Abstract
Background
The benefit of prior statin use to reduce the incidence of arrhythmia in acute coronary syndrome (ACS) is still a matter of debate. Statins have multiple pleiotropic effects, which may reduce the incidence of in-hospital arrhythmia. A systematic review and meta-analysis were performed to evaluate prior statin use and the incidence of in-hospital arrhythmia in ACS.
Methods
This systematic review was conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). We performed a literature search through Pubmed, Proquest, EBSCOhost, and Clinicaltrial.gov. A random-effect model was used due to moderate heterogeneity. Quality assessment was performed using Newcastle Ottawa Scale. Sensitivity analysis was performed by using leave one or two out method. PROSPERO registration number: CRD42022336402.
Results
Nine eligible studies consisting of 86,795 patients were included. A total of 22,130 (25.5%) patients were in statin use before the index ACS event. The prevalence of old myocardial infarction, heart failure, hypertension, diabetes mellitus, and chronic renal failure and concomitant treatment with aspirin, clopidogrel, and beta blocker was higher in the prior statin group compared to no previous statin. Overall, prior statin use was associated with a significantly lower incidence of in-hospital arrhythmia during ACS compared to no previous statin (OR 0.60; 95% CI 0.49–0.72; P < 0.00001; I2 = 54%, P-heterogeneity = 0.03). In subgroup analysis, previous statin use reduced the incidence of atrial fibrillation or atrial flutter (OR 0.64; 95% CI 0.43–0.95; P = 0.03; I2 = 73%, P-heterogeneity = 0.01) and ventricular tachycardia or ventricular fibrillation (OR 0.57; 95% CI 0.49–0.65; P < 0.00001; I2 = 8%, P-heterogeneity = 0.35).
Conclusions
Based on aggregate patient data, prior statin use may reduce the incidence of in-hospital arrhythmia during ACS, particularly atrial fibrillation or atrial flutter and ventricular tachycardia or ventricular fibrillation.
Keywords: Acute coronary syndrome, Arrhythmia, Atrial fibrillation, Atrial flutter, Previous statin, Statin, Ventricular arrhythmia
1. Background
Acute coronary syndrome (ACS) is one of the most common diseases in the world,1 affecting 7 million people worldwide.2 One complication of ACS is arrhythmia which is associated with poor outcomes.3,4 Sustained ventricular tachycardia, ventricular fibrillation, atrioventricular block, and atrial fibrillation are commonly reported during ACS.5, 6, 7, 8, 9 Other arrhythmias such as non-sustained ventricular tachycardia (NSVT), asystole, premature ventricular complex (PVC), and supraventricular tachycardia are also reported in ACS during the period of hospitalization.4
Statin or 3-hydroxy-methylglutaryl coenzyme A (HMG-CoA) has been used to prevent coronary artery disease for 30 years.10 According to the guidelines, statin is recommended as secondary prevention in ACS.11, 12, 13, 14 Besides lipid-lowering effect, statin also possesses pleiotropic effects such as reducing inflammatory cells in atherosclerotic plaques and increasing plaque stability.15 The incidence of atrial fibrillation (AF), PVC, and NSVT also decrease with early intensive statin treatment during the ACS hospitalization period.16,17 The hypothesis was that statin's pleiotropic effects might improve autonomic control and increase the stability of the myocardium.16,17 Also, statin can stabilize plaque and may reduce ischemia-related ventricular arrhythmia.18 Other than secondary prevention, prior statin therapy before ACS was associated with milder ACS presentation and lower in-hospital major adverse cardiovascular events (MACE).19 However, the data regarding previous statin or pre-hospital statin treatment and arrhythmia in ACS are scarce. Also, the benefit of previous statin use in reducing arrhythmia events during ACS hospitalization period is still conflicting.20, 21, 22 Therefore we aim to evaluate the role of previous statin use and in-hospital arrhythmia during acute coronary syndrome.
2. Methods
2.1. Protocol and registration
This study is registered in the International Prospective Register of Systematic Reviews (PROSPERO) by the following number: CRD42022336402.
2.2. Search strategy
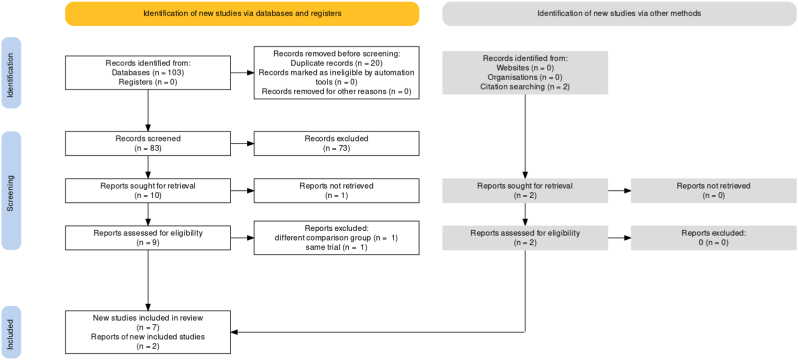
We conducted a structured search to identify research on prior statin use and in-hospital arrhythmia in acute coronary syndrome according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement guideline, with a pre-determined search strategy. The structured search process can be seen in Fig. 1. We systematically searched Pubmed, Proquest, EBSCOhost, and Clinicaltrial.gov databases from inception to June 2022. We combined the search strategy using MeSH terms and [Title/Abstract] with the following keywords: “prior statin”, “previous statin”, “pre-hospital statin”, “arrhythmia”, “arrhythmic”, “supraventricular arrhythmia”, “ventricular arrhythmia”, “atrial fibrillation”, “atrial flutter”, “ventricular tachycardia”, “ventricular fibrillation”, “atrioventricular block”, myocardial infarction”, and “acute coronary syndrome”.
Fig. 1.
PRISMA flow diagram.
2.3. Eligibility criteria and outcome of interest
After searching, all retrieved studies were exported into Zotero. Duplicate studies were removed. Our inclusion criteria were: (1) acute coronary syndrome patients >18 years old; (2) comparing patients with prior statin use and patients without prior statin use. Studies were excluded if they met the following criteria: (1) non-English article; (2) article with study designs such as the letter to the editor, literature review, systematic review, meta-analysis, case report, case series, or correspondence. If there was two or more published article from one trial with the same outcome of interest, the longer study duration was chosen. The outcome of interest was the incidence of arrhythmia.
