Abstract
BACKGROUND
Extracorporeal shock-wave therapy (ESWT) is highly recommended for the management of orthopedic shoulder pathologies. Yet, the clinical relevance of the dose difference effect of radial ESWT approaches in the management of frozen shoulder patients with type 2 diabetes mellitus remains uncertain.
AIM
The aim was to examine the short-term effects of medium-and high-energy levels of radial ESWT (rESWT) in the treatment of frozen shoulder patients with type 2 diabetes mellitus.
DESIGN
Prospective clinical pilot study.
SETTING
This study was conducted in an outpatient clinic.
POPULATION
Thirty-nine patients who had frozen shoulder untreated for at least 3 months, diagnosed with type 2 diabetes mellitus for ≥3 years were included.
METHODS
The patients were randomly allocated to receive either high-energy rESWT (hrESWT), or medium-energy rESWT (mrESWT) or placebo at 8 Hz twice a week for six weeks. The primary outcome measure was pain, evaluated by the Visual Analog Scale (VAS) Score. Secondary outcome measures were function evaluated by the Shoulder Pain and Disability Index (SPADI) Score, and shoulder active range of motion (AROM). The mechanical properties of the deltoid and trapezius muscles were assessed using the MyotonPRO (Myoton AS, Tallinn, Estonia).
RESULTS
The mrESWT resulted in statistically significant reductions in night pain at 6 weeks (ηp2=0.27, P=0.003). Significantly improved function (SPADI scores: -35.42±21.29 vs.-29.59±22.60; ηp2=0.39, P˂0.001) was found in both hrESWT and mrESWT group by 6 weeks. Significantly higher mean shoulder AROM values were recorded for external rotation (ηp2=0.53, P<0.001), and internal rotation (ηp2=0.21, P=0.020), in the hrESWT group at the 6th week. A significantly improved resting tone (ηp2=0.58) and stiffness of deltoid muscle (ηp2=0.62) were found in the mrESWT group (P<0.001). The trapezius muscle resting tone reduced with hrESWT (ηp2=0.17, P=0.033).
CONCLUSIONS
Regardless of the energy levels, rESWT appears to be an effective therapeutic intervention for frozen shoulder patients with type 2 diabetes mellitus in the short-term results.
CLINICAL REHABILITATION IMPACT
Our results suggest that this rESWT can be a useful strategy for the rehabilitation of frozen shoulder patients with type 2 diabetes mellitus. This is the first study on dose difference effectiveness in terms of the clinical significance of rESWT which is key to transfer research evidence into practice.
Key words: Diabetes mellitus, Muscle tonus, Pain
Idiopathic (primary) frozen shoulder, is a painful clinical condition which is characterized by stiffness, loss of joint motion, and painful restrictions in movements of the shoulder manifested by functional disability.1, 2 The pathophysiological mechanisms behind the accumulation of the dense collagen matrix2, 3 and the proliferation of fibroblasts on the shoulder are still unclear.2-4 The risk factors of frozen shoulder include female sex, thyroid disease, hypercholesterolemia, and diabetes.5 Among risk factors, type 2 diabetes is suggested to be the main factor for the development of frozen shoulder.6 The incidence of frozen shoulder is five times higher (prevalence of 30%) among patients with diabetes compared to individuals without the condition.7 Frozen shoulder limits the individual’s functionality, while coexisting type 2 diabetes may increase the pain severity of these patients.1
Extracorporeal shock-wave therapy (ESWT) is an effective method to stimulate tissue healing.8, 9 ESWT is an integrative, noninvasive treatment in which the high-amplitude sound waves are focused on the desired part of the body.10 It is used in the treatment of various disease of musculoskeletal system including osteonecrosis, tendinopathy, enthesopathy, and calcifications.10-13 The ESWT has different forms of application methods as focused ESWT (fESWT) and radial ESWT (rESWT).12 It has been shown that rESWT is less painful and does not require anesthesia in daily practice compared to fESWT, which has a high tissue penetration rate.10 Recently, in few clinical studies, rESWT has been applied in the treatment of frozen shoulder.11, 14-17 The proposed underlying mechanism for frozen shoulder is that inflammatory cytokines transforming growth factor-1 stimulate fibroblast proliferation and differentiation into myofibroblasts.18 The inflammation leading to an imbalance in the extracellular matrix cycle,19 resulting in a stiff glenohumeral capsule containing a large number of type III collagen.4, 18
Patients with both frozen shoulder and type 2 diabetes mellitus have worse functional outcomes than their nondiabetic counterparts.7 Many options are available for improving the pain, range of motion, and functionality in these patient population.20 Anti-inflammation has been proposed as the mechanism responsible for the therapeutic effects of rESWT;12, 21 however, the underlying mechanism of rESWT in individuals with frozen shoulder and type 2 diabetes mellitus still remains unclear. There is only two study that evaluated the usefulness of ESWT in diabetic patients.17, 22 Indeed, it has been reported by Kvaalag et al.23 that radial ESWT is not superior to sham rESWT in addition to supervised exercises in the long term in patients with subacromial pain syndrome. However, in this study, considering the physiological mechanism of ESWT, we wanted to question which dose (high- or medium-energy) is superior to sham rESWT (without supervised exercises), which is applied more intensely (twice a week, 2000 pulses) in the short term (for six-weeks) in individuals with frozen shoulder and type 2 diabetes mellitus. To the best of our knowledge, there is no study examining the efficacy of different energy levels of rESWT on the shoulder pain, range of motion, functionality, and muscle mechanical properties in frozen shoulder patients with type 2 diabetes mellitus. Therefore, the aim of this study was to examine the effectiveness of high- or medium-energy rESWT on pain, functionality, range of motion, and mechanical properties of the muscles in frozen shoulder patients with type 2 diabetes mellitus.
Materials and methods
This prospective clinical pilot study was conducted in frozen shoulder patients with type 2 diabetes mellitus. The research protocol was approved by the University Research Ethics Committee. The study was conducted in accordance with the principles of the Declaration of Helsinki. The study start date was January 25, 2019, and the study ended on September 17, 2019. The trial is registered at ClinicalTrials.gov (CT.gov identifier: NCT03185078). The study protocol was approved by the Medipol University Research Ethics Committee (IRB: 10840098-604.01.01-E.46255). The study was conducted in accordance with the principles of the Declaration of Helsinki. Data collection was performed at the Physical Therapy Department of the outpatient setting. All patients were informed about the nature of the study and possible risks and benefits of the treatment in detail. A written informed consent was obtained from each patient.
The patients received a total of 12 sessions of rESWT exposure, twice a week, for six weeks, and each session was performed at 8 Hz with 2000 pulses The entire treatment lasted 15 min per session. During the session, symptoms such as pain and discomfort, hypersensitivity, edema, hematoma syncope, and nausea were accepted as the termination criteria.
