Abstract
BACKGROUND
Balance impairment and increased fall risk have been demonstrated in individuals with chronic obstructive pulmonary disease (COPD). However, studies investigating the effects of balance training especially when combined with pulmonary rehabilitation (PR) program in home-based setting are scarce.
AIM
To examine whether adding balance training to home-based pulmonary rehabilitation improves balance, fall risk, and disease-related symptoms in individuals with COPD.
DESIGN
Randomized, controlled, assessor-blinded trial with parallel two-group design.
SETTING
Home-based setting.
POPULATION
Forty-eight individuals diagnosed with COPD.
METHODS
Participants with COPD were randomly allocated to either a home-based PR or home-based balance training combined with PR (PR-BT) group (24 per group). Both groups exercised three days per week for eight-week. Primary outcomes were fall risk index and functional balance as measured by the Physiological Profile Assessment (PPA) and Timed Up and Go (TUG), respectively. Secondary outcomes were the Activities-specific Balance Confidence (ABC), Modified Medical Research Council dyspnea (mMRC), Six-Minute Walk Test (6MWT), and COPD assessment test (CAT). All outcome measures were assessed at baseline, post-intervention, and three-month follow-up.
RESULTS
All participants completed the trial, with no reported adverse events. At post-intervention, the PR-BT group demonstrated significantly greater improvements in PPA fall risk score (PR-BT: 1.1±0.8, PR: 2.4±1.5), TUG (PR-BT: 10.7±1.3, PR: 14.4±4.4 s) and these improvements remained at three-month follow-up (all P<0.01). The ABC, mMRC, and CAT scores were also significant better for the PR-BT than the PR group both after intervention and at three-month follow-up (all P<0.05).
CONCLUSIONS
Eight-week home-based balance and PR program is effective in improving balance as well as dyspnea, and well-being in individuals with COPD.
CLINICAL REHABILITATION IMPACT
Home-based balance and PR program is a promising approach for COPD rehabilitation especially in patients who are at risk of falls.
Key words: Pulmonary disease, chronic obstructive; Postural balance; Rehabilitation
Chronic obstructive pulmonary disease (COPD) is a major public health problem and the fourth leading cause of death worldwide.1 It is characterized by persistent respiratory symptoms and airflow limitation that are progressive and not fully reversible.2 In addition to respiratory dysfunctions, muscle dysfunction, decreased exercise capacity, impaired balance are well recognized in individuals with COPD.3-6 Recently, fall prevention has received a great deal of consideration due to the growing evidence of balance impairment and increased fall rates in this population. Fall incidence is approximately four times greater in COPD than healthy peers.7 Approximately 30-50% of individuals with COPD fall at least once during a six-month period.8 As falls often lead to reduced functional independence, increased morbidity and mortality,5, 9 it is imperative to determine effective fall prevention program in COPD.
It is well established that exercise which includes a balance component is an effective fall prevention strategy.10 Despite growing evidence of balance impairment in individuals with COPD, few studies have examined the effectiveness of balance training program in this population.11-17 Among existing studies, balance training was often included as part of the pulmonary rehabilitation (PR), implemented in center-based settings,11-14, 16, 17 and without follow-up period.11-14, 17 Recent systematic reviews concluded that PR with balance training has beneficial effect on balance, however, more research on fall risk and long-term intervention effects is still required.6, 18
While PR is proven to have clinically meaningful benefits, the uptake and adherence of the program is low.19 Transportation problem, travel distance, and time conflict have been reported as major barriers to participation in center-based rehabilitation.20 With this, home-based rehabilitation has been proposed as a viable alternative. A previous systematic review has demonstrated that home-based PR is feasible and effective for applying in COPD patients.21 However, studies investigating the effects of home-based balance training combined with PR program on balance and risk of falls are scarce. Based on our knowledge, only one single-group, non-randomized clinical trial of home-based fall prevention exercise was conducted and found that home-based balance exercise was feasible in promoting long term adherence, improving balance and fall risk in individuals with COPD.22 Randomized controlled trials (RCTs) are needed to confirm previous findings. Therefore, this study aimed to conduct a randomized controlled trial to examine the effects of home-based balance training combined with PR program on balance, fall risk, level of dyspnea, exercise capacity, and health-related Quality of Life (QoL) after training and at three-month follow-up period.
Materials and methods
Participants
Forty-eight COPD patients, aged ≥40 years, were recruited from outpatient clinics in community hospitals, between January 2019 and April 2020. Inclusion criteria included confirmed COPD diagnosis following standard guidelines2, 23 with a ratio of forced expiratory volume in the first second (FEV1) and forced vital capacity (FVC) with < lower limit of normal (LLN),24 ≥10 pack-year smoking history, and impaired balance (Timed-Up and Go [TUG]>11.2 seconds).25 Exclusion criteria were a history of home mechanical ventilator use, exacerbation within six months prior to recruitment, symptomatic cardiovascular diseases, neurological and musculoskeletal conditions that preclude training.
The study protocol was approved by the Human Ethical Review Board of the primary investigator’s institution (COA-AMSEC-61EX-036) and registered in ClinicalTrial.gov (TCTR20190103003). All eligible participants signed an informed consent form prior to enrollment in the study.
Study design
This was a stratified, RCT with assessor-blinded design. Participants were randomly allocated to either a home-based balance training combined with PR (PR-BT) or home-based PR (PR) group. Random sequence was generated by a computer generation with a 1:1 allocation ratio using a block size of four, stratified by Six-Minute Walk Distance (< or ≥350 m)26 and age (< or ≥70 years). The allocation sequence was carried out by a person not involved in the trial, and concealed in opaque, sealed envelopes.
Sample size calculation
The sample size calculation was based on our pilot study in which TUG yielded an effect size of 0.38. With 80% power and 5% type I error, a sample size of 40 was required to detect difference of TUG score between groups. Considering a potential dropout rate of 20%, a total sample size of 48 participants (24 per group) was enrolled into the study.
