Abstract
With the increasing popularity of hip arthroscopy, postoperative iatrogenic instability due to bony and soft-tissue issues has been noted by more orthopaedic surgeons. Although there is a low risk of serious complications in patients with normal hip joint development even without suturing of the joint capsule, for patients with a preoperative high risk of anterior instability—including those with excessive anteversion of the acetabulum or femur, borderline dysplasia of the hip, and hip arthroscopic revision surgery with an anterior defect of the joint capsule—capsulotomy without repair will result in postoperative anterior instability of the hip joint and related symptoms. Capsular suturing techniques that provide anterior stabilization will be of great help for these high-risk patients and reduce the possibility of postoperative anterior instability. In this Technical Note, we introduce the arthroscopic capsular suture-lifting technique for treating femoroacetabular impingement (FAI) patients with a high risk of postoperative hip instability. In the past 2 years, the capsular suture-lifting technique has been used to treat FAI patients with borderline dysplasia of the hip and excessive femoral neck anteversion, and clinical results have shown that the suture-lifting technique provides a reliable and effective solution for FAI patients with a high risk of postoperative anterior hip instability.
Given the evolution of hip arthroscopic surgery over the past 20 years, hip arthroscopy is becoming the treatment of choice for femoroacetabular impingement (FAI) and hip labral tears compared with the conventional surgical dislocation technique.1, 2, 3, 4 However, because of the popularity of hip arthroscopy, there have been unforeseen postoperative complications associated with this technique.4, 5, 6 Postoperative iatrogenic instability including anterior hip dislocation and subluxation is gaining attention from more orthopaedic surgeons.6, 7, 8, 9, 10, 11, 12 For arthroscopic views and exposure of labral tears, an intraportal cut of the anterior capsule between the anterolateral (AL) portal and midanterior portal (MAP) is necessary. There is a low risk of serious complications in patients with normal hip joint development even without suturing of the joint capsule. However, it is worth noting that for patients with a high risk of preoperative anterior instability, capsulotomy and inappropriate joint capsule management may result in postoperative anterior instability of the hip joint and related symptoms. Risk factors include excessive anteversion of the acetabulum or femur, borderline dysplasia of the hip (BDDH), and hip arthroscopic revision surgery with an anterior defect of the joint capsule. As is well known, the anterior joint capsule plays an essential role in anterior stability of the hip joint, especially in patients with a high risk of postoperative anterior instability.9,13, 14, 15, 16, 17 Unlike suture repair or reconstruction of the anterior joint capsule for an anterior defect of the joint capsule, a specific capsular suturing technique is needed to close the incision of the anterior joint capsule and improve anterior stability in high-risk patients. In this Technical Note, we introduce the arthroscopic capsular suture-lifting technique for treating FAI patients with a high risk of postoperative hip instability. We have been using the capsular suture-lifting technique to achieve better anterior stability of the hip joint during surgery. It restores the integrity of the anterior joint capsule and improves the tension of the anterior soft tissue, preventing postoperative anterior instability. We have used the technique in FAI patients with BDDH and excessive femoral neck anteversion in the past 2 years and found that it provides a reliable and effective solution for treating FAI patients with a high risk of postoperative anterior hip instability.
Surgical Technique
The patient is positioned supine on a traction table (Smith & Nephew, Andover, MA) and is prepared and draped in the standard fashion. Considering the greater trochanter and anterior superior iliac spine as anatomic landmarks, 4 portals are established in succession during surgery: AL portal, MAP, distal AL accessory portal (DALA), and proximal midanterior portal (PMAP).