Participants
Frozen shoulder patients with diabetes who were referred to the clinic between December 2018 and January 2019 were evaluated by a physician for eligibility. Recruitment was conducted among patients with both primary adhesive capsulitis and type 2 diabetes mellitus who had been referred to the clinic. Inclusion criteria were patients aged >18 years, unilateral frozen shoulder, symptom duration >3 months, shoulder pain and limited glenohumeral joint active range of motion of greater than 50% in at least three specific movements among abduction, flexion, internal rotation, and external rotation, and first attack of the frozen shoulder. Before the last two weeks of enrollment, all participants underwent a standardized history, physical examination. Patients in whom no radiographic findings on anteroposterior, axillary or scapular y-view shoulder radiographs were found and no medical treatment other than analgesics had been prescribed within the past 3 months were included. Furthermore, having type 2 diabetes for at least 3 years, fasting blood glucose ≥126 mg/dL, and hemoglobin A1c (HbA1c)≥6.5% were other inclusion criteria for this study. Previous shoulder surgeries, massive, minor, and major rotator cuff tears, pain and muscle strength loss due to neurological causes, history or presence of malignancy, osteoporosis or active infection, analgesics or muscle relaxants taken within 72 hours of the examination, and use of pacemakers, and undergone any physiotherapy or steroid treatment within a 3-month period were exclusion criteria.
Randomization and blinding
The patients were assigned to three groups according to a random list in each group by an independent statistician using the MedCalc randomization algorithm (MedCalc Software, Ostend, Belgium) who did not involve in the data collection or analysis. The research assistant who had no knowledge of the study design, randomly assigned the participants to the three groups. The outcome assessor and statistician were blinded to the treatment allocation.
Interventions
All patients were informed about having a light meal before each session. During the session, the patients were instructed to sit with knees flexed in a comfortable position, in a back-supported chair with a forearm assisted at the treatment table. The rESW treatment applied in this study is reported according to the TIDIER Checklist.24 Radial ESWT was applied by a physiotherapist with 5 years of experience using the Enraf-Nonius Endopuls 811 (Enraf-Nonius BV, Echt, the Netherlands) device, and a 25-mm diameter applicator. Due to the nature of the rESWT, it was not possible to blind the physiotherapist who conducted the interventions. For dose adjustment, the classification was performed based on previous studies.15-17 The energy flux density (EFD) of pressure pulses for 1 mm2 of the study groups were arranged according to the energy output power (EOP), and radius of the applicator head (√). The following formula was used:
| EFD = EOP/(πr2) (π = 3.14) |
hrESWT group: EFD: 0.25 mJ/mm2 at 8 Hz; EOP=120 mJ (high-energy);
mrESWT group: EFD: 0.12 mJ/mm2 at 8 Hz; EOP=60 mJ (medium-energy);
prESWT group: simulated rESWT (0.00 mJ/mm2) at 8 Hz (placebo).
After the application of the ultrasound gel, 1,000 pulses were sent to the target area by placing shock waves at two different treatment sites, at right angles to the device applicator. At the first treatment point, rESWT was applied at the anterior side of the shoulder joint, in the superior-inferior direction, below the coracoid process and laterally to include the deltoid muscle, and the anterior side of joint capsule in the wave propagation region. The second treatment site (for 1000 pulses) was placed in the superior-inferior direction along the lateral and upper edge of the scapula, posterior to the shoulder joint for covering the trapezius upper muscle and posterior side of joint capsule.11, 15
The rESWT was simulated in the placebo group according to the previous studies.11, 15, 25 The device applicator was positioned to be the same as the other intervention groups. The previously recorded 8 Hz pulsed shock wave sounds were played, as if the actual application was being performed. The device was in the off mode during the session period without pressing the pedal. In the placebo group, none of the patients were aware of how the treatment was applied. All patients in the ESWT and placebo group were enrolled on different days during the evaluation and treatment sessions to avoid an interaction between the participants to minimize bias.
Outcome measures
The primary outcome measure was that of pain, while the secondary outcome measures were of the active range of motion (AROM), function, and resting tone of deltoid and trapezius upper muscles. All assessments were performed at the baseline, and 6th week, by the same investigator for all patients.
Primary outcome measurements
Pain evaluation
As the primary outcome, pain evaluation of the patients was performed using the Visual Analogue Scale (VAS) for two different conditions such as rest and during night. The use of VAS in shoulder problems has been reported to be one of the simple, easy-to-use, and reliable method for the pain evaluation.26 The patients were informed that, in a 10-cm length scale, 0 indicates no pain, while 10 indicate the worst imaginable pain. The patients were asked to mark the most appropriate score for their pain, and the overall pain score was calculated and recorded.
Secondary outcome measurements
Functionality assessment
Function was assessed using the self-administered Shoulder Pain and Disability Index (SPADI) score. It consists of 13 questions, and measures shoulder function. To answer the questions, patients place a mark on a 10-cm scale for each question. 0 indicates “no difficulty,” while 10 indicates “so difficult it required help.” The answers to these questions are then calculated into percentages, with a higher score indicating disability. The minimal clinically important difference has been reported to be 18% for the SPADI Tool.27
Range of motion evaluation
The active range of motions (AROMs) of the affected shoulder joint was measured using a digital electrogoniometer (Baseline® Absolute+Axis™ digital goniometer; Fabrication Enterprises, Inc., Elmsford, NY, USA), which was shown to be valid and reliable.28 The flexion, abduction, internal rotation, and external rotation AROM measurements were performed while the patients in a supine position on a plinth, with knees flexed at 90°. The blinded assessor manually stabilized the scapula with one hand positioned over the acromion and coracoid processes. A towel roll was placed under the distal humerus to ensure neutral horizontal positioning so that the humerus was level with the acromion process and the olecranon process was at the edge of the plinth. The patient arm was in a neutral start position, near the trunk for abduction and flexion AROM measurements. The arm was positioned in 45° abduction, and the elbow flexed to 90° with neutral pronation/supination for the rotation measurements.29
Mechanical properties assessment
The human resting muscle tone system provides structural and functional support to skeletal muscle and associated myofascial structures such as tendons and fascia in normal life.30 The MyotonPRO™ (Myoton AS, Tallinn, Estonia) is a new portable device designed to measure the muscle mechanical properties and a noninvasive approach to measure stiffness.31 Its reliability has been shown in the muscles around the shoulder in breast cancer patients.32 The reliability and validity of the measurement technique were shown in previous studies.30, 33, 34 The evaluation of the muscle mechanical properties was performed using the MyotonPRO (Myoton AS). The measurements of mechanical properties of the deltoid and trapezius upper muscles were performed in the supine, at rest, neutral arm position. Patient data were recorded to the Myoton (Myoton AS) software program and then, transferred to the device before the measurements were started. The deltoid and trapezius upper muscles were marked with a pencil. In the MyotonPRO (Myoton AS) application, the blinded physiotherapist held the device upright and exerted downward pressure. The pressure was terminated, when the red light on the plexiglass frame of the device probe turned green. The physiotherapist waited steadily, until five taps were performed. For each five taps, the duration of one shot was 15 ms and the time between each tap was 8 ms. Acceleration graph was examined after each application and measurements were repeated, if there was a deviation from normal procedure. In case of deviations, the device warned the operator with both radiographs and loud sound. Recordings were reloaded into the software program and reported for each participant. Therefore, it is a very new research topic, and it is necessary to recognize the obtained values related to the muscle structural properties in the MyotonPRO (Myoton AS) measurements and terms related to the equivalence of these values in mechanical properties.
Intramuscular tension or resting muscle tone corresponded to the frequency (oscillation frequency, Hz) value.
