Abstract
Ramp lesions are characteristic medial meniscus injuries seen in anterior cruciate ligament–injured knees. Anterior cruciate ligament injuries combined with ramp lesions increase the amount of anterior tibial translation and tibial external rotation. Therefore, the diagnosis and treatment of ramp lesions have received increasing attention. However, ramp lesions can be difficult to diagnose on preoperative magnetic resonance imaging. Additionally, ramp lesions are difficult to observe and treat intraoperatively in the posteromedial compartment. Although good results have been reported with the use of a suture hook through the posteromedial portal in the treatment of ramp lesions, the complexity and difficulty of the technique are further problems. The outside-in pie-crusting technique is a simple procedure that can enlarge the medial compartment and facilitate the observation and repair of ramp lesions. After this technique, ramp lesions can be properly sutured, using an all-inside meniscal repair device, without damaging the surrounding cartilage. A combination of the outside-in pie-crusting technique and an all-inside meniscal repair device (with only anterior portals) is effective in the repair of ramp lesions. This Technical Note aims to report in detail the flow of a series of techniques, including our diagnostic and therapeutic methods.
A ramp lesion is a characteristic medial meniscus (MM) injury seen in anterior cruciate ligament (ACL)–injured knees. The ramp lesion is a longitudinal tear in the red zone of the meniscus, meniscotibial ligament, or meniscocapsular ligament at the MM posterior segment. Recent biomechanical studies have reported that ACL injuries combined with ramp lesions increase the amount of anterior tibial translation and tibial external rotation. This kind of injury cannot be completely repaired by ACL reconstruction alone and requires the addition of suture repair of the ramp lesion to provide normal knee stability.1 Therefore, if a ramp lesion is found during ACL reconstruction, appropriate treatment of the ramp lesion is required to avoid overloading the grafted tendon and residual instability in the knee joint.
The outside-in pie-crusting technique provides sufficient space for observation of the ramp lesion in the intercondylar notch view with only anterior portals. Moreover, the outside-in pie-crusting technique allows an all-inside meniscal repair device to be easily used, without chondral injury. A combination of the outside-in pie-crusting technique and an all-inside meniscal repair device (with only anterior portals) is thus reasonable in the repair of ramp lesions. In this report, we describe a series of surgical procedures using a combination of these techniques.
Surgical Technique
In patients with ACL injuries, the presence of a ramp lesion is confirmed by preoperative magnetic resonance imaging (MRI) (Fig 1). The patient is placed in the supine position, and a tourniquet is applied to the proximal thigh. Standard anteromedial and anterolateral portals are created, with observation using a 30° arthroscope (Video 1).
Fig 1.
Preoperative magnetic resonance imaging (MRI) of ramp lesion in right knee. (A) Suspected ramp lesion (arrow) on sagittal view (T2-weighted Dixon sequence). (B) Coronal view (T2-weighted BLADE MRI with fat saturation) showing ramp lesion (arrows).
When the medial compartment is observed, the crevice sign (consisting of 1 longitudinal cartilage fissure or multiple longitudinal cartilage fissures) may sometimes be identified on the distal femoral condyle (Fig 2). An intercondylar notch view should be obtained to observe the ramp lesion. This view is obtained by passing the scope from the anterolateral portal through to the medial margin of the posterior cruciate ligament and the lateral wall of the medial femoral condyle (Fig 3). However, this view has a narrow field of visualization, and the use of surgical instruments can be difficult (Fig 4).
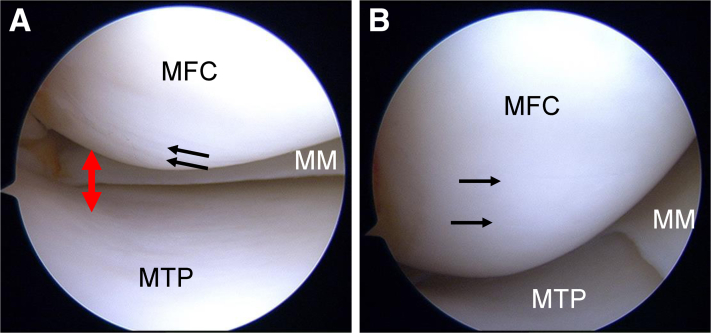
Fig 2.
