 4 weeks to a total of 12-, 45-minute sessions. Therapy sessions were in group form and supervised. Exercises focused on strengthening the hip extensors, abductors and external rotators, as well as, the quadriceps and hamstrings in both open and closed kinetic chain. Open kinetic chain exercises were executed first followed by closed kinetic chain exercises. Exercises with ankle weights or mechanical resistance were set at a load of 70% of one repetition maximum and 3 sets of 10 repetitions. Elastic resistance exercises were based on participants 10 repetitions maximum for 3 sets. The time under tension and tempo of the exercises was set at 1:2 (concentric/eccentric) at 60 bpm with auditory cue, by the Metronome application installed on a Smartphone. Rest between sets was 30 seconds and 2 minutes between exercises (Table I).
Table I. —Treatment protocols performed in the study.
| Parameters (dose) | |
|---|---|
| Group 1 (hip and knee exercise program) | |
| Hip abduction with ankle weights (side-lying)* | 3 sets of 10 rep |
| Hip extension (machine)* | 70% of 1RM (1:2) con/ecc |
| Hip abduction against elastic band (standing)† | 30sec rest / sets |
| Hip external rotation against elastic band (sitting)† | 2min rest / exersices |
| Seated knee extension (90-45°) (sitting)* | 3 sets of 10 rep at 10RM (1:2) con/ecc |
| Prone knee flexion* | 30sec rest / set |
| Squatting (0-45°)* | 2min rest / exercise |
| Single leg press (0-45°) (machine)* | |
| Group 2 (BFR - Hip and Knee Exercise Program) | |
| Hip extension (machine)** | 1st set 30 reps followed by 3 sets of 15 reps |
| Hip abduction (machine)** | 30% of 1RM (2:2) con/ecc |
| Seated single knee extension (machine)**(90-45°) | 70% LOP |
| Single Leg press (0-45°) (machine)** | 30sec rest / sets |
| 2min rest / exersices | |
| Cointervention assisted, passive, static stretching | |
| Hamstrings and plantar flexors | 3 rep. of 30sec |
| Quadriceps | |
| Iliotibial band |
Rep: repetitions; RM: repetition maximum; sec: seconds; con: concentric; ecc: eccentric; LOP: limb occlusion pressure. *3 sets of 10 rep; **1st set 30 reps followed by 3 sets of 15 reps; †3 sets of 10 rep at 10RM (1:2) con/ecc.
Group 2 (experimental group) followed a hip and knee strengthening exercise program using blood flow restriction with a combination of stretching, 3 times a week for 4 weeks to a total of 12,1 hour, sessions. Therapy sessions were in group form and supervised. Sports Rehab Tourniquet© cuffs were used, with a width of 10cm and a length of 116 cm or 84 cm depending on the diameter of the participants thigh. The length of the cuff had to be adequate to wrap around the upper third of the participants thigh and the edges of the cuff had been overlapping with no gap between them. Exercises focused on strengthening the hip extensors and abductors, as well as the quadriceps both in open and closed kinetic chain. Open kinetic chain exercises involving the hip musculature were executed first followed by quadriceps strengthening and closed kinetic chain exercises. Mechanical resistance was used at a load of 30% of one repetition maximum with a limb occlusion pressure of 70%. Four sets were carried out for each exercise. The first set consisted of 30 repetitions and the next 3 sets of 15 repetitions. Time under tension and tempo of the exercises was set at 2:2 (concentric/eccentric) at 60bpm with auditory cue, by the Metronome app installed on a Smartphone. Rest between sets was 30 seconds and 2 minutes between exercises. The cuff stayed inflated during the 30 second rest but was deflated during the 2-minute resting period between exercises (Table I).
Exercise progression was individualized for both groups with weekly repetition maximum testing. Assessments were performed at the beginning of each week. Pain with exercise was not permitted. No modification of exercise was needed for any of the participants. Both groups received passive stretching (3 x 30 second stretches for each muscle group) by the groups physiotherapist. Stretching involved the hamstrings, plantar flexors, quadriceps and iliotibial band.4, 5 Besides stretching no other cointerventions were allowed. No home-based exercises were given and participants were not allowed to exercise for the duration of the treatments nor the end of treatment up to the follow-up period (Table I).