The resistance of the muscle against the external force, hardness was given in the stiffness (Newton/meter [N/m]) value. The stiffness value was calculated as maximum acceleration of oscillation/maximum displacement of the tissue. A higher value indicates a stiffer muscle which is inversely proportional to muscle compliance. As stiffness increased, compliance decreased or vice versa.35, 36
Statistical analysis
Statistical analysis was performed using the SPSS version 22.0 software (IBM Corp., Armonk, NY, USA) and the intention-to-treat concept37 was carried out by a blinded researcher who was not involved in the evaluation and treatment protocols. Descriptive data were expressed in mean±standard deviation (SD), median (min-max), or number and frequency, where applicable. Normality of the data was assessed using the Shapiro-Wilk Test. The χ2 test was used to examine the distribution of categorical variables among the groups. The Kruskal-Wallis Test was used for the inter-group analysis of resting pain variables. For the intra-group post-hoc analyses, the Wilcoxon Signed-Rank Test was performed. Variations of time in normal distribution variables were analyzed using the univariate general linear mixed models in time-dependent group interaction. The Bonferroni adjustments was applied for multiple comparisons, while the partial eta squared (η2) was calculated for the strength association of the between group comparisons. For describing the effect size of the partial η2 values; below 0.01, 0.06, and 0.14 describe small, medium, and large effect sizes, respectively. The mean differences between the groups were also calculated separately in each group using the paired samples t-test. For the normal distributed variables, Cohen’s d effect size and Z-scores were calculated. Cohen suggested that d=0.2 be considered a “small” effect size, 0.5 represents a “medium” effect size and 0.8 a “large” effect size.38 A P value of <0.05 was considered statistically significant.
Results
A total of 58 patients were evaluated for eligibility, and 19 participants who did not meet the inclusion criteria were exclude. Finally, 39 patients were randomly allocated to the high-energy rESWT (hrESWT, N.=13), medium-energy rESWT (mrESWT, N.=13), and simulated placebo group (prESWT, N.=13). One patient in the hrESWT group (lack of time [N.=1]), and two patients in the prESWT group (lack of time [N.=1], lack of efficiency [N.=1]) dropped out. An ITT analysis was conducted for the treatment effects. Flow of the study is presented in Figure 1. No adverse events or a serious life-threatening adverse event that occur during the course of a study.
Figure 1.
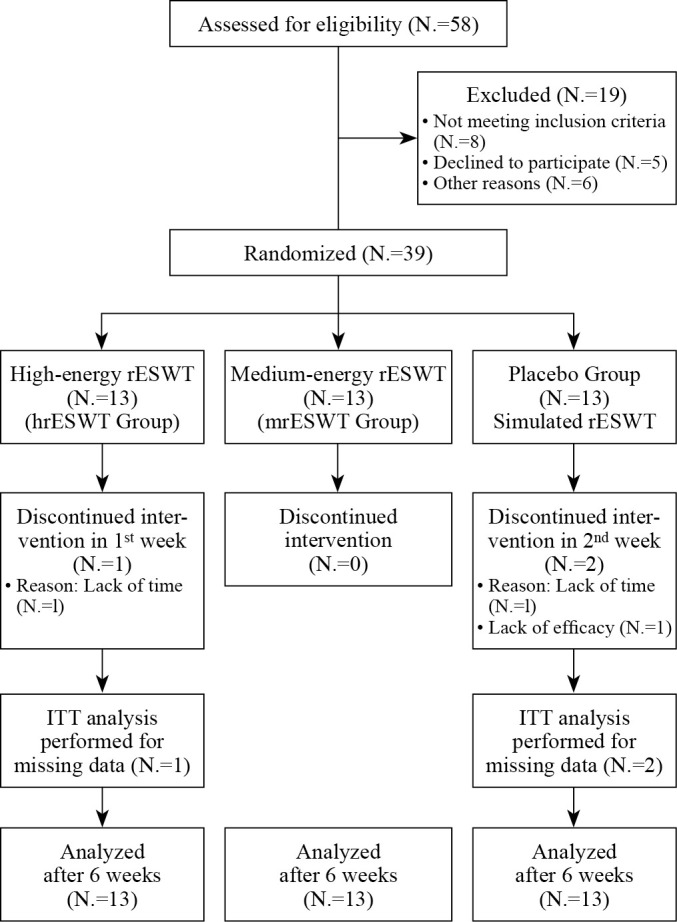
—The study flow. A total of 12, 13, and 11 patients completed the study in: 1) high energy; 2) medium energy; and 3) placebo group, respectively. Three patients drop out of trial due to lack of time, and lack of efficacy. The analysis was performed according to the intention-to-treat principle (ITT). hrESWT: High-energy radial extracorporeal shock wave therapy (0.25 mj/mm2); mrESWT: medium-energy radial extracorporeal shock wave therapy (0.12 mj/mm2); prESWT: placebo radial extracorporeal shock wave therapy (0.0 mj/mm2).
There were no significant differences in baseline demographic and clinical characteristics of the patients between groups (P>0.05) (Table I). All three groups demonstrated a significant reduction in the resting pain severity (P<0.05), and there were no significant differences in the resting pain at six weeks among the groups. Both high- and medium-energy and placebo rESWT improved night pain VAS scores (8.23±1.59 to 4.42±2.1 vs. 8.81±0.99 to 3.54±2.15 and 7.88±1.23 to 5.88±1.61, respectively; P=0.015). According to the mean change pairwise-comparisons, the VAS scores of night pain in the medium-energy rESWT group were lower than the placebo group (mean change -5.27; 95% CI: -6.70 to -3.84, P=0.002). The mean change in high-energy rESWT group was not statistically different from the placebo group (P≥0.05).
Table I. —Baseline demographic and clinical characteristics of patients.
| Characteristics | hrESWT | mrESWT | prESWT | Total | P |
|---|---|---|---|---|---|
| Age (year) | 52.00±5.16 | 54.23±6.04 | 54.23±6.34 | 53.49±5.81 | 0.541 |
| BMI (kg/m2) | 29.91±3.27 | 27.77±3.70 | 28.38±4.05 | 28.69±3.70 | 0.323 |
| Symptom duration (month) | 8.08±3.64 | 8.15±3.48 | 8.69±3.52 | 8.31±3.47 | 0.891 |
| Diabetes diagnosis time (year) | 10.62±6.14 | 9.46±5.17 | 9.69±6.14 | 9.92±5.70 | 0.868 |
| Fasting blood glucose (mg/dL) | 173.02±26.67 | 161.58±20.10 | 156.76±27.86 | 163.78±25.40 | 0.251 |
| HbA1c (%) | 7.63±0.82 | 7.23±0.73 | 7.28±0.73 | 7.38±0.76 | 0.362 |
| Insulin dependent (yes) | 4 (30.8) | 2 (15.4) | 2 (15.4) | 8 (20.5) | 0.533# |
| Sex | |||||
| Female N. (%) | 8 (61.5) | 10 (76.9) | 9 (69.2) | 27 (69.2) | 0.697# |
| Affected side | |||||
| Right N. (%) | 6 (46.2) | 6 (46.2) | 9 (69.2) | 21 (53.8) | 0.395# |
| Dominant side | |||||
| Right N. (%) | 12 (92.3) | 12 (92.3) | 11 (84.6) | 35 (89.7) | 0.757# |
| Smoking | |||||
| Yes N. (%) | 7 (53.8) | 4 (30.8) | 3 (23.1) | 14 (35.9) | 0.235# |
| Previous physiotherapy | |||||
| Treatment before ˃3 months (yes) | 5 (38.5) | 6 (46.2) | 7 (53.8) | 18 (46.2) | 0.734# |
Data are mean±SD or N. (%). 1) hrESWT; 2) mrESWT; 3) prESWT; 1-2 hrESWT statistically different from mrESWT. Statistically significance: P˂0.005. #Analyzed by χ2 test. BMI: Body Mass Index; HbA1c: glycated hemoglobin; hrESWT: high-energy radial extracorporeal shock wave therapy (0.25 mj/mm2); mrESWT: medium-energy radial extracorporeal shock wave therapy (0.12 mj/mm2); prESWT: placebo radial extracorporeal shock wave therapy (0.0 mj/mm2); P: significance level of general linear mixed model test.
