Abstract
Background
Diabetes mellitus and hypertension are the most prominent conditions causing chronic kidney disease and eventually end-stage renal disease. Renal replacement therapy, particularly hemodialysis (HD), is the mainstay of treatment. The aim of this study is to assess the overall survival status of HD patients and potential survival predictors at Saint Paul hospital millennium medical college (SPHMMC) and Myungsung Christian Medical Center (MCM) in Addis Ababa, Ethiopia.
Methods
A retrospective cohort study was conducted on HD patients at SPHMMC and MCM general hospital from January 1, 2013 to December 30, 2020. Kaplan Meier, Log-rank, and Cox proportional regression models were used for the analysis. Estimated risks were reported as hazard ratios with 95% confidence intervals and P<0.05 was considered as having a significant association.
Results
A total of 128 patients were included in the study. Median survival time was 65 months. The predominant co-morbid condition was found to be diabetes mellitus with hypertension (42%). The total risk time for these patients was 143,617 person years. The overall incidence rate of death was 2.9 per 10,000 person years (95% CI=2.2–4). Patients who developed blood stream infection were 2.98-times more likely to die than those without infection. Those using an arteriovenous fistula were 66% less likely to die than those using a central venous catheter. Additionally, patients treated in a government-owned facility were 79% less likely to die.
Conclusion
The study identified that the median survival time of 65 months was comparable with developed nations. Significant predictors of death were found to be blood stream infection and type of vascular access. Government-owned treatment facilities showed better patient survival.
Keywords: survival status, survival predictors, hemodialysis predictors
Introduction
Background
Non-communicable diseases (NCD), including chronic kidney disease (CKD), have become a major global health problem. CKD includes a range of pathophysiological processes associated with abnormal kidney function and a gradual decrease in the rate of glomerular filtration (GFR). Both the GFR and the amount of albuminuria are closely linked to the risk of CKD progression. CKD is differentiated from acute kidney disease by the existence of kidney damage or decreased function of the estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73 mt2, persisting for 3 months or more irrespective of the cause.1
The most prominent conditions causing CKD are diabetes mellitus and hypertension, followed by glomerulonephritis, chronic tubulointerstitial nephritis, and hereditary or cystic diseases which all eventually lead to end-stage renal disease (ESRD).2 Worldwide, over 2 million people undergo dialysis or renal transplantation to remain alive; however, only 20% are treated in about 100 developing countries that make up over 50% of the world population.3
In most parts of Africa, the extent of CKD is unknown, mainly due to a lack of national registries and a lack of community-based studies. Few countries like Egypt, Libya, Algeria, Tunisia, Morocco, South Africa, Mauritius, and Gabon are capable of accommodating dialysis treatment for 100 dialysis patients per million population. In these countries, dialysis outcomes are very poor, with survival ranging from 20–70%.4
In Ethiopia, the first dialysis service was started in 1980 at Tikure Anbessa specialized hospital, but a maintenance dialysis service started in 2001 at Saint Gabriel Hospital. The expansion of the service was restricted to Addis Ababa until recently, and the majority of dialysis services were provided by the private sector. Renal replacement therapy (RRT) in Ethiopia is extremely scarce and available to only a limited number of prosperous city residents.5 ESRD is usually accompanied by complications which significantly lower the survival time of hemodialysis (HD) patients. The opening and development of dialysis centers in countries such as Ethiopia would undoubtedly narrow the RRT gap and solve the issue of accessibility reflected in many African countries.6
Dialysis is one of the RRT alternatives that extends longevity, decreases morbidity, and enhances the quality-of-life. Despite many technical advances, however, the morbidity and mortality of dialysis patients remain unacceptably high, particularly in developing countries.7 High mortality is recorded in the first 3 months after initiation of treatment with HD. Around one-quarter of HD patients die in high-income countries within 1 year of initiation of treatment, and this proportion is even higher in low- and middle-income countries.8
While controversial, changes in the risk of mortality among dialysis patients tend to have been faster than in the general population, indicating that improved care for dialysis treatment patients rather than overall health gains could be partially responsible for these secular trends.9 The factors responsible for these apparent patterns has not been confirmed, but may include improved co-morbidity management, changes in the prevention or treatment of complications associated with dialysis such as infection, and better care before initiation of HD.10
The increasing prevalence of kidney failure, driven by factors such as diabetes and hypertension, is expected to put further strain on health systems, particularly in developing countries. This will likely lead to an increase in the use of HD, which poses major economic challenges. The reasons for the high number of patients with kidney failure in some countries are not well understood. Improving survival outcomes for dialysis patients is a key issue in addressing the adequacy of treatment for this chronic disease.
Materials and Methods
Study Area
The study was carried out at Saint Paul hospital millennium medical college (SPHMMC) and Myungsung Christian medical center (MCM). SPHMMC is one of the tertiary public Hospitals in Ethiopia with more than 350 beds that provide services for different categories of ambulatory and admitted patients coming from different corners of the country. The hospital was established in 1968. It has different clinics which provide an out-patient service where patients with specific chronic disease are referred for follow-up and routine health services for the city community as well as for different populations who come from regional states of Ethiopia. The renal clinic is one of the specialty clinics that provide service to CKD patients. Currently, the hospital has 15 dialysis beds working 24 hours. The other study area is MCM general hospital. It was established in 1993, following the request of the Ethiopian government to improve the medical environment. The hospital served not only the local community but also dialysis patients from abroad that come to Ethiopia on vacation. It is one of few private hospitals that have a dialysis center with around 9 beds.