2.4. Study selection and data collection
Two independent investigators conducted the literature search (KW and RD). We also manually screened for additional eligible studies from the related articles and the references in the relevant studies. Any differences were solved through a discussion. If there is a disagreement between two investigators, the third investigator (KSN) will be asked to make the final decision.
Articles were reviewed based on title, abstract, and full text. After identifying the included studies, data extraction was performed. The following data were extracted from the included studies: first author, publication year, comorbidities (angina, old myocardial infarction, heart failure, hypertension, diabetes mellitus, chronic renal failure, current smoker), left ventricular ejection fraction, final diagnosis (unstable angina [UA], non-ST segment elevation myocardial infarction [NSTEMI], ST-segment elevation myocardial infarction [STEMI]), the minimum duration of statin treatment before admission, type of arrhythmia, study design, baseline lipid parameter (low-density lipoprotein [LDL] cholesterol, high-density lipoprotein [HDL] cholesterol, triglyceride, total cholesterol), concomitant medications before admission (aspirin, clopidogrel, beta blocker, angiotensin-converting enzyme [ACE] inhibitor, angiotensin receptor blocker [ARB], spironolactone), and the type of statin. The corresponding author of the studies was contacted via email to request access to missing data with a maximum of two attempts.
2.5. Risk of bias assessment
The Newcastle Ottawa Scale (NOS) was used to assess the risk of bias for cross-sectional, case–control, and cohort studies.23 KW and RD performed this critical appraisal. Any difference was resolved through a discussion. If the agreement was not reached, the opinion of a third reviewer (KSN) was consulted. The articles’ assessment can be seen in Table 1. The NOS consists of 3 evaluation criteria: selection (0–4 points); comparability (0–2); and outcomes assessment (0–3 points). The maximum score from NOS is 9.
Table 1.
Characteristics of the included studies.
| First Author (Year) | Study type | Population | Type of arrhythmia | Outcome | NOS |
|---|---|---|---|---|---|
| Ishii et al (2006) | Retrospective, single center | AMI (STEMI) patients undergoing reperfusion therapy wih emergency PCI | VF in ≤48 h after reperfusion and VT | Resolution on ST-segment elevation on ECG; achievement of TIMI grade 3 flow; corrected TIMI frame count; maximum serum CK level; and the type and frequency of ventricular arrhythmias | 6 |
| Ramani et al (2007) | Single center, observational | Patients with suspected ACS/NSTEMI | New-onset AF or atrial flutter | The occurrence of new-onset AF and atrial flutter | 8 |
| Vedre et al (2009) | Prospective, multicenter, observational cohort | ACS (UA, NSTEMI, STEMI) patients ≥18 years old | CA or VF, sustained VT, AF or atrial flutter | Primary outcomes were in-hospital AF and the composite end point of VT, VF, and/or cardiac arrest | 9 |
| Ozaydin et al (2010) | Observational | ACS (UA, NSTEMI, STEMI) patients admitted to coronary care unit | New-onset AF | The occurrence of in-hospital AF in patients with and without previous paroxysmal AF | 6 |
| Ozaydin et al (2011) | Observational, case-controlled retrospective | ACS (UA, NSTEMI, STEMI) patients admitted to coronary care unit | Sustained VT or VF | The occurrence of sustained VT or VF | 7 |
| Apiyasawat et al (2013) | Prospective, multicenter, observational cohort | ACS (UA, NSTEMI, STEMI) patients ≥18 years old | Sustained VT or VF | Primary outcome was the occurrence of VA Secondary outcome was a composite endpoint of VA or cardiac death |
8 |
| Marenzi et al (2015) | Prospective, single center | STEMI patients who underwent primary PCI | VT or VF, high-degree conduction disturbances requiring pacemaker | Primary outcomes were infarct size and myocardial salvage index Secondary endpoint was troponin I peak value |
5 |
| Li et al (2016) | Prospective, multicenter | ACS (NSTEMI and STEMI) patients ≥18 years old | In-hospital persistent VT or VT or Mobitz type II or III AV block | ACS severity at presentation, major arrhythmia, MACE (all-cause mortality, non-fatal or reoccurred MI, non-fatal stroke) | 9 |
| Park et al (2018) | Prospective, multicenter, observational | ACS (NSTEMI and STEMI) patients ≥18 years old with successful PCI | VT, VF, and AV block | Primary outcome was the incidence and rate of ventricular tachyarrhythmia and mortality during the index period Secondary endpoint were cardiovascular death and MACEs (all-cause death, recurrent MI, and any revascularization during follow-up) |
9 |
ACS = acute coronary syndrome; AF = atrial fibrillation; AMI = acute myocardial infarction; AV = atrioventricular; CA = cardiac arrest; MACE = major adverse cardiovascular event; MI = myocardial infarction; NOS = newcastle Ottawa scale; NSTEMI = non-ST segment elevation myocardial infarction; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction; UA = unstable angina; VF = ventricular fibrillation, VT = ventricular tachycardia.