An improvement was observed in the SPADI scores compared to baseline in both medium- and high-energy rESWT (mean change: -29.59±22.60 vs. -35.42±21.29 points, respectively; P<0.001) groups. According to the mean change pairwise-comparisons both groups demonstrated a statistically different change in SPADI scores from the placebo group (P≤0.05). There was no significant improvement in functionality in the placebo group (d=-0.30, P=0.303) (Table II, Table III, Table IV).
Table II. —Results of pain and functionality scores of patients: resting pain.
| Variables | hrESWT | mrESWT | prESWT | P¥ | |||||
|---|---|---|---|---|---|---|---|---|---|
| Median 25th to 75th | Min-max | Median 25th to 75th | Min-max | Median 25th to 75th | Min-max | ||||
| Resting pain (0-10 cm) |
Baseline | 5 (3 to 5.5) | 0-7 | 5 (3 to 5) | 0-7 | 4 (0 to 5) | 0-8 | 0.840 | |
| After treatment | 2 (0 to 3.64) | 0-6 | 0 (0 to 2) | 0-4 | 1.64 (0 to 2.5) | 0-7 | 0.395 | ||
| Z | P§ | -2.670 | P=0.008 | -2.944 | P=0.003 | -2.199 | P=0.028 | ||
Data shown are mean±standard deviation and 95% CI values for variables. Statistically significance: P˂0.005. Models Test: 1 (hrESWT); 2 (mrESWT); 3 (prESWT); 1-3 (hrESWT statistically different from prESWT); 2-3 (mrESWT statistically different from prESWT). hrESWT: High-energy radial extracorporeal shock wave therapy (0.25 mj/mm2); mrESWT: medium-energy radial extracorporeal shock wave therapy (0.12 mj/mm2); prESWT: placebo radial extracorporeal shock wave therapy (0.0 mj/mm2); 0: no pain; 10: worst imaginable pain. ¥Significance level of Kruskal Wallis Test; §significance level of Wilcoxon Signed-Rank Test.
Table III. —Results of pain and functionality scores of patients: night pain.
| Variables | hrESWT | mrESWT | prESWT | P* | η2 | Post-hoc PC | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | |||||||||
| Night pain (0-10 cm) |
Baseline | 8.23±1.59 | 8.81±0.99 | 7.88±1.23 | 0.199 | 0.09 | |||||
| After treatment | 4.42±2.1 | 3.54±2.15 | 5.88±1.61 | 0.015 | 0.21 | 2-3 (P=0.022) | |||||
| Mean change (95% CI) | -3.81±2.19 (-5.13; -2.48) |
-5.27±2.37 (-6.70; -3.84) |
-2.01±2.19 (-3.33; -0.69) |
0.003 | 0.27 | 2-3 (P=0.002) | |||||
| Effect size | pp | -1.74 | P<0.001 | -2.22 | P<0.001 | -0.92 | P=0.006 | ||||
Data shown are mean±standard deviation and 95% CI values for variables. Statistically significance: P˂0.005. Models Test: 1 (hrESWT); 2 (mrESWT); 3 (prESWT); 1-3 (hrESWT statistically different from prESWT); 2-3 (mrESWT statistically different from prESWT). hrESWT: High-energy radial extracorporeal shock wave therapy (0.25 mj/mm2); mrESWT: medium-energy radial extracorporeal shock wave therapy (0.12 mj/mm2); prESWT: placebo radial extracorporeal shock wave therapy (0.0 mj/mm2); 0: no pain; 10: worst imaginable pain; η2: partial eta squared; PC: pairwise comparison. ^Significance level of paired sample t-test; *significance level of general linear mixed model test.
Table IV. —Results of functionality scores of patients.
| Variables | hrESWT | mrESWT | prESWT | P* | η2 | Post-hoc PC | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | |||||||||
| Functionality | Baseline | 74.84±11.69 | 67.34±6.46 | 61.36±7.57 | 0.002 | 0.29 | 1-3 (P=0.001) | ||||
| After treatment | 39.42±23.15 | 37.75±22.57 | 58.73±11 | 0.017 | 0.20 | 1-3 (P=0.044) 2-3 (P=0.027) |
|||||
| Mean change (95% CI) | -35.42±21.29 (-48.29; -22.55) |
-29.59±22.60 (-43.24; -15.93) |
-2.63±8.79 (-7.94; 2.69) |
P<0.001 | 0.39 | 1-3 (P˂0.001) 2-3 (P=0.002) |
|||||
| Effect size | P^ | -1.66 | P<0.001 | -1.31 | P<0.001 | -0.30 | P=0.303 | ||||
Data shown are mean±standard deviation and 95% CI values for variables. Statistically significance: P˂0.005. Models Test: 1 (hrESWT); 2 (mrESWT); 3 (prESWT); 1-3 (hrESWT statistically different from prESWT); 2-3 (mrESWT statistically different from prESWT). hrESWT: High-energy radial extracorporeal shock wave therapy (0.25 mj/mm2); mrESWT: medium-energy radial extracorporeal shock wave therapy (0.12 mj/mm2); prESWT: placebo radial extracorporeal shock wave therapy (0.0 mj/mm2); 0: no difficulty in functionality; 100: worst difficulty requiring assistance; η2: partial eta squared; PC: pairwise comparison. ^Significance level of paired sample t-test; *significance level of general linear mixed model test.
At six weeks, both high- and medium-energy rESWT improved the shoulder flexion AROM, which was significantly higher than the placebo group (P<0.001 vs. P<0.001 and P=0.643, respectively). The shoulder abduction and external rotation AROM significantly changed in all three groups (P<0.005). However, according to the mean change pairwise-comparisons, both high- and medium-energy rESWT were similarly successful in improving shoulder abduction AROM, compared to baseline (mean change: 45.95±21.32 vs. 39.04±18.99 degree, respectively; P<0.001) versus to the placebo group at six-week. The high-energy rESWT group had a greater improvement in the external rotation AROM (mean change: 32.22 degree; 95% CI: 41.07 to 23.37) after six weeks versus medium-energy rESWT (P=0.001) and placebo groups (P<0.001). An improvement was observed in the internal rotation AROM scores compared to baseline in both high- and medium-energy rESWT groups (mean change: 25.86±13.24 vs. 18.19±14.63 points, respectively; P<0.001 vs. P=0.001). According to the mean change pairwise-comparisons the internal rotation AROM scores in the high-energy rESWT group were higher than the placebo group (mean change 17.51 degree; 95% CI: 2.99 to 32.03, P=0.015). The mean change of internal rotation AROM scores in the medium-energy rESWT group was not statistically different from the placebo group (P=0.222). There was no significant improvement in the placebo group (P=0.087).
