Abstract
Purpose:
This article reports a case of presumed choroidal metastasis from an oncocytic carcinoma of the parotid gland.
Methods:
A 70-year-old man with history of an oncocytic carcinoma of the parotid gland presented owing to a 1-month history of progressive blurred central vision shortly after metastatic surveillance workup revealed liver, lung, and spine metastases. Fundus examination of the right eye showed a yellow choroidal mass surrounding the optic nerve and extending inferonasally, which is associated with subretinal fluid involving the foveal center. A-scan and B-scan ultrasonography were remarkable for a dome-shaped choroidal mass with medium-to-high internal reflectivity. Fluorescein angiography revealed pinpoint foci of hyperfluorescence over the choroidal lesion with late leakage. Magnetic resonance imaging of the brain showed evidence of metastatic disease to the cerebellum. While the patient underwent systemic chemotherapy, external beam radiotherapy was used to treat the eye.
Results:
Four months later, visual acuity improved, the tumor reduced in size, and the subretinal fluid resolved. Systemic workup disclosed no new metastases.
Conclusion:
Oncocytic carcinoma of the parotid gland is a rare and aggressive malignant neoplasm with frequent recurrences and distant metastases. The current case suggests that oncocytic carcinoma can metastasize to the choroid and, consequently, ocular metastasis surveillance is advised in these patients.
Keywords: choroidal metastasis, oncocytic carcinoma, parotid gland
Introduction
The choroid is the most common site for intraocular metastases. 1 However, salivary gland tumors rarely metastasize to the posterior uvea. Among the few reported cases of choroidal metastases arising from the salivary glands, adenoid cystic carcinoma (ACC) of the submandibular gland is the most common cause. 2 -7 Oncocytic carcinoma of the parotid gland is an extremely rare malignant neoplasm, 8 and to the best of our knowledge, an unknown cause of choroidal metastases. We report a case of presumed choroidal metastasis from an oncocytic carcinoma of the parotid gland.
Case Report
A 70-year-old man was referred after 1 month of progressive blurred central vision. His medical history was remarkable for an oncocytic carcinoma of the parotid gland that was diagnosed 18 months earlier, for which he underwent a left total parotidectomy with radical neck dissection, chemotherapy, and irradiation, owing to perineural invasion and extranodal extension. Routine metastatic surveillance workup showed good response to treatment until 1 month prior to ocular symptoms, when it revealed evidence of liver, lung, and spine metastases.
On presentation, visual acuity was 20/40 in the right eye and 20/20 in the left eye. There was no evidence of afferent pupillary defect. Intraocular pressure was normal for both eyes. Anterior segment examination did not reveal any other abnormalities. Fundus examination of the right eye showed a yellow choroidal mass measuring 5.0 × 6.0 disc diameters. It surrounded the optic nerve, extended inferonasally posterior to the equator, and was associated with subretinal fluid involving the foveal center (Figure 1). Fundus examination of the left eye was unremarkable. A-scan and B-scan ultrasonography showed a dome-shaped choroidal mass with medium-to-high internal reflectivity and an apical height of 2.0 mm (Figure 2). Fluorescein angiography revealed pinpoint foci of hyperfluorescence over the choroidal lesion with late leakage (Figure 3). Optical coherence tomography showed a large, homogenous, hyporeflective, elevated area of choroidal infiltration temporal to the optic nerve that was associated with overlying subretinal fluid involving the foveal center. Inner and outer retinal hyperreflective foci were also noted (Figure 4). Magnetic resonance imaging of the brain was remarkable for a small enhancing lesion in the T2-weighted-Fluid-Attenuated Inversion Recovery signal located in the left cerebellum, a consideration for intracranial metastasis.
Figure 1.

Wide-field fundus photography of the right eye showed a yellow choroidal mass surrounding the optic nerve and extending inferonasally posterior to the equator. Associated subretinal fluid temporal to the optic nerve was also noted.
Figure 2.

B-scan ultrasonography of the right eye showed a dome-shaped choroidal mass with medium-to-high internal reflectivity and an apical height of 2.0 mm.
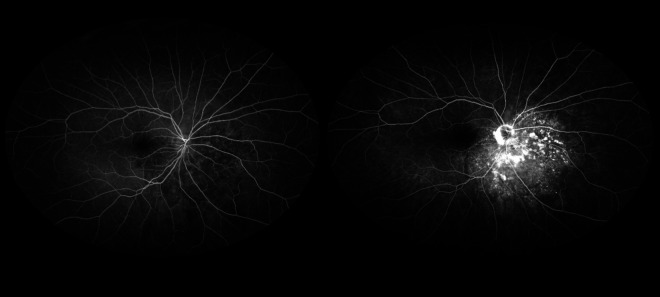
Figure 3.
