Key Points
Question
Is women’s lifetime exposure to intimate partner violence (IPV) associated with poor health outcomes?
Findings
This population-based cross-sectional study found that women’s exposure to any lifetime IPV, as well as specific IPV types (physical, sexual, psychological, controlling behaviors, and economic abuse), was associated with increased likelihood of reporting adverse health outcomes. Furthermore, a cumulative pattern was observed for exposure to multiple IPV types and poor health outcomes.
Meaning
These findings suggest that women’s IPV exposure contributes to population-level burden of disease, reinforcing calls for prevention and necessitating health care systems to be informed and mobilized to address IPV as a priority health issue.
This cross-sectional study assesses the association between lifetime intimate partner violence exposure and self-reported health using data from a representative population-based New Zealand survey.
Abstract
Importance
Intimate partner violence (IPV) is increasingly recognized as a contributing factor for long-term health problems; however, few studies have assessed these health outcomes using consistent and comprehensive IPV measures or representative population-based samples.
Objective
To examine associations between women’s lifetime IPV exposure and self-reported health outcomes.
Design, Setting, and Participants
The cross-sectional, retrospective 2019 New Zealand Family Violence Study, adapted from the World Health Organization’s Multi-Country Study on Violence Against Women, assessed data from 1431 ever-partnered women (63.7% of eligible women contacted) in New Zealand. The survey was conducted from March 2017 to March 2019, across 3 regions, which accounted for approximately 40% of the New Zealand population. Data analysis was performed from March to June 2022.
Exposures
Exposures were lifetime IPV by types (physical [severe/any], sexual, psychological, controlling behaviors, and economic abuse), any IPV (at least 1 type), and number of IPV types.
Main Outcomes and Measures
Outcome measures were poor general health, recent pain or discomfort, recent pain medication use, frequent pain medication use, recent health care consultation, any diagnosed physical health condition, and any diagnosed mental health condition. Weighted proportions were used to describe the prevalence of IPV by sociodemographic characteristics; bivariate and multivariable logistic regressions were used for the odds of experiencing health outcomes by IPV exposure.
Results
The sample comprised 1431 ever-partnered women (mean [SD] age, 52.2 [17.1] years). The sample was closely comparable with New Zealand’s ethnic and area deprivation composition, although younger women were slightly underrepresented. More than half of the women (54.7%) reported any lifetime IPV exposure, of whom 58.8% experienced 2 or more IPV types. Compared with all other sociodemographic subgroups, women who reported food insecurity had the highest IPV prevalence for any IPV (69.9%) and all specific types. Exposure to any IPV and specific IPV types was significantly associated with increased likelihood of reporting adverse health outcomes. Compared with those unexposed to IPV, women who experienced any IPV were more likely to report poor general health (adjusted odds ratio [AOR], 2.02; 95% CI, 1.46-2.78), recent pain or discomfort (AOR, 1.81; 95% CI, 1.34-2.46), recent health care consultation (AOR, 1.29; 95% CI, 1.01-1.65), any diagnosed physical health condition (AOR, 1.49; 95% CI, 1.13-1.96), and any mental health condition (AOR, 2.78; 95% CI, 2.05-3.77). Findings suggested a cumulative or dose-response association because women who experienced multiple IPV types were more likely to report poorer health outcomes.
Conclusions and Relevance
In this cross-sectional study of women in New Zealand, IPV exposure was prevalent and associated with an increased likelihood of experiencing adverse health. Health care systems need to be mobilized to address IPV as a priority health issue.
Introduction
Intimate partner violence (IPV) is an important public health and social issue and is internationally the most widespread form of violence against women.1,2 Global estimates indicate that 15% to 71% of all women experience physical and/or sexual IPV in their lifetime and 4% to 54% experience physical and/or sexual IPV within the preceding year.3 Research has increasingly linked IPV to a wide range of health issues.4,5
Despite the significant prevalence of IPV, there are a number of important gaps in the current evidence base regarding its effects on women. Although most research has focused on gathering data related to physical and/or sexual IPV,2 other types of IPV (eg, psychological abuse and controlling behaviors) have been underexplored.6 This lack of data is problematic because evidence suggests that these behaviors are a pervasive feature of abusive relationships.7,8 Economic abuse is also increasingly considered a key type of IPV.9 Of importance, most women do not experience one type of IPV in isolation, and multiple types often overlap.10,11
Although physical consequences of IPV are commonly understood as immediate impacts (such as injuries or homicide), there is increasing recognition that IPV is an important factor in a range of long-term health problems.4,5,12,13 However, methodological factors raise questions about the comparability and representativeness of existing findings. For example, many studies4,5 have recruited participants from IPV support or health care services rather than population-based samples. Many studies4,5 have inconsistently or incompletely measured IPV exposure, often excluding psychological IPV, not specifying or conflating IPV types in analyses, or collecting data on IPV exposure using nonvalidated tools. This study seeks to address these limitations by assessing the association between lifetime IPV exposure (disaggregated by severity, type, and cumulative exposure) and self-reported health using data from a representative population-based New Zealand (NZ) survey.
Methods
Methods for the 2019 New Zealand Family Violence Study/He Koiora Matapopore (NZFVS) have been described elsewhere but are presented briefly here.14 The NZFVS was a population-based, retrospective, cross-sectional survey based on the World Health Organization (WHO) Multi-Country Study on Violence Against Women (MCS).14 The WHO MCS’s 12-domain questionnaire was adapted to the NZ setting following consultation with government and expert advisers.14 The survey was conducted from March 2017 to March 2019, across 3 regions, which accounted for approximately 40% of the NZ population and covered a range of ethnicities and urbanicity. Ethics approval was granted by the University of Auckland Human Participants Ethics Committee.14 All participants gave written informed consent before the interview. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.15
Study Sample
Random sampling was conducted by selection of second and sixth houses from random starting points within primary sampling units.14,16 Nonresidential and short-term residential properties, rest homes, and retirement villages were excluded. To keep survey content discrete, only 1 randomly selected person per household was eligible to participate.14 Interviewers made up to 7 visits to each selected household to maximize recruitment.14 Participants had to be 16 years or older, able to speak conversational English, and residing in the house for more than 1 month.
