INTRODUCTION
Chronic conditions, such as type 2 diabetes, have increased in prevalence and burden over the last few decades in the USA. The prevalence of diabetes is conservatively estimated to increase to 21% of the US adult population by 2050; nearly doubling a current estimation of 13%.1,2 Chronic disease management for conditions like type 2 diabetes requires monitoring, self-management, coaching, behavioral change, and resources for basic social needs that are critical during the 99.9% of time participants spend outside the health care system and inside their homes, communities, and workplaces.3–6 Increasingly, health care organizations are prioritizing multidisciplinary team-based interventions to improve diabetes care and outcomes for participants with complex health and social needs.7
Collaboration across medical care, social service, and public health agencies has shown great promise in addressing community health disparities and inequities that people with diabetes face.8–10 There are numerous examples of successful, health system–led community health initiatives and the beneficial role they have played in supporting care for people with chronic conditions.7,11 The role of non-healthcare, public health collaboratives in supporting diabetes and/or chronic disease-related outcomes of interest is less known. The state of New Jersey coordinates an innovative approach to support managed care by supporting a Regional Health Hub model where the hubs support state health priorities by “providing healthcare data infrastructure and analysis, supporting care management, and convening community stakeholders in close coordination with the state’s Office of Medicaid Innovation.”12
Four New Jersey Regional Health Hubs (Camden Coalition of Healthcare Providers, Health Coalition of Passaic County, Healthy Greater Newark, Trenton Health Team) support community and clinical care linkages across various sectors. Regional Health Hubs have been successful in engaging various stakeholders and convening coalitions and programs to address long-term health conditions.13–16 We present a case study of community and clinical care integration through the experience of a multi-faceted, community-based initiative in Trenton, NJ, focused on supporting patients with diabetes and barriers they are facing.
SETTING
Trenton Health Team (THT), a non-profit public health collaborative and Regional Health Hub in New Jersey, developed a community-wide initiative called the Capital City Diabetes Collaborative (CCDC). The CCDC addresses clinical and community barriers, at both individual and structural levels, that impact the health of people living with diabetes. The CCDC implements social, environmental, and health care interventions to support community residents living with diabetes in the Trenton area. THT prioritizes cross-sector partnerships with regional healthcare institutions, local social service and community-based agencies, and government entities to improve diabetes care and outcomes at both individual and structural levels. In addition, THT operates a regional Health Information Exchange (HIE) that consolidates updated, real-time clinical data from local healthcare providers into a single platform. The Trenton HIE receives clinical and utilization data from organizations throughout the area and shares this information back to hundreds of users.
Trenton has a higher rate of diabetes and poverty than both the state of New Jersey and federal averages.17 Trenton residents are predominantly African American and Latina/o/x (49.5% African American, 38.1% Latina/o/x, 12.1% non-Hispanic White).18
INTERVENTION DESCRIPTION
THT works as a trusted organization that can understand and represent community needs; engage with community service providers across health care, social care, and public health; and leverage data-driven and cross-sector activities to improve health across the city of Trenton, NJ. THT structured priorities outlined by community residents across three domains: Social, Healthcare, and Environmental. Strategies in each domain align with CCDC’s vision of improving diabetes outcomes and addressing gaps in resources.
SOCIAL AND HEALTHCARE
Establishing Diabetes Education Standards and Community-Based Self-Management Programs
Under the CCDC, THT coordinated with healthcare organizations to establish consistent diabetes education materials throughout the Trenton area. Materials emphasized patient health literacy, best practices in diabetes care, and local stakeholder feedback. The end-product was an English/Spanish diabetes self-management education booklet available to patients through local healthcare providers. THT also implemented an evidence-based peer-led, self-management program, Project Dulce, hosted in Trenton community settings.19,20
Community-Wide Clinical Care Coordination Team (C4T)
THT leveraged its C4T structure to guide CCDC clinical interventions and support population health activities. The C4T developed and coordinated standard protocols (e.g., blood glucose testing standards, social needs screening and referral activities, nutrition education) for diabetes care at Trenton primary care practices. Through C4T collaboration, THT worked with Capital Health to implement Intelligent Retinal Imaging System (IRIS) technology to improve diabetic retinopathy screening and diagnosis in primary care settings.
