Abstract
The “postage stamp fracture” is an anterior glenoid rim fracture following arthroscopic repair of a Bankart lesion. Often occurring at the time of an acute trauma, a fracture line propagates though the previous Bankart repair anchor sites, resulting in recurrent anterior instability of the glenohumeral joint. The resultant glenoid rim fracture edge gives a similar appearance as the edge of a stamp, with the osseous edge having the classic “perforation” pattern. When patients present with a postage stamp fracture, even in the setting of subcritical glenoid bone loss, we believe that additional soft-tissue stabilization procedures and/or fracture fixation pose a significant risk of failure. In our opinion, a Latarjet procedure is recommended in a majority of patients with a postage stamp fracture for restoration of glenohumeral stability. The procedure offers a reliable, reproducible surgical intervention that controls for many of the factors that can make arthroscopic revision unreliable, such as poor bone quality, adhesions, labral degeneration, and bone loss. Here, we outline our preferred surgical technique to restore glenohumeral stability using the Latarjet procedure for a patient with a postage stamp fracture.
The “postage stamp fracture” is an anterior glenoid rim fracture following arthroscopic repair of a Bankart lesion.1 Often occurring at the time of an acute trauma, a fracture line propagates though the previous Bankart repair anchor sites, resulting in recurrent anterior instability of the glenohumeral joint. The resultant glenoid rim fracture edge gives a similar appearance as the edge of a stamp, with the osseous edge having the classic “perforation” pattern.
Risk factors associated with increased risk of a postage stamp fracture include younger age (<25 years old), involvement in a contact sport, use of >3 anchors at time of initial Bankart repair, presence of osteolysis at anchor sites in the anterior glenoid, and use of knotted suture anchors. These fractures often occur at a mean interval of 12 to 24 months following arthroscopic Bankart repair.2
Osseous deficiency has been increasingly recognized as a major risk factor for glenohumeral instability. Initial cadaveric studies of glenohumeral stability suggested that glenoid width bone loss of 19% to 21% significantly compromised soft-tissue repairs.3,4 As we have gained a better understanding of how the glenoid surface area influences glenohumeral stability, we now know that smaller amounts of bone loss, often termed as “subcritical” bone loss can and often are associated with poorer outcomes following soft-tissue–based procedures.5
Patient Evaluation
Patient evaluation in the clinical setting should begin with a thorough history, specifically noting previous surgical history and timing, location of surgical incision, the timing of return of instability and trauma associated with this return, amount of instability events, nocturnal instability, pain, position of maximum instability, and a complete neurovascular examination of the upper extremity.
Imaging
Office imaging should begin with standard radiographs, including anteroposterior, scapular-Y, axillary, and West Point view. Once glenoid insufficiency is confirmed on radiographs (Fig 1), advanced imaging is recommended. We prefer using both magnetic resonance imaging and computed tomography in these patients to assess the labral and chondral integrity as well as more precisely assessing location and size of glenoid rim fracture (Fig 2), respectively.
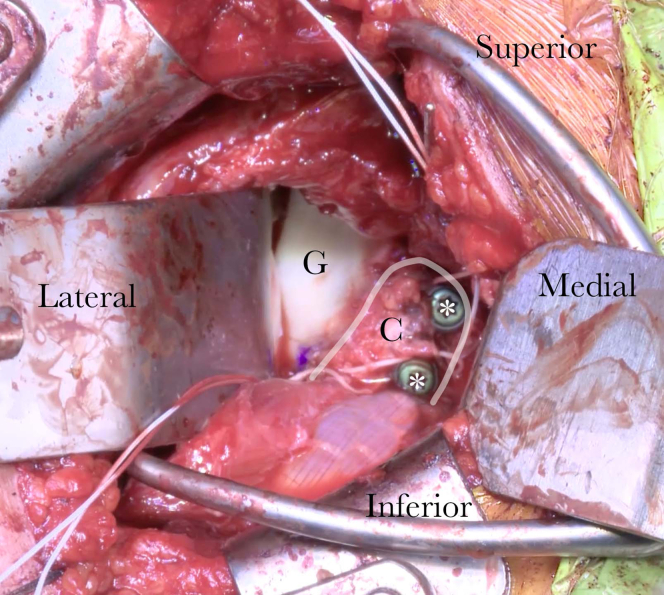
Fig 1.
Clinical radiographs of a patient with recurrent shoulder instability following arthroscopic Bankart repair. West point view of the right shoulder reveals anterior glenoid bone loss (solid line), a medialized bone fragment anterior to the glenoid (dotted line), and posterior impaction injury of the humeral head (∗).
