Summary
Background
On February 2022, Russia invaded Ukraine. Beyond Poland, Romania, Russia, several refugees reached Italy also. In the past, several factors contributed to low vaccination coverage in Ukraine and the occurrence of epidemic outbreaks. The purpose of our study was to analyze the main characteristics of Ukrainian refugees who accessed the Rozzano Vaccination Center (Italy), and the attitude towards proposed vaccinations.
Methods
In March-July 2022, we conducted a cross-sectional study on Ukrainian refugees under the age of 18. On the basis of their vaccination certificates or antibody dosages, the doctor proposed to the parents (or legal guardians) any vaccinations to be carried out on the basis of the Italian childhood vaccination schedule. Refused or accepted vaccinations were registered and the data exported for statistical analysis. COVID-19 vaccination was excluded from the analysis.
Results
27 refugees missed the appointment, so 79 Ukrainian refugees have been included in the study. Females represented the 51.90% of patients; the average age was 7.11 (sd 4.92) years. The most refused vaccinations were: HPV, MMR and men C. Significant differences due to age were found for Men C and Chickenpox acceptance.
Conclusions
The efforts made to ensure complete care and to promote vaccination among refugees, offering them a complete evaluation of the vaccination status and the possibility of being vaccinated for free, seem to be insufficient to convince most refugees to get vaccinated.
Keywords: Ukraine, Vaccine hesitancy, Refugees
Introduction
War causes an enormous amount of deaths and disabilities around the world. It destroys families, communities and cultures, divert scarce resources, disrupts the social infrastructure that supports health. It forces people to leave their homes and to become internally displaced persons or refugees who have fled to other countries [1].
According to UNICEF, about forty percent of partially vaccinated or unvaccinated children live in partially or wholly conflict-affected countries. These children are often the most vulnerable to outbreaks of diseases such as measles and polio, which can cause death or severe disability.
Children in conflict-affected areas lose basic vaccinations due to the failure – and sometimes deliberate destruction – of vital health services [2].
On February 24, 2022, Russia launched a full-scale military invasion of Ukraine. Since then, millions of Ukrainians have fled their homes in search of refuge, especially in neighboring countries such as Poland, Romania and Russia [3].
Italy also welcomed thousands of Ukrainian refugees whose main destinations were the biggest Italian cities such as Milan, Rome, Naples and Bologna [4].
At the end of March 2022 (30th) the Italian authorities had announced that so far about 71,940 Ukrainian refugees had entered the country, of which 37,082 women, 6,661 men and 28,197 minors. About 3,000 Ukrainian refugees had reached Italy every day since the war began.
By the end of April 2022, almost 100,000 Ukrainian refugees arrived in Italy, most of them women and children. Exactly 97,912 people fleeing the war in Ukraine arrived in Italy, of which 50,612 women, 11,833 men and 35,467 minors [4].
Before the war, vaccination rates in Ukraine were among the lowest in Europe. Childhood vaccination coverage has steadily fallen below the WHO target thresholds required to establish herd immunity for some of the most serious diseases. In 2021, 20% of children in Ukraine were not fully vaccinated against measles and 13% were not protected against poliovirus; this percentage is likely to have increased due to the conflict [5].
Likewise, vaccination coverage against COVID-19 has been poor; by February 2022, less than 35% of the general population had received two doses of the vaccine, compared to an average of 65% in the rest of Europe [5].
Several factors have contributed to the low prevalence of vaccination in Ukraine, including widespread hesitancy about the vaccines, fueled in part by social media campaigns that have served to spread vaccine misinformation and undermine public trust in Ukrainian authorities [6].
The World Health Organization (WHO) defined the vaccine hesitancy as a behavior, influenced by a number of factors including issues of confidence (do not trust vaccine or provider), complacency (do not perceive a need for a vaccine, do not value the vaccine), and convenience (access) [7].
Wavering confidence has been compounded by problems with vaccines provision and disruption of immunization services related to the COVID-19 pandemic.
