Abstract
Objectives
To assess differences in willingness to vaccinate children against COVID-19, and factors that may be associated with increased acceptance, among US caregivers of various racial and ethnic identities who presented with their child to the Emergency Department (ED) after emergency use authorization of vaccines for children ages 5–11.
Study design
A multicenter, cross-sectional survey of caregivers presenting to 11 pediatric EDs in the United States in November-December 2021. Caregivers were asked about their identified race and ethnicity and if they planned to vaccinate their child. We collected demographic data and inquired about caregiver concerns related to COVID-19. We compared responses by race/ethnicity. Multivariable logistic regression models served to determine factors that were independently associated with increased vaccine acceptance overall and among racial/ethnic groups.
Results
Among 1916 caregivers responding, 54.67% planned to vaccinate their child against COVID-19. Large differences in acceptance were noted by race/ethnicity, with highest acceptance among Asian caregivers (61.1%) and those who did not specify a listed racial identity (61.1%); caregivers identifying as Black (44.7%) or Multi-racial (44.4%) had lower acceptance rates. Factors associated with intent to vaccinate differed by racial/ethnic group, and included caregiver COVID-19 vaccine receipt (all groups), caregiver concerns about COVID-19 (White caregivers), and having a trusted primary provider (Black caregivers).
Conclusions
Caregiver intent to vaccinate children against COVID-19 varied by race/ethnicity, but race/ethnicity did not independently account for these differences. Caregiver COVID-19 vaccination status, concerns about COVID-19, and presence of a trusted primary provider are important in vaccination decisions.
Keywords: COVID-19, Vaccination, Race/ethnicity, Vaccine hesitancy
1. Introduction
The COVID-19 pandemic has been associated with significant morbidity and mortality, with a disproportionately high burden noted among racial and ethnic minority children in the United States (US) [1], [2], [3]. Black and Hispanic children in the US account for twice as many COVID-19 cases, emergency department (ED) visits, hospitalizations, and episodes of Multisystem Inflammatory Syndrome in Children (MIS-C), compared to White or Asian children [1], [2], [3], [4]. Unfortunately, while vaccines have been shown to mitigate the burden of severe COVID-19 illness in children [5], [6], [7], vaccine hesitancy remains high among caregivers in the US; as of April 2022, only 28% of 5–11 year old children, and 58% of 12–17 year old children, had received two initial doses of vaccine [8]. Multiple studies have demonstrated intended and actual COVID-19 vaccination rates for children are notably lower among racial and ethnic minority caregivers, particularly those identifying as non-Hispanic Black or African American [9], [10], [11], [12], [13], [14], [15].
Intent to vaccinate children against COVID-19 has waned over time, even with the advent of approved adult and pediatric COVID-19 vaccines [16], [17]. While early in the pandemic (prior to vaccine availability for adults), up to 65% of caregivers reported intent to vaccinate their child [18], that number dropped to < 60% after adult vaccine approval. It is therefore of utmost importance to identify and address barriers and facilitators of pediatric COVID-19 vaccination among caregivers, particularly those identifying as racial/ethnic minorities, in order to improve vaccine uptake and health outcomes in these populations and communities. Data regarding minority caregivers is lacking, and even less is known about factors that contribute to vaccine acceptance in different racial and ethnic populations. We evaluated COVID-19 vaccine acceptance for children among US caregivers by self-reported race and ethnicity (including non-Hispanic White, non-Hispanic Black, Hispanic, Asian, Native American/Pacific Islander, Multi-racial, and Other/Not Specified) after emergency use authorization (EUA) for ages five years and above and described factors that may influence uptake rates. We hypothesized that reported intention for vaccine uptake would be lower among non-Hispanic Black caregivers and higher among White caregivers, and that factors associated with plan to vaccinate would be similar across racial/ethnic groups.
2. Methods
2.1. Study design and setting
This study was part of a larger ongoing COVID-19 Parental Attitude Study (COVIPAS), surveying caregivers of children presenting for emergency care, in the era of COVID-19 [16], [19], [20], [21]. We conducted data analysis on an ongoing multicenter, cross-sectional survey of caregivers presenting with their child to 11 pediatric EDs in the US (Atlanta, GA; Oak Lawn, IL; Los Angeles, CA; Louisville, KY; Milwaukee, WI; Pittsburgh, PA; Portland, OR; Minneapolis, MN; Wilmington, DE; Cleveland, OH; and San Diego, CA). The most recent phase of this study recruited caregivers of children age 18 years or younger presenting to pediatric EDs from November 1 to December 31, 2021. Data collection methods have been previously described in detail [21].