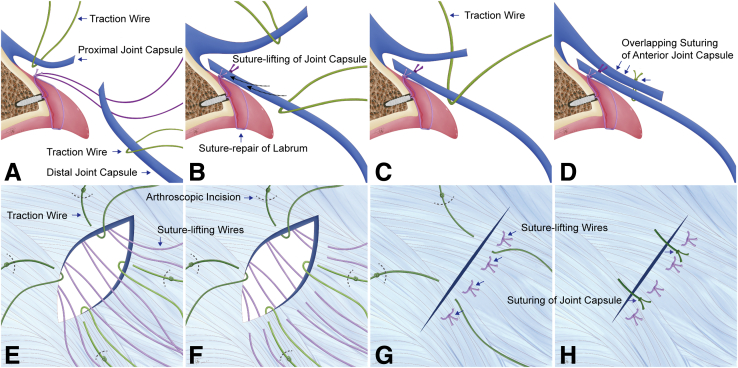
Normally, we use 4 portals during the surgical procedure, as described in our previous study.18 The AL portal is established first. The MAP is made from the AL portal with inspection using a 30° arthroscope. By use of the AL portal and MAP, the joint capsule is cut transversely from the 10- to 3-o’clock position for labral exposure. To avoid a defect of the joint capsule that may be caused by using a banana-blade knife and shaver and to achieve a flat rim of the joint capsule after incision, a radiofrequency device is used for the incision of the joint capsule instead. The DALA portal is established for rim preparation and anchor placement. To obtain a better arthroscopic view for exploration of the labral tear, 2 capsular traction wires are passed through the AL portal and MAP, respectively, for adequate exposure of the acetabular rim (Fig 1 A and E). A cannula is used for assistance while instruments are passed through the portals if necessary. According to the evaluation of the labral tear, suture anchors are placed at a distance of 3 mm from the articular surface, from the 3-o’clock position medially to laterally through the DALA portal, based on the location and range of the labral tear. To achieve efficient lifting of the anterior joint capsule, suture anchors are placed at the 3-, 2-, 1-, and 12-o’clock positions of the acetabulum. Such an anchor distribution could provide a reliable suture-lifting effect for the anterior joint capsule based on the anatomy and shape of the anterior joint capsule and iliofemoral ligament. The PMAP is established next, with fixation of anchors. Double-loaded suture anchors are applied in this technique; 1 suture of the anchor is retrieved from the PMAP and temporarily fixed for further use, and the other suture is used for labral repair with the luggage-tag suture technique (Fig 1 A and B). After suture repair of the labral tear, 2 capsular traction suture wires are used for the distal joint capsule from the AL portal and MAP to provide better exposure of the femoral neck for femoroplasty. The extra-articular side of the capsular traction suture wire is tied with a knot for better distinction between intra- and extra-articular sutures (Fig 1 E and F). By use of the PMAP as a viewing portal, femoroplasty is alternately performed through the AL portal and MAP with a radiofrequency device and a burr.
Fig 1.
Surgical procedures in arthroscopic capsular suture-lifting technique. (A-D) Methods by which anterior joint capsule (A, B) and overlapping suture of joint capsule (C, D) are lifted. (E-H) Simulation of arthroscopic view showing position of suture passing from joint capsule. The purple sutures are from the suture anchors, one of which is used for suture repair of the labrum (E) whereas the other is used for lifting the joint capsule (F, G). The green sutures are the traction sutures. Both proximal and distal traction sutures are used to lift the joint capsule for a better arthroscopic view. (H) The traction wires are passed from proximal to distal for suturing of the interportal cut of the joint capsule, and finally achieve an overlapping suturing of the anterior joint capsule.
The viewing portal is switched from the PMAP to the AL portal, and the hip is flexed to 40° to 60° for relaxation of the anterior joint capsule before suturing. A grasping forceps is used from the PMAP to hold the distal joint capsule, and a bird-beak device is used from the MAP to pierce the distal joint capsule, grab the suture wire, and pull the suture wires out from the MAP (Fig 1 A and F). Considering the hip joint capsule as dense connective tissue, piercing the distal joint capsule using a bird-beak device requires the combined force from the grasping forceps to hold the joint capsule and the assistance of the reaction force from the traction suture wire of the distal joint capsule. Four suture anchors are typically used for suture lifting, and 8 sutures are passed through the distal joint capsule (Fig 1F). The sutures from the same anchor are knotted in pairs to achieve suture lifting and drag the distal joint capsule close to the acetabular rim to improve anterior stability (Fig 1 C and G).