According to the partial η2 (ηp2) values of pain and AROM scores, the findings indicated a large effect for the study outcomes (ηp2=0.27, ηp2=0.39, ηp2=0.48, ηp2=0.47, ηp2=0.53, and ηp2=0.21; for night pain, functionality, flexion, abduction, external rotation AROM, and internal rotation AROM, respectively) (Table V).
Table V. —Results of the shoulder joint active range of motions.
| Active range of motions of shoulder | hrESWT | mrESWT | prESWT | P* | η2 | Post-hoc PC | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | |||||||||
| Flexion AROM° |
Baseline | 118.25±18.02 | 132.42±19.12 | 130.77±18.47 | 0.118 | 0.11 | |||||
| After treatment | 159.89±14.96 | 159.44±17.26 | 132.59±17.19 | <0.001 | 0.39 | 1-3 (P=0.001) 2-3 (P=0.001) |
|||||
| Mean change (95% CI) |
41.64±20.94 (54.29; 28.98) |
27.02±18.13 (37.97; 16.06) |
1.82±13.80 (-10.16; 6.52) |
<0.001 | 0.48 | 1-3 (p˂0.001) 2-3 (P=0.003) |
|||||
| Effect size | P^ | 1.99 | P<0.001 | 1.49 | P<0.001 | 0.13 | P=0.643 | ||||
| Abduction AROM° |
Baseline | 78.18±23.48 | 100.10±28.45 | 91.62±25.79 | 0.110 | 0.12 | |||||
| After treatment | 124.13±32.42 | 139.14±37.14 | 99.68±22.49 | 0.010 | 0.23 | 2-3 (P=0.008) | |||||
| Mean change (95% CI) | 45.95±21.32 (58.83; 33.06) |
39.04±18.99 (50.52; 27.56) |
8.06±12.85 (15.83; 0.28) |
<0.001 | 0.47 | 1-3 (P˂0.001) 2-3 (P˂0.001) |
|||||
| Effect size | P^ | 2.31 | P<0.001 | 2.27 | P<0.001 | 0.65 | P=0.043 | ||||
| External rotation AROM° |
Baseline | 26.75±16.26 | 39.84±18.4 | 32.33±11.26 | 0.114 | 0.11 | |||||
| After treatment | 58.97±18.89 | 55.22±17.38 | 37.38±8.39 | 0.002 | 0.28 | 1-3 (P=0.003) 2-3 (P=0.016) |
|||||
| Mean change (95% CI) |
32.22±14.65 (41.07; 23.37) |
15.38±9.65 (21.21; 9.55) |
5.05±7.47 (9.56; 0.53) |
<0.001 | 0.53 | 1-2 (P=0.001) 1-3 (P˂0.001) |
|||||
| Effect size | P^ | 2.22 | P<0.001 | 1.60 | P<0.001 | 0.72 | P=0.031 | ||||
| Internal rotation AROM |
Baseline | 36.40±18.38 | 58.00±21.87 | 43.46±15.58 | 0.025 | 0.62 | 1-2 (P=0.015) | ||||
| After treatment | 62.26±21.82 | 76.19±19.84 | 51.81±10.76 | 0.186 | 0.23 | ||||||
| Mean change (95% CI) |
25.86±13.24 (17.45; 34.27) |
18.19±14.63 (9.35; 27.03) |
8.35±14.59 (-1.46; 18.15) |
0.020 | 0.21 | 1-3 (P=0.015) | |||||
| Effect size | P^ | 1.28 | P<0.001 | 0.87 | P=0.001 | 0.62 | P=0.087 | ||||
Data shown are mean±standard deviation, mean change, and 95% CI. Statistically significance: P˂0.005. Models Test: 1 (hrESWT); 2 (mrESWT); 3 (prESWT); 1-3 (hrESWT statistically different from prESWT); 2-3 (mrESWT statistically different from prESWT). hrESWT: High-energy radial extracorporeal shock wave therapy (0.25 mj/mm2); mrESWT: medium-energy radial extracorporeal shock wave therapy (0.12 mj/mm2); prESWT: placebo radial extracorporeal shock wave therapy (0.0 mj/mm2); 0: no difficulty in functionality; 100: worst difficulty requiring assistance; η2: partial eta squared (the norms for partial eta-squared [small: 0.01], [medium: 0.06]; [large: 0.14]); PC: pairwise comparison; AROM: active range of motion (° measured in degree). ^Significance level of paired sample t-test; *significance level of general linear mixed model test.
There was no significant change in any of the muscle mechanical properties of the patients in the placebo group (P>0.05 for all) after six weeks. Significantly improved resting tone (frequency score; -2.60±1.51 vs. 2.38±1.98, respectively; partial η2=0.58, P<0.001) and compliance of deltoid muscle (stiffness score, -60.38±38.09 vs. 67.10±43.13, respectively; partial η2=0.62, P<0.001) were found in the medium-energy rESWT group compared to the high-energy rESWT group. Trapezius upper frequency (d=-0.49, P=0.101) and stiffness (d=-0.19, P=0.496) did not significantly change in the medium-energy rESWT group. The trapezius upper stiffness decreased (-36.27±38.65, d=-0.94, P=0.005), and the trapezius upper muscle resting tone remained lower levels (frequency scores; -1.85±1.69 vs. 0.61±3.12, respectively; partial η2=0.17, P<0.005) at six-week in the high-energy rESWT group, compared to the placebo group (Table VI).
Table VI. —Results of deltoid and trapezius upper muscles mechanical properties.