2.6. Statistical analysis
For each included study, the data regarding incidence of arrhythmia were expressed as odds ratio (OR) and 95% confidence intervals (95% CI). A random-effect model was used assuming there will be a significant heterogeneity. The heterogeneity between studies was measured by the I2 value and the I2 value is interpreted as: 0–25% (heterogeneity might not be important); 25–75% (moderate heterogeneity); and 75–100% (considerable heterogeneity).24 Subgroup analysis according to the type of arrhythmia will be performed with sufficient studies. Text and tables were used to provide a descriptive summary and explanation of the findings of the included studies. If there is a minimum 10 included studies, the funnel plot will be used and a meta-regression will be performed. The meta-analysis was performed using Review Manager (Revman) version 5.4. Sensitivity analysis was conducted to study the robustness and to detect the source heterogeneity by using leave one or two out methods.25,26 Eight out of nine included studies used chi-square test or fisher exact test as appropriate to analyze categorical outcome variables.20, 21, 22,27, 28, 29, 30,32 One included study did not specifically mention the statistical method to analyze categorical outcome variables.31
3. Results
Nine eligible studies with a total of 86,795 patients with the acute coronary syndrome were included and only one study reported patients with suspected ACS.20, 21, 22,27, 28, 29, 30, 31, 32 A total of 22,130 (25.5%) patients had consumed statin before the index ACS event. The included studies were published between 2006 and 2018. The characteristics of the included studies are summarized in Table 1. Overall, comorbidities such as old myocardial infarction (MI), heart failure (HF), hypertension, diabetes mellitus (DM), and chronic renal failure were more common in ACS patients with prior statin use compared to ACS patients without prior statin, as seen in Table 2. Left ventricular ejection fraction (LVEF) was comparable between both groups, except from 2 studies.29,30 For final diagnosis during hospitalization, STEMI was more frequent in patients without prior statin use compared to patients with prior statin use. Quality assessment of the included studies can also be seen in Table 1. The reported in-hospital arrhythmias were new-onset AF, new-onset atrial flutter, in-hospital AF or atrial flutter, sustained ventricular tachycardia (VT), ventricular fibrillation (VF), and 2nd or 3rd degree AV block.
Table 2.
Basic demographic of the included studies.
| First Author (Year) |
Ishii et al (2006) |
Ramani et al (2007) |
Vedre et al (2009) |
Ozaydin et al (2010) |
Ozaydin et al (2011) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group (n) | Prior statin (40) | No statin (346) | Prior statin (601) | No statin (925) | Prior statin (17,636) | No statin (47,043) | Prior statin (241) | No statin (759) | Prior statin (241) | No statin (759) |
| Age (years) | 65 ± 10 | 63 ± 10 | NA | NA | 67 (58–76)a | 64 (55–76) | 61 ± 11 | 61 ± 11 | 62 ± 11 | 62 ± 12 |
| Male, n (%) | 29 (72.5) | 282 (81.5) | NA | NA | 11,811 (67) | 31,528 (67) | 158 (65.6)a | 597 (78.7) | 158 (65.6)a | 597 (78.7) |
| Angina, n (%) | NA | NA | NA | NA | 12,137 (69)a | 21,562 (46) | NA | NA | NA | NA |
| Old MI, n (%) | NA | NA | NA | NA | NA | NA | 1 (0.4) | 5 (0.7) | 1 (0.4) | 5 (0.7) |
| Heart failure, n (%) | NA | NA | NA | NA | 2629 (15)a | 3931 (8.4) | 14 (5.8) | 45 (5.9) | 14 (5.8) | 45 (5.9) |
| Hypertension, n (%) | 14 (35) | 104 (30.1) | NA | NA | 12,988 (74)a | 26,893 (58) | 173 (71.8)a | 377 (49.7) | 173 (71.8)a | 377 (49.7) |
| Diabetes mellitus, n (%) | 15 (37.5) | 111 (32.1) | NA | NA | 5838 (34)a | 10,268 (22) | 77 (32)a | 159 (20.9) | 77 (32)a | 159 (20.9) |
| Chronic renal failure, n (%) | NA | NA | NA | NA | 1925 (11)a | 2957 (6.3) | 1 (1.7) | 4 (0.5) | 1 (1.7) | 4 (0.5) |
| Current smoker, n (%) | 12 (30) | 136 (39.3) | NA | NA | NA | NA | 120 (49.8) | 423 (55.7) | 120 (49.8) | 423 (55.7) |
| LVEF (%) | NA | NA | NA | NA | NA | NA | 46 ± 13 (20–75)a | 41 ± 11 (20–70) | 46 ± 13 (20–75)a | 41 ± 11 (20–70) |
| Final diagnosis | ||||||||||
| Unstable angina, n (%) | NA | NA | NA | NA | 7588 (43)a | 12,272 (26) | 180 (74.7)ba | 369 (48.6) | 180 (74.7)ba | 369 (48.6) |
| NSTEMI, n (%) | NA | NA | NA | NA | 6304 (36)a | 14,938 (32) | ||||
| STEMI, n (%) | 40 (100) | 346 (100) | NA | NA | 3744 (21)a | 19,833 (42) | 61 (25.3)a | 390 (51.4) | 61 (25.3)a | 390 (51.4) |
| Minimum duration of statin treatment before admission | ≥1 month | – | NA | – | ≥7 days | – | NA | – | NA | – |
|
Table 2 (continued). Baseline characteristics | ||||||||
|---|---|---|---|---|---|---|---|---|
| First Author (Year) |
Apiyasawat et al (2013) |
Marenzi et al (2015) |
Li et al (2016) |
Park et al (2018) |
||||
| Group (n) | Prior statin (525) | No statin (1482) | Prior statin (50) | No statin (148) | Prior statin (1973) | No statin (12,817) | Prior statin (823) | No statin (354) |
| Age (years) | 66.7 ± 10.8a | 62.4 ± 13.3 | 63 ± 10 | 60 ± 11 | 64.4 ± 11.2a | 63.8 ± 11.9 | 63 (55–72)a | 55.5 (48–66) |
| Male, n (%) | 309 (58)a | 1048 (70.6) | 42 (84) | 141 (78) | 1371 (69.5) | 8908 (69.5) | 588 (71.5)a | 297 (83.9) |
| Angina, n (%) | NA | NA | NA | NA | 1294 (65.6)a | 4819 (37.6) | 165 (20.1)a | 23 (6.5) |
| Old MI, n (%) | 202 (38.5)a | 111 (7.5) | 19 (38)a | 7 (4) | 616 (31.2)a | 1192 (9.3) | 165 (20.1)a | 23 (6.5) |
| Heart failure, n (%) | 164 (31.2)a | 100 (6.7) | NA | NA | 213 (10.8)a | 705 (5.5) | 24 (2.9) | 2 (0.6) |
| Hypertension, n (%) | 436 (83)a | 759 (51.2) | 29 (58) | 77 (43) | 1273 (64.5)a | 7216 (56.3) | 570 (69.3)a | 93 (26.3) |
| Diabetes mellitus, n (%) | 322 (61.3)a | 696 (47) | 11 (22)a | 15 (8) | 527 (26.7)a | 2499 (19.5) | 350 (42.5)a | 86 (24.3) |
| Chronic renal failure, n (%) | 115 (21.9)a | 78 (5.3) | NA | NA | NA | NA | NA | NA |
| Current smoker, n (%) | 72 (13.7)a | 572 (38.6) | 32 (64) | 111 (62) | 442 (22.4)a | 4153 (32.4) | 273 (33.2)a | 189 (53.4) |
| LVEF (%) | 49.2 ± 15 | 48.7 ± 14 | 50 ± 11 | 49 ± 12 | NA | NA | 54 (46–60) | 55 (47–61.5) |
| Final diagnosis | ||||||||
| Unstable angina, n (%) | 116 (22.1)a | 125 (8.4) | 0 | 0 | NA | NA | NA | NA |
| NSTEMI, n (%) | 258 (49.1)a | 406 (27.4) | 0 | 0 | 1572 (79.7) | 7370 (57.5) | 436 (53.1)a | 147 (41.6) |
| STEMI, n (%) | 151 (28.8)a | 951 (64.2) | 50 | 180 | 401 (20.3)c | 5447 (42.5) | 374 (45.6)a | 200 (56.7) |
| Minimum duration of statin treatment before admission (days) | ≥7 days | – | >6 months | – | ≥28 days | – | NA | – |
LVEF = left ventricular ejection fraction; MI = old myocardial infarction; NA = not available; NSTEMI = non-ST segment elevation myocardial infarction; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction; UA = unstable angina.
