Abstract
Background
Intrapartum fetal hypoxia which is one of the leading causes of neonatal morbidity and mortality is a preventable cause. Over the past years, many methods have been employed to diagnose fetal distress, a sign of fetal hypoxia, among these, cardiotocography (CTG) is the most widely used method. Diagnosis of fetal distress based on CTG can have high inter and intraobserver variation leading to either delayed or inessential intervention henceforth increasing maternal morbidity and mortality. Fetal cord arterial blood pH is an objective method to diagnose intrapartum fetal hypoxia, hence by observing the incidence of acidemia in cord blood pH among those newborns born through cesarean section (CS) in view of non-reassuring CTG can help make a judicious decision.
Methods
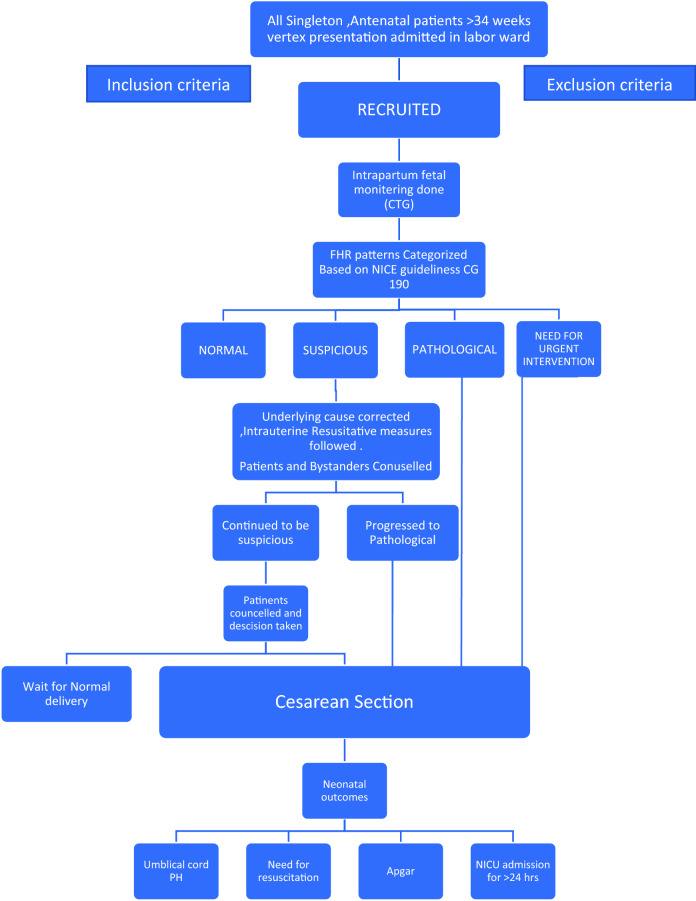
In this single institutional observational study, patients admitted for safe confinement were subjected to CTG in the latent and active phases of labor. Non-Reassuring traces were further classified based on NICE guideline CG190. The cord blood of these neonates born through CS in view of non-reassuring CTG was drawn and sent for ABG analysis.
Results
Among the 87 neonates delivered through CS in view of fetal distress, 19.5% had acidosis. Among those with pathological traces, 16(28.6%) had acidosis and one (100%) which was categorized as the need for urgent intervention showed acidosis. This result showed a statistically significant association (p value-0.003). No statistically significant association was obtained when variation in baseline characters of CTG when taken independently.
Conclusions
In our study, neonatal acidemia which is the objective evidence of fetal distress was seen in 19.5% of our study population who underwent cesarean in view of non-reassuring CTG. Among these, acidemia was significantly associated with pathological CTG trace compared to suspicious trace. We also observed that abnormal FHR features when taken independently showed no significant association with acidosis. Acidosis among newborns certainly increased the requirement for active resuscitation and additional hospital stay. Hence, we conclude that by recognizing specific fetal heart rate patterns associated with acidosis in a fetus, a more judicious decision can be made, thereby preventing both delayed as well as inessential intervention.
Keywords: Caesarean section, Cardiotocography, Fetal distress, pH, Academia
Introduction
In developing countries, birth asphyxia accounts for around seven deaths per 1000 births. The majority of deaths occur soon after birth, while few during the intrapartum period.