To estimate the 1 repetition maximum, the 5-repetition maximum test was chosen,28 as this test uses less resistance and thought to be more tolerable for patient population. Tests were conducted by the physiotherapist of each group. Muscle testing included: single leg press 0-60o, leg extension 90-45o, hip abduction and extension using Technogym® equipment for mechanical resistance and using ankle weights. The 5-repetition maximum was estimated within 3 to 5 trials. The 10-repetition maximum test was used to estimate level of elastic resistance with the use of TheraBand Professional Non-Latex Resistance Bands. Pain was allowed during testing at a level of ≤2/10 on a numeric pain rating scale. These testing procedures are within the guidelines of the National Strength and Conditioning Association.28
Participants limb occlusion pressure for blood flow restriction training was estimated by the groups physiotherapist, at the beginning of each session, for all exercise positions; standing, sitting and semi seated. It was estimated daily to ensure accurate measurements as occlusion pressure changes based on body position and the circadian cycle.29 Measurements were assessed before each session in the following way: The participant was placed in standing position with the cuff (deflated) on the most proximal third of the thigh. The participant would rest for three minutes before assessment commenced. By using a Edan SD3 Vascular Doppler W/8MHZ the arterial pulse was located. Then, the cuff was inflated steadily in increments of approximately 10mmHg until the auditory signal was completely lost. This pressure was recorded as the limb occlusion pressure. Measurements were repeated in the seated and finally in the semi-seated position.30 Exercises were executed using the same pneumatic cuff that was used for limb occlusion assessment.
All outcome measures were assessed by one assessor on three occasions (Baseline, 4 weeks end of treatment and 2-month follow-up). Baseline assessment included clinical characteristics, somatometric and demographic characteristics, as well as baseline level of all outcome measures.
The study outcome measures were as follows: the Greek version of the Kujala Anterior Knee Pain Scale,31 worst pain and usual pain using the visual analogue scale, pain with single leg squat tests (deep and shallow), the decline step down test, the Tampa Scale of kinesiophobia, the pain catastrophizing scale and maximum isometric voluntary contraction strength of knee extensors, hip extensors and hip abductors using hand held dynamometry. The Kujala Anterior Knee Pain Scale32 has a maximum score of 100 (no pain/disability/limitation) and a minimum 0 (worst possible function). This questionnaire has been previously used in patellofemoral pain studies and was found to be valid and reliable.21 The validated Greek version was used.31 The visual analogue scale measuring worst and usual pain are valid and reliable.21 Two depths of squatting (deep and shallow) were used to assess pain with the visual analogue scale with each squat. This testing method has been previously used to assess pain in anterior knee pain patients.17, 18 The Decline Step Down Test33 was used to measure the maximum pain free flexion angle of the knee joint. The test has been found to be reliable with intraobserver reliability ICC=0.83 and inter-observer reliability ICC=0.85.33 The angle was measured whilst patients descended from a 20-cm high step with a surface inclination of 20o, using the Dr. Goniometer application, installed on an Iphone 6S. The Tampa Scale of kinesiophobia was originally constructed by Kori et al.34 Kinesiophobia was assessed using the Greek Version of the Tampa Scale of kinesiophobia that has been found to be valid and reliable.35 This scale consists of 17 items that assess fear of injury due to movement on a four-point Likert Scale, (1 [strongly disagree] to 4 [strongly agree]). Responses were summed after reversing the scores of items 4, 8, 12 and 16. The Pain Catastrophizing Scale assesses the cognitive process by which pain is seen as Fan extreme threat and from which the patient suffers exaggerated negative consequences.36 The questionnaire consists of 13 items (statements) describing pain experience and participants were asked to indicate their level of agreement regarding these statements on a five-point scale, rating from 0 (not at all) to 4 (always). The Pain Catastrophizing Scale measures three subcategories: rumination, magnification and helplessness. Rumination refers to the patients’ inability to apart the pain from their mind, magnification expresses the exaggerated cognitions of pain as a threat, and hopelessness is the estimation that the patient cannot do anything to influence pain.36 The Greek version was used that has been found to be valid and reliable. Strength was assessed by measuring maximum isometric voluntary contraction with the use of a MicroFET2™ hand-held dynamometer. The quadriceps was measured at ≈60o of knee flexion from the seated position with the dynamometer placed on the anterior aspect of the tibia, 5 cm above the lateral malleolus. Hip extensors were assessed from the prone position with the dynamometer placed on the posterior aspect of the tibia, 5 cm above the lateral malleolus and hip abductors were assessed in the side-lying position with the hip abducted to ≈10o with the dynamometer placed laterally, 5 cm above the lateral malleolus. Testing began with 2-3 sub-maximal contractions for familiarization and warm-up followed by a maximal isometric contraction for 5 seconds with standard verbal encouragement. The participant rested for 30 second and the test was repeated. If the two measures differed less than 10% then no other testing was carried out. If measures had a difference greater than 10%, then the tests were repeated until the above criteria was met.17 The mean of the two valid measures was used for analysis.
