Abstract
Antimicrobial resistance (AMR) data on zoonotic and indicator bacteria from humans, animals and food are collected annually by the EU Member States (MSs) and reporting countries, jointly analysed by EFSA and ECDC and presented in a yearly EU Summary Report. This report provides an overview of the main findings of the 2020–2021 harmonised AMR monitoring in Salmonella spp., Campylobacter jejuni and C. coli in humans and food‐producing animals (broilers, laying hens and turkeys, fattening pigs and bovines under 1 year of age) and relevant meat thereof. For animals and meat thereof, indicator E. coli data on the occurrence of AMR and presumptive Extended spectrum β‐lactamases (ESBL)‐/AmpC β‐lactamases (AmpC)‐/carbapenemases (CP)‐producers, as well as the occurrence of methicillin‐resistant Staphylococcus aureus are also analysed. In 2021, MSs submitted for the first time AMR data on E. coli isolates from meat sampled at border control posts. Where available, monitoring data from humans, food‐producing animals and meat thereof were combined and compared at the EU level, with emphasis on multidrug resistance, complete susceptibility and combined resistance patterns to selected and critically important antimicrobials, as well as Salmonella and E. coli isolates exhibiting ESBL‐/AmpC‐/carbapenemase phenotypes. Resistance was frequently found to commonly used antimicrobials in Salmonella spp. and Campylobacter isolates from humans and animals. Combined resistance to critically important antimicrobials was mainly observed at low levels except in some Salmonella serotypes and in C. coli in some countries. The reporting of a number of CP‐producing E. coli isolates (harbouring bla OXA‐48, bla OXA‐181, and bla NDM‐5 genes) in pigs, bovines and meat thereof by a limited number of MSs (4) in 2021, requests a thorough follow‐up. The temporal trend analyses in both key outcome indicators (rate of complete susceptibility and prevalence of ESBL‐/AmpC‐ producers) showed that encouraging progress have been registered in reducing AMR in food‐producing animals in several EU MSs over the last years.
Keywords: antimicrobial resistance, zoonotic bacteria, indicator bacteria, ESBL, MRSA
Summary
In 2020–2021, data on antimicrobial resistance in zoonotic and indicator bacteria submitted by 27 EU Member States (MSs), the United Kingdom (Northern Ireland) and five non‐MSs were jointly analysed by the EFSA and the ECDC and their contractor. Resistance in zoonotic Salmonella and Campylobacter from humans, food‐producing animals (fattening pigs, calves under 1 year of age, broilers and fattening turkeys) and derived meat, as well as resistance in indicator Escherichia coli and methicillin‐resistant Staphylococcus aureus (MRSA) from animals and food were addressed. In 2020, it was mandatory to report AMR data from poultry flocks and derived meat, while in 2021, it was mandatory to report AMR data from fattening pigs and calves and derived meat. ‘Microbiological’ resistance in the isolate populations was assessed using epidemiological cut‐off (ECOFF) values. For some countries, qualitative data on human isolates were interpreted in a way which corresponds closely to the ECOFF‐defined ‘microbiological’ resistance.
New legislation related to the harmonised monitoring and reporting of AMR in food‐producing animals and derived meat was introduced in 2021, requiring MSs to sample imported fresh meat at border control posts for E. coli. New substances were also added in the harmonised antimicrobial panels, including amikacin for Salmonella and E. coli, and chloramphenicol and ertapenem for Campylobacter spp. Also from 2021, whole genome sequencing (WGS) was authorised as an alternative method to supplementary (panel 2) phenotypic testing of Salmonella and E. coli isolates with resistance to extended‐spectrum cephalosporins and carbapenems.
In Salmonella spp. from human cases in 2021, resistance to ampicillin, sulfonamides and tetracyclines was observed at overall high levels, while resistance to third‐generation cephalosporins in 2021 was noted at overall very low levels of 1.1% for both cefotaxime and ceftazidime, respectively. A decline in resistance to ampicillin and tetracycline in isolates from humans was observed in 13 and 11 countries, respectively, over the period 2013–2021. This was particularly evident in S. Typhimurium, a serovar commonly associated with pigs and calves. For cefotaxime, six MSs reported declining trends compared to three MSs reporting increasing trends. A moderate occurrence of resistance to ciprofloxacin (14.9%) was observed in human cases from 2021; however, an extremely high proportion of resistant isolates was noted in S. Kentucky (78.1%) and increasing trends in ciprofloxacin resistance were observed for S. Enteritidis in 10 countries over the period 2013–2021, with this serovar predominantly being associated with poultry.
For Salmonella spp. and indicator E. coli isolates recovered from food‐producing animals and poultry carcases in 2020/2021, resistance to ampicillin, tetracyclines and sulfonamides, ranged from moderate to very high in most MSs. Resistance to third‐generation cephalosporins (cefotaxime and ceftazidime) was seldom detected in animals and derived meat, except for low‐level resistance observed in Salmonella spp. isolates from calves and broiler flocks. These findings mirror those observed in Salmonella isolates reported from human cases. Resistance to (fluoro)quinolones (ciprofloxacin and nalidixic acid) was high to very high among Salmonella spp. and indicator E. coli isolates recovered from broilers, fattening turkeys and poultry carcases/meat in 2020, and low or moderate levels in isolates from pigs and calves in 2021.
Resistance to amikacin, the new substance included in the harmonised panel for 2021, was very low or low in Salmonella spp. and E. coli isolates from fattening pigs and no resistance was detected in Salmonella spp. isolates from bovine animals under 1 year of age. Resistance to colistin was uncommon among Salmonella spp. and E. coli isolates recovered from food‐producing animals and poultry carcases, although moderate resistance was observed in certain Salmonella serovars (S. Enteritidis) and in Salmonella isolates from bovine animals under 1 year of age.
Combined resistance to ciprofloxacin and cefotaxime, categorised as highest priority critically important antimicrobials, was very low in Salmonella isolates from humans and rare or very low in Salmonella isolates in almost all animal and derived meat categories, with the exception of broilers and calves where low levels were detected. While for E. coli isolates low levels were reported in all animal and derived meat. Some Salmonella serovars from poultry sources, such as S. Kentucky and S. Infantis, had comparatively elevated levels of combined resistance to ciprofloxacin and cefotaxime.
In 2021, MSs could submit AMR data on E. coli isolates recovered from fresh/frozen meat sampled at border control posts for the first time. Four MSs contributed data from imported fresh pig meat (n = 13), and six MSs contributed data from imported bovine meat (n = 110). For meat of both origins, resistance was either undetected, observed rarely or at low levels for most of the antimicrobial substances in the harmonised panel.
Overall, the data obtained in 2020–2021 from C. jejuni and C. coli from human and animal origins showed high to extremely high levels of resistance to fluoroquinolones, which are critically important antimicrobials (CIA) for the treatment of Campylobacter infections in humans. High to extremely high resistance levels to ciprofloxacin were observed in human C. jejuni and C. coli isolates in the EU in 2021, ranging from 22.2% to 100%. Very high levels of resistance were observed for ciprofloxacin in isolates from food‐producing animals (ranging from 41.7% to 80.4%). Overall, the levels of resistance to ciprofloxacin obtained from food‐producing animals were higher for C. coli than for C. jejuni, although the level of resistance to ciprofloxacin obtained from C. jejuni isolates from poultry in 2020 were also high (e.g. 77.9% in fattening turkeys – data from nine MSs). The lowest levels of resistance to ciprofloxacin in both C. jejuni and C. coli were observed in isolates from fattening pigs in 2021 (41.7% and 51.7%, respectively). Resistance to erythromycin (also CIA) was detected at low levels in C. jejuni from humans (1.1%) and animals (ranging from 0.8% to 1.7%). However, higher levels of resistance were observed in C. coli isolates from humans (8.5%) and animals (range from 4.4% to 35.7%). The level of overall resistance to tetracycline ranged from high to extremely high (43.3%–90.5%) in food‐producing animals, and was high in C. jejuni and extremely high in C. coli from humans.
Over the period 2013–2021, ciprofloxacin resistance in C. jejuni from humans increased in 12 countries, while erythromycin resistance decreased in seven countries. Similar trends were observed in C. jejuni from broilers over 2009–2020 where resistance to ciprofloxacin increased in 14 countries, and resistance to erythromycin decreased in five countries. In C. coli, a decrease in resistance to erythromycin was observed in isolates from humans, fattening pigs and broilers in few countries while increasing resistance to this substance was only observed in one country in C. coli isolated from broilers. Despite these declining trends, several of the erythromycin‐resistant isolates displayed high MIC values (MIC > 128 mg/L, 128 mg/L < MIC ≤ 512 mg/L or MIC > 512 mg/L), which could indicate a presence of the transferrable macrolide resistance gene erm(B).
The occurrence of combined resistance to ciprofloxacin and erythromycin in Campylobacter spp. is considered of high public health relevance. Overall combined resistance to these antimicrobials was lower in C. jejuni isolates than in C. coli isolates for humans and food‐producing animals. Combined resistance to ciprofloxacin and erythromycin reported from C. jejuni isolates was detected in 0.8% of isolates from humans, 0.7% isolates from broilers, 0.8% of isolates from fattening turkeys and from calves and 1.7% of pig isolates. Combined resistance to ciprofloxacin and erythromycin reported from C. coli isolates was detected in 7.6% of isolates from humans in 2021, 4.1% of broiler samples and 21.2% of isolates from fattening turkeys in 2020 and 32.7% of samples from calves and 9.3% of pig isolates in 2021. The levels of combined resistance to ciprofloxacin and erythromycin increased from 22.4% in 2019 to 32.7% in 2021 in C. coli isolates from calves, which might infer a public health concern. The level of combined resistance to ciprofloxacin and erythromycin observed in C. coli isolated from pigs in 2019 was 8% while in 2021 increased to 9.3%.
Multidrug resistance (MDR) levels were generally low for C. jejuni isolated from humans and the animal species considered. Compared to C. jejuni, it was markedly higher in C. coli isolated from humans, calves and fattening pigs (9.9%, 39.3% and 9.7%, respectively) based on data from 2021 and from fattening turkeys (21%) based on data from 2020. These results agree with the higher levels of resistance to selected antimicrobials seen in C. coli isolates.
The prevalence of resistance to selected antimicrobials in C. coli from fattening pigs in 2021 has been estimated at country level as the proportion of C. coli showing microbiological resistance to each antimicrobial as a percentage of all caecal samples cultured for C. coli. Between‐country variability from low to extremely high levels was observed in the prevalence of ciprofloxacin‐resistant (ranging from 6.9% to 78.2%) and tetracycline‐resistant (ranging from 0.0% to 86.5%) C. coli from fattening pigs. Interestingly, a limited between‐country variation and notably lower levels of prevalence of resistance to erythromycin were found in C. coli from fattening pigs, which have been estimated to be below 10% for 21 MSs and 3 non‐MSs, while ranging from 14.9% to 39.7% in the remaining six reporting MSs. Noteworthy, the MS with the highest prevalence of resistance to erythromycin in C. coli from fattening pigs in 2021 had also the highest level of erythromycin resistance in C. coli from humans, suggesting that pigs could be a reservoir of erythromycin‐resistant C. coli for humans. This finding is of particular public health concern since macrolides, such as erythromycin and azithromycin, have become the first‐line treatment of human campylobacteriosis.
The monitoring included assessment of the levels of presumptive extended‐spectrum β‐lactamase (ESBL)‐/AmpC‐/carbapenemase producers among Salmonella spp. from human cases, food‐producing animals and animal carcases; as well as among indicator E. coli isolates from food‐producing animals. At the reporting MS group level, the proportion of presumptive ESBL or AmpC producers was very low to low among Salmonella spp. isolates recovered from animals/carcases (broilers, laying hens, fattening turkeys, fattening pigs and carcases of broilers and fattening pigs) and very low in isolates from human cases, although higher in some Salmonella serovars. Statistically significant decreasing trends are evident in the prevalence of ESBL‐producing E. coli in broilers, broiler meat and pig meat at the EU level.
Within both the routine and specific monitoring (non‐selective and selective media, respectively), varying occurrence/prevalence rates of presumptive ESBL or AmpC‐producing E. coli were observed in different reporting countries. A larger proportion of isolates were identified as presumptive ESBL‐producers compared with AmpC‐producers based on phenotypic methods in 2020 and 2021. This was supported by WGS that revealed 976 E. coli isolates carrying ESBL genes, 61 isolates carrying AmpC genes and 96 isolates presenting a point mutation in the AmpC promotor.
Furthermore, in 2021, within the specific monitoring of ESBL‐/AmpC‐/CP‐producing E. coli, two CP‐producing isolates from bovine meat and one isolate from pig were detected by Hungary. Those isolates were confirmed as CP‐producers harbouring the bla NDM‐5 gene, responsible for the carbapenemase phenotype, by the EURL‐AR during the confirmatory testing exercise. Moreover, within the specific monitoring of carbapenemase‐producing microorganisms (using selective media for carbapenemase producers), three isolates from bovine meat and one isolate from pig meat were reported by Hungary. The presence of CP‐encoding genes in the Hungarian isolates are pending of confirmation. Additionally, two isolates from fattening pigs detected in Spain, carried the bla OXA‐48 gene. WGS revealed additional 26 E. coli isolates from Italy (21 from pigs and five from bovine animals under 1 year of age) and three isolates from Czechia (all from fattening pigs) carrying CP‐encoding genes under the specific carbapenemase monitoring. These included bla OXA‐181 (4 isolates from calves and 20 from fattening pigs), bla OXA‐48 (one isolate from a fattening pig), and bla NDM‐5 (1 isolate from a calf) detected in the Italian isolates, and bla NDM‐5 (3 isolates from fattening pigs) reported by Czechia. Carbapenemase‐producing Salmonella isolates were not detected in animals in 2020/2021, nor in 2021 for human cases.