2.2. Survey
The anonymous online survey was available for all caregivers presenting with children to participating EDs and was available in English and Spanish. The study was approved by the Institutional Review Board (IRB) of each site. One caregiver per family was asked to complete the survey. Respondents completed the survey on their own smartphones or institutional iPads by logging into REDCap ® secure online data management platform [22]. Caregivers responded to the question “If vaccine/immunization for COVID-19 is available for your child’s age, would you give it to your child?” Prior work has described factors associated with vaccine uptake among caregivers, including in some ethnic groups, and included information on parental vaccination status, relationship to child, presence of a primary care provider (PCP), and concerns about COVID-19 vaccination and illness [10], [13], [18], [23], [24]. We therefore incorporated similar questions and inquired about demographic characteristics (including race and ethnicity of both caregiver and child, child gender, caregiver relationship to child, and caregiver education level), child age (measured continuously), whether the child had a primary care provider (PCP) (and if the caregiver looked to them for advice), caregivers’ worry that the child currently had COVID-19 (measured by Likert scale 0–10, with 0 = not at all worried and 10 = the most worried I have ever been), caregivers’ concerns about their child missing school (Likert scale 0–10), and whether the caregiver/family had experienced loss of income due to the pandemic. Those variables that were measured via Likert scale were then also categorized according to score: 0–3 (low concern), 4–7 (moderate concern), and 8–10 (high concern).
2.3. Data analysis
Descriptive statistics, including means and standard deviations (SD) for continuous variables and counts and frequencies for categorical variables, were used to characterize relevant demographics. Racial and ethnic identities included Non-Hispanic White, Non-Hispanic Black, Hispanic, Asian, Native American/Pacific Islander, Multi-Racial, and Other/Not Specified (including Middle-Eastern/North African and those self-identifying as “other” or not specifying a listed race/ethnicity). The primary outcome was responding “yes” to the question of whether the caregiver would accept vaccine if/when it was available for their child. Logistic regression models were used to assess possible predictors of this outcome overall (controlling for race/ethnicity in addition to other factors in combination) and within racial/ethnic subgroups (controlling for factors that were independently associated with uptake among White, Black, Hispanic, and respondents whose race/ethnicity was not otherwise specified). Results are presented as odds ratios and 95% confidence intervals. All analyses were conducted using R statistical software version 4.0.3.
3. Results
A total of 1916 caregivers completed the survey (November-December 2021), and 1879 shared their willingness to vaccinate their child. Table 1 demonstrates demographic characteristics of the respondents. The mean age of the index child was 7.6 (SD 5.6) years, 50.3% (n = 960) of children were male, and the responding caregivers were mostly mothers (75.1%, n = 1436). Respondents’ identified race/ethnicities included 49.9% identifying White, 19.5% Black, 12.0% Hispanic, and 16.6% “other/not specified.” A majority of responding caregivers had completed at least some post-secondary education beyond high school (69.6%, n = 1315) and most children had a PCP, (93.5%, n = 1760) although fewer reported looking to that person for advice (78.6%, n = 1,480).
Table 1.
Demographic characteristics of responding caregivers.
| Factor | N (%) |
|---|---|
| Gender of Child (n = 1910) | |
| Male | 960 (50.3) |
| Female | 943 (49.4) |
| Non-binary/other | 7 (0.3) |
| Person completing survey (n = 1912) | |
| Mother | 1436 (75.1) |
| Father | 380 (19.9) |
| Other | 96 (5.0) |
| Caregiver race/ethnicity (n = 1916) | |
| White | 956 (49.9) |
| Black | 373 (19.5) |
| Hispanic | 229 (12.0) |
| Asian | 18 (0.9) |
| Native American/Pacific Islander | 4 (0.2) |
| Multi-racial | 27 (1.4) |
| Other/Not Specified* | 319 (16.6) |
| Education level (n = 1889) | |
| Post-secondary education (Some college or more) | 1315 (69.6) |
| No post-secondary education (high school graduate or less) | 574 (30.4) |
| Child has primary care provider (n = 1882) | |
| Yes, and I usually look for his/her advice | 1480 (78.6) |
| Yes, but he/she does not influence my medical decisions | 280 (14.9) |
| No | 122 (6.5) |
| Child’s regular immunization status (n = 1870) | |
| Up to date | 1642 (87.8) |
| Not up to date | 228 (12.2) |
| Caregiver received COVID-19 vaccine (n = 1881) | |
| Yes | 1338 (71.1) |
| No | 543 (28.9) |
Includes Middle Eastern/North African and those self-identifying as “other”
Half (54.7%, n = 1,027) of caregivers planned to vaccinate their children. There were differences in proportion of caregivers planning to vaccinate based on race and ethnicity (Fig. 1 ), with highest acceptance rates among caregivers identifying as Asian (61.1%) or with an unspecified/other race/ethnicity (65.4%). By contrast, 56.2% of White caregivers reported intent to vaccinate their child, along with 55.4% of Hispanic caregivers. Acceptance was lower among Black (44.7%) and Multi-Racial (44.4%) respondents.
