Summary:
Reconstruction of lid-cheek junction defects has a known risk of ectropion. Cervicofacial flaps require significant dissection and can still be prone to ectropion. V-Y advancement flaps have been described as less morbid, but their use is limited to moderate-size defects that do not involve the lid margin. The authors present a technique of combined Tripier and V-Y advancement flaps for reconstruction of large defects of the lid-cheek junction involving the lower eyelid. A retrospective review of patients undergoing the authors’ technique was performed. A facial artery perforator flap was designed in a V-Y fashion and advanced into the cheek. An orbicularis oculi myocutaneous flap (Tripier flap) was elevated from the upper eyelid and rotated into the lower eyelid/upper cheek to meet the superior edge of the V-Y flap. A separate review of patients undergoing cervicofacial flap reconstruction was also performed. Demographics, operative details, and complications were recorded and compared. This technique was applied to five patients with large-size (19.9 ± 5.6 cm2) defects of the lid-cheek. In all cases, healing was achieved without ectropion, hematoma, infection, dehiscence, flap necrosis, or facial nerve injury. Twenty-four patients separately underwent cervicofacial flap reconstruction for defects of comparable size (15.8 ± 10.7 cm2). Two patients developed ectropion, one patient developed a hematoma, and two patients developed an infection. Combined Tripier and V-Y advancement flaps is a useful technique to reconstruct lid-cheek junction defects. This method allows for the reconstruction of large lid-cheek junction defects that involve the lid margin.
Takeaways
Question: Large defects of the lid-cheek junction are difficult to reconstruct due to the risk of ectropion. Traditional cervicofacial flaps involve significant dissection and are still at risk for ectropion, so alternative reconstructive methods are required.
Findings: We describe our novel technique of combined Tripier and V-Y advancement flaps to reconstruct large lid-cheek defects. We have successfully reconstructed large (19.9 ± 5.6 cm2) defects in five patients thus far, without any ectropion or other complications. We compared these results with 24 patients undergoing cervicofacial flap reconstruction.
Meaning: Combined Tripier and V-Y advancement flaps can successfully reconstruct large lid-cheek junction defects involving the lid margin.
INTRODUCTION
Conventional teaching recommends cervicofacial rotation-advancement flaps for the reconstruction of lid-cheek junction defects in order to minimize inferior tension on the lower eyelid and reduce the risk of ectropion.1 An inferior-to-superior V-Y advancement flap has also been described and has not been found to pose an elevated risk of ectropion.2 However, authors recommend its use be limited to defects less than 8 to 9 cm2 in size that are isolated to the cheek and do not include the lid margin. Combinations of flaps have been previously employed for defects involving the eyelid such as cervicofacial and Tripier flaps.3 We describe the use of a combined Tripier and V-Y advancement flap technique to successfully reconstruct large-size defects of the lid-cheek junction that involve the lower eyelid.
SURGICAL TECHNIQUE AND PATIENT CHARACTERISTICS
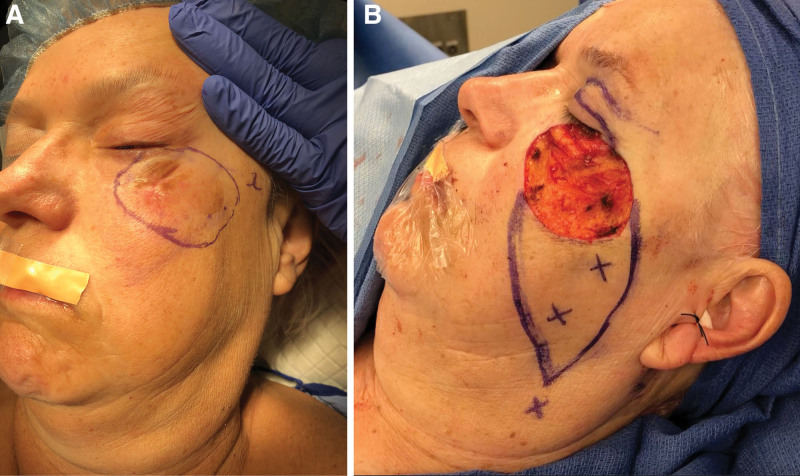
The reconstruction starts by using a Doppler probe to identify the facial artery and then designing an inferolateral fasciocutaneous perforator flap on the cheek in a V-Y advancement fashion based on perforators of the lateral facial artery. The inferior margin of the defect becomes the leading edge of this flap. Next, the pedicle of the superficial temporal artery supplying the orbicularis oculi muscle of the ipsilateral upper eyelid is identified, and then an orbicularis oculi myocutaneous flap (Tripier flap) is designed, which will be later used to resurface the lower eyelid/upper cheek (Fig. 1).
