Abstract
As knowledge about the origin and morphologic characteristics of hip pain in the young adult has evolved, so too has the clinician’s ability to assess for various pathologies of the hip on radiographs, magnetic resonance imaging (MRI)/magnetic resonance arthrography (MRA), and computed tomography (CT). Because there is no algorithm at this time directly indicating what to do in more subtle hip morphologies, such as microinstability and borderline hip dysplasia (BHD), a skilled hip preservation specialist must use multiple imaging sources and know how to interpret them correctly. Imaging parameters used in the workup for hip dysplasia and BHD include the lateral center-edge angle, Tönnis angle, iliofemoral line, and presence of an upsloping lateral sourcil or everted labrum, among many others. The purpose of this narrative review was to detail various established criteria and parameters on anteroposterior pelvis plain radiographs, MRI/MRA, and CT that assist in defining the nature and severity of instability present in a dysplastic hip, thereby aiding in the development of patient-specific surgical treatment plans.
Keywords: imaging, magnetic resonance imaging, hip dysplasia, lateral center-edge angle, upsloping lateral sourcil
Our knowledge of the natural history of prearthritic hip conditions continues to evolve, with an improved understanding of the origin of premature hip failure occurring in the past 20 years. There is now an established body of evidence that femoroacetabular impingement (FAI) and hip dysplasia are the 2 main causes of early hip degeneration. 13 Therefore, there has been a recent focus on preserving the hip joint in these patients before end-stage degeneration.
Patients with frank acetabular hip dysplasia require bony realignment, with periacetabular osteotomy being the current bony procedure of choice. Although not universally accepted by all hip preservation specialists, there are a subset of patients who do not fall directly into the categories of frank dysplasia or normal, instead lying somewhere in between with a condition frequently termed “borderline hip dysplasia” (BHD). These patients with BHD present a challenging treatment decision, as some patients with BHD can benefit from arthroscopy alone, while others necessitate a periacetabular osteotomy 25 in order to obtain favorable long-term outcomes. Unfortunately, there is not a universal definition of BHD, and imaging parameters are instrumental in determining which of these patients may be at higher risk of failure with an arthroscopy-only treatment approach. 25 Given that BHD thus encompasses both unstable and stable hips, it becomes paramount for the clinician to have a broad understanding of the radiographic parameters that can assist in deciphering between the 2 conditions.
As knowledge about the origin and morphologic characteristics of hip pain in the young adult has evolved, so too has the clinician’s ability to assess for various pathologies of the hip on radiographs, magnetic resonance imaging (MRI)/magnetic resonance arthrography (MRA), and computed tomography (CT). Since there is no algorithm at this time directly indicating what to do in more subtle hip morphologies, such as microinstability and BHD, a skilled hip preservation specialist must use multiple imaging sources and know how to interpret them correctly. The ability to analyze imaging modalities of the hip and combine these findings with a patient’s clinical history and examination to determine the correct diagnoses can be challenging, especially in cases of BHD or microinstability. That said, the interpretation of imaging and the final global synthesis of a patient’s hip symptoms can be affected by a clinician’s training and experience. In addition, caution must be taken when employing various hip imaging parameters to define hip instability, as many studies published on this topic have limitations such as retrospective study designs and a lack of proper controls.
The purpose of this narrative review was to detail various acceptable findings and parameters on plain anteroposterior (AP) radiographs, MRI/MRA, and CT that assist in defining the nature and severity of instability present in a dysplastic hip, thereby aiding in the development of patient-specific surgical treatment plans.
RADIOGRAPHIC PARAMETERS
Proper technique is critically important for accurate interpretation of findings on plain AP pelvis radiographs. 55 A true AP view of the pelvis is achieved with the patient in the supine or standing position, with a tube-to-image distance of 120 cm and a photon beam centered midway between the pubic symphysis and the top of the iliac crests. The craniocaudal angle of the beam is set to a distance of 1 to 3 cm from the superior aspect of the pubic symphysis and the sacrococcygeal joint. Proper femoral positioning is recognized when the greater trochanter is seen laterally and the lesser trochanter is partially superimposed on the femoral neck. The rotational image quality is ensured when the obturator rings and acetabular teardrops are symmetric and the midsacral line aligns with the pubic symphysis. Although AP pelvis radiographs are often obtained in the supine position, this may not represent the functional position of the pelvis, and standing radiographs better incorporate the dynamic influences of the periarticular musculature. In addition, technically suboptimal radiographs, especially with regard to nonanatomic pelvic tilt and rotation, have been shown to result in overestimation of abnormal acetabular morphology. 15,18,40 Pelvic tilt and rotation, acetabular version, leg length discrepancy, and previous surgical procedures about the pelvis are all important factors that can alter the interpretation of imaging findings.
Lateral Center-Edge Angle
An estimation of acetabular coverage of the femoral head can be made with measurement of the lateral center-edge angle (LCEA), also called the center-edge angle of Wiberg. 56 It most specifically defines the superolateral acetabular coverage of the femoral head, whereas anterior coverage is best assessed by the anterior center-edge angle, which is measured on a false-profile view of the hip or by axial CT. The LCEA is an angle formed by 2 lines. Both lines originate at the center of the femoral head, with one line extending superiorly and perpendicular to the transverse axis of the pelvis and the other line passing through the lateral edge of the acetabulum. This latter line was more specifically defined to intersect the most superolateral point of the sclerotic weightbearing zone of the acetabulum (sourcil). This refinement of the LCEA was proposed by Ogata et al, 34 who noted that acetabular retroversion in patients with dysplasia yields an overestimate of the functional lateral coverage with the conventional technique of measuring LCEA. Utilization of the Wiberg method has been found to overestimate acetabular coverage by an average of 4° because of inclusion of a bony area that functions as the labral base but does not come into contact with the femoral head, thereby not contributing directly to coverage or bony area that is located posteriorly to the true 12-o’clock position (Figure 1). An LCEA <25° is associated with inadequate femoral head coverage, and values >40° are conversely indicative of overcoverage and pincer-type FAI. Depending on the surgeon, an LCEA of 20° to 25° defines BHD, whereas other surgeons define BHD as 18° to 25°. 25
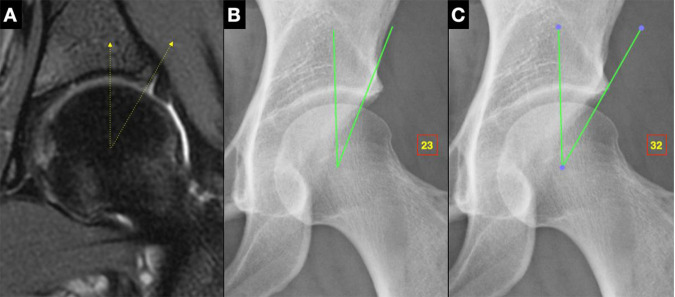
Figure 1.