The voluntary monitoring of MRSA from food and healthy animals in 2020–2021 revealed most MRSA isolates, where typing data were available, was associated with spa‐types assigned to livestock associated (LA‐)MRSA in both reporting years. However, spa‐types associated with community acquired (CA‐) and hospital acquired (HA‐)MRSA were also reported, as well as mecC‐MRSA. The occasional detection of lineages of CA‐ and HA‐MRSA primarily associated with humans is not surprising, since the sporadic interchange of strains between humans and animals may be expected. A notable observation from the 2020 monitoring was the occurrence of a vancomycin‐resistant MRSA t011 isolate in meat from sheep. The isolate lacks the typical vancomycin resistance genes and it is likely that the increased MIC of 4 mg/L was due to multiple point mutations as described in the literature. An important observation from the 2021 monitoring includes the detection of rifampicin resistance in isolates from pig and bovine meat. Vancomycin and rifampicin are important compounds in human medicine for the treatment of MRSA.
The key outcome indicators for AMR in food‐producing animals – complete susceptibility (KOICS) to the harmonised panel of antimicrobials in E. coli and the prevalence of ESBL‐/AmpC‐producing E. coli – have also been analysed over the period 2014–2021. There are marked variations in both key outcome indicators among reporting countries. Statistically significant decreasing trends in the key outcome indicator of ESBL‐ and/or AmpC‐producing E. coli (KOIESC) were observed in 17 MSs and one non‐MS. A statistically significant increasing trend was identified in two MSs, and in the remaining countries, no statistically significant trend was seen. Statistically significant increasing trends in the key outcome indicators of complete susceptibility (KOICS) were registered in 8 MSs and decreasing trends in three countries. The increasing trends in changes to CS and KOICS in indicator E. coli isolates reveal a progress towards lower levels of resistance in several countries and in the MS‐group. The improvement seen in changes to CS was most pronounced in poultry. Both key outcome indicators show that encouraging progress has been registered in reducing AMR in food‐producing animals in several EU MSs over the last years.
1. Introduction
Legal basis
Monitoring of AMR in bacteria from food‐producing animals and derived meat
Regulation (EC) 178/2002 1 Article 33 establishes that EFSA is responsible for examining data on antimicrobial resistance (AMR) collected from the Member States (MSs) in accordance with Directive 2003/99/EC and for preparing the EU Summary Report from the results.
Directive 2003/99/EC 2 on monitoring zoonoses and zoonotic agents lays down the provisions for monitoring AMR in zoonotic and indicator bacteria in food‐producing animals and derived meat. The Directive obliges EU MSs to collect relevant and, where applicable, comparable data on zoonoses, zoonotic agents, AMR and food‐borne outbreaks.
Commission Implementing Decision (EU) 2020/1729 3 on the monitoring and reporting antimicrobial resistance in zoonotic and commensal bacteria repeals Commission Implementing Decision (EU) 2013/652 4 . Commission Implementing Decision 2020/1729 (EU) applies from 2021 to 2027 and sets up priorities for the monitoring of AMR from a public health perspective, prescribes a list of combinations of bacterial species, food‐producing animal populations and foodstuffs and lays down harmonised rules for the period 2021–2027, for the monitoring and reporting of AMR in food‐producing animals and food.
Monitoring of AMR in bacteria from humans
Decision 2018/945/EU 5 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions stipulates mandatory testing and reporting of a representative subset of isolates using methods and criteria specified in the EU protocol for harmonised monitoring of antimicrobial resistance in human Salmonella and Campylobacter isolates (ECDC, 2016).
The data collection on human diseases from MSs is conducted in accordance with Decision 1082/2013/EU 6 on serious cross‐border threats to health.
Terms of Reference
In accordance with the Zoonoses Directive 2003/99/EC, the EU MSs are required to assess trends and sources of zoonoses, zoonotic agents and AMR, as well as outbreaks in their territory, submitting an annual report each year by the end of May to the European Commission covering the data collected.
In accordance with Article 9 of Directive 2003/99/EC, the EFSA shall examine the submitted national reports of the MSs and publish a summary report on the trends and sources of zoonoses, zoonotic agents and AMR in the EU.
The ECDC has provided data on zoonotic infections in humans and their analyses for the EU Summary Reports since 2005. Since 2007, data on human cases have been reported through The European Surveillance System (TESSy), maintained by the ECDC.
The antimicrobial agents used in food‐producing animals and human medicine in Europe are frequently the same or else belong to the same classes. The route of administration and the administered quantities of antimicrobials differ between humans and food‐producing animals. Moreover, there are important variations between and within food‐producing animal populations and countries. Nevertheless, frequently exposing the bacterial biota in both humans and animals to antimicrobial agents might result in the development of AMR by favouring the selection of resistant bacterial clones, regardless of whether these are pathogenic, commensal or environmental bacteria. This could, over time, change the population structure of microbial communities with serious consequences for human and animal health.
Antimicrobial resistance
AMR is defined as the inability or reduced ability of an antimicrobial agent to inhibit the growth of a bacterium, which, in the case of a pathogenic organism, can lead to therapy failure. A bacterial strain can acquire resistance by mutation, by the uptake of exogenous genes by horizontal transfer from other bacterial strains or by the activation/triggering of a genetic cascade, thereby inducing the expression of resistance mechanisms (EMA and EFSA, 2017). AMR is also an acronym for the health problems arising in humans and animals, when antimicrobial‐resistant microorganisms spread within a population or society. The development and spread of resistance can be triggered by different factors such as use of antimicrobials in human and veterinary medicine, poor hygiene conditions and practices in healthcare settings or the food chain that facilitate the transmission of resistant microorganisms. Over time, this makes antimicrobials less effective.
Antimicrobial‐resistant bacteria derived from food‐producing animals can spread to humans by ingestion of, or from handling, food contaminated with zoonotic bacteria such as Campylobacter, Salmonella or Escherichia coli (E. coli), from direct contact with animals, or rarely, by environmental contamination. Infections with antimicrobial‐resistant bacteria may result in treatment failures or the need for second‐line antimicrobials for therapy. The commensal bacterial flora can also form a reservoir of resistance genes, which may be transferred between bacterial species, including organisms capable of causing disease in humans and animals (EFSA, 2008).
The European Commission adopted an Action Plan to tackle AMR on 29 June 2017. 7 The Action Plan is underpinned by a One Health approach that addresses resistance in bacteria from both humans and animals. EU actions have focused on the areas with the highest added value for MSs, such as promoting the prudent use of antimicrobials via antimicrobial stewardship (AMS), enhancing cross‐sectorial work, improving infection prevention and control (IPC), and consolidating surveillance of AMR and antimicrobial consumption (AMC). AMR monitoring in zoonotic and commensal bacteria in food‐producing animals and foodstuffs entails specific and continuous data collection, analysis, and reporting. It enables the understanding of the development and diffusion of resistance, the following of temporal trends in the occurrence and distribution of AMR, the identification of emerging or specific resistance patterns, it provides relevant risk assessment data and helps to evaluate targeted interventions.
The European Commission has announced plans to boost the implementation of the 2017 One Health Action Plan against AMR by the end of 2022 (European Commission, 2022). This is supported by the Trio Presidency of the Council of the EU (France, Czech Republic, and Sweden), who released a Declaration on Antimicrobial Resistance calling for strengthened action and cooperation on AMR, including support for the update of the 2017 Action Plan (Trio Presidency of the Council of the European Union, 2022). Moreover, the Organisation for Economic Cooperation and Development (OECD), in collaboration with the ECDC, EFSA and the European Medicines Authority (EMA), released a briefing note on the One Health response to AMC and AMR in the EU and European Economic Area (EEA), setting out policy options for national governments and the EU (OECD, 2022) (see text box below).
A joint report by ECDC, EFSA, EMA and OECD on antimicrobial resistance and the One Health response in the EU/EAA
In March 2022, the OECD, in collaboration with the ECDC, EFSA and EMA, released a briefing note on the One Health response to AMC and AMR in the EU and European Economic Area (EEA) (OECD, 2022). The briefing note summarises important findings on AMC and AMR in the EU/EAA over the past decade (2011–2020) and sets out policy options for national governments and the EU.
The OECD reports that overall consumption of antibiotics in humans decreased by 23% in the EU/EAA between 2014 and 2020, although there was considerable variability in AMC in the countries evaluated. Much of the reported decrease in AMC (approximately 18%) occurred between 2019 and 2020 during the COVID‐19 pandemic. It is unclear whether reduced AMC in human health settings was sustained in 2021 and if there are implications for AMR. Despite reductions in AMC, the relative use of broad‐spectrum antibiotics in human health increased over the same period, which is a cause for some concern. For food‐producing animals, overall AMC decreased by 43% between 2011 and 2020 in 25 countries with consistent reporting, suggesting that interventions aimed at reducing AMU in these sectors have been successful.
While AMC levels are dropping, AMR in bacteria from humans and animals has increased for many antibiotic–bacterium combinations in the past decade. Of concern in human health is the rise in resistance to critically important antibiotics (CIAs) used to treat common healthcare‐associated infections. In food animals, recent trends in AMR are encouraging, with the proportion of indicator E. coli isolates testing completely susceptible to all tested antibiotics increasing and there is a continuing trend of low‐level occurrence of combined resistance to CIAs in Salmonella and Campylobacter. However, resistance to commonly used antibiotics in bacteria from food‐producing animals remains high (> 20% to 50%) or very high (> 50% to 70%), and there is significant regional variation across the EU/EEA region.
Analyses by the OECD identify urgent priorities for the EU/EAA, including:
Monitoring and evaluating the implementation of national action plans across the EU/EAA
Supporting efforts to strengthen surveillance of AMR through enhanced laboratory network capacity, integration of new data sources and technologies (e.g. WGS), and harmonisation of data collection methods across the EU/EEA
Investing in cost‐effective interventions such as antimicrobial stewardship (AMS) programmes and infection, prevention and control (IPC) initiatives.
The report concludes that there is mounting evidence that AMR can spread between animals, humans and the environment. Reducing the use of antibiotics in food‐producing animals, replacing them where possible, and rethinking livestock production systems in a One Health approach are critical for the future of animal and public health. AMR remains a serious challenge in the EU/EAA, underlying the need for concerted action.
EU4health and HaDEA: new EU initiatives to combat AMR
In 2021, in response to the COVID‐19 pandemic and to strengthen crisis preparedness in the EU, the European Commission announced a €5.3 billion investment in the EU4Health program (2021–2027). 8 Established by Regulation (EU) 2021/522 9 , the programme complements the policies of MSs to build more resilient and accessible health systems and undertake activities in line with the One Health approach. Funding is provided to EU countries, health organisations and non‐government organisations (NGOs) for a range of health priorities, including for activities aimed at reducing the number of AMR infections in human health. EU4Health has four work programmes,(i) crisis preparedness, which includes activities related to tackling AMR, (ii) health promotion and disease prevention, (iii) health systems and healthcare workforce and (iv) digital health. The 2022 work programme for EU4Health includes actions to develop a monitoring and evaluation framework to strengthen the 2017 EU Action Plan against AMR. Work in this area is under active consideration by MSs and the European Commission.
The European Health and Digital Executive Agency (HaDEA) was established in February 2021 to implement European programmes and initiatives on behalf of the European Commission, by managing projects related to health, food safety, digital technologies and networks, industrial capacities and space. One area of responsibility of HaDEA is to improve EU networking and provide support for public health reference laboratory functions for AMR in Salmonella species and Campylobacter species in human samples. 10 The FWD AMR‐RefLabCap project 11 (2021–2024) is a major initiative of HaDEA, which supports capacity building of public health reference laboratories responsible for the microbiological analyses, including antimicrobial susceptibility testing, of food‐borne bacteria from human infections. The outcomes are to strengthen preparedness to respond to food‐borne outbreaks and improve prevention and management of AMR from zoonotic bacteria. The project will achieve this by supporting the implementation and greater use of whole genome sequencing (WGS) in all laboratories, improving networking of national reference laboratories, and strengthening molecular surveillance of AMR throughout the EU.
This EU Summary Report (EUSR) on AMR includes data related to the occurrence of AMR in isolates from animals, foodstuffs and humans. The EUSR on AMR is a collaboration between EFSA and ECDC with the assistance of EFSA's contractors. EU MSs, European Free Trade Association (EFTA), the European Commission and the relevant EU Reference Laboratory for antimicrobial resistance (EURL‐AR) are consulted while preparing the report. The efforts made by the MSs, and the other reporting countries are gratefully acknowledged.
Data on AMR collected by the EU MSs and compiled in the EUSR on AMR are also used to perform wider analyses, such as the Joint Report on Consumption of Antimicrobial Agents and AMR in animals, food, and humans – Joint Interagency Antimicrobial Consumption and Resistance Analysis (JIACRA), produced by ECDC, EFSA and EMA, under a One Health approach on a regular basis (2015, 2017, 2021) (ECDC, EFSA, and EMA, 2021). The JIACRA report provides evidence‐based analysis of the possible association between AMC and AMR in humans and food‐producing animals by focusing on combinations of antimicrobials and bacterial species considered important for public health.
1.1. Monitoring and reporting of antimicrobial resistance in the EU 12
1.1.1. Humans: monitoring of antimicrobial resistance
Together with its Food‐ and Waterborne Diseases and Zoonoses (FWD) network, ECDC has developed an EU protocol for harmonised monitoring of AMR in human Salmonella and Campylobacter isolates (ECDC, 2016, 2021). This document is intended for the National Public Health Reference Laboratories to guide the susceptibility testing required for EU surveillance and reporting to ECDC. Consultation was also sought from EFSA, the European Committee on Antimicrobial Susceptibility Testing (EUCAST) and the EURL‐AR to facilitate comparison of data between countries and with results from the AMR monitoring performed in isolates from animals and food products. The protocol is effective from 2014 and supports the implementation of the 2017 European Commission Action Plan on AMR. One of the recommendations is that, for the joint report with EFSA, human data should also be interpreted based on EUCAST epidemiological cut‐off values (ECOFFs). 13 As this requires quantitative data, ECDC introduced reporting of quantitative antimicrobial susceptibility testing (AST) results in the 2013 data collection. From 2019 data collection, it has also been possible to report resistance predicted from whole genome sequencing. Since Decision 2018/945/EU came into force in July 2018, national public health reference laboratories are obliged to report their AMR test results to ECDC according to the methods and criteria specified in the EU protocol.