Arthroscopic view of crevice sign on medial femoral condyle (MFC) and medial compartment before outside-in pie-crusting technique in right knee (supine position, anterolateral portal). This sign indicates instability of the medial meniscus (MM) in anterior cruciate ligament–deficient knees. When this sign is present, MM injuries (especially ramp lesions) are possibly present and require treatment. (A) Small fissures (black arrows) on the MFC are suspected. The view of the posteromedial compartment is extremely narrow (red arrow). (B) Two longitudinal cartilage fissures (arrows) are evident as the knee joint is placed in mild flexion. This is called the crevice sign. (MTP, medial tibial plateau.)
Fig 3.
Scope path to intercondylar notch view in right knee (supine position, anterolateral portal). The intercondylar notch view is obtained by passing the scope from the anterolateral portal through to the medial margin of the posterior cruciate ligament (PCL) and the lateral wall of the medial femoral condyle (MFC).
Fig 4.
Arthroscopic view of ramp lesion through intercondylar notch view in right knee (supine position, anterolateral portal). (A) Before the outside-in pie-crusting technique is performed, the ramp lesion (black dots) must be confirmed; however, the field that can be observed is narrow, and no space for repair is present. (B) After the outside-in pie-crusting technique is performed, the medial compartment becomes enlarged and the ramp lesion (black dots) can be observed from above. This technique further provides ample space for probing and manipulating all-inside meniscus repair devices. (MFC, medial femoral condyle; MM, medial meniscus.)
The outside-in pie-crusting technique is performed using a standard 18-gauge (1.2 × 40–mm) hypodermic needle. The arthroscope is inserted through the anterolateral portal for accurate needle entry and medial-compartment confirmation. The needle is inserted into the skin after the puncture position is determined while percutaneously touching the meniscus. To avoid damage to the meniscus, the needle is targeted between the meniscus and tibial plateau. While the direction of the needle is changed from anterior to posterior, adequate release of the posterior one-third of the medial collateral ligament and the posterior oblique ligament is performed (Fig 5). At this time, it is crucial to apply constant valgus stress to the knee joint. Often, medial collateral ligament release is represented by an audible pop that corresponds to rapid enlargement of the joint cavity in the medial compartment. This is confirmed by simultaneous visualization of the medial compartment (Fig 6).
Fig 5.
Outside-in pie-crusting technique in right knee. The outside-in pie-crusting technique is performed using a standard 18-gauge (1.2 × 40–mm) hypodermic needle. To avoid damage to the meniscus, the needle is targeted between the meniscus and tibial plateau. While the direction of the needle is changed from anterior to posterior, adequate release of the posterior one-third of the medial collateral ligament (MCL) and the posterior oblique ligament (POL) is performed (red arrow). (MM, medial meniscus.)
Fig 6.
Arthroscopic view of medial compartment after outside-in pie-crusting technique in right knee (supine position, anterolateral portal). The view of the posteromedial compartment (arrow) is considerably enlarged after the outside-in pie-crusting technique. (MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau.)
The intercondylar notch view is used again, and the ramp lesion can be observed more clearly (Fig 4). The ramp lesion and meniscal instability are assessed using a probe. The ramp lesion should be rasped before suturing (Fig 7). After the outside-in pie-crusting technique is performed, an all-inside meniscal repair device (e.g. FAST-FIX; Smith & Nephew, Andover, MA) can be easily used in the posteromedial compartment as well. By use of the all-inside meniscal repair device, anchors are inserted into the meniscus and posterior capsule (Fig 8). To avoid over-tightening of the thread, a probe is used to carefully and gradually tighten the thread to the appropriate tension (Fig 9). Depending on the size of the ramp lesion, multiple sutures may be required using multiple all-inside meniscal repair devices (Fig 10). ACL reconstruction is performed by use of standard procedures, with anatomic double-bundle reconstruction using the semitendinosus tendon (Fig 11).