Lateral center-edge angle (LCEA). The LCEA is an angle formed by a line from the center of the femoral head extending superiorly and perpendicular to the transverse axis of the pelvis and a line from the center of the femoral head through the lateral acetabular rim. (A) Coronal T2 fat-saturated magnetic resonance arthrography illustrating how the LCEA of Wiberg includes part of the labral base that is not actually part of the weightbearing zone. (B and C) Anteroposterior pelvis radiographs illustrating the difference in LCEA as measured by the (B) Ogata method 34 versus (C) Wiberg method. 56
Tönnis Angle
Evaluation of acetabular inclination is one of the most useful and important parameters performed on an AP pelvis radiograph. The Tönnis angle, also referred to as the sourcil angle, acetabular roof obliquity, and horizontal toit externe angle, is the most commonly used measurement for and broadly classifies acetabular inclination. The angle is measured by drawing a horizontal line, parallel to the transverse pelvic axis, at the most medial edge of the sclerotic sourcil and then making a second line extending out from the medial edge to the lateral-most aspect of the sourcil. This angle classifies acetabular inclination into normal, increased, or decreased categories. A normal Tönnis angle is between 0° and 10°. Generally, >10° denotes structural instability and hip dysplasia and <0° places the hip at increased risk for pincer-type FAI.
Sourcil Morphology
A normal sourcil has a concave shape that mirrors, and is congruent with, the femoral head. In dysplasia, the sourcil may have a flattened, incongruous shape creating laterally directed shear forces within the hip joint and/or give rise to labral eversion, which compromises labral suction seal. Klaue et al 20 coined the morphology of some dysplastic acetabuli as having a “short roof,” in which they noted that the acetabular weightbearing zone is short yet remains congruent with the femoral head. This term has been modified to “flat roof,” as roof length is short in most cases of dysplasia because of low volume of the acetabulum. While many instances have an upsloping roof with a sourcil angle >10°, there is a subset with a flat roof that can present with a normal sourcil angle. 57 The sourcil morphology must be taken into consideration when measuring LCEA for assessing true functional lateral coverage in cases of suspected instability.
Upsloping Lateral Sourcil
An upsloping lateral sourcil (ULS) is defined as a caudal-to-cranial inclination of the middle to far lateral aspect of the acetabular sourcil with loss of the normal lateral acetabular concavity on an AP pelvis radiograph (Figure 2). Nearly 90% of patients with frank hip dysplasia were found to have a ULS in a study conducted by Wong et al. 57 Similarly, 3 times as many patients with BHD were found to also have a ULS compared with those with normal acetabular coverage.
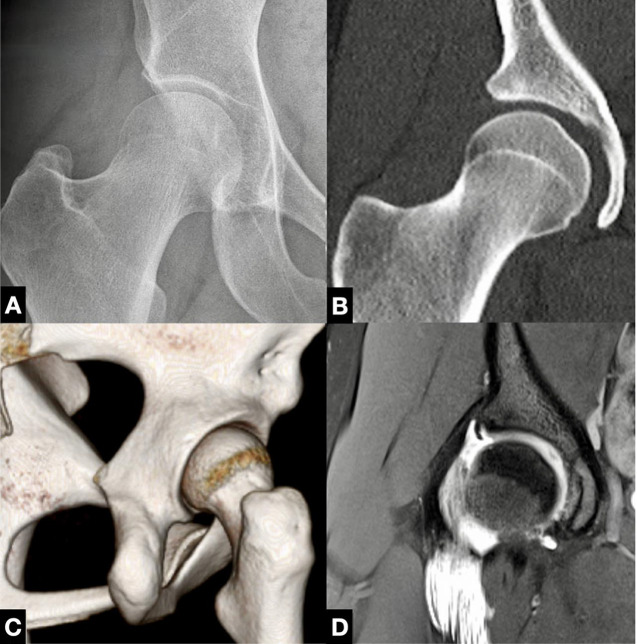
Figure 2.
Upsloping lateral sourcil (ULS). (A) A ULS is a caudal-to-cranial inclination of the middle to far lateral aspect of the acetabular sourcil with loss of the normal lateral acetabular concavity on an anteroposterior pelvis radiograph. This can be visualized on (B and C) computed tomography as well as (D) magnetic resonance imaging.
Sharp’s Angle
Although less commonly used, another measurement of acetabular inclination is Sharp’s angle. 44 This angle provides an estimate of total acetabular inclination. This angle is formed with the vertex at the distal point of the acetabular teardrop and one arm in line with the transverse pelvic axis and the other arm extending out to the superolateral rim of the acetabulum. A Sharp’s angle ≥45° is associated with acetabular dysplasia.
Acetabular Version
Acetabular version is associated with hip pathology, with anteversion strongly correlated to developmental dysplasia and retroversion traditionally correlated to pincer-type FAI. However, it is instrumental to understand that the acetabular version, whether assessed on radiograph or CT, is essentially an indication of the relationship between the anterior and posterior walls. The version cannot capture the volume of the socket and, as a result, can give an inaccurate representation in cases of abnormal acetabular volume such as in dysplasia or global overcoverage. A common example is misinterpreted retroversion in a hypovolemic socket because of a deficient posterior wall/coverage rather than anterior overcoverage. Numerous parameters have been proposed to determine acetabular version on AP pelvis radiographs. Importantly, pelvic tilt has been shown to significantly impact acetabular version on radiographic imaging. An increase in (more positive) pelvic tilt will reduce acetabular version, and a decreased (or negative) pelvic tilt may falsely elevate acetabular anteversion.