Birth asphyxia is an important cause of neonatal mortality and serious morbidities such as hypoxic-ischemic encephalopathy (HIE), seizures, intraventricular hemorrhage, cerebral palsy, and delayed development. The main aim of intrapartum fetal monitoring is to identify fetal hypoxia at right time to prevent subsequent acidemia and associated cell damage [1].
The ultimate goal of a health care provider is a safe mother and baby. Accurate perinatal fetal assessment is the key to safety.
CTG is one of the commonly employed methods for the detection of fetal distress by monitoring fetal heart rate and uterine contractions [2]. Accurate CTG interpretation and timely intervention ensure better neonatal outcomes.
APGAR is the most commonly used method for the assessment of newborn conditions. However, prematurity and meconium-stained liquor can alter the APGAR even in the absence of birth asphyxia. Hence, there is a need for more objective tests for the evaluation of neonates.
Neonatal cord blood acid–base analysis is one such objective tool that can reflect birth asphyxia. When the oxygen supply to the fetus is significantly disrupted, tissue oxygen deprivation with consequent acidosis occurs, and acidaemia results. The development of metabolic acidosis in the fetus is reflected in the low pH of the blood obtained from the umbilical artery soon after birth hence the most useful umbilical cord blood parameter is pH.
The identification of hypoxic cases may guide giving oxygen to these neonates to prevent the development of cerebral lesions.
The incidence of cesarean section is rising these days and one of the commonest indications cited for the same is fetal distress.
The diagnosis of fetal distress is commonly clinical in resource-constrained settings.
As the cesarean section is associated with a higher incidence of maternal morbidity and mortality, the indication for the same should be justifiable.
Hence, proving the correlation between CTG showing fetal distress with umbilical artery blood pH showing acidosis can provide us evidence concerning precise diagnosis and subsequent management at the appropriate time.
Methods
The present study is an institutional ethical and scientific committee review board-approved single institutional prospective observational study conducted over 1 year.
(September 2020–September 2021).
Selection and Description of Participants
Antenatal women with a gestational age of >34 weeks singleton pregnancy, and cephalic presentation were included in the study, while those with multifetal gestation, gestational age <34 weeks, malpresentation, and those who underwent cesarean section for indications other than fetal distress were excluded from the study. Convenience sampling was done.
Based on the proportion (53.6%) of neonatal acidemia in fetal distress observed in an earlier publication (International Journal of Reproduction, Contraception, Obstetrics, and Gynaecology) and with 20% allowable error, 95% confidence, the minimum sample size was 83 (Figs. 1 and 2).
Fig. 1.
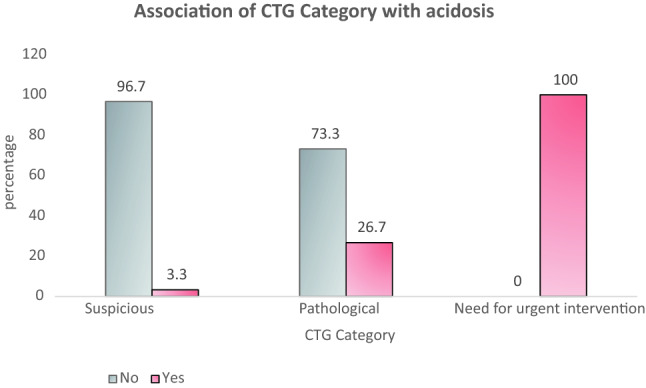
Association of CTG Category with Acidosis
Fig. 2.
Methodology
Technical Information
The primary objective of the study was to determine the incidence of acidaemia in cord blood pH among those neonates delivered through CS in view of non-reassuring CTG. The secondary objective is to study the association between acidaemia in cord blood PH and neonatal outcomes of those neonates born through CS performed in view of fetal distress.
All antenatal women > 34 weeks were admitted for further management or safe confinement, and CTG monitoring was done. The CTG machine used in the study was BPL Diva with the paper speed being 1 cm/min with an external transducer. The CTG was interpreted and classified based on NICE guideline CG 190. (Appendix 1).