The protocol also proposes a testing algorithm for screening and confirmation of ESBL‐producing Salmonella spp., including detection of AmpC. Some laboratories have implemented this, while others use a modification of the algorithm or test the suspected isolates directly with PCR or WGS.
External quality assessments to support laboratories in implementing the recommended test methods and antimicrobials and obtaining high‐quality AST results are provided by ECDC via a contract with Statens Serum Institute in Denmark.
1.1.2. Animals and food: monitoring of antimicrobial resistance
According to Commission Implementing Decision (EU) 2020/1729, which applies from 1 January 2021 until December 2027, monitoring of AMR is mandatory in Salmonella spp., Campylobacter coli (C. coli), Campylobacter jejuni (C. jejuni) and indicator E. coli, in the major domestically produced animal populations and their derived meat. Further characterisation is required for E. coli and Salmonella isolates showing resistance to extended‐spectrum cephalosporins and carbapenems. Moreover, specific monitoring of ESBL‐, AmpC‐ and carbapenemase (CP)‐producing E. coli is also required. Monitoring is performed on a rotating basis, targeting fattening pigs and bovine animals under 1 year of age and meat derived thereof in odd years and poultry populations (broilers, laying hens, fattening turkeys) and derived meat in even years, as specified by the legislation.
Monitoring AMR in food‐producing animals is performed in domestically produced animal populations, corresponding to different production types to collect data that could be combined with data on exposure to antimicrobials. From 2021, monitoring of imported fresh meat at border control posts shall also be undertaken to complement AMR monitoring in food‐producing animals. MSs may also voluntarily perform complementary monitoring for MRSA. Representative random sampling of food‐producing animals and derived meat is based on a generic proportionate stratified sampling and performed according to the legislation and the technical specifications issued by EFSA.
Microdilution methods for testing should be used and results interpreted using EUCAST ECOFFs to understand ‘microbiological’ resistance. The harmonised panels of antimicrobials used for Salmonella, Campylobacter and indicator E. coli include substances important for human health, such as critically important antimicrobials (CIAs), and can provide clearer insight into the resistance mechanisms involved. The concentration ranges to be used encompass both the ECOFF and the clinical breakpoints (CBPs), as defined by EUCAST, allowing for comparison with data coming from humans. For Salmonella and E. coli, a supplementary panel of antimicrobial substances for testing isolates showing resistance to third‐generation cephalosporins or carbapenems in the first panel is also used. From 2021, whole genome sequencing (WGS) is authorised as an alternate method to conventional phenotypic testing for isolates obtained for the specific monitoring of ESBL/AmpC/CP‐producing E. coli and for indicator E. coli or Salmonella spp. isolates showing resistance to extended‐spectrum cephalosporins and carbapenems from routine monitoring. WGS is authorised on a voluntary basis only; however, technical conditions on the WGS technique have been imposed to ensure data comparability (EFSA, 2020).
External quality assurance is provided by the EURL‐AR, which distributes panels of well‐characterised organisms to all MSs for susceptibility testing, arranges proficiency tests (PTs) trials for the National Reference Laboratories for Antimicrobial Resistance (NRLs‐AR) of the MSs every year, and, together with EFSA and the MSs, performs a reference testing exercise that includes re‐testing the antimicrobial susceptibility and WGS analysis of selected isolates (Appendix F, Materials and methods). The EURL‐AR also provides a source of reference for MSs when there are issues or problems with the susceptibility test methodology.
Data reporting is performed at the isolate level to enable analyses on the occurrence of resistance and patterns of multidrug resistance (MDR). The reporting of isolate‐based data also allows in‐depth phenotypic characterisation of certain resistance mechanisms, e.g. third‐generation cephalosporin and carbapenem resistance. The voluntary reporting of WGS data from 2021 on ESBL/AmpC/CP‐producing E. coli and Salmonella isolates will facilitate an understanding of the potential contribution of food‐producing animals and derived food to the burden of AMR in humans (EFSA, 2019).
1.2. Further harmonised monitoring of antimicrobial resistance
To facilitate data comparability, the AMR surveillance methodology should be harmonised across countries as much as possible. The main issues when comparing AMR data originating from different countries are the use of various laboratory methods and different interpretive criteria for resistance. These issues have been addressed by the development of ECDC's protocol for harmonised monitoring and reporting of resistance in humans and by the legislation on harmonised monitoring in food‐producing animals and derived meat. To respond effectively to the constantly evolving threat of AMR, ongoing enhancement and specific adaptations will be regularly required. Under the 2017 Action Plan on AMR, the European Commission is committed to reviewing this legislation to consider new scientific developments and data collection needs. In 2019, EFSA received a mandate from the European Commission to provide recommendations on harmonised randomisation procedures for AMR monitoring. The new technical specifications were published in November 2020 (EFSA, 2020), with the new legislation on the monitoring and reporting of AMR in animals and food enacted on 17 November 2020 (see text box below).
New legislation on the monitoring and reporting of AMR in animals and food comes into effect on 1 January 2021
Monitoring of AMR is essential to have comprehensive and reliable information on the development and spread of resistant bacteria and resistant determinants. AMR data provide insights to inform decision‐making and facilitate the development of appropriate strategies and actions to manage AMR at the EU level. In its Communication of 29 June 2017 to the Council and the European Parliament – A European One Health Action Plan against AMR, the Commission committed to review EU implementing legislation, namely Commission Implementing Decision (EU) 2013/652, on monitoring AMR in zoonotic and commensal bacteria in food‐producing animals and food to take into account new scientific developments and data collection needs. After this, EFSA issued the new technical specifications, for implementing updated guidelines for the harmonised monitoring of AMR in food‐producing animals and derived meat and to ensure continuity in assessing occurrence and temporal trends in resistance (EFSA, 2019).
On November 17, 2020, the European Commission laid down the new technical specifications in Commission Implementing Decision (EU) 2020/1729 and repealed Commission Implementing Decision (EU) 2013/652. The new legislation came into effect on 1 January 2021, and updates technical specifications for harmonised AMR monitoring and reporting to include the monitoring of AMR in derived meat sampled at border control posts, the testing of new substances, and authorises WGS as an alternate method to phenotypic testing, for the specific monitoring of ESBL/AmpC/CP‐producing E. coli and indicator E. coli and Salmonella isolates with resistance to extended cephalosporins or carbapenems. The new rules apply to monitoring performed in 2021 onwards.
1.3. The 2020–2021 EU Summary Report on AMR
This EUSR presents AMR data on zoonotic and indicator bacteria from humans, animals and food collected in 2020 and 2021, jointly analysed by the EFSA and the ECDC. This report includes an introduction section, followed by five main chapters on AMR in Salmonella, Campylobacter, indicator E. coli, ESBL/AmpC/CP‐producing Salmonella and E. coli, and MRSA, with sections detailing resistance in isolates from humans, food‐producing animals and derived meat. A section on key findings is included at the beginning of each chapter. Appendices containing complementary information are located at the end of the report. The list of annexes is available at the end of the report, and available on the EFSA Knowledge Junction community on Zenodo at: https://doi.org/10.5281/zenodo.7544221.
For food‐producing animals and derived meat, most data reported by the MSs in 2021 comprised data collected in accordance with Commission Implementing Decision (EU) 2020/1729. For 2020, the data collected by MS were in accordance with Commission Implementing Decision (EU) 2013/652 (repealed on 17 November 2020). Quantitative antimicrobial susceptibility data for Campylobacter, Salmonella and indicator E. coli isolates from animals and food were interpreted using ECOFFs. The occurrence of resistance, complete susceptibility (CS) and MDR is reported at the country and EU level, along with the results from the phenotypic monitoring of resistance to third‐generation cephalosporins and/or carbapenems caused by ESBL/AmpC/CP‐producing Salmonella and E. coli. Results from the monitoring of MRSA in food and animals are also reported for countries that contribute data.
For human data in 2021, MSs reported results from antimicrobial susceptibility testing of Salmonella spp. and Campylobacter spp. isolates from clinical cases of salmonellosis and campylobacteriosis. Phenotypic test results were reported by MSs to TESSy either as quantitative or categorical/qualitative data at the isolate level according to the EU protocol for harmonised monitoring of AMR in human Salmonella and Campylobacter (ECDC, 2016, 2021). Quantitative phenotypic data were interpreted using EUCAST ECOFFs, where available, to understand microbiological resistance. Qualitative phenotypic data were interpreted using clinical breakpoints (CBPs). CBPs enable clinicians to choose the appropriate treatment based on information relevant to the individual patient while ECOFFs help epidemiologists identify small changes in bacterial susceptibility, which may indicate emerging resistance and allow for appropriate control measures to be considered. The breakpoints for ‘clinical’ resistance are often less sensitive than the ECOFF for a specific bacterium–drug combination resulting in higher levels of ‘microbiological’ resistance than ‘clinical’ resistance. By combining the categories of ‘clinically resistant’ (R) and ‘susceptible with increased exposure’ (I) into one category, however, close correspondence with the ECOFF can be achieved. A couple of countries reported resistance predicted from WGS. Such results are considered to correspond to the ECOFF with a separation between wild‐type and non‐wild‐type isolates. For assessing MDR in Salmonella and Campylobacter, ECDC and EFSA have agreed on a harmonised panel of nine and four antimicrobial classes, respectively, for better comparison between the two sectors.
Information on the materials and methods used in this EUSR on AMR can be found in Appendix F – ‘Materials and methods’ at the end of this document. Additional information on the human data reported in 2020 can also be found in the European Union Summary Report on Antimicrobial Resistance in zoonotic and indicator bacteria from humans, animals and food in 2019/2020 (EFSA and ECDC, 2022).
Effect of the UK withdrawal on the analysis of AMR data at the EU
As a consequence of the UK withdrawal from the EU on 31 January 2020, the entry into force of the Withdrawal Agreement was ratified by the UK and the EU. The AMR data retrieved until 2019 covered all 28 EU Member States (MSs), which during that period included the UK. From 1 February 2020, the UK withdrew and became a ‘third‐country’ in relation to the EU, with final withdrawal effective after a transition period ending on 31 December 2020. The UK's withdrawal from the EU impacts the AMR data reported at the EU level in 2020 and 2021. UK data from 2020 are included in reporting and are shown with non‐MSs in the relevant tables and figures in this report. For 2021, data at the EU level are reported in accordance with the membership of the EU (i.e. EU without the UK). In 2021, the only United Kingdom data that were reported to EFSA were from Northern Ireland. In accordance with the Agreement on the withdrawal of the United Kingdom from the European Union, and in particular with the Protocol on Ireland/Northern Ireland, the European Union requirements on data sampling are also applicable to and in the United Kingdom with respect to Northern Ireland. Therefore, pursuant to Article 5(4) and Section 24 of Annex 2 of the Protocol on Ireland/Northern Ireland, which is an integral part of the Agreement on the withdrawal of the United Kingdom of Great Britain and Northern Ireland from the European Union and the European Atomic Energy Community, for the purpose of this report, references to MSs should be read as including Northern Ireland, despite it being part of the United Kingdom. Hence, the European Union requirements on data sampling were also applicable to Northern Ireland and data transmitted by the United Kingdom (Northern Ireland) have been assigned to the MSs group.
2. Antimicrobial resistance in Salmonella spp.
Monitoring of non‐typhoidal Salmonellas
Non‐typhoidal Salmonellas (NTS) are the focus of this section, which summarises the occurrence and AMR patterns of isolates recovered from various food‐producing animal populations and their derived carcases. Whereas typhoidal salmonellas are human host‐adapted organisms that cause typhoid fever and paratyphoid fever; non‐typhoidal strains may be host generalists, infecting or colonising a broad range of animals or tend to host specificity to particular animal species (Crump et al., 2015). Typhoidal salmonellas refer to Salmonella enterica subsp. enterica serovars Typhi, Paratyphi A, Paratyphi B (d‐tartrate negative) and Paratyphi C, while all other serovars within the subspecies enterica (including the d‐tartrate positive Paratyphi B variant Java) refer to NTS.
The World Health Organisation (WHO) states that transmission of bacterial infection from non‐human sources to humans, with the ability to cause disease, is more evident in particular bacteria (including non‐typhoidal Salmonella, Campylobacter spp. and E. coli) and comments that the potential for such transmission should be recognised (WHO, 2019). In 2021, salmonellosis was the second most common food‐borne zoonosis in the European Union, with 60,050 confirmed human cases (an increase compared with 2020 but still about a 20% decrease compared with the pre‐pandemic situation in 2019), as well as the most frequent cause of food‐borne outbreaks accounting for 19% of all food‐borne outbreaks reported in 2021 (EFSA and ECDC, 2022).
2.1. Key findings
Among the reporting countries the number of Salmonella spp. in isolates from human cases varied considerably: Out of 26 reporting countries (inclusive of EU/EAA countries), six countries reported on very few (< 100) human isolates, while three countries reported more than 1,000 isolates.
Overall resistance to ampicillin, sulfonamides, and tetracyclines was observed at high levels in Salmonella spp. isolates from humans in 2021 and ranged from moderate to very high in isolates from food‐producing animals and poultry carcases, except for laying hens where low levels of resistance were reported.
Over the period, 2013–2021, declining trends in resistance to ampicillin and tetracyclines in isolates from humans was observed in 13 and 11 countries, respectively, accompanied by declines in Salmonella Typhimurium, a serovar commonly associated with pigs and calves.
Overall resistance to fluoroquinolones (ciprofloxacin) was observed at moderate levels in Salmonella isolates from fattening pigs (10.1%) and bovine animals under 1 year of age (calves) (12.7%) from data reported in 2021, and at high to very high levels among isolates recovered from broilers (57.5%), fattening turkeys (65.0%), broiler carcases (69.3%) and turkey carcases (46.9%) in 2020. In Salmonella isolates from humans reported in 2021, the average resistance to ciprofloxacin was 14.9%, with lowest levels observed in S. Typhimurium (7.6%) and S. Typhimurium, monophasic variant (8.9%) and high to extremely high levels in S. Infantis (33.9%) and S. Kentucky (78.1%).