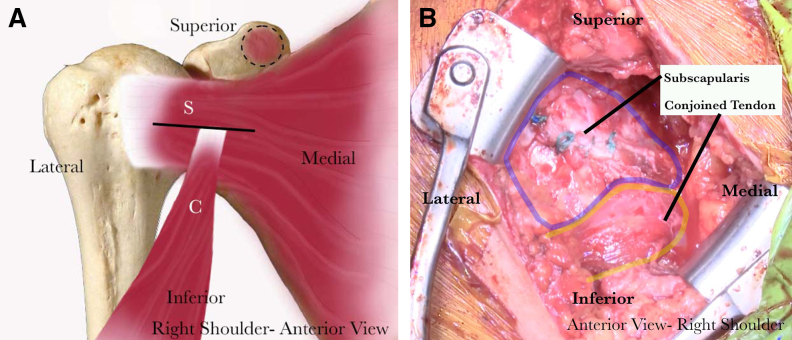
Fig 2.
Sagittal cuts of a CT scan of a right shoulder in a patient with recurrent anterior instability reveal a glenoid rim fracture propagating through the location of previous suture anchor tunnels. This fracture fragment is called a “postage stamp” fracture as the result of the perforated appearance of the fracture edge, which is similar to that of a stamp edge (red line). (CT, computed tomography.)
Indications
A patient should be considered for a bony anterior stabilization procedure in the setting of a postage stamp fracture in nearly all settings. Factors that may push a surgeon to consider bony stabilization include younger age of the patient, amount of dislocation time, sex, and time from fracture until evaluation. In a situation in which the patient has greater than 15% bone loss, especially in the setting of recurrence, we strongly recommend this surgical procedure. In addition, although glenoid fragment open reduction and fixation can be considered, the timing of this procedure and bone quality often make a fixation procedure less likely to be successful in patients with previous glenoid surgery. In our experience, if we are not able to directly fix this fracture within the first 10 days, the bone quality will not allow for stable fixation. Also, in our experience, computed tomography and magnetic resonance imaging often overestimate the quality of bone and should be viewed with caution when choosing between fracture repair versus other bony stabilization procedure. Finally, previous instrumentation and anchor placement into the anterior glenoid often lead to osteolysis around anchors and resultant decrease in osseous integrity.
In patients who present with postage stamp fractures, even in the setting of subcritical bone loss, we feel that additional soft-tissue stabilization procedures and/or fracture repair pose a significant risk of failure. When considering patients for a Latarjet procedure, it is critical that the surgeon have a clear understanding of the risks of this surgical technique as well as the indications and contraindications.6 These are outlined in Table 1.
Table 1.
Indications, Contraindications, and Risks of the Latarjet Procedure for Treatment of Recurrent Anterior Glenohumeral Instability With Postage Stamp Fracture
| Indications |
| Recurrent anterior instability |
| Glenoid bone loss greater than 15% |
Glenoid bone loss less than 15% with
|
| Contraindications |
| Patients 50 years or older with irreparable rotator cuff tear (6) |
| Voluntary anterior dislocators/subluxators (6) |
| Uncontrolled epilepsy (6) |
| Posterior inferior instability (6) |
| Risks |
| Hematoma formation |
| Recurrence of instability |
| Infection |
| Loss of external rotation |
| Bone block nonunion, fracture, resorption |
Surgical Technique (With Video Illustration)
Positioning
We recommend placing the patient in standard beach-chair position. Adjusting the table into a small amount of reverse Trendelenburg positioning assists with exposure and instrumentation of the inferior glenoid. In addition, bolstering the medial scapular border with nonsterile towels can aid in scapular protraction and visualization. When draping, ensure that draping extends medially to the sternoclavicular joint.
Examination Under Anesthesia (EUA)
EUA allows the surgeon to qualify the instability without the patient guarding against the examination. It also allows the surgeon to determine whether the shoulder rests in a dislocated position and allows the surgeon to identify the point of maximum instability, which will be critical to incorporate into final coracoid positioning.
Diagnostic Arthroscopy and Limited Debridement
A standard posterior arthroscopic portal should be used to view the intra-articular pathology. We prefer to use a 5-mm cannula in our anterior portal to assist with flow and make the portal in line with the planned open approach. The anterior glenoid should be thoroughly evaluated and probed, and bone quality should be recorded. In subacute fractures, the fragment often is encased in soft tissue and callus. A 70° arthroscope is helpful for visualization of a medialized anterior glenoid fragment. All previous anchors and sutures should be carefully debrided and removed (Fig 3). Concurrent intra-articular pathology also should be evaluated and addressed during this portion of the case or after coracoid transfer. Given the medial position of these fragments, we prefer maximizing fragment excision under direct arthroscopic visualization to minimize need for aggressive medial retraction. The anterior glenoid is also prepared initially under direct arthroscopic visualization at this time (Fig 4).
