Abstract
Post-traumatic peroneal tendon subluxation or dislocation is most commonly caused by injury to the superior peroneal retinaculum. Classic open surgeries usually require extensive soft-tissue dissection and have potential risks of peritendinous fibrous adhesions, sural nerve injury, limited range of movement, recurrent or persistent peroneal tendon instability, and tendon irritation. The purpose of this Technical Note is to describe the details of endoscopic superior peroneal retinaculum reconstruction using Q-FIX MINI suture anchor. This endoscopic approach has the advantages of minimally invasive surgery, including better cosmesis, less soft-tissue dissection, less postoperative pain, less peritendinous fibrosis, and less subjective tightness at peroneal tendons. Insertion of the Q-FIX MINI suture anchor can be performed inside a drill guide, and trapping of the surrounding soft tissue can be avoided.
Technique Video
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. Peroneal tendoscopy is performed via the proximal and distal portals. The fibrous tissue covering the lateral cortex of the lateral malleolus is resected and the underlying cortical bone is decorticated. Q-FIX MINI suture anchors are inserted into the ridge of the retrofibular groove. The peroneal tendons are shifted medially and splinted with a K-wire. The superior peroneal retinaculum is sutured with the suture limbs of the anchors. The retinaculum is pushed back to the lateral malleolus and the sutures are tied. Finally, the reduction of the retinaculum back to the lateral malleolus is confirmed endoscopically.
Post-traumatic peroneal tendon subluxation or dislocation frequently is caused by injury to the superior peroneal retinaculum after acute ankle sprain. This retinaculum functions as the primary restraint to subluxation or dislocation of the peroneal tendons and is also a secondary restraint to anterolateral ankle instability.1, 2, 3, 4 The injured superior peroneal retinaculum usually strips off from the distal fibula. Nonoperative treatment is suggested for acute injuries in nonathletes with pain relief, activity modification, cast immobilization, and protected weight-bearing for 6 weeks after the injury.3 However, the overall success rate is less than 50%, and 44% to 74% of the patients finally require surgery.4, 5, 6, 7, 8
Surgical procedures for chronic cases fall into 5 categories: anatomical reattachment of the retinaculum,4,9,10 bone-block procedures,8,11, 12, 13 tissue-transfer procedures,14,15 rerouting procedures,16,17 and groove-deepening procedures.8,17,18 The classic open surgeries usually require extensive soft-tissue dissection and have potential risks of peritendinous fibrous adhesions, sural nerve injury, limited range of movement, recurrent or persistent peroneal tendon instability, and tendon irritation.10,19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31
Peroneal tendoscopy provides good outcomes in the treatment of peroneal tendon pathologies.32, 33, 34, 35 Different endoscopic approaches to address peroneal tendon instability have been proposed, including endoscopic groove deepening and endoscopic superior peroneal retinaculum reconstruction.32,36, 37, 38 The groove-deepening procedure can retain the peroneal tendons within the retrofibular groove and reduce the tension of the tendon. In contrast to the open approach, in which the cortical bone plate is preserved, endoscopic groove-deepening simply removes the cortex and the underlying cancellous bone of the retrofibular groove. The resulting rough bone surface may cause peroneal tendinitis due to abrasion within the bone tunnel, and the exposed cancellous bone may cause hematoma formation and peritendinous fibrous adhesions.8,18,31,37
In most of the cases of peroneal tendon instability, the superior peroneal retinaculum, along with periosteum of the distal fibula, is elevated from the lateral malleolus instead of substance tear and anatomical reattachment of the retinaculum to the distal fibula is a logical surgical treatment.31,37 The purpose of this Technical Note is to describe the technical details of endoscopic superficial peroneal retinaculum reconstruction using the Q-FIX MINI suture anchor. It is indicated for Eckert grade 1 (superior peroneal retinaculum stripped from the distal fibula) or 1 or 2 (superior peroneal retinaculum together with the fibrocartilaginous ridge stripped from the distal fibula)1 post-traumatic peroneal tendon instability. It is contraindicated for congenital peroneal tendon dislocation, attenuated superior peroneal retinaculum, and Eckert grade 3 injury (rim avulsion fracture of the retrofibular groove)1 with sizable avulsed fragment, Eckert grade 4 injury with retinacular substance tear at the calcaneal side,1 irreducible peroneal tendons, or the presence of complex peroneal tendon tears requiring open repair (Table 1).
Table 1.