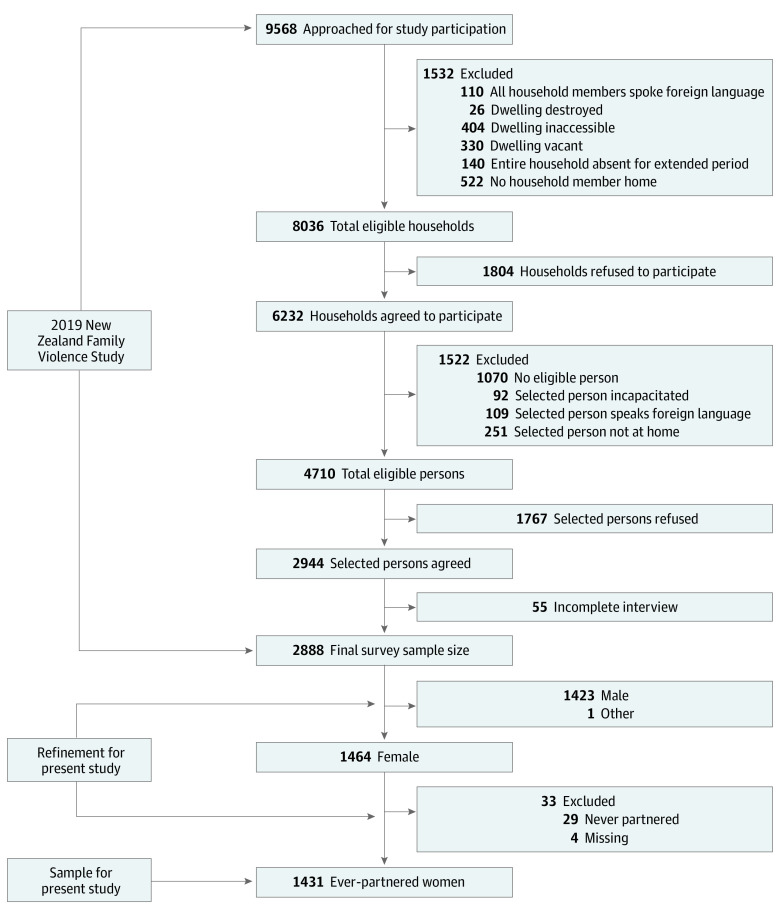
The NZFVS included data from a total of 2887 participants, including men. Complete interviews took place with 1464 women, for a response rate of 63.7% of eligible women contacted (Figure).14 The ethnic and area deprivation composition of the sample was closely representative of the NZ population, although Asian respondents and younger age groups were slightly underrepresented.14,17,18 For the current study, the data set was restricted to ever-partnered women (n = 1431), irrespective of sexual orientation. Findings for men are reported elsewhere.19
Figure. Flowchart of New Zealand Family Violence Study Recruitment and Refinement of the Study Sample.
Measures
Seven self-reported health outcomes were assessed: poor general health, recent pain or discomfort, recent use of pain medication, frequent use of pain medication, recent health care consultation, any diagnosed physical health condition (heart disease, cancer, stroke, diabetes, asthma, arthritis, or other), and any diagnosed mental health condition (depression, anxiety, substance abuse disorder, or other), for which responses were dichotomized (eTable in Supplement 1). Participants’ exposure to IPV was assessed using questions pertaining to lifetime experience of violent behaviors inflicted by a current or previous partner (eTable in Supplement 1). Dichotomous variables (ever or never) were created for lifetime exposure (at least 1 act) to each of 5 IPV types (physical, sexual, psychological, controlling behaviors, and economic abuse). Physical IPV behaviors were disaggregated into moderate (eg, slapping or pushing) or severe (eg, kicking or choking) according to WHO classifications, which are based on the likelihood of causing injury.20 Severe physical IPV was defined as experiencing at least 1 of the severe physical IPV behaviors regardless of whether moderate behaviors were present. Any lifetime IPV was defined by participants reporting exposure to at least 1 IPV type. A count variable was produced for the number of IPV types (at least 1 act per type) ever experienced (no IPV or 1, 2, 3, 4, or 5 types). Sociodemographic characteristics (age, ethnicity, food security, employment status, and educational level) were used to examine the prevalence of IPV and health outcomes among population subgroups and to adjust for potential confounding in multivariable analyses (eTable in Supplement 1).
Statistical Analysis
Survey weighting functions were used to account for sampling methods by weighting data by the number of eligible participants in each household. Missingness issues were minor, with less than 1% missing for all exposure and outcome variables except for economic IPV (13.2%), which was based on “don’t know,” “refused,” or “not applicable” responses. Data were analyzed using Stata version 16 (StataCorp).21
Weighted proportions described the prevalence of IPV types, including by sociodemographic characteristics and exposure to multiple IPV types. Bivariate and multivariable logistic regressions were used to calculate the odds of experiencing health outcomes for those exposed to different IPV types (compared with those who did not report experience of each type), any IPV, and multiple IPV types. Age and prioritized ethnicity (Māori [indigenous peoples of NZ]; Pacific peoples; Asian; Middle Eastern, Latin American, or African; and NZ European) were included in multivariable analyses to account for differences in health status across groups.22 Covariates for measures of socioeconomic status (food security, employment status, and education) improved model fit and were therefore included in multivariable analyses. Results are reported with 95% CIs and statistical significance set at a 2-sided P < .05.
Results
The sample comprised 1431 ever-partnered women (mean [SD] age, 52.2 [17.1] years [range, 16-96 years]; 11.6% Asian; 65.1% European; 14.4% Māori; 1.4% Middle Eastern, Latin American, or African; and 7.4% Pacific). Respondents predominantly identified as heterosexual (96.7%; 95% CI, 95.3%-97.6%). Sociodemographic characteristics of the sample are presented in Table 1.
Table 1. Sociodemographic Characteristics and Prevalence of Lifetime IPV Exposure for 1431 Women in the 2019 New Zealand Family Violence Study.