The average time taken from the diagnosis to the delivery of the baby was 35 min. Either spinal or spinal-epidural anesthesia was used.
The arterial cord blood of the newborn was collected using a preheparinized 2 cc syringe soon after birth. In our hospital setting, the sample is transported through a pneumatic tube system within 5 min of sample collection.
Radiometer ABL 800 Basic was used to analyze the arterial blood gas, the average time to report the analysis was 15 min. A pH value of < 7.2 according to the institutional protocol was considered acidosis.
APGAR score of each newborn was calculated 5 min after birth was.
Other neonatal outcomes including the need for active resuscitative measures, bag and mask ventilation, chest compressions, and medications as well as neonate requiring NICU admission and further interventions were collected (Tables 1, 2, 3 and 4).
Table 1.
Association of CTG category with acidosis
| CTG Category | Acidosis | p value | |
|---|---|---|---|
| No n (%) | Yes n (%) | ||
| Suspicious | 29 (96.7) | 1 (3.3) | 0.003 |
| Pathological | 41 (73.2) | 15 (26.7) | |
| Need for urgent intervention | 0(0) | 1(100) | |
Table 2.
Association of Acidosis in newborn with the need for active resuscitation
| Active resuscitation | Acidosis | p value | |
|---|---|---|---|
| No n (%) | Yes n (%) | ||
| No | 59 (84.3) | 5 (29.4) | < 0.001 |
| Yes | 11 (15.7) | 12 (70.6) | |
Table 3.
Association of isolated FHR patterns with acidosis
| Character | Description | Acidosis | p value | |
|---|---|---|---|---|
| No n (%) | Yes n (%) | |||
| Baseline FHR | Reassuring | 54 (84.4) | 10 (15.6) | 0.063 |
| Non reassuring | 15 (71.4) | 6 (28.6) | ||
| Abnormal | 0 | 1 (100.0) | ||
| Variability | Reassuring | 41 (80.4) | 10 (19.6) | 1.000 |
| Non reassuring | 27 (79.4) | 7 (20.6) | ||
| Abnormal | 2 (100.0) | 0 | ||
| Decelerations | Persistent early deceleration | 17 (100.0) | 0 | |
| Persistent late decelerations | 24 (92.3) | 3 (11.1) | ||
| Variable decelerations | 19 (76.0) | 6 (24.0) | ||
| Prolonged decelerations | 10 (55.6) | 8 (44.4) | ||
Table 4.
Distribution of type of intervention required in the newborn with acidosis
| Type of Intervention | n (%) |
|---|---|
| Observation only | 6(41) |
| Nasal canula | 3(11.7) |
| Bubble CPAP | 4(23.5) |
| Mechanical ventilation | 4(23.5) |
Statistics
Statistical analysis was performed using IBM SPSS version 20.0 software; categorical variables are expressed by frequency and percentage. Continuous variables are presented by mean, median, SD 25 the percentile, and 75 the percentile. To test the statistical significance of the association of categorical variables with acidosis, Chi-square test was used.
To test the statistical significance of the difference in the median hospital stay for acidosis, Mann–Whitney U test was used.
Results
A study was conducted among 87 antenatal women with mean maternal age of 29.32yrs (+/ − 4.9yrs). Out of which 62 (71.3%) were primigravida and 25(28.7%) were multiparous women. It includes 23 (26.4%) preterm and 64 (73.6%) term patients. The onset of labor was spontaneous among 39(44.8%) women and 48 (55.2%) were induced. CTG traces were interpreted, 30 (34.5%) were suspicious, 56(64.4%) were pathological, and 1(1.1) Need for urgent intervention out of which 17(19.5 %) babies were acidotic. Among 56 pathological CTG traces, 15 newborns were acidotic while among 30 suspicious traces and 1 need for urgent intervention, one in each group was acidotic. This association was statistically significant with a p value of 0.003. Individual characters like baseline variability, baseline FHR and different types of decelerations were analyzed and none had a statistically significant association with acidosis. Among the neonates with reassuring APGAR, 6 (6.8%) were acidotic while the remaining 62 were normal. Among the neonates with moderately abnormal APGAR, 9(10.3%) were acidotic. Both the neonates with acidosis had low APGAR at 5 min. In this study, 21.8% (n =19) of deliveries were complicated with MSL of which only 10.5 % (n=2) were associated with acidosis. There was a statistically significant association between acidotic newborn and requirement for active resuscitation at birth with a p value of <0. 001. The median hospital stay was 5 days (0–30). Among those neonates without acidosis compared to 7 days (4–90 days) in those with acidosis. This finding achieved a statistically significant association with a p value of 0.002.
