Abstract
In endodontics, metal artifacts are the major weak points of employing cone-beam computed tomography (CBCT) in teeth with metallic posts and restorations. The aim of this article is to introduce a novel technique for preparation of beneficial CBCT images of anterior teeth with metal posts and/or crowns. In this novel technique, the patient who was instructed to take CBCT images for reason of implant surgery, was asked to puff out his cheeks/lips during the rotation of x-ray tube. By comparing the image taken with this technique to normal image it was obvious that after applying the cheek puffing technique, the metal artifacts around restored anterior teeth significantly reduced. Then it seems that this novel technique removes the metal artifacts from the crowned teeth to distances far from the tooth structure and enables more accurate diagnosis.
Key Words: Artifact, Cone-Beam Computed Tomography, Cone-Beam Computer-Assisted Tomography, Endodontics, Metal Artifact Reduction
Introduction
Success of endodontic diagnosis and treatment depends on diagnostic imaging techniques that provide information about the target tooth and its surrounding structures [1]. Radiographic examination provides a basis for all aspects of endodontics from diagnosis and treatment planning to outcome assessment [2]. Although the conventional periapical radiography has held on to its place as the endodontic imaging principle, modern techniques of medical imaging have also been successfully utilized in endodontics [3]. These efforts started from applying conventional computed tomography (CT) and micro-CT in dental practice and upon introduction of maxillofacial cone-beam computed tomography (CBCT) [aka. digital volume tomography (DVT)] in 1996, provided the first clinically and practically applicable three-dimensional (3D) imaging technology for dentistry and more specifically endodontics [3]. By providing true 3D images at a lower cost than conventional CT and with radiation risks almost comparable to current methods of intraoral imaging, CBCT can be labeled as the major advancement in dentoalveolar imaging [3, 4]. CBCT 3D images have been successfully applied in implantology, endodontics, detection of oral and maxillofacial lesions, orthodontics, periodontics, temporomandibular joint disorders (TMD), etc. [2, 4]. CBCT has cone-shaped x-ray beam that captures a 3D volume of data, described as the field of view (FOV) [5]. A single sweep of the scanner (beam source) scans the field of interest and the sensor that rotates 180-360 degrees around the patient’s head, captures the 3D image [6, 7].
In endodontics, the application of CBCT should be limited to conditions such as identification of apical periodontitis [8], expansion of lesions into the maxillary sinus [9], thickening of the sinus membrane [10], missed canals [11], planning of surgical endodontic treatment [12], spatial relationship of the specific tooth root to adjacent anatomical structures [13-15], detecting the severity of traumatic dental injuries [16], localizing and differentiation of types of root resorption [17] and determining the prognosis and treatment planning [18], detection and management of anatomical and morphological anomalies such as dens invaginatus and tooth fusion [11], and the last but not the least, detecting the presence of vertical root fractures (VRFs) [19, 20].
The problem with detection of VRF from radiographic appearances such as J-shaped and halo-shaped radiolucencies is that they do not appear until the occurrence of considerable bone destruction [2]. Moreover, they may also be similar to radiolucencies that occur in cases of apical periodontitis not associated with VRF [21]. Studies have shown that CBCT is more sensitive in identification of VRF [19, 21, 22]. However, due to the artifacts produced by the root filling or other high-density intraradicular materials, CBCT may not always correctly suggest the presence/absence of a VRF [22, 23]. The similar scenario stands for detection of extra/missed canals in cases of endodontic retreatment [1].
Artifacts have always caused difficulties in diagnosis and are induced by discrepancies between the actual physical conditions of the measuring object and the simplified mathematical assumptions used for 3D reconstruction [24, 25]. It is no surprise that the technical community puts considerable efforts into developing techniques for artifact reduction. It would be expected that improvement of the artefact can be achieved by compensating for the added intensity recorded by the detector owing to beam hardening and scatter radiation. The aim of this article is to introduce a novel, available and viable technique for reducing the metal artifacts in anterior segments of the jaws that can potentially cause diagnosis challenges in endodontics.