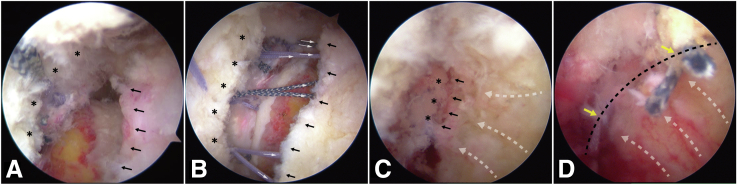
The proximal joint capsule traction suture is pulled out through the distal joint capsule and knotted for closure of the joint capsule (Fig 1 D and H), ensuring more reliable suturing of the joint capsule and providing a “retention suture” for the suture-lifting wires. Finally, the hip joint is slowly extended after closure of the joint capsule (Fig 2). Video 1 shows the main surgical procedures of the suture-lifting technique.
Fig 2.
Arthroscopic view of capsular suture-lifting technique. (A) By use of the anterolateral portal as the viewing portal and the midanterior portal and proximal midanterior portal as the working portals, the suture-lifting technique is performed. The asterisks indicate the proximal joint capsule, and the black arrows indicate the distal joint capsule. (B) A total of 8 “lifting” suture wires (4 pairs) (white arrows) are passed through the distal joint capsule. (C) The distal joint capsule is perfectly lifted and fixed to the acetabular rim. The joint capsule is overlapped and sutured with traction wire. (D) The white arrows indicate a lifting effect on the distal joint capsule after suturing in C and the yellow arrows indicate reliable closure of the joint capsule using suture-lifting technique.
Discussion
Postoperative anterior instability due to developmental factors is an intractable complication of hip arthroscopy. The risk factors for hip instability after arthroscopy include dysplasia and iatrogenic factors. Although postoperative anterior instability occurs after unrepaired capsulectomy or could be pathologic in most cases, for patients with ligamentous hyperlaxity, excessive femoral and acetabular anteversion, or BDDH, we can reduce the incidence of postoperative instability through improvements in suturing techniques.
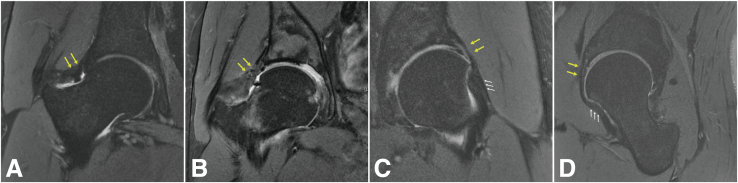
Additionally, although postoperative instability of the hip joint can be caused by multiple factors, the most common of these factors—iatrogenic factors—can be avoided by strict control of surgical indications, improvements in surgical techniques, and appropriate management of the joint capsule for high-risk patients.19, 20, 21, 22, 23 Our capsular suture-lifting technique restores the integrity of the anterior capsule of the hip joint, improves the tension of the anterior soft tissue, and prevents postoperative anterior instability in high-risk patients. Over the past 2 years, we have applied this surgical technique for the treatment of FAI patients with a high risk of postoperative hip instability, including BDDH and excessive femoral or acetabular anteversion (Table 1); Figure 3 shows healing and the morphology of the lifted joint capsule 1 year after surgery. However, for patients who undergo multiple hip arthroscopies or open hip surgical procedures and who may have an anterior joint capsule defect and persistent instability symptoms, anterior capsular reconstruction via arthroscopic or open surgery will be necessary instead of the suture-lifting technique. Therefore, in our experience, “suture lifting” can be a reliable technique for most at-risk patients, and only a few cases will require reconstruction of the anterior joint capsule or iliofemoral ligament. Only 1 patient among more than 1,000 cases treated in our department underwent arthroscopic anterior capsule reconstruction using fascia lata owing to a previous arthroscopic capsulotomy.
Table 1.