Study Design and Period
A retrospective cohort study was conducted on HD patients who came to SPHMMC and MCM general hospital in Addis Ababa, Ethiopia from January 1, 2013, to December 30, 2020.
Study Population
The study population consists of patients above the age of 18 who were diagnosed with CKD and underwent HD treatment at SPHMMC and MCM general hospital during the study period from January 1, 2013 to December 30, 2020.
Inclusion Criteria
For this study, all adult patients with CKD who were evaluated for HD and underwent dialysis for more than 30 days between January 1, 2013 to December 30, 2020 were screened for inclusion.
Exclusions Criteria
Medical records were not included in the study if they contained HD for acute renal cases, had less than 1 month of HD records or if they were incomplete.
Sample Size Determination
Sample size determination starts by determining d (number of events), in this study the event is time to death.
 |
Then, the required total number of patients can be computed as  . From a similar study in Addis Ababa, we took a survival probability of 60% for our sample size calculation.11 We also know that
. From a similar study in Addis Ababa, we took a survival probability of 60% for our sample size calculation.11 We also know that  . Using the power of 80%.
. Using the power of 80%.
 |
 |
Adjusting for a loss of 10%,  .
.
Sampling Techniques
A systematic sampling technique was applied to select 128 samples. It was expected that the number of population (charts) would be very low. Each chart had a number assigned. Then numbers are selected randomly for the chart to be included in the study.
Study Variables
Dependent Variable
The outcome variable was death measured from dialysis initiation until the event occurs. Patients who were lost to follow-up, transferred out of the hospital to another center, who underwent kidney transplant, or remained in the study to the end of the study period were considered right-censored.
Independent Variables
Socio demographic factors.
Anthropometric measurements.
Co-morbid conditions.
Laboratory and diagnostic tests.
Type of vascular access.
Type of cardiac disease.
Blood stream infections.
Treatment facility.
Dialysis hour.
Dialysis frequency per week.
Data Collectors
The data collection was conducted by three nurses and one supervisor. One day training was given to all data collectors prior to data collection on how to fill the checklist details.
Data Collection Techniques
Since the study design is a retrospective cohort, data was collected from medication chart review. This was done using a checklist. The checklist contained information on socio-demographic details, anthropometric measures, co-morbid conditions, laboratory results, and other medical conditions.
Data Processing and Analysis
After data was checked for completeness, it was edited, coded, and entered into Epi Info software version 7.1.4 and was analyzed using STATA version 16.0. Kaplan Meier (KM) was used for preliminary descriptive analysis. The null hypothesis was tested using Log rank test to determine if there was a difference in the survival of various groups. Cox proportional regression was used to model how the risk of death depends on several predictors or variables. Estimated risks were reported as hazard ratios (HR) with 95% confidence intervals and P<0.05 was considered as having a significant association.
Results
Baseline Patient Characteristics
A total of 128 patients were followed during the study period. Males account for 81 (63%) of the overall HD patients and females were 47 (37%). Most of the patients belong to the 15–47 age groups (67; 52%). The predominant co-morbid condition was found to be diabetes with hypertension which accounts for 42%. Hypertension alone contributes 35% and diabetes is 10%. In all three co-morbid categories, males account for higher percentages than females. In terms of vascular access, most patients start with central venous catheter (CVC) but the most widely used vascular access in most patients at the time of the study was arteriovenous fistula (AVF) (82; 64%). Arteriovenous graft (AVG) is the least used vascular access in both study areas (4; 3%). Most patients had a 3-hour dialysis session thrice weekly (80% and 86%, respectively) (Table 1).
Table 1.
Baseline Characteristics of Hemodialysis Patients Admitted to St. Paul’s Hospital Millennium Medical College and Myungsung Christian Medical Center, Addis Ababa, Ethiopia
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Sex | Male | 81 | 63 |
| Female | 47 | 37 | |
| Age | 18–47 | 67 | 52 |
| 48–63 | 32 | 25 | |
| ≥64 | 29 | 23 | |
| Hypertension | Male | 28 | 35 |
| Female | 17 | ||
| Diabetes mellitus | Male | 9 | 10 |
| Female | 4 | ||
| Hypertension + diabetes | Male | 35 | 42 |
| Female | 19 | ||
| Cardiovascular access | CVC | 42 | 33 |
| AVF | 82 | 64 | |
| AVG | 4 | 3 | |
| Dialysis hour | 3 hour | 103 | 80 |
| 3.5 hour | 8 | 6 | |
| 4 hour | 17 | 14 | |
| Dialysis frequency per week | 2 times | 18 | 14 |
| 3 times | 110 | 86 |
Mortality and Survival of Hemodialysis Patients
A total of 42 (33%) HD patients died during this study period and 86 (67%) were censored. Among these censored patients, two were lost to follow-up, three of them had a kidney transplant, one patient transferred out, and for the rest of the patients the study ended. The total risk time for these patients was 143,617 person years. Forty-two deaths occurred within this time period, which gives an overall incidence rate of death as 2.9 per 10,000 person years (95% CI=2.2–4). The mortality rate for males was 2.8 per 10,000 person years, which was lower than females, 3.13 per 10,000 person years. Mortality increases with increasing age with the age group 15–47 years having lower mortality, 1.75 per 10,000 person years (95% CI=1.03–2.9) compared with the >64 age group, 6.5 per 10,000 person years (95% CI=4–11). Mortality was also higher in those who developed blood stream infection. Those patients with hypertension, diabetes mellitus, and both hypertension with diabetes had increasing incidence of risk (Table 2).