Interventions
Home-based PR program
The home-based PR program consisted of breathing, stretching, strengthening, endurance exercises, and education (i.e. COPD symptoms, coping skills, self-medication, and management of exacerbations).27, 28 The program started with diaphragmatic breathing exercise followed by stretching of eight muscle groups (i.e. shoulder, elbow, hip flexors and extensors, ankle dorsi- and plantar-flexors). Strengthening of upper- and lower-extremity muscles (i.e. biceps, triceps, pectoral, quadriceps, hip abductors and gluteus muscles) was performed by using resistance bands. The amount of resistance used was based on participant’s ability to complete 10 repetitions without compensatory movements. The strengthening exercise was progressed by increasing the number of sessions and repetitions. For endurance exercise, participants were asked to walk on flat ground for 15 minutes or as they could tolerate. The training progression for each exercise component is described in Table I. A self-management education session was provided on the first visit. The PR took approximately 45 minutes per session.
Table I. —Training progression for PR.
| Exercises | Level 1 | Level 2 | Level 3 |
|---|---|---|---|
| Breathing and Stretching exercise (warm-up) | 6 times/set, 5 sets/day (breathing exercise) 10 secs/time, 5 times/muscle group (8 muscle groups stretching exercise) |
||
| Strengthening exercise (6 muscle groups, resistance by elastic band) | 10 reps/set, 2 sets/muscle group | 10 reps/set, 3 sets/muscle group (adjusted resistance) | 12 reps/set, 3 sets/muscle group (adjusted resistance) |
| Endurance exercise (walking) | Intensity; Borg Scale 3-4 Duration; 15-min (or as tolerated) |
Intensity; Borg Scale 4-5 Duration; 20-min (or as tolerated) |
Intensity; Borg Scale 5-6 Duration; 25-min (or as tolerated) |
| Stretching exercise (cool-down) | 10 secs/time, 5 times/muscle group (8 muscle groups stretching exercise) | ||
| Self-management | on the first visit | ||
min: minute; reps: repetitions; secs: seconds.
Home-based balance training combined with PR program
Participants in the PR-BT undertook balance exercises in addition to the PR program. The balance training program consisted of stance exercises with different bases of support and surfaces, walking and functional exercises which were modified from a previous study.29 The training was progressed by decreasing hand support and increasing number of repetitions. The balance exercises with training progression prescribed in this study are shown in Table II. The balance training program took approximately 20 minutes per session.
Table II. —Training progression for balance exercise.
| Balance exercise | Level | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Narrow stance | 10 secs x 1 set, hands support | 10 secs x 2 sets, hands support | 10 secs x 2 sets, no support | 30 secs x 2 sets, no support |
| Narrow stance on foam | 10 secs x 1 set, hands support | 10 secs x 2 sets, hands support | 10 secs x 2 sets, no support | 30 secs x 2 sets, no support |
| Tandem stance | 10 secs x 1 set, hands support | 10 secs x 2 sets, hands support | 10 secs x 2 sets, no support | 30 secs x 2 sets, no support |
| Tandem stance on foam |
10 secs x 1 set, hands support | 10 secs x 2 sets, hands support | 10 secs x 2 sets, no support | 30 secs x 2 sets, no support |
| One leg stance | 10 secs/side x 1 set, hands support | 10 secs/side x 2 sets, hands support | 10 secs/side x 2 sets, no support | 30 secs/side x 1 set, no support |
| Toe stand | 10 secs x 1 set, hands support | 10 secs x 2 sets, hands support | 10 secs x 2 sets, no support | 30 secs x 2 sets, no support |
| Heel stand | 10 secs x 1 set, hands support | 10 secs x 2 sets, hands support | 10 secs x 2 sets, no support | 30 secs x 2 sets, no support |
| Sit-to-stand | 5 times x 1 set, hands support | 10 times x 1 set, hand support | 10 times x 1 set, no support | 10 times x 2 sets, no support |
| Narrow base walking | 5 steps x 1 round, hand support | 5 steps x 2 rounds, hand support | 5 steps x 1 round, no support | 5 steps x 2 rounds, no support |
| Narrow base walking backward | 5 steps x 1 round, hand support | 5 steps x 2 rounds, hand support | 5 steps x 1 round, no support | 5 steps x 2 rounds, no support |
reps: repetitions; secs: seconds.
Both groups exercised three days a week for eight-week. All participants were visited by a physical therapist four times; at the beginning of the trial to prescribe and set up exercises, and 2nd, 4th, and 6th week to progress the exercise programs. They also received an exercise poster, logbook, and a weekly phone call to assist and facilitate their exercises.
Baseline characteristics and outcome measures
Characteristics of the participants, spirometry, and all outcome measures were assessed using standard, structured protocols at baseline, post eight-week intervention, and three-month follow-up by trained assessors blinded to group assignment.
Primary outcome measures
The Physiological Profile Assessment (PPA) is a valid and reliable test used to determine physiological impairments contributing to falls.30 It consists of five sensorimotor components (i.e., visual contrast sensitivity, proprioception, quadriceps muscle strength, hand reaction time, and postural sway). The PPA composite score was calculated from the five subcomponents through the NeuRA FallScreen® (https://fbirc.neura.edu.au/fallscreen). Detailed descriptions of the PPA administration have been published.30 Low PPA composite scores indicate low risk of falling.
The TUG was used to assess functional balance. The TUG demonstrates excellent reliability in older adults with and without health conditions including COPD.31-33 Time taken to stand up from a standard chair, walk at a comfortable and safe pace for three meters, then turn and walk back to the chair, and sit down was measured. Two trials were performed and the best time was used for analysis.