Fig. 1.
Proportion of US caregivers intending to vaccinate their child (November to December 2021), by race/ethnicity.
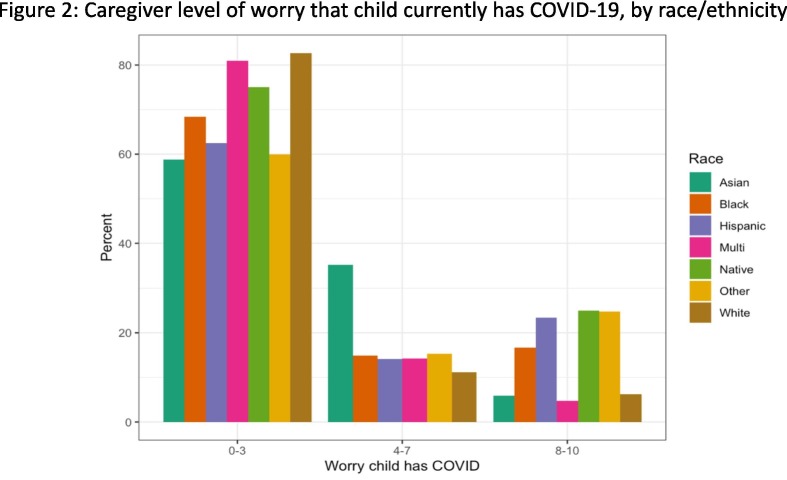
Table 2 describes factors that may contribute to vaccine-related decisions for children among racial/ethnic groups. Vaccination rates for caregivers themselves were lower among those identifying as Black (53.8%) and Multi-racial (51.9%) compared to other groups (Hispanic 82.5%, Other/Not Specified 80.9%, Asian 77.8%, White 72.8%). White and Asian caregivers were more likely to have obtained education beyond high school, and were less likely to report a loss of income due to COVID-19, than those identifying as Black, Hispanic, Multi-racial, or who didn’t specify a race/ethnicity. Black and Multi-Racial caregivers were somewhat less likely to report their child’s scheduled childhood vaccines were up-to-date compared to other groups. White and Asian caregivers reported the lowest level of concern that their child currently had COVID-19 (median Likert scores: White 1.47, Asian 2.47, Black 2.64, Hispanic 3.2, see Fig. 2 ); White caregivers were also less likely to worry about their child missing school (median Likert scores: White 3.02, Asian 3.81, Black 3.84, Hispanic 4.69, see Fig. 3 ).
Table 2.
Social, behavioral, and economic factors and COVID-related concerns among caregivers, by race/ethnicity.
| Factor | White (n, %) |
Black (n, %) |
Hispanic (n, %) |
Asian (n, %) |
Multi-racial (n, %) |
Other/Not Specified (n, %) |
|---|---|---|---|---|---|---|
| Caregiver-related factors | ||||||
| Caregiver received COVID-19 vaccine | ||||||
| Yes | 693 (72.8) | 199 (53.8) | 188 (82.5) | 14 (77.8) | 14 (51.9) | 228 (80.9) |
| No | 259 (27.2) | 171 (46.2) | 40 (17.5) | 4 (22.2) | 13 (48.1) | 54 (19.1) |
| Caregiver education level | ||||||
| Any post-secondary education | 764 (80.1) | 224 (60.1) | 128 (55.9) | 17 (94.4) | 20 (76.9) | 160 (56.1) |
| No post-secondary education | 190 (19.9) | 149 (39.9) | 101 (44.1) | 1 (5.56) | 6 (23.1) | 125 (43.9) |
| COVID-19 led to loss of income | ||||||
| Yes | 290 (31.6) | 170 (50.9) | 105 (49.1) | 2 (11.8) | 11 (50.0) | 137 (50.9) |
| No | 628 (68.4) | 164 (49.1) | 109 (50.9) | 15 (88.2) | 11 (50.0) | 132 (49.1) |
| Child-related factors | ||||||
| Child has PCP | ||||||
| Yes, and I usually look to them for advice | 794 (83.2) | 292 (78.7) | 166 (73.5) | 14 (82.4) | 16 (59.3) | 195 (68.9) |
| Yes, but they don’t influence my decisions | 133 (13.9) | 52 (14.0) | 44 (19.5) | 3 (17.6) | 7 (25.9) | 40 (14.1) |
| No | 27 (2.83) | 27 (7.28) | 16 (7.08) | 0 (0.0) | 4 (14.8) | 48 (17) |
| Child up-to-date on regular vaccines | ||||||
| Yes | 844 (88.7) | 315 (85.8) | 197 (87.9) | 16 (88.9) | 20 (74.1) | 246 (88.2) |
| No | 107 (11.3) | 52 (14.2) | 27 (12.1) | 2 (11.1) | 7 (25.9) | 33 (11.8) |
Fig. 2.