Discussion
The most common and routinely practiced method to diagnose fetal distress is CTG, which most other studies have concluded has a high false-positive rate leading to an increased frequency of inessential intervention. This is due to high inter- and intraobserver variation. Hence, it calls for an objective method for analyzing the CTG and timely decision-making. Henceforth, various guidelines have been proposed for cardiotocography interpretation. In this study, NICE guideline CG 190 has been used for CTG interpretation. There has been previous literature validating these guidelines. Eighty-seven patients who underwent cesarean section because of non-reassuring CTG were included in the study. CTG Interpretation was later correlated to cord blood pH and significant perinatal outcomes. Cord blood pH was used, as it has shown to provide objective evidence of hypoxia during labor and is found to be more resourceful than APGAR alone.
Disagreements concerning the ability of abnormal fetal heart rate patterns to predict fetal well-being still exist. While many authors found abnormal fetal heart rate patterns significantly associated with adverse outcomes [3–6], others did not. However, most studies have concluded that these abnormal FHR patterns led to increased intervention in terms of operative vaginal deliveries or cesarean sections [7, 8].In our study, fetal monitoring was done in latent and active phase labor. Abnormal CTG was further classified, into suspicious (34.5%), pathological (64.4%), and need for immediate intervention tracing (1.1%) before subjecting to cesarean section.
In this study, pH < 7.2 was taken as a cutoff value to define acidosis in a neonate according to institutional protocol, Kaban et al. used the cutoff value for defining acidosis as cord blood pH < 7.2.
However, Modarressnejad V used a cutoff value of pH < 7.1.7 to define acidosis. Of 87 neonates included in the study,17 (19.5%) neonates had acidosis (pH < 7.2) while the remaining 70 (80.5%) neonates were born healthy and without acidosis. As most fetuses were shown to tolerate acidaemia during labor with a pH cutoff of 7.0 without experiencing neurologic impairment, [9, 10], the clinical importance of these findings is debatable.
In our study, there was no significant difference among either gender who developed acidosis. Conversely, previous studies like Lau et al. [11] showed that male fetuses were at higher risk for developing distress during labor. This discrepancy can be because of our small sample size, therefore, larger studies are required for more appropriate results.
In our study, intrauterine resuscitative measures as mentioned above were used in response to abnormal FHR, thereby confounding the analysis of the correlation between the outcome and the observed abnormality. However, patients with persistent abnormal FHR who underwent cesarean section were only included in the study leaving a smaller sample size.
In our study, it is evident that there is a significant association between the intrapartum CTG category and acidosis among neonates. This association was confirmed in a study by Aboulghar W et al. who also concluded that pathological CTG rather than suspicious CTG increased the risk of acidosis significantly. But none of the newborns had HIE, hence accurate interpretation and timely intervention can help reduce morbidity and mortality among newborns.
Apart from bradycardia, none of the FHR patterns in our study were independently associated with fetal acidosis. As confirmed by Lau TK et al., if decelerations are not accompanied by a rise in FHR baseline (or tachycardia) with worsening variability, they do not represent fetal hypoxia [12]. Prolonged deceleration in our study has shown to be substantially associated with acidosis as seen in 44% neonates.
As concluded by Lysander et al. they study that “There was no significant difference between those with MSL and those without MSL in terms of pH [13]”. In this study, 21.8% (n = 19) of deliveries were complicated with MSL of which only 10.5% (n = 2) were associated with acidosis.