Care Management
The CCDC initiative includes a community-based care management team who coordinate care for patients from hospitals and clinics across Trenton. THT’s care management team is comprised of a director, nurse care manager, a licensed social worker, and seven community health workers. THT’s care management team is based on the standardized, University of Pennsylvania CHW model—Individualized Management for Patient-Centered Targets (IMPaCT).21 THT care management staff were trained to utilize the IMPaCT model by the Penn Center for Community Health Workers. THT staff completed additional trainings in other critical areas including behavioral health, substance use support and naloxone treatment, and COVID-19 safety and personal protective equipment protocols. Due to variability in patient needs, THT care management works with participants in varying levels of engagement. Some participants may require assistance with food assistance applications or with transportation for a particular medical appointment. Other participants may want consistent contact and support to navigate multiple medical and social needs. THT care management provides care to participants based on their preferences and to ensure support for unmet medical and social needs (e.g., transportation support, patient assistance programs to access medications and healthy food).
Social Needs Screening and Referral Implementation
With blended and braided funding streams, THT implemented a social needs screening and referral platform, NowPow. Based on key informant interviews and stakeholder engagement, THT recognized that a secure, cross-sector platform could facilitate both social needs screening and referral navigation for organizations from multiple sectors. NowPow is integrated into the HIE to provide access to screening and referral results and track notes from referral providers and receivers. In addition, THT utilizes population-level data in discussions with both clinical and social service sectors to address gaps in available resources.
ENVIRONMENTAL
Trenton Food Stakeholders
THT convenes a local committee, Trenton Food Stakeholders, which utilizes expertise across sectors to develop strategies that will improve food access in the community. The group developed an online, food resource guide available to the public and provides oversight on CCDC food insecurity and education initiatives.
Produce Distribution and Educational Programs (Produce Rx, “Cook Fresh, Feel Good”)
Through cross-sector collaboration with Snipes Farm and Education Center, THT and Snipes developed two programs to support food access among patients with diabetes: Produce Rx and Cook Fresh, Feel Good. Participants were referred via NowPow by THT’s care management team, community-based partners, and healthcare providers. In Produce Rx, three cohorts of up to 50 participants received free weekly produce, recipes, and diabetes education materials for 8 weeks from Snipes staff. In Cook Fresh, Feel Good, participants attend a 6-week cooking education program where patients with diabetes and their caregivers receive free weekly ingredients for each session. Participants also received fresh produce for 10 weeks following classes.
PROGRAM EVALUATION
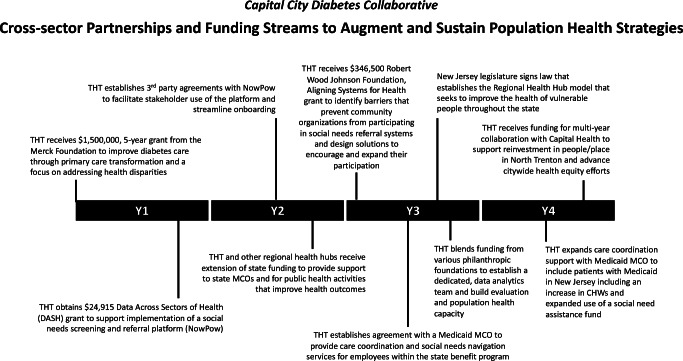
The authors utilized the RE-AIM evaluation framework constructs to assess reach and effectiveness of CCDC programs and interventions within three pillars: social, healthcare, and environmental.5 Evaluation metrics across each critical CCDC program were collected and compiled in Table 1. Examples of strategies to ensure sustainability of programs are highlighted in Figure 1.
Table 1.