Secondary outcome measures
The Activities-specific Balance Confidence (ABC) scale was used to determine the participant’s confidence in performing daily activities without losing balance. The confidence level is classified as low (scores ≤50%), medium (scores 50-80%), and high (scores >80%).34 The ABC scale demonstrates good internal consistency, validity, and reliability.34
The modified Medical Research Council dyspnea scale (mMRC) was used to identify disability level related to dyspnea. It is a Five-Likert Scale (0-4), with high scales indicate more breathlessness. The mMRC has good test-retest reliability.35
The Six-Minute Walk Test (6MWT) was used to evaluate exercise capacity.36 The 6MWT was conducted according to the standard guidelines.36 Participants walked with their own pace along a 30-meter corridor for six minutes twice, with 30-minute rest between each trial. The farthest distance of the two trials was used for analysis. The 6MWT has an excellent test-retest reliability.37
The COPD assessment test-Thai version (CAT-TH), a short, simple, valid and reliable self-administered questionnaire was used to determine health-related QoL.38 High CAT scores indicate low QoL.
Statistical analysis
Independent t-test and Chi-square test were performed to compare demographic characteristics between the two groups. A linear mixed model with Bonferroni post-hoc adjustment was used to analyze the differences between and within groups. Gender, %predicted FEV1, and baseline data were entered as covariates for between-group comparisons. A partial eta squared (ηp2) was calculated to determine effect size. An effect size of 0.01, 0.06 and 0.14 was regarded as small, medium, and large, respectively.39 The significance level was set at P<0.05. Data were analyzed using SPSS software (version 21.0, IBM Corporation, Chicago, IL, USA).
Results
Participant characteristics
Of 131 participants with COPD, 48 were eligible and randomized either to the PR-BT or PR group (Figure 1).
Figure 1.
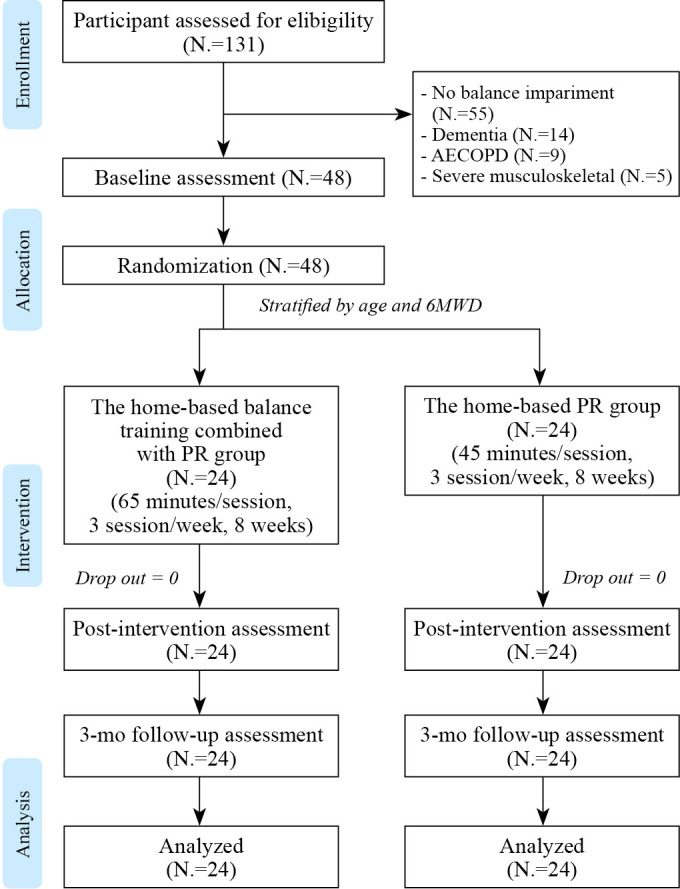
—Consolidation of trial flow diagram. AECOPD: acute exacerbation of chronic obstructive pulmonary disease; N., number; mo: month.
All participants completed the training program with no reported adverse events. The average exercise attendance rate was 98.1% and 97.6% for the PR-BT and PR, respectively. No differences in demographic characteristics between the two groups were observed at baseline, except for gender (Table III). The PR-BT showed a trend to have higher %predicted FEV1 than the PR (P=0.06). Therefore, gender and %predicted FEV1 were entered as covariates in between-group comparisons.
Table III. —Participants characteristics (N.=48).
| Variables | PR-BT (N.=24) |
PR (N.=24) |
P value* |
|---|---|---|---|
| Age (years) | 74.5±5.3 | 75.4±6.8 | 0.62 |
| Gender (male, %) | 20 (83) | 12 (50) | 0.01 |
| BMI (kg/m2) | 19.4±3.5 | 17.9±4.0 | 0.17 |
| FEV1 (L) | 0.8±0.4 | 0.7±0.4 | 0.42 |
| FVC (L) | 1.6±0.6 | 1.3±0.6 | 0.16 |
| FEV1/FVC (%) | 51.4±10.9 | 55.1±9.8 | 0.22 |
| Predicted FEV1 (%) | 62.9±17.4 | 53.3±17.7 | 0.06 |
| Stage of airflow obstruction (Mdn, IQR) | 2 (0.75) | 2 (1) | 0.23 |
| GOLD stage I (%) | 3 (13) | 3 (13) | - |
| GOLD stage II (%) | 15 (62) | 10 (42) | - |
| GOLD stage III (%) | 5 (21) | 9 (37) | - |
| GOLD stage IV (%) | 1 (4) | 2 (8) | - |
| mMRC dyspnea (Mdn, IQR) | 2 (2) | 2 (2) | 0.56 |
| Level 0 (N., %) | 3 (13) | 4 (17) | - |
| Level 1 (N., %) | 8 (33) | 3 (13) | - |
| Level 2 (N., %) | 5 (21) | 8 (33) | - |
| Level 3 (N., %) | 8 (33) | 9 (37) | - |
| Level 4 (N., %) | 0 (0) | 0 (0) | - |
| Current smoker (N., %) | 13 (54.17) | 13 (54.17) | 1.00 |
| Medication used (N., %) | 24 (100.0) | 24 (100.0) | 0.9 |
| 1 type (N.) | 11 | 13 | - |
| 2 types (N.) | 6 | 6 | - |
| 3 types (N.) | 6 | 4 | - |
| ≥4 types (N.) | 1 | 1 | - |
| Co-morbidity (N., %) | 13 (54) | 11 (46) | 0.9 |
| 1 disease (N.) | 6 | 6 | - |
| 2 diseases (N.) | 6 | 4 | - |
| 3 diseases (N.) | 1 | 1 | - |
The data are expressed as mean±standard deviation, otherwise as indicated. *Using Independent sample t-test, except for gender, current smoker, co-morbidity and medication (using χ2 Test) and mMRC dyspnea, and disease severity (using Mann-Whitney U test). BMI: Body Mass Index; GOLD: Global Initiative for Chronic Obstructive Lung Disease; PR: pulmonary rehabilitation group; PR-BT: balance training combined with PR group; IQR: interquartile range; kg: kilogram; m2: square meter; Mdn: median; N.: number.