Neck Axis Distance
Neck axis distance is measured on the AP pelvis radiograph by first drawing a line (line N) down the axis of the femoral neck that bisects the center of a best-fit circle about the femoral head. The distance between the anterior wall and the posterior wall along line N is then measured. A measurement ≥14 mm is associated with excessive anteversion. 32
Shenton Line
The Shenton line is a commonly used qualitative radiographic marker of acetabular dysplasia. 38 It is defined as an unbroken arch formed by the top of the obturator foramen and the inner side of the femoral neck. The Shenton line is determined to be broken, suggesting superolateral hip subluxation, if the inferior femoral neck projection is cephalad to the superior arch of the obturator foramen. A break in the Shenton line is indicative of more severe forms of acetabular dysplasia with a superolateral hip center, whereas a continuous line does not exclude an unstable hip.
Joint-Space Width
Joint-space width (JSW) is defined as the distance between the bony contour of the acetabular rim and femoral head in 2 locations on the AP radiograph: the lateral JSW is measured at the lateral sourcil as a continuous line from the outer ilium cortical lip, and the medial JSW is measured at a point halfway between the lateral and medial sourcil borders. The average JSW in a prearthritic hip is between 4 and 4.5 mm. 22 However, significant variability in normal JSW exists. 27 A study by Lequesne et al 27 showed that JSW varied from 3 to 8 mm at the superolateral edge and from 2 to 6 mm at the superomedial edge. Furthermore, up to 5.9% of healthy individuals in this study demonstrated right to left asymmetry of JSW. Frankly dysplastic and borderline dysplastic hips have higher JSW than normal and pincer-shaped hips. 22 In a study by Kraeutler et al, 22 the lateral JSWs in hips with frank dysplasia were 5.0 and 4.8 mm in BHD compared with 4.5 mm in hips with normal acetabular coverage and 4.3 mm in pincer-type hips.
Iliofemoral Line
The iliofemoral line is defined as the smooth line extending from the apex of the concavity of the lateral femoral neck through the inner cortical lip of the ilium on an AP pelvis radiograph. 21 The percentage medialization of the iliofemoral line is defined as the horizontal distance of the exposed femoral head lateral to the iliofemoral line relative to the horizontal femoral head width at the center of the femoral head. Values of percent medialization exceeding 22% represent frank hip dysplasia, while those between 15% and 22% equate with borderline dysplasia. 21
Femoral Head Extrusion Index
A more complex, but very useful, quantification of acetabular coverage is called the femoral head extrusion index and is the percentage of the femoral head not covered by the acetabulum. 16 This percentage is calculated by measuring the width of the femoral head that lies lateral to the lateral extent of the acetabulum (A), dividing it by the total horizontal width of the covered femoral head (B), and multiplying the quotient by 100 ([A/B] × 100). A normal hip was defined as having an extrusion index of <25%. Similar to this measurement is “femoral head coverage,” which measures the distance between the medial cortex of the femoral head and the lateral acetabular rim divided by the diameter of the femoral head. In this calculation, a value <75% is pathologic and indicates undercoverage or potential dysplasia. Of note, this parameter does not take into account the morphology of the sourcil; hence, a normal index may be measured, although an incongruous sourcil may represent continued instability.
Cliff Sign
In order to assess for the presence of a cliff sign, a perfect circle is created around the femoral head on an AP pelvis radiograph, and if the lateral femoral head does not completely fill the perfect circle, this is considered a positive cliff sign. 35 In the study by Packer et al 35 describing this parameter, a positive cliff sign was associated with microinstability of the hip joint, which was defined by intraoperative findings of either minimal traction required to distract the hip, lack of hip reduction after release of negative intra-articular pressure, or straight anterior or straight lateral labral tears. 35 Similar to many other parameters, note should be made that a positive cliff sign can exist in patients without instability.
Femoroepiphyseal Acetabular Roof Index
The femoroepiphyseal acetabular roof (FEAR) index is measured by drawing a straight line along the central portion of the femoral head physeal scar (Figure 3). 58 A second line is drawn from the most medial to lateral portions of the sclerosis of the sourcil. A positive FEAR index is indicated by a laterally directed angle. A FEAR index of <5° represents a stable hip in patients with borderline dysplasia.
Figure 3.
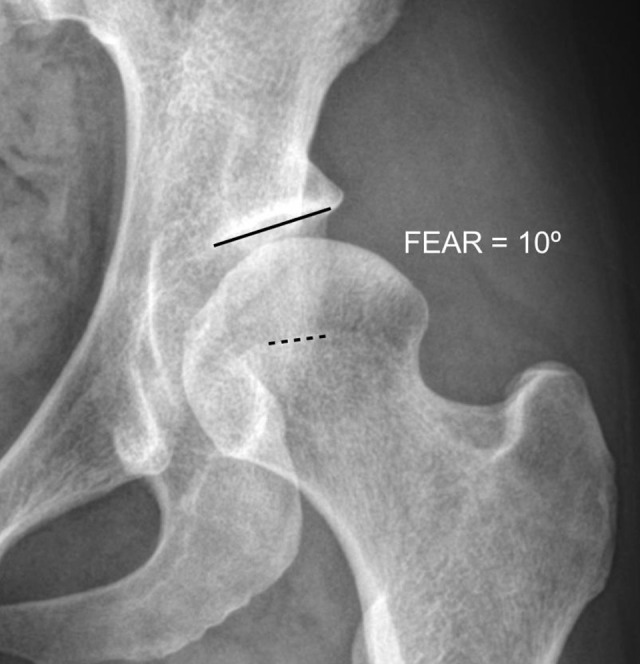
Femoroepiphyseal acetabular roof (FEAR) index. A laterally directed angle represents a positive FEAR index, with an angle >5° at higher risk of instability.