Evaluation of the Capital City Diabetes Collaborative Through RE-AIM Framework
| Focus area | Intervention | Reach | Effectiveness | |||
|---|---|---|---|---|---|---|
| Social | Project Dulce | People involved in Project Dulce program (virtual and in-person) | 87 | Number of people who graduated from the Project Dulce program | 75 (86%) | |
| Survey results for Project Dulce Graduates | Pre (n=49) | Post (n=47) | ||||
| Reporting frequent physical activity, 4+ days/week | 45% | 64%* | ||||
| Reporting low consumption of sugary beverages, 0–2/day | 71% | 81%* | ||||
| Reporting following a healthy eating plan, 4+ days/week | 49% | 75%* | ||||
| Reporting eating 5+ servings fruit or vegetables, 4+ days/week | 53% | 68%* | ||||
| Healthcare | Care Management | People with diabetes enrolled by THT care management | 145 | Patients with an HbA1c <9% | Pre (n=54) | Post (n=54) |
| 28% | 46%* | |||||
| Intelligent Retinal Imaging System | People screened for diabetic retinopathy | 101 | Patients screened with early signs of diabetic retinopathy | 14 (14%) | ||
| NowPow, Social Needs Screening and Referral | People screened for social needs within THT care management and Project Dulce programs | 144 | Prevalence of at-risk social needs among those screened | 49% | ||
| Referrals initiated to address social needs | 89 | |||||
| Referrals successfully closed to address identified need | 89% | |||||
| Environmental | Produce Rx | People referred for produce support | 124 | People who received 2 or more produce distributions | 94 (76%) | |
| Cook Fresh, Feel Good | People supported by cooking class and food distribution program | 42 | Survey results for “Cook Fresh, Feel Good” program | Pre (n=42) | Post (n=36) | |
| Reporting confidence in choosing the best-priced form of fruits and vegetables | 57% | 69%* | ||||
| Reporting confidence in buying healthy foods for your family on a budget | 60% | 69%* | ||||
| Reporting confidence in helping family eat healthier | 74% | 84%* | ||||
| Reporting confidence in choosing the right foods to eat when hungry | 47% | 70%* | ||||
| Reporting confidence in understanding the recommended portions for someone with diabetes | 42% | 86%* | ||||
*Denotes statistically significant improvement (P<0.05)
Figure 1.
Cross-sector partnerships and funding streams to augment and sustain population health activities.
Reach
Between November 2016 and July 2021, THT reached 477 people with diabetes through social and healthcare programs such as care management, diabetic retinopathy screening, and Project Dulce (Table 1). During the COVID-19 pandemic (April 2020 to July 2021), THT and their partners supported 166 people with diabetes through food access initiatives.
Effectiveness
After attempting contact with 233 individuals, THT enrolled 145 individuals into their care management program. HbA1c was available in the Trenton HIE for 54 enrolled participants at pre- and post-enrollment . The proportion of care management participants that reported an HbA1c <9% increased by 18.5% post-enrollment (P<0.03).
Among the 101 IRIS screenings completed, 14 (14%) showed early signs of diabetic retinopathy. Primary care–based retinopathy screening provides an early opportunity to coordinate care (e.g., ophthalmologist) and further tailor diabetes education and self-management support for patients.
NowPow social needs screenings (n=144) highlighted the prevalence of unmet social needs in 49% of the care management and Project Dulce population. Staff initiated 89 referrals to address these unmet social needs and 89% of these referrals led to resources provided to patients.
Project Dulce staff measure program effectiveness based on uptake of patient education and those who graduated from the program. 86.2% of Project Dulce enrollees graduated from the Project Dulce curriculum. Comparison of pre-/post-surveys found those who completed Project Dulce classes were more likely to have improved self-management behaviors (e.g., physical activity, sugar-sweetened beverages, healthy eating, health knowledge) (Table 1).
To evaluate effectiveness of the produce distribution program, Produce Rx, staff considered the program to be successful if patients utilized the service at least twice. Seventy-six percent of those referred to the program met this goal.
Cook Fresh, Feel Good participants completed pre-/post-surveys to evaluate confidence in self-management behaviors. A two-sample z test of proportions was conducted among the 9 self-management confidence questions asked and statistically significant increase in the prevalence of healthy behaviors was observed in 5 of the 9 confidence questions, with the other 4 measures trending higher as well (Table 1).