Indications and Contraindications of Endoscopic Superior Peroneal Retinaculum Reconstruction Using the Q-FIX MINI Suture Anchor
| Indications | Contraindications |
|---|---|
| Eckert grade 1 (superior peroneal retinaculum stripped from the distal fibula) post-traumatic peroneal tendon instability | Congenital peroneal tendon dislocation |
| Eckert grade 2 (superior peroneal retinaculum together with the fibrocartilaginous ridge stripped from the distal fibula) post-traumatic peroneal tendon instability | Attenuated superior peroneal retinaculum |
| Eckert grade 3 injury (rim avulsion fracture of the retrofibular groove) with sizable avulsed fragment | |
| Eckert grade 4 injury with retinacular substance tear at the calcaneal side | |
| Irreducible peroneal tendons | |
| Presence of complex peroneal tendon tears requiring open repair |
Surgical Technique (With Video Illustration)
Preoperative Planning and Patient Positioning
Post-traumatic peroneal tendon instability is a clinical diagnosis. Radiographs and computed tomography of the involved ankle are useful for the detection of rim avulsion fracture of the retrofibular groove. Magnetic resonance imaging is useful to confirm the presence of frank subluxation or dislocation of the peroneal tendons and assess the concomitant pathologies of the retinaculum and tendons, such as the presence of peroneus quartus and low-lying peroneus brevis muscle, which may cause crowding in the retrofibular groove and contribute to peroneal tendons dislocation or tear.2,35
The patient is placed in the lateral position. A thigh tourniquet is applied to provide a bloodless operative field. Fluid inflow is by gravity, and no arthro-pump is used. A 2.7-mm 30° arthroscope is used for this procedure.
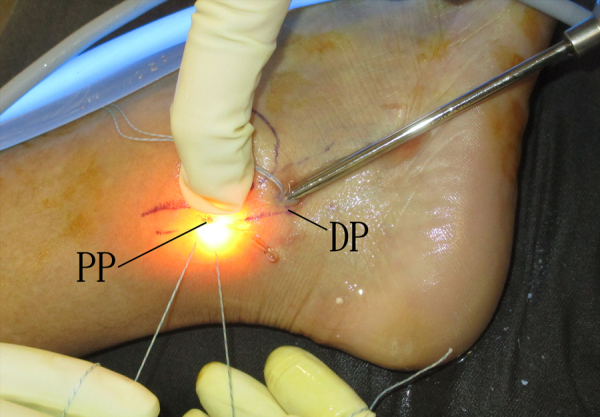
Portal Placement
This procedure is performed via the distal and proximal portals along the peroneal tendon sheath. The distal portal is just distal to the tip of the lateral malleolus. The proximal portal is 2 cm proximal to the tip of the lateral malleolus, which is approximately the proximal edge of the superior peroneal retinaculum (Fig 1).31 Five-millimeter incisions are made at the portals and the subcutaneous tissue is bluntly dissected with a hemostat. The peroneal tendon sheath is then incised open.
Fig 1.
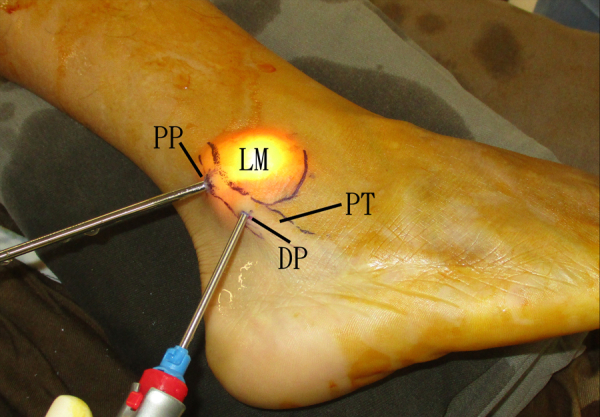
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. This procedure is performed via the distal and proximal portals along the peroneal tendon sheath. The distal portal is just distal to the tip of the lateral malleolus. The proximal portal is 2 cm proximal to the tip of the lateral malleolus which is approximately the proximal edge of the superior peroneal retinaculum. (DP, distal portal; LM, lateral malleolus; PP, proximal portal; PT, peroneal tendons.)
Preparation of the Lateral Cortex of the Lateral Malleolus for Reattachment of the Stripped Periosteum
The distal portal is the viewing and the proximal portal is the working portal. The tendons are examined for any low-lying muscle, tenosynovitis, or tear. Endoscopic synovectomy, debridement, or repair of the torn tendons is performed if needed. The integrity of the superior peroneal retinaculum is examined. The elevated retinaculum together with the periosteum of the lateral malleolus is noted.31 The soft-tissue covering the proximal half of the lateral cortex of the lateral malleolus is resected with an arthroscopic shaver (DYONICS; Smith & Nephew, Andover, MA) to expose the cortical bone (Fig 2). The arthroscope is then switched to the proximal portal and the soft tissue covering the distal half of the lateral cortex is resected with the shaver via the distal portal (Fig 3). It is important to avoid further stripping of the periosteum from the lateral malleolus.
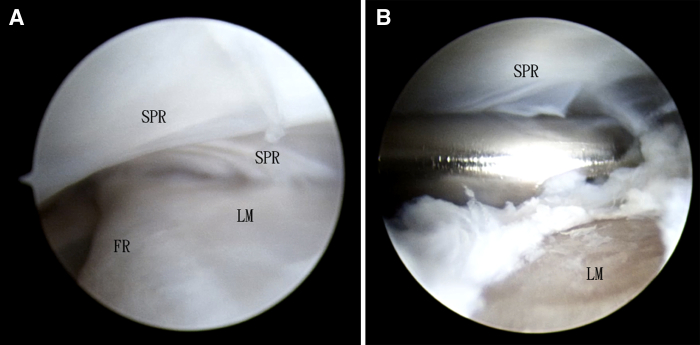
Fig 2.
