Abstract
Introduction:
While the body of research investigating anterior cervical disk fusion (ACDF) for symptomatic cervical disk herniations in high-level athletes is large, evidence for cervical disk replacement (CDR) is sparse. The amount of patients able to return to sport after an ACDF is estimated to be 73.5%, causing surgeons to search for alternatives with better outcomes in this population. This case report describes the successful treatment of a symptomatic collegiate American football player with C6–C7 disk herniation and C5–C6 central canal stenosis.
Case Report:
This is a 21-year-old American football safety who underwent a C5–6 and C6–7 cervical disk arthroplasty. Three weeks postoperatively, the patient demonstrated nearly complete resolution of weakness, full resolution of radiculopathy, and normal cervical range of motion in all planes.
Conclusion:
The CDR may be considered as an alternative to the ACDF in the treatment of high-level contact athletes. Compared to the ACDF, CDR has been shown in prior studies to decrease the long-term risk of adjacent segment degeneration. Future studies comparing ACDF to CDR in the high-level contact sport athlete population are needed. CDR appears to be a promising surgical intervention for symptomatic patients in this population.
Keywords: Cervical disk replacement, anterior cervical disk fusion, contact sports, cervical disk arthroplasty
Learning Point of the Article:
Cervical disc arthroplasty is a reliable and safe option in a high level athletes to return to sport after injury.
Introduction
Cervical disk replacement (CDR) and anterior cervical disk fusion (ACDF) have both been used to treat cervical disk disease in symptomatic high-level athletes [1, 2, 3, 4]. Given the imperative need for full cervical range of motion in contact sports such as American football, CDR has been used with increasing popularity to avoid the single- and sometimes multi-level cervical fusion associated with ACDF. CDR has been shown to maintain physiologic distribution of range of motion throughout the cervical spine. In contrast, ACDF is associated with increased range of motion contribution from adjacent segments (in relation to the fusion) to maintain gross cervical mobility [5]. This increased motion in the adjacent segment has been associated with adjacent segment degeneration, a long-term complication that CDR has been shown to mitigate [6, 7, 8]. There have been other case reports of high-level athletes undergoing CDR with good outcomes [4, 9]. This report demonstrates further success of CDR in a collegiate American football player.
Case Report
The patient presented as a right hand-dominant 21-year-old male collegiate football player (safety position) with a 7-day history of the right-sided muscle spasms, aching, and numbness/tingling that radiated to his right index and middle finger. The symptoms appeared after a weight training session. Medical history was significant for a right ulna percutaneous pinning 8 years ago due to a previous fracture. Athletic training staff at his school had attempted therapeutic ultrasound and dry needling with no relief. His pain and spasms were in the posterior shoulder region.
On physical examination, the patient demonstrated full range of motion bilaterally with tenderness to palpation in the paraspinal muscles as well as rhomboids with no palpable trigger point. Spurling’s test was positive, recreating his pain in the posterior shoulder blade. Shoulder range of motion was within normal limits and 5/5 strength was observed throughout both upper extremities. Right shoulder and cervical X-rays revealed no acute osseous abnormalities with slight loss of cervical lordosis. At his first visit, the patient was given a Medrol Dospak (methylprednisolone 4 mg) to address suspected cervical radiculopathy.
Eight days later, an MRI was performed of the cervical spine which revealed (1) degenerative changes of the cervical spine most prominent at C5–6 with moderate spinal canal stenosis, cord deformity and cord edema signal, moderate left, mild right foraminal stenosis, and (2) at C6–C7, right paracentral and right foraminal disk herniation causing mild spinal canal stenosis, cord deformity, and severe right foraminal stenosis (Fig. 1, 2).
Figure 1.
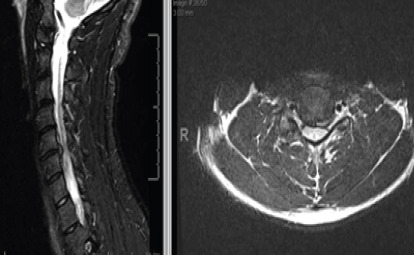
C5–6 with moderate spinal canal stenosis, cord deformity, and cord edema signal, moderate left, and mild right foraminal stenosis.
Figure 2.
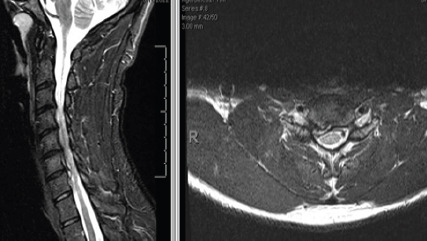
C6–C7 right paracentral and right foraminal disk herniation causing mild spinal canal stenosis, cord deformity, and severe right foraminal stenosis.
Subsequent follow-up with a fellowship-trained orthopedic spine surgeon revealed improving symptoms, but now with 4+/5 right wrist extension strength and positive Hoffmann’s bilaterally. At this time, it was recommended that the patient not return to play due to concern regarding the cord edema.
Over the course of the next month and a half, his numbness and tingling worsened with prolonged sitting, and he was starting to notice difficulty with push-ups due to weakness in his right pectoralis major muscle. He presented for a follow-up visit now ~3 months post injury. On physical examination, he demonstrated 4/5 right biceps and right triceps strength. In addition, finger extensors were 4/5 bilaterally. Sensory examination showed no focal deficits in the upper extremities. At this visit, surgical intervention was recommended and described as C5–6 and C6–7 anterior discectomy with arthroplasty with possible fusion with allograft plating.