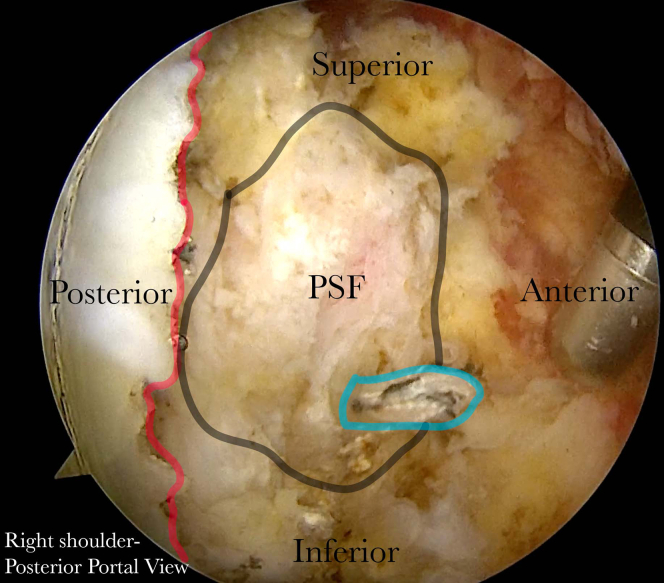
Fig 3.
The anterior glenoid rim of the right shoulder is viewed from the posterior viewing portal. The postage stamp fracture (PSF) is outlined and found to be medially displaced with significant adhesions. The previous suture anchor can be visualized, still within the fragment (blue line). The anterior rim of the glenoid is marked with the red line.
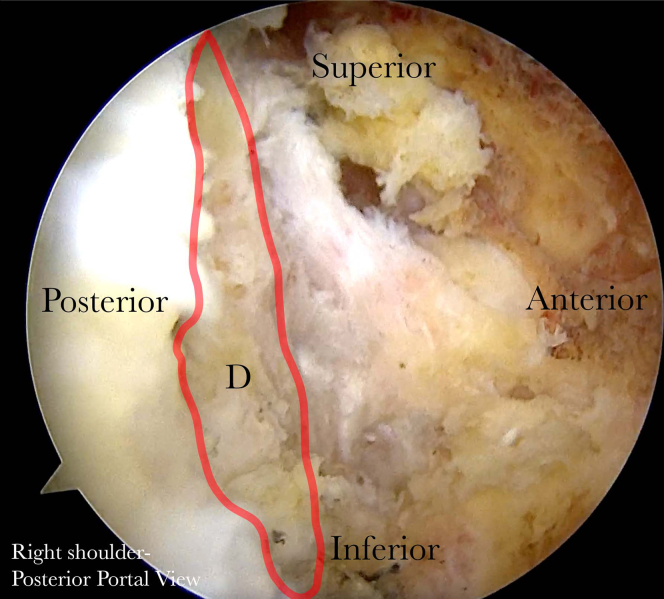
Fig 4.
The anterior glenoid rim of the right shoulder is viewed from the posterior viewing portal. The postage stamp fracture has been removed and the anterior glenoid rim defect (D) is outlined in red.
Coracoid Harvest and Preparation
Our incision is made from the tip of the coracoid extending distally along the deltopectoral interval to the superior aspect of the axillary fold, in this case 7 cm. The incision is taken down to the clavipectoral fascia to create full-thickness flaps with the Bovie for hemostasis. The fascia is incised with Metzenbaum's along with the deltopectoral interval and bluntly dissected between the deltoid and pectoralis. The cephalic vein is dissected laterally to minimize transection of bridging veins and risk of hematoma formation. Subpectoral dissection is performed with a Cobb and curved Mayos. A Kolbel retractor is placed between the deltoid and pectoralis major. The red–white stripe of the short head of the biceps and conjoined tendon is identified and the fascia just lateral to the red stripe is incised. Finger dissection is then used to free the posterior adhesions deep to the conjoined. The coracoacromial ligament is then released, leaving a 1-cm cuff of tissue attached to the coracoid for future incorporation into the repair. The coracoid is then exposed to its base, removing lateral and superior adhesions, while maintaining the coracoclavicular ligaments. The pectoralis minor is meticulously released directly off the medial coracoid. At this stage, care is taken to ensure that the trapezoidal ligament, which is 2 to 3 mm anterior to the elbow, is not released.7 After the coracoid is skeletonized, the planned cut is measured and marked at approximately 25 mm from the tip of the coracoid. We prefer using a 90° sagittal saw from superior to inferior for a majority of the coracoid release, finishing the osteotomy with a 0.5-inch curved osteotome from superomedial to inferolateral.
