Abstract
Objectives
Primary objective: to determine the point prevalence and incidence rate of severe myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in children aged 5–16 years over 13 months. Secondary objectives: to describe the demographic features, symptoms, impact on activities of daily living, school attendance and time to diagnosis.
Design
Prospective surveillance study conducted by the British Paediatric Surveillance Unit. Paediatricians was asked if they had assessed a child with severe ME/CFS (screening definition for prevalence and incidence: children (5–16 years) diagnosed with ME/CFS so severe that they are unable to attend school for more than 1 hour a week during the last 6 weeks of the school term).
Participants
Patients 5–16 years of age, seen by paediatricians and two large ME/CFS specialist services across the UK and Ireland.
Outcome measures
Paediatrician-completed questionnaires describing demographics, symptoms, function and treatment, (applying National Institute for Health and Care Excellence (NICE)-recommended criteria to assess severity of ME/CFS). Diagnosis of severe, probable severe or possible severe ME/CFS was made only with evidence of NICE-recommended screening blood tests.
Results
285 cases were reported, of which of which 33 were severe, 4 probable severe and 55 possible severe. Estimated prevalence was 3.2 per million children (95% CI 2.2 to 4.5). Including possible/probable severe ME/CFS gave 8.9 per million children (95% CI 7.2 to 11). The incidence rate was 0.90 per million children-years (95% CI 0.43 to 1.65) (1.97 per million children-years (95% CI 1.24 to 2.99)). Median age was 13 years and 58% of cases were female. Median time to diagnosis was 0.47 years.
Conclusions
Although the incidence of children presenting with severe ME/CFS is low, all were very disabled. In addition, the majority receive little or no education. Paediatricians need to consider how to provide rehabilitation and education for these disabled young people.
Keywords: chronic fatigue syndrome, child health, paediatrics
This national study investigated prevalence and incidence rates of severe ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome) in 5-16 year-olds, as well as describing key demographic and clinical characteristics.
What is already known on this topic
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a heterogeneous condition that ranges in severity; when moderate–severe, it can significantly impact on a child’s quality of life and school attendance.
Previous estimates of the prevalence of severe ME/CFS are poor, largely featuring patient-reported, community-based studies of unconfirmed ME/CFS.
Caring for these children and young people (CYP) is difficult, with National Institute for Health and Care Excellence guidelines recommending domiciliary assessments for those with confirmed severe ME/CFS.
What this study adds
Prevalence and incidence rates of 3.2 per million children and 0.90 per million children-years, respectively.
Shorter time from symptom onset to diagnosis, but otherwise similar demographics and symptoms to wider forms of ME/CFS.
Twenty of 33 (63%) CYP with severe ME/CFS were receiving no tuition in the 6 weeks preceding assessment.
How this study might affect research, practice or policy
Service provision for domiciliary assessment and treatment of patients with severe ME/CFS can be informed by this study’s incidence/prevalence figures.
The low take-up or availability of home schooling identified by this study should guide efforts to meeting this need by local authorities.
This study has suggested possible barriers to diagnosis for female and non-white patients with severe ME/CFS. Further research should focus on identifying these.
Introduction
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a heterogeneous condition. Symptoms include disabling fatigue, postexertional malaise, unrefreshing sleep, cognitive difficulties, pain and other symptoms.1 A diagnosis can be made in children and young people (CYP, defined here as children and adolescents between the ages of 5 and 16) after 3 months of symptoms, and a paediatrician must see the child to rule out other causes.2 While symptomatic fatigue is common in CYP, diagnosed ME/CFS is much less common with an estimated population prevalence of 0.89% among children/adolescent populations.3
ME/CFS can vary widely in severity and duration,4 but little is known about the epidemiology of CYP with severe ME/CFS.5 6 Severe ME/CFS is defined differently, depending on the country, population and methodology used. In the UK, the 2007 National Institute for Health and Care Excellence (NICE) guidance7 defined severe ME/CFS as fatigue so severe that people are unable to do any activity for themselves or can carry out minimal daily tasks only (such as face washing and cleaning teeth). They have severe cognitive difficulties and depend on a wheelchair for mobility. They are often unable to leave the house or have a severe and prolonged after-effect if they do so. The 2021 guidance defines it similarly though describes some overlap with moderate ME/CFS as CYP living with moderate ME/CFS ‘have usually stopped work or education’.2 There are few case studies and most prevalence estimates lack a clinical diagnosis. We need to understand how many CYP with ME/CFS are severe to determine service provision.2
This surveillance study aims to establish the prevalence and incidence of severe ME/CFS in the UK and Ireland in children 5–16 years of age. We will also report the clinical features (including function) of CYP with severe ME/CFS.