| Characteristic | Total No. (weighted%) | Participants, No. (weighted %) | ||||||
|---|---|---|---|---|---|---|---|---|
| Physical | Sexual | Psychological | Controlling | Economic | Any IPV | |||
| Severea | Any | |||||||
| Total | 1431 (100) | 239 (16.0) | 407 (28.0) | 191 (12.4) | 696 (47.7) | 309 (21.6) | 210 (16.2) | 794 (54.7) |
| Age group, y | ||||||||
| 16-29 | 156 (14.7) | 21 (11.4) | 40 (24.0) | 17 (8.7) | 79 (46.5) | 42 (24.0) | 13 (9.6) | 91 (53.9) |
| 30-49 | 474 (33.8) | 73 (15.1) | 141 (28.5) | 66 (13.1) | 257 (50.4) | 115 (22.8) | 77 (16.6) | 288 (57.1) |
| 50-69 | 547 (36.7) | 112 (19.7) | 173 (31.8) | 78 (13.7) | 269 (50.0) | 113 (21.9) | 88 (17.8) | 306 (57.1) |
| ≥70 | 252 (14.8) | 31 (12.6) | 51 (21.2) | 28 (10.8) | 89 (36.4) | 38 (15.1) | 31 (17.3) | 107 (43.0) |
| Ethnicity | ||||||||
| Asian | 152 (11.6) | 15 (8.0) | 28 (16.4) | 14 (7.0) | 50 (32.3) | 23 (12.4) | 21 (14.4) | 60 (38.3) |
| European | 1006 (65.1) | 146 (14.4) | 266 (26.7) | 129 (12.3) | 509 (51.6) | 199 (20.3) | 135 (15.6) | 566 (57.4) |
| Māori | 183 (14.4) | 62 (30.9) | 85 (46.0) | 39 (20.7) | 104 (54.8) | 62 (34.7) | 39 (22.6) | 123 (64.1) |
| MELAA | 22 (1.4) | 3 (12.5) | 7 (34.8) | 3 (13.0) | 11 (47.8) | 8 (34.8) | 4 (20.0) | 13 (60.9) |
| Pacific | 66 (7.4) | 13 (14.1) | 21 (22.8) | 6 (5.5) | 22 (24.4) | 17 (19.7) | 11 (11.7) | 32 (37.8) |
| Educational level | ||||||||
| Primary or secondary | 578 (40.9) | 110 (17.5) | 169 (28.9) | 85 (13.2) | 254 (43.5) | 126 (22.3) | 81 (15.4) | 295 (50.6) |
| Tertiary | 847 (59.1) | 128 (14.9) | 236 (27.4) | 104 (11.8) | 439 (50.6) | 180 (20.9) | 128 (16.8) | 496 (57.5) |
| Food security | ||||||||
| Secure | 1146 (79.5) | 151 (12.5) | 264 (22.7) | 121 (9.9) | 517 (44.5) | 208 (18.1) | 134 (12.7) | 590 (50.8) |
| Insecure | 279 (20.5) | 87 (29.5) | 141 (48.6) | 69 (22.2) | 177 (60.2) | 101 (35.2) | 76 (30.5) | 202 (69.9) |
| Employment | ||||||||
| Student | 61 (6.2) | 10 (10.3) | 15 (19.8) | 8 (8.5) | 30 (43.4) | 15 (19.8) | 6 (12.3) | 34 (49.1) |
| Not working | 90 (6.5) | 18 (19.6) | 31 (36.6) | 16 (16.1) | 51 (55.4) | 18 (21.4) | 19 (26.5) | 54 (60.7) |
| Housework | 146 (10.4) | 27 (17.9) | 43 (27.9) | 19 (12.9) | 61 (38.6) | 30 (19.6) | 31 (21.3) | 69 (44.1) |
| Retired | 355 (21.6) | 40 (11.8) | 68 (21.0) | 31 (8.2) | 120 (35.7) | 42 (13.1) | 36 (12.8) | 146 (43.3) |
| Employed | 778 (55.3) | 144 (17.5) | 250 (30.7) | 117 (14.0) | 434 (53.7) | 204 (25.5) | 118 (15.5) | 491 (60.9) |
Abbreviations: IPV, intimate partner violence; MELAA, Middle Eastern, Latin American, or African.
Severe physical IPV includes any exposure to a severe physical IPV behavior, irrespective of moderate behaviors. Any physical IPV includes any moderate or severe physical IPV.
Experience of lifetime IPV was highly prevalent among ever-partnered women; more than half (54.7%) reported experiencing at least 1 of the 5 types of IPV (Table 1). Among women exposed to any IPV, 58.8% were exposed to at least 2 IPV types, and 20.7% reported all 5 types. Physical IPV was experienced by 28.0% of women, sexual IPV by 12.4%, economic abuse by 16.2%, and psychological IPV by 47.7%.
By ethnicity, Māori women reported the highest prevalence of any lifetime IPV (64.1%); physical, psychological, and sexual IPV; and economic abuse (Table 1). Pacific and Asian women reported the lowest prevalence for all IPV types. Compared with all other sociodemographic subgroups, women who reported food insecurity had the highest prevalence for any IPV (69.9%) and all specific types.
Irrespective of IPV exposure, taking medication for pain or discomfort was the most common health outcome, reported by more than half (56.7%) of women in the sample (Table 2). Almost half (46.9%) had been diagnosed with a physical health condition and 21.9% with a mental health condition (Table 2). Health outcomes were more prevalent among older women (>50 years of age), Māori and Pacific women, women with only primary or secondary schooling, and women with food insecurity. For example, poor self-rated general health was reported by 36.7% of Pacific and 34.8% of Māori women (vs 26.1% of Middle Eastern, Latin American, or African women; 21.0% of Asian women; and 19.1% of NZ European women) and by 44.6% of those reporting food insecurity (vs 17.5% of those with food security).
Table 2. Association Between Women’s Exposure to IPV Types and Health Outcomesa.