| Mechanical properties – Myoton PRO | hrESWT | mrESWT | prESWT | P* | η2 | Post-hoc PC | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | |||||||||
| Deltoid frequency (Hz) | Baseline | 14.27±2.15 | 17.24±1.76 | 14.56±2.3 | 0.001 | 0.31 | 2-1 (P=0.002) 2-3 (P=0.006) |
||||
| After treatment | 16.65±3.38 | 14.64±1.12 | 14.87±2.27 | 0.085 | 0.13 | ||||||
| Mean change (95% CI) |
2.38±1.98 (1.19;3.58) |
-2.60±1.51 (-3.51; -1.69) |
0.31±1.85 (-0.81; 1.43) |
<0.001 | 0.58 | 1-2 (P˂0.001) 1-3 (P=0.017) 2-3 (P=0.001) |
|||||
| Effect size | P^ | 1.20 | P=0.001 | -1.72 | P<0.001 | 0.17 | P=0.556 | ||||
| Trapezius upper frequency (Hz) | Baseline | 15.34±2.29 | 14.7±10 | 13.26±1.52 | 0.011 | 0.22 | 1-3 (P=0.009) | ||||
| After treatment | 13.49±1.63 | 13.79±1.92 | 13.87±2.38 | 0.878 | 0.01 | ||||||
| Mean change (95% CI) |
-1.85±1.69 (-2.87; -0.82) |
-0.91±1.84 (-2.02; 0.20) |
0.61±3.12 (-1.27; 2.50) |
0.033 | 0.17 | 1-3 (P=0.027) | |||||
| Effect size | P^ | -1.09 | P=0.002 | -0.49 | P=0.101 | 0.20 | P=0.493 | ||||
| Deltoid stiffness (N/m) | Baseline | 267.15±45.5 | 329.62±45.46 | 272.23±65.93 | 0.008 | 0.23 | 1-2 (P=0.013) 2-3 (P=0.024) |
||||
| After treatment | 334.25±74.6 | 269.23±21.79 | 289.35±51.64 | 0.012 | 0.22 | 1-2 (P=0.011) | |||||
| Mean change (95% CI) |
67.10±43.13 (41.03; 93.16) |
-60.38±38.09 (-83.40; -37.37) |
17.12±47.15 (-11.37; 45.62) |
<0.001 | 0.62 | 1-2 (P˂0.001) 1-3 (P=0.016) 2-3 (P˂0.001) |
|||||
| Effect size | P^ | 1.56 | P<0.001 | -1.59 | P<0.001 | 0.36 | P=0.215 | ||||
| Trapezius upper stiffness (N/m) | Baseline | 289.92±43.62 | 267.62±24.37 | 250.69±40.34 | 0.036 | 0.17 | 1-3 (P=0.028) | ||||
| After treatment | 253.66±22.93 | 259.77±30.39 | 259.45±56.27 | 0.905 | 0.01 | ||||||
| Mean change (95% CI) |
-36.27±38.65 (-59.62; -12.91) |
-7.85±40.26 (-32.18; 16.48) |
8.76±76.42 (-37.42; 54.94) |
0.119 | |||||||
| Effect size | P^ | -0.94 | P=0.005 | -0.19 | P=0.496 | 0.11 | P=0.687 | ||||
Data shown are mean±standard deviation, mean change, and 95% CI. Statistically significance: P˂0.005. Models Test: 1 (hrESWT); 2 (mrESWT); 3 (prESWT); 1-3 (hrESWT statistically different from prESWT); 2-3 (mrESWT statistically different from prESWT). hrESWT: High-energy radial extracorporeal shock wave therapy (0.25 mj/mm2); mrESWT: medium-energy radial extracorporeal shock wave therapy (0.12 mj/mm2); prESWT: placebo radial extracorporeal shock wave therapy (0.0 mj/mm2); 0: no difficulty in functionality; 100: worst difficulty requiring assistance; η2: partial eta squared (the norms for partial eta-squared [small: 0.01], [medium: 0.06]; [large: 0.14]); PC: pairwise comparison; AROM: active range of motion (° measured in degree). ^Significance level of paired sample t-test; *significance level of general linear mixed model test.
Discussion
The study results showed that high- and medium-energy rESWT yield a wide range of effectiveness in terms of night pain, shoulder rotational range of motion, and mechanical properties of the deltoid, trapezius upper muscles of frozen shoulder patients with type 2 diabetes mellitus. The best improvement was observed in night pain with medium-energy rESWT. Functionality significantly increased with the application of both medium- and high-energy rESWT.
The studies utilizing ESWT suggest that shockwave exposure increase the effectiveness of conservative physiotherapy and decrease pain,39 compared to steroid treatment.25 Santoboni et al. reported that ESWT was effective in the shoulder pain management in the short and long-term period.17 Instead of analyzing dose difference efficacy in patients with diabetes related or unrelated frozen shoulder patients, most of the previous studies addressed into the comparison of ESWT with conservative physiotherapy,39 steroid treatment25 or placebo.15 Consistent with literature and this presented study results, we can speculate that the different types or energy levels of ESWT are effective in reducing pain. Considering the underlying mechanism, the high- or medium-energy rESWT could be effective in the regulation of peripheral pain systems by suppressing inflammation with pressure wave effects on nociceptor and mechanoreceptors.10, 40 Based on study results, we can suggest that different energy levels of rESWT show a variable extent of improvement of night pain, which is the main complaint of frozen shoulder patients with type 2 diabetes mellitus.1 To achieve more favorable results, we could recommend six-week medium-energy rESWT attendance for pain, especially night pain reduction in frozen shoulder patients with type 2 diabetes mellitus in short-term period.
Previous studies using rESWT15 and fESWT11, 39 have demonstrated improvements in flexion,11, 39 external rotation,11, 15, 39 abduction ROM11, 15 both in the short- and long-term. Treatments to break the vicious cycle in the dynamic interaction between chronic pain, limited range of motion, and dysfunction should be effective enough to stimulate the upper centers for the central sensitization in frozen shoulder.41 In this presented study, it was observed that rESWT applied at high- or medium-energy for six weeks enhanced the improvement in flexion and abduction AROM without any superiority, and this gain could be transferred to shoulder functionality adequately. Similarly, Hussein et al. showed that the rESWT was effective in improving participation in daily living activities at 4-weeks.15 The increase in movements of gleno-humeral joint as shown in previous studies11, 15, 39 could be attributed to the direct effects of rESWT on the reorganization of various cytokines that control the position of collagen, the formation of adhesion molecules, and soft tissue healing.19 Based on current study results, compared to the medium-energy level, the high-energy rESWT was more effective in improvement the internal and external rotation AROM. Therefore, we recommend the high-energy rESWT applications in frozen shoulder patients with diabetes who have more restrictions with internal rotation, external rotation motions of shoulder joint. However, it should be known this effectiveness is comparable in terms of functionality.
In patients with frozen shoulder, stiffness may affect the muscles around the shoulder.2, 5, 42, 43 The main problem with a frozen shoulder is the contracture of the joint capsule, while the secondary problem is the increase in the muscle tone of the adjacent muscles.2 In addition, previous studies still remain insufficient to conclude whether changes in muscle tone contribute to improvements in pain and AROM. The number of studies using the rESWT15 and the fESWT11, 17, 25, 39 for frozen shoulder is limited. There is no study examining the dose difference effectiveness on muscle mechanical properties of shoulder complex in frozen shoulder patients with type 2 diabetes mellitus. Objective demonstration of the intramuscular mechanical properties has been reported to help in understanding both structural improvements and deficiencies.31, 33 In studies in which the muscle mechanical properties were examined, the resting muscle tone increased and the compliance decreased in the presence of a pathology and advanced age.30-32, 44 Choi et al. showed the effectiveness of kinesiotape application in addition to conservative physiotherapy in patients with shoulder pain by examining the mechanical properties of the deltoid muscle.45 They reported a decrease in the resting muscle tone and an increase in the muscle compliance. Indeed, in the study examining the efficacy of Maitland’s Mobilization and kinesiotape application in subacromial impingement disease, reduced resting muscle tone and increased muscle compliance of the deltoid and trapezius upper muscles were observed.46 Radial ESWT has been shown to be as effective as dry needling in the treatment of upper trapezius trigger points.47 Similar to this presented study and a previous study in which myofascial trigger point relaxation therapy was applied to patients with shoulder pain, the compliance and elasticity of the trapezius upper muscle increased.44 Accordingly, the mechanical properties of the trapezius upper muscle were not affected by the medium-energy rESWT, while the high-energy rESWT reduced the resting muscle tone and increased the muscle compliance. According to these data, we can mention that the effectiveness of rESWT on mechanical properties depends on the targeted muscle and varies according to the dose differences. Therefore, if the rESWT is to be used for the treatment of frozen shoulder patients with type 2 diabetes mellitus and the mechanical properties of the deltoid muscle are desired to be increased, we can recommend the use of the medium-energy. However, if the targeted muscle is the trapezius upper for these patients, the clinicians should use high-energy to achieve an effective change in the mechanical properties.
Limitations of the study
Nonetheless, a major limitation of our pilot study is the small sample size. The second one is the follow-up was conducted only once. Other limitations include the lack of using a pain pressure threshold method and the lack of an evaluation of the muscle mechanical changes with other objective tools such as shear-wave elastography. Furthermore, further large-scale, long-term, prospective studies using different evaluation methods and different energy levels of rESWT in frozen shoulder patients with diabetes are warranted.