Statistical analysis
Statistical analysis was performed by the studies assessor, using the IBM SPSS “Statistical Package for the Social Sciences” (SPSS, Version 20.0). Numeric, normally distributed data was presented as mean and standard deviation and non-normally distributed data was presented as median and interquartile range. A normality was assessed using the One Sample Kolmogorov-Smirnov Test (P<0.05). For differences between groups, the chi-squared test was used to test categorical variables. The Independent-samples t-test for normally distributed numerical variables and the Mann-Whitney U-Test for variables with non-normal distribution. In order to estimate differences between the two groups the mixed methods two-way ANOVA Test was used with “time” as the within-subjects factor and “treatment” as the between subjects factor. Outliers were assessed using the Studentized Residual value ±3 and normality of distribution by analyzing the Studentized Residual values on a Q-Q plot. No outliers were excluded from the analysis due to genuinely unusual values and they did not significantly influence results. Homogeneity of variance was checked with the Levene Test <0.05 and covariances with Box’s Test P>0.001. Sphericity was assessed with Mauchly’s Test P>0.05. If the assumption of sphericity was violated a Greenhouse-Geisser correction was applied. In cases of a significant group time interaction a General linear model Univariate analysis for assessing differences between groups at the different time points was conducted and a General linear model Repeated measures analysis for assessing differences within groups (4 weeks - baseline, 2-month follow-up - baseline and 2-month follow-up - 4weeks). Results are presented as, F values, P values and partial η2. Interpretation of partial η2: 0.01= small effect, 0.06= moderate effect, 0.14= large effect.37
Results
We examined 87 patients for eligibility to the study: 18 were excluded as they did not meet inclusion criteria or met exclusion criteria as well as 1 patient who did not want to participate due to time constraints; 68 patients were randomized into the two groups but a total of 8 participants did not receive the allocated intervention due to time inconvenience of treatments. Finally, 30 participants received treatment for each group and completed at least 10 out of the 12 sessions. this was monitored and reported by the groups physiotherapist at the end of the 4 week sessions. No participants were lost to follow-up and all participants were analyzed at all assessments (Figure 1). No differences were found between groups for age, gender, height, weight, ΒΜΙ, symptom duration, involved limb or level of physical activity P>0.05 (Table II). No adverse effects were reported or observed during or at the end of the study. Patients did not report use of pain medication during the study.
Table II. —Baseline somatometric, demographic characteristics and differences between groups.
| Group 1 (N.=30) | Group 2 (N.=30) | P value | |
|---|---|---|---|
| Age (yrs) | 30.5(16) [18-40] | 25.5(14) [18-40] | P=0.122 |
| Height (m) | 1.7(0.13) [1.5-1.8] | 1.7(0.1) [1.6-1.8] | P=0.496 |
| Weight (kg) | 72.4 (±16.9) [48-115] | 72.5 (±11.1) [49-95] | P=0.971 |
| ΒΜΙ (kg/m2) | 24.7 (±4.3) [18.4-36.7] | 24.6 (±3) [18.6-32.8] | P=0.879 |
| Pain duration (months) | 11(17) [3-48] | 14(16) [3-36] | P=0.169 |
| Gender N. (%) | P>0.999 | ||
| Male | 16 (53) | 17 (57) | |
| Female | 14 (47) | 13 (43) | |
| Limb/s with pain N. (%) | P=0.266 | ||
| Right | 16 (53) | 7 (23.3) | |
| Left | 6 (20) | 10 (33.3) | |
| Bilateral | 8 (27) | 13 (43.3) | |
| Involved limb N. (%) | P=0.067 | ||
| Right | 9 (30) | 13 (43) | |
| Left | 21 (70) | 17 (57) | |
| IPAQ, N. (%) | P>0.999 | ||
| Low | 9 (30) | 10 (33) | |
| Moderate | 21 (70) | 20 (67) |
Data are presented as: mean ±SD [min-max] or median (IQR) [min-max] unless otherwise indicated.
Regarding the main outcome there was no statistically significant interaction between interventions and time on the Kujala Anterior Knee Pain Scale values F(1,79)=27.10, P=0.39, partial η2=0.14, worst pain values F(2,98)=1.09, P=0.33, partial η2=0.02, usual pain values F(2,89)=0.20, P=0.76, partial η2=0.004, pain with shallow single leg squat F(2,88)=0.20, P=0.76, partial η2=0.003 or pain with deep pain single leg squat F(2,102)=0.74, P=0.46, partial η2=0.01. There was a statistically significant interaction between interventions and time on the maximum pain free flexion angle values F(2,102)=3.71, P=0.03, partial η2=0.06. Between group differences showed that there was a statistically significant difference in maximum pain free flexion angles between groups at Baseline F(1,58)=4.59, P=0.04, partial η2=0.07. Measures were statistically significantly greater in the blood flow restriction group 67.6 (65.56, 69.64) compared to the reference group 64.5 (62.36, 66.64) with a mean difference of -3.1 (-5.99, -0.2). Mean differences between groups were not statistically significant post-treatment 0.34 (-2.52, 3.19) P>0.05 nor at 2-month follow-up 1.34 (-1.01, 3.70) P>0.05 (Supplementary Digital Material 1: Supplementary Table I).
