Abstract
Selective serotonin reuptake inhibitors (SSRIs) are the most common antidepressants used due to their comparatively less cardiotoxic effects than tricyclic antidepressants. Corrected QT interval (QTc) prolongation is the most common electrocardiography (ECG) change that has been encountered with SSRI overdose. This case report is about a 22-year-old woman who was brought to the emergency department (ED) with an alleged history of consumption of 200 mg of escitalopram. Her ECG showed T-wave inversions in anterior leads one to five, which reverted (in leads four and five) the next day with supportive management. After 24 hours, she developed dystonia, which resolved with mild doses of benzodiazepine. Hence, ECG changes like T-wave inversions may occur even with a small overdose of an SSRI without any significant adverse effects.
Keywords: ssri, qtc prolongation, t wave inversions, ecg changes, overdose, emergency medicine
Introduction
Drug-induced arrhythmias can lead to serious cardiovascular events such as torsade de pointes and sudden cardiac arrest [1]. QT interval prolongation is accepted as a surrogate marker for identifying the proarrhythmic potential of a drug under development [2]. Various anti-depressants and antipsychotic medications have been shown to cause prolongation of the QT interval in adults across a wide age range [3]. The cardiovascular effects of antidepressants have been the subject of recent debate, and the dose of citalopram was modified owing to the risk of QTc prolongation [4].
Escitalopram, which is a selective serotonin reuptake inhibitor (SSRI), is an S-enantiomer of citalopram used for the treatment of anxiety disorder and depression. According to FDA reports, thorough QT (TQT) studies showed that citalopram causes significant prolongation of the QT interval at a dose of 60 mg/day, whereas escitalopram causes a prolongation of the QT interval in a dose-dependent manner without clinically relevant findings [5]. However, there are no studies showing that QTc prolongation can have clinically negative outcomes, such as sudden cardiac death [6].
This case report is about a 22-year-old woman who presented to the emergency department (ED) with an escitalopram overdose and developed ECG changes.
Case presentation
A 22-year-old woman was brought to the emergency department with a history of consuming 20 tablets of escitalopram (10 mg) one hour prior to her presentation to the ED, followed by one episode of vomiting and agitation after that. She had a medical history of depressive disorder for two years, during which she was on escitalopram and clonazepam tablets.
On physical examination, her vitals were as follows: pulse rate: 102/min, blood pressure: 130/80 mm Hg, respiratory rate: 20/min, oxygen saturation: 97% on room air, and temperature: 97.6°F. There were old hesitation cuts on the flexor aspect of her left wrist. She was fully conscious and oriented, and her systemic exam was within normal limits.
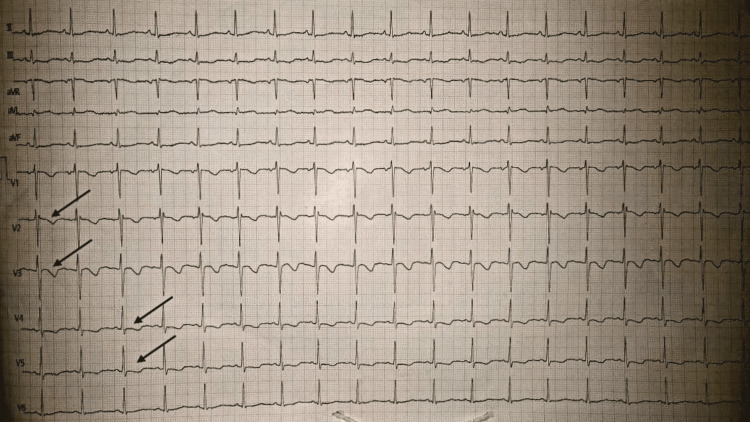
An ECG demonstrated T-wave inversions in the precordial chest that led from one to five, as can be seen in Figure 1.
Figure 1. An ECG showing T-wave inversions in precordial leads.