Extremely high resistance to ciprofloxacin was also reported in S. Kentucky isolates from broilers (78.0%), laying hens (91.9%), fattening turkeys (96.6%), broiler carcases (100%) and turkey carcases (93.3%). In S. Enteritidis, the most common serovar detected in humans, resistance to ciprofloxacin and nalidixic acid was 22.6% and 24.8%, respectively. Resistance trends calculated for 2013 to 2021 for human data showed increasing trends in resistance to ciprofloxacin in nine MSs and decreasing trends in five MSs, primarily accompanied by an increase in S. Enteritidis.
Overall resistance to third‐generation cephalosporins was noted at very low levels in isolates from humans in 2021 (1.1% to ceftazidime and 1.1% to cefotaxime on average) and was seldom detected in animal and carcase origins in 2020–2021, except for calves (2.6% to cefotaxime and 1.3% to ceftazidime) and broiler flocks (2.1% to cefotaxime and 2.0% to ceftazidime). Overall, combined resistance to fluoroquinolones and cephalosporins was very low in isolates from both humans and animals but higher in certain Salmonella serovars, e.g. S. Kentucky and S. Infantis.
Among isolates from human cases, S. Enteritidis had the highest levels of resistance to ciprofloxacin and colistin (22.6% and 17.6%, respectively) compared to all serovars (14.9% and 5.1%, respectively). S. Kentucky isolates from human cases were characterised by overall high to extremely resistance levels for ampicillin 62%, ciprofloxacin 77%, tetracycline 57%, sulfamethoxazole 51%, gentamicin 27.9%, and low to moderate levels of resistance to cefotaxime/ceftazidime 6% and chloramphenicol 12.6%.
Multidrug resistance (MDR) was overall high (22.5%) among Salmonella spp. reported in human cases in the EU, ranging from low levels among S. Enteritidis (1.9%) to very high among S. Kentucky (54.8%) and extremely high for monophasic S. Typhimurium 1,4,[5],12:i:‐ (78.4%). Similarly, MDR was observed at moderate to very high levels in Salmonella spp. recovered from carcases of turkeys and broilers (19.1% and 53.6%, respectively) and at high levels for fattening pigs (39.1%), calves (30.4%), fattening turkeys (41.7%) and fattening broilers (44.0%), except for laying hens which had low‐level MDR (6.0%).
Overall, in 2021, complete susceptibility (CS) in Salmonella spp. isolates from humans was observed to be 60.0%. For animal data where there is some difference in the harmonised panel of antimicrobials included for CS analysis compared to human data (e.g. inclusion of amikacin for 2021 animal data), CS was high for pigs (40.5%) and very high in calves (55.7%). For 2020 data on poultry flocks and carcase origins, CS ranged from high (24.4%) in meat from broilers to extremely high (75.6%) in laying hens.
At the reporting EU group level, the overall proportion of presumptive ESBL‐ or AmpC‐ producers was from very low to low among Salmonella isolates recovered from all food‐producing animal populations and carcases of broilers and very low in isolates from human cases, although higher resistance was observed in specific Salmonella serovars. No carbapenemase‐producing Salmonella spp. were isolated from human cases in 2021, nor in animal isolates from 2020 to 2021.
2.2. Data on AMR in Salmonella spp. addressed
Commission Implementing Decision (EU) 2020/1729 stipulates detailed protocols for harmonising AMR monitoring and reporting in zoonotic and commensal bacteria. In 2020, the monitoring of carcases of broilers and fattening turkeys at slaughter was mandatory, in accordance with Regulation (EC) No 2073/2005. Additionally, in 2020, the monitoring of AMR in Salmonella isolates recovered from faecal samples and/or environmental samples (boot swabs or dust) of broiler, laying hen and fattening turkey flocks was mandatory, in accordance with Regulation (EC) No 2160/2003, collected as part of National Control Programmes (NCPs) for Salmonella in poultry. While for 2021, the AMR monitoring in Salmonella isolates recovered from caecal contents of fattening pigs and bovine animals under 1 year of age taken at slaughter was mandatory.
This chapter describes 2021 AMR data from bovine animals under 1 year of age (referred to as ‘calves’) and fattening pigs (referred to as ‘pigs’). As well as 2020 AMR data on Salmonella isolates collected from flocks of broilers, fattening turkeys, and laying hens. Data for Salmonella spp. from human cases are reported for both 2020 and 2021. Section 2.3 however only presents data for 2021 since 2020 data from humans were published in the EU Summary report for 2019/2020 (EFSA and ECDC, 2022). Results from antimicrobial susceptibility testing (AST) in Salmonella isolates from human cases includes that of prevalent serovars corresponding to those occurring in animal species.
Data from Salmonella spp. isolates include results for all serovars reported from the different carcases/animal origins, with one isolate per Salmonella serovar from the same epidemiological unit per year being tested for AMR (Commission Implementing Decision (EU) 2020/1729). As the potential for acquiring AMR markedly varies between serovars, the relative contribution of different serovars to the total occurrence of resistance results can influence the overall resistance levels reported for Salmonella spp. for the different carcases/animal origins. Therefore, results are also presented for selected serovars if they have a high prevalence (i.e. recovery rate from samples) or are considered important to public health. Resistance profiles were also considered when less than ten isolates were recovered from a given carcase/animal in a country to account for the low prevalence of certain serovars, to prevent exclusion of emerging serovars, and to ensure that the analysis included all relevant data. Note that some figures in this chapter only present individual MS data where ten or more Salmonella spp. were reported, although the occurrence of resistance at the MS‐group level includes all reported isolates.
Variations in Salmonella prevalence from food‐producing animal or carcase origins
In 2020 and 2021, countries reported Salmonella spp. data from the different origins according to their national situation. Of note, some MSs did not obtain any Salmonella isolates from animal or meat origins, therefore data are not presented for those countries. In 2020, the number of countries reporting results for broiler carcases was considerably higher than for turkey carcases because the size of the turkey sector is relatively small in some MSs, with production levels below the threshold at which mandatory monitoring is required. Similarly, in 2021, the number of MSs reporting data from pigs was considerably higher than MSs reporting data from calves. Additionally, the number of isolates reported by countries differed due to varying Salmonella prevalence, and these factors may introduce a source of variation in results when considering all reporting countries.
In this chapter, the occurrence of resistance refers to microbiological resistance (i.e. determined by the ECOFF value) unless otherwise stated. The level of resistance is described as either ‘rare’: < 0.1%, ‘very low’: 0.1%–1.0%, ‘low’: > 1%–10.0%, ‘moderate’: > 10.0%–20.0%, ‘high’: > 20.0%–50.0%, ‘very high’: > 50.0%–70.0%, ‘extremely high’: > 70.0%. The significance of a given level of resistance depends on the antimicrobial substance and its relative importance in human and veterinary medicine. The small sample size from some reporting countries should be considered when interpreting results.
2.3. Humans: occurrence of antimicrobial resistance in Salmonella
2.3.1. Data reported
For 2021, 24 MSs and two non‐MSs reported data on AMR in Salmonella isolates from human cases of non‐typhoidal salmonellosis. This is four countries more than in 2020. Twenty‐one countries provided data as measured values (quantitative data), four as data interpreted with clinical breakpoints and one as predicted phenotypic resistance based on whole genome sequencing. Not all countries reported results for all antimicrobials in the harmonised panel (ECDC, 2016, 2021). The reported data represented 20.6% of the confirmed human cases with non‐typhoidal Salmonella reported in the EU/EEA in 2021.
2.3.2. Occurrence of resistance to commonly used antimicrobials in human and/or veterinary medicine
In 2021, high proportions of human Salmonella isolates were resistant to ampicillin (25.3%), sulfonamides (26.8%), and tetracyclines (26.2%) (see Figure 1; Table 1; Annex A). By serovar, resistance to these compounds ranged from low (3.1%–4.9%) in S. Enteritidis to extremely high in S. Kentucky (51.6%–62.9%) and monophasic S. Typhimurium 1,4,[5],12:i:‐ (84.5%–88.2%) (Annex A, Tables 2, 4, and 6). The variation in the proportion of resistance was large when considering countries reporting ten or more isolates. Overall, for all Salmonella spp., outliers in terms of high proportion of resistance were observed in Luxembourg for sulfonamides (75.0%) and Italy for tetracycline (52.4%) (Annex A, Table 1). For S. Enteritidis, outliers with a high proportion of resistance were observed in Greece (28.0%) and Luxembourg (70.7%) for sulfonamides, and in Slovakia for tetracycline (15.0%) (Annex A, Table 2). For S. Typhimurium, outliers were observed in Lithuania for ampicillin (90.9%), and Luxembourg for sulfonamides (71.4%) (Annex A, Table 3). For monophasic S. Typhimurium 1,4,[5],12:i:‐, Estonia and Sweden reported a higher proportion of ampicillin resistance (100%) compared to other countries and Austria and Hungary a lower proportion (70.5% and 78.3%, respectively) (Annex A, Table 4). Austria also reported a lower proportion of resistance to sulfonamides in the same serovar. For S. Infantis, Italy reported a much higher proportion of resistance to ampicillin than the EU average (65.6% vs. 15.7%) and for tetracycline (81.2%), along with Austria (64.2%) (Annex A, Table 5). Considering S. Derby, only France observed high levels of resistance to sulfonamides (43.1%) (Annex A, Table 7). Only three countries reported more than 10 S. Kentucky isolates, meaning there was insufficient data to be included in the analysis presented in Figure 1.
Figure 1.
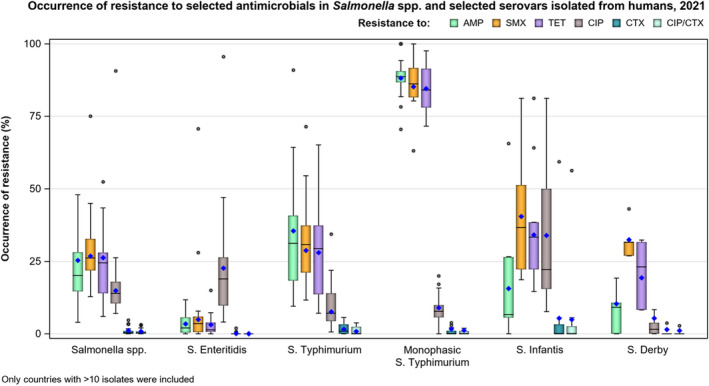
- Horizontal line: median; diamond: resistance at reporting MS group level; lower and upper box boundaries: 25th and 75th percentiles. For each serovar, only countries reporting 10 or more isolates are included. S. Kentucky is excluded from analysis as only three countries reported sufficient number of isolates.
Table 1.
Occurrence of resistance to selected and critically important antimicrobials in Salmonella spp. and selected serovars from humans, 2021
| EU total | AMP | SMX | TET | CIP | CTX | Combined CIP/CTX | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % Res | N | % Res | N | % Res | N | % Res | N | % Res | N | % Res | |
| Salmonella spp. (24 MSs) | 11,832 | 25.3 | 6,872 | 26.8 | 10,949 | 26.2 | 11,725 | 14.9 | 11,572 | 1.1 | 11,532 | 0.8 |
| S. Enteritidis (23 MSs) | 3,194 | 3.4 | 1,724 | 4.9 | 2,616 | 3.1 | 3,103 | 22.6 | 3,005 | 0.1 | 2,973 | 0 |
| S. Typhimurium (22 MSs) | 1,382 | 35.5 | 872 | 28.8 | 1,330 | 28.0 | 1,373 | 7.6 | 1,355 | 1.6 | 1,353 | 0.9 |
| Monophasic S. Typhimurium (17 MSs) | 1,958 | 88.2 | 1,236 | 85.2 | 1,913 | 84.5 | 1,958 | 8.9 | 1,957 | 1.7 | 1,957 | 1.2 |
| S. Infantis (20 MSs) | 530 | 15.7 | 336 | 40.5 | 499 | 34.1 | 528 | 33.9 | 525 | 5.3 | 525 | 5.0 |
| S. Kentucky (12 MSs) | 105 | 62.9 | 62 | 51.6 | 86 | 58.1 | 105 | 78.1 | 105 | 5.7 | 105 | 5.7 |
| S. Derby (14 MSs) | 261 | 10.3 | 148 | 32.4 | 259 | 19.3 | 260 | 5.4 | 261 | 1.5 | 260 | 1.2 |
Overall, resistance to gentamicin was low (1.8%) and across all reported serovars (Annex A, Tables 1–7) except in S. Kentucky where gentamicin resistance was high (27.9%) at the EU level (Annex A, Table 6). Similarly, levels of trimethoprim resistance were overall low among Salmonella spp. (5.8%) (Annex A, Table 1), but moderate in S. Infantis (15.5%) and high in S. Kentucky (24.4%) (Annex A, Tables 5 and 6).
2.3.3. Occurrence of resistance to highest‐priority critically important antimicrobials (hpCIAs) and last resort antimicrobials
The proportion of Salmonella isolates resistant to the highest‐priority critically important antimicrobial (hpCIA) ciprofloxacin was overall 14.9% (see Figure 1; Table 1). A high proportion of resistance to ciprofloxacin was observed in S. Infantis isolates (33.9%), while an extremely high proportion was observed in S. Kentucky isolates (78.1%) (Figure 1; Annex A, Tables 5 and 6). At the country‐level, an extremely high proportion of ciprofloxacin in Salmonella spp. was observed in Poland (90.7%), with much of the resistance to be found in S. Enteritidis isolates (95.5%) (Annex A, Tables 1 and 2). For Poland, 2021 is the first year that quantitative data has been provided to ECDC, allowing for the application of the most up to date ECOFF and CBP to the test values. Austria and Italy also reported extremely high resistance to ciprofloxacin in S. Infantis isolates (73.6% and 81.3%, respectively) (Annex A, Table 5). Caution should be taken when interpreting results for some countries as they report data on a small number of isolates.