The main effects of time showed a statistically significant difference at different time points for the means of Kujala Anterior Knee Pain Scale values F(1,79)=496.63, P<0.001, partial η2=0.89, Worst pain values F(2,98)=895.32, P<0.001, partial η2=0.94, Usual pain values F(2,89)=834.74, P<0.001, partial η2=0.93, pain with shallow single leg squat values F(2,88)=1135.70, P<0.001, partial η2=0.95. Pain with deep single leg squat values F(2,102)=795.61, P<0.001, partial η2=0.93 and maximum pain free flexion angle values F(2,102)=751.17, P<0.001, partial η2=0.93 for both groups but no differences were found for the effect of group. When assessing between group differences there was a statistically significant difference in worst pain scores post treatment F(1,58)=5.27, P=0.02, partial η2=0.08. Measures were statistically significantly lower in the blood flow restriction group 0.76 (0.48, 1.04) compared to the hip and knee group 1.30 (0.91, 1.68) with a mean difference of 0.54 (0.07, 1.00) P=0.02 post treatment. There were no differences at Baseline F(1,58)=0.95, P=0.33, partial η2=0.02 or at 2-month follow-up F(1,58)=2.91, P=0.09, partial η2=0.05 (Supplementary Table I).
There was no statistically significant interaction between interventions and time for kinesiophobia F(1,77)=2.72, P=0.09, partial η2=0.04 or catastrophizing F(1,68)=55.71, P=0.09, partial η2=0.05. There was no statistically significant interaction between interventions and time for Magnification scores F(1,76)=0.32, P=0.63, partial η2=0.01 or Hopelessness values F(1,67)=0.97, P=0.34, partial η2=0.02. There was a statistically significant interaction for Rumination values F(1,91)=7.38, P=0.002, partial η2=0.11. Between group differences for Rumination showed a statistically significant difference in means at baseline F(1,58)=8.17 P=0.006 η2=0.12 but no statistically significant difference in means was observed at post-treatment or 2-month follow-up (Supplementary Digital Material 1: Supplementary Table II).
The main effects of time showed a statistically significant difference in means of kinesiophobia scores F(1,77)=76.77, P<0.001, partial η2=0.81, Catastrophizing scores F(1,68)=293.08, P<0.001, partial η2=0.83 and for subscales, Rumination F(1,91)=288.03, P<0.001, partial η2=0.83, Magnification F(1,76)=159.22, P<0.001, partial η2=0.73 and Hopelessness F(1,67)=162.07, P<0.001, partial η2=0.74 at the different time points for both groups. No differences were observed for the effect of group for any values (Supplementary Table II).
No statistically significant interaction between interventions and time was observed for maximum isometric contraction hip extensor values F(2,101)=0.24, P=0.76, partial η2=0.004 or hip abductor values F(2,116)=0.34, P=0.71, partial η2=0.006. There was a statistically significant interaction between interventions and time for the knee extensor values F(1,81)=4.69, P=0.02, partial η2=0.07. Assessment of between groups differences for Knee extensor values showed no differences at Baseline F(1,58)=1.58, P=0.21, partial η2=0.03 or at 4 weeks post treatment F(1,58)=2.89, P=0.09, partial η2=0.05. There was a statistically significant difference at 2-month follow-up F(1,58)=5.56, P=0.02, partial η2=0.09 and values were significantly greater in the blood flow restriction group 459.4 (412.13, 506.64) compared to the reference group 380.68 (333.42, 427.93) with a mean difference of 78.7 (11.88, 145.54) P=0.02 (Table III).
Table III. —Group scores, between and within group differences for MVIC strength values.
| Secondary outcomes | Baseline | End of treatment 4 weeks | Follow-up 2 months | 4 weeks - baseline | 2 months - baseline | 2 months - 4 weeks |
|---|---|---|---|---|---|---|
| MVIC Knee ext.a, b | ||||||
| Group 1 (N.=30) | 229.1 (212.6, 245.69) |
312.6 (336.69, 424.66) |
380.7 (333.42, 427.93) |
136.1 (103.20, 168.99)* |
151.5 (108.37, 194.70)* |
15.4 (-5.53, 36.45) |
| Group 2 (N.=30) | 249.6 (220.66, 278.61) |
412.9 (367.20, 458.72) |
459.4 (412.13, 506.64) |
163.3 (126.42, 200.23)* |
209.7 (167.84, 251.66)* |
46.4 (23.84, 69.01)* |
| Between groups dif. | 20.4 (-12.16, 53.15) |
47.7 (-8.45, 103.90) |
78.7 (11.88, 145.54)* |
|||
| MVIC Hip ext a, b | ||||||
| Group 1 (N.=30) | 171.9 (151.7, 195.04) |
204.9 (187.04, 222.83) |
211.1 (191.94, 230.17) |
32.9 (22.35, 43.61)* |
39.1 (27.35, 50.84)* |
6.1 (-1.37, 13.61) |
| Group 2 (N.=30) | 215.3 (192.22, 235.56) |
252.2 (234.33, 270.13) |
254.1 (234.95, 273.18) |
36.9 (25.27, 48.58)* |
38.7 (29.27, 48.25)* |
1.8 (-6.34, 10.01) |
| Between groups dif. | -43.3 (-71.99, -14.69)* |
-47.3 (-72.61, -21.98)* |
-43.0 (-70.04, -15.98)* |
|||
| MVIC Hip abd a, b | ||||||
| Group 1 (N.=30) | 114.6 (104.79, 124.52) |
133.4 (121.11, 145.71) |
134.9 (123.88, 146.02) |
18.7 (11.50, 26.01)* |
20.3 (13.39, 27.19)* |
1.5 (-4.76, 7.84) |
| Group 2 (N.=30) | 124.9 (113.44, 136.49) |
147.3 (137.36, 157.35) |
148.7 (137.87, 159.69) |
22.3 (13.91, 30,87)* |
23.8 (15.65, 31.99)* |
1.4 (-4.47, 7.33) |
| Between groups dif. | -10.3 (-25.16, 4.54) |
-13.9 (-29.46, 1.56) |
-13.8 (-29.04, 1.38) |
|||
Values are presented as mean (95% CI). MPFFA: Maximum Pain Free Flexion Angle. aHigh values indicate greater strength; bvalues are in Newtons; *P<0.05.