Due to low vaccination coverage, Ukraine has recently experienced vaccine-preventable disease outbreaks. In 2017-2020, Ukraine reported over 115,000 measles cases and 40 measles-related deaths, representing the largest epidemic in Europe in over a decade [8].
An outbreak of type 2 poliovirus was confirmed in 2021. The poliovirus was isolated from over 20 children, two of whom suffered from acute flaccid paralysis [8]. A mass vaccination campaign in response to this outbreak began in February 2022, but was ultimately halted by the Russian invasion, putting Ukraine’s children at risk.
The risk of further vaccine-preventable disease outbreaks has been heightened by the conflict. Ukraine has experienced widespread disruption of health services, including immunization programs. Most internally displaced people flee to rural areas or small towns in Ukraine, which do not have the adequate infrastructure to run disease surveillance programs or vaccination campaigns [9].
Most families who have fled Ukraine include young children, the elderly (aged > 60), or people with chronic illnesses, and many are temporarily housed in crowded shelters. There is therefore a risk that crucial doses of vaccines will be missed or delayed.
The risk of epidemic outbreaks of vaccine-preventable diseases in the structures responsible for welcoming migrants, led the Italian Ministry of Health to provide instructions to the Health Authorities to manage the migratory phenomenon [10], indications that have then been declined in regional and local instructions.
The purpose of our study was therefore to analyze the main characteristics of the Ukrainian refugees who accessed the Rozzano Vaccination Center (Milan, Italy), analyzing some socio-demographic data and the attitude towards proposed vaccinations (acceptance or refusal).
Methods
The so called Azienda Socio Sanitaria Territoriale (ASST, translated as Territorial Social and Health Authority) Melegnano e della Martesana tries to respond to the multiple needs of daily life of the citizens who live and work in certain areas of the metropolitan city of Milan. It is present in the territory with: 6 hospitals, 14 territorial clinics, 23 social and health structures.
Vaccinations are administered in eleven vaccination centers (Rozzano, Melegnano, San Giuliano M., San Donato M., Peschiera Borromeo, Melzo, Gorgonzola, Pioltello, Segrate,Trezzo d’Adda). A clinic dedicated to travel medicine is active in Rozzano and Melzo. In the period March-July 2022, a cross sectional study was conducted in Rozzano Vaccination Center (VC).
In response to regional and ministerial indications, the strategic direction of ASST Melegnano Martesana has organized a specific path for taking charge of Ukrainian refugees.
At the beginning of March 2022, a single point for managing migrants was instituted, with the following registration to the national health service (giving them a Straniero Temporaneamente Presente “STP” code, translated as Temporarily Present Foreigner), the execution of a rapid antigenic nasopharyngeal swab for COVID and a complete clinical anamnesis. At the end of the visit, the refugees were then assigned an appointment in Rozzano vaccination center.
On the day of the appointment, the responsible doctor, with basic Ukrainian language knowledge, assessed patients’ vaccination status (by evaluating the vaccination certificates in the original language or antibody dosages). Then the doctor recorded the vaccinations in the software used in the Lombardy Region (called Siavr), and proposed to the parents (or legal guardians assigned by the court) any vaccinations to be carried out on the basis of the Italian childhood vaccination schedule. The vaccinations carried out or refused have been registered in Siavr as per regional indications.
The software, connected to the registry, made it possible to obtain information such as the age and sex of the patient.
All the collected data were then exported in an Excel sheet for statistical analysis.
Percentages, means and standard deviation were calculated from the collected data. The Shapiro Wilk test was performed to evaluate the normality of the continuous variables. The Mann - Whitney test was then applied. Odds ratios were calculated to understand the relationship between vaccination refusal and gender. Data were organized and processed by Stata® SE software, version 12.1 (StataCorp, College Station, Texas, USA). The significance level was set at p < 0.05.
The study was conducted in a totally anonymous way and approved by the Health Direction of the ASST Melegnano Martesana (Vizzolo Predabissi, Milan, Italy).