For cefotaxime and ceftazidime, representing third‐generation cephalosporins, another class of hpCIAs for Salmonella, resistance levels were generally low among Salmonella spp. (1.1%, respectively) (Annex A, Table 1), with low levels of resistance ranging from 0.1% to 6.2% across the serovars of interest (Annex A). Resistance was more pronounced in S. Infantis and S. Kentucky isolates (range: 5.2%–6.2%) (Annex A, Tables 5 and 6). When only considering countries with more than 10 isolates for a serotype, more reported low resistance to either third‐generation cephalosporin, except for Italy, which reported very high resistance in S. Infantis isolates (59.4% and 56.3%, respectively) (Annex A, Table 5).
Only nine countries tested resistance to last line antimicrobials azithromycin and tigecycline. Resistance was overall low among Salmonella spp. (0.5% and 1.4%, respectively, Annex A, Table 1). Among the individual serovars, the highest proportion of isolates resistant to azithromycin was observed in S. Infantis and S. Derby (both 2.0%) and S. Kentucky (3.9% – see Annex A, Tables 5–7). In 2021, the ECOFF applied for azithromycin was changed from MIC > 1 mg/L to MIC > 0.5 mg/L to harmonise with EFSA animal and carcase data. This likely explains the higher proportion of isolates resistant to azithromycin compared to 2020 (1.4% compared to 0.2%) Resistance to colistin was detected in 5.1% of Salmonella isolates, with resistance being most pronounced in S. Enteritidis isolates (17.6%), a serovar belonging to group D Salmonella which tend to show a higher natural tolerance to colistin (Agersø et al., 2012; Ricci et al., 2020).
Combined resistance to both ciprofloxacin and cefotaxime was overall very low in Salmonella spp. in human cases (0.8%) (Figure 2a; Annex A, Table 8). Notably, for S. Enteritidis, combined resistance to ciprofloxacin and cefotaxime was only reported in one isolate out of 2,973 (< 0.1%) (Annex A, Table 8). Similarly, for S. Typhimurium and monophasic S. Typhimurium, combined resistance was also observed to be very low or low (0.9% and 1.2%, respectively) (Figure 2c). When considering other serovars, combined resistance was observed to be low in S. Derby isolates (1.2%) and higher in S. Infantis and S. Kentucky isolates (overall 5.0% and 5.7%, respectively) although few countries reported more than ten isolates (Figure 2b; Annex A, Tables 11 and 12). For S. Infantis, Italy was the major contributor to overall combined microbiological and clinical resistance, with 56.3% of isolates displaying combined resistance (Figure 2b; Annex A, Table 11).
Figure 2.
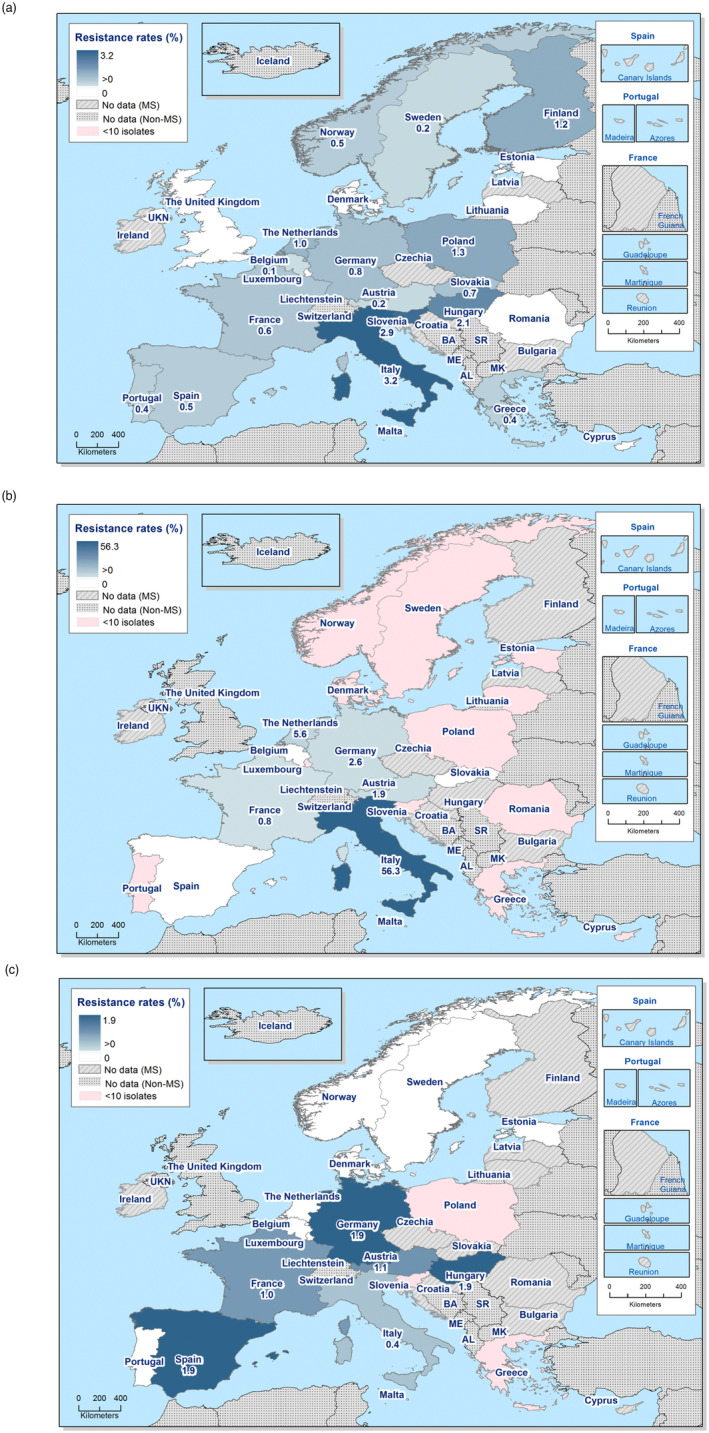
Spatial distribution of combined ‘microbiological’ resistance to ciprofloxacin and cefotaxime among (a) Salmonella spp., (b) S. Infantis and (c) monophasic S. Typhimurium isolated from human cases, 2021 (pink indicates fewer than ten isolates tested)
2.3.4. ESBL, AmpC and carbapenemase‐producing Salmonella
In 2021, of the 23 MSs and one non‐MS reporting data on third‐generation cephalosporins, 16 MSs and one non‐MS reported very low‐ or low‐level resistance, and six MSs reported no resistance. Two countries reporting cephalosporin‐resistant isolates did not provide further details on phenotypic/genotypic characterisation, and these isolates were excluded from analysis in Table 2 and Annex A, Table 15. A small number of isolates from one country that were not further typed were also not included in Table 2 and Annex A, Table 15. In Italy, there is a special focus on ESBL/AmpC monitoring in Salmonella where primary laboratories are requested to send any isolates resistant to cefotaxime and/or ceftazidime to the national public health reference laboratory for confirmation. This may have resulted in an overrepresentation of such isolates in the Salmonella AMR dataset from Italy.
Table 2.
ESBL, AmpC and carbapenemase phenotypes and genotypes in Salmonella spp. isolates from humans by serovar for all reporting EU/EEA countries, 2021
| Serovar | Tested for CTX and/or CAZ | Res to CTX and/or CAZ | Resistance phenotype | Genotype | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ESBL | AmpC | AmpC + ESBL | Carbapenemase | ||||||||
| N | N | N | % | N | % | N | % | N | % | ||
| S. Brandenburg | 110 | 2 | 2 | 1.8 | blaCMY‐2 (1), blaCMY‐4 (1) | ||||||
| S. Derby | 260 | 4 | 3 | 1.2 | blaCTX‐M‐1 (3) | ||||||
| S. Enteritidis | 2,448 | 1 | 1 | Unknown | |||||||
| S. Give | 34 | 1 | 1 | 2.9 | blaCTX‐M‐3 (1) | ||||||
| S. Goldcoast | 39 | 2 | 2 | 5.1 | blaCMY‐2 (2) | ||||||
| S. Infantis | 517 | 29 | 27 | 5.2 | blaCTX‐M‐9 group (3), blaCMY‐2 (1), blaCTX‐M‐1 (14), blaCTX‐M‐55 (1), blaSHV‐12 (2), blaSHV‐134 (1), blaSHV‐2a (1), blaCTX‐M (1), blaCTX‐M‐65 (5) | ||||||
| S. Paratyphi B var Java | 53 | 1 | 1 | 1.9 | blaCTX‐M (1) | ||||||
| S. Kedougou | 32 | 1 | 1 | 3.1 | blaCTX‐M‐8 (1), blaSHV‐12 (1) | ||||||
| S. Kentucky | 105 | 7 | 4 | 3.8 | blaCTX‐M‐14 (1), blaCTX‐M‐14b (1), blaCTX‐M (1) | ||||||
| S. Kenya | 19 | 1 | 1 | 5.3 | blaCTX‐M‐15 (1) | ||||||
| Monophasic S. Typhimurium 1,4,[5],12:1:‐ | 1,867 | 30 | 23 | 1.2 | 6 | 0.3 | blaCMY‐2 (6), blaCTX‐M‐9 (2), blaCTX‐M (2), blaCTX‐M‐1 (12), blaCTX‐M‐14 (1), blaCTX‐M‐32 (1), blaCTX‐M‐55 (1) | ||||
| S. Newport | 234 | 1 | 1 | 0.4 | blaCTX‐M‐55 (1) | ||||||
| S. Rissen | 49 | 1 | 1 | 2.0 | blaCMY‐2 (1) | ||||||
| S. Subsp I (enterica) | 44 | 2 | 2 | 4.5 | blaCTX‐M‐1 (1) | ||||||
| S. Typhimurium | 1,246 | 14 | 11 | 0.9 | 1 | 0.1 | blaCMY‐2 (1), blaCTX‐M‐1 (1), blaCTX‐M‐5 (1), blaCTX‐M‐65 (1), blaCTX‐M‐9 (5), blaCTX‐M (1), blaCTX‐M‐8 (1) | ||||
| S. Worthington | 4 | 1 | 1 | 2.5 | blaCTX‐M (1) | ||||||
CTX: cefotaxime; CAZ: ceftazidime; ESBL: extended spectrum beta‐lactamase. Genotypic data are reported at the family level. Slovakia and Hungary did not report results that could be included in this table.
Presumptive ESBL‐producing Salmonella were identified in 0.8% of the tested isolates, ranging by MS from 0.1% in Belgium to 3.5% in Italy (Annex A, Table 15). AmpC was less frequent, identified in 0.1% of tested isolates, with the highest occurrence in Italy (1.3%). No isolates were reported presumptive AmpC‐ and ESBL‐producing, or as carbapenemase‐producing Salmonella (Annex A, Table 15). ESBL was reported in 12 serovars (and in S. enterica subspecies I) in 2021, with the highest proportions observed in S. Infantis isolates (5.2%, n = 517), S. Kenya (5.3%, n = 19) and S. enterica subspecies I (4.5%, n = 44) (Table 2). AmpC‐type β‐lactamases were overall reported in 0.1% of tested isolates and in five serovars, with the highest proportion observed in S. Goldcoast (5.1%, n = 39). No isolates were reported as resistant to meropenem in 2021 (Annex A, Table 1). It should however be noted that in six of 24 reporting countries, meropenem results were interpreted using the EUCAST clinical breakpoint (CBP), which is substantially higher (+4 dilutions) than the ECOFF.
2.3.5. Complete susceptibility (CS) and multidrug resistance (MDR)
In this report, complete susceptibility (CS) is defined as susceptibility to each of the nine antimicrobial classes tested in the harmonised panel described by the ECDC (ECDC, 2016, 2021). Multidrug resistance (MDR) is defined as resistance to three or more antimicrobial classes among Salmonella isolates from human cases.
The level of CS was 60.0% in Salmonella spp. with the highest proportion in S. Enteritidis (72.1%), followed by S. Derby (61.5%), S. Typhimurium (58.9%) and S. Infantis (54.5%). The lowest levels of CS were observed in S. Kentucky (19.4%) and monophasic S. Typhimurium (4.5%) (Figure 3; Annex A, Tables 16–22).
Figure 3.
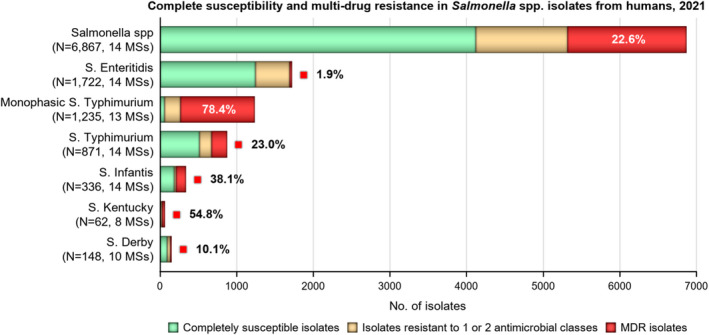
Number of multidrug (MDR) resistant isolates, isolates resistant to one and/or two antimicrobial classes and completely susceptible Salmonella isolates from humans in 2021
MDR was high overall (22.6%, n = 6,867) among Salmonella spp. reported from human cases in the EU (Figure 3; Annex A, Table 16). For the investigated serovars, MDR was most frequently reported among monophasic S. Typhimurium 1,4,[5],12:i:‐ (78.4%, n = 871), S. Kentucky (54.8%, n = 62), followed by S. Infantis (38.1%, n = 336), S. Typhimurium (23.0%, n = 871), S. Derby (10.1%, n = 148) and lastly S. Enteritidis (1.9%, n = 1,722) (Figure 3; Annex A, Tables 17–22). Ten isolates (four S. Infantis, three S. Typhimurium and one each of S. Brandenburg, S. enterica subsp. I and monophasic S. Typhimurium) were resistant to eight of the nine tested substances, only susceptible to meropenem.
2.3.6. Temporal trends
Trends in resistance over the period 2013–2021 were assessed with logistic regression. In 2020, the statistical power of the model used to determine temporal trends was reduced because the number of isolates reported by country was markedly lower in almost all countries compared to previous years as an effect of the pandemic. However, in 2021, most countries reported more data than the year before which has slightly improved the power of the model. Trends varied by country for the different serovars and antimicrobials (Table 3; Annex A, Figures 1–6). As the number of isolates tested in humans is high, small changes in resistance may come out as significant. For Salmonella spp. overall, 13 and 11 countries observed a decrease in resistance to ampicillin and tetracycline, respectively, whereas four and six countries reported an increase. For cefotaxime and ciprofloxacin, six and five countries, respectively, observed a decrease in resistance, while four and nine countries reported an increase (Table 3; Figure 4).