APGAR score, despite the controversy concerning its reliability as a measure for morbidity in newborns, is in wide practice to evaluate the newborn condition and the need for immediate resuscitation. In this study, newborns with acidosis certainly had poor APGAR scores. But among those with APGAR > 7 at 5 min, six neonates (8%) had acidosis. In a study conducted by Anyaegbunam A et Al., 20.7% had an abnormal pH (< 7.20) and normal Apgar (> 7). Respiratory acidosis unlike metabolic acidosis is of less concern and tends to settle soon after birth. Hence, many of these infants with low arterial cord pH may have a normal 5-min Apgar score. [14].In a study by Richa Gangwar et al., which included 146 neonates, poor outcomes were seen in 14% of cases which is comparable to our study where 12.7% of neonates had poor outcomes requiring further intervention. [15].
However, neonatal acidaemia is weakly associated with adverse outcomes. Most neonates with neurological morbidity have normal cord pH values. Other variables must influence adverse outcomes and account for more of these than acidaemia.
In the study by Sunitha et al., no significant association was found between abnormal CTG patterns with that of NICU admission (p value − 0.5). In a study conducted by Gupta et al., similar findings were noted [16]. In agreement with other studies, in this study, no significant association was found between the type of CTG trace and the requirement for NICU admission (p value = 0.106) In our study, 23 babies were admitted to NICU for observation and further management.
Strengths and Limitations
Strengths
Availability of CTG monitoring for all the in-labor patients and round-the-clock availability of facilities for emergency interventions. Every CTG in the study was followed by only one observer, hence overcoming the inter-observer variation in interpretation. During analyzing the arterial blood gases, value error is minimized as the investigation is done in the same standardized laboratory.
Limitations: Small sample size. Lack of facilities like fetal blood sampling (FBS), decisions had to be taken only based on CTG findings without adjuvant confirmatory test. The positive and negative predictive values of CTG could not be calculated since our study included only those with abnormal CTG traces. In this study, we could not perform long-term follow-up, hence long-term problems like mental retardation, cerebral palsy, and poor school performance could not be observed.
Conclusions
In our study, neonatal acidemia which is objective evidence of fetal distress was seen in 19.5% of our study population who underwent cesarean in view of non-reassuring CTG. Among these, acidemia was significantly associated with pathological CTG trace compared to suspicious trace. We also observed that abnormal FHR features when taken independently showed no significant association with acidosis. Acidosis among newborns certainly increased the requirement for active resuscitation and additional hospital stay. Hence, we conclude that by recognizing specific fetal heart rate patterns associated with acidosis in a fetus, a more judicious decision can be made, thereby preventing both delayed as well as inessential intervention.
Appendix 1
Interpretation of CTG, Adapted from NICE Clinical Guideline 190
| Description | Feature | ||
|---|---|---|---|
| Baseline (beats/ minute) | Baseline variability (beats/ minute) | Decelerations | |
| Reassuring | 110–160 | 5–25 | None or early Variable decelerations with no concerning characteristics* for less than 90 min |
| Nonreassuring | 100–109 OR 161–180 | Less than 5 for 30–50 min OR More than 25 for 15–25 min | Variable decelerations with no concerning characteristics* for 90 min or more OR Variable decelerations with any concerning characteristics* in up to 50% of contractions for 30 min or more OR Variable decelerations with any concerning characteristics* in over 50% of contractions for less than 30 min OR Late decelerations in over 50% of contractions for less than 30 min, with no maternal or fetal clinical risk factors such as vaginal bleeding or significant meconium |
| Abnormal | Below 100 OR Above 180 | Less than 5 for more than 50 min OR More than 25 for more than 25 min OR Sinusoidal | Variable decelerations with any concerning characteristics* in over 50% of contractions for 30 min (or less if any maternal or fetal clinical risk factors OR Late decelerations for 30 min (or less if any maternal or fetal clinical risk factors) OR Acute bradycardia, or a single prolonged deceleration lasting 3 min or more |
*Regard the following as concerning characteristics of variable decelerations: lasting more than 60 s; reduced baseline variability within the deceleration; failure to return to baseline; biphasic (W) shape; no shouldering. † Although a baseline fetal heart rate between 100 and 109 beats/minute is a non-reassuring feature, continue usual care if there is normal baseline variability and no variable or late decelerations.