Fig 7.
Rasping of lamp lesion in right knee (supine position, anterolateral portal). The ramp lesion should be rasped before suturing. (MFC, medial femoral condyle; MM, medial meniscus.)
Fig 8.
Suturing of ramp lesion using all-inside meniscal repair device (e.g. FAST-FIX) in right knee (supine position, anterolateral portal). (A) By use of the FAST-FIX device, the first anchor is inserted into the meniscus; after the pie-crusting technique, this device can easily be used without damaging the cartilage. (B) The second anchor is inserted into the posterior capsule across the ramp lesion. (MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau.)
Fig 9.
Adjustment of suture tension using probe in right knee (supine position, anterolateral portal). To avoid over-tightening of the thread, a probe is used to carefully and gradually tighten the thread to the appropriate tension. (MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau.)
Fig 10.
Arthroscopic view of suturing with all-inside meniscal repair device in right knee (supine position, anterolateral portal). The ramp lesion is shown after the placement of 2 stitches by use of the all-inside meniscal repair device. (MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau.)
Fig 11.
Arthroscopic view after reconstruction of anterior cruciate ligament in right knee (supine position, anterolateral portal). Anterior cruciate ligament reconstruction is performed using standard procedures, with anatomic double-bundle reconstruction of the semitendinosus tendon. (LFC, lateral femoral condyle; MFC, medial femoral condyle.)
The operated knee is placed in a knee brace, and range-of-motion and loading exercises are prohibited for the first 2 weeks after surgery. Starting in the third week after surgery, weight bearing is increased by 30 kg every other week and knee flexion is increased by 30° every other week. However, knee flexion is limited to only 120° until 6 weeks after surgery. A return to sports is allowed at 6-9 months postoperatively.
Discussion
The outside-in pie-crusting technique facilitates the treatment of ramp lesions using an all-inside meniscal repair device. Technically, both time-wise and safety-wise, the combination of the outside-in pie-crusting technique and an all-inside meniscal repair device is the most affordable option in the treatment of ramp lesions (Table 1).
Table 1.
Advantages and Disadvantages of Outside-in Pie-Crusting Technique With All-Inside Meniscal Repair Device
| Advantages |
| The outside-in pie-crusting technique is useful to access ramp lesions easily. |
| An all-inside meniscal repair device is technically simple to use and allows for quick suturing of ramp lesions. |
| This procedure is simple and can be performed with only an anterior portal and a 30° arthroscope. |
| Disadvantages |
| Care should be taken not to damage the meniscus with an 18-gauge hypodermic needle when performing the outside-in pie-crusting technique. |
| All-inside meniscal repair devices carry the risk of anchor irritation, device failure, and cartilage damage. |
| The intercondylar notch view must be obtained for the observation of ramp lesions (although there are few technical requirements). |
Ramp lesions occur in 15% to 24% of ACL-reconstructed knees in adults; however, roughly 77% of these lesions are difficult to diagnose on MRI.2 Additionally, a deep posterior lateral femoral condyle, varus alignment, and a steep medial tibial slope have been reported as risk factors for ramp lesions in ACL-injured knees.3 Another method to detect ramp lesions, using ultrasound, has been reported.4 The presence of ramp lesions should be suspected and purposefully checked for during arthroscopy in ACL reconstruction, regardless of preoperative status. Intraoperatively, the crevice sign (longitudinal fissure located on the distal medial femoral condyle) indicates instability of the MM in ACL-deficient knees.5 When this sign is present, MM injuries (especially ramp lesions) are possibly present and require treatment.6
Ramp lesions can be observed either by using an intercondylar notch view (from an anterior portal) or by creating a new posterior portal, each of which has advantages and disadvantages. Without additional procedures, the intercondylar notch view often has a narrow field of view, which makes the proper diagnosis and treatment of ramp lesions difficult. In contrast, the use of a posteromedial portal carries the risk of damage to the neurovascular bundle. In addition, adequate observation may not be possible if portals are not created in the proper location.