Methods
Study design
A prospective surveillance study covering the UK and Ireland was completed using the British Paediatric Surveillance Unit (BPSU)8 (www.rcpch.ac.uk/work-we-do/bpsu) for patients seen by paediatricians between February 2018 and February 2019. Consultant paediatricians throughout the UK and Ireland return notification cards in response to monthly emails highlighting selected conditions. They then receive study-specific questionnaires on the cases they have reported; this covers demographics, clinical manifestations, investigations and management of their patients (online supplemental appendix 1). Investigations included the NICE-recommended urinalysis and blood tests.7 Reminder emails and data collection via phone calls were sent/made as necessary to maximise follow-up. Duplicates were identified and removed using date of birth, NHS number and then gender, locality and reporting paediatrician. Using this approach, BPSU has enjoyed a consistently high response rate from all registered paediatricians in the UK (over 90%).
archdischild-2022-324319supp001.pdf (3MB, pdf)
An additional method of reporting was used for the two largest specialist ME/CFS centres, Royal United Hospitals, Bath, and University College London Hospitals, London where CYP are assessed and treated by therapists and not paediatricians (following their initial referral and diagnosis). In these centres, data were also collected on eligible CYP by therapists and returned without prior notification. While the reporting methods are independent sources of cases, they do not represent capture–recapture for the purposes of ascertainment estimation; this approach was used to ensure cases were not missed.
Case definition
CYP with severe ME/CFS were defined using a three-stage procedure. First, paediatricians used a surveillance case definition to identify CYP (box 1). The study team then applied the exclusion criteria. Cases were then reviewed by the expert ME/CFS panel, which consisted of three paediatricians with expertise in ME/CFS and two similarly experienced psychiatrists. The group applied the analytical case definition to verify the diagnosis of ME/CFS and to categorise the cases as to whether the CYP had severe ME/CFS or whether further information was required. School attendance featured in the surveillance definition but was not the sole discriminant in the analytical case definition (box 1), which also applied functional impact on activities of daily living (ADLs). Attending school is one of several possible measures because not only is it important and readily available but also it is the usual activity for CYP of this age who do not have ME/CFS.
Box 1. Criteria for case identification and definition.
Surveillance case definition
Child aged 5–16 years.
Clinical diagnosis of ME/CFS.
Fatigue that is so severe that they are unable to attend school for more than 1 hour a week during the last 6 weeks of the school term.
Study team exclusion criteria
CYP over 16 years of age at the time of reporting.
Cases reported outside of the surveillance period.
CYP with alternative diagnoses that could explain the fatigue.
CYP without routine blood tests and investigations suggestive of another cause for the fatigue.
CYP that attended school more than 1 hour a week.
Analytical case definitions
Severe ME/CFS: fulfils the criteria in item 1 and one symptom from item 2.
Probable severe ME/CFS: item 1 criteria met, with the exception of a dependence on assistance with activity of daily living.
Possible severe ME/CFS: fulfils most of item 1 and one symptom from item 2, but it is not known if the NICE-recommended screening blood is normal or information on function is missing.
Does not have severe ME/CFS.
Item 1
New onset (not lifelong) of severe fatigue occurring for 3 consecutive months or greater duration, which is unrelated to exertion, is not substantially relieved by rest and is not a result of other medical conditions.
The fatigue causes a significant reduction in ability to carry out activities of daily living such that they are unable or can only carry out minimal daily tasks such as face washing and teeth cleaning.
Unable to leave the house without a severe and prolonged after-effect. Therefore, either completely housebound or bedbound or only leaves the house occasionally (eg, for medical appointments).