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The distal portal is the viewing portal and the proximal portal is the working portal. (A) The elevated retinaculum together with the periosteum of the lateral malleolus is noted. (B) The soft tissue covering the proximal half of the lateral cortex of the lateral malleolus is resected with an arthroscopic shaver to expose the cortical bone. (FR, fibrocartilaginous ridge; LM, lateral malleolus; SPR, superior peroneal retinaculum.)
Fig 3.
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The proximal portal is the viewing portal and the distal portal is the working portal. The soft tissue covering the distal half of the lateral cortex of the lateral malleolus is resected with an arthroscopic shaver to expose the cortical bone. (LM, lateral malleolus; SPR, superior peroneal retinaculum.)
Decorticate Lateral Cortex of the Lateral Malleolus
The proximal and distal portals are interchangeable as the viewing and working portals. The exposed lateral cortex of the lateral malleolus is decorticated with an arthroscopic burr (DYONICS) (Fig 4).
Fig 4.
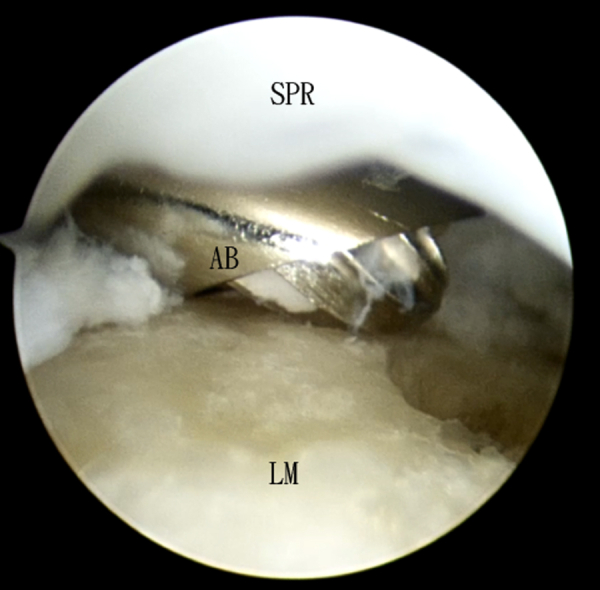
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The distal portal is the viewing portal and the proximal portal is the working portal. The proximal half of the exposed lateral cortex of the lateral malleolus is decorticated with an arthroscopic burr. (AB, arthroscopic burr; LM, lateral malleolus; SPR, superior peroneal retinaculum.)
Insertion of the Q-FIX MINI Suture Anchor
The distal portal is the viewing portal and the proximal portal is the working portal. The Q-FIX MINI drill guide is inserted and sits on the fibular ridge at the level of proximal edge of the stripped retinaculum. A drill hole is made on the ridge of the retrofibular groove, and the Q-FIX MINI suture anchor (Smith & Nephew) is inserted into it via the drill guide (Fig 5). Similarly, another Q-FIX MINI suture anchor is inserted into the ridge of the retrofibular groove at the level of distal edge of the stripped retinaculum via the distal portal with the proximal portal as the viewing portal (Fig 6).
Fig 5.
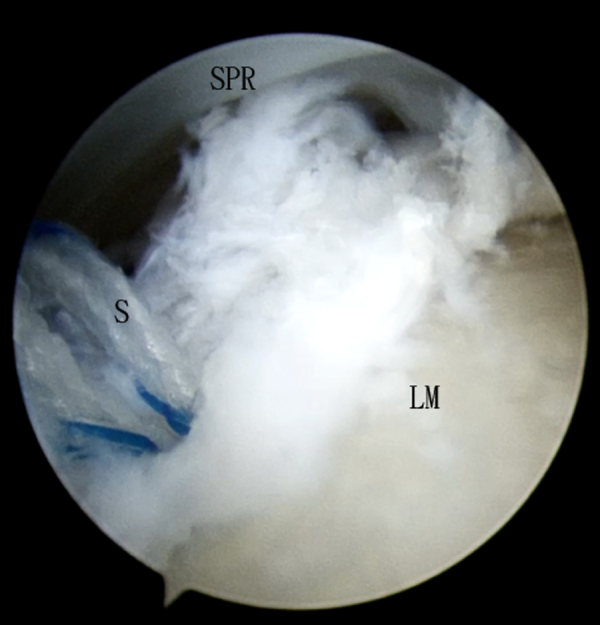
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The distal portal is the viewing portal. A Q-FIX MINI suture anchor is inserted via the proximal portal into the ridge of the retrofibular groove. (LM, lateral malleolus; S, suture limbs of Q-FIX MINI; SPR, superior peroneal retinaculum.)
Fig 6.