Following completion of the osseous cut, the coracoid is held at the level of the skin incision with a grasping forceps and the posterior insertion of the coracohumeral ligament is released. The musculocutaneous nerve is palpated, visualized, and gently released free of tension all the way to its insertion into the biceps muscle belly. During these steps, the surgeon should be very mindful of the tension placed on the coracoid to avoid a neural injury. We use a sagittal saw to lightly decorticate the coracoid and prepare the osseous bed for repair to the anterior glenoid. Using the drill guide clamp, 2 drill holes are provisionally drilled in the coracoid piece from the planned anterior surface to the planned deep surface. The coracoid is then tucked into the wound and retracted away for later retrieval.
Glenoid Exposure and Preparation
The arm is then externally rotated to place the subscapularis on tension. The superior and inferior borders of the subscapularis tendon are identified. The fibers of the subscapularis are then split at the 60/40 junction, extending from the lesser tuberosity laterally to the level of the glenoid medially. Mayo scissors are used to develop a plane between the subscapularis and anterior glenohumeral capsule. Gelpi retractors are placed in the subscapularis split and identified the anterior glenohumeral capsule. At the level of the glenoid, the capsular split is then extended straight inferiorly. The superomedial corner of the capsule of the inferior capsule is tagged for later identification during capsular repair. With a Bovie and Cobb elevator, the anteroinferior labrum is further dissected subperiosteally off the glenoid. The soft tissues are dissected off the anterior glenoid neck and remnant deep hardware removed. The fracture bed is prepared and contoured to accept the coracoid transfer (Fig 5).
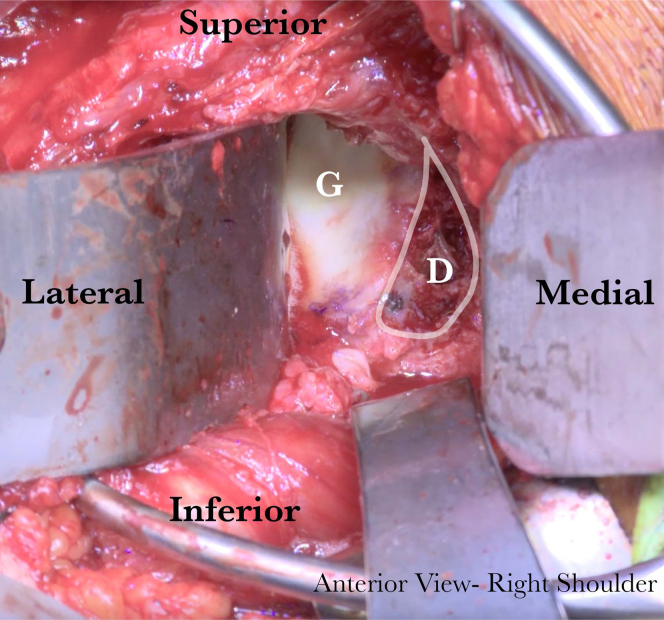
Fig 5.
The right glenoid (G) is visualized through a deltopectoral approach. The bony defect (D) is outlined in white. Once the approach is complete, before coracoid fixation, the anterior rim is contoured and flattened. Callus and fibrous tissue are removed to improve bone to bone healing.
Coracoid Transfer
The coracoid is retrieved from within the wound and secured along the glenoid neck, flush with the glenoid laterally. The optimal position of the coracoid is confirmed using digital palpation and held in place with a K-wire (Fig 6). An additional K-wire is placed outside the planned screw trajectory, and drill holes are placed through the coracoid into the glenoid using a 3.5-mm drill. The 4.0 mm, fully threaded, noncannulated bicortical screws are then inserted with suture washers (Fig 7). In our case, a small step off is noted between the coracoid and the glenoid. This is contoured using a high-speed burr to smooth the lateral prominence of the coracoid graft.