Caregiver level of worry that the child currently has COVID-19, by race/ethnicity.
Fig. 3.
Caregiver level of worry that child will miss school due to COVID-19, by race/ethnicity.
In multivariable analysis (Table 3 ), no racial/ethnic identity was independently associated with an increased likelihood of intent to vaccinate when controlling for other factors. The most decisive factor that was associated with vaccine uptake was caregivers’ COVID-19 vaccination status (OR 29.11, 95% CI 20.59–42.12). Other factors included having a PCP to whom the caregiver looked for advice (OR 1.86, 95% CI 1.07–3.19), child age (OR 1.08, 95% CI 1.05–1.11), and caregiver concern that the child currently had COVID-19 (OR 1.05, 95% CI 1–1.09). Table 4 describes factors that were independently associated with vaccine uptake for each specific racial/ethnic group (including White, Black, Hispanic, and Other/Not Specified). Caregiver receipt of COVID-19 vaccine was associated with increased intent to vaccinate among all these groups. Child age was also associated with increased vaccination, with each year of increase in age associated with a linear increase in uptake. Notably, caregiver COVID-19 vaccine receipt doubled the odds of acceptance among White respondents (OR 46.4, 95% CI 26.91–86.39) compared to Hispanic (OR 23.92, 95% CI 7.3–102.9) or Black (18.07, 95% CI 9.75–35.28). Factors associated with increased likelihood of vaccine acceptance among specific racial/ethnic groups included: concern the child has COVID-19 while in the ED (White caregivers only, OR 1.09, 95% CI 1.02–1.18) and having a primary provider to whom caregivers looked for advice (Black caregivers only, OR 4.03, 95% CI 1.17–15.51). Loss of income due to COVID-19 was associated with decreased likelihood of vaccination among caregivers not identifying as a listed specific race/ethnicity (OR 0.38, 95% CI 0.18–0.77) but did not affect intent among other groups.
Table 3.
Multivariable analysis, factors independently associated with increased likelihood of intent to vaccinate child, overall.
| Factor | OR (95% CI) | P-value |
|---|---|---|
| Race | ||
| White | (reference) | (reference) |
| Black | 1.07 (0.75, 1.54) | 0.72 |
| Hispanic | 0.76 (0.52, 1.13) | 0.17 |
| Asian | 1.22 (0.35, 4.86) | 0.77 |
| Native American/Pacific Islander | Unable to estimate* | |
| Multi-racial | 1.32 (0.39, 4.68) | 0.66 |
| Other/Not Specified | 1.44 (0.98, 2.15) | 0.07 |
| Child age | 1.08 (1.05, 1.11) | <0.001 |
| Caregiver received COVID-19 vaccine | 29.11 (20.59, 42.12) | <0.001 |
| Child has PCP, and I usually look for his/her advice | 1.86 (1.07, 3.19) | 0.03 |
| Child has PCP, but he/she does not influence my medical decisions | 0.84 (0.45, 1.55) | 0.58 |
| Concern that child has COVID | 1.05 (1, 1.09) | 0.04 |
| Concern about child missing school | 0.99 (0.96, 1.03) | 0.75 |
| Loss of income due to COVID-19 | 0.79 (0.61, 1.03) | 0.09 |
Sample size too small
Table 4.
Multivariable analysis, factors independently associated with increased likelihood of intent to vaccinate child, by race/ethnicity.