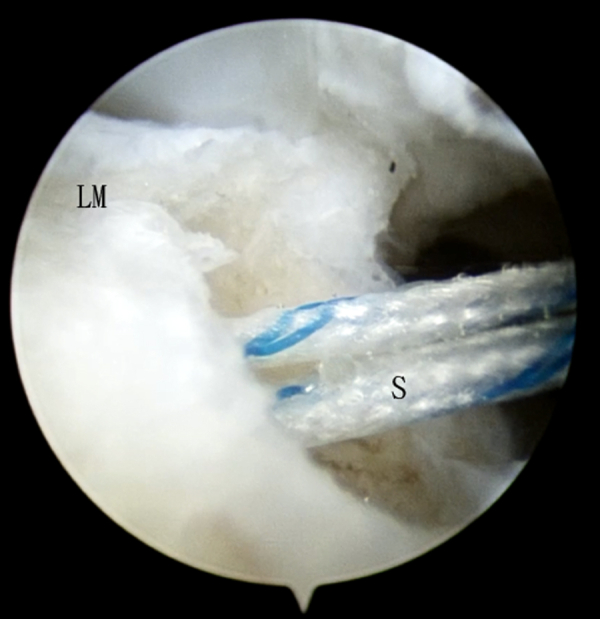
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The proximal portal is the viewing portal. A Q-FIX MINI suture anchor is inserted via the distal portal into the ridge of the retrofibular groove. (LM, lateral malleolus; S, suture limbs of Q-FIX MINI.)
Retraction of Peroneal Tendons With K-Wire
In case of frank dislocation or subluxation of the peroneal tendons, the tendons should be reduced and splinted with a 1.6-mm K-wire (Zimmer, Warsaw, IN) which is inserted percutaneously into the retrofibular groove, before preparation of the lateral cortex of the lateral malleolus.31 The K-wire should pierce through the retinaculum as posteriorly as possible to avoid hindrance of reduction of the retinaculum and the fibular periosteum back to the lateral malleolus and also minimize the risk of sural nerve injury.31 Even if the peroneal tendons are not frankly dislocated or subluxated, shifting the tendons medially and splinted with a K-wire is preferable (Fig 7). This can increase the working area for suturing of the superior peroneal retinaculum. Either the proximal or distal portal can be used as the viewing portal.
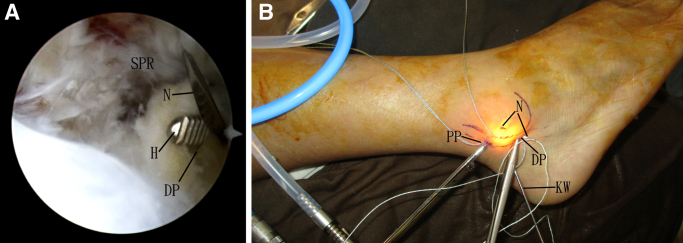
Fig 7.
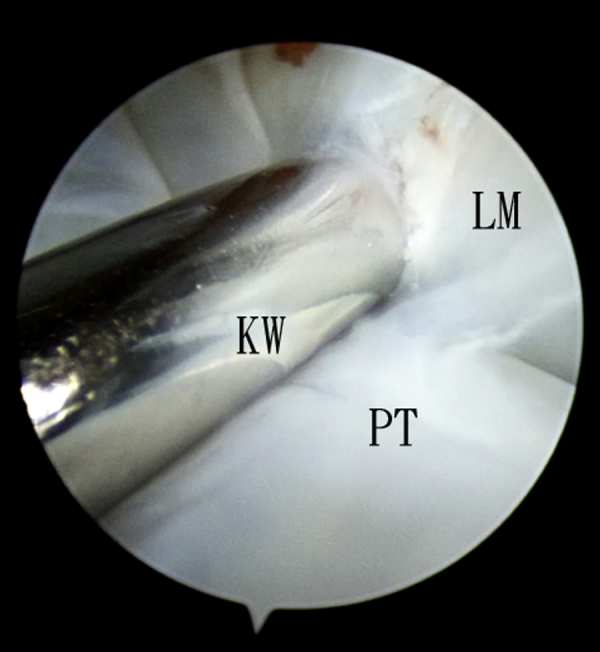
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The distal portal is the viewing portal. The tendons are shifted medially and splinted with a K-wire, which is inserted percutaneously. (KW, K-wire; LM, lateral malleolus; PT, peroneal tendons.)
Suturing the Superior Peroneal Retinaculum
The distal portal is the viewing portal. The suture limbs of the proximal suture anchor are passed through the retinaculum and the overlying skin by means of an eyed needle (FavorMed, Ningbo, China) via the proximal portal. Caution should be paid not to catch the peroneal tendons by the sutures. The suture limbs are retrieved at the surface of retinaculum back to the proximal portal by a hemostat. The arthroscope is switched to the proximal portal. The suture limbs of the distal suture anchor are passed through the retinaculum and the overlying skin by means of an eyed needle via the distal portal (Fig 8). The suture limbs are retrieved at the surface of the retinaculum back to the distal portal by a haemostat.31
Fig 8.