Item 2 (symptoms at presentation required to fulfil diagnostic criteria for ME/CFS)
Impaired memory or concentration.
Postexertion malaise, where physical or mental exertions bring on ‘extreme, prolonged exhaustion and sickness’.
Problems with sleep, including unrefreshing sleep.
CYP, children and young people; ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome; NICE, National Institute for Health and Care Excellence.
Data analysis
Data were analysed using Stata V.16.0 (Statcorp, Texas, USA). Population estimates for 2019/2020 were obtained from the Office for National Statistics for UK and from Central Statistics Office of Ireland and were used to calculate prevalence and incidence rates. Incident case diagnoses were randomly occurring events within the given time interval, so Poisson distribution was applied. CIs were calculated accordingly using the formula provided by Bégaud et al.9
Incidence was defined as patients whose date (of becoming housebound) falls within the reporting interval or were ‘new to reporting clinician within the preceding 4 weeks’. Those who’s symptom onset began before this time period were considered to be prevalent cases. A sensitivity analysis was carried out to evaluate the possible effect of missing questionnaires on prevalence and incidence. A statistical analysis plan was prewritten before analysis (OSF: Open Science Framework).
Results
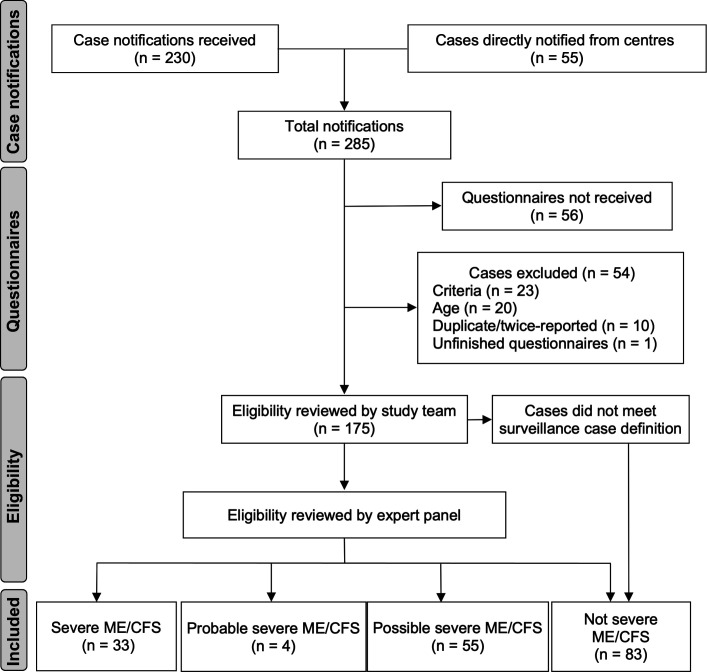
A total of 285 notifications were received (figure 1), of which 56 did not return questionnaires (though some were from referral centres and so reported separately); 20 were CYP older than 16; and 10 were duplicates. Of the 175 valid questionnaires received, 55 were provided by the two large referral centres, and the remainder were through BPSU notifications.
Figure 1.
Schematic of reported cases20: reported cases of severe ME/CFS in children 5–16 years old from January 2018 to January 2019.
Data were complete enough in 33 cases to determine confirmed prevalence of severe ME/CFS. Eighty-three were considered not to have severe ME/CFS. Missing data were seen in 59 cases, which were defined as probable or possible severe ME/CFS. This was due to missing demographic information, incompletely reported symptoms or missing/unknown test results. Probable cases were defined as those that met item 1 criteria for severe ME/CFS (box 1), but it was not clear whether they had experienced a significant reduction in ADLs. Twenty-eight (47%) of these 59 possible cases were unable to be confirmed as severe due to one or more missing test results.