Table 2.
Incidence Rate of Hemodialysis Patients Admitted to St. Paul’s Hospital Millennium Medical College and Myungsung Christian Medical Center Addis Ababa, Ethiopia
| Variable | Category | Person Year | Event (Death) | Rate (95% CI) |
|---|---|---|---|---|
| Outcome | Death | 37,132 | 42 | 0.0011 (0.00084– 0.0015) |
| Censored | 106,485 | 0 | 0 | |
| Total | 143,617 | 42 | 0.00029 (0.00022– 0.0004) | |
| Sex | Male | 92,536 | 26 | 0.00028 (0.00019– 0.00041) |
| Female | 51,081 | 16 | 0.00031 (0.00019– 0.00051) | |
| Age group | 15–47 | 80,193 | 14 | 0.00017 (0.0001– 0.00029) |
| 48–63 | 38,693 | 12 | 0.00031 (0.00017– 0.00054) | |
| >64 | 24,461 | 16 | 0.00065 (0.0004– 0.0011) | |
| Infection | No | 92,575 | 19 | 0.00021 (0.00013– 0.00032) |
| Yes | 51,042 | 23 | 0.00045 (0.00029– 0.00068) | |
| Co-morbid | Hypertension | 56,974 | 10 | 0.00018 (0.00094– 0.00033) |
| Diabetes | 16,241 | 3 | 0.00019 (0.000059– 0.00057) | |
| HTN+DM | 55,095 | 20 | 0.00036 (0.00023– 0.00056) |
Probability of Survival Functions
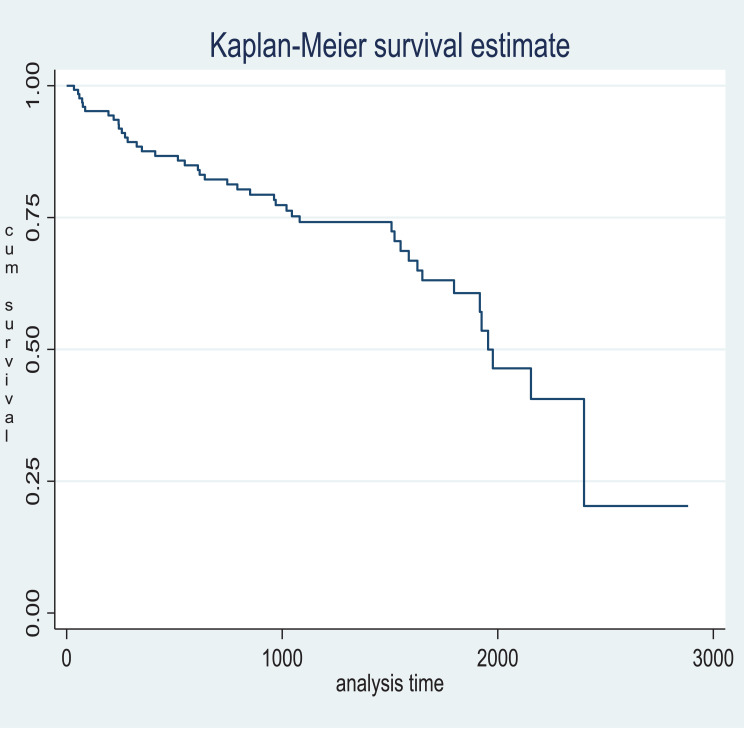
Kaplan Meier (K-M) survival function shows median survival times were to be 1,955 days. That means at least 50% of patients survived for 1,955 days or 65 months (Figure 1).
Figure 1.
Kaplan Meier (K-M) survival function.
Log Rank Test for Equality of Survivor Functions
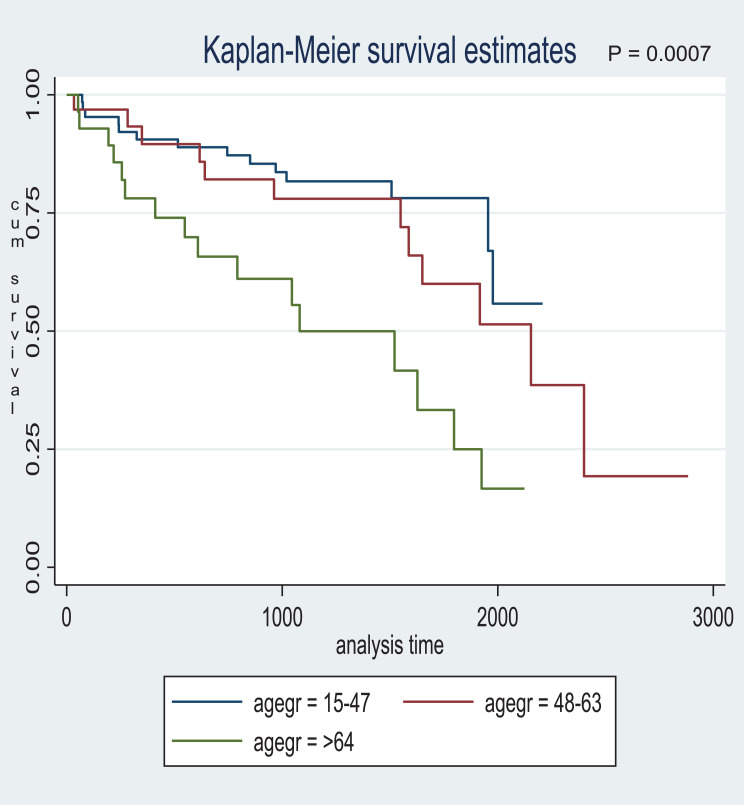
Log rank test shows a significant difference in the survival for age group, type of vascular access used, whether the patient developed infection and type of treatment facility. The Log rank test of equality of survival curves by age groups according to the results displayed in Table 3 indicated that, out of 42 deaths observed within the study period, 14 are observed from the age group 15–47 against 22.17 expected as compared to 16 observed against 7.09 expected from the age group >64. A Chi-square statistic value of 14.40 with 1 degree of freedom and a P-value of 0.0007 are recorded in the results. There is significant difference between the survival curves of the age groups. Hence, the Kaplan Meier estimate of survival curves provided in Figure 2 is significant and, thus, showed that the older age group has a lower survival time than the younger age group at both hospitals (Figure 2).