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. (A) The proximal portal is the viewing portal. The suture limb of the distal suture anchor is pierced through the retinaculum by means of an eyed needle via the distal portal. The distal portal is opened up by a hemostat to guide insertion of the needle. (B) The needle passed through the skin overlying the superior peroneal retinaculum. (DP, distal portal; H, hemostat; KW, K-wire; N, eyed needle; PP, proximal portal; SPR, superior peroneal retinaculum.)
Reattachment of Superior Peroneal Retinaculum to the Lateral Malleolus
The superior peroneal retinaculum is manually pushed back to the lateral malleolus by the assistant. Sutures of the proximal and distal anchors are tied through the respective portals to hold the retinaculum onto lateral malleolus (Fig 9). The K-wire can be removed before this step if there is no frank dislocation or subluxation of the tendons.
Fig 9.
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The superior peroneal retinaculum is manually reduced back to the lateral malleolus by the assistant. The suture limbs of the proximal anchor are tied through the proximal portal. (DP, distal portal; PP, proximal portal.)
Confirmation of Completeness of the Procedure
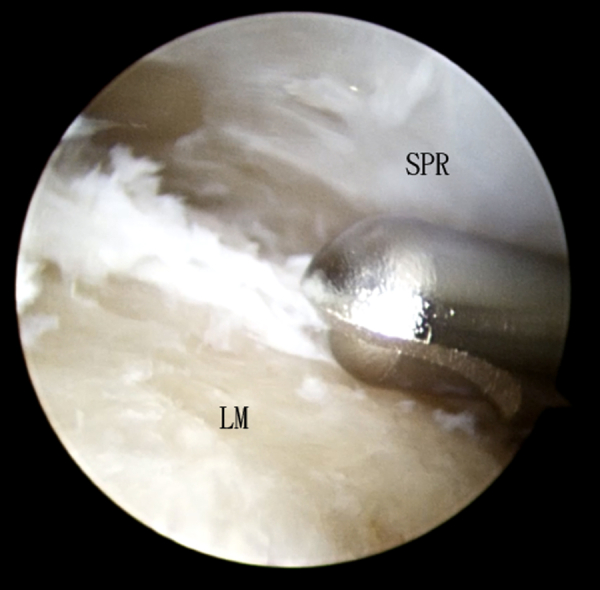
The K-wires are removed and peroneal tendoscopy is performed again with the distal portal as the viewing portal. Deduction of the tendons and repair of the retinaculum is confirmed (Fig 10, Video 1, Table 2).
Fig 10.
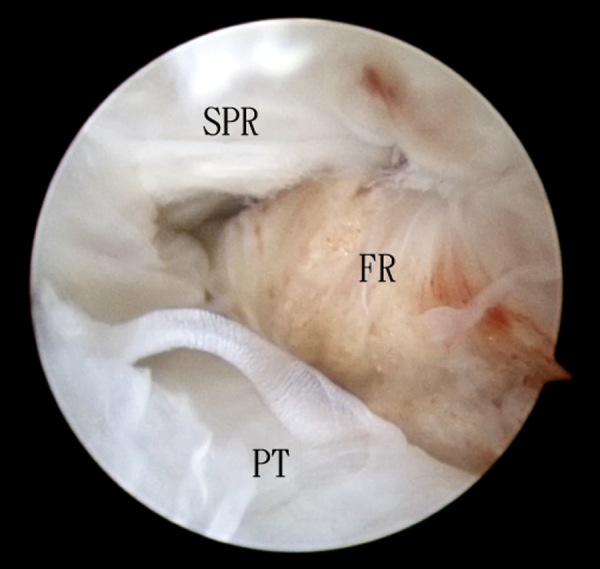
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. The distal portal is the viewing portal. Reattachment of the superior peroneal retinaculum back to the lateral malleolus is confirmed. (FR, fibrocartilaginous ridge; PT, peroneal tendons; SPR, superior peroneal retinaculum.)
Table 2.
Pearls and Pitfalls of Endoscopic Superior Peroneal Retinaculum Reconstruction Using the Q-FIX MINI Suture Anchor
| Pearls | Pitfalls |
|---|---|
| The remaining insertion of the superior peroneal retinaculum should be preserved during resection of soft tissue covering the lateral cortex of the lateral malleolus. | Smaller-sized suture anchor will increase the risk of pullout. |
| The drill guide can prevent trapping of the surrounding soft tissue during insertion of the suture anchor. | Slipping of the drill guide during drilling may cause suboptimal positioning of the suture anchor. |
| The peroneal should be shifted medially before insertion of the needle into the peroneal tendon sheath. | |
| K-wires should pierce through the retinaculum as posteriorly as possible. | |
| Opening the portal with a hemostat during insertion of the needle and avoid piercing of the surrounding soft tissue. |
Postoperatively, the operated ankle is immobilized in a short leg cast for 3 weeks and then dorsiflexion exercise in an air cast is instructed. Circumduction of the foot should be avoided for 3 months.31
Discussion
A study demonstrated that reattachment of the superior retinaculum alone without groove deepening followed by proper rehabilitation is a sufficient treatment of recurrent dislocation of the peroneal tendon.39 This approach can avoid the complications associated with groove-deepening surgery. Compared with the bone-block procedure, the time to return to sports activity after the reattachment of the superior peroneal retinaculum was shown to be shorter.40
Tendoscopy is a useful tool to detect and treat peroneal tendon pathology.32,34 It demonstrates several advantages over conventional open surgery, including less pain, shorter hospital stays, better cosmesis, and faster recovery.32,34,36,37,41 In this reported technique, Q-FIX MINI suture anchor is used because the bone tunnel drilling and insertion of the suture anchor can be performed within the drill guide. This can avoid trapping of the surrounding soft tissue. Even without frank dislocation or subluxation of the peroneal tendons, displacing the peroneal tendon medially and splinted with K-wire is recommended, as this will increase the working space during suturing of the retinaculum and avoid anchoring of the tendon by the sutures.