| Poor general health | Recent pain or discomfort | Recent pain medication | Frequent pain medication | Recent health care consultation | Physical health condition | Mental health condition | |
|---|---|---|---|---|---|---|---|
| No. (weighted %) | 330 (23.0) | 443 (30.6) | 816 (56.7) | 247 (15.9) | 496 (33.2) | 685 (46.9) | 322 (21.9) |
| Physical | |||||||
| Moderate | |||||||
| OR (95% CI) | 1.57 (1.07-2.29)b | 1.25 (0.86-1.80) | 1.02 (0.72-1.45) | 1.20 (0.79-1.81) | 1.36 (0.94-1.95) | 0.97 (0.68-1.37) | 2.85 (1.97-4.14)b |
| aOR (95% CI)c | 1.38 (0.91-2.11) | 1.22 (0.83-1.80) | 0.94 (0.66-1.36) | 1.18 (0.76-1.83) | 1.31 (0.90-1.91) | 1.01 (0.70-1.46) | 2.50 (1.69-3.70)b |
| Severe | |||||||
| OR (95% CI) | 2.02 (1.50-2.71)b | 2.18 (1.59-2.99)b | 1.90 (1.37-2.63)b | 1.98 (1.40-2.79)b | 1.37 (1.01-1.85)b | 1.70 (1.24-2.32)b | 2.25 (1.63-3.11)b |
| aOR (95% CI)c | 1.54 (1.10-2.15)b | 2.05 (1.48-2.85)b | 1.82 (1.30-2.54)b | 1.67 (1.14-2.44)b | 1.28 (0.93-1.77) | 1.63 (1.15-2.31)b | 1.91 (1.34-2.72)b |
| Any | |||||||
| OR (95% CI) | 2.08 (1.60-2.70)b | 1.91 (1.45-2.51)b | 1.53 (1.18-1.99)b | 1.80 (1.31-2.46)b | 1.45 (1.13-1.87)b | 1.40 (1.07-1.84)b | 3.17 (2.39-4.22)b |
| aOR (95% CI)c | 1.65 (1.20-2.26)b | 1.85 (1.40-2.44)b | 1.44 (1.10-1.88)b | 1.60 (1.13-2.27)b | 1.38 (1.06-1.80)b | 1.40 (1.05-1.87)b | 2.78 (2.05-3.77)b |
| Sexual | |||||||
| OR (95% CI) | 1.74 (1.24-2.44)b | 1.88 (1.34-2.65)b | 1.64 (1.17-2.29)b | 1.78 (1.22-2.59)b | 1.52 (1.08-2.14)b | 1.30 (0.92-1.84) | 2.32 (1.58-3.40)b |
| aOR (95% CI)c | 1.43 (0.97-2.09) | 1.82 (1.29-2.56)b | 1.49 (1.06-2.10)b | 1.60 (1.07-2.40)b | 1.42 (1.00-2.02)b | 1.28 (0.88-1.85) | 2.03 (1.39-2.99)b |
| Psychological | |||||||
| OR (95% CI) | 1.68 (1.28-2.21)b | 1.81 (1.32-2.49)b | 1.43 (1.12-1.84)b | 1.23 (0.91-1.67) | 1.33 (1.04-1.70)b | 1.13 (0.87-1.48) | 3.17 (2.37-4.23)b |
| aOR (95% CI)c | 1.79 (1.32-2.43)b | 1.97 (1.47-2.63)b | 1.33 (1.03-1.71)b | 1.27 (0.92-1.76) | 1.28 (1.00-1.64) | 1.31 (0.99-1.73) | 2.59 (1.93-3.48)b |
| Controlling | |||||||
| OR (95% CI) | 1.75 (1.31-2.35)b | 1.77 (1.30-2.41)b | 1.47 (1.11-1.94)b | 1.56 (1.12-2.17)b | 1.28 (0.95-1.74) | 1.32 (0.99-1.76) | 2.24 (1.66-3.01)b |
| aOR (95% CI)c | 1.52 (1.09-2.12)b | 1.87 (1.34-2.59)b | 1.43 (1.07-1.92)b | 1.51 (1.04-2.18)b | 1.30 (0.94-1.80) | 1.48 (1.08-2.04)b | 1.96 (1.42-2.70)b |
| Economic | |||||||
| OR (95% CI) | 1.69 (1.22-2.35)b | 1.65 (1.16-2.36)b | 1.31 (0.95-1.81) | 1.65 (1.12-2.42)b | 1.47 (1.07-2.03)b | 1.57 (1.13-2.20)b | 2.92 (2.07-4.11)b |
| aOR (95% CI)c | 1.32 (0.90-1.94) | 1.60 (1.13-2.26)b | 1.25 (0.91-1.72) | 1.36 (0.90-2.07) | 1.33 (0.95-1.88) | 1.54 (1.08-2.21)b | 2.93 (2.05-4.18)b |
| Any IPV | |||||||
| OR (95% CI) | 1.99 (1.49-2.64)b | 1.72 (1.23-2.41)b | 1.35 (1.05-1.74)b | 1.35 (0.99-1.84) | 1.33 (1.04-1.70)b | 1.27 (0.96-1.68) | 3.39 (2.49-4.60)b |
| aOR (95% CI)c | 2.02 (1.46-2.78)b | 1.81 (1.34-2.46)b | 1.24 (0.96-1.59) | 1.37 (0.99-1.89) | 1.29 (1.01-1.65)b | 1.49 (1.13-1.96)b | 2.78 (2.05-3.77)b |
Abbreviations: aOR, adjusted odds ratio; IPV, intimate partner violence; OR, odds ratio.
Reference category for each IPV type was no exposure to this type.
Statistically significant.
Adjusted for age, ethnicity, food security, employment status, and educational level.
After adjustment for sociodemographic factors, women’s exposure to moderate physical IPV was significantly associated with having a mental health condition (Table 2). Exposure to severe physical IPV was significantly associated with all assessed health outcomes, aside from recently consulting health care.
At the multivariable level, all 5 IPV types were associated with reporting any mental health diagnosis (Table 2). Recent pain or discomfort was associated with all IPV types (Table 2). Different types of IPV were associated with health outcomes to varying degrees. Women exposed to any physical IPV were significantly more likely to experience all assessed health outcomes (adjusted odds ratios [AORs] ranged from 1.38 [95% CI, 1.06-1.80] for recently consulting health care to 2.78 [95% CI, 2.05-3.77] for having a diagnosed mental health condition) (Table 2). Women exposed to sexual IPV had increased odds of experiencing 5 health outcomes, of which 3 were pain related: recent pain or discomfort (AOR, 1.82; 95% CI, 1.29-2.56), recent use of pain medication (AOR, 1.49; 95% CI, 1.06-2.10), and frequent use of pain medication (AOR, 1.6; 95% CI, 1.07-2.40). Experience of any lifetime IPV was associated with 5 of the 7 assessed health outcomes (poor general health, recent pain or discomfort, recent health care consultation, and diagnosed physical or mental health conditions) (Table 2).
Women who experienced psychological IPV were significantly more likely to report 4 of the 7 health outcomes, including a 2-fold increased likelihood of reporting recent experience of pain or discomfort (AOR, 1.97; 95% CI, 1.47-2.63). Women exposed to controlling behaviors were significantly more likely to experience 6 of the explored health outcomes, including recent use of pain medication (AOR, 1.43; 95% CI, 1.07-1.92) and any mental health condition (AOR, 1.96; 95% CI, 1.42-2.70) (Table 2). Women who experienced economic abuse were significantly more likely to report 3 of the 7 assessed health outcomes, including experiencing recent pain or discomfort and reporting a diagnosed physical health condition, and had the greatest odds for a diagnosed mental health condition (AOR, 2.93; 95% CI, 2.05-4.18) of all 5 IPV types (Table 2).