Estimated prevalence (n=33) and incidence rate (n=10)
Prevalence of severe ME/CFS seen by specialists was estimated at 3.2 per million CYP aged 5–16 years (95% CI 2.2 to 4.5); 21 of these were reported through the BPSU and 12 directly from specialist centres. Prevalence of cases including both confirmed and possible/probable severe ME/CFS was 8.9 per million children (95% CI 7.2 to 11). The severe ME/CFS incidence rate across the UK and Ireland was 0.90 per million children-years aged 5–16 years (95% CI 0.43 to 1.65). The incidence rate (including possible and probable cases) was 1.97 per million children-years aged 5–16 years (95% CI 1.24 to 2.99). This means that at least 33 (or between 33 and 92) CYP are seen each year in specialist services with severe ME/CFS. The burden is likely greater when one considers the very strict criteria used to defined ME/CFS. The number of CYP with severe health needs that were reported to this survey with high levels of fatigue was 175. Fifty-six missing questionnaires might have caused an underestimation of case prevalence. One-way sensitivity analysis projected the prevalence if all 56 missing questionnaires had reported cases of severe ME/CFS to be 8.6 per million children (95% CI 6.9 to 11) and prevalence of 4.0 per million children (95% CI 2.8 to 5.4) if proportions of severe/probable/possible cases remained extant. Incidence rates were 5.7 per million children-years (95% CI 4.4 to 7.3) and 1.08 per million children-years (95% CI 0.56 to 1.88), respectively.
Demographic features
The median age of onset of diagnosis was 13 years (IQR 11–14) (table 1); the median age of first fatigue was 12 years (IQR 10–13); and the median age of becoming housebound was 13 years (IQR 12–14). Of the 30 cases where age at diagnosis was reported, 1 (3%) was under 9 years of age; 13 (43%) were in the age range of 9–12 years; and 16 (53%) were in the age range of 13–16 years.
Table 1.
Description of case demographics and prediagnostic symptomatic interval
| Characteristics | Severe ME/CFS | Probable severe ME/CFS | Possible severe ME/CFS | ||||
| n=33 | n=4 | n | n=55 | ||||
| Age at diagnosis (years), median (IQR) | 13 | (11–14) | 14 | (13–14) | 14 | 46 | (14–15) |
| Female, n (%) | 19 | (58) | 4 | (100) | 31 | 54 | (57) |
| Ethnicity A1, n (%) | 32 | (97) | 3 | (100) | 50 | 52 | (96) |
| Time: fatigue onset to diagnosis (years) | |||||||
| Time, median (IQR) | 0.47 | (0.35–0.67) | 0.97 | (0.65–1.65) | 0.82 | (0.36–2.01) | |
ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome.
There was no significant difference in numbers of female and male CYP confirmed with severe ME/CFS, with similar proportions seen in the possible cases. Ethnicity was recorded via Coding for Ethnic Group (Office for National Statistics, 2001). Ninety-seven per cent of CYP were white (32/33).
Clinical features: symptoms
Clinical features were reported by paediatricians. Most CYP had described impaired memory and concentration (94%), and paediatricians reported both postexertion malaise and sleep disturbance in 97% (table 2). Muscle pain was common (88%). Approximately two-thirds of cases reported pain in multiple joints and headaches (of a new kind or greater severity). Forty-three per cent of CYP reported frequent and/or recurring sore throats, and only 4/33 CYP (14%) reported tender lymphadenopathy. Symptoms were similar between male and female patients.
Table 2.