The patient was given gastric lavage in the emergency department, and her vitals were closely monitored. Routine investigations, comprising a complete hemogram, liver function tests, and kidney function tests, were within normal limits. A gastric lavage sample sent for toxicologic analysis confirmed the diagnosis.
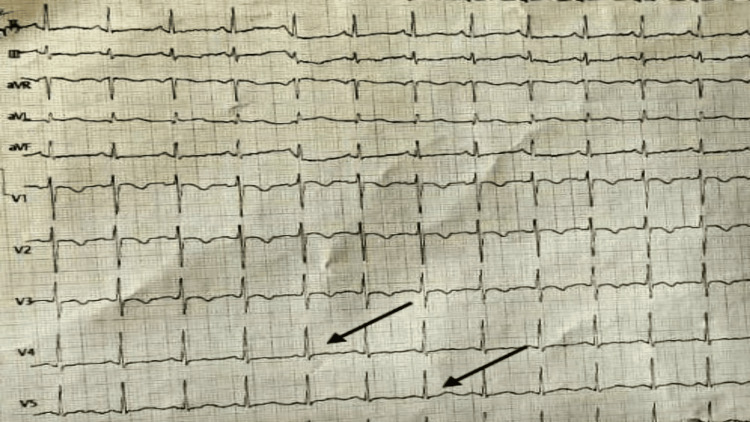
The patient was admitted to the intensive care unit. The two-dimensional echo showed a normal study with good left ventricular systolic function (LVEF of 60%). She was given psychotherapy in the form of dialectical behavior therapy, which consisted of group skills training, individual therapy, etc. Her ECG changes reverted in leads four and five the next day, as can be seen in Figure 2.
Figure 2. A repeat ECG showing upright T-waves in precordial leads four and five.
Twenty-four hours later, the patient developed dystonia and exaggerated bilateral knee jerks. Magnetic resonance imaging of the brain showed no obvious abnormalities in the brain parenchyma. She was managed with low doses of benzodiazepines and her symptoms subsided gradually. She became stable and was discharged on the fifth day after admission.
Discussion
Overdoses with SSRIs alone rarely cause fatalities, and most patients improve without any sequelae. A moderate overdose (30 times the daily dose) leaves no or minor symptoms. At 50-75 times the daily dose, there can be symptoms like drowsiness, tremor, nausea, and vomiting. At higher doses, serious adverse effects like ECG changes, decreased level of consciousness, and seizures may occur. Fatalities may occur with exceptionally large acute overdoses (>150 times the usual daily dose), especially when co-ingested with other drugs [7].
A comparative analysis of antidepressant overdoses in suicidal adults found that although all SSRIs had low hazard indices, citalopram had the highest hazard index among the SSRIs [8]. In addition to the mild transient complaints seen with all SSRIs, citalopram produces seizures and QT prolongation, which ranges from 12% to 68% in case series involving admitted adult patients [9]. Patients have developed torsades de pointes (TdP) with either therapeutic or supratherapeutic doses of citalopram [10-13].
This case report is of a 22-year-old woman who presented to the emergency department with an SSRI overdose of 200 mg and symptoms of irritability and agitation. Her ECG showed T-wave inversions in the anterior chest leads (one to five), which reverted after supportive management without any two-dimensional echo changes or adverse clinical sequelae. She developed dystonia, which gradually subsided with benzodiazepines.
ECG changes with such a small overdose of SSRI have not been reported in the literature to date. The majority of the studies reported showed QTc prolongation as ECG changes with SSRI overdosage, but no studies showing T-wave inversions were reported. However, other physiological causes of T wave inversions, such as those seen in anemic patients, females, and athletes, should be considered. Although very little is known about the adverse effects of SSRI overdose, very few case fatalities have been reported, making them safer than tricyclic antidepressants (TCAs). More research should be done on patients focusing on ECG changes with mild SSRI overdoses to see if there is a causal relationship.