Acetabular Quotient
The acetabular quotient assesses the relationship of the depth of the acetabulum to its width. It is determined by dividing the width of the acetabulum, measured as the distance from inferior teardrop to the lateral rim, by the depth of the acetabulum, measured from a perpendicular line starting at the midpoint of the width line to the acetabular dome. This value is then multiplied by 1000. 36 A value <250 denotes an abnormally shallow hip socket, consistent with hip dysplasia. This quotient is a modification of the Heyman and Herndon 16 acetabular index of depth to width.
Femoral Neck-Shaft Angle
The femoral neck-shaft angle (NSA) depicts where in the coronal plane the femoral head lies in relation to the anatomic axis of the femur. The angle’s apex lies at the intertrochanteric line and is at the intersection of a line going down the intramedullary canal of the femur and a second line parallel to the neck of the proximal femur. A normal NSA is between 120° and 140°. An NSA >140° is referred to as coxa valga, and <120° is termed coxa vara. 10,41,50 Coxa valga and increased external femoral torsion (anteversion), which will often present itself on an AP pelvis radiograph as coxa valga, are found in higher frequency in patients with hip dysplasia. 7,33 In contrast, coxa vara is more commonly associated with FAI. 3,11 Similar to assessing the quality of the radiograph before measuring acetabular parameters, it is important to ensure that the feet have been internally rotated for correct measurement of the NSA to avoid overestimation.
Alpha Angle
On an AP pelvis radiograph, the alpha angle is measured by making a circle collinear with the curvature of the femoral head. The apex of the angle is at the center of the femoral head (circle center) with one arm going down the shaft of the femoral neck and the other arm extending to the location where the femoral head-neck junction breaks the circle. An alpha angle measurement >50° to 55° is indicative of abnormal head-neck contour indicating (lateral) cam-type FAI. 2 An anterolateral or cam-type deformity at the 12-o’clock to 1-o’clock positions is often called a pistol-grip deformity. 31 To be noted, the most sensitive radiographic view for identifying cam morphology is a 45° Dunn lateral view, which suggests an anterolateral apex of deformity. 45 The importance of acknowledging a cam-type hip shape in a patient with frank or borderline dysplasia is important. If a cam lesion is not addressed during hip arthroscopy before periacetabular osteotomy, it can result in impingement and reduction in range of motion in a newly stabilized hip joint. Along another vein, if a patient has BHD and a significant cam lesion, then the surgeon must consider if the cam lesion or BHD is the main factor for the patient’s symptoms.
MRI/MRA PARAMETERS
MRA is the touchstone for imaging of the labrum and cartilage within the hip joint. MRI is more sensitive at identifying labral injury relative to chondral lesions. 30,51 Over the past 20 years, advances in magnetic resonance technology have continued to increase the accuracy in detecting intra-articular hip pathology. 28,46 In addition to detecting labral and cartilage injuries, MRI is also capable at providing insight into the stability, or lack thereof, of the dysplastic and BHD hip.
Labral Hypertrophy
It has been found in both MRA-based and arthroscopy-based studies that labral length is inversely proportional to lateral acetabular coverage. 12 The average lateral labral length in a normally covered hip (LCEA, 25.0°-39.9°) is 7.68 mm. 12 Patients with borderline and frank dysplasia have mean labral lengths of 9.44 and 10.12 mm, respectively. 12 The theories behind labral hypertrophy in the unstable hip include (1) adaptive hypertrophy in the setting of increased shear forces within the joint or (2) incomplete ossification of the cartilaginous acetabulum during hip development. 23 Interestingly, Kraeutler et al 23 found that the total osseolabral coverage remains statistically equivalent between hips with normal acetabular coverage and those with dysplasia due to the phenomenon of labral hypertrophy.
Femoroacetabular Cartilage Hypertrophy
Similar to labral hypertrophy, evaluation of cartilage thickness on MRA has also shown evidence of increased thickness with lower acetabular coverage. In addition to noting that the lateral sourcil cartilage thickness was significantly greater than the middle sourcil and fovea thickness, Ashwell et al 1 also found that lateral cartilage thickness increased as LCEA decreased. The average cartilage thickness in normally covered hips (LCEA, 25.0°-39.9°) was 3.20 mm compared with 3.68 mm in BHD and 4.33 mm in frankly dysplastic hips. Counter to this, though, is that female sex yields a reduction in cartilage thickness relative to the male counterpart. 1 The hypothesis for this phenomenon is also thought to result from a compensatory mechanism for increased focal loads and shear stress. 1
Everted Labrum
Counter to labral hypertrophy, an everted labrum may also be present in BHD and frank hip dysplasia. This labral pathology is characterized by a labrum that sits on the capsular side of the acetabular rim, not contacting the femoral head, and thereby providing no suction seal for normal hip mechanics (Figure 4). 54 Vogel et al 54 found that 36.8% of everted labrum cases were in patients with an LCEA <25°. An everted labrum was found to sit off the femoral head by a mean of 1.4 mm on coronal MRI/MRA in the anterior-superior quadrant, was significantly shorter compared with control hips, and was more often blunted than triangular in appearance.
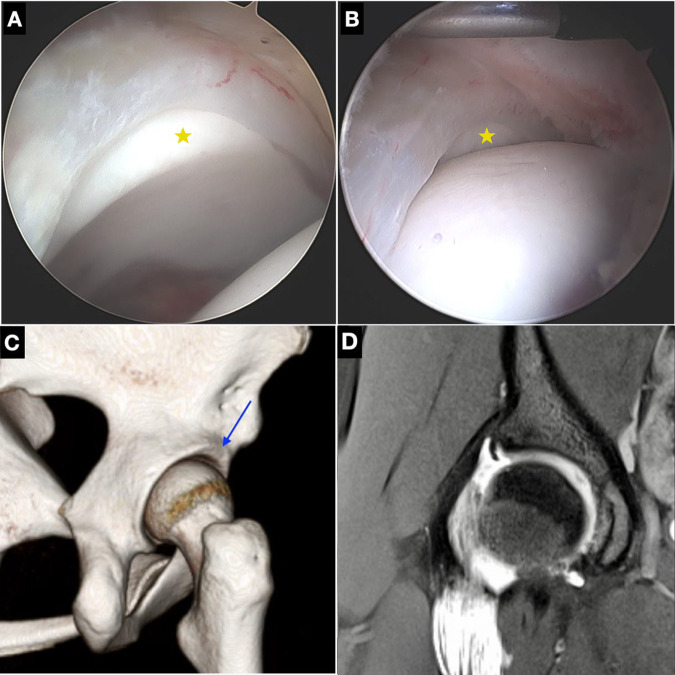
Figure 4.