| Factor | White OR (95% CI) |
P | Black OR (95% CI) |
P | Hispanic OR (95% CI) |
P | Other/Not Specified* OR (95% CI) |
P |
|---|---|---|---|---|---|---|---|---|
| Child age |
1.05 (1.02, 1.09) |
< 0.001 |
1.08 (1.02, 1.14) |
0.01 |
1.25 (1.15, 1.37) |
< 0.001 |
1.1 (1.03, 1.18) |
0.01 |
| Caregiver received COVID-19 vaccine |
46.4 (26.91, 86.39) |
< 0.001 |
18.07 (9.75, 35.28) |
< 0.001 |
23.92 (7.3, 102.9) |
< 0.001 |
33.29 (12.71, 103.65) |
< 0.001 |
| Child has PCP, looks to them for advice | 1.23 (0.36, 3.81) |
0.73 |
4.03 (1.17, 15.51) |
0.03 | 1.13 (0.2, 5.45) |
0.88 | 1.97 (0.78, 4.85) |
0.14 |
| Child has PCP, does not influence medical decisions | 0.52 (0.14, 1.76) |
0.31 | 2.11 (0.49, 9.75) |
0.32 | 0.77 (0.12, 4.31) |
0.77 | 0.81 (0.25, 2.66) |
0.73 |
| Caregiver with higher education | 1.49 (0.92, 2.4) |
0.11 | 1.08 (0.57, 2.01) |
0.81 | 0.66 (0.3, 1.42) |
0.29 | 0.57 (0.26, 1.18) |
0.13 |
| Caregiver worried child currently has COVID-19 |
1.09 (1.02, 1.18) |
0.02 | 1.03 (0.95, 1.13) |
0.44 | 1.09 (0.99, 1.21) |
0.07 | 0.97 (0.88, 1.06) |
0.47 |
| Caregiver worried about child missing school | 0.95 (0.91, 1) |
0.07 | 1.03 (0.95, 1.11) |
0.51 | 0.99 (0.9, 1.09) |
0.91 | 1.03 (0.94, 1.13) |
0.55 |
| Loss of income due to COVID-19 | 0.90 (0.61, 1.33) |
0.58 | 0.99 (0.55, 1.8) |
0.98 | 0.68 (0.3, 1.5) |
0.34 |
0.38 (0.18, 0.77) |
0.01 |
Includes those self-identifying as “other” or Middle Eastern/North African; excludes multi-racial, Asian, and Native-American/Pacific Islander groups due to small sample size.
4. Discussion
Caregiver intent to vaccinate children against COVID-19 varied by race/ethnicity in this study, but race/ethnicity did not independently account for these differences. Caregiver COVID-19 vaccination status is a major factor in their decision-making process across racial and ethnic groups. Although concerns about COVID-19 and presence of a trusted primary provider are also important factors, these differ by race and ethnicity and may provide the basis for targeted interventions to improve vaccination rates among adults (and therefore children) in minority populations.
Racial and ethnic disparities in vaccination rates persist despite availability of vaccines [14], [25], [26], [27]. According to the Kaiser Family Foundation (KFF) Vaccine Monitor program, pediatric COVID-19 vaccination increased overall in 2021, with larger shares of parents reporting their 12–17 year old children have been vaccinated, while the proportion of those definitely not planning to vaccinate has dropped [28]. Vaccination rates are lower among children 5–11 years old, although they have increased from November 2021 to February 2022 as the vaccine became available to this age group [28], [29]. Many studies have reported on factors associated with increased COVID-19 vaccine uptake for children, most of which occurred either before vaccine was approved for children, or shortly after EUA for ages 12–17 years [13], [15], [16], [18], [27], [30], [31] To our knowledge, this study is the first large-scale, national survey to report on caregiver vaccination plans and attitudes since the availability of vaccine for children under 12 years.
In prior surveys, race and ethnicity were predictors of intent to vaccinate children against COVID-19, with Black caregivers reporting lower intent to vaccinate compared to non-Hispanic White groups [10], [11], [12], [13], [14], [15], [27]. Other previously reported factors associated with increased vaccination include caregiver education level, family income, caregiver COVID-19 vaccination status/intent, caregiver political affiliation, concerns about COVID-19 illness, child’s regular and/or influenza vaccination status, and child age [10], [11], [16], [24]. We identified similar factors associated with overall intent to vaccinate in this study (specifically child age and caregiver vaccination status); however, despite the fact that Black and Multi-racial caregivers had lower reported intent to vaccinate compared to Whites or Hispanics, we did not find that race/ethnicity was associated with plan to vaccinate when controlling for other factors. Rather, other factors may be responsible for truncated vaccination rates in minority populations. This has been explored in adults [23], [32], [33], [34], but is a crucial and unique finding regarding caregivers’ intent to vaccinate children in this study. Prior studies suggest that understanding the concerns or factors influencing decision-making among racial/ethnic minority parents is crucial to inform and improve strategies for providing targeted information about vaccination to these groups [11], and we confirm that understanding these more specific factors may be critical to improving vaccine uptake.
The single strongest predictor of vaccination across all groups in this study was caregiver receipt of COVID-19 vaccine. This finding is consistent with previous reports from earlier in 2021 [11], [13], [14], [35], and the ongoing association between caregiver and pediatric vaccination makes sense given the correlation between increasing adult and pediatric vaccination rates throughout 2021 and early 2022. Given the particularly strong relationship between adult and child vaccination across racial and ethnic groups, public health initiatives targeting improved vaccination of adults may be among the most important methods to improve vaccination rates among children across racial/ethnic groups. Such initiatives must take into account factors that are of particular significance to different racial and ethnic groups, targeting campaigns toward factors, such as COVID-19 related concerns or trust in a PCP, that are most likely to improve uptake for a specific population.