Case Report
The CBCT images were taken from a patient who was referred for surgical evaluation for implantation of tooth #9. Patient had full porcelain-fused-to-metal prosthetic crowns on all maxillary incisors and canines that could cause artifacts using Scanora 3D CBCT device (Soredex, Orion Corp. Ltd., Helsinki, Finland). Pre-implant surgery image was taken with cheek puffing-out technique, while post-implant image was taken with conventional technique. Similar to usual approaches, in this modification, CBCT images were taken with patient sitting, and then the patient’s head was immobilized by a chin cap, bite fork, etc; however, before starting the imaging process, the patient was instructed to blow in his cheeks with his lips sealed.
Results
Figures 1 and 2 show the CBCT images of same patient before and after applying puffed-out cheeks technique. As it is obvious, presence of air between the labial soft tissue and teeth, minimizes the streaks and beam hardening artifacts. If images are taken with routine techniques, these artifacts stay limited to the surrounding soft tissues without being visible in the outer space.
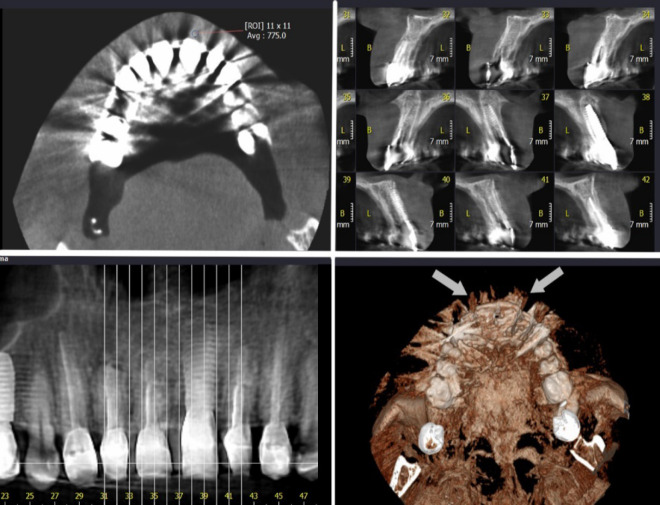
Figure 1.
Axial, cross sectional, panoramic and reconstructed three-dimensional image of maxilla with metallic crowns on the anterior teeth, taken with conventional technique for evaluation after implantation of tooth 9. The metal artifacts can be seen as white opaque lines lining towards buccal and palatal (white arrow in reconstructed image); Note the gray value of the buccal soft tissue
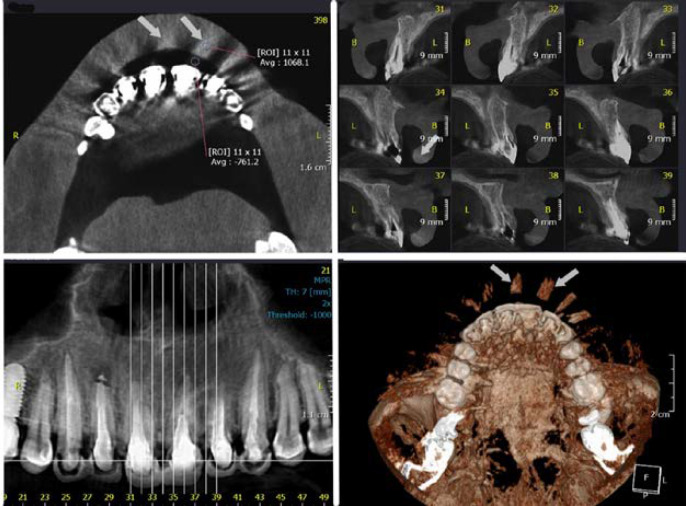
Figure 2.
Axial, cross sectional, panoramic and reconstructed three-dimensional image of maxilla with metallic crowns on the anterior teeth, taken with cheek puffing technique from the same patient before implantation of tooth 9. The white opaque lines (metal artifacts) are not present on teeth anymore; instead they have moved far from the teeth inside the soft tissue (white arrow in reconstructed image); Note the gray value of the buccal soft tissue
Discussion
This article introduced a novel and easily applicable technique for reducing the different CBCT artifacts caused by differential absorption of large amounts of x-ray beam by the existing metallic structures (implants, metallic crowns, posts, etc.) that reduce the diagnostic ability of CBCT images. These artifacts include beam hardening, streaks and cupping effect.