Table 3.
Log Rank Test of Equality of Survival Function Among HD Patients Admitted to St. Paul’s Hospital Millennium Medical College and Myungsung Christian Medical Center Addis Ababa, Ethiopia
| Variable | Category | Events Observed | Events Expected | Chi2 Value | p-value |
|---|---|---|---|---|---|
| Sex | Male | 26 | 27.15 | 0.14 | 0.7110 |
| Female | 16 | 14.85 | |||
| Age | 15–47 | 14 | 22.17 | 14.40 | 0.0007 |
| 48–63 | 12 | 12.74 | |||
| ≥64 | 16 | 7.09 | |||
| Type of vascular access | CVC | 19 | 9.69 | 12.08 | 0.0024 |
| AVF | 21 | 30.10 | |||
| GRAFT | 2 | 2.21 | |||
| Blood stream infection | Yes | 23 | 15.33 | 6.08 | 0.0137 |
| No | 19 | 26.67 | |||
| Dialysis frequency per week | Two | 9 | 5.84 | 2.07 | 0.1505 |
| Three | 33 | 36.16 | |||
| Treatment facility | Private | 29 | 15.5 | 20.43 | 0.0000 |
| Government | 13 | 26.5 | |||
| Dialysis hour | 3 hr | 32 | 34.61 | 1.72 | 0.4225 |
| 3.5 hr | 2 | 2.14 | |||
| 4 hr | 8 | 5.25 |
Figure 2.
Survival function by age group. P-value=0.0007.
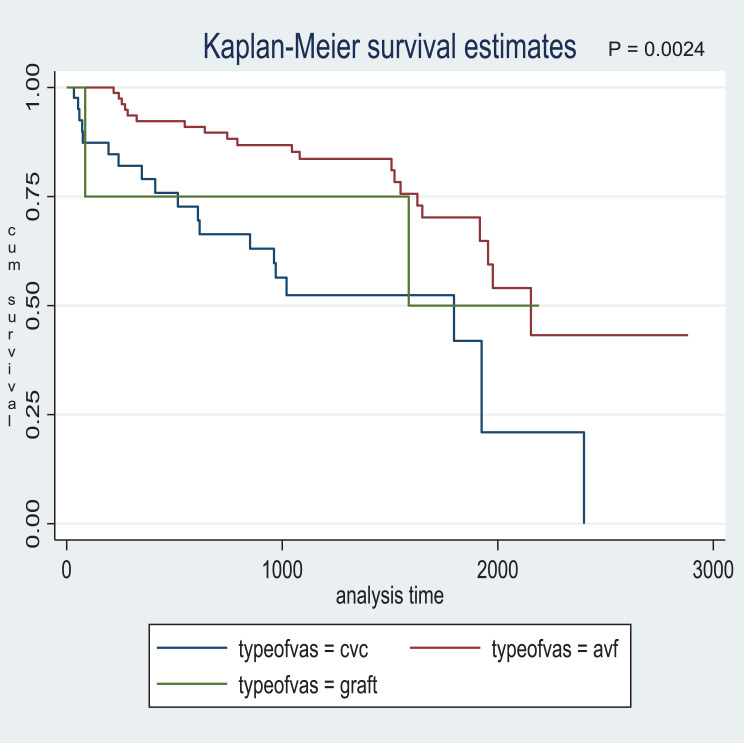
Results shown in Table 3 for type of vascular access indicated that out of 42 deaths observed within the study period, 19 are observed from the CVC against 9.69 expected as compared to 21 observed against 30.10 expected from the AVF. A Chi-square statistic value of 12.08 with 1 degree of freedom and a probability value of 0.0024 recorded in the results show a significant difference between the survival curves of the type of vascular access used. Hence, the K-M estimate of survival curves provided by Figure 3 is significant and, thus, showed that those using AVF has a higher survival time than those who use CVC at both health facilities (Figure 3).
Figure 3.
Survival functions by type of vascular access used. P-value=0.0024.