Everted labrum. This labral pathology is characterized by a labrum that sits on the capsular side of the acetabular rim, not contacting the femoral head, and thereby providing no suction seal necessary for normal hip mechanics. (A) Arthroscopic image with star demonstrating cartilage rim that is visible because labrum is everted. (B) Star in arthroscopic image demonstrates that with traction off, the cartilage rim remains visible because the labrum is everted away from the femoral head, thus compromising the suction seal. (C) Computed tomography shows upsloping lateral sourcil with blue arrow pointing to the superior rim where the labrum is attached. (D) Coronal T2 fat-saturated magnetic resonance arthrography image demonstrates how an everted labrum can be visualized as a blunted structure (as opposed to a normal triangular shape) that does not come into contact with the femoral head.
Fovea Alta
Another MRI measurement associated with hip dysplasia is fovea alta (delta angle, <10°). 4 This is measured on an MRI/MRA coronal slice in which both the acetabular sourcil and fovea capitis are best visualized. The delta angle is then made with the vertex at the center of the femoral head, one arm going to the medial aspect of the sourcil and the other arm going to the superior aspect of the fovea capitis. A negative delta angle is made when the superior edge of the fovea capitis is lateral to the medial-most aspect of the sourcil. Beltran et al 4 found a delta angle of <10° (fovea alta) to have a high specificity for hip dysplasia. Similarly, the mean delta angle in dysplastic hips in this study was 3.4° compared with 21.7° in normal hips. Interestingly, there was no significant difference in delta angle between BHD and normal hips.
Cartilage Delamination
MRI is known to underestimate cartilage delamination. 8,26 Intra-articular injection of contrast improves the diagnostic accuracy of cartilage lesions compared with conventional MRI but remains reduced relative to labral pathology diagnoses. 47 The reason why cartilage delamination and other chondral damage is not accurately diagnosed on magnetic resonance imaging is thought to be because of the compressive force between the femoral head and acetabular cartilage layers. This has been demonstrated in the improved performance of MRA in diagnosing chondral lesions when done under traction. 42 However, in some cases of standard MRI/MRA, synovial fluid or the contrast agent does demonstrate cartilage delamination. The pattern of delamination can differentiate between the “outside-in” chondral flap associated with FAI and the “inside-out” delamination seen with instability (Figure 5). 24
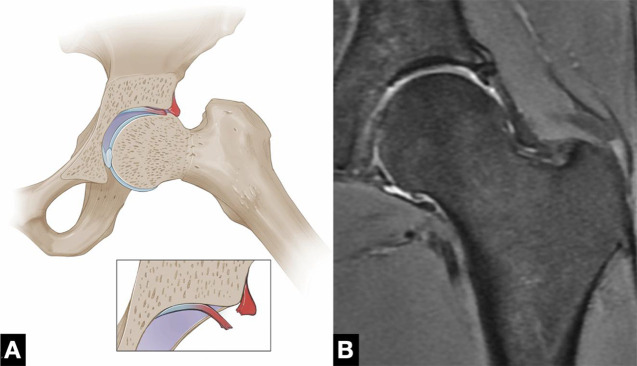
Figure 5.
Cartilage delamination. The pattern of cartilage damage varies by osseous pathology. (A) Cartilage delaminates from the outside-in with cam-type femoroacetabular impingement, whereas in cases of instability, the damage occurs from inside-out. In some cases, magnetic resonance imaging/magnetic resonance arthrography (MRA) will show the pattern of delamination, assisting in the diagnoses. (B) Coronal T2 fat-saturated MRA image demonstrates outside-in chondral delamination.
Anterior Acetabular Bone Cysts
Subchondral bone cysts are found to initially develop in the anterior portion of the acetabulum in patients with hip dysplasia. 17 In patients with dysplasia, these cysts may be assumed to communicate directly with the joint space, 17 even if an intra-articular breach is not clearly visible. With progression of osteoarthritis, an additional finding of subchondral edema localized anteriorly in dysplastic hips can also be appreciated on MRI. 53
CT PARAMETERS
CT gives the treating hip preservation specialist the most detailed understanding of the bony 3-dimensional pathology of a patient’s hip. It is with CT that objective measurements of a patient’s acetabular version and femoral torsion can be made accurately. There exist multiple methods of measuring these parameters and others on CT, making standardization of patient positioning in the scanner and knowledge of the measurement techniques employed paramount in analyzing this imaging modality.