An image artifact may be defined as a visualized structure in the reconstructed data that is not present in the real object [23]. Generally speaking, artefacts [including beam hardening, extinction, scatter, noise, exponential edge gradient effect, aliasing, partial volume effect, and object motion [26] are important problems in CBCT imaging that are induced by discrepancies between the actual physical conditions of the measuring object and the simplified mathematical assumptions used for 3D reconstruction [24, 25]. Beam hardening is one of the most prominent sources of artefacts [27]. When the X-ray beam encounters the subject, lower energy photons (with lower wavelength) in the polychromatic spectrum of the X-ray beam, are absorbed by the very high-density objects such as enamel or metallic restorations [25]. The higher the atomic number (density) of the material, the larger the amount of absorbed wavelengths [22]. As a result, highly absorbing material functions as a filter positioned within the object and the mean energy of the X-ray beam increases, which is referred to as beam hardening [24]. It has been shown that even light metal (such as titanium in implant fixtures) causes massive beam hardening for the typical kilovoltages applied in CBCT machines [28]. This phenomenon produces two types of artifact that can reduce the diagnostic yield of the images: distortion of metallic structures, called cupping artifact and the appearance of streaks and dark bands between two dense structures [7].
Cupping artifact appears at sharp edges with high contrast (e.g. at metallic crown borders) to neighboring structures. It happens when the inversion formulas assume true lines in a mathematical sense, whereas in reality the lines measured the average absorption over a finite line width [24]. Streaks happen when the emitted spectrum contains more relatively low-energy rays than that recorded on the detector (in other words the beam is hardened). In the 3D reconstruction, the error is back projected into the volume, resulting in darks streaks [7]. Artefact formations by beam hardening and scatter are very similar because they both reduce the measured attenuation coefficients by amounts which depend on the measured intensity and produce a common artefact known as the cupping effect artefact. In clinical practice, reducing the size of FOV, separating the patient’s dental arches, increasing the kilovoltages/milliamperages or decreasing the slice thickness have been suggested to minimize these artifacts.
The idea of puffing out the cheeks is not a new era in oromaxillofacial radiology. Intraoral or lateral x-ray imaging of sialoliths in the distal portion of the Stensen’s duct or parotid
gland is always accompanied by superimposition of bony structures on the sialoliths. However, if the posterioanterior skull projection is taken with the cheeks puffed out, the image of sialoliths is rendered visible free of the adjacent bone. If puffed-out cheeks are not possible for any reason, placement of a cotton role in the labial vestibule can mimic the air in terms of gray value (the amount of Hounsfield units (HU) for cotton role and air in CBCT is ~1000).
The theory of the presented technique stemmed from the fact that each CBCT image is interpreted from two-dimensional frame rates: the higher the number of frame rates, the higher signal-to-noise ratio and reduced metallic artifacts. However it is also associated with longer scan time and patient dose. Another way could be increasing the quality of frame rates instead of their number. For instance, in CBCT images the air surrounding patient’s head is shown with close-to-real HU gray values (~-1000) but the similar air present in the sinus cavities are presented with gray values far way different from the true values (Figure 3). This phenomenon is attributed to the fact that x-ray beams in the space outside patient’s head reach the detector without being weakened while those beams that represent the intra-sinus air to the detector, have been weakened and altered after passing through the skull and prosthetic structures. It can be assumed that if some x-ray beams with little or no attenuation reach the detector, the final CBCT image will be constructed of pixels that have not much gray values. If the image is taken with puffed-out cheeks, the frame rates that are created with beams tangent to the anterior teeth, will have much lower attenuation and resultant images will have low gray values. In other words, in case of existing metallic structures, the streaks and cupping artifacts are moved away from the tooth surface and are present in the buccal soft tissues separated from the teeth with air-filled space.
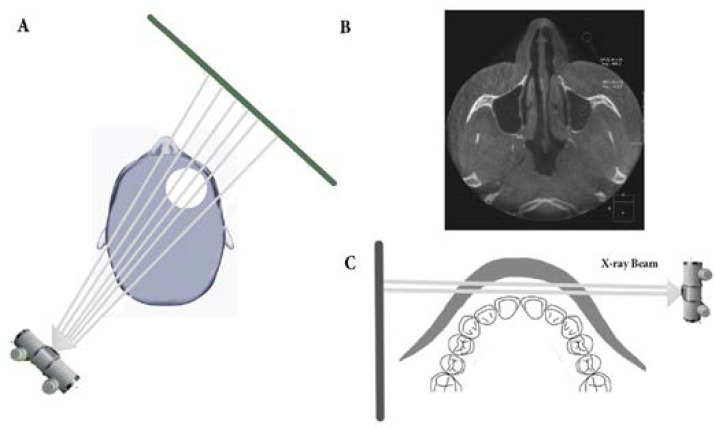
Figure 3.