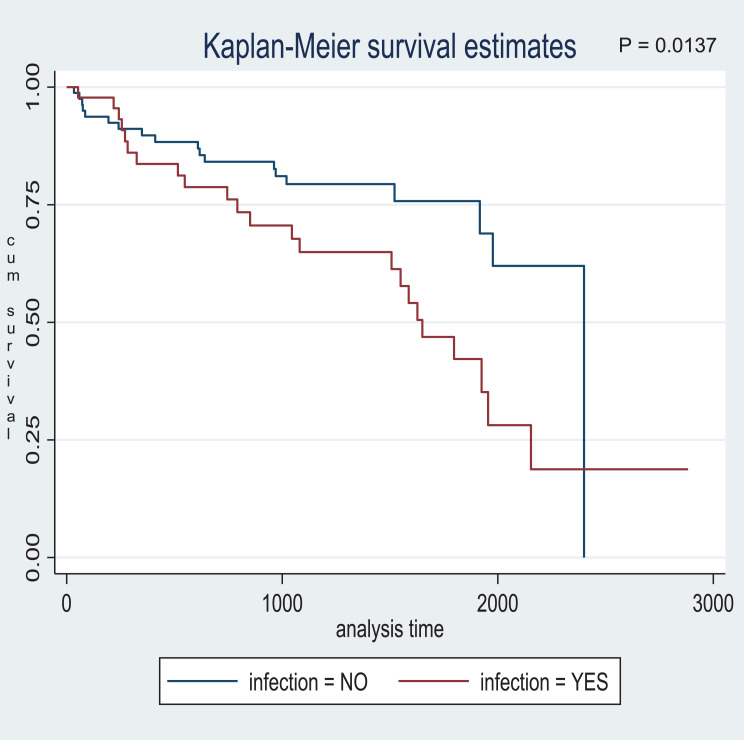
The log rank test in Table 3 indicated that, out of 42 deaths observed within the study period, 23 are observed from those who developed blood stream infection against 15.33 expected as compared to 19 observed against 26.67 expected from those who has no infection. A Chi-square statistic value of 6.08 with 1 degree of freedom and a probability value of 0.0137 show a significant difference in survival between these two groups. Hence, the K-M estimates proved to be significant. Therefore, patients who did not develop blood stream infection tend to survive longer than their counterparts (Figure 4).
Figure 4.
Survival function by blood stream infection. P-value=0.0137.
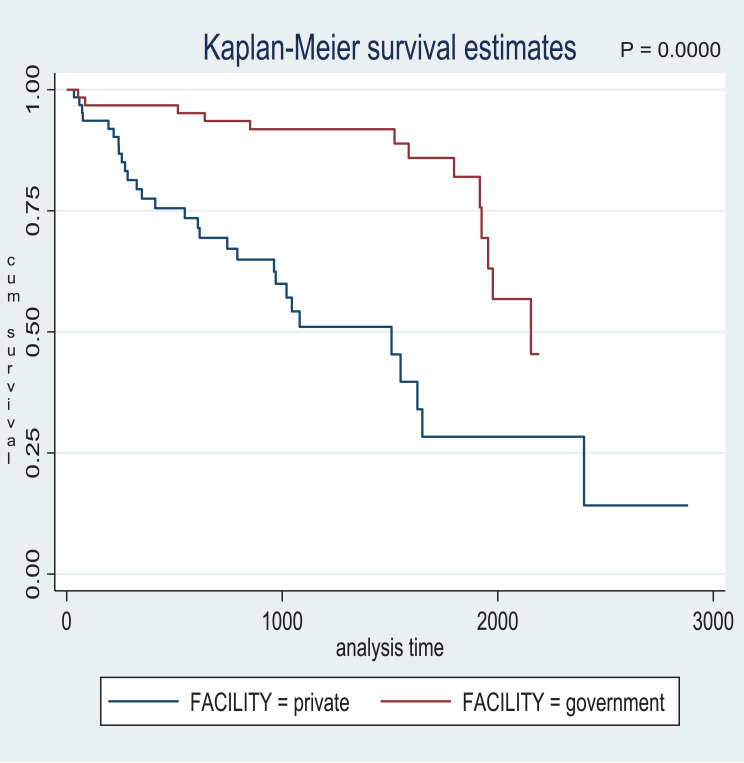
The KM estimates shown in Figure 5 for the treatment facility also proved to be significant as the log rank test indicated that out of 42 deaths observed within the study period, 29 are observed from the private hospital (MCM) against 15.5 expected as compared to 13 observed against 26.5 expected from the government hospital (SPHMMC) with a chi statistic value of 20.43, with 1 degree of freedom and a probability value of 0.0000. It can be concluded that those HD patients treated in SPHMMC survive longer (Figure 5).
Figure 5.
Survival function by treatment facility. P-value=0.0000.
Cox Proportional Hazard Regression
Predictors for Time to death were identified with Cox regression. Nine variables were selected that fulfilled the assumption of independent observation. The selected nine variables were again checked for proportional hazard (PH) assumption. Goodness of fit (GOF) test revealed all nine predictors except one (inter-dialysis weight gain) met the PH assumption. Lastly, time varying covariate tests showed only seven predictor variables were found to be fit to be included in the Cox regression model. The final multivariable (adjusted) Cox regression model is presented in Table 4.
Table 4.