A cumulative pattern was observed between number of IPV types experienced and associations with health outcomes. Women who experienced 1 IPV type had an increased likelihood of reporting poor general health, physical health condition, or mental health condition compared with women who had experienced no lifetime IPV (Table 3). Women exposed to 2 IPV types were significantly more likely to report 3 health outcomes, whereas those exposed to 3 types of IPV were significantly more likely to report 4 health outcomes. Women exposed to 4 or 5 IPV types had significantly increased odds of experiencing all 7 health outcomes, which persisted after adjustment for sociodemographic factors (Table 3). Experience of additional IPV types also increased the magnitude of the AORs. For example, AORs for experience of recent pain or discomfort ranged from 1.89 (95% CI, 1.22-2.92) for exposure to 2 IPV types to 2.24 (95% CI, 1.38-3.64) for exposure to 3 IPV types to 2.63 (95% CI, 1.71-4.04) for exposure to 4 or 5 IPV types. The overall trend suggests that a cumulative or dose-response association is present for exposure to multiple IPV types, although some other health outcomes did not present a consistent incremental increase and a few associations failed to reach statistical significance (Table 3).
Table 3. Association Between Number of IPV Types Experienced by Women and Health Outcomesa.
| Health outcome | 1 IPV type | 2 IPV types | 3 IPV types | 4 or 5 IPV types | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | aOR (95% CI)b | OR (95% CI) | aOR (95% CI)b | OR (95% CI) | aOR (95% CI)b | OR (95% CI) | aOR (95% CI)b | |
| Poor general health | 1.69 (1.15-2.48)c | 1.92 (1.28-2.87)c | 1.63 (1.08-2.46)c | 1.81 (1.15-2.86)c | 2.61 (1.66-4.12)c | 2.50 (1.49-4.20)c | 2.54 (1.69-3.81)c | 2.05 (1.28-3.29)c |
| Recent pain or discomfort | 1.24 (0.83-1.86) | 1.36 (0.93-2.00) | 1.85 (1.17-2.92)c | 1.89 (1.22-2.92)c | 2.08 (1.29-3.34)c | 2.24 (1.38-3.64)c | 2.48 (1.59-3.86)c | 2.63 (1.71-4.04)c |
| Recent pain medication | 1.11 (0.81-1.52) | 1.05 (0.76-1.43) | 1.17 (0.80-1.72) | 1.05 (0.71-1.55) | 1.94 (1.22-3.08)c | 1.83 (1.14-2.93)c | 1.74 (1.18-2.59)c | 1.59 (1.07-2.37)c |
| Frequent pain medication | 1.03 (0.67-1.58) | 1.15 (0.74-1.78) | 1.17 (0.71-1.93) | 1.15 (0.67-1.95) | 1.53 (0.96-2.45) | 1.62 (0.99-2.63) | 2.13 (1.37-3.32)c | 1.92 (1.17-3.16)c |
| Recent health care consultation | 1.21 (0.89-1.65) | 1.23 (0.91-1.66) | 1.26 (0.85-1.89) | 1.19 (0.80-1.77) | 1.01 (0.65-1.56) | 1.02 (0.66-1.58) | 2.04 (1.40-2.98)c | 1.92 (1.27-2.92)c |
| Any physical health condition | 1.24 (0.89-1.72) | 1.56 (1.10-2.20)c | 1.02 (0.70-1.47) | 1.03 (0.71-1.50) | 1.11 (0.71-1.72) | 1.38 (0.84-2.27) | 1.90 (1.26-2.86)c | 2.18 (1.42-3.36)c |
| Any mental health condition | 2.22 (1.53-3.23)c | 1.87 (1.28-2.72)c | 4.17 (2.78-6.26)c | 3.56 (2.38-5.32)c | 3.94 (2.43-6.38)c | 3.16 (1.92-5.22)c | 5.00 (3.28-7.64)c | 4.22 (2.74-6.50)c |
Abbreviations: aOR, adjusted odds ratio; IPV, intimate partner violence; OR, odds ratio.
The reference category was no IPV.
Adjusted for age, ethnicity, food security, employment status, and educational level.
Statistically significant.
Discussion
Overall, women’s exposure to any lifetime IPV was associated with an increased likelihood of reporting poor health outcomes. Specific IPV types had differential associations with health outcomes. Severe physical IPV was associated with increased likelihood of reporting most health outcomes; however, moderate physical IPV was not. Of note, experience of nonphysical IPV types (psychological, controlling behaviors, and economic abuse) was also associated with adverse health outcomes. A cumulative pattern was observed between the number of IPV types experienced and associations with health outcomes, with women who reported exposure to 4 or 5 IPV types having increased likelihood of reporting all health outcomes measured. This finding is relevant because experiences of multiple IPV types were prevalent, with more than half (58.8%) of women who reported any IPV having experienced at least 2 IPV types.
The IPV prevalence in this study is consistent with international findings despite variation in settings and IPV measures, including WHO’s aggregated prevalence estimates of 37.6% of women experiencing lifetime IPV.23 Globally, WHO reported that physical IPV is experienced by 29.2% (28.0% in this sample) of women, sexual IPV by 20.5% (12.4% in this sample), and economic abuse by 12.0% of women (16.2% in this sample).23 The higher prevalence of psychological IPV (47.7% in the present sample compared with 25.7% in WHO estimates) may be partially attributable to the single measure threshold (at least 1 act) for psychological IPV used in the current study.23
Findings from the current study strengthen indications from previous research that experience of any IPV among women is associated with a range of adverse health outcomes, including heightened risk of poor self-rated health,4,5,24,25 chronic pain (including headaches),5,13,26 and diagnoses for chronic physical health conditions (eg, gastrointestinal, cardiovascular, musculoskeletal, respiratory, liver, urinary and kidney diseases).4,27 A companion study19 from the NZFVS exploring men’s IPV exposure and health outcomes found that although men’s exposure to IPV (particularly severe physical IPV) was associated with increased likelihood for reporting some health outcomes, associations with poor health were inconsistent, and a cumulative pattern by exposure to multiple types of IPV was not observed.