A) X-ray beams pass a notable tissue mass before and after entering the lucent air inside the sinuses. However, the photons passing through the air outside patient’s head, are not attenuated; B) Note the great difference between gray values of air inside the sinus and air the air surrounding patient’s head; C) In cheek puffing technique, the photons that pass perpendicular to the sagittal plan, are rarely attenuated
After evaluation of this patient by the authors, this technique proved to be effective in elimination the metal artifacts from the anterior teeth were the overlying labial soft tissues can be displaced by blowing the cheeks. However, it cannot be applied for posterior teeth because of the existing bony structures.
Conclusion
It seems that application of cheek puffed-out technique can considerably reduce the metal artifacts of CBCT images from anterior teeth with metallic posts and crowns; employing the novel technique lead to more accurate endodontic diagnosis.
Acknowledgment
Authors wish to thank Prof. Saeed Asgary.
Conflict of Interest:
‘None declared’.
References
- 1.Matherne RP, Angelopoulos C, Kulild JC, Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro. J Endod. 2008;34(1):87–9. doi: 10.1016/j.joen.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 2.Liang YH, Li G, Wesselink PR, Wu MK. Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod. 2011;37(3):326–31. doi: 10.1016/j.joen.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 3.Cohenca N, Shemesh H. Clinical applications of cone beam computed tomography in endodontics: A comprehensive review. Quintessence Int. 2015;46(8):657–68. doi: 10.3290/j.qi.a34396. [DOI] [PubMed] [Google Scholar]
- 4.Mota de Almeida FJ, Knutsson K, Flygare L. The impact of cone beam computed tomography on the choice of endodontic diagnosis. Int Endod J. 2015;48(6):564–72. doi: 10.1111/iej.12350. [DOI] [PubMed] [Google Scholar]
- 5.Kamburoglu K. Use of dentomaxillofacial cone beam computed tomography in dentistry. World J Radiol. 2015;7(6):128–30. doi: 10.4329/wjr.v7.i6.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiarudi AH, Eghbal MJ, Safi Y, Aghdasi MM, Fazlyab M. The applications of cone-beam computed tomography in endodontics: a review of literature. Iran Endod J. 2015;10(1):16–25. [PMC free article] [PubMed] [Google Scholar]
- 7.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008;52(4):707–30, v. doi: 10.1016/j.cden.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Estrela C, Silva JA, de Alencar AH, Leles CR, Decurcio DA. Efficacy of sodium hypochlorite and chlorhexidine against Enterococcus faecalis--a systematic review. J Appl Oral Sci. 2008;16(6):364–8. doi: 10.1590/S1678-77572008000600002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bornstein MM, Wasmer J, Sendi P, Janner SF, Buser D, von Arx T. Characteristics and dimensions of the Schneiderian membrane and apical bone in maxillary molars referred for apical surgery: a comparative radiographic analysis using limited cone beam computed tomography. J Endod. 2012;38(1):51–7. doi: 10.1016/j.joen.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 10.Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone-beam computed tomography evaluation of maxillary sinusitis. J Endod. 2011;37(6):753–7. doi: 10.1016/j.joen.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 11.de Toubes KM, Cortes MI, Valadares MA, Fonseca LC, Nunes E, Silveira FF. Comparative analysis of accessory mesial canal identification in mandibular first molars by using four different diagnostic methods. J Endod. 2012;38(4):436–41. doi: 10.1016/j.joen.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 12.Bornstein MM, Lauber R, Sendi P, von Arx T. Comparison of periapical radiography and limited cone-beam computed tomography in mandibular molars for analysis of anatomical landmarks before apical surgery. J Endod. 2011;37(2):151–7. doi: 10.1016/j.joen.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Kovisto T, Ahmad M, Bowles WR. Proximity of the mandibular canal to the tooth apex. J Endod. 2011;37(3):311–5. doi: 10.1016/j.joen.