Both the inside-out and all-inside techniques have been reported for the repair of ramp lesions, with each technique being further associated with its own advantages and disadvantages. The inside-out technique offers a variety of suture positions and allows surgeons to pass more sutures to create stronger sutures. However, with the inside-out technique, because of the posteromedial location of the ramp lesion, meniscal repair is technically challenging (owing to the high risk of damage to the saphenous neurovascular bundle). Conversely, the all-inside technique is characterized by low technical demands, no additional incisions, and a low risk of neurovascular injury. However, with the all-inside technique, there is a possible risk of anchor irritation, device failure, and cartilage damage.
There have been several reports on the outcomes of ramp lesion treatment. Thaunat et al.7 reported good results with all-inside suture repair of ramp lesions using a suture hook through the posteromedial portal. Furthermore, good results have been described after FAST-FIX repair of ramp lesions.8 Siboni et al.9 showed that a method of creating 2 posteromedial portals is effective in the visualization and treatment of ramp lesions. A systematic review reported that stable ramp lesions smaller than 2 cm showed good clinical results with debridement alone and that larger or unstable ramp lesions showed good results with the all-inside technique.10
A sufficient field of view and space for instrumentation are required for appropriate diagnosis and treatment of ramp lesions. The outside-in pie-crusting technique facilitates the observation and treatment of ramp lesions (with only an anterior portal) and eliminates the need to replace the 30° arthroscope with a 70° arthroscope. The outside-in pie-crusting technique does not result in residual postoperative valgus knee instability or affect postoperative clinical outcomes.11 We sometimes confirm the presence of a ramp lesion using the outside-in pie-crusting technique, not only in cases in which the presence of a ramp lesion is suspected based on preoperative MRI but also in cases in which the crevice sign or MM instability is observed intraoperatively. The most effective combination in the treatment of ramp lesions is the outside-in-pie-crusting technique, which is easy and quick to perform, and an easy-to-use all-inside meniscal repair device.
Finally, the described technique has a few limitations. First, although each technique is relatively easy to learn, it takes some time to master the techniques to make a reliable diagnosis and perform treatment. Second, although the combination of this series of observation techniques may reduce the number of missed ramp lesions, this is not certain.
Acknowledgment
The authors thank Editage (www.editage.com) for English-language editing.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Ramp lesion repair using outside-in pie-crusting technique with all-inside meniscal repair device. The patient is placed in the supine position, and a tourniquet is applied to the proximal thigh. Standard anteromedial and anterolateral portals are created, with observation using a 30° arthroscope. The anterior cruciate ligament (ACL) is evaluated for tears or looseness. When the medial compartment is observed, the crevice sign (consisting of 1 longitudinal cartilage fissure or multiple longitudinal cartilage fissures) may sometimes be identified on the distal femoral condyle. The crevice sign indicates medial meniscal instability in ACL-deficient knees. An intercondylar notch view is used to observe the ramp lesion. This view is obtained by passing the scope from the anterolateral portal through to the medial margin of the posterior cruciate ligament and lateral wall of the medial femoral condyle. The outside-in pie-crusting technique can be used to facilitate the observation and repair of ramp lesions. After rasping of the tear, an all-inside meniscal repair device (e.g. FAST-FIX) is used to suture the ramp lesion. By use of the all-inside meniscal repair device, anchors are inserted into the meniscus and posterior capsule. To avoid over-tightening of the thread, a probe is used to carefully and gradually tighten the thread to the appropriate tension. Depending on the size of the ramp lesion, multiple sutures may be required using multiple all-inside meniscal repair devices. ACL reconstruction is performed using standard procedures, with anatomic double-bundle reconstruction of the semitendinosus tendon.