INCLUSION AND EXCLUSION CRITERIA
The study was conducted on all Ukrainian refugees under the age of 18 who accessed VC Rozzano during the study period. Minors had to be accompanied by a parent or guardian. The examined vaccinations were all those included in the Italian childhood vaccination schedule(obligatory or not). The anti COVID-19 vaccination was excluded from the study.
Results
From 23 March 2022 to 13 July 2022, 106 Ukrainian refugees received an appointment at VC Rozzano. Of these 27 (25.27%) missed the appointment.
The temporal trend of accesses to the Rozzano CV is summarized in Figure 1.
Fig. 1.
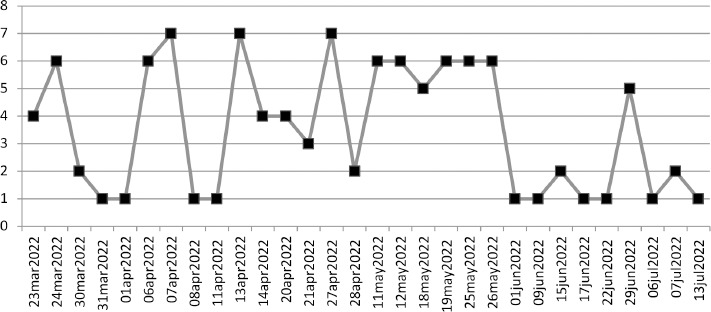
Temporal trend of the accesses to the Rozzano vaccination center in the study period.
Females represented the 51.90% of patients (N = 41); the overall average age was 7.11 (sd ± 4.92, median 6.49 years). There was no statistically significant age difference between the two genders(p = 0.26) as assessed by the Mann Whitney test (level of significance 95%).
Vaccinations that have been accepted or refused are resumed in Table I.
Tab. I.
Accepted or refused vaccinations (anti-poliomyelitis, anti-diphtheria, anti-tetanus, anti-hepatitis B, anti-pertussis, anti-Haemophilus influenzae type b, anti-measles, anti-rubella, anti-mumps, anti-chickenpox are obligatory in Italy from 2017).
| Vaccinations | Accepted (N) | % | Refused (N) | % |
|---|---|---|---|---|
| Hexavalent (DTaP-HepB-IPV-Hib i.e. diphtheria and tetanus toxoids and acellular pertussis adsorbed, hepatitis B and inactivated poliovirus vaccine, Haemophilus influenzae type b conjugate and hepatitis B vaccine) | 9 | 64.29 | 5 | 35.71 |
| Men ACWY (Meningitis ACYW) | 8 | 72.73 | 3 | 27.27 |
| Men C | 16 | 39.02 | 25 | 60.98 |
| Men B | 8 | 47.06 | 9 | 52.94 |
| MMR (Measles, Mumps, and Rubella) | 3 | 37.50 | 5 | 62.50 |
| MMR + Chickenpox | 15 | 83.33 | 3 | 16.67 |
| PCV 13 (Pneumococcal Conjugate Vaccine) | 12 | 54.55 | 10 | 45.45 |
| Rotavirus | 3 | 60.00 | 2 | 40.00 |
| Chickenpox | 8 | 57.14 | 6 | 42.86 |
| Hepatitis B | 3 | 75.00 | 1 | 25.00 |
| dTp - Polio | 6 | 66.67 | 3 | 33.33 |
| HPV (Papillomavirus) | 0 | 0 | 1 | 100.00 |
| Polio | 2 | 100.00 | 0 | 0 |
As evidenced from the percentages reported in Table I, the vaccines that parents (or guardians) decided mostly to refuse were: the vaccine against HPV 100% (N = 1), against measles-mumps-rubella 62.50% (N = 5), against meningococcus C 60.98% (N = 25).
Moreover, the anti-Men C vaccine was the most refused if we consider the total refusals (25 refusals).
There was no difference in the vaccine acceptance if the child was a male or a female(all p > 0.05).