Other factors that may contribute to pediatric COVID-19 vaccination decisions include caregiver concerns about both illness and vaccines, which may vary by race and ethnicity. In December 2021, the KFF Vaccine Monitor reported that Black and Hispanic caregivers were more likely to be worried about their child becoming seriously sick from COVID-19, compared to Whites [29]. Families identifying as non-White have also reported increased frequency of socioeconomic disruption, including loss of income, throughout the pandemic [27], [36]. We report similar findings, with higher proportions of Black and Hispanic caregivers reporting high levels of concern about their child having COVID-19 or missing school compared to White or Asian caregivers. Black and Hispanic caregivers were also more likely to report loss of income due to COVID-19, although reasons for loss of income were not evaluated; however, this was also not associated with differences in vaccine uptake. Significant contrast exists, therefore, between caregiver concerns about COVID-19 illness and likelihood of vaccination, where those groups most concerned/affected are not necessarily those most likely to vaccinate. This dichotomy may indicate that concerns about vaccines are overcoming concerns about the virus and its impact on family dynamics.
While concerns about COVID-19 or loss of income were not significant factors contributing to vaccination intent among Black caregivers in this study, it is noteworthy that the presence of a PCP, to whom caregivers looked for advice, was significantly associated with vaccination in this group. Other studies have reported that despite vaccine hesitancy and institutional mistrust among Black patients, vaccine recommendations from a trusted provider, particularly from a same-race medical professional, or from a same-race vaccine study participant, may be a facilitator of vaccination in adults [26], [37]. Many Black caregivers report that their child’s doctor is a key source of information [14], and up to 74% of Black parents report that their child’s pediatrician is a trusted resource [29]. The association between intent to vaccinate and presence of a trusted provider in our study underscores the importance for physicians to develop and maintain strong working relationships with families, and not to underestimate the importance of their recommendations for vaccination to minority caregivers.
Limitations of this study included the use of a convenience sample at all participating sites, such that the population of caregivers responding to the survey may not represent all caregivers. There may have been bias in terms of survey completion based on pre-existing vaccination beliefs in the participants; however, this could apply to both vaccine supporters as well as vaccine-hesitant caregivers. Of note, the majority of caregivers in this study were highly educated and vaccinated for COVID-19, which may have influenced their decision to participate; as a result, our findings may not be representative of the population as a whole. We reported on caregiver’s intended plan to vaccinate and did not corroborate vaccination status among those who may have already received vaccine. Additionally, we did not address all potential factors (such as income level, insurance status, religion, or political affiliation) that may contribute to decision-making among various groups. This is of particular importance given the topic of race and ethnicity—while we chose socioeconomic covariates based on prior literature related to vaccine uptake among patients and caregivers, the variables included in this study are unlikely to represent the breadth of socioeconomic-related factors (including educational, housing, employment, and other inequities/systemic disenfranchisement) which may confound the association between race/ethnicity and vaccine beliefs. Finally, we assessed racial and ethnic groups according to those utilized by the US Census; however, not all groups had equal numbers of respondents--Asians, Native American/Pacific Islanders, and Multi-racial groups all had a small sample size in the study population. As a result, causality cannot be determined in these populations as well as in other subgroups. Additionally, a number of caregivers did not specify their identity, and therefore generalizability for this group is limited.
5. Conclusions
In conclusion, while caregiver intent to vaccinate children against COVID-19 varied by race and ethnicity, racial identity did not independently account for these differences when controlling for other factors. Caregiver COVID-19 vaccination is a major factor in pediatric vaccine uptake across all racial and ethnic groups, and public health officials should target improvement in adult vaccination rates to ultimately improve pediatric vaccine uptake. Other factors, such as concerns about COVID-19 and presence of a trusted PCP, may be particularly important in caregiver vaccination decisions among certain groups, and could serve as the basis for future interventions to improve adult, and thereby pediatric, vaccination among minority children and the pediatric population as a whole.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge the members of the COVID-19 Parental Attitude Survey (COVIPAS) study group, including Dr. Renana Gelernter, MD (Tel Aviv University, Israel), Dr. Gianluca Gualco, MD (Pediatric Institute of Ticino, Switzerland), Dr. Danna Krupik, MD (Ziv Hospital Center, Safed, Israel), Dr. Ahmed Mater, MD (Jim Pattison Children’s Hospital, Saskatoon, Canada), Dr. Sergio Manzano, MD (Geneva Children’s Hospital, Switzerland), Dr. Nina Muhammad (Advocate Children’s Hospital, Oak Lawn, IL), Dr. Michelle Seiler (Children’s Hospital Zurich, Switzerland), and Dr. Graham Thompson (Alberta Children’s Hospital, University of Calgary, Alberta, Canada).