Wide-field fluorescein angiography of the right eye (left) revealed early-phase pinpoint foci of hyperfluorescence over the choroidal lesion with (right) late leakage.
Figure 4.

Optical coherence tomography of the right eye showed a large, homogenous, hyporeflective, elevated area of choroidal infiltration temporal to the optic nerve, which is associated with overlying subretinal fluid involving the foveal center. Inner and outer retinal hyperreflective foci were also noted.
While receiving chemotherapy consisting of carboplatin plus 5-fluorouracil and cetuximab, the patient received a single intravitreal injection of bevacizumab (IVB) 1.25 mg/0.05 mL. Three weeks later, the subretinal fluid and choroidal mass remained unchanged. After discussing the findings with the patient, the decision to pursue a more definitive treatment was made. External beam radiotherapy (EBRT) (30 Gy) was then used to treat the eye and stereotactic radiation (25 Gy) to treat the cerebellum. Four months later, visual acuity improved to 20/30, the tumor reduced in size, and the subretinal fluid completely resolved. Systemic workup disclosed no new metastases.
Discussion
The most common cancers with metastasis to the uveal tract are breast (47%), lung (21%), and gastrointestinal tract (4%). 1 Uveal metastasis from the major salivary glands is rare. At present, only 9 case reports of uveal metastasis from major salivary glands have been published, including 7 cases originating from the submandibular gland and 2 from the parotid gland. 2 -7,9 -11
The parotid gland is the largest of the major salivary glands. Both cases of uveal metastasis originating from the parotid gland were ACCs. Montero et al 10 described a 64-year-old man with iris metastasis from an ACC of the parotid gland 5 years after diagnosis; Mouzari et al 9 reported a 52-year-old man who had a choroidal metastasis as an initial presentation of an ACC of the parotid gland. To our knowledge, the current case is the first one of an oncocytic carcinoma of the parotid gland with presumed metastasis to the choroid. A choroidal biopsy was deferred, given the patient’s relatively recent diagnosis of an oncocytic carcinoma confirmed by histopathologic and immunohistochemical examination following total parotidectomy.
Oncocytic carcinoma is an extremely rare malignant neoplasm accounting for less than 1% of all salivary gland tumors. 8 The malignant nature of this neoplasm can be recognized by its morphologic features and infiltrative growth with distant metastasis frequently reported. 12 Common reported sites include the lung, liver, kidney, mediastinum, thyroid gland, and bone. 13 However, choroidal metastasis has not been previously reported. Similar to prior reports, our patient also showed evidence of liver, lung, and spine metastases around the time that choroidal metastasis was diagnosed.
At present, radiotherapy remains a preferred treatment modality for choroidal metastasis, as data on IVBs for choroidal metastasis are scarce. 14 Among the previously mentioned cases of choroidal metastasis from ACC, 4 were treated with EBRT without IVB and showed favorable clinical response. 2,5 -7 Our patient was treated with a single IVB followed by EBRT in combination with systemic chemotherapy. Four months later, ophthalmic examination revealed improved visual function, reduced tumor size, and complete resolution of the secondary exudative retinal detachment. The results from the current case suggest that a single use of 1.25 mg/0.05 mL of bevacizumab may be insufficient despite receiving systemic chemotherapy, as no improvement in subretinal fluid was noted. Among previously reported cases of choroidal metastasis, multiple cycles of IVBs were administered, to which the patients responded favorably while undergoing systemic chemotherapy. 15,16 A recent report was unable to replicate similar favorable outcomes, although most patients were not initiated while simultaneously on systemic therapy. 17 Nonetheless, in the current case, EBRT in combination with systemic chemotherapy was sufficient to achieve tumor regression.
Oncocytic carcinoma of the parotid gland is a rare and aggressive malignant neoplasm with reported frequent recurrences and distant metastases. Although not previously reported, the current case suggests that oncocytic carcinoma can metastasize to the choroid and, consequently, ocular metastasis surveillance is advised in these patients.
Footnotes
Ethical Approval: This case report is institutional review board exempt and has been approved by all authors.