=P ≤ 0.05 for the differences according to the respective study.
= unstable angina or NSTEMI.
= P ≤ 0.05 compared to NSTEMI.
The minimum duration between statin initiation and index ACS event can be seen in Table 2, which varies from ≥7 days to >6 months. The reported statins were rosuvastatin, atorvastatin, pravastatin, fluvastatin, and simvastatin. However, only 1 study reported the average statin dose which was 22 ± 10 mg/day.21 No studies reported a specific dose for each statin. The duration between statin initiation and index ACS event was reported in 3 studies.21,29,30 In new-onset AF and sustained VT or VF, the duration between statin initiation and index ACS event was 258 ± 256 days.29,30 In VT or VF and high-degree conduction disturbances requiring a pacemaker, the duration between statin initiation and index ACS event was 5 ± 3.5 years.21
The baseline lipid parameter can be seen in Table 3. Overall, patients with prior statin use presented with lower LDL and total cholesterol level compared to patients without prior statin. This difference might explain patients’ compliance regarding statin use which resulted in lower LDL and total cholesterol level. The number of ACS patients who had concomitant medication use such as aspirin, clopidogrel, beta blocker, angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB), and spironolactone were more frequent in patients with prior statin use compared to patients without prior statin.
Table 3.
Baseline lipid parameter and concomitant medications before admission.
| First Author (Year) |
Ishii et al (2006) |
Ramani et al (2007) |
Vedre et al (2009) |
Ozaydin et al (2010) |
Ozaydin et al (2011) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group (n) | Prior statin (40) | No statin (346) | Prior statin | No statin | Prior statin | No statin | Prior statin (241) | No statin (759) | Prior statin (241) | No statin (759) |
| Baseline lipid parameter | ||||||||||
| LDL cholesterol (mg/dL) | NA | NA | NA | NA | NA | NA | NA | NA | 94 ± 41a | 111 ± 49 |
| HDL cholesterol (mg/dL) | 48 ± 11 | 44 ± 12 | NA | NA | NA | NA | NA | NA | 40 ± 9 | 30 ± 10 |
| Triglyceride (mg/dL) | 165 ± 137 | 127 ± 152 | NA | NA | NA | NA | NA | NA | 147 ± 65 | 147 ± 68 |
| Total cholesterol (mg/dL) | 208 ± 33 | 199 ± 57 | NA | NA | 164 ± 46a | 199 ± 49 | NA | NA | 172 ± 46a | 186 ± 41 |
| Concomitant medications before admission | ||||||||||
| Aspirin, n (%) | 11 (27.5)a | 33 (9.5) | NA | NA | NA | NA | 198 (82.2)a | 281 (37) | 198 (82.2)a | 281 (37) |
| Clopidogrel, n (%) | NA | NA | NA | NA | NA | NA | NA | NA | 23 (9.5) | 28 (3.6) |
| Beta blocker, n (%) | 3 (7.5)a | 4 (1.2) | NA | NA | NA | NA | 127 (52.7)a | 137 (18.1) | 127 (52.7)a | 137 (18.1) |
| ACE Inhibitor or ARB, n (%) | 6 (15)a | 16 (4.6) | NA | NA | NA | NA | 121 (50.2)a | 170 (22.4) | 121 (50.2)a | 170 (22.4) |
| Spironolactone, n (%) | NA | NA | NA | NA | NA | NA | NA | NA | 14 (5.8) | 28 (3.6) |
| Rosuvastatin, n (%) | – | – | NA | – | NA | – | 9 (3.7) | – | 9 (3.7) | – |
| Atorvastatin, n (%) | 2 (5) | – | NA | – | NA | – | 154 (63.9) | – | 154 (63.9) | – |
| Pravastatin, n (%) | 25 (62.5) | – | NA | – | NA | – | 10 (4.2) | – | 10 (4.2) | – |
| Fluvastatin, n (%) | 3 (7.5) | – | NA | – | NA | – | 27 (11.2) | – | 27 (11.2) | – |
| Simvastatin, n (%) | 2 (5) | – | NA | – | NA | – | 41 (17) | – | 41 (17) | – |
|
Table 3 (continued). Baseline lipid parameter and concomitant medications before admission | ||||||||
|---|---|---|---|---|---|---|---|---|
| First Author (Year) |
Apiyasawat et al (2013) |
Marenzi et al (2015) |
Li et al (2016) |
Park et al (2018) |
||||
| Group (n) | Prior statin (525) | No statin (1482) | Prior statin (50) | No statin (148) | Prior statin (1973) | No statin (12,817) | Prior statin (823) | No statin (354) |