Increased risk of adverse health outcomes for women exposed to physical and/or sexual IPV is well established4 and supported by present findings. Findings presented in this study also suggest that associations between any physical IPV and adverse health outcomes appear to be associated with severe rather than moderate physical IPV. The severity of IPV has been long posited as an important variable in worse health outcomes,11,28 although few studies have comparably assessed severe physical behaviors, including one from New Zealand.29 Many studies compared severe physical IPV to no IPV exposure30,31,32 or defined severity using combined types.26,33,34 This study extends previous findings by assessing and identifying health associations for a broader range of IPV types. The associations found here between psychological IPV and 4 explored health outcomes highlight that assessment of this IPV type should be consistently included in research on IPV and its health impacts and must be addressed in policy and practice initiatives.4
Women’s exposure to the other assessed nonphysical IPV types (economic abuse and controlling behaviors) was also associated with a range of adverse health outcomes. Supporting findings from another study35 we found that controlling behaviors were consistently associated with 6 of the health outcomes explored here, which highlights the need to directly measure controlling behaviors in IPV research.8 This is also important because controlling behaviors have been considered indicators for severe IPV and co-occurring psychological and physical IPV.7 Despite not receiving much direct attention in the literature to date, our findings confirm that economic abuse is an important area for future attention.36
Women’s experience of 4 or 5 IPV types was associated with increased likelihood of reporting all health outcomes measured in the current study, including a 2-fold increased likelihood of having a recent health care consultation and having a diagnosed physical health condition. Findings reinforce longstanding but undersubstantiated claims about the cumulative impact of exposure to different IPV types,11 which may potentially capture women’s IPV experiences more accurately. Few previous studies37,38 have explored associations by the number of IPV types experienced and, where incorporated, have measured or defined IPV inconsistently. A comparable study39 using the WHO MCS also found a cumulative effect of women’s IPV exposure on health outcomes.
In the current analysis, a near 3-fold increased likelihood was observed between any IPV exposure and reporting a diagnosis of any mental health condition, and women exposed to 4 or 5 types of IPV were more than 4 times more likely to report a diagnosed mental health condition. Exposure to IPV was substantially associated with increased likelihood of poor mental health outcomes, consistent with previous findings,26,40,41,42 including research that found that experiencing more than 1 type of IPV increased the odds of reporting symptoms and severity of depression, posttraumatic stress disorder (PTSD), and suicidal ideation.5
Although the association of IPV with mental health outcomes has been well explored in the literature, it has also been posited that mental health conditions (particularly depression and PTSD) may mediate the pathway to physical health.4,5,41,43 Causal pathways between IPV experience and poor physical health outcomes could not be explored in this cross-sectional study; this is an important avenue for future research. Other research has proposed pathways between trauma and physical health, which include psychological correlates (primarily depression and PTSD), biological functions, prolonged physiological stress activity, and health-risk behavioral factors.12,44
These findings call attention to the long-term implications of IPV for women’s physical and mental health and situates IPV in a similar position to other key determinants of health, such as smoking and obesity. To adequately address the increased likelihood of adverse health outcomes associated with women’s exposure to IPV, health professionals need to be engaged in nuanced understanding of IPV identification and appropriate responses and should be well supported to provide robust referral options within proactive and dynamic health care systems. Given the higher rates of violence exposure for Māori women and women who were food insecure, health and referral services also need to be equipped to address these disparities. Development of these responsive health care systems must be underpinned by well-designed and comprehensive IPV curricula in medical and health training, as suggested elsewhere.45,46,47
This study substantiated findings on associations between women’s IPV exposure and health outcomes using a purposefully designed analysis to address underexplored IPV types, stringent sampling and data collection methods, and a pretested and robust questionnaire based on the reputable WHO MCS. The representative and community-dwelling sample reflected the broader population, not only those seeking support from health care or IPV services. This approach addressed a limitation of previous studies,34,37,48 which may have been biased because of the use of convenience samples from health care settings. Although the presented associations do not imply causation, consistent and cumulative associations suggest that causal pathways may exist. Given the generalizability of the sample to NZ women and comparability with international IPV prevalence estimates, the findings can inform wider international understanding on the associations between IPV and health outcomes.
Limitations
This study has some limitations. Several sampling factors may have underestimated the prevalence of IPV, including exclusion of inaccessible housing, women who could not speak English, and residents of facilities such as prisons.14 Women recently exposed to IPV, such as those engaged with IPV service providers or currently in abusive and controlling relationships, might have been less likely to participate.1,14 Although NZFVS data collection was conducted in compliance with WHO’s recommendations for maximizing participant safety and disclosure,49 recall or social desirability biases may have compromised self-reported measures, including IPV exposure.28 The prevalence of health outcomes may have been underestimated by capturing a relatively healthy sample because women requiring care in rest homes and hospitals were excluded, and those who were unwell may have been less likely to participate. Furthermore, correlation does not equal causation; it is possible that those with poor health are more likely to experience IPV.
Use of single-measure thresholds (at least 1 act) for each IPV type may have captured sporadic occurrences rather than systematic patterns of violence or control. A lack of consensus currently exists as to when psychologically aggressive acts meet a threshold for definition as IPV.50,51 Further research should assess health impacts by IPV intensity and frequency. Analyses of the associations of specific IPV types with health are indicative, but independent effects could not be examined as the different types often co-occur. Furthermore, this study did not differentiate between those who currently or historically experienced IPV or the timing of IPV exposure in relation to experiencing poorer health consequences.
Conclusions
This cross-sectional study substantiated and extended previous findings on associations between women’s IPV exposure and health outcomes by assessing a range of IPV types, including underexplored IPV types and cumulative experience of IPV types. As found here, women who have experienced IPV had higher rates of health issues and presented to health services more often than women unexposed to IPV.
This research presents a strong case for addressing IPV and its health consequences for women, both in NZ and internationally. Women’s IPV exposure contributes to population-level burden of disease, necessitating health care systems to be mobilized to address IPV as a priority health issue. Furthermore, IPV prevention efforts are essential to mitigate and eliminate the personal, social, and community burden of IPV.