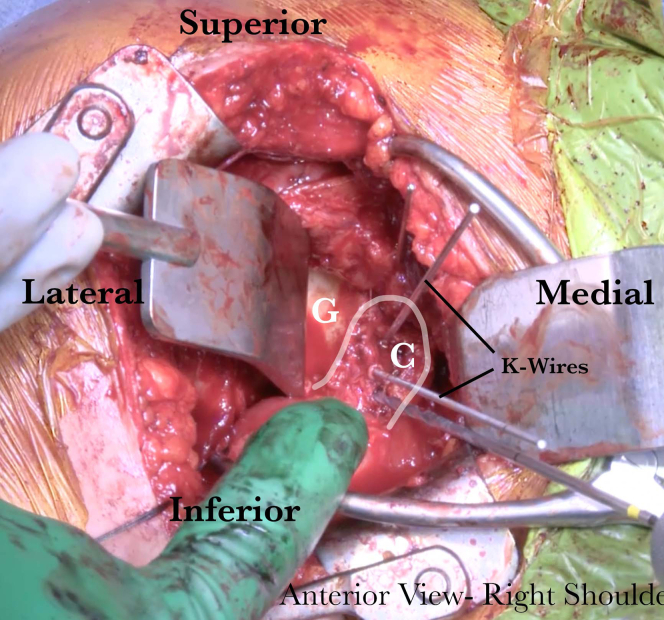
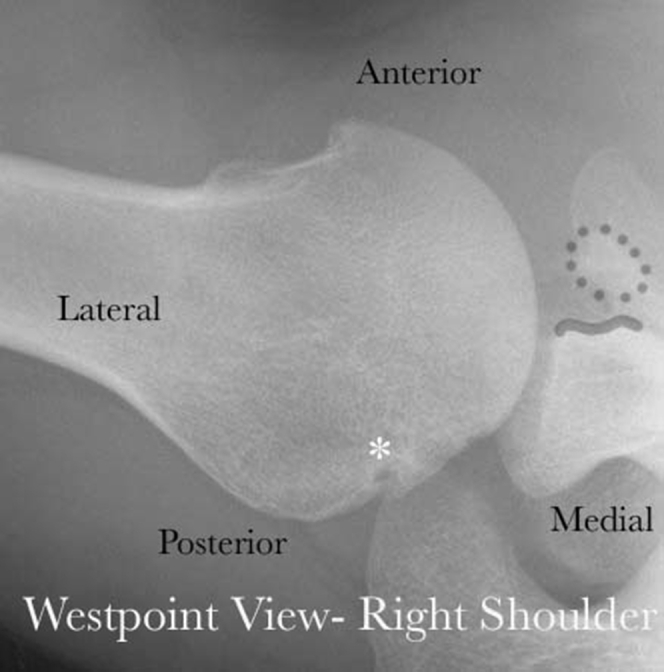
Fig 6.
The right glenoid (G) is visualized through a deltopectoral approach. Following glenoid rim preparation, the coracoid (C) is positioned at the anterior inferior glenoid and provisionally held in place with K-wires. The K-wires are intentionally placed outside planned screw trajectory.
Fig 7.
The right glenoid (G) is visualized through a deltopectoral approach. Following provisional fixation, the coracoid (C), two 4.0-mm solid, fully threaded screws are placed through the graft, and into the glenoid with bicortical fixation. The screws are loaded with suture washers (∗), which contain a permanent, high-tensile suture. This suture will allow for soft tissue to be attached directly to the graft without the need of additional holes/anchors to be placed.
Capsule and Subscapularis Repair
With the arm placed approximately at 45° of external rotation, the capsule is repaired using #2 FiberWire (Arthrex, Naples, FL) suture preloaded on the suture washers. The remaining stump of the coracoacromial ligament is incorporated in the capsule repair. Using a SutureTape (Arthrex), the subscapularis is then repaired carefully to avoid incarceration of the long head of the biceps at the lateral aspect of the repair. After completion of the repair of the capsule and the subscapularis, the conjoined tendon will be found medially exiting between the superior and inferior split of the subscapularis tendon (Fig 8).