Multivariable Cox Proportional Hazard Regression Output Among Hemodialysis Patients in St. Paul’s Hospital Millennium Medical College, and Myungsung Medical Center Addis Ababa, Ethiopia
| Variable | Category | Frequency | HR (95%, CI) | p-value | |
|---|---|---|---|---|---|
| Death | Censored | ||||
| Sex | Male | 26 | 55 | 0 (base) | |
| Female | 16 | 31 | 1.17 (0.56–2.49) | 0.674 | |
| Dialysis hour | 3 hr | 32 | 71 | 0 (base) | |
| 3:30 hr | 2 | 6 | 0.52 (0.11–2.54) | 0.422 | |
| 4 hr | 17 | 9 | 0.76 (0.24–2.34) | 0.629 | |
| Age group | 15–47 | 14 | 53 | 0 (base) | |
| 48–63 | 12 | 20 | 0.78 (0.33–1.87) | 0.58 | |
| ≥64 | 16 | 13 | 1.69 (0.62–4.58) | 0.304 | |
| Infection | Yes | 23 | 23 | 2.98 (1.36–6.49) | 0.006 * |
| No | 19 | 63 | 0 (base) | ||
| Dialysis frequency per week | 2 times | 9 | 9 | 0 (base) | |
| 3 times | 33 | 77 | 1.26 (0.53–2.97) | 0.601 | |
| Type of vascular access | CVC | 19 | 23 | 0 (base) | |
| AVF | 21 | 61 | 0.34 (0.16–0.73) | 0.006 * | |
| Graft | 2 | 2 | 1.26 (0.26–6.18) | 0.778 | |
| Facility | Private | 29 | 35 | 0 (base) | |
| Government | 13 | 51 | 0.21 0.08–0.54) | 0.001 * | |
Note: Significance level: * p<0.05.
Among the seven variables entered into the final model, only three variables (indicated by *) remained statistically significant at the 0.05 level of significance. Significant predictors of death were blood stream infection, type of vascular access, and treatment facility.
Accordingly, patients who developed blood stream infection at any time point during the study period were 2.98-times more likely to die than those patients who did not develop blood stream infections holding other predictors constant (HR=2.98; 95% CI=1.36–6.49).
Type of vascular access also remained statistically significant in which patients who were using AVF at any time point during the study period were 66% less likely to die than patients who were using CVC as an option for long-term use in hemodialysis patients while holding other predictors constant (HR=0.34; 95% CI=0.16–0.73).
The other statistically significant predictor of death was the treatment facility, in which patients treated in the government hospital (SPHMMC) at any time point during the study period were 79% less likely to die compared with those in the private hospital (MCM) (HR=0.21; 95% CI=0.08–0.54) (Table 4).
Discussion
The general aim of the study was to determine the overall survival status of hemodialysis patients and to find significant predictors of death in St Paul hospital millennium medical college and Myungsung Christian Medical center. The study presents the results of a 7 year retrospective study for a total number of 128 patients. The study revealed the incidence of death as 2.9 per 10,000 person years and median survival times of 1,955 days. Using AVF was associated with longer survival times than using CVC while the presence of blood stream infection was associated with lower survival times. Additionally, patients in the government-owned treatment facility had longer survival times.
The incidence of death of 2.9 per 10,000 person years was lower than a study conducted in Ayder hospital in Tigray region which puts the incidence rate as 1.4 per 1,000 person years.12 Differences in incidence could be attributed to those reasons formulated by Donabedian in his conceptual model of dimensions of care. According to the model the structure of the health care which includes equipment, human resources, and organizational characteristics such as staff training and payment methods and the processes in the facility which includes diagnosis, treatment, preventive care, and patient education all affect the outcome in HD patients.13
The Median survival times were found to be 1,955 days or 65 months. In contrast, a study conducted in Canada showed a median survival times of 39.8 months.14 This variation in survival time raises a question of how patients in a developing country have better survival times compared to a developed nation like Canada. One possible explanation to this question could be survival times highly differ across age groups. It is evident that most dialysis patients in Canada or any other developed nations are mostly older.15 But in this study most patients are 15–47 years of age, which is considered young. An additional study in one of the private hospitals in Addis Ababa shows a median survival time of only 263 days. This low number might be attributed to no pre-ESKD treatment care at the time. Also the study in Ayder hospital in Tigray region shows a median survival time of only 378 days. These studies are similar in that they contain mostly older age groups and the study in Ayder hospital was conducted for only 3 years.11,12 So it is not a surprise that younger age groups survive more since they are free from those conditions which the elderly face like frailty, concurrent co-morbid conditions, deteriorating physical and psychological conditions and the likes.16
One of the major predictors of death in the study was type of vascular access used. In this study, use of AVF is associated with lower mortality than using CVC. This result is supported by many studies including those conducted solely on vascular access type on HD patients.17 A recent study in Palestine also showed HD patients who were using CVC for HD were at approximately 50% higher risk for mortality compared with those patients with an AVF for HD access.18 Similarly, a large cohort of study in United States revealed CVC use was associated with 1.73-times higher risk for mortality when compared with AVF access.19 Disruption of dermal barriers to gain access for vascular access is the main reason for the occurrence of infection and subsequent death.20
Another predictor of death in this study was blood stream infection. The study revealed that those patients developing blood stream infection had 2.98-times higher death risk. This result corresponds to the findings of several studies which reported blood stream infection as the second leading cause of death among dialysis patients and the first cause of hospitalization.21,22 A similar study conducted in India reported that out of 113 patients, deaths due to vascular access related infections and catheter-related infection were about 36%.23 This huge proportion of death due to blood stream infection is attributed to various predisposing factors. For example, the presence of uremia, malnourishment, and diabetes mellitus, which are very common in HD patients, interact with each other to easily impair the immune system and, thus, lead to infection.24
Another finding in this study was survival difference in public and private hospitals. Although the main objective of this study was not survival comparison between public and private facilities, this study shows better patient survival in the government (SPHMMC) facility. This contradicts studies in Romania where patients enrolled in a private (for-profit) hospital generally had a better outcome than those in a government (non-profit) hospital.25 Although different factors play a role for this difference, it majorly comes down to economic factors. For example, the fact that the Addis Ababa city administration sponsored all HD patients in SPHMMC for the past 2 years favors HD patients to put their money on other necessities that increase their quality-of-life. Also, the standard three times per week HD sessions were not skipped due to financial problems, which furthers their survival probabilities. Since there is a difference in patient characteristics and clinical practices between facilities, studies which take into account this effects would potentially reveal a better conclusion.