The main effects of time showed a statistically significant difference in means of all strength measures at the different time points. For knee extensors F(1,81)=206.21, P<0.001, partial η2=0.78, hip extensors F(2,101)=76.77, P<0.001, partial η2=0.57 and Hip abductors F(2,116)=48.69, P<0.001, partial η2=0.46 (Table III).
The main effect of intervention showed no statistically significant difference in strength for Hip abductor or Knee extensors even though Knee extensor values were close to statistical significance F(1,58)=811.49, P=0.051, partial η2=0.78. There was a statistically significant difference in means of Hip extensor values F(1,58)=11.92, P=0.001, partial η2=0.17. From assessing differences between groups for Hip extensor values at the different time points, differences were statistically significantly greater in the blood flow restriction group at Baseline F(1,58)=9.17, P<0.05, partial η2=0.14, at 4 weeks post-treatment F(1,58)=13.99, P<0.001, partial η2=0.19 and at 2-month follow-up F(1,58)=10.15, P<0.05, partial η2=0.15 (Table III).
Discussion
This study compared hip and knee focused exercises versus hip and knee focused exercises with the use of blood flow restriction training in adults with patellofemoral pain. Results showed that both interventions were successful in reducing symptoms and increasing maximal isometric contraction strength. Differences between groups were evident for maximum pain free flexion angle, worst pain, Rumination and maximum voluntary isometric contraction strength for knee and hip extensor strength measures. The only true differences were found for worst pain at post-treatment and for the Knee extensor strength.
The interaction between interventions and time on the maximum pain free flexion angle was statistically significant. However, when assessing between group differences, results showed that values were lower in the reference group at baseline, thus indicating they had a larger window of improvement which could be the reason for this result since both groups where similar at end of treatment and the 2-month follow-up.
There was no significant interaction or effect for worst pain. When assessing differences at the different time points it was evident that a statistically significant greater reduction existed for the Blood flow restriction group post-treatment. The effect was not statistically significant possibly because both groups had minimal to no pain at 2-month follow-up and no difference occurred between them at that point. Nevertheless, greater pain reduction could also be appointed to the use of blood flow restriction. It has been shown that low load blood flow restriction training at 80% limb occlusion pressure could have a hypoalgesic effect on anterior knee pain patients and it has been hypothesized that this might be due to: 1) conditioned pain modulation through the diffuse noxious conditioning controls effect; 2) exercise related release of endogenous substances which inhibit nociceptive pathways; and 3) induced hypoxia17, 38 but these mechanisms have not yet been investigated. There may also be a blood flow restriction dose response effect related to pain reduction. In another study in patellofemoral pain patients, assessing the effectiveness of blood flow restriction strengthening (30% 1 repetition maximum, 1 set of 30 and 3 sets of 15 repetitions, at 60% limb occlusion pressure) compared to usual strengthening, no between group differences were found for worst pain values.19 From a dose response view point, their study used a lower percent of limb occlusion pressure (60%) for exercise compared to the present study (70%) and others (80%) that have noticed differences in pain values.17, 18 It could be that higher limb occlusion pressure might have some effect on hypoalgesia and if so, possibly due to a greater release or accumulation of endogenous substances which inhibit the nociceptive pathways. Another explanation might be the time under tension with Blood flow restriction. An increase of time under tension also translates to a longer time with the muscles under a “hypoxic” like state, that could lead to the accumulation of substances and a longer exposure to them. In the present study, as well as the studies by Korakakis et al.,17, 18 time under tension was similar with a tempo of 2:2 and 4 sets of 30/15/15/15 repetitions. But tempo used in the study by Giles et al.19 is not stated. Additionally, the present study treatment involved both strengthening of hip and knee musculature in contrast to the study by Giles et al.19 It has been shown that strengthening of both hip and knee musculature have better outcomes4, 5 than just knee focused exercises.3 Regardless, mechanisms are unclear and future research should address these issues.