Through the Mann Whitney’s test we could observe a difference in vaccine acceptance related to child’s age for the following vaccinations:
men C (p = 0.01): average age of child if parent/guardian decided to refuse 6.25 (sd 3.46) years, average age of child if parent/guardian decided to accept 3.72 (sd 3.09) years;
chickenpox (p = 0.03): average age of child if parent/guardian decided to refuse 7.73 (sd 4.30) years, average age of child if parent/guardian decided to accept 3.22 (sd 0.87) years.
Discussion
Our study tried to analyze the main characteristics of Ukrainian (minor) refugees who accessed the Rozzano Vaccination Center in a limited time span (almost three months), analyzing their socio-demographic data and the attitude of their parents / guardians towards the proposed vaccinations. War is, in fact, one of the most difficult emergencies [11], characterized by the interruption of basic social functions, including health care. In the health system, treatment takes priority and less attention is paid to prevention and rehabilitation. The implementation of the mandatory immunization program is also overlooked as one of the most important achievements in medicine and one of the most important prevention programs, the introduction of which has saved millions of lives [12].
For example, during the war in Bosnia and Herzegovina (1992-1995), the immunization program in the Sarajevo canton was completely interrupted. There were several problems related to immunization implementation. The main ones were: vaccine shortages, problems with maintaining the cold chain, difficulties to take children to vaccination centers, a large number of orphaned children, a large number of injured children. Immunization has sometimes been overlooked by parents, but also by healthcare workers [12].
Surely the Ukraine case had further complications.
Between 2012 and 2013, vaccination coverage in Ukraine was maintained at 76% (DPT3 i.e. Diphtheria-tetanus-pertussis 3rd dose) (WHO UNICEF estimates), after which it dropped dramatically to 23% in 2014 following the onset of the conflict (the so called Donbass war) [13, 14].
Poor coverage has been amplified by the ongoing conflict and displacements in the east. In 2015, two circulating cases of vaccine-derived type 1 poliovirus were confirmed [14, 15], along with 3667 cases of rubella, 2937 cases of pertussis and 995 cases of mumps [16].
The ever-known vaccine hesitancy in Ukraine led to low childhood vaccination rates between 2008 and 2016. In 2016, only 19% of children received the third dose of the diphtheria-tetanus-pertussis vaccine, 31% the second dose of the measles, mumps and rubella vaccine and 56% received the third recommended dose of the oral polio vaccine. Vaccination rates increased dramatically thereafter, due to a major measles outbreak that resulted in numerous deaths [17].
Furthermore, the Ukrainian vaccination schedule does not include rotavirus and this infection accounts for a large percentage of childhood gastroenteritis [18].
Hepatitis B vaccinations were introduced in Ukraine in 2002. Initial coverage was high (92-98%) in 2004-2007, but then dropped to 21-48% in 2010-2016. Despite low vaccination rates, the prevalence of hepatitis B is low in Ukraine. Some areas of the country have reported a seroprevalence of the surface antigen of the hepatitis B virus (HbsAg) > 0.5% [19].
Fortunately the latest WHO data indicated that Ukraine had much higher childhood vaccination rates in 2019-2020 than in the decade before [18].
In our study, the highest rejection rates concerned the HPV vaccine 100% (N = 1), measles mumps rubella 62.50% (N = 5), and meningococcus C 60.98% (N = 25). The latter vaccination was the one most rejected in absolute numerical terms (25 refusals).
