Abstract
Dermatobia hominis , the human botfly, is native to South and Central America with cases of infestation seen in travelers to these areas. Myiasis is the cutaneous manifestation of larvae between two periods of molting (instar) and presents as a firm furuncular mass with a central pore that can be easily clinically overlooked. Ultrasound is useful in the diagnostic workup and has specific features and techniques to demonstrate live larva. We present a patient who acquired cutaneous furuncular myiasis caused by D. hominis , the human botfly, during her jungle trek in the Amazon forests in South America. Over 5 weeks, she developed a firm furuncular lesion with a central pore. Ultrasound revealed a hypoechoic mass with a hyperechoic oblong-shaped core that showed a fluid circulation, confirming the presence of a viable larva. Surgery was performed and a second-instar D. hominis larva was confirmed. We discuss the key ultrasound findings and management of cutaneous furuncular myiasis with the aim of raising awareness of this condition, adding to the growing body of literature likely associated with the re-opening of global travel routes.
Keywords: bubbling sign, cutaneous furuncular myiasis, musculoskeletal mass, ultrasound
Introduction
With increasing global travel and the rise of exotic holidays, diseases and parasitic infestations that were deemed uncommon and specific to continents can present with unusual signs and symptoms not uncommonly. Common investigative modalities are used in the initial investigation of presenting pathology. We describe a case of unusual parasitic infestation related t6o travel history and suggest characteristic signs for the diagnosis on ultrasound imaging.
Case Report
Clinical Presentation
A 39-year-old female patient was referred by a general surgeon to attend our musculoskeletal ultrasound clinic. She presented with a slow-growing painful lesion on her mid-lower leg, gradually increasing in size, over a month. Examination revealed a red, inflamed, elevated furuncular lesion with a central punctum. She gave a history of a possible insect bite that occurred on her recent jungle trek in the Amazon forests of Brazil, South America.
Investigations/Imaging Findings
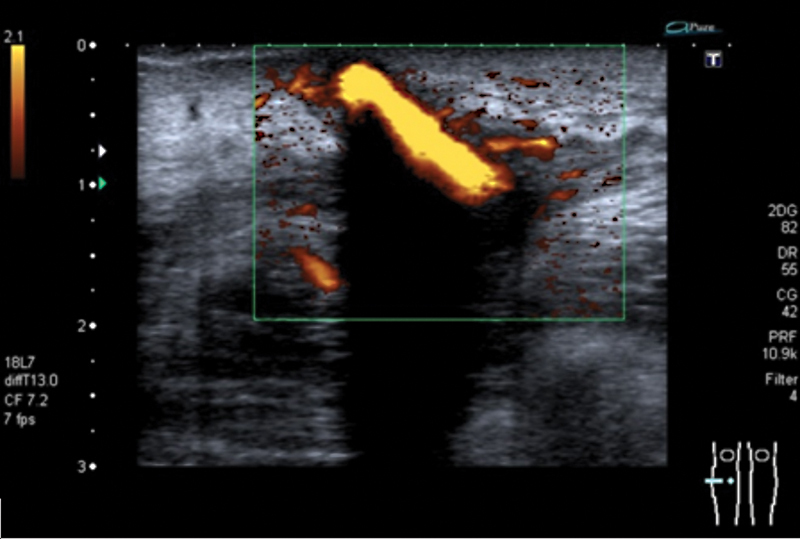
Video 1 Live video capture of a transverse ultrasound larval “bubbling phenomenon” due to transient asphyxia from occlusion of the central pore with ultrasound jelly.
Ultrasound, using a 6–15Hz linear array probe (GE Logiq 9, Bucks, United Kingdom) demonstrated a 2.1 cm (transverse plane) oblong-shaped hypoechoic mass with a hyperechoic structure in its core within the hypodermal fat, protruding into the dermal region that was identified as a layer of hyper-echogenicity. There was an associated posterior acoustic shadowing ( Figs. 1 – 2 ). Larval and fluid circulation were elicited within the central core on complete occlusion of the central pore with ultrasound jelly due to the ‘bubbling’ phenomenon from larval asphyxia ( Video 1 ).
Fig. 1.