Strength measures for knee extensors, hip extensors and hip abductors showed improvement in both groups of this study as indicated by the effect of time. The interaction of interventions and time was statistically significant only for the knee extensors. Between groups, differences for the knee extensors showed that values were statistically significantly greater in the blood flow restriction group compared to the reference group at 2-month follow-up. The main effect of intervention was close to statistical significance F(1,58)=811.49, P=0.051, partial η2=0.78. The main effect of intervention was statistically significant only for Hip extensor values but from assessing differences between groups values were statistically significantly greater at all the different time points for the blood flow restriction group so the results might not indicate a true effect of treatment. The results of this study seem to be different than those of the study by Giles et al.19 They had found no statistically significant differences for knee extensor strength when comparing low level blood flow restriction to usual strengthening after 8 weeks of treatment and at 6 months follow-up but they had found that patients with higher levels of pain with knee extension had greater increases in strength with blood flow restriction. In the present study, no subgroup analysis was made as it was not previously planned and thought to be unnecessary since pain was not allowed with exercise. Moreover, it is possible that the higher limb occlusion pressure (70%) used in the present study might be related to this difference. It could be that exercising with a greater occlusion pressure >60% may be needed to observe greater changes in muscle strength. Higher occlusion pressures (80%) have been correlated to proximal muscle strength changes even on the contra-lateral side.15 This is though due to the fact that lower pressures cause less blood pooling and result in less metabolic stress to the muscles especially when occlusion is intermittent and not continuous.39 Future studies could focus on this dose response relationship. It must also be pointed out that strength comparisons in the present study could not be made between involved limb and the contra lateral due to the fact that patients with bilateral symptoms were included.
Results of the present study showed similar improvements of kinesiophobia and catastrophizing in both treatment groups. This finding strengthens the result of true function and pain improvement of the participants.40 The only statistically significant interaction found was for the Pain Catastrophizing subscale Rumination. This finding could be explained by the fact that groups were not similar regarding Rumination at baseline with the reference group having higher scores than the Blood Flow Restriction group. No other differences were observed post-treatment or at 2-month follow-up.
Limitations of the study
This study is not without limitations. A placebo group was not used in this study and comparison to placebo blood flow restriction was not possible. Exercises where not matched in the two groups due to the increased time it would take to implement the reference group exercises with the use of blood flow restriction and this could raise the risk of adverse effects.34 Results of this study cannot be generalized to other Patellofemoral pain populations such as adolescents, ages over 40 years, patients with patellofemoral instability, patients with a high level of physical activity or athletes. Finally, studies with longer follow-ups are needed as it is unknown if effects would carry on for a longer period of time as this study only observed short term effects at 2 months.
Conclusions
Intermittent low level Blood Flow Restriction strengthening of the hip and knee musculature as used in this study seems to be as effective as usual high level strength exercises of the hip and knee musculature with the combination of stretching for increasing function, reducing levels of usual pain, kinesiophobia and catastrophizing. There is an indication that blood flow restriction may have a greater effect on reducing levels of worst pain in the short term and have provide greater increases in knee extensor strength than usual exercise. More studies are needed to investigate these effects in relation to dose response, mechanisms of action, other populations and longer follow-ups.
Supplementary Digital Material 1
Supplementary Table I
Group scores, Between and within group differences for Function and Pain outcome measures#.
Supplementary Digital Material 2
Supplementary Table II
Group scores, Between and within group differences for Kinesiophobia and Catastrophizing#.