Fig. 1.
Planned excision marked preoperatively (A) with resultant defect and V-Y advancement and Tripier flap designs marked intraoperatively (B).
A tarsal strip advancement is performed to reconstruct the canthal region of the lower eyelid. The cheek V-Y advancement flap is then elevated. Incision is performed through the skin and subcutaneous tissue as well as the submuscular aponeurotic system (SMAS) layer of the cheek. The SMAS layer is split 360 degrees around the previously identified facial artery perforators, which enables a significant amount of advancement. (See Video [online], which displays the extent of V-Y flap advancement possible after 360 degree release of the submuscular aponeurotic system.)
Video 1. A video demonstrating the extent of V-Y flap advancement possible after 360 degree release of the submuscular aponeurotic system.
The flap is elevated on these perforators and advanced superiorly into the lower eyelid defect. The flap is anchored to the periosteum of the zygoma using clear nylon sutures. The flap is inset using Vicryl and Monocryl sutures. The donor site is closed primarily.
Next, the Tripier flap is elevated by incising through the skin and subcutaneous tissue of the upper eyelid as well as through the underlying orbicularis oculi muscle, then further incising the flap all the way back to the temporal area where the pedicle of the superficial temporal artery had previously been identified. This flap is then rotated into the lower eyelid defect and sutured to the facial artery perforator V-Y advancement flap to complete the reconstruction (Fig. 2).
Fig. 2.
Inset of the Tripier flap and the V-Y advancement flap.
The authors reviewed the records of all patients who underwent lid-cheek reconstruction at our institution from 2014 to 2022. Patients who underwent combined Tripier and V-Y advancement flap reconstruction were identified. Patients who underwent cervicofacial flap reconstruction were identified. Demographic data, operative details, and complications were recorded and compared using Fisher exact probability test and unpaired t test. Differences with P values of 0.05 or less were considered significant.
RESULTS
Five patients have undergone this procedure at our institution over 3 years. All patients had defects of the lid-cheek junction, underwent surgery at an ambulatory surgery center, and were discharged home on the day of surgery. All patients achieved healing without any instances of ectropion, hematoma, infection, flap necrosis, or facial nerve injury.
Twenty-four patients have separately undergone cervicofacial flap reconstruction for lid-cheek junction defects over 8 years. These patients had similar defect sizes and demographic characteristics (Table 1). Two patients (8.3%) developed ectropion, which resolved with nonoperative management. One patient (4.2%) developed a hematoma which necessitated a return to the operating room. Two patients (8.3%) developed infections which resolved with oral antibiotics.
Table 1.
Demographics, Operative Details, and Complications
| Tripier and V-Y Flap Cohort | Cervicofacial Flap Cohort | ||
|---|---|---|---|
| n = 5 (17.24%) | n = 24 (82.76%) | ||
| N (%) | N (%) | P | |
| Gender | 0.343 | ||
| Men | 1 (20.0) | 12 (50.0) | |
| Women | 4 (80) | 12 (50.0) | |
| Mean age at surgery ± SD, y | 69.4 ± 14.3 | 68.0 ± 16.5 | 0.861 |
| Current smoker | 0 | 0 | — |
| Diabetic | 2 (40.0) | 3 (12.5) | 0.195 |
| Mean length of hospital stay ± SD, d |
0 ± 0 | 0.2 ± 0.5 | 0.442 |
| Patients with hospital stay ≥ 1 d | 0 | 3 (12.5) | 0.566 |
| Mean operative time ± SD, min | 115.8 ± 30.1 | 91 ± 52.3 | 0.320 |
| Defect size ± SD, cm2 | 19.9 ± 5.6 | 15.8 ± 10.7 | 0.404 |
| Follow-up duration ± SD, d | 53.6 ± 31.7 | 48.3 ± 30.3 | 0.726 |
| Readmissions | 0 | 1 (4.2) | 1.000 |
| Total complications | 0 | 5 (20.8) | 0.565 |
| Ectropion | 0 | 2 (8.3) | 1.000 |
| Hematoma | 0 | 1 (4.2) | 1.000 |
| Infection | 0 | 2 (8.3) | 1.000 |
| Dehiscence | 0 | 0 | — |
| Flap necrosis | 0 | 0 | — |
| Facial nerve injury | 0 | 0 | — |
DISCUSSION
Cervicofacial flaps have been the conventional standard for reconstruction of the lid-cheek junction. Ectropion of the lower eyelid remains a known complication, regardless of plane of dissection or attempts to overcorrect the inset or anchor the flap at a level superior to the lateral canthus.4–7 An inferior-to-superior V-Y cheek advancement flap has been described as a less-invasive reconstructive option without posing an increased risk of ectropion. However, advocates recommend its use be limited to reconstruction of modest-size defects less than 8 to 9 cm2 in size that do not involve the lower eyelid.2 A second option for smaller defects in this area could be a horizontally-oriented V-Y flap that avoids placing downward tension on the lower lid.8
The authors have used cervicofacial flaps to reconstruct lid-cheek junction defects over the past 8 years; the observed complication rates of ectropion (8.3%), hematoma (4.2%), and infection (8.3%) are comparable to those reported by others.9 More recently, the authors have begun to use a technique of combined Tripier and V-Y advancement flaps, with promising results in five patients thus far. The authors have successfully reconstructed large-size defects (19.9 ± 5.6 cm2), some involving the lower eyelid, without any ectropion, hematoma, infection, dehiscence, or flap necrosis (Table 1).