Table 3.
Number of countries with statistically significant (p < 0.05) increasing or decreasing trends in resistance to selected antimicrobials for Salmonella spp. and selected serovars in humans in 2013–2021
| Serovar | Ampicillin | Cefotaxime | Ciprofloxacin/quinolones | Tetracycline | ||||
|---|---|---|---|---|---|---|---|---|
| Incr. | Decr. | Incr. | Decr. | Incr. | Decr. | Incr. | Decr. | |
| Salmonella spp. (24 MSs + 3 non‐MS) | 4 (BE, FI, HU, SI) | 13 (BE, DE, DK, EL, ES, FR, HU, IE, IS, LT, PT, SE, UK) | 4 (HU, IT, SI, UK) | 6 (EE, FR, IE, MT, PL, SK) | 9 (AT, BE, DE, EE, FI, NL, NO, PL, SK) | 5 (ES, FR, HU, MT, SE) | 6 (BE, EE, FI, HU, SI, SK) | 11 (AT, DK, EL, ES, FR, IE, LU, NL, NO, PT, SE) |
| S. Enteritidis (23 MSs + 2 non‐MS) | 5 (AT, BE, NL, SI, SK) | 5 (ES, IE, LT, MT, RO) | – | 1 (PL) | 10 (AT, BE, DE, EE, HU, NO, PL, RO, SI, SK) | 5 (ES, FR, MT, PT, SE) | 8 (AT, BE, DE, IT, NL, SI, SK, UK) | 4 (ES, LT, PL, RO) |
| S. Typhimurium (23 MSs + 3 non‐MS) | – | 13 (AT, CY, DE, EE, ES, FR, IE, IS, LU, NO, PT, SI, UK) | 2 (DE, HU) | 2 (AT, BE) | 4 (DE, LT, NO, SK) | 1 (SI) | – | 13 (AT, DE, EE, EL, ES, FR, HU, IE, LU, NL, NO, PT, UK) |
| Monophasic S. Typhimurium (15 MSs + 2 non‐MSs) | 6 (EE, IT, MT, NL, NO, SE) | 1 (AT) | 1 (IT) | 1 (BE) | 4 (AT, HU, LU, PT) | 2 (IT, NO) | 3 (DK, IT, SE) | 6 (AT, ES, FR, HU, IE, PT) |
| S. Infantis (12 MSs + 1 non‐MS) | 7 (AT, BE, FR, HU, LT, NL, SK) | 1 (ES) | 2 (DE, UK) | 1 (BE) | 5 (BE, DE, ES, NL, SK) | 3 (HU, MT, UK) | 2 (ES, NL) | – |
| S. Kentucky (7MSs + 1 non‐MS) | – | – | – | 1 (MT) | 1 (DE) | – | – | 1 (AT) |
| S. Derby (7 MSs + 1 non‐MS) | 1 (LT) | – | – | – | 1 (DE) | – | 1 (LT) | 1 (FR) |
AT: Austria; BE: Belgium: BG: Bulgaria; CY: Cyprus; DE: Germany; DK: Denmark; EE: Estonia; EL: Greece; ES: Spain; FI: Finland; HU: Hungary; FR: France; IS: Iceland; IT: Italy; LU: Luxembourg; LV: Latvia; MT: Malta; NL: Netherlands; NO: Norway; PL: Poland; PT: Portugal; RO: Romania; SE: Sweden; SI: Slovenia; SK: Slovakia; UK: United Kingdom.
Figure 4.
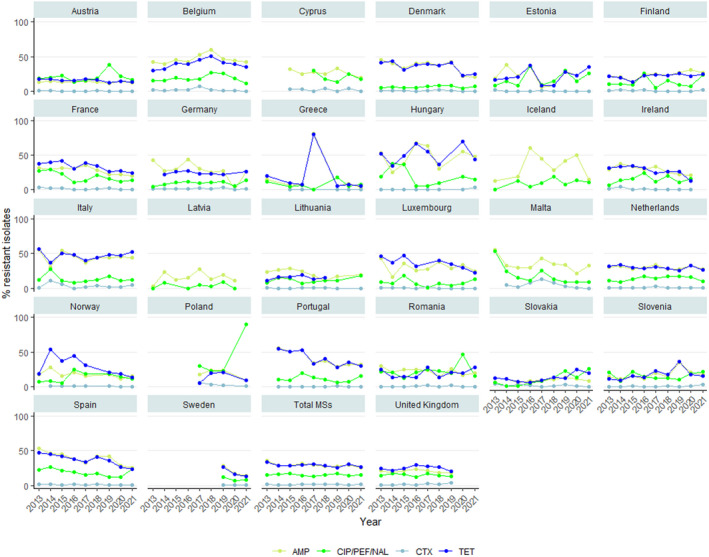
- Data from the United Kingdom included up to 2019. Trend at EU MS group level is excluding UK data.
By serovar, increasing trends in resistance were more commonly observed for ciprofloxacin/quinolones in S. Enteritidis (10 countries) and S. Infantis (five countries). Thirteen countries reported decreasing trends in resistance to ampicillin and to tetracycline in S. Typhimurium while for monophasic S. Typhimurium and S. Infantis, increasing trends in ampicillin resistance were observed in six and seven countries (Annex A, Figures 1–6).
2.3.7. High‐level ciprofloxacin resistance
In 2021, 1.2% (n = 6,162) of Salmonella spp. expressed high‐level resistance to ciprofloxacin (MIC ≥ 4 mg/L, Table 4). Such isolates were reported from eight of the thirteen countries reporting MIC values for ciprofloxacin. Among the twelve serovars reported with MICs of ≥ 4 mg/L, high‐level ciprofloxacin resistance was most frequently observed in S. Kentucky (81.2% of tested S. Kentucky).
Table 4.
Occurrence of high‐level resistance to ciprofloxacin (MIC ≥ 4 mg/L) in Salmonella serovars from human cases in 2021
| Serovar | N | High‐level resistance to ciprofloxacin (MIC ≥ 4 mg/L) | |
|---|---|---|---|
| n | % | ||
| S. Bonn | 1 | 1 | NA |
| S. Enteritidis | 1,174 | 1 | 0.1 |
| S. Infantis | 364 | 3 | 0.8 |
| S. Kedougou | 20 | 1 | 5.0 |
| S. Kentucky | 69 | 56 | 81.2 |
| S. Newport | 153 | 1 | 0.7 |
| S. Potsdam | 5 | 1 | 20.0 |
| S. Rissen | 22 | 1 | 4.5 |
| S. Saintpaul | 27 | 2 | 7.4 |
| S. Thompson | 30 | 1 | 3.3 |
| S. Typhimurium | 840 | 2 | 0.2 |
| Monophasic S. Typhimurium | 1,155 | 1 | 0.1 |
| Unknown | 209 | 5 | 2.4 |
| Other | 2,093 | 0 | 0 |
| Total (13 MSs) | 6,162 | 76 | 1.2 |
Additional data on certain resistance traits of Salmonella isolates from humans are provided hereafter and presented in parallel to corresponding data on Salmonella spp. from animals and food.
2.4. Food‐producing animals and meat thereof: occurrence of antimicrobial resistance in Salmonella
2.4.1. Data reported
In 2021, 25 MS, the United Kingdom (Northern Ireland) and one non‐MS reported AMR data on Salmonella isolates recovered from the caecal contents of pigs at slaughter, and 10 MSs reported AMR data on Salmonella isolates recovered from the caecal contents of calves at slaughter. In addition, three MSs voluntarily reported AMR data on Salmonella isolates recovered from flocks of broilers; six MSs for laying hens and two MSs for fattening turkeys before slaughter. In 2019, under the previous legislation (Commission Implementing Decision (EU) 2013/652), AMR data was mandatory for Salmonella isolates recovered from carcases at slaughter, and a similar number of MSs reported AMR data on pigs (26 MSs, one non‐MS), and calves (seven MS).While, the sampling of caecal contents for Salmonella was voluntary in 2019, and nine MS reported data on pigs, and three MSs reported data on calves.
In 2020, under the previous legislation, AMR data for Salmonella isolates recovered from carcases of broilers and fattening turkeys at slaughter, was reported by 18 MSs and two non‐MSs for broilers, and 8 MSs for fattening turkeys. Additionally, in 2020, 22 MSs and three non‐MSs reported AMR data for Salmonella isolates recovered from flocks of broilers; 24 MSs and two non‐MSs for laying hens and 16 MSs and one non‐MS for fattening turkeys at slaughter.
The reporting of isolate‐based data enables the analysis of MDR patterns, the detection of high‐level ciprofloxacin resistance and combined resistance to ciprofloxacin and cefotaxime (first‐line agents critically important for treating human salmonellosis). As required by Commission Implementing Decision (EU) 2020/1729, the MSs included information on serovars and production type, which allowed for detailed analysis of the occurrence of resistance and MDR by serovar for the different animal/carcase origins (see Appendix C).
Changes in the harmonised panel of antimicrobial substances for the monitoring of AMR in animals and food for Salmonella spp. according to the new legislation
The Commission Implementing Decision (EU) 2020/1729 lays down specific technical requirements, for AMR testing and reporting in representative isolates deriving from randomised sampling in food‐producing animals performed at farm and/or at slaughter and derived meat performed at retail and at border control posts. The new rules apply to monitoring performed from 2021 onwards.
In 2021, amikacin has been added to the harmonised panel of antimicrobials for the monitoring and reporting of AMR in Salmonella and was included in the analyses of the occurrence of resistance, CS and MDR. While amikacin is not used in food‐producing animals, it is commonly used in hospitals to treat urinary tract infections, bacteraemia and intra‐abdominal infections caused by Gram‐negative bacteria. Amikacin was added to the harmonised panel because it is thought to improve the detection of 16S RNA methyltransferases (RMTases) (EFSA, 2019). RMTases have been increasingly associated with carbapenemases, AmpC or ESBL enzymes and fluoroquinolone resistance in Enterobacteriaceae, particularly outside Europe and recently also detected in human cases within Europe (Arca‐Suárez et al., 2022; Fournier et al., 2022).
Additionally, under the new legislation, the ECOFFs and CBPs used to determine the microbiological resistance of Salmonella isolates to some antimicrobial substances have also changed. This is the case for tigecycline: the ECOFF has changed from > 1 to > 0.5 mg/L. Also, the ECOFF for nalidixic acid changed from MIC > 16 mg/L to MIC > 8 mg/L, while the CBP for ciprofloxacin changed from MIC > 1 mg/L to MIC > 0.064 mg/L.
Based on the changes on the current legislation in this report, the occurrence of resistance to tigecycline and nalidixic acid for 2021 data (i.e. pigs and calves) is determined using the new ECOFFs (MIC > 0.5 mg/L and MIC > 8 mg/L, respectively), and for 2020 poultry and meat derived data, tigecycline and nalidixic acid resistance are analysed using the previous ECOFFs (i.e. MIC > 1 mg/L and MIC > 16 mg/L). Also, for ciprofloxacin, clinical resistance will be determined using the previous CBP (MIC > 1 mg/L) for 2020 data, and the new CBP (MIC > 0.064 mg/L) for 2021 data.
Summary data on the occurrence of resistance to commonly used antimicrobials in veterinary medicine (ampicillin, sulfamethoxazole and tetracycline) as well as hpCIAs (ciprofloxacin, cefotaxime and combined resistance to these two antimicrobials) are displayed in Figure 5 for Salmonella isolates from (a) poultry carcases and (b) food‐producing animals and are described in the following text. Annex A presents the occurrence of AMR (%), CS, MDR and combined resistance to ciprofloxacin and cefotaxime, in Salmonella spp. from pigs, calves (corresponding to 2021 data), as well as broilers, laying hens, turkeys and derived meat (corresponding to 2020 data), at the MS and MS‐group level. (Annex A is available on the EFSA Knowledge Junction community on Zenodo at: https://doi.org/10.5281/zenodo.7544221).
Figure 5.
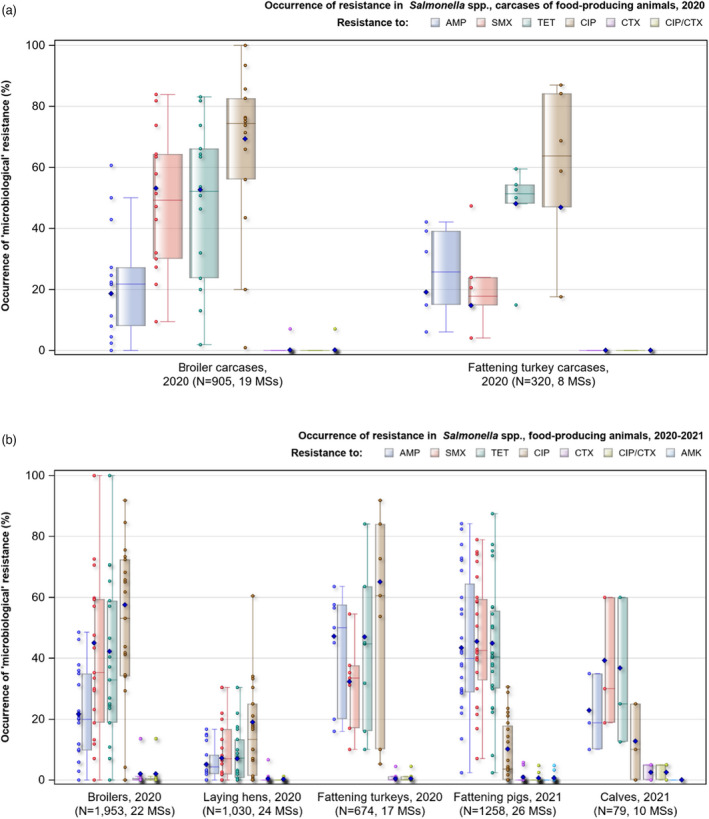
- AMP: ampicillin; SMX: sulfamethoxazole; TET: tetracycline; CIP: ciprofloxacin; CTX: cefotaxime; CIP/CTX: combined ‘microbiological’ resistance to ciprofloxacin and cefotaxime; AMK: amikacin; N: total number of Salmonella spp. isolates reported by MSs; blue diamond shows resistance at the reporting‐MS group level. Horizontal lines represent median; Lower and upper box boundaries, 25th and 75th percentiles, respectively; Blue diamond: resistance at the reporting MS group level Note: Only MSs reporting data for 10 or more isolates are shown in the graph; however, all isolates are included in the calculation of resistance at the reporting‐MS group level.