Primary outcomes: balance performance and fall risk
Descriptive data for primary outcomes from baseline to post-intervention and follow-up period are summarized Table IV and results of analysis of changes between- and within-groups are presented in Table V.
Table IV. —Outcome variables at baseline, postintervention, 3-month follow-up.
| Outcome variables | PR-BT (N.=24) | PR (N.=24) | ||||
|---|---|---|---|---|---|---|
| Baseline | Postintervention | 3-month follow-up | Baseline | Postintervention | 3-month follow-up | |
| Primary outcomes | ||||||
| TUG (s) | 13.0±1.4 | 10.7±1.3 | 11.6±1.6 | 14.7±3.0 | 14.4±4.4 | 15.6±4.1 |
| PPA composite scores (points) | 1.8±1.2 | 1.1±0.8 | 1.1±1.0 | 2.6±1.2 | 2.4±1.5 | 2.8±1.2 |
| - Visual contrast sensitivity (dB) | 18.9±2.4 | 18.3±2.1 | 18.2±2.9 | 17.4±3.0 | 14.7±6.2 | 15.8±3.5 |
| - Proprioception (deg) | 2.5±1.1 | 1.9±1.0 | 1.3±0.6 | 2.0±0.9 | 2.0±1.2 | 2.2±1.0 |
| - Quadriceps strength (kg) | 20.2±6.0 | 21.8±7.1 | 24.1±6.6 | 15.5±4.5 | 17.8±7.2 | 16.9±6.8 |
| - Reaction time (ms) | 295.8±52.7 | 283.9±43.9 | 280.3±41.9 | 392.5±74.8 | 362.7±102.1 | 359.8±62.6 |
| - Sway path length (mm) | 197.4±114.8 | 121.4±39.3 | 144.9±70.7 | 188.0±89.6 | 156.3±79.0 | 213.0±125.9 |
| Secondary outcomes | ||||||
| ABC (%) | 85.7±15.6 | 90.8±9.3 | 94.5±6.2 | 69.2±28.4 | 70.1±24.7 | 69.1±26.0 |
| mMRC dyspnea (level) (Mdn, IQR) | 2 (2) | 0 (1) | 1 (1) | 2 (2) | 1.5 (1.75) | 2 (2) |
| 6MWD (m) | 297.9±37.4 | 331.0±47.4 | 325.3±65.1 | 236.0±103.8 | 265.6 ±93.0 | 239.4±107.3 |
| CAT-TH (points) | 15.6±7.7 | 9.2±5.4 | 10.8±5.6 | 16.5±6.0 | 17.5±7.6 | 16.0±5.9 |
The data are expressed as mean±standard deviation, otherwise as indicated. dB: decibel; deg: degree; IQR: interquartile range; kg: kilogram; Mdn: median; mm: millimeter; ms: millisecond; PR-BT: balance training combined with PR group; PR: pulmonary rehabilitation group; s: second.
Table V. —Means (standard errors) for changes within-group and adjusted means (95% confidence intervals) for differences in changes between-groups for all outcome variables.
| Outcome variables | Time frame | Changes within groups* | Changes between groups# | Effect size (partial η2) |
||||
|---|---|---|---|---|---|---|---|---|
| PR-BT (N.=24) | P-value | PR (N.=24) | P value | Difference | P value | |||
| Primary outcomes | ||||||||
| TUG (s) | Baseline- postintervention | -2.3 (0.6) | 0.002 | -0.3 (0.6) | 1.00 | -2.8 (-4.8 to -0.8) | 0.01 | 0.16 |
| Baseline-3-month follow-up | -1.4 (0.6) | 0.06 | 1.0 (0.6) | 0.23 | -2.8 (-4.6 to -1.1) | 0.002 | 0.20 | |
| Postintervention-3-month follow-up | 0.9 (0.4) | 0.09 | 1.2 (0.4) | 0.03 | - | - | - | |
| PPA composite scores (points) | Baseline- postintervention | -0.7 (0.3) | 0.01 | -0.2 (0.3) | 1.00 | -1.1 (-1.8 to -0.4) | 0.01 | 0.17 |
| Baseline-3-month follow-up | -0.7 (0.3) | 0.07 | 0.2 (0.3) | 1.00 | -1.4 (-2.0 to -0.7) | <0.001 | 0.28 | |
| Postintervention-3-month follow-up | 0 (0.3) | 1.00 | 0.4 (0.3) | 0.94 | - | - | - | |
| - Visual contrast sensitivity (dB) | Baseline- postintervention | -0.6 (0.8) | 0.88 | -2.7 (0.8) | 0.88 | 2.1 (-0.6 to 4.7) | 0.12 | 0.05 |
| Baseline-3-month follow-up | -0.7 (0.5) | 0.48 | -1.6 (0.5) | 0.48 | 0.6 (-0.8 to 2.1) | 0.38 | 0.02 | |
| Postintervention-3-month follow-up | -0.1 (0.8) | 1.00 | 1.1 (0.8) | 0.46 | - | - | - | |
| - Proprioception (deg) | Baseline- postintervention | -0.6 (0.3) | 0.11 | 0.0 (0.3) | 1.00 | -0.3 (-1.0 to 0.4) | 0.35 | 0.02 |
| Baseline-3-month follow-up | -1.2 (0.2) | <0.001 | 0.2 (0.2) | 1.00 | -1.0 (-1.5 to -0.5) | <0.001 | 0.25 | |