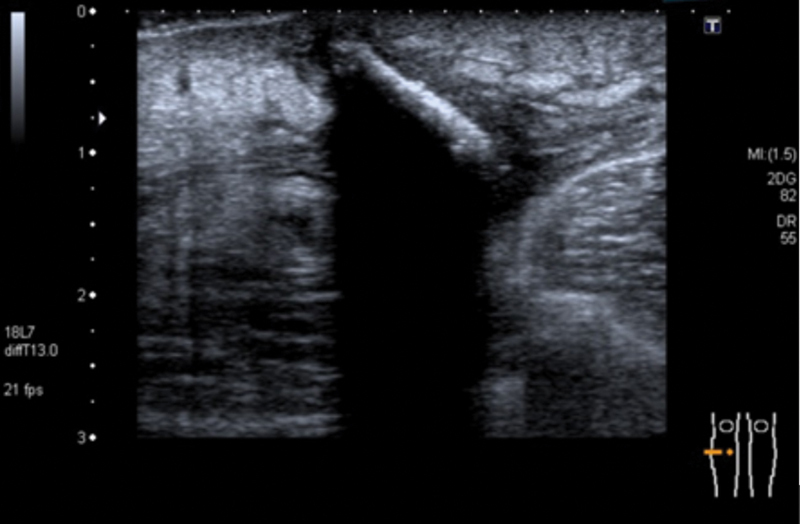
A 39-year-old female patient with a slowly growing painful lesion in the midcalf. Ultrasound with power Doppler (PwD) along the long axis of the lesion demonstrates an oblong hypoechoic mass with intense PwD signal and posterior acoustic shadowing.
Fig. 2.
A 39-year-old female patient with a slowly growing painful lesion in the midcalf. Ultrasound with power Doppler (PwD) along the long axis of the lesion demonstrates an oblong hypoechoic mass linear hyperechogenicity of a foreign body and posterior acoustic shadowing.
Treatment
Surgical excision of the lesion was performed with an excision debridement and a betadine wound wash. Debrided tissue specimen revealed an empty cavity where the larva was previously embedded and the second instar larva with rows of caudally pointing barb-like spines ( Fig. 3 ).
Fig. 3.
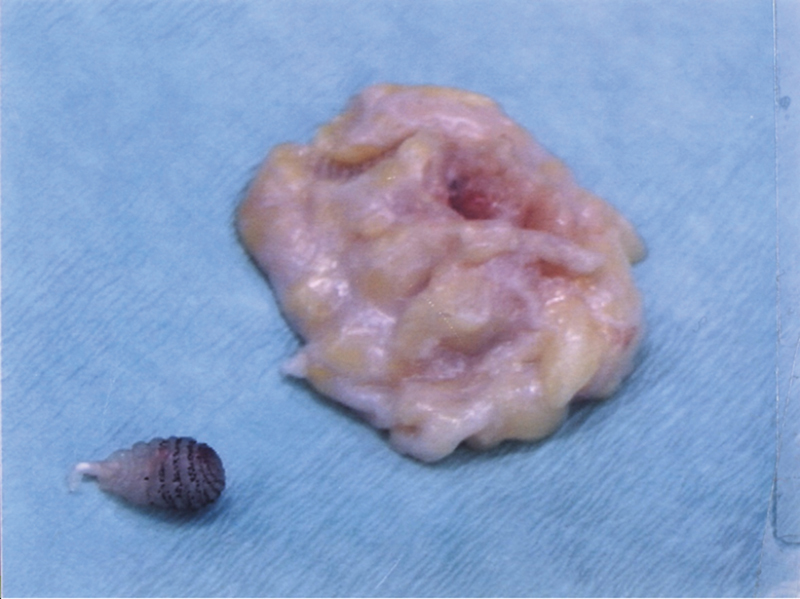
Gross specimen from surgical excision and debridement demonstrates the empty cavity and a bag-like structure that contained the larva. The larva is adjacent, black, and oval with rows of caudal barbs that allow embedding in the tissue.
Discussion
The patient's presentation elicited two key characteristic features of a cutaneous furuncular myiasis caused by D. hominis : a travel history to an endemic region and a 5-week slow-growing furuncular-like lesion with a central pore.