eTable. Variable Questions and Definitions From the 2019 New Zealand Family Violence Survey Used in Analysis
Data Sharing Statement
References
- 1.World Health Organization . Violence Against Women Prevalence Estimates, 2018: Global, Regional and National Prevalence Estimates for Intimate Partner Violence Against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence Against Women. World Health Organization; 2021. Accessed February 1, 2022. https://apps.who.int/iris/handle/10665/341337
- 2.Devries KM, Mak JYT, García-Moreno C, et al. Global health: the global prevalence of intimate partner violence against women. Science. 2013;340(6140):1527-1528. doi: 10.1126/science.1240937 [DOI] [PubMed] [Google Scholar]
- 3.García-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH; WHO Multi-country Study on Women’s Health and Domestic Violence against Women Study Team . Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368(9543):1260-1269. doi: 10.1016/S0140-6736(06)69523-8 [DOI] [PubMed] [Google Scholar]
- 4.Stubbs A, Szoeke C. The effect of intimate partner violence on the physical health and health-related behaviors of women: a systematic review of the literature. Trauma Violence Abuse. 2022;23(4):1157-1172. doi: 10.1177/1524838020985541 [DOI] [PubMed] [Google Scholar]
- 5.Dillon G, Hussain R, Loxton D, Rahman S. Mental and physical health and intimate partner violence against women: a review of the literature. Int J Family Med. 2013;2013:313909. doi: 10.1155/2013/313909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fanslow J, Malihi Z, Hashemi L, Gulliver P, McIntosh T. Change in prevalence of psychological and economic abuse, and controlling behaviours against women by an intimate partner in two cross-sectional studies in New Zealand, 2003 and 2019. BMJ Open. 2021;11(3):e044910. doi: 10.1136/bmjopen-2020-044910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aizpurua E, Copp J, Ricarte JJ, Vázquez D. Controlling behaviors and intimate partner violence among women in Spain: an examination of individual, partner, and relationship risk factors for physical and psychological abuse. J Interpers Violence. 2021;36(1-2):231-254. doi: 10.1177/0886260517723744 [DOI] [PubMed] [Google Scholar]
- 8.Myhill A. Measuring coercive control: what can we learn from national population surveys? Violence Against Women. 2015;21(3):355-375. doi: 10.1177/1077801214568032 [DOI] [PubMed] [Google Scholar]
- 9.Haifley CK. Economic abuse: a literature review of a salient yet overlooked form of intimate partner violence. Theory Action. 2021;14(2):82-91. doi: 10.3798/tia.1937-0237.2114 [DOI] [Google Scholar]
- 10.Dutton MA, Kaltman S, Goodman LA, Weinfurt K, Vankos N. Patterns of intimate partner violence: correlates and outcomes. Violence Vict. 2005;20(5):483-497. doi: 10.1891/vivi.2005.20.5.483 [DOI] [PubMed] [Google Scholar]
- 11.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano RE, eds. World Report on Violence and Health. World Health Organization; 2002.
- 12.Black MC. Intimate partner violence and adverse health consequences: implications for clinicians. Am J Lifestyle Med. 2011;5(5):428-439. doi: 10.1177/1559827611410265 [DOI] [Google Scholar]
- 13.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331-1336. doi: 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- 14.Fanslow J, Gulliver P, Hashemi L, Malihi Z, McIntosh T. Methods for the 2019 New Zealand Family Violence Study- a study on the association between violence exposure, health and well-being. Kotuitui. 2021;16(1):196-209. doi: 10.1080/1177083X.2020.1862252 [DOI] [Google Scholar]
- 15.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800-804. doi: 10.1097/EDE.0b013e3181577654 [DOI] [PubMed] [Google Scholar]
- 16.Hashemi L, Fanslow J, Gulliver P, McIntosh T. Exploring the health burden of cumulative and specific adverse childhood experiences in New Zealand: Results from a population-based study. Child Abuse Negl. 2021;122:105372. doi: 10.1016/j.chiabu.2021.105372 [DOI] [PubMed] [Google Scholar]
- 17.Stats NZ. Age and sex by ethnic group (grouped total responses), for census night population counts, 2006, 2013, and 2018 Censuses. Accessed August 25, 2021. https://nzdotstat.stats.govt.nz/wbos/Index.aspx?DataSetCode=TABLECODE8317#
- 18.Exeter DJ, Zhao J, Crengle S, Lee A, Browne M. The New Zealand Indices of Multiple Deprivation (IMD): a new suite of indicators for social and health research in Aotearoa, New Zealand. PLoS One. 2017;12(8):e0181260. doi: 10.1371/journal.pone.0181260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mellar BM, Gulliver PJ, Selak V, Hashemi L, McIntosh TKD, Fanslow JL. Association between men’s exposure to intimate partner violence and self-reported health outcomes in New Zealand. JAMA Netw Open. 2023;6(1):e2252578. doi: 10.1001/jamanetworkopen.2022.52578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.García-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts C. World Health Organization Multi-Country Study on Women’s Health and Domestic Violence Against Women. World Health Organization; 2005. Accessed February 2, 2022. https://apps.who.int/iris/handle/10665/43309
- 21.StataCorp. Stata Statistical Software [software program]. Release 16. StataCorp LLC; 2019. [Google Scholar]
- 22.Ministry of Health . HISO 10001: 2017. ethnicity data protocols. Accessed May 28, 2022. https://www.health.govt.nz/publication/hiso-100012017-ethnicity-data-protocols
- 23.World Health Organization . Intimate partner violence. Violence Info. Accessed October 21, 2021. https://apps.who.int/violence-info/intimate-partner-violence
- 24.Brown SJ, Conway LJ, FitzPatrick KM, et al. Physical and mental health of women exposed to intimate partner violence in the 10 years after having their first child: an Australian prospective cohort study of first-time mothers. BMJ Open. 2020;10(12):e040891. doi: 10.1136/bmjopen-2020-040891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coker AL, Bush HM, Brancato CJ, Sprang G. Can the impact of interpersonal violence on current health-related quality of life be mitigated? J Womens Health (Larchmt). 2019;28(10):1355-1367. doi: 10.1089/jwh.2018.7017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23(4):260-268. doi: 10.1016/S0749-3797(02)00514-7 [DOI] [PubMed] [Google Scholar]
- 27.Liu X, Logan J, Alhusen J. Cardiovascular risk and outcomes in women who have experienced intimate partner violence: an integrative review. J Cardiovasc Nurs. 2020;35(4):400-414. doi: 10.1097/JCN.0000000000000654 [DOI] [PubMed] [Google Scholar]