| Post-intervention-3-month follow-up | -0.6 (0.3) | 0.20 | 2.2 (0.3) | 1.00 | - | - | - | |
| - Quadriceps strength (kg) | Baseline- postintervention | 1.7 (1.1) | 1.00 | 2.3 (1.1) | 0.04 | -1.1 (-4.4 to 2.3) | 0.53 | 0.01 |
| Baseline-3-month follow-up | 4.0 (1.2) | 0.03 | 1.4 (1.2) | 0.39 | 3.0 (-0.5 to 6.5) | 0.09 | 0.06 | |
| Postintervention-3-month follow-up | 2.3 (1.0) | 0.07 | -0.9 (1.0) | 1.00 | - | - | - | |
| - Reaction time (ms) | Baseline- postintervention | -11.9 (19.2) | 0.69 | -29.8 (19.2) | 1.00 | -68.3 (-127.1 to -9.5) | 0.02 | 0.11 |
| Baseline-3-month follow-up | -15.6 (16.7) | 0.54 | -32.7 (16.7) | 0.46 | -80.8 (-119.4 to -42.2) | <0.001 | 0.29 | |
| Postintervention-3-month follow-up | -3.6 (16.6) | 1.00 | -2.9 (16.6) | 1.00 | - | - | - | |
| - Sway path length (mm) | Baseline- postintervention | -76.1 (20.8) | 0.001 | -31.7 (20.8) | 0.83 | -38.7 (-77.1 to -0.2) | 0.04 | 0.09 |
| Baseline-3-month follow-up | -52.5 (20.7) | 0.04 | 25.1 (20.7) | 0.63 | -69.3 (-127.8 to -12.9) | 0.02 | 0.13 | |
| Postintervention-3-month follow-up | 23.5 (22.7) | 0.65 | 56.7 (22.7) | 0.08 | - | - | - | |
| Secondary outcomes | ||||||||
| ABC (%) | Baseline- postintervention | 5.1 (3.8) | 0.26 | 1.0 (3.8) | 1.00 | 11.2 (1.8 to 20.6) | 0.02 | 0.12 |
| Baseline-3-month follow-up | 8.8 (4.1) | 0.04 | -0.1 (4.1) | 1.00 | 17.4 (7.0 to 27.8) | 0.002 | 0.21 | |
| Postintervention-3-month follow-up | 3.7 (3.7) | 0.95 | -1.0 (3.7) | 1.00 | - | - | - | |
| mMRC dyspnea (level) | Baseline- Postintervention | -1.0 (0.2) | <0.001 | -0.3 (0.2) | 0.02 | -1.1 (-1.5 to -0.6) | <0.001 | 0.32 |
| Baseline-3-month follow-up | -0.7 (0.2) | 0.01 | -0.04 (0.2) | 0.80 | -0.9 (-1.5 to -0.4) | 0.001 | 0.21 | |
| Postintervention-3-month follow-up | 0.3 (0.2) | 0.14 | -0.4 (0.2) | 1.00 | - | - | - | |
| 6MWD (m) | Baseline- Postintervention | 33.1 (10.4) | 0.01 | 29.6 (10.4) | 0.04 | 17.2 (-14.0 to 48.5) | 0.27 | 0.02 |
| Baseline-3-month follow-up | 27.4 (14.4) | 0.35 | 3.4 (14.4) | 1.00 | 32.0 (-12.8 to 76.9) | 0.16 | 0.05 | |
| Postintervention-3-month follow-up | -5.7 (12.0) | 1.00 | -26.2 (12.0) | 0.20 | - | - | - | |
| CAT-TH (points) | Baseline- Postintervention | -6.4 (1.3) | <0.001 | 1.0 (1.3) | 1.00 | -7.0 (-10.4 to -3.6) | <0.001 | 0.29 |
| Baseline-3-month follow-up | -4.8 (1.1) | <0.001 | -0.5 (1.1) | 1.00 | -4.3 (-7.1 to -1.5) | 0.004 | 0.18 | |
| Postintervention-3-month follow-up | 1.6 (1.0) | 0.30 | -1.5 (1.0) | 0.33 | - | - | - | |
#Adjusted for baseline values, gender, and %predictedFEV1. #For differences between-groups, negative values in TUG, PPA composite scores, proprioception, reaction time, sway path length, mMRC dyspnea, and CAT-TH favor the PR-BT group in the pairwise comparison. *For changes within-groups, negative values denote improvement, except for visual contrast sensitivity, quadriceps strength, ABC and 6MWD where positive values denote improvement. dB: decibel; deg: degree; kg: kilogram; mm: millimeter; ms: millisecond; PR-BT: balance training combined with PR group; PR: pulmonary rehabilitation group; s: second; η2: eta squared.
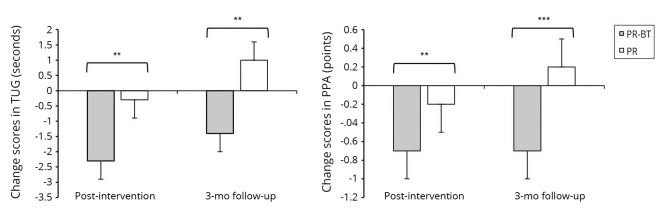
Figure 2 presents the change scores from baseline for TUG and PPA after eight-week intervention and three-month follow-up for the two groups. The PR-BT had significantly greater improvement in TUG and PPA scores than the PR at post-intervention and three-month follow-up (TUG P<0.01, ηp2=0.16 and 0.20, respectively; PPA P<0.01, ηp2=0.17 and 0.28, respectively). Analyses of the PPA subcomponents revealed that the PR-BT had significant lower sway path length and reaction time than the PR.