References
- 1.Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, et al. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One 2018;13:e0190892. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29324820&dopt=Abstract 10.1371/journal.pone.0190892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crossley KM, Stefanik JJ, Selfe J, Collins NJ, Davis IS, Powers CM, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med 2016;50:839–43. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27343241&dopt=Abstract 10.1136/bjsports-2016-096384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collins NJ, Barton CJ, van Middelkoop M, Callaghan MJ, Rathleff MS, Vicenzino BT, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med 2018;52:1170–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29925502&dopt=Abstract 10.1136/bjsports-2018-099397 [DOI] [PubMed] [Google Scholar]
- 4.Fukuda TY, Melo WP, Zaffalon BM, Rossetto FM, Magalhães E, Bryk FF, et al. Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up. J Orthop Sports Phys Ther 2012;42:823–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22951491&dopt=Abstract 10.2519/jospt.2012.4184 [DOI] [PubMed] [Google Scholar]
- 5.Fukuda TY, Rossetto FM, Magalhães E, Bryk FF, Lucareli PR, de Almeida Aparecida Carvalho N. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther 2010;40:736–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21041965&dopt=Abstract 10.2519/jospt.2010.3246 [DOI] [PubMed] [Google Scholar]
- 6.Khayambashi K, Mohammadkhani Z, Ghaznavi K, Lyle MA, Powers CM. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. J Orthop Sports Phys Ther 2012;42:22–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22027216&dopt=Abstract 10.2519/jospt.2012.3704 [DOI] [PubMed] [Google Scholar]
- 7.Khayambashi K, Fallah A, Movahedi A, Bagwell J, Powers C. Posterolateral hip muscle strengthening versus quadriceps strengthening for patellofemoral pain: a comparative control trial. Arch Phys Med Rehabil 2014;95:900–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24440362&dopt=Abstract 10.1016/j.apmr.2013.12.022 [DOI] [PubMed] [Google Scholar]
- 8.Ferber R, Bolgla L, Earl-Boehm JE, Emery C, Hamstra-Wright K. Strengthening of the hip and core versus knee muscles for the treatment of patellofemoral pain: a multicenter randomized controlled trial. J Athl Train 2015;50:366–77. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25365133&dopt=Abstract 10.4085/1062-6050-49.3.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bolgla LA, Earl-Boehm J, Emery C, Hamstra-Wright K, Ferber R. Pain, Function, and Strength Outcomes for Males and Females With Patellofemoral Pain Who Participate in Either a Hip/Core- or Knee-Based Rehabilitation Program. Int J Sports Phys Ther 2016;11:926–35. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27904794&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 10.Baldon R M, Serrão FV, Scattone Silva R, Piva SR. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: a randomized clinical trial. J Orthop Sports Phys Ther 2014;44:240–51, A1–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24568258&dopt=Abstract 10.2519/jospt.2014.4940 [DOI] [PubMed]
- 11.American College of Sports Medicine . American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc 2009;41:687–708. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19204579&dopt=Abstract 10.1249/MSS.0b013e3181915670 [DOI] [PubMed] [Google Scholar]
- 12.Loenneke JP, Wilson GJ, Wilson JM. A mechanistic approach to blood flow occlusion. Int J Sports Med 2010;31:1–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19885776&dopt=Abstract 10.1055/s-0029-1239499 [DOI] [PubMed] [Google Scholar]
- 13.Fahs CA, Loenneke JP, Thiebaud RS, Rossow LM, Kim D, Abe T, et al. Muscular adaptations to fatiguing exercise with and without blood flow restriction. Clin Physiol Funct Imaging 2015;35:167–76. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24612120&dopt=Abstract 10.1111/cpf.12141 [DOI] [PubMed] [Google Scholar]
- 14.Ladlow P, Coppack RJ, Dharm-Datta S, Conway D, Sellon E, Patterson SD, et al. Low-load resistance training with blood flow restriction improves clinical outcomes in musculoskeletal rehabilitation: A single-blind randomized controlled trial. Front Physiol 2018;9:1269. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30246795&dopt=Abstract 10.3389/fphys.2018.01269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bowman EN, Elshaar R, Milligan H, Jue G, Mohr K, Brown P, et al. Proximal, Distal, and Contralateral Effects of Blood Flow Restriction Training on the Lower Extremities: A Randomized Controlled Trial. Sports Health 2019;11:149–56. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30638439&dopt=Abstract 10.1177/1941738118821929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scott BR, Loenneke JP, Slattery KM, Dascombe BJ. Exercise with blood flow restriction: an updated evidence-based approach for enhanced muscular development. Sports Med 2015;45:313–25. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25430600&dopt=Abstract 10.1007/s40279-014-0288-1 [DOI] [PubMed] [Google Scholar]
- 17.Korakakis V, Whiteley R, Epameinontidis K. Blood Flow Restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Phys Ther Sport 2018;32:235–43. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29879638&dopt=Abstract 10.1016/j.ptsp.2018.05.021 [DOI] [PubMed] [Google Scholar]
- 18.Korakakis V, Whiteley R, Giakas G. Low load resistance training with blood flow restriction decreases anterior knee pain more than resistance training alone. A pilot randomised controlled trial. Phys Ther Sport 2018;34:121–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30268966&dopt=Abstract 10.1016/j.ptsp.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 19.Giles L, Webster KE, McClelland J, Cook JL. Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. Br J Sports Med 2017;51:1688–94. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28500081&dopt=Abstract 10.1136/bjsports-2016-096329 [DOI] [PubMed] [Google Scholar]
- 20.Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20332509&dopt=Abstract 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil 2004;85:815–22. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15129407&dopt=Abstract 10.1016/S0003-9993(03)00613-0 [DOI] [PubMed] [Google Scholar]
- 22.Hott A, Liavaag S, Juel NG, Brox JI. Study protocol: a randomised controlled trial comparing the long term effects of isolated hip strengthening, quadriceps-based training and free physical activity for patellofemoral pain syndrome (anterior knee pain). BMC Musculoskelet Disord 2015;16:40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25879452&dopt=Abstract 10.1186/s12891-015-0493-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox A, Ferber R, Saunders N, Osis S, Bonacci J. Gait Kinematics in Individuals with Acute and Chronic Patellofemoral Pain. Med Sci Sports Exerc 2018;50:502–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29077638&dopt=Abstract 10.1249/MSS.0000000000001465 [DOI] [PubMed] [Google Scholar]
- 24.Papathanasiou G, Georgoudis G, Papandreou M, Spyropoulos P, Georgakopoulos D, Kalfakakou V, et al. Reliability measures of the short International Physical Activity Questionnaire (IPAQ) in Greek young adults. Hellenic J Cardiol 2009;50:283–94. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19622498&dopt=Abstract [PubMed] [Google Scholar]
- 25.Waryasz GR, McDermott AY. Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dyn Med 2008;7:9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18582383&dopt=Abstract 10.1186/1476-5918-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manske RC, Davies GJ. Examination of the Patellofemoral Joint. Int J Sports Phys Ther 2016;11:831–53. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27904788&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 27.Sealed Envelope Ltd. 2019. Create a blocked randomisation list; 2019 [Internet] Available from: https://www.sealedenvelope.com/simple-randomiser/v1/lists [cited 2022, Jan 10].