Indications and Contraindications of Technique
| Indications |
| Acetabular anteversion angle > 20° |
| Femoral anteversion angle > 20° |
| BDDH with LCEA of 18°-25° |
| Arthrochalasis |
| Arthroscopic revision for postsurgical instability without hip capsular deficiency |
| Contradictions |
| Moderate or severe DDH |
| Postsurgical instability with hip capsular deficiency |
BDDH, borderline developmental dysplasia of hip; DDH, developmental dysplasia of hip; LCE, lateral center-edge angle.
Fig 3.
Healing and morphology of lifted joint capsule 1 year after surgery. (A, B) Magnetic resonance imaging of healed anterolateral joint capsules (yellow arrows) in right hips of 29-year-old female patient and 26-year-old male patient in oblique coronal plane. (C, D) Magnetic resonance imaging of lifted joint capsule (yellow arrows) in left hip of 37-year-old female patient in oblique coronal plane (C) and oblique sagittal plane (D). The white arrows indicate the lifted zona orbicularis after suturing of the joint capsule using the suture-lifting technique.
The hip joint capsule, especially the anterior ligament, is an important stabilizer of the hip joint in terms of anterior stability.24, 25, 26 By resisting anterior translation of the femoral head and external rotation of the extended hip, the iliofemoral ligament plays a dominant role in anterior stabilization. An unrepaired anterior capsulotomy has been suggested to lead to postoperative anterior instability, especially for at-risk patients with excessive femoral neck or acetabular anteversion. Moreover, regarding anterior capsulotomy, labral debridement is a risk factor for anterior instability in patients with subtle or borderline dysplastic features, and owing to the dynamic role of the iliopsoas as the anterior stabilizer of the hip joint, iliopsoas tenotomy should also be avoided in these patients. With this surgical technique, we use at least 6 sutures passing through the iliofemoral ligament during the operation to ensure closure of the iliofemoral ligament for restoration of anterior stability of the hip joint. Technical pearls and pitfalls of this technique are described in Table 2. With the suture-lifting technique, the joint capsule incision is closed whereas anterior stability of the hip joint is improved, making it possible to address impingement, labral tears, and microinstability in a single arthroscopic procedure. The suture-lifting technique provides a “belt-and-braces” approach for suturing the hip joint capsule, from both suture anchor and capsular traction sutures (Fig 1), making our technique more reliable than previous suturing techniques for the hip joint capsule (Table 3). In this Technical Note, we have aimed to raise awareness of this preventable complication and provide an efficient and reliable suture-lifting technique for arthroscopic restoration of anterior instability.
Table 2.
Pearls and Pitfalls
| Pearls |
| The extra-articular side of the capsular traction suture wire is tied with a knot for better distinction between intra- and extra-articular sutures. |
| For relaxation of the anterior joint capsule, it is necessary to flex the hip joint to 40°-60° before suturing of the joint capsule. |
| A grasping forceps is used from the PMAP to hold the distal joint capsule, and a bird-beak device is used from the MAP to pierce the distal joint capsule, grab the suture wire, and pull the suture wires out from the MAP. Piercing the distal joint capsule using a bird-beak device requires the combined force from the grasping forceps to hold the joint capsule and the assistance of the reaction force from the traction suture wire of the distal joint capsule. |
| Pitfalls |
| To avoid a defect of the joint capsule that may be caused by using a banana-blade knife and shaver and to achieve a flat rim of the joint capsule after incision, an RF device is used for the incision of the joint capsule instead. |
MAP, midanterior portal; PMAP, proximal midanterior portal; RF, radiofrequency.
Table 3.
Advantages and Limitations of Technique
| Advantages |
| By use of the suture-lifting technique, the joint capsule incision is finally closed; meanwhile, anterior stability of the hip joint is improved by suturing, making it possible for treatment of femoroacetabular impingement, labral tears, and microinstability in a single arthroscopic procedure. |
| The suture-lifting technique provides a “belt-and-braces” approach for suturing the hip joint capsule, from both suture anchor and capsular traction sutures, making our technique more reliable than the previous suturing techniques for the hip joint capsule. |
| Limitations |
| Clinical experiences is required for hip arthroscopy because the tension-free state of the joint capsule makes it difficult to perform the arthroscopic suture-lifting technique. |
| Currently, we do not have scoring or quantitative standards for evaluating high-risk factors for preoperative hip instability; therefore, it is impossible to perform individualized suturelifting technique based on preoperative assessment. |
Footnotes
K.T. and G.G. contributed equally to this work and share first authorship.