Figure 2.
—Differences in TUG and PPA between groups. mo: month; PR-BT: balance training combined with PR group; PR: pulmonary rehabilitation group. **P<0.01; ***P<0.001 adjusted for baseline data, gender, and %predicted FEV1.
Secondary outcomes: balance confidence, dyspnea, exercise capacity, and health-related QoL
Descriptive data for secondary outcomes from baseline to post-intervention and follow-up period are summarized Table IV and results of analysis of changes between- and within-groups are presented in Table V. The PR-BT had a significantly better ABC, mMRC and CAT-TH scores than the PR both after eight-week training and three-month follow-up (all P<0.05). No difference in the 6MWD was found between the two groups at any assessment time points.
Discussion
This randomized controlled trial provides evidence that home-based balance training combined with PR significantly improved balance and reduced fall risk compared to the home-based PR alone, and such improvement maintained for at least three-month after the intervention cessation. The effect size estimates indicate that adding balance training to home-based PR had large effect on balance and fall risk improvement, suggesting practical meaningfulness. Greater improvement was also evident for dyspnea symptom and quality of life. The training adherence was high with no adverse events. Thus, the present study demonstrates that the balance training combined with PR is effective for individuals with COPD to practice at home.
The findings that home-based balance training combined with PR improved balance and reduced fall risk while align with results from previous studies that were conducted in center-based settings,11-14, 16, 17 it further suggests the potential for implementing the intervention in home-based setting which could enhance adherence. Training adherence has been recognized as a significant factor contributing to sustainable rehabilitation.40, 41 Consistent with previous findings,12, 14 this study demonstrated that adding balance training to the PR program resulted in significant improvement in TUG performance. The change of TUG score in the present study is clinically meaningful as it exceeds the minimal clinically important difference identified in individuals with COPD.25
The significant decrease in PPA score indicates a greater fall risk reduction in the PR-BT compared to the PR. To our knowledge, no study has investigated the effect of home-based balance training combined with PR on physiological fall risk. The PPA evaluates key sensorimotor parameters critical for falls,30 thus it is useful in guiding the exercise prescription and monitoring the effects of the intervention on specific impairments.42 In this study, the PPA was used to further elucidate the underlying mediators by which the balance training program decreases fall risk. Results of subcomponent analyses suggest that decreased postural sway and reaction time may potentially contribute to fall risk reduction in the PR-BT.
It was expected that balance exercises in this study which comprised of sit to stand, one leg stand, stand with narrow base of support, stand on foam surface, functional strengthening, and walking should have promoted balance, lower extremity muscle strength, and proprioception. Nevertheless, the PPA subcomponents analyses revealed no significant improvement in quadriceps strength and knee proprioception after training. We postulated that the intensity of lower limb strength and proprioceptive training might have been sub-optimal as the balance training in this study was focused mainly on changing and reducing base of support. Known risk factors for falls include not only balance impairment but also lower limb muscle weakness, impaired proprioception, gait deficits;30, 43 and these impairments manifest in individuals with COPD.44 Lower limb muscle dysfunction, both at structural and functional levels are common in individuals with COPD due to multiple COPD-related factors including hypoxia, hypercapnia, systemic inflammation, and physical inactivity.3, 45 A previous study has suggested that training aimed to improve muscle strength should be prescribed to this population.11 Therefore, future study should consider adding lower limb strengthening exercises in the program and examine whether and to what extent such training program further reduce the risk of falling in individuals with COPD.
Analyses of the secondary outcomes (i.e., balance confidence, dyspnea symptom, exercise capacity, and quality of life) revealed that all outcomes except for exercise capacity were significantly better for the PR-BT than the PR at the end of the eight-week intervention and three-month follow-up. There were no significant differences in 6MWD between the two groups which is consistent with findings of a previous study.13 As improvement in health-related QoL is an important goal in COPD management, determining the impact of the intervention on health-related QoL would provide valuable clinical implications. In this study, CAT, a short, validated, COPD specific health-related QoL questionnaire was used and its finding indicated the superior effect of the balance training combined with PR, which is in accordance with findings of a previous study using the 36-Item Short-Form Health Survey.11 Improvement in balance, dyspnea symptoms, and exercise capacity is likely to contribute to improved health-related QoL. Specifically, such improvements might allow individuals with COPD to engage more in functional daily activities which in turn improve their quality of life. Several studies have reported the link between dyspnea symptoms, exercise capacity and quality of life of patients with COPD.38, 46
Limitations of the study
This study is one of the few that has investigated the effects of home-based balance and PR program on fall risk in individuals with COPD. While findings provide promising evidence for 1) using home-based approach to overcome the low adherence of the traditional center-based exercise, and 2) adding balance training to PR program to reduce fall risk, certain limitations in this study should be noted. First, only participants with stable COPD and without co-morbid conditions that affect training were included in the study. Thus, results on the adherence rate and effect of the intervention might be overestimated for typical individuals with COPD who often present with multiple co-morbidities. Second, although participants were asked to fill in the logbook immediately after their exercise sessions, some may have backfilled their logbooks which could result in recall issues. Finally, the sample size was not determined for PPA and its subcomponents, therefore the study may not have sufficient power to detect effects of the intervention program on PPA subcomponents.
Conclusions
The 8-week home-based balance and PR program is effective in improving balance performance, reducing risk of falls, and improving health-related quality of life of individuals with COPD. Given immense evidence of balance impairment and falls, this study highlights the value of additional balance training to the PR program in home-based setting. Further research is needed to determine the optimal intervention to maximize the benefits of the intervention program for individuals with COPD.
References
- 1.GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1859–922. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30415748&dopt=Abstract 10.1016/S0140-6736(18)32335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease [Internet]. USA: c2020 Available from https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf [cited 2020, May 21].