- 28.Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C; WHO Multi-country Study on Women’s Health and Domestic Violence against Women Study Team . Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet. 2008;371(9619):1165-1172. doi: 10.1016/S0140-6736(08)60522-X [DOI] [PubMed] [Google Scholar]
- 29.Fanslow J, Robinson E. Violence against women in New Zealand: prevalence and health consequences. N Z Med J. 2004;117(1206):U1173. [PubMed] [Google Scholar]
- 30.Lacey KK, Mouzon DM. Severe physical intimate partner violence and the mental and physical health of U.S. Caribbean Black women. J Womens Health (Larchmt). 2016;25(9):920-929. doi: 10.1089/jwh.2015.5293 [DOI] [PubMed] [Google Scholar]
- 31.Lacey KK, Sears KP, Matusko N, Jackson JS. Severe physical violence and Black women’s health and well-being. Am J Public Health. 2015;105(4):719-724. doi: 10.2105/AJPH.2014.301886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Basu A, Levendosky AA, Lonstein JS. Trauma sequelae and cortisol levels in women exposed to intimate partner violence. Psychodyn Psychiatry. 2013;41(2):247-275. doi: 10.1521/pdps.2013.41.2.247 [DOI] [PubMed] [Google Scholar]
- 33.Alhalal E, Falatah R. Intimate partner violence and hair cortisol concentration: A biomarker for HPA axis function. Psychoneuroendocrinology. 2020;122:104897. doi: 10.1016/j.psyneuen.2020.104897 [DOI] [PubMed] [Google Scholar]
- 34.Hegarty KL, O’Doherty LJ, Chondros P, et al. Effect of type and severity of intimate partner violence on women’s health and service use: findings from a primary care trial of women afraid of their partners. J Interpers Violence. 2013;28(2):273-294. doi: 10.1177/0886260512454722 [DOI] [PubMed] [Google Scholar]
- 35.Stöckl H, Penhale B. Intimate partner violence and its association with physical and mental health symptoms among older women in Germany. J Interpers Violence. 2015;30(17):3089-3111. doi: 10.1177/0886260514554427 [DOI] [PubMed] [Google Scholar]
- 36.Jury A, Thorburn N, Weatherall R. “What’s his is his and what’s mine is his”: financial power and the economic abuse of women in Aotearoa. Aotearoa NZ Soc Work. 2017;29(2):69-82. doi: 10.11157/anzswj-vol29iss2id312 [DOI] [Google Scholar]
- 37.Montero I, Martín-Baena D, Escribà-Agüir V, Ruiz-Pérez I, Vives-Cases C, Talavera M. Intimate partner violence in older women in Spain: prevalence, health consequences, and service utilization. J Women Aging. 2013;25(4):358-371. doi: 10.1080/08952841.2013.838854 [DOI] [PubMed] [Google Scholar]
- 38.Winter A, Stephenson R. Intimate partner violence and symptoms of reproductive tract infections among married Indian women. Int J Gynaecol Obstet. 2013;121(3):218-223. doi: 10.1016/j.ijgo.2012.12.018 [DOI] [PubMed] [Google Scholar]
- 39.Potter LC, Morris R, Hegarty K, García-Moreno C, Feder G. Categories and health impacts of intimate partner violence in the World Health Organization multi-country study on women’s health and domestic violence. Int J Epidemiol. 2021;50(2):652-662. doi: 10.1093/ije/dyaa220 [DOI] [PubMed] [Google Scholar]
- 40.Kendall-Tackett KA. Inflammation, cardiovascular disease, and metabolic syndrome as sequelae of violence against women: the role of depression, hostility, and sleep disturbance. Trauma Violence Abuse. 2007;8(2):117-126. doi: 10.1177/1524838007301161 [DOI] [PubMed] [Google Scholar]
- 41.Dutton MA, Green BL, Kaltman SI, Roesch DM, Zeffiro TA, Krause ED. Intimate partner violence, PTSD, and adverse health outcomes. J Interpers Violence. 2006;21(7):955-968. doi: 10.1177/0886260506289178 [DOI] [PubMed] [Google Scholar]
- 42.Dokkedahl SB, Kirubakaran R, Bech-Hansen D, Kristensen TR, Elklit A. The psychological subtype of intimate partner violence and its effect on mental health: a systematic review with meta-analyses. Syst Rev. 2022;11(1):163. doi: 10.1186/s13643-022-02025-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Scott-Storey K. Cumulative abuse: do things add up? An evaluation of the conceptualization, operationalization, and methodological approaches in the study of the phenomenon of cumulative abuse. Trauma Violence Abuse. 2011;12(3):135-150. doi: 10.1177/1524838011404253 [DOI] [PubMed] [Google Scholar]
- 44.Schnurr PP, Green BL. A context for understanding the physical health consequences of exposure to extreme stress. In: Schnurr PP, Green BL, eds. Trauma and Health: Physical Health Consequences of Exposure to Extreme Stress. American Psychological Association; 2004:3-10. doi: 10.1037/10723-001 [DOI] [Google Scholar]
- 45.Ambikile JS, Leshabari S, Ohnishi M. Curricular limitations and recommendations for training health care providers to respond to intimate partner violence: an integrative literature review. Trauma Violence Abuse. 2022;23(4):1262-1269. doi: 10.1177/1524838021995951 [DOI] [PubMed] [Google Scholar]
- 46.García-Moreno C, Hegarty K, d’Oliveira AFL, Koziol-McLain J, Colombini M, Feder G. The health-systems response to violence against women. Lancet. 2015;385(9977):1567-1579. doi: 10.1016/S0140-6736(14)61837-7 [DOI] [PubMed] [Google Scholar]
- 47.Clark OW, Glasson J, August AM, et al. Physicians and domestic violence: ethical considerations. JAMA. 1992;267(23):3190-3193. doi: 10.1001/jama.1992.03480230082033 [DOI] [PubMed] [Google Scholar]
- 48.Prosman G-J, Lo Fo Wong SH, Bulte E, Lagro-Janssen ALM. Healthcare utilization by abused women: a case control study. Eur J Gen Pract. 2012;18(2):107-113. doi: 10.3109/13814788.2012.675503 [DOI] [PubMed] [Google Scholar]
- 49.Ellsberg M, Heise L, Peña R, Agurto S, Winkvist A. Researching domestic violence against women: methodological and ethical considerations. Stud Fam Plann. 2001;32(1):1-16. doi: 10.1111/j.1728-4465.2001.00001.x [DOI] [PubMed] [Google Scholar]
- 50.Hayes BE, Kopp PM. Gender differences in the effect of past year victimization on self-reported physical and mental health: findings from the 2010 National Intimate Partner and Sexual Violence Survey. Am J Crim Justice. 2020;45(2):293-312. doi: 10.1007/s12103-019-09510-7 [DOI] [Google Scholar]
- 51.Heise L, Pallitto C, García-Moreno C, Clark CJ. Measuring psychological abuse by intimate partners: constructing a cross-cultural indicator for the Sustainable Development Goals. SSM Popul Health. 2019;9:100377. doi: 10.1016/j.ssmph.2019.100377 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Variable Questions and Definitions From the 2019 New Zealand Family Violence Survey Used in Analysis
Data Sharing Statement