The advantages of this minimally invasive approach include better cosmesis, less soft-tissue dissection, no wound retraction needed, better assessment of retinaculum integrity, grading of injury, detection of coexisting pathology, less postoperative pain, less peritendinous fibrosis, and less subjective tightness at peroneal tendons.31,32,34,36,37,41,42 The potential risk of this procedure includes sural nerve injury, iatrogenic fracture of the lateral malleolus, iatrogenic tear of the superior peroneal retinaculum, peroneal tendon injury and recurrence of peroneal tendon instability (Table 3). Endoscopic superior peroneal retinaculum reconstruction is not technically difficult and can be attempted by averaged foot and ankle arthroscopists.
Table 3.
Advantages and Risks of Endoscopic Superior Peroneal Retinaculum Reconstruction Using the Q-FIX MINI Suture Anchor
| Advantages | Risks |
|---|---|
| Better cosmesis | Sural nerve injury |
| Less soft-tissue dissection | Iatrogenic fracture of the lateral malleolus |
| No wound retraction needed | Iatrogenic tear of the superior peroneal retinaculum |
| Better assessment of retinaculum integrity, grading of injury and detection of coexisting pathology | Peroneal tendon injury |
| Less postoperative pain | Recurrence of peroneal tendon instability |
| Less peritendinous fibrosis | |
| Subjective tightness at peroneal tendons |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. Peroneal tendoscopy is performed via the proximal and distal portals. The fibrous tissue covering the lateral cortex of the lateral malleolus is resected and the underlying cortical bone is decorticated. Q-FIX MINI suture anchors are inserted into the ridge of the retrofibular groove. The peroneal tendons are shifted medially and splinted with a K-wire. The superior peroneal retinaculum is sutured with the suture limbs of the anchors. The retinaculum is pushed back to the lateral malleolus and the sutures are tied. Finally, the reduction of the retinaculum back to the lateral malleolus is confirmed endoscopically.
References
- 1.Eckert W., Davis E. Acute rupture of the peroneal retinaculum. J Bone Joint Surg Am. 1976;58:670–672. [PubMed] [Google Scholar]
- 2.Arrowsmith S.R., Fleming L.L., Allman F.L. Traumatic dislocations of the peroneal tendons. Am J Sports Med. 1983;11:142–146. doi: 10.1177/036354658301100306. [DOI] [PubMed] [Google Scholar]
- 3.McGarvey W.C., Clanton T.O. Peroneal tendon dislocations. Arch Phys Med Rehabil. 1971;52:431–433. [Google Scholar]
- 4.Alm A., Lamke L., Liljedahl S. Surgical treatment of dislocation of the peroneal tendons. Injury. 1975;7:14–19. doi: 10.1016/0020-1383(75)90053-4. [DOI] [PubMed] [Google Scholar]
- 5.Earle A., Moritz J., Tapper E. Dislocation of the peroneal tendons at the ankle: An analysis of 25 ski injuries. Northwest Med. 1972;71:108–110. [PubMed] [Google Scholar]
- 6.Murr S. Dislocation of the peroneal tendons with marginal fracture of the lateral malleolus. Bone Joint J. 1961;4:563–565. [Google Scholar]
- 7.Escalas F., Figueras J., Merino J. Dislocation of the peroneal tendons. Long-term results of surgical treatment. J Bone Joint Surg Am. 1980;62:451–453. [PubMed] [Google Scholar]
- 8.McLennan J.G. Treatment of acute and chronic luxations of the peroneal tendons. Am J Sports Med. 1980;8:432–436. doi: 10.1177/036354658000800609. [DOI] [PubMed] [Google Scholar]
- 9.Beck E. Operative treatment of recurrent dislocation of the peroneal tendons. Arch Orthop Trauma Surg. 1981;98:247–250. doi: 10.1007/BF00378876. [DOI] [PubMed] [Google Scholar]
- 10.De S.D., Balasubramaniam P. A repair operation for recurrent dislocation of peroneal tendons. Bone Joint J. 1985;67:585–587. doi: 10.1302/0301-620X.67B4.4030855. [DOI] [PubMed] [Google Scholar]
- 11.Wirth C. A modified Viernstein and Kelly surgical technic for correcting chronic recurrent peroneal tendon dislocation. Z Orthop Ihre Grenzgeb. 1989;128:170–173. doi: 10.1055/s-2008-1039495. [DOI] [PubMed] [Google Scholar]