Compared with V-Y advancement flap alone, the authors believe that by interposing an additional myocutaneous Tripier flap along the lower eyelid-cheek margin, tension from an inferior-to-superior V-Y advancement flap is directly offloaded from the eyelid, and the risk of ectropion is decreased. Because the majority of patients already have redundant upper eyelid skin, the added morbidity of incorporating the Tripier flap is minimal. Raising a V-Y advancement as an adjunct as opposed to a cervicofacial flap is less invasive, requires a smaller area of dissection, and may have lower rates of hematoma and overall complications.2 Additionally, patients undergoing cervicofacial flap reconstruction often require an overnight hospital stay. Patients undergoing the combined technique are safely discharged home on the day of surgery. The cosmesis is acceptable, with no dissatisfied patients thus far (Fig. 3). (See figure, Supplemental Digital Content, which displays the representative example of healed right-sided surgical site at 6 months postoperative. http://links.lww.com/PRSGO/C450.)
Fig. 3.
Healing surgical site at 6 weeks postoperative.
The main limitation of this study is the small sample size; therefore it is difficult to draw definitive conclusions. Future efforts should be directed at increasing the sample size and studying patients prospectively. However, the results so far are promising, demonstrating in a limited series of patients that combined Tripier and V-Y advancement flaps can successfully reconstruct large lid-cheek junction defects involving the lid margin and protect against ectropion.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Mustardé JC. The use of flaps in the orbital region. Plast Reconstr Surg. 1970;45:146–150. [PubMed] [Google Scholar]
- 2.Sugg KB, Cederna PS, Brown DL. The V-Y advancement flap is equivalent to the mustardé flap for ectropion prevention in the reconstruction of moderate-size lid-cheek junction defects. Plast Reconstr Surg. 2013;131:28e–36e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eroglu L, Simsek T, Gumus M, et al. Simultaneous cheek and lower eyelid reconstruction with combinations of local flaps. J Craniofac Surg. 2013;24:1796–1800. [DOI] [PubMed] [Google Scholar]
- 4.Kroll SS, Reece GP, Robb G, Black J. Deep-plane cervicofacial rotation-advancement flap for reconstruction of large cheek defects. Plastic and Reconstructive Surgery. 1994;94: 88–93. [DOI] [PubMed] [Google Scholar]
- 5.Nq Huynh M, Rokui S, McRae MC. An outcome comparison of superficial versus deep plane dissection of cervicofacial flaps: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2021;74:730–739. [DOI] [PubMed] [Google Scholar]
- 6.Tan ST, MacKinnon CA. Deep plane cervicofacial flap: a useful and versatile technique in head and neck surgery. Head Neck. 2006;28:46–55. [DOI] [PubMed] [Google Scholar]
- 7.Austen WG, Jr, Parrett BM, Taghinia A, et al. The subcutaneous cervicofacial flap revisited. Ann Plast Surg. 2009; 62:149–153. [DOI] [PubMed] [Google Scholar]
- 8.Marchac D, de Lange A, Bine-bine H. A horizontal v-y advancement lower eyelid flap. Plast Reconstr Surg. 2009;124:1133–1141. [DOI] [PubMed] [Google Scholar]
- 9.Rapstine ED, Knaus WJ, II, Thornton JF. Simplifying cheek reconstruction: a review of over 400 cases. Plast Reconstr Surg. 2012; 129:1291–1299. [DOI] [PubMed] [Google Scholar]