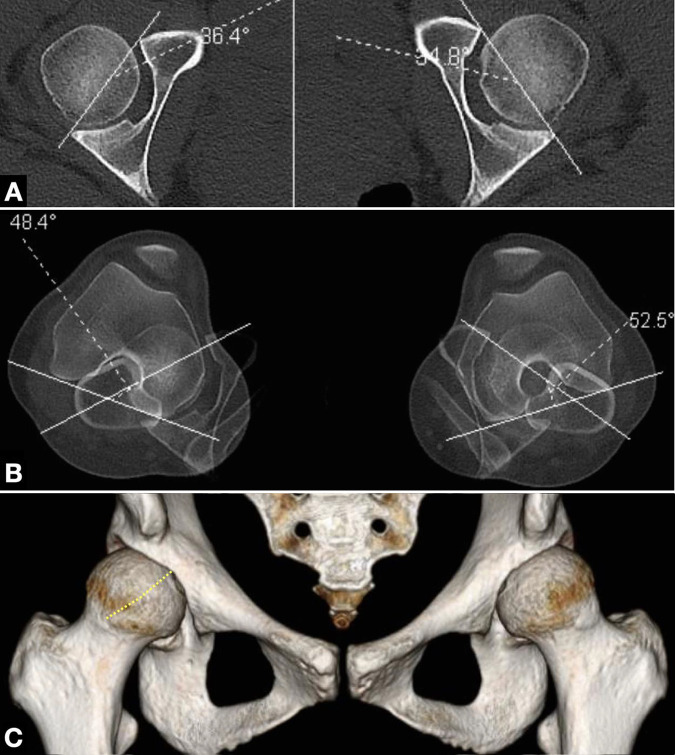
Acetabular Version
Acetabular version is the orientation of the socket relative to the sagittal plane, representing the relationships between the anterior and posterior walls (Figure 6A). Specifically, on axial images it is the angle between a perpendicular line from the horizontal axis of the posterior acetabuli and a line between the posterior and anterior rim of the acetabulum. When measuring at the level of the midfemoral heads, this produces the global version of the acetabulum (otherwise considered the version at 3 o’clock). Normal acetabular version at this level is considered 15° to 20°. Anteversion >25° indicates anterior undercoverage and may result in anterior hip instability. 49 Acetabular retroversion can be indicative of posterior-superior undercoverage, which is associated with hip instability, or anterior overcoverage, which is representative of hip impingement. 37 Increased posterior pelvic tilt (which is demonstrated when the distance between the coccyx and symphysis is reduced) will magnify acetabular anteversion and needs to be considered in patient positioning for CT. 9,39
Figure 6.
“Too much head sign.” (C) Frank anterior instability can be visualized on 3-dimensional computed tomography reconstruction by visualization of the fovea capitis, with the dotted line demonstrating visualization of the entire anterior femoral head not being contained within the bony acetabulum. This is because of (A) acetabular anteversion or (B) femoral antetorsion, and usually a combination of both.
Femoral Neck-Shaft Angle
On CT, the femoral NSA is measured in the midcoronal image when the center of the femoral head is found by using a localizer line on the axial images. A normal NSA is between 120° and 140°. A femoral NSA >140° is indicative of coxa valga and can be associated with adverse outcomes after hip arthroscopy given its association with hip dysplasia. 52
Femoral Torsion
Femoral torsion is a projected angular measurement that incorporates the femoral neck inclination and femoral shaft rotation (Figure 6B). There are a variety of described methods for making femoral torsion measurements, but all require including slices of the proximal and distal femur on CT such that they can be superimposed for angular measurement. Schmaranzer et al 43 performed a study showing that femoral torsion values increase the more distal the femoral neck axis is measured, with up to a 17° difference depending on the technique utilized. Fortunately, all methods have high intraobserver and interobserver agreement, 19 although it is important to delineate which axial sequence is used (axial-oblique vs standard axial), as measurements will differ between these 2 methods. 14 Standard values of normal femoral torsion range from 7° to 24°, with some studies showing that women have a higher mean femoral torsion than men. 14 Regardless of technique used, increased femoral antetorsion has been well described as a source for hip instability whether in conjunction with acetabular dysplasia or as a singular diagnosis. 5,48
Upsloping Lateral Sourcil
Similar to radiographs, ULS can be noted on CT in patients with borderline or frank hip dysplasia (Figure 2, B and C). 53 The prevalence of the ULS increases with the degree of undercoverage as defined by LCEA. 53 It is also found more frequently in patients with joint hypermobility. As such, it can be a useful adjunct to determining the presence and amount of instability, especially in patients evaluated with microinstability and BHD.
Anterior Subchondral Cysts
Acetabular cysts usually form initially in the anterior acetabulum in patients with dysplasia and then progress to other areas of the joint with increasing severity of degenerative changes. 16 While radiographs and MRI can reveal the presence of subchondral cysts, CT provides greater bony detail to allow for more accurate sizing and localization of the cyst. Because of its higher resolution, it may also locate the intra-articular breach. This is important as subchondral cysts often require treatment in the form of cyst decompression, microfracture, and/or bone grafting, depending on their size. 13 Of course, treatment of the underlying pathology (ie, hip dysplasia and/or FAI) is paramount to prevent recurrence.
Too Much Head Sign
Frank anterior instability can be visualized on 3-dimensional CT reconstruction by visualization of the fovea capitis (Figure 6C). This is because of acetabular anteversion, femoral antetorsion, and usually a combination of both to produce the “too much head sign” (Figure 6, A and B). Care must be taken that the position of the femur is standardized when evaluating for this sign, as positioning can significantly impact femoral torsion and anterior visualization of the femoral head. 29 Objectively, the summation of femoral torsion and acetabular version (both previously described) has been coined the COTAV (combined femoral torsion–acetabular version) index. 6 A COTAV value >45° is associated with anterior hip instability.
SUMMARY
Hip dysplasia is not a black-and-white diagnosis. As such, hip preservation specialists need to be able to consider multiple factors from the patient’s history, examination, and imaging to determine the best treatment plan. Valuable initial information can be gleaned from a good AP pelvis radiograph, but further detailed understanding of a patient’s hip instability is established with advanced imaging, namely MRI/MRA and CT. Especially in cases of microinstability and BHD, knowledge of the various imaging findings that indicate the presence and severity of instability is paramount in determining whether hip arthroscopy alone or in conjunction with a reorienting osteotomy is necessary. Once a surgical plan has been decided, imaging is integral in the planning and execution of treatment for each hip. This review provides the salient signs and parameters found on radiograph, MRI/MRA, and CT imaging that aid the hip preservation specialist in determining the nature of each patient’s hip instability and thereby developing the best patient-specific surgical plan possible.