Statement of Informed Consent: Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104(8):1265–1276. doi:10.1016/s0161-6420(97)30148-1 [DOI] [PubMed] [Google Scholar]
- 2. Cai Q, Zhang R, Wu G, Dong X. Adenoid cystic carcinoma of submandibular salivary gland with late metastases to lung and choroid: a case report and literature review. J Oral Maxillofac Surg. 2014;72(9):1744–1755. doi:10.1016/j.joms.2014.04.011 [DOI] [PubMed] [Google Scholar]
- 3. Tang EW, Tsang CS, Li KK. Presumed bilateral choroidal metastases from mucoepidermoid carcinoma of the submandibular gland. Retin Cases Brief Rep. 2012;6(3):330–332. doi:10.1097/ICB.0b013e3182378deb [DOI] [PubMed] [Google Scholar]
- 4. John SS, Horo S, Braganza AD, Kuriakose T. Bilateral choroidal metastasis from carcinoma of the submandibular gland. Indian J Ophthalmol. 2008;56(1):75–76. doi:10.4103/0301-4738.37608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Demirci H, Vine AK, Elner VM. Choroidal metastasis from submandibular salivary gland adenoid cystic carcinoma. Ophthalmic Surg Lasers Imaging. 2008;39(1):57–59. doi:10.3928/15428877-20080101-03 [DOI] [PubMed] [Google Scholar]
- 6. Shields JA, Carvalho C, Shields CL, Singh AD, Wagner D. Bilateral choroidal metastasis from adenoid cystic carcinoma of the submandibular gland. Retina. 2000;20(4):406–407. doi:10.1097/00006982-200004000-00018 [DOI] [PubMed] [Google Scholar]
- 7. Jenrette JM, Fitzgeral RH. Metastasis to the choroid complicating adenoid cystic carcinoma. Arch Otolaryngol. 1982;108(8):509–510. doi:10.1001/archotol.1982.00790560047014 [DOI] [PubMed] [Google Scholar]
- 8. Huang JW, Zhang JG, Zhang J, et al. Oncocytic carcinoma of the parotid gland. Laryngoscope. 2013;123(2):381–385. doi:10.1002/lary.23696 [DOI] [PubMed] [Google Scholar]
- 9. Mouzari Y, Chekhchar M, Aitelhaj H, Bouia Y, et al. Bilateral choroidal metastasis as initial presentation of parotid gland adenoid cystic carcinoma. Immunological Disorders and Immunotherapy. 2017;2:1–3. [Google Scholar]
- 10. Montero J, Shields CL, Bianciotto C, Shields JA, Ehya H. Iris metastasis from adenoid cystic carcinoma of parotid gland. Cornea. 2011;30(3):351–353. doi:10.1097/ICO.0b013e3181e9af33 [DOI] [PubMed] [Google Scholar]
- 11. Sautter H. Bilateral choroidal metastases in a case of alveolar carcinoma (salivary gland carcinoma). Ophthalmologica. 1979;179:243–247. doi:10.1159/000308901 [DOI] [PubMed] [Google Scholar]
- 12. Giordano G, Gabrielli M, Gnetti L, Ferri T. Oncocytic carcinoma of parotid gland: a case report with clinical, immunohistochemical and ultrastructural features. World J Surg Oncol. 2006;4:54. doi:10.1186/1477-7819-4-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nakada M, Nishizaki K, Akagi H, Masuda Y, Yoshino T. Oncocytic carcinoma of the submandibular gland: a case report and literature review. J Oral Pathol Med. 1998;27(5):225–228. doi:10.1111/j.1600-0714.1998.tb01946.x [DOI] [PubMed] [Google Scholar]
- 14. Jardel P, Sauerwein W, Oliver T, et al. Management of choroidal metastases. Cancer Treat Rev. 2014;40:1119–1128. doi:10.1016/j.ctrv.2014.09.006 [DOI] [PubMed] [Google Scholar]
- 15. Singh N, Kulkarni P, Aggarwal AN, et al. Choroidal metastasis as a presenting manifestation of lung cancer: a report of 3 cases and systematic review of the literature. Medicine (Baltimore). 2012;91(4):179–194. doi:10.1097/MD.0b013e3182574a0b [DOI] [PubMed] [Google Scholar]
- 16. Maturu VN, Singh N, Bansal P, et al. Combination of intravitreal bevacizumab and systemic therapy for choroidal metastases from lung cancer: report of two cases and a systematic review of literature. Med Oncol. 2014;31(4):901. doi:10.1007/s12032-014-0901-z [DOI] [PubMed] [Google Scholar]
- 17. Maudgil A, Sears KS, Rundle PA, et al. Failure of intravitreal bevacizumab in the treatment of choroidal metastasis. Eye (Lond). 2015;29(5):707–711. doi:10.1038/eye.2015.21 [DOI] [PMC free article] [PubMed] [Google Scholar]