Conclusions
T-wave inversion with SSRI overdose has not been reported to date. ECG changes may occur with a mild overdose of an SSRI. Hence, close monitoring is recommended in patients with SSRI overdose, even though SSRIs are considered much safer than tricyclic antidepressants. T-wave inversions may be seen in the anterior leads in normal individuals also, which may produce a dilemma in diagnosis. However, a thorough history-taking and investigation may aid in the diagnosis.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Genetic variations of KCNQ1, KCNH2, SCN5A, KCNE1, and KCNE2 in drug-induced long QT syndrome patients. Paulussen AD, Gilissen RA, Armstrong M, et al. J Mol Med (Berl) 2004;82:182–188. doi: 10.1007/s00109-003-0522-z. [DOI] [PubMed] [Google Scholar]
- 2.A thorough QT study to evaluate the QTc prolongation potential of two neuropsychiatric drugs, quetiapine and escitalopram, in healthy volunteers. Kim A, Lim KS, Lee H, et al. Int Clin Psychopharmacol. 2016;31:210–217. doi: 10.1097/YIC.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 3.Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. Beach SR, Kostis WJ, Celano CM, Januzzi JL, Ruskin JN, Noseworthy PA, Huffman JC. J Clin Psychiatry. 2014;75:0–9. doi: 10.4088/JCP.13r08672. [DOI] [PubMed] [Google Scholar]
- 4.QTc prolongation, torsades de pointes, and psychotropic medications. Beach SR, Celano CM, Noseworthy PA, Januzzi JL, Huffman JC. Psychosomatics. 2013;54:1–13. doi: 10.1016/j.psym.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Drug Safety Communication. [ Nov; 2022 ]. 2011. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-revised-recommendations-celexa-citalopram-hydrobromide-related https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-revised-recommendations-celexa-citalopram-hydrobromide-related
- 6.Association between citalopram, escitalopram and QTc prolongation in a real-world geriatric setting. Crépeau-Gendron G, Brown HK, Shorey C, et al. J Affect Disord. 2019;250:341–345. doi: 10.1016/j.jad.2019.02.060. [DOI] [PubMed] [Google Scholar]
- 7.SSRI safety in overdose. Barbey JT, Roose SP. https://www.nlm.medscape.idmu.unboundmedicine.unboundmedicine.com/medline/citation/9786310/SSRI_safety_in_overdose_. J Clin Psychiatry. 1998;59 Suppl 15:42–48. [PubMed] [Google Scholar]
- 8.Suicidal antidepressant overdoses: a comparative analysis by antidepressant type. White N, Litovitz T, Clancy C. J Med Toxicol. 2008;4:238–250. doi: 10.1007/BF03161207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose. Isbister GK, Bowe SJ, Dawson A, Whyte IM. J Toxicol Clin Toxicol. 2004;42:277–285. doi: 10.1081/clt-120037428. [DOI] [PubMed] [Google Scholar]
- 10.Citalopram-induced long QT syndrome and torsade de pointes: role for concomitant therapy and disease. de Gregorio C, Morabito G, Cerrito M, Dattilo G, Oreto G. Int J Cardiol. 2011;148:226–228. doi: 10.1016/j.ijcard.2009.05.060. [DOI] [PubMed] [Google Scholar]
- 11.Citalopram induced torsade de pointes, a rare life threatening side effect. Kanjanauthai S, Kanluen T, Chareonthaitawee P. Int J Cardiol. 2008;131:0–4. doi: 10.1016/j.ijcard.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Torsade de pointes induced by citalopram and amiodarone. Fayssoil A, Issi J, Guerbaa M, Raynaud JC, Heroguelle V. Ann Cardiol Angeiol (Paris) 2011;60:165–168. doi: 10.1016/j.ancard.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Drug-induced torsades de pointes: a review of the Swedish pharmacovigilance database. Aström-Lilja C, Odeberg JM, Ekman E, Hägg S. Pharmacoepidemiol Drug Saf. 2008;17:587–592. doi: 10.1002/pds.1607. [DOI] [PubMed] [Google Scholar]