- 12.Marti R. Dislocation of the peroneal tendons. Am J Sports Med. 1977;5:19–22. doi: 10.1177/036354657700500104. [DOI] [PubMed] [Google Scholar]
- 13.Micheli L.J., Waters P.M., Sanders D.P. Sliding fibular graft repair for chronic dislocation of the peroneal tendons. Am J Sports Med. 1989;17:68–71. doi: 10.1177/036354658901700111. [DOI] [PubMed] [Google Scholar]
- 14.Mick C., Lynch F. Reconstruction of the peroneal retinaculum using the peroneus quartus. A case report. J Bone Joint Surg. 1987;69:296–297. [PubMed] [Google Scholar]
- 15.Miller J. Dislocation of peroneal tendons—a new operative procedure. A case report. Am J Orthop. 1967;9:136–137. [PubMed] [Google Scholar]
- 16.Platzgummer H. On a simple procedure for the operative therapy of habitual peroneal tendon luxation. Arch Orthop Unfallchir. 1967;61:144–150. doi: 10.1007/BF00418812. [DOI] [PubMed] [Google Scholar]
- 17.Poll R., Duijfjes F. The treatment of recurrent dislocation of the peroneal tendons. Bone Joint J. 1984;66:98–100. doi: 10.1302/0301-620X.66B1.6693487. [DOI] [PubMed] [Google Scholar]
- 18.Jones E. Operative treatment of chronic dislocation of the peroneal tendons. J Bone Joint Surg. 1932;14:574–576. [Google Scholar]
- 19.Ferran N.A., Oliva F., Maffulli N. Recurrent subluxation of the peroneal tendons. Sports Med. 2006;36:839–846. doi: 10.2165/00007256-200636100-00003. [DOI] [PubMed] [Google Scholar]
- 20.Heckman D.S., Reddy S., Pedowitz D., Wapner K.L., Parekh S.G. Operative treatment for peroneal tendon disorders. J Bone Joint Surg. 2008;90:404–418. doi: 10.2106/JBJS.G.00965. [DOI] [PubMed] [Google Scholar]
- 21.Hui J., De S.D., Balasubramaniam P. The Singapore operation for recurrent dislocation of peroneal tendons. J Bone Joint Surg Br. 1998;80:325–327. doi: 10.1302/0301-620x.80b2.8293. [DOI] [PubMed] [Google Scholar]
- 22.Mendicino R.W., Orsini R.C., Whitman S.E., Catanzariti A.R. Fibular groove deepening for recurrent peroneal subluxation. J Foot Ankle Surg. 2001;40:252–263. doi: 10.1016/s1067-2516(01)80026-0. [DOI] [PubMed] [Google Scholar]
- 23.Ogawa B.K., Thordarson D.B., Zalavras C. Peroneal tendon subluxation repair with an indirect fibular groove deepening technique. Foot Ankle Int. 2007;28:1194–1197. doi: 10.3113/FAI.2007.1194. [DOI] [PubMed] [Google Scholar]
- 24.Ozbag D., Gumusalan Y., Uzel M., Cetinus E. Morphometrical features of the human malleolar groove. Foot Ankle Int. 2008;29:77–81. doi: 10.3113/FAI.2008.0077. [DOI] [PubMed] [Google Scholar]
- 25.Porter D., McCarroll J., Knapp E., Torma J. Peroneal tendon subluxation in athletes: Fibular groove deepening and retinacular reconstruction. Foot Ankle Int. 2005;26:436–441. doi: 10.1177/107110070502600602. [DOI] [PubMed] [Google Scholar]
- 26.Raikin S.M., Elias I., Nazarian L.N. Intrasheath subluxation of the peroneal tendons. J Bone Joint Surg. 2008;90:992–999. doi: 10.2106/JBJS.G.00801. [DOI] [PubMed] [Google Scholar]
- 27.Tan V., Lin S.S., Okereke E. Superior peroneal retinaculoplasty: A surgical technique for peroneal subluxation. Clin Orthop Rel Res. 2003;410:320–325. doi: 10.1097/01.blo.0000063594.67412.32. [DOI] [PubMed] [Google Scholar]
- 28.Thomas J.L., Lopez-Ben R., Maddox J. A preliminary report on intra-sheath peroneal tendon subluxation: A prospective review of 7 patients with ultrasound verification. J Foot Ankle Surg. 2009;48:323–329. doi: 10.1053/j.jfas.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Title C.I., Jung H.-G., Parks B.G., Schon L.C. The peroneal groove deepening procedure: A biomechanical study of pressure reduction. Foot Ankle Int. 2005;26:442–448. doi: 10.1177/107110070502600603. [DOI] [PubMed] [Google Scholar]
- 30.Walther M., Morrison R., Mayer B. Retromalleolar groove impaction for the treatment of unstable peroneal tendons. Am J Sports Med. 2009;37:191–194. doi: 10.1177/0363546508324310. [DOI] [PubMed] [Google Scholar]