Conclusions
Based on this pilot study short-term treatment results, the medium-energy rESWT seems to be the most effective option in the night pain, and deltoid muscle mechanical properties. The high-energy rESWT provides more favorable results in trapezius upper muscle mechanical properties and in the improvement of internal rotation, external rotation motions of shoulder joint. Hence, significant improvements in pain, AROM, and its reflection on functionality show that irrespective of the energy level, the rESWT may be an alternative treatment, at least in the short-term, for frozen shoulder patients with type 2 diabetes mellitus.
References
- 1.Hsu CL, Sheu WH. Diabetes and shoulder disorders. J Diabetes Investig 2016;7:649–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27182002&dopt=Abstract 10.1111/jdi.12491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ryan V, Brown H, Minns Lowe CJ, Lewis JS. The pathophysiology associated with primary (idiopathic) frozen shoulder: A systematic review. BMC Musculoskelet Disord 2016;17:340. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27527912&dopt=Abstract 10.1186/s12891-016-1190-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bunker TD, Reilly J, Baird KS, Hamblen DL. Expression of growth factors, cytokines and matrix metalloproteinases in frozen shoulder. J Bone Joint Surg Br 2000;82:768–73. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10963182&dopt=Abstract 10.1302/0301-620X.82B5.0820768 [DOI] [PubMed] [Google Scholar]
- 4.Wong CK, Levine WN, Deo K, Kesting RS, Mercer EA, Schram GA, et al. Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy 2017;103:40–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27641499&dopt=Abstract 10.1016/j.physio.2016.05.009 [DOI] [PubMed] [Google Scholar]
- 5.Cucchi D, Marmotti A, De Giorgi S, Costa A, D’Apolito R, Conca M, et al. SIGASCOT Research Committee . Risk factors for shoulder stiffness: current concepts. Joints 2017;5:217–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29270559&dopt=Abstract 10.1055/s-0037-1608951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park HB, Gwark JY, Kam M, Jung J. Association between fasting glucose levels and adhesive capsulitis in a normoglycemic population: a case-control study. J Shoulder Elbow Surg 2020;29:2240–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32713668&dopt=Abstract 10.1016/j.jse.2020.03.017 [DOI] [PubMed] [Google Scholar]
- 7.Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J 2016;6:26–34. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27331029&dopt=Abstract 10.32098/mltj.01.2016.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qureshi AA, Ross KM, Ogawa R, Orgill DP. Shock wave therapy in wound healing. Plast Reconstr Surg 2011;128:721e–7e. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21841528&dopt=Abstract 10.1097/PRS.0b013e318230c7d1 [DOI] [PubMed] [Google Scholar]
- 9.Reilly JM, Bluman E, Tenforde AS. Effect of shockwave treatment for management of upper and lower extremity musculoskeletal conditions: a narrative review. PM R 2018;10:1385–403. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29775801&dopt=Abstract 10.1016/j.pmrj.2018.05.007 [DOI] [PubMed] [Google Scholar]
- 10.Gerdesmeyer L, Gollwitzer H, Diehl P, Wagner K. Radial extracorporeal shockwave therapy (rESWT) in orthopaedics. J Miner Stoffwechs. 2004;11:36–9. [Google Scholar]
- 11.Vahdatpour B, Taheri P, Zade AZ, Moradian S. Efficacy of extracorporeal shockwave therapy in frozen shoulder. Int J Prev Med 2014;5:875–81. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25104999&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 12.Wang CJ. Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res 2012;7:11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22433113&dopt=Abstract 10.1186/1749-799X-7-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abo Al-Khair MA, El Khouly RM, Khodair SA, Al Sattar Elsergany MA, Hussein MI, Eldin Mowafy ME. Focused, radial and combined shock wave therapy in treatment of calcific shoulder tendinopathy. Phys Sportsmed 2021;49:480–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33283581&dopt=Abstract 10.1080/00913847.2020.1856633 [DOI] [PubMed] [Google Scholar]
- 14.Ahmed MM, Osama SA, Mohamed MN, Kassem SH, Ahmed ATF. Effects of shock wave therapy on inflammatory markers in diabetic and non-diabetic frozen shoulder. Drug Invention Today 2020;14. [Google Scholar]
- 15.Hussein AZ, Donatelli RA. The efficacy of radial extracorporeal shockwave therapy in shoulder adhesive capsulitis: a prospective, randomised, double-blind, placebo-controlled, clinical study. Eur J Physiother 2016;18:63–76. 10.3109/21679169.2015.1119887 [DOI] [Google Scholar]
- 16.Muthukrishnan R, Rashid AA, Al-Alkharji F. The effectiveness of extracorporeal shockwave therapy for frozen shoulder in patients with diabetes: randomized control trial. J Phys Ther Sci 2019;31:493–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31417208&dopt=Abstract 10.1589/jpts.31.493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santoboni F, Balducci S, D’Errico V, Haxhi J, Vetrano M, Piccinini G, et al. Extracorporeal shockwave therapy improves functional outcomes of adhesive capsulitis of the shoulder in patients with diabetes. Diabetes Care 2017;40:e12–3. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27899492&dopt=Abstract 10.2337/dc16-2063 [DOI] [PubMed] [Google Scholar]
- 18.Kraal T, Lübbers J, van den Bekerom MP, Alessie J, van Kooyk Y, Eygendaal D, et al. The puzzling pathophysiology of frozen shoulders - a scoping review. J Exp Orthop 2020;7:91. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33205235&dopt=Abstract 10.1186/s40634-020-00307-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodeo SA, Hannafin JA, Tom J, Warren RF, Wickiewicz TL. Immunolocalization of cytokines and their receptors in adhesive capsulitis of the shoulder. J Orthop Res 1997;15:427–36. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9246090&dopt=Abstract 10.1002/jor.1100150316 [DOI] [PubMed] [Google Scholar]
- 20.Redler LH, Dennis ER. Treatment of Adhesive Capsulitis of the Shoulder. J Am Acad Orthop Surg 2019;27:e544–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30632986&dopt=Abstract 10.5435/JAAOS-D-17-00606 [DOI] [PubMed] [Google Scholar]
- 21.Waugh CM, Morrissey D, Jones E, Riley GP, Langberg H, Screen HR. In vivo biological response to extracorporeal shockwave therapy in human tendinopathy. Eur Cell Mater 2015;29:268–80, discussion 280. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25978115&dopt=Abstract 10.22203/eCM.v029a20 [DOI] [PubMed] [Google Scholar]
- 22.El Naggar TE, Maaty AI, Mohamed AE. Effectiveness of radial extracorporeal shock-wave therapy versus ultrasound-guided low-dose intra-articular steroid injection in improving shoulder pain, function, and range of motion in diabetic patients with shoulder adhesive capsulitis. J Shoulder Elbow Surg 2020;29:1300–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32553435&dopt=Abstract 10.1016/j.jse.2020.03.005 [DOI] [PubMed] [Google Scholar]
- 23.Kvalvaag E, Roe C, Engebretsen KB, Soberg HL, Juel NG, Bautz-Holter E, et al. One year results of a randomized controlled trial on radial Extracorporeal Shock Wave Treatment, with predictors of pain, disability and return to work in patients with subacromial pain syndrome. Eur J Phys Rehabil Med 2018;54:341–50. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28655271&dopt=Abstract 10.23736/S1973-9087.17.04748-7 [DOI] [PubMed] [Google Scholar]