A C5–6 and C6–7 anterior discectomy and arthroplasty were performed exactly 3 months after the initial office visit by a fellowship-trained spine surgeon (Fig. 3).
Figure 3.
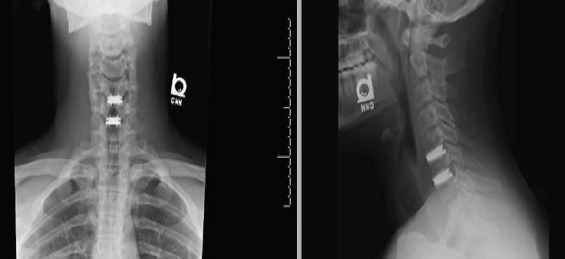
Cervical disk arthroplasty at C5–C6 and C6–C7.
Three weeks postoperatively, the patient presented with resolution of arm pain, numbness, or tingling, taking ibuprofen as needed for pain related to surgery site. Upper extremity motor examination was intact bilaterally C5–T1 except mild wrist flexor weakness bilaterally (5−/5). Sensory examination revealed intact sensation bilaterally. Cervical range of motion in all planes (bilateral rotation, lateral bending, flexion, and extension) was normal and painless. Post-operative X-rays demonstrated the C5–7 disk arthroplasties in good position.
Discussion
This case report describes a rare injury within the collegiate football player population that was successfully treated with CDR. Cervical spine injuries are common in NCAA collegiate football athletes with nearly 7500 such injuries reported from 2009 to 2014. However, only a small fraction of these (0.02%) were related to cervical disk injury. An even smaller percentage (0.01%) of these injuries involved central spinal stenosis [10].
ACDF is a procedure that is well-researched in high-level contact athletes, with mostly excellent results [1, 2, 11]. A few studies have assessed the efficacy of CDR with excellent results and no setbacks in returning to play [9, 11, 12]. This report shows a quick resolution of radiculopathy in a young collegiate football player. This case study demonstrates that CDR is an effective surgery for cervical disk disease in contact athletes and should be considered in this population.
Conclusion
The small, yet growing body of literature supporting CDR for high-level athletes is promising. Its effectiveness and potential to decrease long-term complications, as in adjacent segment degeneration, make it a good alternative to ACDF in this population. However, further comparative studies are needed to determine the most effective surgical intervention in the symptomatic high-level contact athlete population.
Clinical Message.
Cervical disk arthroplasty is a viable treatment option for cervical disk herniation in high-level athletes. Long-term studies and data are recommended.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Leider J, Piche JD, Khan M, Aleem I. Return-to-play outcomes in elite athletes after cervical spine surgery:A systematic review. Sports Health. 2021;13:437–45. doi: 10.1177/19417381211007813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McAnany SJ, Overley S, Andelman S, Patterson DC, Cho SK, Qureshi S, et al. Return to play in elite contact athletes after anterior cervical discectomy and fusion:A meta-analysis. Global Spine J. 2017;7:552–9. doi: 10.1177/2192568217700112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Watkins RG, 4th, Chang D, Watkins RG., 3rd Return to play after anterior cervical discectomy and fusion in professional athletes. Orthop J Sports Med. 2018;6:2325967118779672. doi: 10.1177/2325967118779672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindi-Sugino R, Hartl R, Klezl Z. Cervical arthroplasty in a professional kick-boxing fighter, 7 years follow-up. Acta Ortop Mex. 2021;35:282–5. [PubMed] [Google Scholar]
- 5.Chang SW, Bohl MA, Kelly BP, Wade C. The segmental distribution of cervical range of motion:A comparison of ACDF versus TDR-C. J Clin Neurosci. 2018;57:185–93. doi: 10.1016/j.jocn.2018.08.050. [DOI] [PubMed] [Google Scholar]
- 6.Xu S, Liang Y, Zhu Z, Qian Y, Liu H. Adjacent segment degeneration or disease after cervical total disc replacement:A meta-analysis of randomized controlled trials. J Orthop Surg. 2018;13:244. doi: 10.1186/s13018-018-0940-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steinberger J, Qureshi S. Cervical disc replacement. Neurosurg Clin N Am. 2020;31:73–9. doi: 10.1016/j.nec.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Limanówka B, Sagan L. Changes in cervical range of motion following anterior cervical discectomy with fusion-preliminary results. Neurol Neurochir Pol. 2020;54:568–75. doi: 10.5603/PJNNS.a2020.0098. [DOI] [PubMed] [Google Scholar]
- 9.Satalich J, Carter S, Fisichella A, Widmeyer J, Kalluri P, Vap A. Return to football after a cervical disk arthroplasty:A case report. J Orthop Case Rep. 2022;12:19–21. doi: 10.13107/jocr.2022.v12.i05.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung AS, Makovicka JL, Hassebrock JD, Patel KA, Tummala SV, Deckey DG, et al. Epidemiology of cervical injuries in NCAA football players. Spine (Phila Pa 1976) 2019;44:848–54. doi: 10.1097/BRS.0000000000003008. [DOI] [PubMed] [Google Scholar]
- 11.Mai HT, Chun DS, Schneider AD, Hecht AC, Maroon JC, Hsu WK. The difference in clinical outcomes after anterior cervical fusion, disk replacement, and foraminotomy in professional athletes. Clin Spine Surg. 2018;31:E80–4. doi: 10.1097/BSD.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 12.Reinke A, Behr M, Preuss A, Villard J, Meyer B, Ringel F. Return to sports after cervical total disc replacement. World Neurosurg. 2017;97:241–6. doi: 10.1016/j.wneu.2016.10.042. [DOI] [PubMed] [Google Scholar]