Beyond the historic vaccine hesitancy in Ukraine, a study conducted in Messina in 2017 partially tried to explain plausible reasons related to the vaccine hesitancy towards meningococcal and pneumococcal vaccinations. In this study 81.1% (95% CI: 78.3-84.0) of the parents agreed, while 18.9% (95% CI: 13.0-24.8) responded that these vaccinations are not necessary. The explanation given by the unfavorable parents was the fear of side effects for 44.4% (95% CI: 40.8-48.0), the lack of information received for 30.3% (95% CI: 23, 4-37.2) and doubts about the actual efficacy of these vaccines for 13.1% (95% CI: 8.4-17.8). Furthermore, 53.7% (95% CI: 49.5-57.9) stated that they had received information on these vaccinations and the main sources of information were doctors for 82% (95% CI: 77.8-86.2). Among the respondents, 46.3% (95% CI: 41.8-50.8) replied that they had not received information on these vaccinations. In particular, the misinformation involved vaccines for HPV, meningococcus C and pneumococcus. Compared to HPV vaccination, meningococcal C and pneumococcal vaccinations have received more attention from parents. In fact, on the basis of the parents’ declaration, these vaccinations were carried out respectively in 52.2% and 46.4% of cases, compared to the percentage of 66.6% in favor of them. These data is probably due to the outbreaks of meningitis in some Italian regions. Furthermore, most of those who received pneumococcal vaccination did so because it was administered together with other mandatory vaccinations [20, 21].
This latter aspect could certainly also explain our results which highlight significant differences in age-related acceptance for vaccinations against MenC and against chickenpox: in fact the average age of children who do not undergo these vaccinations is significantly higher (Men c almost 6 years, Chickenpox almost 8 years).
In Italy, the so-called “Vaccines Decree” has increased the number of obligatory vaccinations in childhood and adolescence from four to ten. The goal is to counter the gradual decline in vaccinations, both mandatory and recommended, in place since 2013, which resulted in an average vaccination coverage in Italy < 95%.
The Law Decree 7 June 2017 n. 73 “Urgent provisions on vaccine prevention”, amended by the conversion law 31 July 2017, n. 119, provides for the following compulsory vaccinations for minors between the ages of zero and sixteen and for unaccompanied foreign minors:
anti-poliomyelitis;
anti-diphtheria;
anti-tetanus;
anti-hepatitis B;
anti-pertussis
anti-Haemophilus influenzae type b;
anti-measles;
anti-rubella;
anti-mumps
anti-chickenpox.
The following vaccinations, instead, are actively offered (free of charge)by the Regions and Autonomous Provinces, but are not obligatory:
anti-meningococcal B;
anti-meningococcal C;
anti-pneumococcal;
anti-rotavirus.
Obligatory vaccinations are free of charge and must all be given to those born after 2017 [22].
In general, meningococcal C vaccination is offered in conjunction with measles-mumps-rubella-chickenpox vaccination [23].
So probably, even in our case, the parents/guardians of the youngest Ukrainian children have better accepted vaccinations because they are associated with other obligatory ones.
However, the problem of refusing vaccinations is a very important problem. In several studies, vaccine rejection has been associated with outbreaks of invasive Haemophilus influenzae type b disease, chickenpox, pneumococcal disease, measles, and whooping cough [24, 25].
In particular, a study conducted in Colorado in 1998-2008 found that children of parents who refuse chickenpox vaccinations are at higher risk of chickenpox infection than vaccinated children [1].
Chickenpox is a common vaccine-preventable disease that usually presents in children as a mild infection; however, serious complications also occur. The chickenpox burden is significant in terms of the incidence, complications and hospitalization rate related to chickenpox and obviously also in terms of the economic burden of the disease. Despite the evidence for the overall positive effects of chickenpox vaccination, there are large differences in the implementation of chickenpox vaccination and vaccine adoption from country to country. Improving the acceptance of chickenpox vaccination at the national and individual levels would reduce the burden of the disease on children’s health and health resources.
The determinants of chickenpox vaccine acceptance have been examined in several studies and according to these, the most important factors associated with chickenpox vaccination were the doctor’s recommendation of this vaccination and the perception of chickenpox as a sufficiently serious disease.
For most vaccine-preventable diseases, many parents may not be aware of the danger: since they have not personally seen the devastating effect of tetanus, measles, whooping cough or polio, some of them do not consider the vaccination enough important. This is not the case of chickenpox, as most parents had chickenpox as a child and / or saw the disease in others. However, this factor could backfire on accepting chickenpox vaccination. If parents remember chickenpox as a mild infection and if they have learned to accept chickenpox as a normal part of childhood, these elements can undermine their willingness to vaccinate their children [26].