Footnotes
Final revision submitted October 16, 2022; accepted November 8, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.L.W. has received education payments from Smith & Nephew and hospitality payments from Stryker. T.G. and O.M.-D. have received consulting fees from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ashwell ZR, Flug J, Chadayammuri V, Pascual-Garrido C, Garabekyan T, Mei-Dan O. Lateral acetabular coverage as a predictor of femoroacetabular cartilage thickness. J Hip Preserv Surg. 2016;3(4):262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barton C, Salineros MJ, Rakhra KS, Beaule PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469(2):464–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beall DP, Sweet CF, Martin HD, et al. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34(11):691–701. [DOI] [PubMed] [Google Scholar]
- 4. Beltran LS, Mayo JD, Rosenberg ZS, et al. Fovea alta on MR images: is it a marker of hip dysplasia in young adults? AJR Am J Roentgenol. 2012;199(4):879–883. [DOI] [PubMed] [Google Scholar]
- 5. Buly RL, Sosa BR, Poultsides LA, Caldwell E, Rozbruch SR. Femoral derotation osteotomy in adults for version abnormalities. J Am Acad Orthop Surg. 2018;26(19):e416–e425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chadayammuri V, Garabekyan T, Bedi A, et al. Passive hip range of motion predicts femoral torsion and acetabular version. J Bone Joint Surg Am. 2016;98(2):127–134. [DOI] [PubMed] [Google Scholar]
- 7. Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009;467(1):128–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crespo Rodríguez AM, de Lucas Villarrubia JC, Pastrana Ledesma MA, Millán Santos I, Padrón M. Diagnosis of lesions of the acetabular labrum, of the labral-chondral transition zone, and of the cartilage in femoroacetabular impingement: correlation between direct magnetic resonance arthrography and hip arthroscopy. Radiologia. 2015;57(2):131–141. [DOI] [PubMed] [Google Scholar]
- 9. Dandachli W, Ul Islam S, Tippett R, Hall-Craggs MA, Witt JD. Analysis of acetabular version in the native hip: comparison between 2D axial CT and 3D CT measurements. Skeletal Radiol. 2011;40(7):877–883. [DOI] [PubMed] [Google Scholar]
- 10. Dolan MM, Heyworth BE, Bedi A, Duke G, Kelly BT. CT reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res. 2011;469(3):831–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15(7):475–481. [DOI] [PubMed] [Google Scholar]
- 12. Garabekyan T, Ashwell Z, Chadayammuri V, et al. Lateral acetabular coverage predicts the size of the hip labrum. Am J Sports Med. 2016;44(6):1582–1589. [DOI] [PubMed] [Google Scholar]
- 13. Garabekyan T, Chadayammuri V, Pascual-Garrido C, Mei-Dan O. Arthroscopic bone grafting of deep acetabular cysts using a curved delivery device. Arthrosc Tech. 2016;5(1):e113–e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hartel MJ, Petersik A, Schmidt A, et al. Determination of femoral neck angle and torsion angle utilizing a novel three-dimensional modeling and analytical technology based on CT datasets. PLoS One. 2016;11(3):e0149480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Henebry A, Gaskill T. The effect of pelvic tilt on radiographic markers of acetabular coverage. Am J Sports Med. 2013;41(11):2599–2603. [DOI] [PubMed] [Google Scholar]
- 16. Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32A(4):767–778. [PubMed] [Google Scholar]
- 17. Inui A, Nakano S, Yoshioka S, et al. Subchondral cysts in dysplastic osteoarthritic hips communicate with the joint space: analysis using three-dimensional computed tomography. Eur J Orthop Surg Traumatol. 2013;23(7):791–795. [DOI] [PubMed] [Google Scholar]
- 18. Jacobsen S, Sonne-Holm S, Lund B, et al. Pelvic orientation and assessment of hip dysplasia in adults. Acta Orthop Scand. 2004;75(6):721–729. [DOI] [PubMed] [Google Scholar]
- 19. Kaiser P, Attal R, Kammerer M, et al. Significant differences in femoral torsion values depending on the CT measurement technique. Arch Orthop Trauma Surg. 2016;136(9):1259–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423–429. [DOI] [PubMed] [Google Scholar]
- 21. Kraeutler MJ, Ashwell ZR, Garabekyan T, et al. The iliofemoral line: a radiographic sign of acetabular dysplasia in the adult hip. Am J Sports Med. 2017;45(11):2493–2500. [DOI] [PubMed] [Google Scholar]
- 22. Kraeutler MJ, Garabekyan T, Goodrich JA, Fioravanti MJ, Chadayammuri V, Mei-Dan O. Standardizing the prearthritic hip joint space width: an analysis of 994 hips. Arthroscopy. 2018;34(7):2114–2120. [DOI] [PubMed] [Google Scholar]
- 23. Kraeutler MJ, Goodrich JA, Ashwell ZR, Garabekyan T, Jesse MK, Mei-Dan O. Combined lateral osseolabral coverage is normal in hips with acetabular dysplasia. Arthroscopy. 2019;35(3):800–806. [DOI] [PubMed] [Google Scholar]
- 24. Kraeutler MJ, Goodrich JA, Fioravanti MJ, Garabekyan T, Mei-Dan O. The “outside-in” lesion of hip impingement and the “inside-out” lesion of hip dysplasia: two distinct patterns of acetabular chondral injury. Am J Sports Med. 2019;47(12):2978–2984. [DOI] [PubMed] [Google Scholar]
- 25. Kraeutler MJ, Safran MR, Scillia AJ, Ayeni OR, Garabekyan T, Mei-Dan O. A contemporary look at the evaluation and treatment of adult borderline and frank hip dysplasia. Am J Sports Med. 2020;48(9):2314–2323. [DOI] [PubMed] [Google Scholar]
- 26. Lee GY, Kim S, Baek SH, Jang EC, Ha YC. Accuracy of magnetic resonance imaging and computed tomography arthrography in diagnosing acetabular labral tears and chondral lesions. Clin Orthop Surg. 2019;11(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lequesne M, Malghem J, Dion E. The normal hip joint space: variations in width, shape, and architecture on 223 pelvic radiographs. Ann Rheum Dis. 2004;63(9):1145–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Link TM, Schwaiger BJ, Zhang AL. Regional articular cartilage abnormalities of the hip. AJR Am J Roentgenol. 2015;205(3):502–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Morvan G, Guerini H, Carré G, Vuillemin V. Femoral torsion: impact of femur position on CT and stereoradiography measurements. AJR Am J Roentgenol. 2017;209(2):W93–W99. [DOI] [PubMed] [Google Scholar]