Myiasis is defined as an infestation of human tissue by larvae of different fly species within the arthropod order Diptera. In human myiasis, three families within the order Diptera cause myiasis: Calliphoridae (blow flies), Oestridae (bot and warble flies), and Sarcophagidae (flesh flies). Myiasis can be classified based on its anatomy or entomology. Anatomical classification divides myiasis into cutaneous, aural, urogenital, pulmonary, and intestinal, and is more useful in the clinical identification of fly species. In contrast, the entomological classification organizes myiasis into three different host–parasite relationships namely, obligatory, facultative, and accidental myiasis. Obligatory parasites rely on living tissues for larval development, whereas facultative larvae can develop on either living tissues or decaying tissue. When non-parasitic larvae are accidentally ingested or inhaled, it causes accidental myiasis. 1 2 3
Cutaneous myiasis is the most common type and occurs at the site of egg penetration. It can be further divided into furuncular, wound, migrating, and cavitary myiasis. D. hominis , the human botfly, is a common cause of furuncular cutaneous myiasis in a broad range of mammals. It is a type of obligatory parasite and is endemic to Central and South America where the climate is warm and moist. 3 4 In human hosts, D. hominis infestations often cause one to four furuncular lesions. Maier and Honigsmann provide a useful table to differentiate other flies that cause furuncular myiasis in humans, based on their clinical appearance and travel destinations. 2 The life cycle of D. hominis is well described in the literature. The third stage larva is most relevant in humans, forming a furuncle-like nodule with a central pore on the skin that allows for larval respiration and air exchange. 2 3 4 5
Diagnosis is made primarily on clinical grounds, with a particular focus on the patient's travel history and the ineffectiveness of antibiotic treatments. Common symptoms may include pruritus, piercing pain, serohemorrhagic discharge, non-healing wound, drilling sensation, or sensation of movement under the skin. Similar to a boil-like appearance, D. hominis myiasis is often mistaken for an arthropod bite, a pyoderma, an inflamed/infected epidermoid cyst, cutaneous larva migrans, cutaneous leishmaniasis, and tungiasis. Due to the need for larval respiration, bubbling will occur in a live larva when the lesion is submerged underwater. 2 3 Also, spontaneously emerging spiracles may be observed using a magnifying lens through the central punctum. 5 If the diagnosis remains uncertain, especially when the lesion is small and the punctum has not appeared, ultrasonography is a highly sensitive technique to diagnose the soft tissue presence of D. hominis larvae. 6
Both high-resolution grayscale and Doppler sonography have been useful in diagnosing suspected lesions caused by D. hominis . 5 6 According to Bouer et al, better definition images have been achieved using ultrasound scanners with > 15 MHz probes. 7 Our patient's sonography findings are in keeping with those described in previous studies: an oval-shaped structure with hypoechoic rim and hyperechoic center, presence of segmentations on longitudinal section, presence of spontaneous movements of viable larva, presence of fluid circulation within the larva and associated posterior acoustic shadowing artifact. In addition, Doppler ultrasound is highly sensitive in identifying the number and size of parasites, as well as, the stage of larval development with the stage 3 instar larvae located in the subdermal fat and its characteristic movement on asphyxia. 5 6 7 D. hominis myiasis is generally self-resolving and harmless. However, the infestation of skin covering the fontanelles of infants has resulted in fatal cerebral myiasis but this is rare. 8 Most common human complications of D. hominis myiasis are secondary infection and tetanus. 3
Furuncular myiasis can be managed by a variety of strategies. The main treatment consists of occlusion of the central pore to impede larval respiration, with an aim for the larva to migrate toward the skin surface. In unsuccessful cases, the larvae become asphyxiated and fail to emerge upward. The presence of caudally pointing spines and the larva's obovate shape makes manual retrieval difficult. Surgery is often required and is performed by making a cruciate incision under local anesthesia with lidocaine. Great care must be taken to ensure that there is a complete removal of the larva, including its debris, to prevent any severe inflammatory reaction. Alternatively, the use of topical ivermectin has been reported to be safe and effective against human myiasis. Systemic ivermectin can be used in rare widespread lesions. 2 3 4 6 The most frequent differential diagnoses are infected sebaceous cyst or a furuncle with associated lymphadenopathy. 9 The infected sebaceous cyst or furncle, would not demonstrate the “bubbling sign” on the closure of the punctum, if identifiable.