The problem of whether or not to accept vaccinations is certainly much broader.
In research, individual and interpersonal approaches have long been used to examine and facilitate behavior change. More recently, the factors that facilitate and / or hinder the implementation of health behaviors are addressed using a new approach: the social determinants of health (Social Determinants of Health SDoH) [27].
SDOH include elements in an individual’s neighborhood, community and environment determined by where the individual is born, resides, learns, works, worships, etc. As a result, the Healthy People 2030 SDoH Framework classifies SDoH indicators into five categories: social and community context, education, economic stability, neighborhood and built environment, health and healthcare [27].
SDoH includes access to education, affordable housing and health services, public safety, food safety [28].
SDoH are affected by the distribution of resources that improve quality of life and public health outcomes. For example, in the United States, people residing in certain metropolitan statistical areas (MSAs), non-MSAs (mostly rural), and without health insurance are disproportionately less likely to be vaccinated [29].
Also, parental education; living conditions and family income; access to health care; philosophical and cultural beliefs; religious affiliations; and urban vs rural residence are some of the SDoHs that influence childhood vaccination rates [30].
In 2019, a study conducted on American families showed that the prevalence of vaccine hesitancy was 6.1% for routine childhood vaccinations and 25.8% for influenza vaccines; 12% firmly and 27% somehow agreed to have concerns about the serious side effects of both routine childhood vaccines and influenza. A total of 70% firmly agreed that routine childhood vaccines are effective against 26% of the flu vaccine (P < .001). Also in this study, applying multivariable models, an education level below a college degree and a household income below 400% of the federal poverty level predicted hesitation on both routine childhood vaccines and influenza [31].
STUDY LIMITS
Some limits should be certainly reported in our study: first, the limited number of patients (and their parents), that could not be representative of the entire population; second, although refugees received information in their language, the language barriers have represented a great problem for an efficient communication. Moreover, in case of vaccine refusal, the reasons have not been asked, so we are not able to have a complete overview of vaccine hesitancy phenomenon among Ukrainian refugees.
Conclusions
The war in Ukraine and the resulting migration crisis represent a major challenge for public health in Italy.
Years of organizational and vaccine procurement difficulties, as well as a long history of vaccine hesitancy in the country, widely spread both in the general population and among health workers, have resulted in low vaccination coverage in Ukraine and the occurrence of epidemic outbreaks. Low vaccination rates against major vaccine-preventable infectious diseases in Ukraine can certainly reduce the ability to effectively control probable outbreaks in the immediate and future.
The efforts made by the ASST Melegnano Martesana and the Rozzano Vaccination Center to ensure complete care and promote vaccination among refugees, offering them a complete evaluation of the vaccination status and the possibility of being vaccinated for free, seem however to be insufficient to convince most refugees to get vaccinated.
Acknowledgments
No one.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Authors’ contribution
GTr had the idea of the study, collected and analyzed data, AN and GTo supervised the work and helped to conceptualize the ideas
Figures and tables
References
- [1].Sidel VW, Levy BS. The health impact of war. Int J Inj Contr Saf Promot 2008;15:189-95. https://doi.org/10.1080/17457300802404935 10.1080/17457300802404935 [DOI] [PubMed] [Google Scholar]
- [2].UNICEF. Immunization and conflict. Available at: https://www.unicef.org/immunization/immunization-and-conflict (Accessed on: 31/08/2022).
- [3].Forum We. This map shows how many refugees are fleeing Ukraine 2022. Available at: https://www.weforum.org/agenda/2022/06/ukraine-refugee-crisis-europe-conflict-migration/ (Accessed on: 19/08/2022).
- [4].Shengen visa News. Timeline of Ukrainian Refugees Reaching EU Countries Amid Russian Invasion 2022. Available at: https://www.schengenvisainfo.com/news/timeline-of-ukrainian-refugees-reaching-eu-countries-amid-russian-invasion/ (Accessed on: 19/08/2022).