- 3.Roig M, Eng JJ, MacIntyre DL, Road JD, Reid WD. Deficits in muscle strength, mass, quality, and mobility in people with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev 2011;31:120–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21037481&dopt=Abstract 10.1097/HCR.0b013e3181f68ae4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beauchamp MK, Sibley KM, Lakhani B, Romano J, Mathur S, Goldstein RS, et al. Impairments in systems underlying control of balance in COPD. Chest 2012;141:1496–503. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22116798&dopt=Abstract 10.1378/chest.11-1708 [DOI] [PubMed] [Google Scholar]
- 5.Liwsrisakun C, Pothirat C, Chaiwong W, Bumroongkit C, Deesomchok A, Theerakittikul T, et al. Exercise performance as a predictor for balance impairment in COPD patients. Medicina (Kaunas) 2019;55:171. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31137581&dopt=Abstract 10.3390/medicina55050171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chuatrakoon B, Ngai SP, Sungkarat S, Uthaikhup S. Balance impairment and effectiveness of exercise intervention in chronic obstructive pulmonary disease-a systematic review. Arch Phys Med Rehabil 2020;101:1590–602. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32113975&dopt=Abstract 10.1016/j.apmr.2020.01.016 [DOI] [PubMed] [Google Scholar]
- 7.Loughran KJ, Atkinson G, Beauchamp MK, Dixon J, Martin D, Rahim S, et al. Balance impairment in individuals with COPD: a systematic review with meta-analysis. Thorax 2020;75:539–46. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32409612&dopt=Abstract 10.1136/thoraxjnl-2019-213608 [DOI] [PubMed] [Google Scholar]
- 8.Roig M, Eng JJ, MacIntyre DL, Road JD, FitzGerald JM, Burns J, et al. Falls in people with chronic obstructive pulmonary disease: an observational cohort study. Respir Med 2011;105:461–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20869227&dopt=Abstract 10.1016/j.rmed.2010.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17132052&dopt=Abstract 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 2017;51:1750–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27707740&dopt=Abstract 10.1136/bjsports-2016-096547 [DOI] [PubMed] [Google Scholar]
- 11.Beauchamp MK, Janaudis-Ferreira T, Parreira V, Romano JM, Woon L, Goldstein RS, et al. A randomized controlled trial of balance training during pulmonary rehabilitation for individuals with COPD. Chest 2013;144:1803–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23975185&dopt=Abstract 10.1378/chest.13-1093 [DOI] [PubMed] [Google Scholar]
- 12.Mkacher W, Mekki M, Tabka Z, Trabelsi Y. Effect of 6 months of balance training during pulmonary rehabilitation in patients with COPD. J Cardiopulm Rehabil Prev 2015;35:207–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25763921&dopt=Abstract 10.1097/HCR.0000000000000109 [DOI] [PubMed] [Google Scholar]
- 13.Mounir KM, Elserty NS, Obaya HE. Balance training: its influence on pulmonary rehabilitation. Bull Fac Phys Ther 2019;24:8–13. 10.4103/bfpt.bfpt_14_18 [DOI] [Google Scholar]
- 14.Marques A, Jácome C, Cruz J, Gabriel R, Figueiredo D. Effects of a pulmonary rehabilitation program with balance training on patients with COPD. J Cardiopulm Rehabil Prev 2015;35:154–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25517104&dopt=Abstract 10.1097/HCR.0000000000000097 [DOI] [PubMed] [Google Scholar]
- 15.Harrison SL, Beauchamp MK, Sibley K, Araujo T, Romano J, Goldstein RS, et al. Minimizing the evidence-practice gap - a prospective cohort study incorporating balance training into pulmonary rehabilitation for individuals with chronic obstructive pulmonary disease. BMC Pulm Med 2015;15:73. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26202647&dopt=Abstract 10.1186/s12890-015-0067-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harrison SL, Araujo T, Goldstein R, Brooks D. Balance measures over 12 months in individuals with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev 2019;39:E21–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31022009&dopt=Abstract 10.1097/HCR.0000000000000435 [DOI] [PubMed] [Google Scholar]
- 17.Jácome C, Marques A. Impact of pulmonary rehabilitation in subjects with mild COPD. Respir Care 2014;59:1577–82. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24803497&dopt=Abstract 10.4187/respcare.03091 [DOI] [PubMed] [Google Scholar]
- 18.Delbressine JM, Vaes AW, Goërtz YM, Sillen MJ, Kawagoshi A, Meijer K, et al. Effects of exercise-based interventions on fall risk and balance in patients with chronic obstructive pulmonary disease: a systematic review. J Cardiopulm Rehabil Prev 2020;40:152–63. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32355076&dopt=Abstract 10.1097/HCR.0000000000000513 [DOI] [PubMed] [Google Scholar]
- 19.Holland AE. Pulmonary rehabilitation for chronic obstructive pulmonary disease: has it peaked? Respirology 2019;24:103–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30467927&dopt=Abstract 10.1111/resp.13447 [DOI] [PubMed] [Google Scholar]
- 20.Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis 2011;8:89–99. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21596892&dopt=Abstract 10.1177/1479972310393756 [DOI] [PubMed] [Google Scholar]
- 21.Pinto D, Pereira S, Machado P, Padilha M, Sousa P. Home-based pulmonary rehabilitation and follow-up strategies in COPD patients: a systematic review. Eur Respir J Epub 2019. [Google Scholar]
- 22.Beauchamp MK, Ellerton C, Kirkwood R, Brooks D, Richardson J, Goldstein RS, et al. Feasibility of a 6-month home-based fall prevention exercise program in older adults with COPD. Int J Chron Obstruct Pulmon Dis 2021;16:1569–79. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34113090&dopt=Abstract 10.2147/COPD.S309537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. ATS/ERS Task Force . Standardisation of spirometry. Eur Respir J 2005;26:319–38. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16055882&dopt=Abstract 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 24.Dejsomritrutai W, Nana A, Maranetra KN, Chuaychoo B, Maneechotesuwan K, Wongsurakiat P, et al. Reference spirometric values for healthy lifetime nonsmokers in Thailand. J Med Assoc Thai 2000;83:457–66. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10863890&dopt=Abstract [PubMed] [Google Scholar]