| Baseline lipid parameter | ||||||||
| LDL cholesterol (mg/dL) | NA | NA | 106 (78–123)a | 127 (102–149) | NA | NA | 91 (69–116)a | 129 (104–162) |
| HDL cholesterol (mg/dL) | NA | NA | 43 (36–51) | 40 (34–46) | NA | NA | 42 (36–50) | 41 (35–48) |
| Triglyceride (mg/dL) | NA | NA | 107 (77–149) | 110 (74–154) | NA | NA | 114 (76–168)a | 131 (85–213) |
| Total cholesterol (mg/dL) | NA | NA | 170 (145–193)a | 193 (168–220) | NA | NA | NA | NA |
| Concomitant medications before admission | ||||||||
| Aspirin, n (%) | 386 (73.5)a | 170 (11.5) | 32 (64)a | 66 (37) | NA | NA | NA | NA |
| Clopidogrel, n (%) | 122 (23.2)a | 29 (2) | NA | NA | NA | NA | NA | NA |
| Beta blocker, n (%) | 264 (50.3)a | 138 (9.3) | 18 (36)a | 19 (11) | NA | NA | NA | NA |
| ACE Inhibitor or ARB, n (%) | 191 (36.4)a | 114 (7.7) | 20 (40) | 47 (23) | NA | NA | NA | NA |
| Spironolactone, n (%) | NA | NA | NA | NA | NA | NA | NA | NA |
| Rosuvastatin, n (%) | NA | – | 11 (22) | – | NA | – | NA | – |
| Atorvastatin, n (%) | NA | – | 23 (46) | – | NA | – | NA | – |
| Pravastatin, n (%) | NA | – | 1 (2) | – | NA | – | NA | – |
| Fluvastatin, n (%) | NA | – | NA | – | NA | – | NA | – |
| Simvastatin, n (%) | NA | – | 15 (30) | – | NA | – | NA | – |
ACE = angiotensin converting enzyme; ARB = angiotensin receptor blocker; HDL = high density lipoprotein; LDL = low density lipoprotein; NA = not available.
= P ≤ 0.05 for the differences according to the respective study.
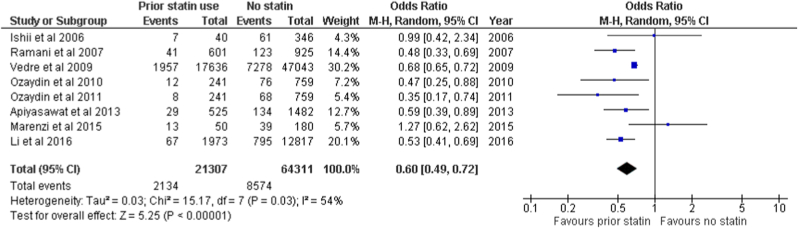
The forest plot for the incidence of overall arrhythmia can be seen in Fig. 2A. Only 8 studies with a total 85,618 patients were involved in the meta-analysis. The random-effects model was used since there was a moderate heterogeneity (P = 0.03; I2 = 54%). The pooled analysis showed that the incidence of in-hospital arrhythmia during ACS was significantly lower in patients with prior statin use compared to patients without prior statin use (OR 0.60; 95% CI 0.49–0.72; P < 0.00001).
Fig. 2.
Arrhythmia in acute coronary syndrome.
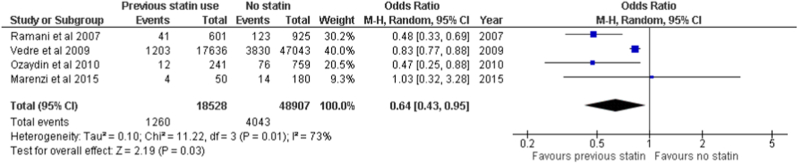
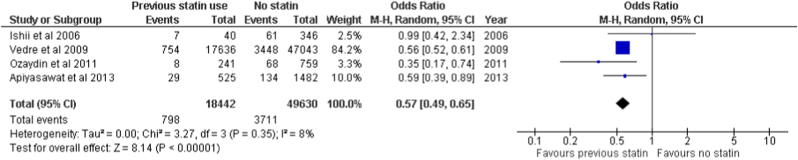
The subgroup analysis was performed in AF or atrial flutter and ventricular arrhythmia (VA). The VA consists of ventricular tachycardia or ventricular fibrillation. In AF or atrial flutter, the pooled analysis found that the incidence of AF or atrial flutter in ACS was significantly lower in patients with prior statin use compared to patients without prior statin use (OR 0.64; 95% CI 0.43–0.95; P = 0.03). Moderate heterogeneity was also observed in ACS patients with AF or atrial flutter (P = 0.01; I2 = 73%) and can be seen in Fig. 2B. In VA, the pooled analysis found that the incidence of VA in ACS was significantly lower in patients with prior statin use compared to patients without prior statin use (OR 0.57; 95% CI 0.49–0.65; P < 0.00001). Low heterogeneity was observed in a subgroup of ACS patients with VA (P = 0.35; I2 = 8%) and can be seen in Fig. 2C.
Moderate heterogeneity was observed in the incidence of overall arrhythmia and AF or atrial flutter. In the incidence of arrhythmia, sensitivity analysis was performed by excluding Vedre et al study. The heterogeneity reduced to 36% and the association remained significant (OR 0.57; 95% CI 0.45–0.71; P < 0.00001) (Supplementary Fig. 1). By further excluding Marenzi et al, the heterogeneity of overall arrhythmia reduced to 0% and the association remained significant (OR 0.53; 95% CI 0.44–0.62; P < 0.00001) (Supplementary Fig. 2). For AF or atrial flutter, sensitivity analysis was conducted by excluding Vedre et al study. The heterogeneity of AF or atrial flutter reduced to 0% and the association remained significant (OR 0.50; 95% CI 0.37–0.68; P < 0.00001) (Supplementary Fig. 3).