References
- 1.Smith A.R., DeVies J., Caruso E., et al. Emergency department visits for COVID-19 by race and ethnicity - 13 States, October-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(15):566–569. doi: 10.15585/mmwr.mm7015e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goyal MK, Simpson JN, Boyle MD, et al. Racial and/or Ethnic and Socioeconomic Disparities of SARS-CoV-2 Infection Among Children. Pediatrics. 2020;146(4)doi:10.1542/peds.2020-009951. [DOI] [PubMed]
- 3.Prevention CfDCa. Disparities in COVID-19 associated hospitalizations. Centers for Disease Control and Prevention. Updated January 27, 2022. Accessed February 4, 2022. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-hospitalization.html.
- 4.Lee E.H., Kepler K.L., Geevarughese A., et al. Race/ethnicity among children with COVID-19-associated multisystem inflammatory syndrome. JAMA Netw Open. 2020;;3(11) doi: 10.1001/jamanetworkopen.2020.30280. e2030280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuehn B.M. COVID-19 vaccine highly effective against adolescent hospitalizations. JAMA. 2021;326 doi: 10.1001/jama.2021.20143. [DOI] [PubMed] [Google Scholar]
- 6.Klein N.P., Stockwell M.S., Demarco M., et al. Effectiveness of COVID-19 Pfizer-BioNTech BNT162b2 mRNA Vaccination in Preventing COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Nonimmunocompromised Children and Adolescents Aged 5–17 Years - VISION Network, 10 States, April 2021-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(9):352–358. doi: 10.15585/mmwr.mm7109e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zambrano L.D., Newhams M.M., Olson S.M., et al. Effectiveness of BNT162b2 (Pfizer-BioNTech) mRNA vaccination against multisystem inflammatory syndrome in children among persons aged 12–18 years - United States, July-December 2021. MMWR Morb Mortal Wkly Rep. 2022;71(2):52–58. doi: 10.15585/mmwr.mm7102e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pediatrics AAo. Summary of data publicly reported by the Centers for Disease Control and Prevention Date: 4/27/22. American Academy of Pediatrics. Updated April 27, 2022. Accessed May 6, 2022. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-vaccination-trends/#:∼:text=Child%20vaccination%20rates%20vary%20widely%20across%20states%3A,50%25%20have%20received%201%20dose.
- 9.Prevention CfDCa. COVID data tracker. Centers for Disease Control and Prevention. Accessed April 15, 2021. https://covid-cdc-gov.echo.louisville.edu/covid-data-tracker/?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcases-updates%2Fcases-in-us.html#datatracker-home
- 10.Alfieri N.L., Kusma J.D., Heard-Garris N., et al. Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health. 2021;21 doi: 10.1186/s12889-021-11725-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teasdale C.A., Borrell L.N., Shen Y., et al. Parental plans to vaccinate children for COVID-19 in New York city. Vaccine. 2021;39(36):5082–5086. doi: 10.1016/j.vaccine.2021.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.K. Viswanath, M. Bekalu, D. Dhawan, R. Pinnamaneni, J. Lang, R. McLoud, Individual and social determinants of COVID-19 vaccine uptake, BMC Public Health. 21(1) (2021) 818. doi:10.1186/s12889-021-10862-1. [DOI] [PMC free article] [PubMed]
- 13.Fisher C.B., Gray A., Sheck I. COVID-19 pediatric vaccine hesitancy among racially diverse parents in the United States. Vaccines (Basel) 2021;10 doi: 10.3390/vaccines10010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Szilagyi P.G., Shah M.D., Delgado J.R., et al. Parents' intentions and perceptions about COVID-19 vaccination for their children: results from a national survey. Pediatrics. 2021;148 doi: 10.1542/peds.2021-052335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rane M.S., Robertson M.M., Westmoreland D.A., Teasdale C.A., Grov C., Nash D. Intention to vaccinate children against COVID-19 among vaccinated and unvaccinated US parents. JAMA Pediatr. 2021 doi: 10.1001/jamapediatrics.2021.5153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldman R.D., Krupik D., Ali S., et al. Caregiver willingness to vaccinate their children against COVID-19 after adult vaccine approval. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph181910224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teherani M., Banskota S., Camacho-Gonzalez A., et al. Intent to vaccinate SARS-CoV-2 infected children in US households: a survey. Vaccines (Basel) 2021;9 doi: 10.3390/vaccines9091049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldman R.D., Yan T.D., Seiler M., et al. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine. 2020;38(48):7668–7673. doi: 10.1016/j.vaccine.2020.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.R.D. Goldman, J.N. Bone, R. Gelernter, et al., Willingness to accept expedited COVID-19 vaccine research for children aged <12 years after adult vaccine approval, Clin. Therapeut. 16 2021;doi:10.1016/j.clinthera.2021.11.003. [DOI] [PMC free article] [PubMed]