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 14.Dalili Kajan Z, Taramsari M, Khosravi Fard N, Kanani M. Accuracy of Cone-beam Computed Tomography in Comparison with Standard Method in Evaluating Root Canal Morphology: An In Vitro Study. Iran Endod J. 2018;13(2):181–7. doi: 10.22037/iej.v13i2.18614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safi Y, Hosseinpour S, Aziz A, Bamedi M, Malekashtari M, Vasegh Z. Effect of Amperage and Field of View on Detection of Vertical Root Fracture in Teeth with Intracanal Posts. Iran Endod J. 2016;11(3):202–7. doi: 10.7508/iej.2016.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Faus-Matoses V, Martinez-Vinarta M, Alegre-Domingo T, Faus-Matoses I, Faus-Llacer VJ. Treatment of multiple traumatized anterior teeth associated with an alveolar bone fracture in a 20-year-old patient: A 3-year follow up. J Clin Exp Dent. 2014;6(4):e425–9. doi: 10.4317/jced.51374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Estevez R, Aranguren J, Escorial A, de Gregorio C, De La Torre F, Vera J, Cisneros R. Invasive cervical resorption Class III in a maxillary central incisor: diagnosis and follow-up by means of cone-beam computed tomography. J Endod. 2010;36(12):2012–4. doi: 10.1016/j.joen.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 18.Kamburoglu K, Kursun S, Yuksel S, Oztas B. Observer ability to detect ex vivo simulated internal or external cervical root resorption. J Endod. 2011;37(2):168–75. doi: 10.1016/j.joen.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Melo SL, Bortoluzzi EA, Abreu M Jr, Correa LR, Correa M. Diagnostic ability of a cone-beam computed tomography scan to assess longitudinal root fractures in prosthetically treated teeth. J Endod. 2010;36(11):1879–82. doi: 10.1016/j.joen.2010.08.025. [DOI] [PubMed] [Google Scholar]
- 20.Dalili Kajan Z, Taramsari M, Khosravi Fard N, Khaksari F, Moghasem Hamidi F. The Efficacy of Metal Artifact Reduction Mode in Cone-Beam Computed Tomography Images on Diagnostic Accuracy of Root Fractures in Teeth with Intracanal Posts. Iran Endod J. 2018;13(1):47–53. doi: 10.22037/iej.v13i1.17352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edlund M, Nair MK, Nair UP. Detection of vertical root fractures by using cone-beam computed tomography: a clinical study. J Endod. 2011;37(6):768–72. doi: 10.1016/j.joen.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 22.Safi Y, Aghdasi MM, Ezoddini-Ardakani F, Beiraghi S, Vasegh Z. Effect of Metal Artifacts on Detection of Vertical Root Fractures Using Two Cone Beam Computed Tomography Systems. Iran Endod J. 2015;10(3):193–8. doi: 10.7508/iej.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iikubo M, Osano T, Sano T, Katsumata A, Ariji E, Kobayashi K, Sasano T, Wakoh M, Seki K, Kojima I, Sakamoto M. Root canal filling materials spread pattern mimicking root fractures in dental CBCT images. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):521–7. doi: 10.1016/j.oooo.2015.06.030. [DOI] [PubMed] [Google Scholar]
- 24.Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, Schoemer E. Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011;40(5):265–73. doi: 10.1259/dmfr/30642039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ritter L, Mischkowski RA, Neugebauer J, Dreiseidler T, Scheer M, Keeve E, Zoller JE. The influence of body mass index, age, implants, and dental restorations on image quality of cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(3):e108–16. doi: 10.1016/j.tripleo.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Nabha W, Hong YM, Cho JH, Hwang HS. Assessment of metal artifacts in three-dimensional dental surface models derived by cone-beam computed tomography. Korean J Orthod. 2014;44(5):229–35. doi: 10.4041/kjod.2014.44.5.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hunter AK, McDavid WD. Characterization and correction of cupping effect artefacts in cone beam CT. Dentomaxillofac Radiol. 2012;41(3):217–23. doi: 10.1259/dmfr/19015946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schulze RK, Berndt D, d'Hoedt B. On cone-beam computed tomography artifacts induced by titanium implants. Clin Oral Implants Res. 2010;21(1):100–7. doi: 10.1111/j.1600-0501.2009.01817.x. [DOI] [PubMed] [Google Scholar]