4. Discussion
From this meta-analysis, prior statin use was significantly associated with a lower incidence of in-hospital arrhythmia during ACS. The benefit of statin in reducing the incidence of AF or atrial flutter and VT or VF was supported by the subgroup analysis, as seen in Fig. 3, Fig. 4. The spectrum of AF ranged from new-onset AF in 2 studies27,29 and in-hospital AF from patients with a history of AF in 1 study.28 One study did not define the type of AF.21 Two studies reported no difference in the incidence of arrhythmia.20,21 However, the incidence of arrhythmia was not the primary endpoint of both studies.20,21
Fig. 3.
Atrial fibrillation or atrial flutter.
Fig. 4.
Ventricular tachycardia or fibrillation.
The reduction of high-degree AV block varies between the two studies. In one study, the incidence of high-degree AV block was comparable between prior statin use and without prior statin use.21 Another study reported a significantly lower incidence of high-degree AV block in ACS patients with prior statin use compared to ACS patients without prior statin use. However, this study defined the outcome of major arrhythmia as persistent VT or VF or Mobitz type II or III AV Block.31 Therefore, we can not conclude that previous statin can reduce the incidence of II or III-degree AV block in patients with ACS.
Only one previous meta-analysis reported the benefits of the previous statin and the incidence of AF in ACS,33 and our subgroup analysis in AF or atrial flutter was in line with a previous meta-analysis. A 35% reduction in the risk of new-onset or recurrence AF was reported in ACS patients with prior statin use.33 We noticed that the previous meta-analysis also included several same studies. From our inclusion criteria, another study was included. However, the included study did not assess AF or atrial flutter as its primary endpoint. Also, two randomized controlled trials (RCTs) from the early 2000s comparing statin and placebo in patients with previous MI and UA or non-Q wave MI did not assess previous statin use and the incidence of arrhythmia during ACS.34,35
The benefit of statins beyond the lipid-lowering effect is well known.10,15 Statin possesses anti-inflammatory, anti-thrombotic, anti-proliferative, and anti-oxidant effect.18,36, 37, 38 These pleiotropic effects may directly or indirectly reduce the incidence of ventricular arrhythmia (VA).18 Statin can lower the incidence of VA in ACS by reducing sarcoplasmic injury, intracellular calcium overload, and late ventricular potential in diseased myocardium.36,39
Other than VA, statin can also reduce the incidence of AF in patients with concomitant coronary artery disease (CAD).40 Pravastatin, atorvastatin, and simvastatin can reduce the incidence of AF in stabilized ACS patients and the reduction was not dose-dependent.40 The possible mechanisms of new-onset AF in ACS are neurohormonal and autonomic nervous changes and/or changes in the atrial substrate due to atrial ischemia.41,42 Other than the anti-inflammatory effect, statin can increase the bioavailability of nitric oxide (NO), which can protect the atrial myocardium during atrial ischemia.38 This effect can further slow or reverse structural remodeling in AF patients.38
Other than a statin, LVEF and concomitant drugs may impact the incidence of arrhythmia. Concomitant treatment with aspirin, clopidogrel, beta blocker, and ACE Inhibitor or ARB was higher in ACS patients with prior statin use compared to ACS patients without statin. Beta-blockers can reduce the incidence of AF and VA during ACS, while the benefit of ACE inhibitors or ARB in reducing the incidence of AF or VA during ACS is unclear.18,43, 44, 45 Of note, the concomitant use of beta blocker and Renin-Angiotensin-Aldosterone (RAAS) Blocker in previos statin group from included studies varied from 7.5 to 52.7% and 15–50.2%, respectively (Table 3). The possibilities of interaction among statin, beta blocker, and ACE Inhibitor or ARB still remain, and the benefit of arrhythmia reduction in prior statin use may not solely be due to statin. Two studies reported a significant difference in LVEF between statin and non-statin groups.29,30 The LVEF was significantly higher in ACS patients with prior statin use than those without prior statin use and may be a confounding factor in the incidence of arrhythmia.
Moderate heterogeneity was observed from Vedre et al and Marenzi et al.21,28 The potential source of heterogeneity may be due to the concomitant routine medication and the type of statin, which was not reported from Vedre et al study. Also, the primary endpoint of Marenzi et al was not the incidence of arrhythmia, which may become a potential source of heterogeneity. Other than that, the comorbidities may impact the heterogeneity.
There are several limitations in our meta-analysis. Not all studies assess the incidence of arrhythmia as a primary endpoint. We could not assess the type of statin (lipophilic or hydrophilic), dose, and duration of statin treatment due to minimum data. Moreover, our meta-analysis only reported the incidence of in-hospital arrhythmia. Whether prior statin use can reduce the long-term incidence of arrhythmia is still unknown. Also, we only included the article in English, which may not represent the whole population. Several covariates, such as age, LVEF, and concomitant medication with antiarrhythmic potential (beta blocker and ACE-inhibitor), may confound the incidence of arrhythmia. However, we could not perform a meta-regression analysis to investigate the effect of the covariates. In addition, the meta-analysis was only performed based on aggregate-patient data and we weren't able to obtain individual-patient data from all included studies. Thus, we weren't able to perform meta-analysis based on individual-patient data.
5. Conclusions
Based on aggregate-patient data, prior statin use may reduce the incidence of in-hospital arrhythmia during acute coronary syndrome, particularly in new-onset atrial fibrillation or atrial flutter and ventricular tachycardia or ventricular fibrillation. Statin may not solely reduce the incidence of in-hospital arrhythmia during acute coronary syndrome due to concomitant use of beta-blocker and RAAS Blocker. Further studies are needed to confirm this finding and assess the association between statin type, dose, and duration with the incidence of in-hospital arrhythmia during acute coronary syndrome.
Funding
There is no funding in this review.