- 28.Haff G, Triplett T. Essentials of Strength Training and Conditioning. Fourth edition. Champaign, IL: Human Kinetics; 2016. [Google Scholar]
- 29.Hughes L, Jeffries O, Waldron M, Rosenblatt B, Gissane C, Paton B, et al. Influence and reliability of lower-limb arterial occlusion pressure at different body positions. PeerJ 2018;6:e4697. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29736337&dopt=Abstract 10.7717/peerj.4697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Papadopoulos C, Constantinou A, Cheimonidou AZ, Stasinopoulos D. Greek cultural adaption and validation of the Kujala anterior knee pain scale in patients with patellofemoral pain syndrome. Disabil Rehabil 2017;39:704–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27049481&dopt=Abstract 10.3109/09638288.2016.1161834 [DOI] [PubMed] [Google Scholar]
- 31.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy 1993;9:159–63. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=8461073&dopt=Abstract https://doi.org/ 10.1016/S0749-8063(05)80366-4 [DOI] [PubMed] [Google Scholar]
- 32.Ophey MJ, Bosch K, Khalfallah FZ, Wijnands AM, van den Berg RB, Bernards NT, et al. The decline step-down test measuring the maximum pain-free flexion angle: A reliable and valid performance test in patients with patellofemoral pain. Phys Ther Sport 2019;36:43–50. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30641448&dopt=Abstract https://doi.org/ 10.1016/j.ptsp.2018.12.007 [DOI] [PubMed] [Google Scholar]
- 33.Georgoúdis G, Katsoulákis K, Kanéllou V. Gnosiakí Axiológisi tou Chroníou Myoskeletikoú Pónou: I períptosi tou fóvou tou asthenoús gia travmatismó í epanatravmatismó. Thémata Fysikotherapeías 2005;3:57–66. Greek. [Google Scholar]
- 34.Kori SH, Miller RP, Todd DD. Kinesophobia: A new view of chroni pain behaviour. Pain Manage 1990;35–43. [Google Scholar]
- 35.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and Validation. Psychological Assessment 1995;7:524–32. 10.1037/1040-3590.7.4.524 [DOI] [Google Scholar]
- 36.Maffiuletti NA. Assessment of hip and knee muscle function in orthopaedic practice and research. J Bone Joint Surg Am 2010;92:220–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20048117&dopt=Abstract 10.2106/JBJS.I.00305 [DOI] [PubMed] [Google Scholar]
- 37.Laerd Statistics. Two-way mixed ANOVA using SPSS Statistics. Statistical tutorials and software guides; 2015 [Internet]. Retrieved from https://statistics.laerd.com [cited 2022, Jan 10].
- 38.Patterson SD, Hughes L, Warmington S, et al. Blood Flow Restriction Exercise Position Stand: Considerations of Methodology, Application, and Safety. Front Physiol 2019;10:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maclachlan LR, Collins NJ, Matthews ML, Hodges PW, Vicenzino B. The psychological features of patellofemoral pain: a systematic review. Br J Sports Med 2017;51:732–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28320733&dopt=Abstract 10.1136/bjsports-2016-096705 [DOI] [PubMed] [Google Scholar]
- 40.Bond CW, Hackney KJ, Brown SL, Noonan BC. Blood flow restriction resistance exercise as a rehabilitation modality following orthopaedic surgery: A review of venous thromboembolism risk. J Orthop Sports Phys Ther 2019;49:17–27. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30208794&dopt=Abstract 10.2519/jospt.2019.8375 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table I
Group scores, Between and within group differences for Function and Pain outcome measures#.
Supplementary Table II
Group scores, Between and within group differences for Kinesiophobia and Catastrophizing#.