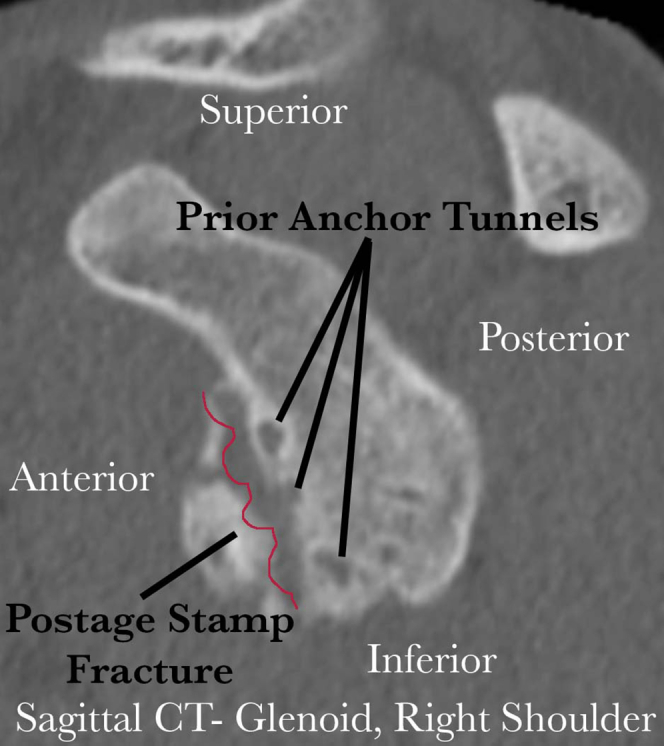
Fig 8.
(A) A illustrative representation of the right shoulder anatomy following a coracoid transfer through subscapularis split for a postage stamp fracture, viewed from anterior. The subscapularis tendon (S) is split at the 60/40 interval to the level of the glenoid (solid black line). The conjoined tendon (C), attached to the coracoid, is then transferred through the split so that the tendon acts as a sling over top of the inferior subscapularis. (B) The completed sling construct of a right shoulder, viewed from anterior, following coracoid transfer for anterior instability due to a postage stamp fracture. The subscapularis tendon is outlined in blue, and conjoined tendon (outlined in yellow) can be seen traversing superficial to the inferior subscapularis before diving deep to the superior subscapularis and inserting onto the coracoid which is now secured to the anterior glenoid. This repair construct provides increased glenohumeral stability through the dynamic stabilization offered by the conjoined tendon and inferior subscapularis.
Closure and Postoperative Plan
At this point, the wound is closed per surgeon preference. Postoperatively, we place the operative arm into a padded abduction sling for 6 weeks. External rotation is restricted to 30° for the first 3 weeks. The full rehabilitation protocol is outlined in Table 2.
Table 2.
Rehabilitation Protocol for Patients Following Open Latarjet Procedure for Postage Stamp Fracture Instability
| Phase 1 (Surgery to 6 weeks Postsurgery) | |
| Appointment | Postoperative appointment 10-14 days |
| Rehab goals | Protect the shoulder postoperatively |
| Restore passive range of motion (ROM), 120° of forward flexion and 60° of external rotation | |
| Precautions | Sling for 6 weeks |
| ROM restrictions | |
| 0-3 weeks | |
| External rotation (ER): 30 | |
| Forward flexion (FF): 100 | |
| Internal rotation (IR): Full as tolerated | |
| Abduction (ABD): Full as tolerated | |
| >3-6 weeks | |
| ER: 60 | |
| FF: 120 | |
| IR: Full as tolerated | |
| ABD: Full as tolerated | |
| Suggested therapeutic exercises | Weeks 1-6 |
| Cervical ROM exercises | |
| Elbow/hand/wrist ROM | |
| Ball squeezes | |
| Ankle pumps | |
| Scapular retraction and depression | |
| Weeks 3-6 | |
| Pendulums | |
| Aquatherapy for active assist range of motion (AAROM) | |
| Progression criteria | Full passive range of motion (PROM) |
| Phase 2 (6 weeks-13) | |
| Appointment | |
| Rehab goals | Full active range of motion (AROM) |
| Strengthen shoulder in protected positions | |
| Begin restoring neuromuscular control | |
| Precautions | No AROM until week 7 |
| No low load prolonged stretching until week 8 | |
| Suggested therapeutic exercises | Weeks 6-9 |
| AAROM IR, ER, flexion, extension, abduction | |
| Isometrics IR, ER, flexion, extension, abduction | |
| Weeks 7-13 | |
| AROM | |
| Bench press series | |
| Modified military press | |
| Side-lying ER | |
| Salutes | |
| Full can | |
| Prone row | |
| Weeks 8-13 | |
| AROM | |
| Prone Ys | |
| Low-load prolonged stretching | |
| Towel IR | |
| Cross arm stretch | |
| Sleeper stretch | |
| Weeks 9-13 | |
| Initial resistance strengthening | |
| IR/ER | |
| Double-arm ER | |
| Full can | |
| Forward punch + | |
| Rows | |
| Bicep curls | |
| Triceps extensions | |
| Lat pull downs | |
| Activities of daily living | Full use of arm |
| Eating/drinking | |
| Dressing | |
| Washing/showering | |
| Progression criteria | Full AROM |
| Negative apprehension and impingement | |
| Good muscle contraction | |
| Phase 3 (weeks 13-16) | |
| Activities of daily living (ADLs) | No limitations in ADLs at this point |
| Progression criteria | Strength is 4/5 when compared bilaterally, |
| Full pain-free ROM | |
| Phase 4 (weeks 16-25) | |
| Appointment | |
| Rehab goals | Restore full strength (5/5) with all planes |
| Stability with high velocity plyometrics | |
| Full pain-free ROM | |
| Precautions | Deceleration movements until week 21 |
| Suggested therapeutic exercises | Continued strengthening- 25 |
| Bear hugs | |
| ER @ 45 & @ 90 | |
| Rhythmic stabilization | |
| 17-25 | |
| Plyometrics | |
| Advanced closed-chain stability | |
| 21-25 | |
| Decelerations | |
| Progression criteria | |
| Pain free ROM | |
| Maximized strength | |
| Proper scapulothoracic movement | |
| No apprehension to return to activity | |
| Phase 5 (week 25+) | |
| Rehab goals | Progress to full activity |
| Work capacity of cardiovascular endurance for specific sports demands | |
| Precautions | Gradually build into sport-specific demands |