Description of clinical features and function of CYP with severe ME/CFS
| Severe ME/CFS Sex |
||||
| % (n) | Female | Male | P value | |
| Symptoms | ||||
| Impaired memory and concentration (32) | 94 (30) | 90 (17) | 93 (13) | 0.86 |
| Postexertion malaise (33) | 97 (32) | 95 (18) | 100 (14) | 0.38 |
| Sleep disturbance (including unrefreshing sleep) (33) | 97 (32) | 100 (19) | 93 (13) | 0.24 |
| Muscle pain (32) | 88 (28) | 89 (16) | 86 (12) | 0.79 |
| Pain in multiple joints (31) | 68 (21) | 65 (11) | 71 (10) | 0.69 |
| Headaches (new kind/greater severity) (30) | 63 (19) | 69 (11) | 57 (8) | 0.51 |
| Sore throat (frequent/recurring) (30) | 43 (13) | 50 (8) | 36 (5) | 0.43 |
| Tender lymph nodes (cervical/axillary) (29) | 14 (4) | 13 (2) | 15 (2) | 0.82 |
| Function: school attendance (32) | ||||
| No tuition (no home tuition or schooling) | 63 (20) | 72 (13) | 50 (7) | 0.20 |
| Home tuition | 31 (10) | 22 (4) | 43 (6) | 0.21 |
| Attending school or hospital school for <1 hour a week | 6.3 (2) | 5.6 (1) | 7.1 (1) | 0.86 |
| Function: independence with ADLs (32) | ||||
| Requires help with all ADLs | 13 (4) | 0 (0) | 31 (4) | 0.78 |
| Requires some help with daily activities sometimes | 81 (26) | 95 (18) | 62 (8) | 0.02 |
| Able to do all daily activities over the last 6 weeks | 6.3 (2) | 5.3 (1) | 7.7 (1) | |
ADLs, activities of daily living; CYP, children and young people; ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome.
Function: ADLs
Table 2 shows function (independence of ADLs) of CYP with severe ME/CFS. The majority needed at least some help with ADLs at least some of the time (a criterion for severe case definition). Thirteen per cent needed help with all ADLs, and 81% required some help with daily activities sometimes. Those CYP (n=2, 6.3%) not requiring help were either beneath the age cut-off at which ADLs would be expected to be performed independently or were wheelchair-bound by their fatigue (qualifying as severe on that criterion).
Function: school attendance
Twenty of 32 CYP (63%) had received no tuition in the 6 weeks preceding assessment, and this included no school attendance or home tuition. Widening the case definition to include probable and possible cases found 39 of 86 CYP (45%, p=0.097). Home tuition was being received by 10 CYP with severe ME/CFS. Only two CYP were attending school/hospital school for <1 hour a week, and no CYP were attending for >1 hour a week.
Length of time from symptom onset to diagnosis
The median time from first symptom onset to diagnosis was 0.47 years (IQR 0.35–0.67) for definite/probable cases and 0.82 years (IQR 0.35–2.01) for possible cases. In severe cases, 15 cases were diagnosed within 6 months of experiencing their fatigue, and 6 CYP waited a year or longer.
Discussion
In this study, 175 questionnaires were received about CYP who were reported to have severe ME/CFS in the UK over 13 months. However, using a stringent definition (including a full set of test results), results showed that only 33 of these met criteria for severe ME/CFS. An additional 59 CYP had probable/possible severe ME/CFS. Forty-two per cent of those with confirmed and possible/probable ME/CFS (39/92) were not receiving no tuition of any kind in the 6 weeks preceding their assessment.
Strengths and limitations
The BPSU provides excellent coverage of registered paediatricians and typically receives >90% response rates, making it well suited for screening for rare conditions.10 Despite this, 56 questionnaires were not returned following notifications, despite reminder emails/phone calls, and it is unclear whether these represent missed cases or duplicates (preidentified by reporters). This was higher than expected and may have been made worse as the study was conducted during a global pandemic. We were unable to conduct the 12 month follow-up because of the pandemic, which would have provided additional information about outcome and treatment. Use of the expert panel applying the analytical case definition provided an external view on case classification. The requirement for full blood test results meant that many CYP were excluded. This may mean our prevalence estimate is too low. We introduced additional methodology to capture CYP assessed by therapists in the two largest centres as therapists do not receive BPSU bulletins; however, these CYP had been assessed by paediatricians before referral for therapy. It is possible that we have missed CYP seen by therapists in other centres but, as far as we are aware, they are all assessed by paediatricians and therefore should have been reported. Ascertainment robustness has not been quantified in this study and a low rate of duplicates suggests cases may have been underestimated.
Epidemiology
This is the first nationwide prospective study into the epidemiology of severe ME/CFS in children 5–16 years of age in the UK and Ireland, and few credible comparators exist to provide context for it. Most figures are estimations of paediatric ME/CFS of all degrees of severity. Our prevalence for severe ME/CFS seen by paediatric services is several orders of magnitude lower than previous estimates of ME/CFS reported in Lim et al’s recent systematic review3 and other studies.11 12 Lim et al reported a prevalence of 0.89%, but this figure included those CYP experiencing more mild disease.