- [5].Hill M, Vanderslott S, Volokha A, Pollard AJ. Addressing vaccine inequities among Ukrainian refugees. Lancet Infect Dis 2022;22:935-6. https://doi.org/10.1016/S1473-3099(22)00366-8 10.1016/S1473-3099(22)00366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Broniatowski DA, Jamison AM, Qi S, AlKulaib L, Chen T, Benton A, Quinn SC, Dredze M. Weaponized health communication: twitter bots and russian trolls amplify the vaccine debate. Am J Public Health 2018;108:1378-84. https://doi.org/10.2105/AJPH.2018.304567 10.2105/AJPH.2018.304567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health 2021;194:245-51. https://doi.org/10.1016/j.puhe.2021.02.025 10.1016/j.puhe.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Health Cluster Ukraine Ukraine public health situation analysis (PHSA)–short-form. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/ukraine-phsa-shortform-030322.pdf (Accessed on: 03/03/2022).
- [9].International Organization for Migration UN Migration Ukraine internal displacement report. Available at: https://displacement.iom.int/reports/ukraine-internal-displacement-report-general-population-survey-round-4-29-april-3-may-2022 (Accessed on: 03/05/2022).
- [10].Ministero Della Salute. Oggetto: Crisi Ucraina - Prime Indicazioni per Aziende Sanitarie Locali 2022. Available at: https://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2022&codLeg=86063&parte=1%20&serie=null (Accessed on: 1/05/2022).
- [11].Nante N, Gialluca L, De Corso M, Troiano G, Verzuri A, Messina G. Quality of life in refugees and asylum seekers in Italy: a pilot study. Ann Ist Super Sanità 2016;52:424-7. [DOI] [PubMed] [Google Scholar]
- [12].Obradovic Z, Balta S, Obradovic A, Mesic S. The impact of war on vaccine preventable diseases. Mater Sociomed 2014;26:382-4. https://doi.org/10.5455/msm.2014.26.382-384 10.5455/msm.2014.26.382-384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].World Health Organisation (WHO). Country Profile Ukraine. Available at: http://www.who.int/immunisation/monitoring_surveillance/data/ukr.pdf (Accessed on: 08/09/2018).
- [14].Grundy J, Biggs BA. The impact of conflict on immunisation coverage in 16 countries. Int J Health Policy Manag 2019;8:211-21. https://doi.org/10.15171/ijhpm.2018.127 10.15171/ijhpm.2018.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].World Health Organisation (WHO). Circulating vaccine-derived poliovirus – Ukraine. WHO website. Available at: http://www.who.int/csr/don/01-september-2015-polio/en/ (Accessed on: 8/09/2018).
- [16].Bagcchi S. Inadequate vaccine coverage fuels polio outbreak in Ukraine. Lancet Infect Dis 2015;15:1268-9. https://doi.org/10.1016/S1473-3099(15)00367-9 10.1016/S1473-3099(15)00367-9 [DOI] [PubMed] [Google Scholar]
- [17].Hadjipanayis A, van Esso D, Del Torso S, Dornbusch HJ, Michailidou K, Minicuci N, Pancheva R, Mujkic A, Geitmann K, Syridou G, Altorjai P, Pasinato A, Valiulis A, Soler P, Cirstea O, Illy K, Mollema L, Mazur A, Neves A, Zavrsnik J, Lapii F, Efstathiou E, Kamphuis M, Grossman Z. Vaccine confidence among parents: Large scale study in eighteen European countries. Vaccine 2020;38:1505-12. https://doi.org/10.1016/j.vaccine.2019.11.068 10.1016/j.vaccine.2019.11.068 [DOI] [PubMed] [Google Scholar]