References
- 1.Stephen J.M., Halewood C., Kittl C., Bollen S.R., Williams A., Amis A.A. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44:400–408. doi: 10.1177/0363546515617454. [DOI] [PubMed] [Google Scholar]
- 2.Malatray M., Raux S., Peltier A., Pfirrmann C., Seil R., Chotel F. Ramp lesions in ACL deficient knees in children and adolescent population: A high prevalence confirmed in intercondylar and posteromedial exploration. Knee Surg Sports Traumatol Arthrosc. 2018;26:1074–1079. doi: 10.1007/s00167-017-4471-4. [DOI] [PubMed] [Google Scholar]
- 3.Kim S.H., Park Y.B., Won Y.S. An increased lateral femoral condyle ratio is an important risk factor for a medial meniscus ramp lesion including red-red zone tear. Arthroscopy. 2021;37:3159–3165. doi: 10.1016/j.arthro.2021.03.078. [DOI] [PubMed] [Google Scholar]
- 4.Nakase J., Asai K., Yoshimizu R., Kimura M., Tsuchiya H. How to detect meniscal ramp lesions using ultrasound. Arthrosc Tech. 2021;10:e1539–e1542. doi: 10.1016/j.eats.2021.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murgier J., Hansom D., Clatworthy M. Knee arthroscopy: The “crevice sign,” a new pathognomonic sign for unstable posterior medial meniscal tear in anterior cruciate ligament-deficient knees. Arthrosc Tech. 2020;9:e263–e265. doi: 10.1016/j.eats.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murgier J., Bayle-Iniguez X., Clatworthy M. The crevice sign: A new indicator of meniscal instability in ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2022;30:1888–1892. doi: 10.1007/s00167-021-06823-1. [DOI] [PubMed] [Google Scholar]
- 7.Thaunat M., Fayard J.M., Guimaraes T.M., Jan N., Murphy C.G., Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5:e871–e875. doi: 10.1016/j.eats.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li W.P., Chen Z., Song B., Yang R., Tan W. The FasT-Fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27:56–60. doi: 10.5792/ksrr.2015.27.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siboni R., Pioger C., Jacquet C., et al. Meniscal ramp repair: A 2-portal posteromedial approach. Arthrosc Tech. 2022;11:e1163–e1169. doi: 10.1016/j.eats.2022.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acosta J., Ravaei S., Brown S.M., Mulcahey M.K. Examining techniques for treatment of medial meniscal ramp lesions during anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2020;36:2921–2933. doi: 10.1016/j.arthro.2020.05.041. [DOI] [PubMed] [Google Scholar]
- 11.Han X., Wang P., Yu J., Wang X., Tan H. Arthroscopic pie-crusting release of the posteromedial complex of the knee for surgical treatment of medial meniscus injury. BMC Musculoskelet Disord. 2020;21:301. doi: 10.1186/s12891-020-03336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Ramp lesion repair using outside-in pie-crusting technique with all-inside meniscal repair device. The patient is placed in the supine position, and a tourniquet is applied to the proximal thigh. Standard anteromedial and anterolateral portals are created, with observation using a 30° arthroscope. The anterior cruciate ligament (ACL) is evaluated for tears or looseness. When the medial compartment is observed, the crevice sign (consisting of 1 longitudinal cartilage fissure or multiple longitudinal cartilage fissures) may sometimes be identified on the distal femoral condyle. The crevice sign indicates medial meniscal instability in ACL-deficient knees. An intercondylar notch view is used to observe the ramp lesion. This view is obtained by passing the scope from the anterolateral portal through to the medial margin of the posterior cruciate ligament and lateral wall of the medial femoral condyle. The outside-in pie-crusting technique can be used to facilitate the observation and repair of ramp lesions. After rasping of the tear, an all-inside meniscal repair device (e.g. FAST-FIX) is used to suture the ramp lesion. By use of the all-inside meniscal repair device, anchors are inserted into the meniscus and posterior capsule. To avoid over-tightening of the thread, a probe is used to carefully and gradually tighten the thread to the appropriate tension. Depending on the size of the ramp lesion, multiple sutures may be required using multiple all-inside meniscal repair devices. ACL reconstruction is performed using standard procedures, with anatomic double-bundle reconstruction of the semitendinosus tendon.