The authors report the following potential conflicts of interest or sources of funding: The study was supported by Beijing Municipal Natural Science Foundation (No. Z200003), Peking University Medicine Seed Fund for Interdisciplinary Research (No. BMU2021MX022), National Natural Science Foundation of China (No. 81601901), and Natural Science Foundation of Liaoning (No. 2019-MS-079). Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Main surgical procedures of suture-lifting technique. Capsular suturing techniques that provide anterior stabilization will be of great help for these high-risk patients and reduce the possibility of postoperative anterior instability. In this technical note, we introduce the arthroscopic capsular suture-lifting technique for treating femoroacetabular impingement (FAI) patients with a high risk of postoperative hip instability. Video 1 shows the main surgical procedures of the suture-lifting technique: the patient is positioned supine and four portals --anterolateral (AL), mid-anterior portal (MAP), distal AL accessory portal (DALA), and proximal mid-anterior portal (PMAP) --are established in succession during surgery. Using the AL portal and MAP, the joint capsule is cut transversely from the 10 o'clock to 3 o'clock positions for labrum exposure. The DALA portal is established for rim preparation and anchor placement. Two capsular traction wires are passed through the AL portal and MAP, respectively, for adequate exposure of the acetabular rim. According to the evaluation of labrum tears, suture anchors are placed at a distance of 3 mm from the articular surface, from 3 o'clock of the medial to lateral through the DALA portal based on the location and range of the labral tear. The suture anchors are placed at 3, 2, 1, and 12 o'clock positions of the acetabulum. PMAP was established following with fixation of anchors. Double-loaded suture anchors are applied in this technique, one suture of the anchor is retrieved from the PMAP and temporarily fixed for further use, and the other suture is used for labrum repair with the luggage-tag suture technique. Following with femoroplasty, the viewing portal is switched from PMAP to AL, and the hip is flexed to 40°-60° for relaxation of the anterior joint capsule before suturing. A grasping forceps is used from the PMAP to hold the distal joint capsule, and a bird beak is used from the MAP to pierce the distal joint capsule, grab the suture wire, and pull the suture wires out from the MAP. Four suture anchors are typically used for suture-lifting, and eight sutures are passed through the distal joint capsule. The sutures from the same anchor are knotted in pairs to achieve suture-lifting and drag the distal joint capsule close to the acetabular rim to improve the anterior instability. The proximal joint capsule traction suture is pulled out through the distal joint capsule and knotted for closure of the joint capsule.
References
- 1.Chandrasekaran S., Vemula S.P., Martin T.J., Suarez-Ahedo C., Lodhia P., Domb B.G. Arthroscopic technique of capsular plication for the treatment of hip instability. Arthrosc Tech. 2015;4:e163–e167. doi: 10.1016/j.eats.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levy D.M., Grzybowski J., Salata M.J., Mather R.C., III, Aoki S.K., Nho S.J. Capsular plication for treatment of iatrogenic hip instability. Arthrosc Tech. 2015;4:e625–e630. doi: 10.1016/j.eats.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyin C., Maldonado D.R., Go C.C., Shapira J., Lall A.C., Domb B.G. Mid- to long-term outcomes of hip arthroscopy: A systematic review. Arthroscopy. 2021;37:1011–1025. doi: 10.1016/j.arthro.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Shapira J., Kyin C., Go C., et al. Indications and outcomes of secondary hip procedures after failed hip arthroscopy: A systematic review. Arthroscopy. 2020;36:1992–2007. doi: 10.1016/j.arthro.2020.02.028. [DOI] [PubMed] [Google Scholar]
- 5.Kowalczuk M., Bhandari M., Farrokhyar F., et al. Complications following hip arthroscopy: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1669–1675. doi: 10.1007/s00167-012-2184-2. [DOI] [PubMed] [Google Scholar]