In 2000 a small study of CYP with ME/CFS (n=25) suggested that 68% had been severely affected at some point in their illness13 14; 57% had been bedbound and totally unable to attend school at some point during their worst episode (defined by both severity of physical symptoms and functional impairment). This difference from our study is likely to be due to prospective, not retrospective, recruitment; our strict eligibility criteria; the requirement for paediatricians to make the diagnosis; and our recruitment taking place over 1 year (rather than the retrospective study, which reviewed severity after a latency of over 3 years).
Symptoms and demographics
Our study showed a distribution of symptoms similar to those of studies which have explored symptoms across the full spectrum of disease severity.11 Age of incidence is comparable to these studies, with a peak age of incidence of 13–15 years old. Fifty-five per cent of our patients are female, which is lower than previous studies, as past studies of adolescent ME/CFS suggest a more typical proportion of 60%–65% women.15
School attendance
Thirty-nine of 86 CYP (45%) with possible, probable and confirmed severe ME/CFS were known to be receiving no tuition of any kind in the 6 weeks preceding their assessment. This figure bears no easy comparison to other studies because previous explorations of school attendance in paediatric ME/CFS have included all severities of the condition, and severely affected CYP will likely be under-represented.16 Lack of education provision will likely have significant short-term, medium-term and long-term consequences for this patient group.17 18 The general paucity of home tuition as a potential substitute for school attendance is noteworthy, although this should be less of a factor when one considers the debilitating nature of severe fatigue.
Diagnosis
CYP appeared to access secondary care faster than previously reported.19 However, previous reports were mainly from a large tertiary service in the Southwest, where a cohort of 590 adolescents waited a mean of 25 months before assessment. While our numbers remain small, it is possible that severe cases may be assessed and diagnosed more quickly than those with less severe disease.
Conclusions
This study reports a low incidence of severe ME/CFS; however, children reported are very sick with few receiving home tuition, and clinicians should be aware that this group are unlikely to be receiving tuition at home. As fewer women and non-white individuals were found than we initially expected, we should aim to understand whether barriers to diagnosis exist for these populations. Further studies could explore early predictors of severe illness, where intervention might affect symptom progression.
Acknowledgments
The authors thank all the paediatricians who reported cases and completed the surveillance questionnaires. We acknowledge and thank Hacer Sonmez and Eirini Triantafyllou for their contribution to data collection and database maintenance. The authors also thank Richard Lynn, Jacob Avis and the team at the British Paediatric Surveillance Unit for their continued support throughout the study.
Footnotes
Twitter: @terryheller1
Contributors: This study was conceived and designed by EMC and AB. APR, MR, SB and TYS performed data collection, analysis and interpretation. APR wrote the manuscript. EMC is guarantor.
Funding: The study was funded by The National Institute for Health Research (Senior Research Fellowship, SRF-2013-06-013) and a grant from the Royal United Hospitals Bath NHS Foundation Trust.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. All data relevant to the study are included in the article or uploaded as supplementary information. Data were collected having been granted Section 251 Confidentiality Advisory Group permission (Ref: 18/CAG/00051). To that end, no further data are available to be shared.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by National Research Ethics System Committee South West-Central Bristol Research Ethics Committee (Ref: 18/SW/0051, IRAS project ID: 223838), collected under British Paediatric Surveillance Unit (surveillance system for the study of rare diseases). It was granted Section 251 Confidentiality Advisory Group permission (ref: 18/CAG/00051) and Public Benefit and Privacy Panel for Health and Social Care approval (ref: 1718–0341).
References
- 1. Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International chronic fatigue syndrome Study Group. Ann Intern Med 1994;121:953–9. 10.7326/0003-4819-121-12-199412150-00009 [DOI] [PubMed] [Google Scholar]
- 2. NICE . Chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy): diagnosis and management. NG2062021.