Sustainability Strategies
Since the onset of the CCDC, THT developed additional partnerships and successfully applied for funding to maintain and scale various programs. Figure 1, a timeline of key partnerships and funding streams, provides illustrative examples of sustainability efforts that have increased staffing and resources to establish, augment, and sustain population health strategies that address long-standing health disparities. Grants and other funding sources (e.g., state Regional Health Hub, public health agencies, foundations, other city/county funding) have been critical to building the CCDC model and would likely be required for model replication in other communities. Insurance cannot cover all aspects of the model because the CCDC includes programs and services (e.g., food assistance, peer diabetes education support, CHW navigation support) that are typically not eligible for reimbursement. However, collaboration with healthcare systems and payors helped engage key sectors in identifying value and building long-term feasibility for new social, healthcare, and environmental interventions that support population health.
DISCUSSION
This case study provides a review of a multi-faceted initiative that required various implementation considerations and evaluation methods. THT’s CCDC evaluation highlights improvement across programs and early successes in implementing evidence-based practices. THT utilized key stakeholder feedback to guide the interventions offered and support provided to the community. THT’s success with cross-sector collaboration was evident in the variety of programs available to people with diabetes and underscores one critical reason why the CCDC was successful in reaching people with their services.
This study did have several limitations to note. First, given the nature of the CCDC’s individual programs and program-specific evaluation methodologies, we were unable to standardize the metrics that each program could be evaluated on and thus required several different process and outcomes metrics to report. Second, some programs were developed in response to the COVID-19 pandemic (e.g., Produce Rx) while others were developed before (e.g., Project Dulce, Care Management, IRIS). Authors were unable to adjust for the pandemic’s impact on utilization and engagement. Last, although the use of health information technology is a critical aspect of THT’s community health initiatives, we faced difficulties with data standardization and what was extractable from the Trenton HIE/NowPow systems. We were unable to evaluate the role of screening and referral for THT’s Care Management program, but we were able to evaluate the data in a less granular fashion (e.g., screening results among all patients with diabetes, referrals successfully closed among program participants). Further evaluation into the role of the care management team in supporting the unmet medical and social needs of patients is warranted.
For communities to address long-standing health disparities, cross-sector collaboration yields opportunities to leverage the social capital and resources available across sectors (e.g., healthcare, social services, government). THT established long-standing, cross-sector partnerships with regional healthcare institutions, local social service and community-based agencies, and government entities to improve diabetes care and outcomes at both individual and structural levels. THT has exemplified the role of an integrator organization through their efforts to develop, sustain, and expand CCDC initiatives.22 THT provides a model for other public health-focused partnerships that aim to improve chronic disease management and address both immediate socials needs and structural determinants of health.
Acknowledgements
The authors would like to thank Greg Paulson, Executive Director of Trenton Health Team, for his guidance and support throughout the manuscript process.
Funding
All authors acknowledge funding support from the Merck Foundation’s initiative Bridging the Gap: Reducing Disparities in Diabetes Care. THT co-authors (EM, CT, SA, AM, CRS, JB, KH) acknowledge funding from the Data Across Sectors for Health grant to support NowPow implementation and a Robert Wood Johnson Foundation, Aligning Systems for Health grant (#77404) to evaluate barriers to implementing social needs referral systems.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jacob P. Tanumihardjo, Email: jtanumihardjo@uchicago.edu.
Eric Schwartz, Email: ESchwartz2@capitalhealth.org.
References
- 1.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. [DOI] [PMC free article] [PubMed]
- 2.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020.