- 24.Negrini S. Application of the TIDieR checklist to improve understanding and replicability of studies in Physical and Rehabilitation Medicine. Eur J Phys Rehabil Med 2015;51:667–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26782678&dopt=Abstract [PubMed] [Google Scholar]
- 25.Chen CY, Hu CC, Weng PW, Huang YM, Chiang CJ, Chen CH, et al. Extracorporeal shockwave therapy improves short-term functional outcomes of shoulder adhesive capsulitis. J Shoulder Elbow Surg 2014;23:1843–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25441567&dopt=Abstract 10.1016/j.jse.2014.08.010 [DOI] [PubMed] [Google Scholar]
- 26.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 2001;8:1153–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11733293&dopt=Abstract 10.1111/j.1553-2712.2001.tb01132.x [DOI] [PubMed] [Google Scholar]
- 27.Breckenridge JD, McAuley JH. Shoulder pain and disability index (SPADI). J Physiother 2011;57:197–197. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21843839&dopt=Abstract 10.1016/S1836-9553(11)70045-5 [DOI] [PubMed] [Google Scholar]
- 28.Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry. Philadelphia, PA: FA Davis; 2016. [Google Scholar]
- 29.Cools AM, De Wilde L, Van Tongel A, Ceyssens C, Ryckewaert R, Cambier DC. Measuring shoulder external and internal rotation strength and range of motion: comprehensive intra-rater and inter-rater reliability study of several testing protocols. J Shoulder Elbow Surg 2014;23:1454–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24726484&dopt=Abstract 10.1016/j.jse.2014.01.006 [DOI] [PubMed] [Google Scholar]
- 30.Schoenrock B, Zander V, Dern S, Limper U, Mulder E, Veraksitš A, et al. Bed rest, exercise countermeasure and reconditioning effects on the human resting muscle tone system. Front Physiol 2018;9:810. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30018567&dopt=Abstract 10.3389/fphys.2018.00810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roch M, Morin M, Gaudreault N. The MyotonPRO: A reliable tool for quantifying the viscoelastic properties of a trigger point on the infraspinatus in non-traumatic chronic shoulder pain. J Bodyw Mov Ther 2020;24:379–85. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33218538&dopt=Abstract 10.1016/j.jbmt.2020.05.002 [DOI] [PubMed] [Google Scholar]
- 32.Yeo SM, Kang H, An S, Cheong I, Kim Y, Hwang JH. Mechanical Properties of Muscles around the Shoulder in Breast Cancer Patients: Intra-rater and Inter-rater Reliability of the MyotonPRO. PM R 2020;12:374–81. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31359596&dopt=Abstract 10.1002/pmrj.12227 [DOI] [PubMed] [Google Scholar]
- 33.Kerins CM, Moore SD, Butterfield TA, McKeon PO, Uhl TL. Reliability of the myotonometer for assessment of posterior shoulder tightness. Int J Sports Phys Ther 2013;8:248–55. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23772341&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 34.Liu CL, Feng YN, Zhang HQ, Li YP, Zhu Y, Zhang ZJ. Assessing the viscoelastic properties of upper trapezius muscle: Intra- and inter-tester reliability and the effect of shoulder elevation. J Electromyogr Kinesiol 2018;43:226–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29103836&dopt=Abstract 10.1016/j.jelekin.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 35.Feng YN, Li YP, Liu CL, Zhang ZJ. Assessing the elastic properties of skeletal muscle and tendon using shearwave ultrasound elastography and MyotonPRO. Sci Rep 2018;8:17064. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30459432&dopt=Abstract 10.1038/s41598-018-34719-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee Y, Kim M, Lee H. The measurement of stiffness for major muscles with shear wave elastography and myoton: a quantitative analysis study. Diagnostics (Basel) 2021;11:524. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33804273&dopt=Abstract 10.3390/diagnostics11030524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elkins MR, Moseley AM. Intention-to-treat analysis. J Physiother 2015;61:165–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26096012&dopt=Abstract 10.1016/j.jphys.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 38.Armijo-Olivo S, Warren S, Fuentes J, Magee DJ. Clinical relevance vs. statistical significance: using neck outcomes in patients with temporomandibular disorders as an example. Man Ther 2011;16:563–72. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21658987&dopt=Abstract 10.1016/j.math.2011.05.006 [DOI] [PubMed] [Google Scholar]
- 39.Lee S, Lee S, Jeong M, Oh H, Lee K. The effects of extracorporeal shock wave therapy on pain and range of motion in patients with adhesive capsulitis. J Phys Ther Sci 2017;29:1907–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29200621&dopt=Abstract 10.1589/jpts.29.1907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mariotto S, de Prati AC, Cavalieri E, Amelio E, Marlinghaus E, Suzuki H. Extracorporeal shock wave therapy in inflammatory diseases: molecular mechanism that triggers anti-inflammatory action. Curr Med Chem 2009;16:2366–72. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19601786&dopt=Abstract 10.2174/092986709788682119 [DOI] [PubMed] [Google Scholar]
- 41.Arribas-Romano A, Fernández-Carnero J, Molina-Rueda F, Angulo-Diaz-Parreño S, Navarro-Santana MJ. Efficacy of Physical Therapy on Nociceptive Pain Processing Alterations in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-analysis. Pain Med 2020;21:2502–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32100027&dopt=Abstract 10.1093/pm/pnz366 [DOI] [PubMed] [Google Scholar]
- 42.Yun SJ, Jin W, Cho NS, Ryu KN, Yoon YC, Cha JG, et al. Shear-wave and strain ultrasound elastography of the supraspinatus and infraspinatus tendons in patients with idiopathic adhesive capsulitis of the shoulder: a prospective case-control study. Korean J Radiol 2019;20:1176–85. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31270981&dopt=Abstract 10.3348/kjr.2018.0918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ 2005;331:1453–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16356983&dopt=Abstract 10.1136/bmj.331.7530.1453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gordon CM, Andrasik F, Schleip R, Birbaumer N, Rea M. Myofascial triggerpoint release (MTR) for treating chronic shoulder pain: A novel approach. J Bodyw Mov Ther 2016;20:614–22. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27634087&dopt=Abstract 10.1016/j.jbmt.2016.01.009 [DOI] [PubMed] [Google Scholar]
- 45.Choi JH. Effects of Kinesio Taping on Muscle Tone, Stiffness in Patients with Shoulder Pain. Korean Society of Physical Medicine. 2017;12:43–7. 10.13066/kspm.2017.12.3.43 [DOI]
- 46.Park SE, Kim YR, San Wang J. Immediate Effects of Maitland Joint Mobilization with Kinematic Taping on Shoulder Pain, ROM, and Muscle Tone in Subacromial Impingement Syndrome. Journal of International Academy of Physical Therapy Research. 2017;8:1206–10. 10.20540/JIAPTR.2017.8.3.1206 [DOI] [Google Scholar]
- 47.Luan S, Zhu ZM, Ruan JL, Lin CN, Ke SJ, Xin WJ, et al. Randomized trial on comparison of the efficacy of extracorporeal shock wave therapy and dry needling in myofascial trigger points. Am J Phys Med Rehabil 2019;98:677–84. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31318748&dopt=Abstract 10.1097/PHM.0000000000001173 [DOI] [PubMed] [Google Scholar]