- 20.Goldman R.D., Marneni S.R., Seiler M., et al. Caregivers' willingness to accept expedited vaccine research during the COVID-19 pandemic: a cross-sectional survey. Clin Ther. 2020;42(11):2124–2133. doi: 10.1016/j.clinthera.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldman R.D., McGregor S., Marneni S.R., et al. Willingness to vaccinate children against influenza after the coronavirus disease 2019 pandemic. J Pediatr. 2021;228:87–93.e2. doi: 10.1016/j.jpeds.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.A.B. Bagasra, S. Doan, C.T. Allen, Racial differences in institutional trust and COVID-19 vaccine hesitancy and refusal. BMC Public Health. 21(1) (2021) 2104. doi:10.1186/s12889-021-12195-5 [DOI] [PMC free article] [PubMed]
- 24.Hamel LLLKAKASGSMBM. KFF COVID-19 Vaccine Monitor: Parents and the Pandemic. Kaiser Family Foundation. Accessed September 21, 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-parents-and-the-pandemic/.
- 25.N.H.L. Ndugga, S. Artiga, S. Haldar, Latest data on COVID-19 vaccinations by race/ethnicity. Kaiser Family Foundation; 2022. February 2, 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/#:∼:text=Percent%20Who%20Have%20Received%20At%20least%20One%20Dose&text=These%20data%20will%20differ%20from,for%20Black%20people%20(55%25).
- 26.Kricorian K., Turner K. COVID-19 vaccine acceptance and beliefs among black and hispanic americans. PLoS One. 2021;16(8) doi: 10.1371/journal.pone.0256122. e0256122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kreuter M.W., Garg R., Marsh A., et al. Intention to vaccinate children for COVID-19: a segmentation analysis among Medicaid parents in Florida. Prev Med. 2022;156 doi: 10.1016/j.ypmed.2022.106959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.M HLSGLLSMB. KFF COVID-19 Vaccine Monitor: January 2022 Parents and Kids Update. Kaiser Famly Foundation. Accessed February 21, 2022. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-january-2022-parents-and-kids-update/.
- 29.M HLLLKASMKASGaB. KFF COVID-19 Vaccine Monitor: Winter 2021 Update on Parents’ Views of Vaccines for Kids. Kaiser Family Foundation. Accessed February 21, 2022. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-winter-2021-update-on-parents-views-of-vaccines/.
- 30.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020;38(49):7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pan F., Zhao H., Nicholas S., Maitland E., Liu R., Parents' H.Q. Decisions to vaccinate children against COVID-19: a scoping review. Vaccines (Basel) 2021;9 doi: 10.3390/vaccines9121476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwal R., Dugas M., Ramaprasad J., Luo J., Li G., Gao G.G. Socioeconomic privilege and political ideology are associated with racial disparity in COVID-19 vaccination. Proc Natl Acad Sci USA. 2021;118 doi: 10.1073/pnas.2107873118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thompson H.S., Manning M., Mitchell J., et al. Factors associated with racial/ethnic group-based medical mistrust and perspectives on COVID-19 vaccine trial participation and vaccine uptake in the US. JAMA Netw Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.11629. e2111629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Woko C., Siegel L., Hornik R. An investigation of low COVID-19 vaccination intentions among black Americans: the role of behavioral beliefs and trust in COVID-19 information sources. J Health Commun. 2020;25(10):819–826. doi: 10.1080/10810730.2020.1864521. [DOI] [PubMed] [Google Scholar]
- 35.Teasdale C.A., Borrell L.N., Kimball S., et al. Plans to vaccinate children for coronavirus disease 2019: a survey of United States parents. J Pediatr. 2021;237:292–297. doi: 10.1016/j.jpeds.2021.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Radey M., Langenderfer-Magruder L., Brown S.J. “I don't have much of a choice”: low-income single mothers' COVID-19 school and care decisions. Fam Relat. 2021;70(5):1312–1326. doi: 10.1111/fare.12593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Momplaisir F., Haynes N., Nkwihoreze H., Nelson M., Werner R.M., Jemmott J. Understanding drivers of coronavirus disease 2019 vaccine hesitancy among blacks. Clin Infect Dis. 2021;73(10):1784–1789. doi: 10.1093/cid/ciab102. [DOI] [PMC free article] [PubMed] [Google Scholar]