2.4.2. Occurrence of resistance to commonly used antimicrobials in veterinary medicine
Since 2014, the antimicrobial substances included in the harmonised panel for the monitoring and reporting of AMR in Salmonella from food animals and derived meat have provided continuity of monitoring data and epidemiological tracing of isolates (particularly serovars) with patterns of resistance of interest to public health. The antimicrobial substances included in the panel have been selected because they are either of public health importance or are commonly used in veterinary medicine. Antimicrobial substances such as ampicillin, sulfamethoxazole and tetracycline have been widely used in veterinary medicine for treating infections in production animals. The WHO categorises ampicillin as a ‘critically important antimicrobial’ (CIA) in human medicine, while sulfamethoxazole and tetracycline are categorised as ‘highly important antimicrobials’ (HIA) in human medicine (WHO, 2019).
Carcases of poultry
In 2020, considering all MSs reporting Salmonella spp. data from poultry carcases, the overall resistance to ampicillin, sulfamethoxazole and tetracycline ranged from moderate to very high (Figure 5a; Annex A). Ampicillin resistance was reported at overall moderate levels in both broiler carcases and turkey carcases (18.6% and 19.1%, respectively); sulfamethoxazole resistance was noted at a very high level in broiler carcases and a moderate level in turkey carcases (53.2% and 14.7%, respectively); while tetracycline resistance was noted at an overall very high level in broiler carcases and at a high level in turkey carcases (52.6% and 48.1%, respectively) (Annex A). In addition, among Salmonella isolates recovered from turkey carcases, resistance levels were substantially lower than those obtained from broiler carcases for trimethoprim (3.8% and 16.2%, respectively) (Annex A).
Food‐producing animals
In 2021, among Salmonella spp., most MSs reported high resistance to tetracyclines and sulfonamides recovered from pigs and calves. Overall tetracycline resistance was reported at high levels for pigs and calves (44.9% and 36.7%, respectively), and overall high sulfamethoxazole resistance was also reported at levels of 45.5% and 39.2%, respectively (Annex A). Ampicillin resistance levels were generally observed at similar levels to those of tetracycline and sulfamethoxazole in pigs (43.4%) and slightly lower in calves (22.8%). Overall, resistance levels in Salmonella isolates recovered from both species were low to moderate for other antimicrobial substances in the harmonised panel (Annex A). In 2019, similar overall levels of resistance to the antimicrobial substances in the harmonised panel were reported for pigs, considering the difference in the total number of isolates between the two time periods (EFSA and ECDC, 2021).
For data from 2020 on poultry flocks, overall resistance was high for tetracyclines and sulfonamides in broilers and fattening turkeys. For tetracycline, overall resistance was 42.2% for broilers and 47.0% for fattening turkeys, while for flocks of laying hens, low tetracycline resistance was reported (7.0%) (Annex A). For sulfamethoxazole, high resistance levels were reported for broiler flocks (45.0%) and fattening turkeys (32.3%) in contrast to flocks of laying hens (7.2%) (Annex A). Considering ampicillin, overall resistance was observed at somewhat lower levels than those of tetracycline and sulfamethoxazole within all poultry flocks, with the highest resistance levels in isolates from turkeys (47.2%) (Figure 4b; Annex A).
2.4.3. Occurrence of resistance to highest priority critically important antimicrobials (hpCIAs) and last resort antimicrobials
Use of critically important antimicrobials (CIAs) for the treatment of human infections
(Fluoro)quinolones and third‐generation cephalosporins are categorised as highest‐priority critically important antimicrobials (hpCIA) in human medicine (WHO, 2019). These hpCIAs often constitute first‐line treatment for invasive salmonellosis in humans, and as such, the monitoring of resistance to these compounds in zoonotic bacteria, including Salmonella spp., originating from animals is of particular interest. Fluoroquinolones and third‐generation cephalosporins are represented by ciprofloxacin and cefotaxime/ceftazidime, respectively, in the harmonised antimicrobial panel for the monitoring and reporting of AMR in Salmonella spp. from food animals and derived meat. Additionally, the CIAs, tigecycline and azithromycin, also included in the Salmonella monitoring from food‐producing animals and derived meat, are used as alternative treatments for MDR Salmonella spp. Colistin, categorised as an hpCIA, is not used in the treatment of salmonellosis, but it is used as a last‐resort antimicrobial for treating healthcare‐associated infections due to carbapenemase‐producing Gram‐negative bacteria such as Klebsiella pneumoniae and Acinetobacter baumannii.
Carcases of poultry
As the WHO categorises (fluoro)quinolones as hpCIAs in human medicine, their use in food‐producing animals is subject to prudent use initiatives. Considering Salmonella spp. recovered from broiler carcases in 2020, resistance to the (fluoro)quinolones (ciprofloxacin and nalidixic acid) were reported at very high to extremely high levels by many of the MSs included in the analysis (with overall resistance at 69.3% and 66.6%, respectively) (Annex A). Resistance levels to ciprofloxacin and nalidixic acid in isolates from turkey carcases ranged from low or not detected to extremely high among reporting MSs (overall, 46.9% and 32.5%, respectively) (Annex A).
In certain Salmonella serovars recovered from carcases of poultry, isolates resistant to ciprofloxacin but not to nalidixic acid were observed; possibly indicating the occurrence of plasmid‐mediated quinolone resistance (PMQR) mechanisms – see text box below. This was particularly the case for specific serovars recovered from broilers carcases in 2020, where 15 S. Agona isolates from the United Kingdom, six S. Hadar isolates from Hungary and two S. Derby from Poland displayed ciprofloxacin resistance, yet none showed resistance to nalidixic acid.
Quinolone/fluoroquinolone resistance in Salmonella
Quinolone/fluoroquinolone (i.e. nalidixic acid and ciprofloxacin) resistance in Salmonella usually arises due to point mutations within the DNA gyrase (gyrA and gyrB) and topoisomerase IV (parC and parE) genes, at locations comprising the quinolone resistance‐determining regions (QRDR) of the bacterial chromosome. Additionally, plasmid‐mediated quinolone resistance (PMQR) mechanisms have also been recognised, including the action of efflux pumps (qepA and oqxAB genes), enzymatic modifications (aac(6′)Ib‐cr gene – also conferring resistance to kanamycin) and protection of the DNA gyrase (qnrA, qnrB, qnrC, qnrD, qnrS and qnrVC genes) (Li et al., 2013; Luk‐In et al., 2017).
The presence of two‐point mutations in the QRDR will usually confer resistance to ciprofloxacin, with isolates typically exhibiting a ciprofloxacin minimum inhibitory concentration (MIC) > 1 mg/L, as well as conferring resistance to nalidixic acid. In contrast, isolates harbouring only one‐point mutation in the QRDR will still display resistance to ciprofloxacin and nalidixic acid, but the degree of resistance to ciprofloxacin is reduced (MIC > 0.064 mg/L). Salmonella isolates causing systemic infections in humans and displaying MICs of > 0.064 mg/L but < 1 mg/L have shown a poor response to treatment in some studies. This evidence provided the rationale for the new legislation (1729/2020/EU) to change the clinical breakpoint for ciprofloxacin from MIC > 1 mg/L to MIC > 0.06 mg/L to allow for the monitoring of low‐level resistance. The new legislation also modified the ECOFF for nalidixic acid from MIC > 16 mg/L to MIC > 8 mg/L.
In the absence of other fluoroquinolone resistance mechanisms, the presence of PMQR determinants (i.e. primarily qnr genes) in a bacterium usually confers resistance to ciprofloxacin (MIC > 0.06 mg/L), but the isolate remains susceptible to nalidixic acid (MIC > 8 mg/L). This contrasts with a mutation in the QRDR regions of the bacterial chromosome, which confer resistance to both ciprofloxacin and nalidixic acid.
In 2020, resistance to third‐generation cephalosporins (cefotaxime and ceftazidime) in Salmonella spp. from poultry carcases was only found in isolates from two reporting MSs; Italy and Iceland, with both reporting resistance in a single Salmonella isolate from broiler carcases (Annex A). No reporting countries detected third‐generation cephalosporin resistance among Salmonella isolates from the carcases of turkeys (Annex A). Section 2.3.6 provides further information on the phenotypic characterisation of third‐generation cephalosporin resistance among Salmonella isolates from broiler carcases.
Considering all reporting MSs, combined resistance to ciprofloxacin and cefotaxime among isolates from broiler carcases were observed at overall very low levels (0.1%) (Figure 5a; Annex A). Only Italy and Iceland reported combined resistance to ciprofloxacin and cefotaxime in single isolates of S. Infantis Notably, no isolates exhibited clinical resistance to these compounds when 2020 CBPs were applied. Overall resistance to azithromycin in Salmonella spp. isolates from broiler and turkey carcases were low (2% and 0.6%, respectively) (Annex A). When considering MSs, Italy was an exception, reporting high‐level azithromycin resistance in 10 isolates from broiler carcases (21.4%, N = 14) (Annex A).
Overall, tigecycline resistance was reported at low levels from carcases of broilers and turkeys (1.6% and 2.5%, respectively) (Annex A). Where countries reported resistance to tigecycline, generally very low or low levels were observed, except for Cyprus, which reported high‐level resistance to tigecycline in 2/8 isolates from broilers (25.0%), and Hungary, which reported moderate‐level resistance in 6/46 isolates from turkey carcasses (13.0%) (Annex A). Where tigecycline resistance was reported, MDR was often a feature, with all resistant isolates recovered from carcases of broilers and turkeys exhibiting multiresistance (n = 14 and n = 8, respectively) (Annex A).
Overall, colistin resistance was reported at very low or low levels among isolates from carcases of broilers and turkeys (1.6% each) (Annex A). Where countries reported resistance to colistin among isolates from carcases, generally very low or low levels were noted. Of those countries that reported colistin resistance in Salmonella isolates from broiler carcases, Cyprus, France, Germany and Portugal only reported a single resistant isolate, while Poland reported two resistant isolates and Spain reported eight resistant isolates (6.5%, N = 124) (Annex A). For turkey carcases, two countries reported colistin resistance in five isolates: France reported two resistant isolates, and Germany reported three (Annex A). The contribution of different serovars can influence these outputs because of the degree of intrinsic resistance to colistin in Group D Salmonella isolates. In total, five of the 14 colistin‐resistant isolates from broiler carcasses belonged to Group D Salmonella serovars.
Food‐producing animals
As previously indicated, for nalidixic acid, the ECOFF used to define microbiological resistance for 2020 data for poultry populations is MIC > 16 mg/L, while for 2021 data on pigs and calves, the new ECOFF (MIC > 8 mg/L) is used. When considering all MSs reporting 2020 AMR data on poultry flocks, high or very high levels of resistance to ciprofloxacin and nalidixic acid were observed in Salmonella isolates from broilers (57.5% and 54.1%, respectively) and turkeys (65.0% and 39.0%, respectively), compared with moderate levels observed in Salmonella isolates from laying hens (19.0% and 18.2%, respectively) (Figure 5b; Annex A). Salmonella isolates exhibiting ciprofloxacin resistance and nalidixic acid susceptibility were most frequently observed in Salmonella isolates from turkeys, possibly indicating the occurrence of PMQR mechanisms. This was particularly the case for 13 S. Hadar isolates from Hungary, 46 S. Anatum isolates from Italy and 43 S. Derby isolates from Spain, where all isolates displayed resistance to ciprofloxacin and susceptibility to nalidixic acid. Notably, S. Agona isolates exhibiting a similar fluoroquinolone phenotype were reported from the UK in low numbers in other poultry sources, including turkeys (n = 1), laying hens (n = 4) and broilers (n = 2) which may suggest clonal spread of this variant in poultry in the UK.
For ciprofloxacin, in 2021, overall resistance was reported at 10.1% for pigs and 12.7% for calves, while resistance to nalidixic acid was 9.8% and 10.1%, respectively (Figure 5b; Annex A). Of the Salmonella isolates from pigs with ciprofloxacin resistance and nalidixic acid susceptibility, (), two were S. Derby (one each from Belgium and Romania), and one each was S. Typhimurium (Spain), monophasic S. Typhimurium (Poland), S. Bovismorbificans (Romania), S. Uganda (Spain) and S. Rissen (Bulgaria). Just two Salmonella isolates from calves displayed ciprofloxacin resistance and nalidixic acid sensitivity (S. Agama and S. Typhimurium), both from Italy.
In 2021, zero resistance to the third‐generation cephalosporins, cefotaxime and ceftazidime in Salmonella isolates from pigs and calves was reported by most countries (Annex A). Overall resistance to cefotaxime and ceftazidime was very low (0.9%, each antimicrobial in pigs). Of the few countries that reported resistance to both third‐generation antimicrobials in Salmonella isolates from pigs included six isolates from Romania (5.8%, N = 104), four from Hungary (5.0%, N = 80) and one from Italy (1.1%, N = 91) (Annex A). For Salmonella isolates from calves, only Italy reported a single isolate (S. Ngor) as resistant to both substances (N = 20), while Spain reported a single isolate (S. Derby) as resistant to cefotaxime and susceptible to ceftazidime (N = 20) (Annex A).