- 6.Mortensen A.J., Tomasevich K.M., Ohlsen S.M., O'Neill D.C., Featherall J., Aoki S.K. Previous arthroscopic hip surgery increases axial distractibility compared to the native contralateral hip and may suggest instability. Arthroscopy. 2022;38:1466–1477. doi: 10.1016/j.arthro.2021.09.021. [DOI] [PubMed] [Google Scholar]
- 7.Mei-Dan O., McConkey M.O., Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: Can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. doi: 10.1016/j.arthro.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Featherall J., O'Neill D.C., Mortensen A.J., Tomasevich K.M., Metz A.K., Aoki S.K. Three-dimensional magnetic resonance arthrography of post-arthroscopy hip instability demonstrates increased effective intracapsular volume and anterosuperior capsular changes. Arthrosc Sports Med Rehabil. 2021;3:e1999–e2006. doi: 10.1016/j.asmr.2021.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Safran M.R., Murray I.R., Andrade A.J., et al. Criteria for the operating room confirmation of the diagnosis of hip instability: The results of an international expert consensus conference. Arthroscopy. 2022;38:2837–2849.e2. doi: 10.1016/j.arthro.2022.03.027. [DOI] [PubMed] [Google Scholar]
- 10.Parvaresh K.C., Rasio J., Azua E., Nho S.J. Hip instability in the athlete: Anatomy, etiology, and management. Clin Sports Med. 2021;40:289–300. doi: 10.1016/j.csm.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Beckert M., Meneghini R.M., Meding J.B. Instability after primary total hip arthroplasty: Dual mobility versus jumbo femoral heads. J Arthroplasty. 2022;37:S571–S576. doi: 10.1016/j.arth.2022.02.113. [DOI] [PubMed] [Google Scholar]
- 12.Heckmann N.D., Yang J., Ong K.L., et al. Revision surgery for instability after total hip arthroplasty: Does timing matter? J Arthroplasty. 2021;36:1779–1783.e2. doi: 10.1016/j.arth.2020.12.035. [DOI] [PubMed] [Google Scholar]
- 13.Mei-Dan O., Garabekyan T., McConkey M., Pascual-Garrido C. Arthroscopic anterior capsular reconstruction of the hip for recurrent instability. Arthrosc Tech. 2015;4:e711–e715. doi: 10.1016/j.eats.2015.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larson C.M. Editorial Commentary: Psoas tenotomy in the setting of a borderline dysplastic hip risks iatrogenic instability: Be extremely cautious and particularly in athletes. Arthroscopy. 2021;37:2485–2487. doi: 10.1016/j.arthro.2021.04.025. [DOI] [PubMed] [Google Scholar]
- 15.Wylie J.D., Beckmann J.T., Maak T.G., Aoki S.K. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44:39–45. doi: 10.1177/0363546515608162. [DOI] [PubMed] [Google Scholar]
- 16.Alrabaa R.G., Kannan A., Zhang A.L. Capsule closure of periportal capsulotomy for hip arthroscopy. Arthrosc Tech. 2022;11:e1117–e1122. doi: 10.1016/j.eats.2022.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turner E.H.G., Markhardt B.K., Cotter E.J., et al. Patients with generalized joint hypermobility have thinner superior hip capsules and greater hip internal rotation on physical examination. Arthrosc Sports Med Rehabil. 2022;4:e1417–e1427. doi: 10.1016/j.asmr.2022.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tian K., Gao G., Dong H., Zhang W., Wang J., Xu Y. Arthroscopic synovectomy of the hip joint: The regional surgical technique. Arthrosc Tech. 2022;11:e1181–e1187. doi: 10.1016/j.eats.2022.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hatem M.A., Helal A., Khoury A.N., Martin H.D. Anteroinferior hip instability in flexion during dynamic arthroscopic examination is associated with abnormal anterior acetabular horn. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120965564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clohisy J.C., Nepple J.J., Larson C.M., Zaltz I., Millis M. Academic Network of Conservation Hip Outcome Research (ANCHOR) Members. Persistent structural disease is the most common cause of repeat hip preservation surgery. Clin Orthop Relat Res. 2013;471:3788–3794. doi: 10.1007/s11999-013-3218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Canham C.D., Yen Y.M., Giordano B.D. Does femoroacetabular impingement cause hip instability? A systematic review. Arthroscopy. 