Strength and Limitation of the Study
One of the strengths of the study is that it took the data from both private and public health facilities which make the findings more generalizable. But the study has limitations inherent to the study design. Some important variables such as single pool kt/v and BMI were not included in the study because of insufficient information in patient charts. Exclusion of these potential factors could affect the association of predictors and outcomes, especially when modeling in Cox regression. Different record keeping practices between facilities force the study to concentrate on only those factors recorded in both facilities. Additionally this study overlooks those patients who need hemodialysis but cannot afford treatment due to financial problems or shortages of dialysis machines.
Recommendations
Appropriate guidelines should be formulated and implemented by the Ministry of Health (MOH) to decrease the prevalence of end stage renal disease. Since younger age groups are being diagnosed with ESRD, the MOH should focus on prevention and conduct research on this area to limit ESRD. Physicians should keep an eye on hypertensive and diabetes patients on potential kidney failures and help to prevent the prognosis to ESRD. Further research is needed to limit mortality due to vascular access and related infections.
Conclusion
Survival times were comparable to those in developed nations which show treatment was more or less similar with the exception of individual life style. More people within the range of 15–47 years old are on HD treatment, unlike developed countries with older patients on dialysis. Co-morbid conditions, mainly hypertension and diabetes, were prevalent in HD patients. Types of vascular access used highly affect the survival outcome in HD patients. Blood stream infection contributes to increased mortality in HD patients in both SPHMMC and MCM hospitals. Cost of dialysis plays a significant role in any health care system. Most people (roughly 99%) did not have either private or public health insurance until the end of 2019. After this year the government attempted to start community-based health insurance and it is still at the beginning stage so for the study we undertook, insurance plays no role at all. The average per capita income of Ethiopians is around $936. The cost of single dialysis secession at the government facility is about $18, while in the private it is about $57. Those people who got the chance to secure a bed at the government hospital prolong their life with the minimum amount of money. This could be the reason why there was a better patient survival time in SPHMMC.
Acknowledgment
We are grateful to Yekatit 12 Hospital Medical College’s department of public health for accommodating all of our needs during this endeavor. We owe a similar obligation to all of the healthcare facilities involved in this initiative for their full cooperation to have this study done. Last but not least, we would like to acknowledge and thank the data collectors, supervisors, and data clerks of the respective healthcare facilities for their genuine support in assisting us in gathering the data for this study.
Funding Statement
The research was funded by the authors.
Abbreviations
AVF, Arteriovenous Fistula; AVG, Arteriovenous Graft; BMI, Body Mass Index; CKD, Chronic Kidney Disease; CVD, Cardiovascular Disease; CVE, Cardiovascular Events; DSL, Dialysis Secession Length; ESRD, End-Stage Renal Disease; GFR, Glomerular Filtration; GOF, Goodness of Fit; HD, Hemodialysis; HR, Hazard Ratios; KM, Kaplan Meier; LVH, Left Ventricular Hypertrophy; MCM, Myungsung Christian Medical Center; NCD, Non-Communicable Disease; PH, Proportional Hazard; RRT, Renal Replacement Therapy; SPHMMC, Saint Paul Hospital Millennium Medical College; VC, Vascular Calcification; VIF, Variance Inflation Factor.
Ethics Approval and Informed Consent
The Ethical Review Board of Yekatit 12 Hospital Medical College evaluated the research proposal and determined that obtaining informed consent was not necessary, as the study only involved the collection and analysis of existing data, documents, and information that were recorded in a manner that would prevent the direct or indirect identification of research participants. This decision was in accordance with the National Research Ethics Review Guideline, Sixth Edition, Chapter 7, Section 7.2, and was consistent with the Declaration of Helsinki. As a result, the proposal was authorized for ethical approval under protocol number 48/21. Subsequently, permission letters were issued to Saint Paul Hospital Millennium Medical College and Myungsung Christian Medical Center to proceed with data collection.