- 3. Lim E-J, Ahn Y-C, Jang E-S, et al. Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J Transl Med 2020;18:100. 10.1186/s12967-020-02269-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pheby D, Sneddon P, Heinrich I, et al. Severe ME/CFS in Adults-A report from the CHROME Database. Medical Statistician 2012. [Google Scholar]
- 5. Burgess M, Chalder T. Adolescents with severe chronic fatigue syndrome can make a full recovery. BMJ Case Rep 2011;2011. 10.1136/bcr.01.2011.3716. [Epub ahead of print: 10 May 2011]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Strassheim V, Lambson R, Hackett KL, et al. What is known about severe and very severe chronic fatigue syndrome? A scoping review. Fatigue: Biomedicine, Health & Behavior 2017;5:167–83. 10.1080/21641846.2017.1333185 [DOI] [Google Scholar]
- 7. NICE Turnbull N, Shaw EJ, Baker R, eds. Chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy): diagnosis and management of chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy) in adults and children. London, UK: Royal College of General Practitioners, 2007. [Google Scholar]
- 8. Hall SM, Glickman M. The British paediatric surveillance unit. Arch Dis Child 1988;63:344–6. 10.1136/adc.63.3.344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bégaud B, Martin K, Abouelfath A, et al. An easy to use method to approximate Poisson confidence limits. Eur J Epidemiol 2005;20:213–6. 10.1007/s10654-004-6517-4 [DOI] [PubMed] [Google Scholar]
- 10. Verity C, Preece M. Surveillance for rare disorders by the BPSU. The British paediatric surveillance unit. Arch Dis Child 2002;87:269–71. 10.1136/adc.87.4.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nijhof SL, Maijer K, Bleijenberg G, et al. Adolescent chronic fatigue syndrome: prevalence, incidence, and morbidity. Pediatrics 2011;127:e1169–75. 10.1542/peds.2010-1147 [DOI] [PubMed] [Google Scholar]
- 12. Chalder T, Goodman R, Wessely S, et al. Epidemiology of chronic fatigue syndrome and self reported myalgic encephalomyelitis in 5-15 year olds: cross sectional study. BMJ 2003;327:654–5. 10.1136/bmj.327.7416.654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rangel L, Garralda ME, Levin M, et al. The course of severe chronic fatigue syndrome in childhood. J R Soc Med 2000;93:129–34. 10.1177/014107680009300306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cox DL, Findley LJ. Severe and very severe patients with chronic fatigue syndrome. J Chronic Fatigue Syndr 2000;7:33–47. 10.1300/J092v07n03_04 [DOI] [Google Scholar]
- 15. Crawley E. Pediatric chronic fatigue syndrome: current perspectives. Pediatric Health Med Ther 2017;9:27–33. 10.2147/PHMT.S126253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pendergrast T, Brown A, Sunnquist M, et al. Housebound versus nonhousebound patients with myalgic encephalomyelitis and chronic fatigue syndrome. Chronic Illn 2016;12:292–307. 10.1177/1742395316644770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Knight SJ, Politis J, Garnham C, et al. School functioning in adolescents with chronic fatigue syndrome. Front Pediatr 2018;6:302. 10.3389/fped.2018.00302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sankey A, Hill CM, Brown J, et al. A follow-up study of chronic fatigue syndrome in children and adolescents: symptom persistence and school absenteeism. Clin Child Psychol Psychiatry 2006;11:126–38. 10.1177/1359104506059133 [DOI] [PubMed] [Google Scholar]
- 19. Crawley EM, Emond AM, Sterne JAC. Unidentified chronic fatigue Syndrome/myalgic encephalomyelitis (CFS/ME) is a major cause of school absence: surveillance outcomes from school-based clinics. BMJ Open 2011;1:e000252. 10.1136/bmjopen-2011-000252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rennie D. CONSORT revised--improving the reporting of randomized trials. JAMA 2001;285:2006–7. 10.1001/jama.285.15.2006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
archdischild-2022-324319supp001.pdf (3MB, pdf)
Data Availability Statement
No data are available. All data relevant to the study are included in the article or uploaded as supplementary information. Data were collected having been granted Section 251 Confidentiality Advisory Group permission (Ref: 18/CAG/00051). To that end, no further data are available to be shared.