2016;32:203–208. doi: 10.1016/j.arthro.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Featherall J., Tomasevich K.M., O'Neill D.C., Mortensen A.J., Aoki S.K. Arthroscopic hip capsule reconstruction for anterior hip capsule insufficiency in the revision setting. Arthrosc Tech. 2021;10:e1339–e1344. doi: 10.1016/j.eats.2021.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ankem H.K., Diulus S.C., Meghpara M.B., et al. Arthroscopic triple reconstruction in the hip joint: Restoration of soft-tissue stabilizers in revision surgery for gross instability. Arthrosc Tech. 2021;10:e1239–e1248. doi: 10.1016/j.eats.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nguyen K.H., Shaw C., Link T.M., et al. Changes in hip capsule morphology after arthroscopic treatment for femoroacetabular impingement syndrome with periportal capsulotomy are correlated with improvements in patient-reported outcomes. Arthroscopy. 2022;38:394–403. doi: 10.1016/j.arthro.2021.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Odri G.A., Sanchez J., Sverzut J.M., Laredo J.D., Sedel L., Bizot P. Does load-bearing materials influence hip capsule thickness in total hip replacement? An MRI case-matched study. Orthop Traumatol Surg Res. 2021;107 doi: 10.1016/j.otsr.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 26.Jansson H.L., Bradley K.E., Zhang A.L. A systematic approach to arthroscopic femoroplasty with conservative management of the hip capsule. Arthrosc Tech. 2021;10:e797–e806. doi: 10.1016/j.eats.2020.10.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Main surgical procedures of suture-lifting technique. Capsular suturing techniques that provide anterior stabilization will be of great help for these high-risk patients and reduce the possibility of postoperative anterior instability. In this technical note, we introduce the arthroscopic capsular suture-lifting technique for treating femoroacetabular impingement (FAI) patients with a high risk of postoperative hip instability. Video 1 shows the main surgical procedures of the suture-lifting technique: the patient is positioned supine and four portals --anterolateral (AL), mid-anterior portal (MAP), distal AL accessory portal (DALA), and proximal mid-anterior portal (PMAP) --are established in succession during surgery. Using the AL portal and MAP, the joint capsule is cut transversely from the 10 o'clock to 3 o'clock positions for labrum exposure. The DALA portal is established for rim preparation and anchor placement. Two capsular traction wires are passed through the AL portal and MAP, respectively, for adequate exposure of the acetabular rim. According to the evaluation of labrum tears, suture anchors are placed at a distance of 3 mm from the articular surface, from 3 o'clock of the medial to lateral through the DALA portal based on the location and range of the labral tear. The suture anchors are placed at 3, 2, 1, and 12 o'clock positions of the acetabulum. PMAP was established following with fixation of anchors. Double-loaded suture anchors are applied in this technique, one suture of the anchor is retrieved from the PMAP and temporarily fixed for further use, and the other suture is used for labrum repair with the luggage-tag suture technique. Following with femoroplasty, the viewing portal is switched from PMAP to AL, and the hip is flexed to 40°-60° for relaxation of the anterior joint capsule before suturing. A grasping forceps is used from the PMAP to hold the distal joint capsule, and a bird beak is used from the MAP to pierce the distal joint capsule, grab the suture wire, and pull the suture wires out from the MAP. Four suture anchors are typically used for suture-lifting, and eight sutures are passed through the distal joint capsule. The sutures from the same anchor are knotted in pairs to achieve suture-lifting and drag the distal joint capsule close to the acetabular rim to improve the anterior instability. The proximal joint capsule traction suture is pulled out through the distal joint capsule and knotted for closure of the joint capsule.