Discussion
Variability in treatment for patients with recurrent anterior instability from a postage stamp fracture exists. We recommend the use of a bony stabilization procedure over fragment reduction and fixation or other soft-tissue/arthroscopic procedures. In our opinion, previous anchor placement disrupts normal glenoid anatomy and changes the biomechanical properties of the anterior glenoid bone. In addition, unless a fixation procedure can be performed immediately, often the delay in surgical intervention causes the bony fragment to lose its structural integrity. Even in settings in which a postage stamp fracture can be surgically addressed immediately, we are concerned that additional fixation placed through the already compromised fragment will place a high risk of recurrent fracture on the repair.
When evaluating the shoulder during the EUA and arthroscopic procedure, concurrent intra-articular pathology should be carefully examined. If a large Hill–Sachs defect exists, consideration should be given for additional posterior stabilization. In the rare case that posterior labral tears occur simultaneously with anterior instability events and postage stamp fractures, the sequence of fixation should prevent damage to areas following repair. We prefer performing the coracoid transfer and finishing with arthroscopic posterior labral repair; Fukuda placement during coracoid transfer would place a high amount of stress on the posterior labrum and risk damage to repair site. In addition, patients who have been immobilized for a longer period of time before surgical stabilization may require selective soft-tissue releases.
Although there are many variants in technique for performing a coracoid transfer, our preference is to split the subscapularis and capsule in line with one another. This ensures that we have access to the anterior glenoid without risk of overly medializing/lateralizing the capsular split. In addition, the split allows the coracoid to be repaired to the anterior glenoid with the conjoined tendon functioning as a sling to the inferior subscapularis, providing a dynamic stabilization effect. A longitudinal split allows a capsular repair to be performed directly to the subscapularis and allows medialization of the repair to the level of the coracoid. A full list of pearls and pitfalls for this surgical technique are outlined in Table 3.
Table 3.
Pearls and Pitfalls of the Latarjet Procedure for Restoring Glenohumeral Stability in a Patient With a Postage Stamp Fracture
| Technique | Pearls | Pitfalls |
|---|---|---|
| Examination under anesthesia | Note if shoulder is sitting in a dislocated position at rest Note position of maximum instability |
Failure to note position of maximum instability may result in coracoid positioning at improper location on glenoid |
| Diagnostic arthroscopy and debridement | Complete diagnostic arthroscopy should evaluate for concurrent pathology such as labral tear, capsular avulsion, rotator cuff tear, and quality of glenoid bone | If posterior labral repair is performed at time of arthroscopy, there is risk of damage to this repair during retractor placement for open portion of surgical procedure |
| Coracoid harvest and preparation | Leave 1-cm cuff of coracoacromial ligament attached to coracoid—this will be incorporated into capsular repair at end of surgery A 90° sagittal saw blade is often approximately 25 mm from blade bend to the saw handle. This can help with visualizing appropriate depth of resection The trapezoid component of the coracoclavicular ligament is, on average, 2-3 mm closer to the tip of the coracoid than the elbow of the coracoid7 |
Positioning the curved osteotomy so that the blade angles towards the scapula may result in propagation of fracture from coracoid base into scapular body Failure to release musculocutaneous nerve adhesions, or pulling coracoid out of the incision during drilling may result in undue traction and nerve paralysis Skeletonizing the superior coracoid all the way to the elbow will destabilize the coracoclavicular ligamentous complex |
| Glenoid exposure and preparation | A K-wire may be placed into the scapula to retract the superior subscapularis Ensure that medial exposure will allow for appropriate drilling trajectory—often the surgeon's hand will need to be medial to the incision with a medial to lateral instrument trajectory |
Prolonged medial retraction may increase risk of nerve palsy or injury Splitting the subscapularis too superiorly (i.e. at the mid-point) will make accessing the inferior glenoid difficult. The subscapularis split should be through the inferior half of the subscapularis; we recommend a 60/40 split. |