- 31.Hau W.W.S., Lui T.H., Ngai W.K. Endoscopic superior peroneal retinaculum reconstruction. Arthrosc Tech. 2017;7:e45–e51. doi: 10.1016/j.eats.2017.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Dijk C.N., Kort N. Tendoscopy of the peroneal tendons. Arthroscopy. 1998;14:471–478. doi: 10.1016/s0749-8063(98)70074-x. [DOI] [PubMed] [Google Scholar]
- 33.Lui T.H., Mak C.Y. Peroneus longus tendoscopy at the sole: A cadaveric study. Arthroscopy. 2015;31:1338–1342. doi: 10.1016/j.arthro.2015.01.024. [DOI] [PubMed] [Google Scholar]
- 34.Jerosch J., Aldawoudy A. Tendoscopic management of peroneal tendon disorders. Knee Surg Sports Traumatol Arthrosc. 2007;15:806–810. doi: 10.1007/s00167-006-0227-2. [DOI] [PubMed] [Google Scholar]
- 35.van Dijk P., Yasui Y., Murawski C., Duke G., Kennedy J. Functional outcomes of peroneal tendoscopy in the treatment of peroneal tendon disorders. Arthroscopy. 2016;32(suppl):e21. doi: 10.1007/s00167-016-4012-6. [DOI] [PubMed] [Google Scholar]
- 36.de Leeuw P.A., van Dijk C.N., Golanó P. A 3-portal endoscopic groove deepening technique for recurrent peroneal tendon dislocation. Tech Foot Ankle Surg. 2008;7:250–256. [Google Scholar]
- 37.Lui T.H. Endoscopic Peroneal retinaculum reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:478–481. doi: 10.1007/s00167-005-0691-0. [DOI] [PubMed] [Google Scholar]
- 38.Lui T.H. Concomitant lateral ankle and peroneal tendon instability treated with simultaneous arthro-scopic Brostrom and tendoscopic superior peroneal retinaculum repair: A case report. J Foot Ankle Surg. 2021;60:850–855. doi: 10.1053/j.jfas.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 39.Park S.H., Choi Y.R., Lee J., Seo J., Lee H.S. Treatment of recurrent peroneal tendon dislocation by peroneal retinaculum reattachment without fibular groove deepening. J Foot Ankle Surg. 2021;60:994–997. doi: 10.1053/j.jfas.2020.04.027. [DOI] [PubMed] [Google Scholar]
- 40.Deng E., Shi W., Jiao C., et al. Reattachment of the superior peroneal retinaculum versus the bone block procedure for the treatment of recurrent peroneal tendon dislocation: Two safe and effective techniques. Knee Surg Sports Traumatol Arthrosc. 2019;27:2877–2883. doi: 10.1007/s00167-019-05479-2. [DOI] [PubMed] [Google Scholar]
- 41.Lui T.H. Endoscopic management of recalcitrant retrofibular pain without peroneal tendon subluxation or dislocation. Arch Orthopaedic Trauma Surg. 2012;132:357–361. doi: 10.1007/s00402-011-1392-4. [DOI] [PubMed] [Google Scholar]
- 42.Lui T.H. Eckert and Davis grade 3 superior peroneal retinaculum injury: Treated by endoscopic peroneal retinaculum reconstruction and complicated by malposition of the suture anchors. J Orthop Case Rep. 2015;5:73. doi: 10.13107/jocr.2250-0685.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. Peroneal tendoscopy is performed via the proximal and distal portals. The fibrous tissue covering the lateral cortex of the lateral malleolus is resected and the underlying cortical bone is decorticated. Q-FIX MINI suture anchors are inserted into the ridge of the retrofibular groove. The peroneal tendons are shifted medially and splinted with a K-wire. The superior peroneal retinaculum is sutured with the suture limbs of the anchors. The retinaculum is pushed back to the lateral malleolus and the sutures are tied. Finally, the reduction of the retinaculum back to the lateral malleolus is confirmed endoscopically.
Endoscopic reconstruction of the right superior peroneal retinaculum using the Q-FIX MINI suture anchor. The patient is in the lateral position. Peroneal tendoscopy is performed via the proximal and distal portals. The fibrous tissue covering the lateral cortex of the lateral malleolus is resected and the underlying cortical bone is decorticated. Q-FIX MINI suture anchors are inserted into the ridge of the retrofibular groove. The peroneal tendons are shifted medially and splinted with a K-wire. The superior peroneal retinaculum is sutured with the suture limbs of the anchors. The retinaculum is pushed back to the lateral malleolus and the sutures are tied. Finally, the reduction of the retinaculum back to the lateral malleolus is confirmed endoscopically.