- 3.Gunter KE, Peek ME, Tanumihardjo JP, et al. Population health innovations and payment to address social needs among patients and communities with diabetes. Milbank Q. 2021;99(4):928-973. [DOI] [PMC free article] [PubMed]
- 4.Peek ME, Harmon SA, Scott SJ, et al. Culturally tailoring patient education and communication skills training to empower African-Americans with diabetes. Transl Behav Med. 2012;2(3):296-308. [DOI] [PMC free article] [PubMed]
- 5.Hessler D, Bowyer V, Gold R, Shields-Zeeman L, Cottrell E, Gottlieb LM. Bringing social context into diabetes care: intervening on social risks versus providing contextualized care. Curr Diab Rep. 2019;19(6):30. [DOI] [PubMed]
- 6.Rutledge SA, Masalovich S, Blacher RJ, Saunders MM. Diabetes self-management education programs in nonmetropolitan counties - United States, 2016. MMWR Surveill Summ. 2017;66(10):1-6. [DOI] [PMC free article] [PubMed]
- 7.Wang G, Gauthier R, Gunter KE, et al. Improving diabetes care through population health innovations and payments: lessons from Western Maryland. In: In preparation for Journal of General Internal Medicine Supplement; 2022. [DOI] [PMC free article] [PubMed]
- 8.Tung EL, Gunter KE, Bergeron NQ, Lindau ST, Chin MH, Peek ME. Cross-sector collaboration in the high-poverty setting: qualitative results from a community-based diabetes intervention. Health Serv Res. 2018;53(5):3416-3436. [DOI] [PMC free article] [PubMed]
- 9.Towe VL, Leviton L, Chandra A, Sloan JC, Tait M, Orleans T. Cross-sector collaborations and partnerships: essential ingredients to help shape health and well-being. Health Aff (Millwood). 2016;35(11):1964-1969. [DOI] [PubMed]
- 10.Johnston LM, Finegood DT. Cross-sector partnerships and public health: challenges and opportunities for addressing obesity and noncommunicable diseases through engagement with the private sector. Annu Rev Public Health. 2015;36:255-271. [DOI] [PubMed]
- 11.Tanumihardjo JP, Gunter, Kathryn E, Peek, Monica E. Integrating technology and human capital to address social needs: lessons to promote health equity in diabetes care. In. Vol 32: Journal of Health Care for the Poor and Underserved; 2021:241-261.
- 12.Raths D. N.J. Legislation Creates Four Regional Health Hubs. In: Healthcare Innovation; 2020.
- 13.Nash DB. Improving population health by working with communities. Am Health Drug Benefits. 2016;9(5):257-258. [PMC free article] [PubMed]
- 14.Perry RE, Stephenson C. Improving population health through collaboration and innovation. Popul Health Manag. 2013;16 Suppl 1:S34-37. [DOI] [PubMed]
- 15.Nicholson J. Community health collaboratives: supporting innovation in public policy, care delivery, and coordination. Popul Health Manag. 2013;16 Suppl 1:S2-3. [DOI] [PubMed]
- 16.Truchil A, Dravid N, Singer S, Martinez Z, Kuruna T, Waulters S. Lessons from the Camden Coalition of healthcare providers' first Medicaid shared savings performance evaluation. Popul Health Manag. 2018;21(4):278–284. doi: 10.1089/pop.2017.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trenton Health Team. Trenton Community Health Needs and Assets Assessment. https://trentonhealthteam.org/reports/tht-community-health-needs-assets-assessment-2019/. Published June 2019. Accessed 4 Apr 2022.
- 18.U.S. Cenus Bureau. QuickFacts, Population Estimates - Trenton, NJ. 2021. https://www.census.gov/quickfacts/trentoncitynewjersey. Accessed 4 Apr 2022.
- 19.Gilmer TP, Philis-Tsimikas A, Walker C. Outcomes of Project Dulce: a culturally specific diabetes management program. Ann Pharmacother. 2005;39(5):817-822. [DOI] [PubMed]
- 20.Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, Walker C, Gallo LC. Peer-led diabetes education programs in high-risk Mexican Americans improve glycemic control compared with standard approaches: a Project Dulce promotora randomized trial. Diabetes Care. 2011;34(9):1926-1931. [DOI] [PMC free article] [PubMed]
- 21.Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med. 2014;174(4):535-543. [DOI] [PubMed]
- 22.Billioux A, Conway PH, Alley DE. Addressing population health: integrators in the accountable health communities model. JAMA. 2017;318(19):1865-1866. [DOI] [PubMed]