- [18].Ludvigsson JF, Loboda A. Systematic review of health and disease in Ukrainian children highlights poor child health and challenges for those treating refugees. Acta Paediatr 2022;111:1341-53. https://doi.org/10.1111/apa.16370 10.1111/apa.16370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Khetsuriani N, Zaika O, Chitadze N, Slobodianyk L, Allahverdiyeva V, O’Connor P, Huseynov S. Seroprevalence of hepatitis B virus infection markers among children in Ukraine, 2017. Vaccine 2021;39:1485-92. https://doi.org/10.1016/j.vaccine.2021.02.004 10.1016/j.vaccine.2021.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Facciolà A, Visalli G, Orlando A, Bertuccio MP, Spataro P, Squeri R, Picerno I, Di Pietro A. Vaccine hesitancy: An overview on parents’ opinions about vaccination and possible reasons of vaccine refusal. J Public Health Res 2019;8:1436. https://doi.org/10.4081/jphr.2019.1436 10.4081/jphr.2019.1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Troiano G, Nardi A. Instagrammers’ attitude towards Human Papillomavirus (HPV) vaccine: A review. J Hum Behav Soc Environ 2022;32:274-82. https://doi.org/10.1080/10911359.2021.1885554 10.1080/10911359.2021.1885554 [DOI] [Google Scholar]
- [22].Capano D, Mercurio I, Gabbrielli M, Troiano G, Macrì PG. Vaccinations: Individual freedom vs the interest of the community. legislative updates and liability concerns. Rivista Italiana di Medicina Legale e del Diritto in Campo Sanitario 2019;35:1319-37. [Google Scholar]
- [23].Ministero Della Salute. Legge vaccini 2021. Available at: https://www.salute.gov.it/portale/vaccinazioni/dettaglioContenutiVaccinazioni.jsp?lingua=italiano&id=4824&area=vaccinazioni&menu=vuoto (Accessed on: 27/8/2022).
- [24].Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the united states: a review of measles and pertussis. JAMA 2016;315:1149-58. https://doi.org/10.1001/jama.2016.1353 10.1001/jama.2016.1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Glanz JM, McClure DL, Magid DJ, Daley MF, France EK, Hambidge SJ. Parental refusal of varicella vaccination and the associated risk of varicella infection in children. Arch Pediatr Adolesc Med 2010;164:66-70. https://doi.org/10.1001/archpediatrics.2009.244 10.1001/archpediatrics.2009.244 [DOI] [PubMed] [Google Scholar]
- [26].Horváth A. Acceptance of varicella vaccination. Hum Vaccin Immunother 2021;17:1699-702. https://doi.org/10.1080/21645515.2020.1843337 10.1080/21645515.2020.1843337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Thompson EL, Rosen BL, Maness SB. Social determinants of health and human papillomavirus vaccination among young adults, national health interview survey 2016. J Community Health 2019;44:149-58. https://doi.org/10.1007/s10900-018-0565-2 10.1007/s10900-018-0565-2 [DOI] [PubMed] [Google Scholar]
- [28].US- Department of Health and Human Services. Social determinants of health - 2014. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health (Accessed on: 01/03/2021).
- [29].Pingali C, Yankey D, Elam-Evans LD, Markowitz LE, Williams CL, Fredua B, McNamara LA, Stokley S, Singleton JA. national, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2020. MMWR Morb Mortal Wkly Rep 2021;70:1183-90. https://doi.org/10.15585/mmwr.mm7035a1 10.15585/mmwr.mm7035a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Glatman-Freedman A, Nichols K. The effect of social determinants on immunization programs. Hum Vaccin Immunother 2012;8:293-301. https://doi.org/10.4161/hv.19003 10.4161/hv.19003 [DOI] [PubMed] [Google Scholar]
- [31].Kempe A, Saville AW, Albertin C, Zimet G, Breck A, Helmkamp L, Vangala S, Dickinson LM, Rand C, Humiston S, Szilagyi PG. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics 2020;146:e20193852. https://doi.org/10.1542/peds.2019-3852 10.1542/peds.2019-3852 [DOI] [PMC free article] [PubMed] [Google Scholar]