| Coracoid transfer | Two K-wires can be used to fix the coracoid in place and allow access to both screw holes simultaneously Screw purchase should be the priority with coracoid transfer. If the coracoid is slightly proud, we recommend using a burr to contour the lateral coracoid after fixation rather than removing the screw and adjusting, which would risk losing fixation. |
Placing K-wires through the predrilled holes on the coracoid to provisionally fix the graft will allow significant toggling of the coracoid and lead to difficulty with screw insertion Positioning the coracoid too superior on the glenoid, which is often easier to access, will lead to inadequate restoration of the glenoid surface area. |
| Capsule and subscapularis repair | Preloaded washers with a permanent, high-tensile suture can be used to improve compression of the coracoid and allow for soft tissue to be repaired directly to the coracoid. | Repairing the subscapularis with the arm in internal rotation will lead to reduced length of subscapularis side to side repair, increasing risk of failure |
In cases in which the labrum is intact and nondegenerative, even in chronic fractures, the surgeon may consider retention of the labrum and repair of the labrum directly to the coracoid after transfer. This may improve stability, but does increase the risk of fracture of the coracoid given additional anchor placement in the coracoid.
In the setting of a postage stamp fracture and recurrent glenohumeral instability, we believe that this technique offers a reliable, reproducible, and highly effective surgical solution that will maximize patient outcomes while minimizing risk of recurrent instability and future surgery.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.P. reports consulting fees from Arthrex, Joint Reuter Foundation (JRF), and Arthrosurface; editorial or governing board member for Arthroscopy, Knee, Orthopaedics, and SLACK Inc. and board or committee member for AANA, American Academy of Orthopaedic Surgeons, American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine, The San Diego Shoulder Institute, and The Society of Military Orthopaedic Surgeons. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
In patients with an anterior glenoid rim fracture through prior anchors from a Bankart Repair, also known as a postage stamp fracture, surgical treatment should be aimed at restoring bony stability to the glenohumeral joint. In this video, we outline our preferred technique to restore stability to the glenohumeral joint utilizing a Latarjet procedure.
References
- 1.Provencher M.T., Sanchez A., Sanchez G., et al. Ed 1. Elsevier; Philadelphia: 2017. Shoulder and elbow injuries in athletes: Prevention, treatment and return to sport; pp. 31–38. [Google Scholar]
- 2.Woolnough T., Shah A., Sheean A.J., Lesniak B.P., Wong I., Sa D. “Postage stamp” fractures: A systematic review of patient and suture anchor profiles causing anterior glenoid rim fractures after Bankart repair. Arthroscopy. 2019;35:2501–2508.e2. doi: 10.1016/j.arthro.2019.02.047. [DOI] [PubMed] [Google Scholar]
- 3.Itoi E., Lee S.B., Berglund L.J., Berge L.L., An K.N. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: A cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto N., Muraki T., Sperling J.W. Stabilizing mechanism in bone-grafting of a large glenoid defect. J Bone Joint Surg Am. 2010;92:2059–2066. doi: 10.2106/JBJS.I.00261. [DOI] [PubMed] [Google Scholar]
- 5.Shaha J.S., Cook J.B., Song D.J. Redefining “critical” bone loss in shoulder instability: Functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43:1719–1725. doi: 10.1177/0363546515578250. [DOI] [PubMed] [Google Scholar]
- 6.Domos P., Lunini E., Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 2018;10:15–24. doi: 10.1177/1758573217728716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shibata T., Izaki T., Miyake S., et al. Predictors of safety margin for coracoid transfer: A cadaveric morphometric analysis. J Orthop Surg Res. 2019;14:174. doi: 10.1186/s13018-019-1212-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In patients with an anterior glenoid rim fracture through prior anchors from a Bankart Repair, also known as a postage stamp fracture, surgical treatment should be aimed at restoring bony stability to the glenohumeral joint. In this video, we outline our preferred technique to restore stability to the glenohumeral joint utilizing a Latarjet procedure.