Authors' contributions
KW conceived and designed the study. KW and RD performed study selection. KW performed data extraction and interpreted the data. KW, RD, and KSN performed extensive search of relevant topics. KW performed statistical analysis. PAS, SS, and YA performed review and extensive editing of the manuscript. All authors contributed significantly to the writing of the manuscript. All authors approved the final manuscript.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Acknowledgements
There is no acknowledgements in this review.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2023.01.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Hodzic E., Perla S., Iglica A., Vucijak M. Seasonal incidence of acute coronary syndrome and its features. Mater Sociomed. 2018;30(1):10–14. doi: 10.5455/msm.2018.30.10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatt D.L., Lopes R.D., Harrington R.A. Diagnosis and treatment of acute coronary syndromes: a review. JAMA. 2022;327(7):662–675. doi: 10.1001/jama.2022.0358. [DOI] [PubMed] [Google Scholar]
- 3.Gorenek B., Blomström Lundqvist C., Brugada Terradellas J., et al. Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EHRA, ACCA, and EAPCI task force. EP Europace. 2014;16(11):1655–1673. doi: 10.1093/europace/euu208. [DOI] [PubMed] [Google Scholar]
- 4.Winkler C., Funk M., Schindler D.M., Hemsey J.Z., Lampert R., Drew B.J. Arrhythmias in patients with acute coronary syndrome in the first 24 hours of hospitalization. Heart Lung. 2013;42(6) doi: 10.1016/j.hrtlng.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Avezum Á., Piegas L.S., Goldberg R.J., et al. Magnitude and prognosis associated with ventricular arrhythmias in patients hospitalized with acute coronary syndromes (from the GRACE registry) Am J Cardiol. 2008;102(12):1577–1582. doi: 10.1016/j.amjcard.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 6.Piccini J.P., White J.A., Mehta R.H., et al. Sustained ventricular tachycardia and ventricular fibrillation complicating non–ST-segment–elevation acute coronary syndromes. Circulation. 2012;126(1):41–49. doi: 10.1161/CIRCULATIONAHA.111.071860. [DOI] [PubMed] [Google Scholar]
- 7.Singh S.M., FitzGerald G., Yan A.T., et al. High-grade atrioventricular block in acute coronary syndromes: insights from the Global Registry of Acute Coronary Events. Eur Heart J. 2015;36(16):976–983. doi: 10.1093/eurheartj/ehu357. [DOI] [PubMed] [Google Scholar]
- 8.Aguiar Rosa S., Timóteo A.T., Ferreira L., et al. Complete atrioventricular block in acute coronary syndrome: prevalence, characterisation and implication on outcome. Eur Heart J Acute Cardiovasc Care. 2018;7(3):218–223. doi: 10.1177/2048872617716387. [DOI] [PubMed] [Google Scholar]
- 9.Almendro-Delia M., Valle-Caballero M.J., Garcia-Rubira J.C., et al. Prognostic impact of atrial fibrillation in acute coronary syndromes: results from the ARIAM registry. Eur Heart J Acute Cardiovasc Care. 2014;3(2):141–148. doi: 10.1177/2048872613517370. [DOI] [PubMed] [Google Scholar]
- 10.Oesterle A., Laufs U., Liao J.K. Pleiotropic effects of statins on the cardiovascular system. Circ Res. 2017;120(1):229–243. doi: 10.1161/CIRCRESAHA.116.308537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ibanez B., James S., Agewall S., et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2017;39(2):119–177. doi: 10.1093/eurheartj/ehx393. 2018. [DOI] [PubMed] [Google Scholar]
- 12.Collet J.P., Thiele H., Barbato E., et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2020;42(14):1289–1367. doi: 10.1093/eurheartj/ehaa575. 2021. [DOI] [PubMed] [Google Scholar]
- 13.O'Gara P.T., Kushner F.G., Ascheim D.D., et al. ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation. 2013;127(4):e362–e425. doi: 10.1161/CIR.0b013e3182742cf6. 2013. [DOI] [PubMed] [Google Scholar]
- 14.Amsterdam E.A., Wenger N.K., Brindis R.G., et al. AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes. Circulation. 2014;130(25):e344–e426. doi: 10.1161/CIR.0000000000000134. 2014. [DOI] [PubMed] [Google Scholar]
- 15.Kavalipati N., Shah J., Ramakrishan A., Vasnawala H. Pleiotropic effects of statins. Indian J Endocrinol Metab. 2015;19(5):554–562. doi: 10.4103/2230-8210.163106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Danchin N., Fauchier L., Marijon E., et al. Impact of early statin therapy on development of atrial fibrillation at the acute stage of myocardial infarction: data from the FAST-MI register. Heart. 2010;96(22):1809–1814. doi: 10.1136/hrt.2010.201574. [DOI] [PubMed] [Google Scholar]
- 17.He X zhi, Zhou S hua, hong Wan X., Wang H yu, Zhong Q hua, Xue J fang. The effect of early and intensive statin therapy on ventricular premature beat or non-sustained ventricular tachycardia in patients with acute coronary syndrome. Cardiol J. 2010;17(4):381–385. [PubMed] [Google Scholar]
- 18.Abuissa H., O'Keefe J.H., Bybee K.A. Statins as anti-arrhythmics: a systematic review Part II: effects on risk of ventricular arrhythmias. Clin Cardiol. 2009;32(10):549–552. doi: 10.1002/clc.20435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yun K.H., Shin I.S., Shin S.N., et al. Effect of previous statin therapy in patients with acute coronary syndrome and percutaneous coronary intervention. Korean Circ J. 2011;41(8):458–463. doi: 10.4070/kcj.2011.41.8.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ishii H., Ichimiya S., Kanashiro M., et al. Effects of receipt of chronic statin therapy before the onset of acute myocardial infarction: a retrospective study in patients undergoing primary percutaneous coronary intervention. Clin Therapeut. 2006;28(11):1812–1819. doi: 10.1016/j.clinthera.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Marenzi G., Cosentino N., Cortinovis S., et al. Myocardial infarct size in patients on long-term statin therapy undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction. Am J Cardiol. 2015;116(12):1791–1797. doi: 10.1016/j.amjcard.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 22.Apiyasawat S., Sritara P., Ngarmukos T., Sriratanasathavorn C., Kasemsuwan P. Association of statin therapy with ventricular arrhythmias among patients with acute coronary syndrome. Heart Asia. 2013;5(1):39–41. doi: 10.1136/heartasia-2012-010225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luchini C., Stubbs B., Solmi M., Veronese N. Assessing the quality of studies in meta-analyses: advantages and limitations of the newcastle Ottawa scale. World J Meta-Anal. 2017;5(4):80–84. doi: 10.13105/wjma.v5.i4.80. [DOI] [Google Scholar]