- 25.Mesquita R, Wilke S, Smid DE, Janssen DJ, Franssen FM, Probst VS, et al. Measurement properties of the Timed Up & Go test in patients with COPD. Chron Respir Dis 2016;13:344–52. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27165963&dopt=Abstract 10.1177/1479972316647178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Celli B, Tetzlaff K, Criner G, Polkey MI, Sciurba F, Casaburi R, et al. COPD Biomarker Qualification Consortium ; Insights from the COPD Biomarker Qualification Consortium. The 6-minute-walk distance test as a chronic obstructive pulmonary disease stratification tool. Insights from the COPD biomarker qualification consortium. Am J Respir Crit Care Med 2016;194:1483–93. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27332504&dopt=Abstract 10.1164/rccm.201508-1653OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beauchamp MK, O’Hoski S, Goldstein RS, Brooks D. Effect of pulmonary rehabilitation on balance in persons with chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2010;91:1460–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20801268&dopt=Abstract 10.1016/j.apmr.2010.06.021 [DOI] [PubMed] [Google Scholar]
- 28.Ramos EM, de Toledo-Arruda AC, Fosco LC, Bonfim R, Bertolini GN, Guarnier FA, et al. The effects of elastic tubing-based resistance training compared with conventional resistance training in patients with moderate chronic obstructive pulmonary disease: a randomized clinical trial. Clin Rehabil 2014;28:1096–106. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24647863&dopt=Abstract 10.1177/0269215514527842 [DOI] [PubMed] [Google Scholar]
- 29.Yang XJ, Hill K, Moore K, Williams S, Dowson L, Borschmann K, et al. Effectiveness of a targeted exercise intervention in reversing older people’s mild balance dysfunction: a randomized controlled trial. Phys Ther 2012;92:24–37. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21979272&dopt=Abstract 10.2522/ptj.20100289 [DOI] [PubMed] [Google Scholar]
- 30.Lord SR, Menz HB, Tiedemann A. A physiological profile approach to falls risk assessment and prevention. Phys Ther 2003;83:237–52. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12620088&dopt=Abstract 10.1093/ptj/83.3.237 [DOI] [PubMed] [Google Scholar]
- 31.Marques A, Cruz J, Quina S, Regêncio M, Jácome C. Regêncio M, Jácome C. Reliability, agreement and minimal detectable change of the Timed Up & Go and the 10-meter walk tests in older patients with COPD. COPD 2016;13:279–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26643361&dopt=Abstract 10.3109/15412555.2015.1079816 [DOI] [PubMed] [Google Scholar]
- 32.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=1991946&dopt=Abstract 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- 33.Beauchamp MK. Balance assessment in people with COPD: an evidence-based guide. Chron Respir Dis 2019;16:1479973118820311. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30789019&dopt=Abstract 10.1177/1479973118820311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci 1995;50A:M28–34. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7814786&dopt=Abstract 10.1093/gerona/50A.1.M28 [DOI] [PubMed] [Google Scholar]
- 35.Mahler DA, Ward J, Waterman LA, McCusker C, ZuWallack R, Baird JC. Patient-reported dyspnea in COPD reliability and association with stage of disease. Chest 2009;136:1473–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19696126&dopt=Abstract 10.1378/chest.09-0934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories . ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12091180&dopt=Abstract 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 37.Hamilton DM, Haennel RG. Validity and reliability of the 6-minute walk test in a cardiac rehabilitation population. J Cardiopulm Rehabil 2000;20:156–64. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10860197&dopt=Abstract 10.1097/00008483-200005000-00003 [DOI] [PubMed] [Google Scholar]
- 38.Pothirat C, Kiatboonsri S, Chuchottaworn C. Validation of the new COPD assessment test translated into Thai in patients with chronic obstructive pulmonary disease. BMC Pulm Med 2014;14:193. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25471671&dopt=Abstract 10.1186/1471-2466-14-193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen J. Statistical power analysis for the behavioral sciences. New York: Hillsdale, NJ: L. Erlbaum Associates; 1988. [Google Scholar]
- 40.Guo SE, Bruce A. Improving understanding of and adherence to pulmonary rehabilitation in patients with COPD: a qualitative inquiry of patient and health professional perspectives. PLoS One 2014;9:e110835. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25357128&dopt=Abstract 10.1371/journal.pone.0110835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morris NR, Hill K, Walsh J, Sabapathy S. Exercise & Sports Science Australia (ESSA) position statement on exercise and chronic obstructive pulmonary disease. J Sci Med Sport 2021;24:52–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32928654&dopt=Abstract 10.1016/j.jsams.2020.08.007 [DOI] [PubMed] [Google Scholar]
- 42.Lord SR, Delbaere K, Gandevia SC. Use of a physiological profile to document motor impairment in ageing and in clinical groups. J Physiol 2016;594:4513–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26403457&dopt=Abstract 10.1113/JP271108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas 2013;75:51–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23523272&dopt=Abstract 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 44.Roig M, Eng JJ, Road JD, Reid WD. Falls in patients with chronic obstructive pulmonary disease: a call for further research. Respir Med 2009;103:1257–69. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19419852&dopt=Abstract 10.1016/j.rmed.2009.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax 2004;59:574–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15223864&dopt=Abstract 10.1136/thx.2003.019588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nonato NL, Díaz O, Nascimento OA, Dreyse J, Jardim JR, Lisboa C. Behavior of quality of life (SGRQ) in COPD patients according to BODE scores. Arch Bronconeumol 2015;51:315–21. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25622995&dopt=Abstract 10.1016/j.arbr.2015.04.001 [DOI] [PubMed] [Google Scholar]