- 30. Naraghi A, White LM. MRI of labral and chondral lesions of the hip. AJR Am J Roentgenol. 2015;205(3):479–490. [DOI] [PubMed] [Google Scholar]
- 31. Nepple JJ, Martel JM, Kim YJ, Zaltz I, Clohisy JC, Group AS. Do plain radiographs correlate with CT for imaging of cam-type femoroacetabular impingement? Clin Orthop Relat Res. 2012;470(12):3313–3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nitschke A, Lambert JR, Glueck DH, et al. Validation of a new radiographic measurement of acetabular version: the transverse axis distance (TAD). Skeletal Radiol. 2015;44(11):1679–1686. [DOI] [PubMed] [Google Scholar]
- 33. Noble PC, Kamaric E, Sugano N, et al. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;(417):27–40. [PubMed] [Google Scholar]
- 34. Ogata S, Moriya H, Tsuchiya K, Akita T, Kamegaya M, Someya M. Acetabular cover in congenital dislocation of the hip. J Bone Joint Surg Br. 1990;72(2):190–196. [DOI] [PubMed] [Google Scholar]
- 35. Packer JD, Cowan JB, Rebolledo BJ, et al. The cliff sign: a new radiographic sign of hip instability. Orthop J Sports Med. 2018;6(11):2325967118807176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pedersen DR, Lamb CA, Dolan LA, Ralston HM, Weinstein SL, Morcuende JA. Radiographic measurements in developmental dysplasia of the hip: reliability and validity of a digitizing program. J Pediatr Orthop. 2004;24(2):156–160. [PubMed] [Google Scholar]
- 37. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81(2):281–288. [DOI] [PubMed] [Google Scholar]
- 38. Rhee PC, Woodcock JA, Clohisy JC, et al. The Shenton line in the diagnosis of acetabular dysplasia in the skeletally mature patient. J Bone Joint Surg Am. 2011;93(suppl 2):35–39. [DOI] [PubMed] [Google Scholar]
- 39. Ross JR, Nepple JJ, Philippon MJ, Kelly BT, Larson CM, Bedi A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am J Sports Med. 2014;42(10):2402–2409. [DOI] [PubMed] [Google Scholar]
- 40. Ross JR, Tannenbaum EP, Nepple JJ, Kelly BT, Larson CM, Bedi A. Functional acetabular orientation varies between supine and standing radiographs: implications for treatment of femoroacetabular impingement. Clin Orthop Relat Res. 2015;473(4):1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Saikia KC, Bhuyan SK, Rongphar R. Anthropometric study of the hip joint in northeastern region population with computed tomography scan. Indian J Orthop. 2008;42(3):260–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schmaranzer F, Klauser A, Kogler M, et al. Diagnostic performance of direct traction MR arthrography of the hip: detection of chondral and labral lesions with arthroscopic comparison. Eur Radiol. 2015;25(6):1721–1730. [DOI] [PubMed] [Google Scholar]
- 43. Schmaranzer F, Lerch TD, Siebenrock KA, Tannast M, Steppacher SD. Differences in femoral torsion among various measurement methods increase in hips with excessive femoral torsion. Clin Orthop Relat Res. 2019;477(5):1073–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sharp IK. Acetabular dysplasia—the acetabular angle. J Bone Joint Surg Br. 1961;43(2):268–272. [Google Scholar]
- 45. Smith KM, Gerrie BJ, McCulloch PC, Lintner DM, Harris JD. Comparison of MRI, CT, Dunn 45° and Dunn 90° alpha angle measurements in femoroacetabular impingement. Hip Int. 2018;28(4):450–455. [DOI] [PubMed] [Google Scholar]
- 46. Sundberg TP, Toomayan GA, Major NM. Evaluation of the acetabular labrum at 3.0-T MR imaging compared with 1.5-T MR arthrography: preliminary experience. Radiology. 2006;238(2):706–711. [DOI] [PubMed] [Google Scholar]
- 47. Sutter R, Zubler V, Hoffmann A, et al. Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol. 2014;202(1):160–169. [DOI] [PubMed] [Google Scholar]
- 48. Tibor LM, Liebert G, Sutter R, Impellizzeri FM, Leunig M. Two or more impingement and/or instability deformities are often present in patients with hip pain. Clin Orthop Relat Res. 2013;471:3762–3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81(12):1747–1770. [DOI] [PubMed] [Google Scholar]
- 50. Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res. 2009;467(4):876–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;186(2):449–453. [DOI] [PubMed] [Google Scholar]
- 52. Uchida S, Utsunomiya H, Mori T, et al. Clinical and radiographic predictors for worsened clinical outcomes after hip arthroscopic labral preservation and capsular closure in developmental dysplasia of the hip. Am J Sports Med. 2016;44(1):28–38. [DOI] [PubMed] [Google Scholar]
- 53. Vogel LA, Garabekyan T, Mei-Dan O. Surgical technique: hip arthroscopy for hip dysplasia. In: Nho SJ, Asheesh B, Salata MJ, Mather RC III, Kelly BT, eds. Hip Arthroscopy and Hip Joint Preservation Surgery. Springer; 2021:1–22. [Google Scholar]
- 54. Vogel LA, Kraeutler MJ, Jesse MK, et al. The everted acetabular labrum: patho-anatomy, magnetic resonance imaging and arthroscopic findings of a native variant. Arthroscopy. 2022;38(1):72–79. [DOI] [PubMed] [Google Scholar]
- 55. Welton KL, Jesse MK, Kraeutler MJ, Garabekyan T, Mei-Dan O. The anteroposterior pelvic radiograph: acetabular and femoral measurements and relation to hip pathologies. J Bone Joint Surg Am. 2018;100(1):76–85. [DOI] [PubMed] [Google Scholar]
- 56. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(58):53–68. [Google Scholar]
- 57. Wong TY, Jesse MK, Jensen A, Kraeutler MJ, Coleman C, Mei-Dan O. Upsloping lateral sourcil: a radiographic finding of hip instability. J Hip Preserv Surg. 2018;5:435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wyatt M, Weidner J, Pfluger D, Beck M. The femoro-epiphyseal acetabular roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia? Clin Orthop Relat Res. 2017;475(3):861–869. [DOI] [PMC free article] [PubMed] [Google Scholar]