Data Sharing Statement
The research’s findings were derived from the data collected and examined using the specified techniques and resources. On request, the original data that supports this conclusion will always be made available.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Levin AS, Bilous RW, Coresh J. Chapter 1: definition and classification of CKD. Kidney Int Suppl. 2013;3(1):19–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Massarelli JJ. Harrison’s principles of internal medicine. JAMA. 1984;251(6):807. doi: 10.1001/jama.1984.03340300091039 [DOI] [Google Scholar]
- 3.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80(12):1258–1270. doi: 10.1038/ki.2011.368 [DOI] [PubMed] [Google Scholar]
- 4.Barsoum RS, Khalil SS, Arogundade FA. Fifty years of dialysis in Africa: challenges and progress. Am J Kidney Dis. 2015;65(3):502–512. doi: 10.1053/j.ajkd.2014.11.014 [DOI] [PubMed] [Google Scholar]
- 5.Hussein M, Muleta G, Seyoum D, Kifle D, Bedada D. Survival analysis of patients with end stage renal disease the case of Adama Hospital, Ethiopia. Clin Med Res. 2017;6(6):201. doi: 10.11648/j.cmr.20170606.15 [DOI] [Google Scholar]
- 6.Muleta M. Original article milestones of renal replacement therapy in Ethiopia. Ethiop Med J. 2020;3:5–13. [Google Scholar]
- 7.Thamer M, Kaufman JS, Zhang Y, Zhang Q, Cotter DJ, Bang H. Predicting early death among elderly dialysis patients: development and validation of a risk score to assist shared decision making for dialysis initiation. Am J Kidney Dis. 2015;66(6):1024–1032. doi: 10.1053/j.ajkd.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan KE, Maddux FW, Tolkoff-Rubin N, Karumanchi SA, Thadhani R, Hakim RM. Early outcomes among those initiating chronic dialysis in the United States. Clin J Am Soc Nephrol. 2011;6(11):2642–2649. doi: 10.2215/CJN.03680411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Storey BC, Staplin N, Harper CH, et al. Declining comorbidity-adjusted mortality rates in English patients receiving maintenance renal replacement therapy. Kidney International. 2018;93(5):1165–1174. doi: 10.1016/j.kint.2017.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Himmelfarb J, Vanholder R, Mehrotra R, Tonelli M. The current and future landscape of dialysis. Nat Rev Nephrol. 2020;16(10):573–585. doi: 10.1038/s41581-020-0315-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shibiru T, Gudina EK, Habte B, Deribew A, Agonafer T. Survival patterns of patients on maintenance hemodialysis for end stage renal disease in Ethiopia: summary of 91 cases. BMC Nephrol. 2013;14(1):127. doi: 10.1186/1471-2369-14-127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belachew AB, Mohammed AN, Kahsay AB. Determinants of Survival among Hemodialysis Patients at Ayder Comprehensive Specialized Hospital, Tigray, North Ethiopia: a Retrospective Cohort Study. Res Rev J Oncol Hematol. 2019;7(3):22–29. [Google Scholar]
- 13.Ibn El Haj H, Lamrini M, Rais N. Quality of care between Donabedian model and ISO9001V2008. Int J Qual Res. 2013;7(1):1. [Google Scholar]
- 14.Ebad M. Survival Analysis of Chronic Dialysis Patients. University of Waterloo; 2018. [Google Scholar]
- 15.Register COR. CORR Preliminary Report: Preliminary Statistics for Renal Failure and Solid Organ Transplantation in Canada. Ottawa, ON: Canadian Organ Replacement Register; 2008. [Google Scholar]
- 16.Anand S, Tamura MK, Chertow GM. The elderly patients on hemodialysis. Minerva Urol Nefrol Ital J Urol Nephrol. 2010;62(1):87. [PMC free article] [PubMed] [Google Scholar]
- 17.Kim DH, Park JI, Lee JP, et al. The effects of vascular access types on the survival and quality of life and depression in the incident hemodialysis patients. Ren Fail. 2020;42(1):30–39. doi: 10.1080/0886022X.2019.1702558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamadneh SA, Nueirat SA, Y. Qunibi W, Qunibi WY, Hamdan Z, Hamdan Z. Vascular access mortality and hospitalization among hemodialysis patients in Palestine. Saudi J Kidney Dis Transplant. 2018;29(1):120. doi: 10.4103/1319-2442.225184 [DOI] [PubMed] [Google Scholar]
- 19.Rivara MB, Soohoo M, Streja E, et al. Association of vascular access type with mortality, hospitalization, and transfer to in-center hemodialysis in patients undergoing home hemodialysis. Clin J Am Soc Nephrol. 2016;11(2):298–307. doi: 10.2215/CJN.06570615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ni N, Mojibian H, Pollak J, Tal M. Association between disruption of fibrin sheaths using percutaneous transluminal angioplasty balloons and late onset of central venous stenosis. Cardiovasc Intervent Radiol. 2011;34(1):114–119. doi: 10.1007/s00270-010-9875-1 [DOI] [PubMed] [Google Scholar]
- 21.Laurin L-P, Harrak H, Elftouh N, Ouimet D, Vallée M, Lafrance J-P. Outcomes of infection-related hospitalization according to dialysis modality. Clin J Am Soc Nephrol. 2015;10(5):817–824. doi: 10.2215/CJN.09210914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Powe NR, Jaar B, Furth SL, Hermann J, Briggs W. Septicemia in dialysis patients: incidence, risk factors, and prognosis. Kidney Int. 1999;55(3):1081–1090. doi: 10.1046/j.1523-1755.1999.0550031081.x [DOI] [PubMed] [Google Scholar]
- 23.Chandrashekar A, Ramakrishnan S, Rangarajan D. Survival analysis of patients on maintenance hemodialysis. Indian J Nephrol. 2014;24(4):206. doi: 10.4103/0971-4065.132985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sahathevan S, Khor B-H, Ng H-M, et al. Understanding development of malnutrition in hemodialysis patients: a narrative review. Nutrients. 2020;12(10):3147. doi: 10.3390/nu12103147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ştefan G, Podgoreanu E, Mircescu G. Hemodialysis system privatization and patient survival: a report from a large registry Eastern Europe cohort. Ren Fail. 2015;37(9):1481–1485. doi: 10.3109/0886022X.2015.1077320 [DOI] [PubMed] [Google Scholar]