- 24.Higgins J.P.T., Thomas J., Chandler J., et al., editors. Cochrane Handbook for Systematic Reviews of Interventions. 2021. www.training.cochrane.org/handbook version 6.2 (updated February 2021). Cochrane. Available from: [Google Scholar]
- 25.Jamialahmadi T., Alidadi M., Atkin S.L., et al. Effect of bariatric surgery on flow-mediated vasodilation as a measure of endothelial function: a systematic review and meta-analysis. J Clin Med. 2022;11(14):4054. doi: 10.3390/jcm11144054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patsopoulos N.A., Evangelou E., Ioannidis J.P. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramani G., Zahid M., Good C.B., Macioce A., Sonel A.F. Comparison of frequency of new-onset atrial fibrillation or flutter in patients on statins versus not on statins presenting with suspected acute coronary syndrome. Am J Cardiol. 2007;100(3):404–405. doi: 10.1016/j.amjcard.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 28.Vedre A., Gurm H.S., Froehlich J.B., et al. Impact of prior statin therapy on arrhythmic events in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;104(12):1613–1617. doi: 10.1016/j.amjcard.2009.07.045. [DOI] [PubMed] [Google Scholar]
- 29.Ozaydin M., Turker Y., Erdogan D., et al. The association between previous statin use and development of atrial fibrillation in patients presenting with acute coronary syndrome. Int J Cardiol. 2010;141(2):147–150. doi: 10.1016/j.ijcard.2008.11.172. [DOI] [PubMed] [Google Scholar]
- 30.Ozaydın M., Türker Y., Erdoğan D., et al. Effect of previous statin use on the incidence of sustained ventricular tachycardia and ventricular fibrillation in patients presenting with acute coronary syndrome. Anadolu Kardiyol Derg. 2011;11(1):22–28. doi: 10.5152/akd.2011.005. [DOI] [PubMed] [Google Scholar]
- 31.Li M., Huang Y., Du X., et al. Impact of prior use of four preventive medications on outcomes in patients hospitalized for acute coronary syndrome--results from CPACS-2 study. PLoS One. 2016;11(9) doi: 10.1371/journal.pone.0163068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park J.S., Kim B.W., Hong T.J., et al. Lower in-hospital ventricular tachyarrhythmia in patients with acute myocardial infarction receiving prior statin therapy. Angiology. 2018;69(10):892–899. doi: 10.1177/0003319718775902. [DOI] [PubMed] [Google Scholar]
- 33.Zhou X., Du J lin, Yuan J., qing Chen Y. Statins therapy can reduce the risk of atrial fibrillation in patients with acute coronary syndrome: a meta-analysis. Int J Med Sci. 2013;10(2):198–205. doi: 10.7150/ijms.5248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwartz G.G., Olsson A.G., Ezekowitz M.D., et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001;285(13):1711–1718. doi: 10.1001/jama.285.13.1711. [DOI] [PubMed] [Google Scholar]
- 35.Pedersen T.R., Faergeman O., Kastelein J.J.P., et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005;294(19):2437–2445. doi: 10.1001/jama.294.19.2437. [DOI] [PubMed] [Google Scholar]
- 36.Beri A., Contractor T., Khasnis A., Thakur R. Statins and the reduction of sudden cardiac death. Am J Cardiovasc Drugs. 2010;10(3):155–164. doi: 10.2165/11536690-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 37.Dawe D.E., Ariyarajah V., Khadem A. Is there a role for statins in atrial fibrillation? Pacing Clin Electrophysiol. 2009;32(8):1063–1072. doi: 10.1111/j.1540-8159.2009.02440.x. [DOI] [PubMed] [Google Scholar]
- 38.Hadi H.A., Mahmeed W.A., Suwaidi J.A., Ellahham S. Pleiotropic effects of statins in atrial fibrillation patients: the evidence. Vasc Health Risk Manag. 2009;5(3):533–551. doi: 10.2147/vhrm.s4841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kostapanos M.S., Liberopoulos E.N., Goudevenos J.A., Mikhailidis D.P., Elisaf M.S. Do statins have an antiarrhythmic activity? Cardiovasc Res. 2007;75(1):10–20. doi: 10.1016/j.cardiores.2007.02.029. [DOI] [PubMed] [Google Scholar]
- 40.Beri A., Sural N., Mahajan S.B. Non-atheroprotective effects of statins: a systematic review. Am J Cardiovasc Drugs. 2009;9(6):361–370. doi: 10.2165/11315710-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 41.Rubenstein J.C., Cinquegrani M.P., Wright J. Atrial fibrillation in acute coronary syndrome. J Atr Fibrillation. 2012;5(1):551. doi: 10.4022/jafib.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lau D.H., Sanders P. New-onset atrial fibrillation and acute coronary syndrome. Expet Rev Cardiovasc Ther. 2010;8(7):941–948. doi: 10.1586/erc.10.61. [DOI] [PubMed] [Google Scholar]
- 43.Thomas D.E., Jex N., Thornley A.R. Ventricular arrhythmias in acute coronary syndromes—mechanisms and management. Cont Cardiol Educ. 2017;3(1):22–29. doi: 10.1002/cce2.51. [DOI] [Google Scholar]
- 44.Makkar K.M., Sanoski C.A., Spinler S.A. Role of angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and aldosterone antagonists in the prevention of atrial and ventricular arrhythmias. Pharmacotherapy. 2009;29(1):31–48. doi: 10.1592/phco.29.1.31. [DOI] [PubMed] [Google Scholar]
- 45.Pesaro A.E., de Matos Soeiro A., Serrano C.V., Giraldez R.R., Ladeira R.T., Nicolau J.C. Effect of β-blockers on the risk of atrial fibrillation in patients with acute myocardial infarction. Clinics. 2010;65(3):265–270. doi: 10.1590/S1807-59322010000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.