Management Based on Interpretation of Cardiotocograph Traces
| Category | Definition | Management |
|---|---|---|
| Normal | All features are reassuring |
Continue CTG (unless it was started because of concerns arising from intermittent auscultation and there are no ongoing risk factors; see recommendation 1.10.8) and usual care Talk to the woman and her birth companion(s) about what is happening |
| Suspicious |
1 Non-reassuring feature AND 2 Reassuring features |
Correct any underlying causes, such as hypotension or uterine hyperstimulation Perform a full set of maternal observations Start 1 or more conservative measures* Inform an obstetrician or a senior midwife Document a plan for reviewing the whole clinical picture and the CTG findings Talk to the woman and her birth companion(s) about what is happening and take her preferences into account |
| Pathological | 1 Abnormal feature OR 2 non-reassuring features |
Obtain a review by an obstetrician and a senior midwife Exclude acute events (for example, cord prolapse, suspected placental abruption, or suspected uterine rupture) Correct any underlying causes, such as hypotension or uterine hyperstimulation Start 1 or more conservative measures* Talk to the woman and her birth companion(s) about what is happening and take her preferences into account If the cardiotocograph trace is still pathological after implementing conservative measures:—obtain a further review by an obstetrician and a senior midwife—offer digital fetal scalp stimulation (see recommendation 1.10.38) and document the outcome If the cardiotocograph trace is still pathological after fetal scalp stimulation:—consider fetal blood sampling—consider expediting the birth—take the woman's preferences into account |
| Need for urgent intervention | Acute bradycardia, or a single prolonged deceleration for 3 min or more |
Urgently seek obstetric help If there has been an acute event (for example, cord prolapse, suspected placental abruption, or suspected uterine rupture), expedite the birth Correct any underlying causes, such as hypotension or uterine hyperstimulation Start 1 or more conservative measures* Make preparations for an urgent birth Talk to the woman and her birth companion(s) about what is happening and take her preferences into account Expedite the birth if the acute bradycardia persists for 9 min If the fetal heart rate recovers at any time up to 9 min, reassess any decision to expedite the birth, in discussion with the woman |
* If there are any concerns about the baby's well-being, be aware of the possible underlying causes and start one or more of the following conservative measures based on an assessment of the most likely cause(s): encourage the woman to mobilize or adopt an alternative position (and to avoid being supine); offer intravenous fluids if the woman is hypotensive; reduce contraction frequency by reducing or stopping oxytocin if it is being used and/or offering a tocolytic drug (a suggested regimen is subcutaneous terbutaline 0.25 mg).
Funding
No funding was obtained from any agency.
Declarations
Conflict of interest
This is an original article based on a prospective study performed at the Amrita Institute of Medical Sciences, Kochi, Kerala, India. The authors declare that there is no conflict of interest related to this work.
Ethical Approval
This study was approved by the Institutional review board and ethics committee. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
Informed consent was taken from all the participants in the study.