For travelers who visit areas where D. hominis is endemic, the main prevention strategy is to avoid or minimize direct contact with the responsible vector, most commonly a mosquito, fly, or tick. This can be achieved with proper long-sleeved clothing and skin covering, use of insect repellents, insecticides, window screens, and mosquito nettings. 4 6
Conclusion
In this report, we discuss the classification of myiasis, life cycle of D. hominis , differential diagnoses, ultrasound findings, and management of cutaneous furuncular myiasis. An increased awareness of this diagnosis, the importance of a travel history, and the specific techniques on ultrasound investigation are critical for the radiologist in this age of global frequent travel.
Learning Points
Raise awareness in physicians to have a high level of suspicion for cutaneous furuncular myiasis caused by D. hominis , a common travel-associated condition in Central and South America.
Thorough travel history and the ineffectiveness of antibiotics treatments are key to proper diagnosis and ultimately, treatment of cutaneous myiasis.
Ultrasound is a highly sensitive diagnostic technique in identifying the number of D. hominis larvae in the lesion.
Describe the sonographic features of D. hominis cutaneous myiasis with the “bubbling sign.”
Conflict of Interest None declared.
Informed Consent Statement
Written informed consent was obtained from the patient for publication of this case report, including accompanying images.
References
- 1.Ryan E, Hill D, Solomon T, Endy T, Aronson N. 10th ed. Amsterdam, Netherlands: Elsevier; 2019. Hunter's Tropical Medicine and Emerging Infectious Diseases. [Google Scholar]
- 2.Maier H, Hönigsmann H. Furuncular myiasis caused by Dermatobia hominis , the human botfly J Am Acad Dermatol 200450(2, Supp)S26–S30. [DOI] [PubMed] [Google Scholar]
- 3.McGraw T A, Turiansky G W.Cutaneous myiasis J Am Acad Dermatol 20085806907–926., quiz 927–929 [DOI] [PubMed] [Google Scholar]
- 4.Diaz J H. The epidemiology, diagnosis, management, and prevention of ectoparasitic diseases in travelers. J Travel Med. 2006;13(02):100–111. doi: 10.1111/j.1708-8305.2006.00021.x. [DOI] [PubMed] [Google Scholar]
- 5.Richter J, Schmitt M, Müller-Stöver I, Göbels K, Häussinger D. Sonographic detection of subcutaneous fly larvae in human myiasis. J Clin Ultrasound. 2008;36(03):169–173. doi: 10.1002/jcu.20410. [DOI] [PubMed] [Google Scholar]
- 6.Quintanilla-Cedillo M R, León-Ureña H, Contreras-Ruiz J, Arenas R. The value of Doppler ultrasound in diagnosis in 25 cases of furunculoid myiasis. Int J Dermatol. 2005;44(01):34–37. doi: 10.1111/j.1365-4632.2004.02471.x. [DOI] [PubMed] [Google Scholar]
- 7.Bouer M, Rodriguez-Bandera A I, Albizuri-Prado F, Lobos A, Gubeling W, Wortsman X. Real-time high-frequency colour Doppler ultrasound detection of cutaneous Dermatobia hominis myiasis . J Eur Acad Dermatol Venereol. 2016;30(12):e180–e181. doi: 10.1111/jdv.13492. [DOI] [PubMed] [Google Scholar]
- 8.Rossi M A, Zucoloto S. Fatal cerebral myiasis caused by the tropical warble fly, Dermatobia hominis. Am J Trop Med Hyg. 1973;22(02):267–269. doi: 10.4269/ajtmh.1973.22.267. [DOI] [PubMed] [Google Scholar]
- 9.Harbin L J, Khan M, Thompson E M, Goldin R D. A sebaceous cyst with a difference: Dermatobia hominis. J Clin Pathol. 2002;55(10):798–799. doi: 10.1136/jcp.55.10.798. [DOI] [PMC free article] [PubMed] [Google Scholar]