Footnotes
Vinya Paladugu (MBBS) is a Junior Resident at Department of obstetrics and gynecology, Amrita Institute of Medical Sciences, Kerala, India. Sarala Sreedhar is an Professor at Department of Obstetrics and Gynaecology. R.Chitra is an Associate Professor at Department of Obstetrics and Gynaecology. Sai Tejaswi Mannava is a Junior Resident at Department of Obstetrics and Gynaecology. Saranya Sreekumar is an Assistant Professor at Department of Obstetrics and Gynaecology. Janu Mangalakanthi is an Associate Professor at Department of Obstetrics and Gynaecology.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Beard RW, Filshie GM, Knight CA, et al. The significance of the changes in the continuous fetal heart rate in the first stage of labor. J Obstet Gynaecol Br Commonw. 1971;78(10):865–881. doi: 10.1111/j.1471-0528.1971.tb00198.x. [DOI] [PubMed] [Google Scholar]
- 2.Stout MJ, Cahill AG. Electronic fetal monitoring: past, present, and future. Clinics in Perinatology. 2011;38(1):127–142. doi: 10.1016/j.clp.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Krebs HB, Petres RE, Dunn LJ. Intrapartum fetal heart rate monitoring. Am J Obstet Gynecol. 1983;145(3):297–305. doi: 10.1016/0002-9378(83)90714-7. [DOI] [PubMed] [Google Scholar]
- 4.Gilstrap LC, Hauth JC, Toussaint S. Second stage fetal heart rate abnormalities and neonatal acidosis. Obstet Gynecol. 1984;63(2):209–213. [PubMed] [Google Scholar]
- 5.Tranquilli AL. Fetal heart rate in the second stage of labor: recording, reading, interpreting, and acting. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2012;25(12):2551–2554. doi: 10.3109/14767058.2012.718395. [DOI] [PubMed] [Google Scholar]
- 6.Gull I, Jaffa AJ, Oren M, et al. Acid accumulation during end-stage bradycardia in term fetuses: how long is too long? Br J Obstet Gynaecol. 1996;103(11):1096–1101. doi: 10.1111/j.1471-0528.1996.tb09589.x. [DOI] [PubMed] [Google Scholar]
- 7.Loghis C, Salamalekis E, Panayotopoulos N, et al. The effect of early second stage bradycardia on newborn status. Eur J Obstet Gynecol Reprod Biol. 1997;72(2):149–152. doi: 10.1016/S0301-2115(96)02683-8. [DOI] [PubMed] [Google Scholar]
- 8.Morgan JA, Hankins ME, Wang Y, et al. Prolonged Fetal Heart Rate Decelerations in Labor: Can We Reduce Unplanned Primary Cesarean Sections in This Group? Adv Ther. 2020;37(10):4325–4335. doi: 10.1007/s12325-020-01468-x. [DOI] [PubMed] [Google Scholar]
- 9.Freeman JM, Nelson KB. Intrapartum asphyxia and cerebral palsy. Pediatrics. 1988;82(2):240–249. doi: 10.1542/peds.82.2.240. [DOI] [PubMed] [Google Scholar]
- 10.Gilstrap LC, Leveno KJ, Burris J, et al. Diagnosis of birth asphyxia based on fetal pH, Apgar score, and newborn cerebral dysfunction. Am J Obstet Gynecol. 1989;161(3):825–830. doi: 10.1016/0002-9378(89)90410-9. [DOI] [PubMed] [Google Scholar]
- 11.Lau TK, Chung KH, Haines CJ, et al. Fetal sex as a risk factor for fetal distress leading to abdominal delivery. Aust N Z J Obstet Gynaecol. 1996;36(2):146–149. doi: 10.1111/j.1479-828X.1996.tb03271.x. [DOI] [PubMed] [Google Scholar]
- 12.Vintzileos AM, Smulian JC. Decelerations, tachycardia, and decreased variability: have we overlooked the significance of longitudinal fetal heart rate changes for detecting intrapartum fetal hypoxia? Am J Obstet Gynecol. 2016;215(3):261–264. doi: 10.1016/j.ajog.2016.05.046. [DOI] [PubMed] [Google Scholar]
- 13.Lysander SD, Jayalalitha PC. Correlation between umbilical cord blood pH and meconium stained deliveries. Int J Contemp Pediatrics. 2020;7(3):670. doi: 10.18203/2349-3291.ijcp20200698. [DOI] [Google Scholar]
- 14.Anyaegbunam A, Fleischer A, Whitty J, et al. Association between Umbilical Artery Cord pH, Five-Minute Apgar Scores and Neonatal Outcome. Gynecol Obstet Invest. 1991;32(4):220–223. doi: 10.1159/000293036. [DOI] [PubMed] [Google Scholar]
- 15.Gangwar R, Chaudhary S. Caesarean Section for Foetal Distress and Correlation with Perinatal Outcome. J Obstet Gynaecol India. 2016;66(Suppl 1):177–180. doi: 10.1007/s13224-015-0831-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta M, Gupta P. Role of cardiotocography in high risk pregnancy and its correlation with increase cesarean section rate. Int J Reprod Contracept Obstet Gynecol. 2016;20(6):168. doi: 10.18203/2320-1770.ijrcog20164651. [DOI] [Google Scholar]