For 2020 data on poultry flocks, the overall occurrence of resistance to both third‐generation cephalosporins in Salmonella isolates was very low or low, with most countries reporting zero resistance in all isolates tested (Annex A). Of those countries that reported isolates with resistance to cefotaxime and ceftazidime in broilers, resistant isolates were most numerous in Italy reporting 29 isolates (13.6%, N = 214) and Malta reporting seven isolates (13.5%, N = 52), while Hungary reported a single Salmonella isolate resistant to cefotaxime and three isolates resistant to ceftazidime (Annex A). For laying hens, just two countries, Italy (N = 172) and Hungary (N = 30) reported two isolates each, with resistance to cefotaxime and ceftazidime. Similarly, for turkeys, Italy (N = 170) reported two isolates and Poland (N = 22) reported a single isolate with resistance to both third‐generation cephalosporins (Annex A). Section 2.3.6 provides further information on the phenotypic characterisation of third‐generation cephalosporin resistance among Salmonella isolates from animal origins.
Overall combined resistance to ciprofloxacin and cefotaxime in Salmonella isolates from poultry flocks in 2020 and pigs and calves in 2021 was at very low or low levels (broilers: 2.0%, laying hens: 0.2%, turkeys: 0.5%, pigs 0.6%, calves 2.5%), although some exceptions were noted in some countries (Annex A). For instance, there was a moderate level of combined resistance in isolates from broilers: in 29 isolates from Italy (13.6%, N = 214) and 7 isolates from Malta (13.5%, N = 52). When considering pig data from 2021, two isolates from Hungary (2.5%, N = 80) and five isolates from Romania (4.8%, N = 104) had combined microbiological resistance to ciprofloxacin and cefotaxime. For calves, a single isolate each from Italy (N = 20) and Spain (N = 20) was detected with combined resistance to both substances (Annex A).
Overall resistance to Azithromycin in Salmonella from all food‐producing animal groups was very low to low, except for calves, where no resistance was detected (broilers: 2.1%, laying hens: 0.5%, turkeys: 1.5%, pigs: 1.9%) (Annex A). However, exceptions were noted in some countries, for instance, there was a high level of resistance in isolates from pigs: in four isolates each from Portugal (21.1%, N = 19) and Slovenia (22.2%, N = 18).
For amikacin, the new substance included in the harmonised test panel of antimicrobials from 2021, resistance was very low in pigs (0.6%), being reported for one single isolate in Austria (14.3%, N = 7), Germany (3.3%, N = 30), Romania (1%, N = 104) and Spain (0.6%, N = 170) and three isolates from the Netherlands (4.8%, N = 63). No resistance was reported in calves (Annex A).
Regarding tigecycline, the new ECOFF (MIC > 0.5 mg/L) laid down in the current legislation was used for the analysis of 2021 AMR data. Considering all reporting countries, overall resistance to tigecycline was reported at a low level for pigs (7.0%) and at a moderate level for calves (10.1%). Lowering the tigecycline ECOFF from MIC > 1 mg/L to MIC > 0.5 mg/L may have been in part responsible for a higher‐than‐expected level of resistance in Salmonella isolates from pigs and calves, as many of these isolates were reported with MICs within one dilution range of the new ECOFF. For example, 74/88 tigecycline resistant isolates from pig were reported to have an MIC of 1 mg/L. Under the previous legislation, these isolates would have been categorised as susceptible to tigecycline. Also, instability of tigecycline in the Mueller‐Hinton broth medium used in MIC‐testing can result in inconsistencies in MIC values (Bradford et al., 2005).
Poultry populations data from 2020 was analysed using the ECOFF (MIC > 1 mg/L) according to the previous legislation. For this data, overall resistance was observed at low levels among isolates from broilers (1.0%) and turkeys (5.5%), and at very low levels in isolates from laying hens (0.2%). When only considering countries reporting data for more than ten isolates, a high‐level of resistance was observed in 36 isolates from turkeys from Hungary (21.1%, N = 170) and moderate resistance in isolates from pigs in 18 isolates from Ireland (14.6%, N = 123), in eight isolates from Poland (16.7%, n = 48) and 14 isolates from Romania (13.5%, n = 104) and high‐resistance in four isolates from Portugal (21.1%, n = 19) and three isolates from Estonia (27.3%, N = 11) (Annex A). Note, some countries reporting moderate or high levels of tigecycline resistance reported data on a very low number of isolates which needs to be considered when interpreting individual results.
In 2020, overall colistin resistance in Salmonella isolates was reported at low levels among isolates from broilers, laying hens and turkeys (2.5%, 7.2% and 0.9%, respectively) (Annex A). While in 2021, overall resistance to colistin in Salmonella isolates from pigs was low (1.0%) but moderate for calves (11.4%) (Annex A). The small overall sample size of Salmonella isolates from calves (N = 79) compared to the other animal groups (i.e. pigs, N = 1,258) should be taken into consideration when interpreting these results. Across all animal groups, most individual countries reported no resistance or very low levels of resistance to colistin. Of those countries reporting > 10 isolates, several reported moderate to high levels of resistance to colistin. These countries include Cyprus (12.5%, N = 16) and Germany (23.5%, N = 17) for broiler flocks, Austria (19.2%, N = 26), Belgium (22.5%, N = 40), Cyprus (34.8%, N = 23) and Germany (26.9%, N = 78) for laying hen flocks (Annex A).
Figure 5a,b summarises the overall resistance to commonly used antimicrobials in veterinary medicine (ampicillin, sulfamethoxazole and tetracycline), as well as hpCIAs (represented by ciprofloxacin, cefotaxime and combined resistance to these two antimicrobials) among Salmonella isolates recovered from (a) carcases of broilers and turkeys, and (b) broilers, laying hens, fattening turkeys, pigs and calves.
2.4.4. Tigecycline and colistin resistance in Salmonella serovars
Tigecycline resistance in Salmonella serovars
Mechanisms of tigecycline resistance
Tigecycline, categorised as a CIA by the WHO (WHO, 2019), it is considered a last resort for the treatment of serious infections in adults caused by MDR bacteria. Tigecycline is structurally related to the tetracycline class of antibiotics and is active against Gram‐positive and Gram‐negative bacteria, as well as tetracycline‐resistant bacteria and some anaerobes (Yaghoubi et al., 2022).
Resistance mechanisms to tigecycline include non‐mobile tet(X) and mobile‐plasmid‐mediated transmissible tet(X) and resistance‐nodulation‐division (RND) efflux pump mediated tmexCD‐toprJ genes (Anyanwu et al., 2022) Of most concern is the transferable plasmid‐mediated spread of tigecycline resistance genes such as tet(X3) and tet(X4), which confer high levels of resistance to all tetracyclines, including tigecycline (MICs of ≥ 32 mg/L). Two recent studies looking at the global distribution, evolution pattern and spread of tet(X) genes, identified isolates carrying tet(X) genes from over 20 countries across five continents (Pan et al., 2020; Wang et al., 2021).
The first report of transferable high‐level tigecycline (HLT) resistance by tet(X3) and tet(X4) genes in Enterobacteriaceae from food animals, meat and the environment came from China in 2019 (He et al., 2019). Another study from China in the same year identified tet(X4) positive MDR E. coli isolates from retail pork samples (Bai et al., 2019). The tet(X4) gene in these isolates was located on various conjugative plasmids of diverse replicon types, indicating that the gene may be captured by a range of mobile genetic elements circulating among bacterial strains. Since then, additional plasmid‐mediated tet(X) genes, including tet(X5) and tet(X6), have been identified in over 10 different Gram‐negative species, although rarely in Salmonella spp. (Wang et al., 2021).
While tigecycline is not used in food‐producing animals, it is postulated that the excessive use of tetracycline antibiotics in food‐producing animals may contribute to the emergence of plasmid‐mediated tet(X) genes, with the potential for spread to human bacterial species (Pan et al., 2020; Anyanwu et al., 2022). The potential for other bacteria within the Enterobacteriaceae family (such as Salmonella) to acquire such transferable tigecycline resistance genes is highlighted, and the importance of monitoring tigecycline resistance through the determination of MICs or by molecular investigation such as WGS is further underlined.
The number of tigecycline‐resistant Salmonella isolates detected from (a) poultry flocks and derived carcases, and (b) pigs and calves and the predominant serovars accounting for this resistance, by MSs are shown in Figure 6. Particular serovars displayed microbiological resistance to tigecycline, suggesting clonal expansion of microbiologically‐resistant strains of these serovars.
Figure 6.
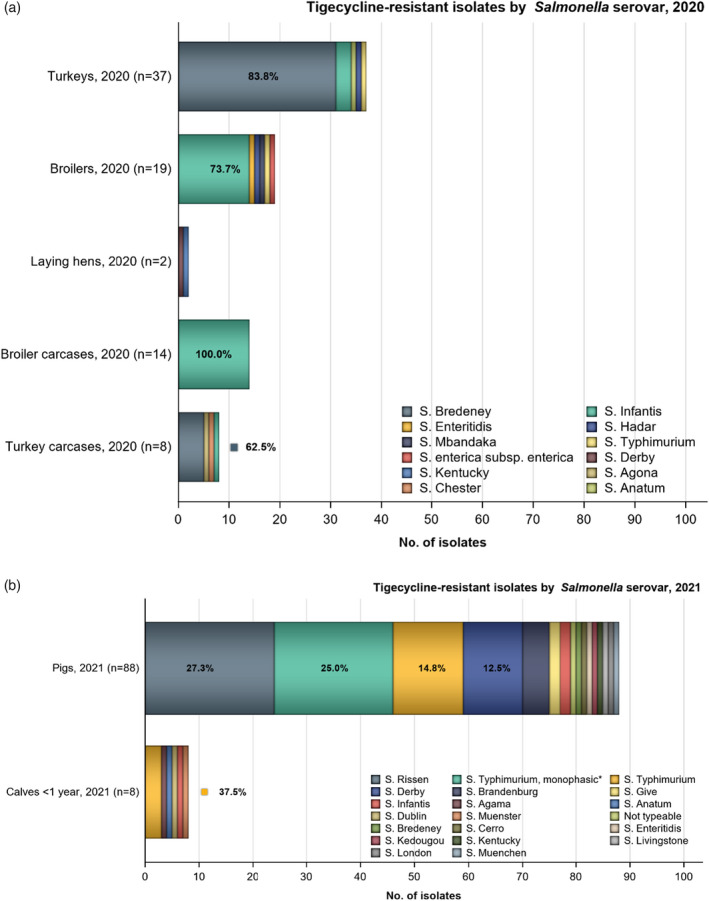
- n: Total number of tigecycline‐resistant isolates reported by MSs; predominant serovars are also expressed as a percentage; *Monophasic S. Typhimurium includes antigenic formulas; salmonellas in the legend are listed according to their predominance within all the animal/carcase origins. The ECOFF used to determine resistance to tigecycline in boilers, turkeys, laying hens was MIC > 1 mg/L. The ECOFF used to determine tigecycline resistance in pig and calf data was MIC > 0.5 mg/L.
In 2020, Serovar Infantis accounted for the majority (60.9%, n = 14) of the tigecycline resistant isolates recovered from broilers and for all tigecycline resistant isolates of their derived carcases (100%, n = 14), while S. Bredeney accounted for most (75.6%, n = 31) of the tigecycline‐resistant isolates recovered from turkeys and turkey carcasses (62.5%, n = 5). In 2021, S. Rissen (27.3%, n = 24), monophasic S. Typhimurium (25.0%, n = 22), S. Typhimurium (14.8%, n = 13) and S. Derby (12.5%, n = 11) accounted for most of the resistant isolates recovered from pigs. For calves, of the eight Salmonella isolates resistant to tigecycline, three were serotyped as S. Typhimurium and the remaining were S. Infantis, S. Dublin, S. Anatum, S. Agama and S. Muenchen, one each.
MDR was often a feature where tigecycline resistance was reported among certain serovars within the carcase/animal origins. For instance, among broilers and their derived carcases, all tigecycline‐resistant S. Infantis isolates were multi‐resistant, with resistance to ciprofloxacin, nalidixic acid, sulfamethoxazole and tetracycline, a common feature of all these isolates. This is a resistance pattern typical of MDR broiler clones of S. Infantis (Nógrády et al., 2012). Among turkeys, all tigecycline‐resistant S. Bredeney isolates (n = 31) were multi‐resistant, with ampicillin, nalidixic acid, ciprofloxacin and tetracycline resistance being a feature of these isolates. For pigs, MDR was present in 16 of the 24 tigecycline‐resistant S. Rissen isolates, with most having ampicillin, nalidixic acid, sulfamethoxazole and tetracycline resistance. For calves, all tigecycline‐resistant S. Typhimurium isolates (N = 3) were MDR, showing resistance to sulfamethoxazole and tetracycline.
Considering individual countries reporting tigecycline resistance, certain features relating to resistance were also evident. For example, 87.8% of tigecycline‐resistant isolates recovered from turkeys were reported by Hungary. The reporting countries responsible for most of the tigecycline‐resistant isolates in pigs (n = 88) were Ireland (n = 18), Spain (n = 17) Romania (n = 14), Poland (n = 8) and France (n = 6). While in calves, Italy reported four of the eight tigecycline‐resistant isolates (Annex A).
Colistin resistance in Salmonella spp.
Mechanisms of colistin resistance
Colistin, an antimicrobial belonging to the polymyxin class, is considered a highest‐priority CIA (hpCIA) and a last resort for treating serious human infection with some Gram‐negative bacteria (WHO, 2019). Although not frequently used in human medicine due to its nephrotoxic effects, colistin has been widely used in veterinary medicine for prophylactic/metaphylactic treatment (Kieffer et al., 2017). Various mechanisms of polymyxin resistance in Gram‐negative bacteria have been described (lipopolysaccharide modifications, efflux pumps, capsule formation and over‐expression of membrane protein, Olaitan et al., 2014); and transferable mobile colistin resistance (mcr) genes have also been detected in Salmonella isolates (Campos et al., 2016; Carnevali et al., 2016; Skov and Monnet, 2016).
Group D Salmonella serovars
Among Salmonella isolates recovered from poultry in 2020, resistance to colistin (i.e. MIC > 2 mg/L) was generally observed in S. Enteritidis isolates; this serovar accounting for 35.7%, 53.1% and 55.4% of the colistin‐resistant isolates recovered from broiler carcases, broilers and laying hens, respectively (Figure 7). Two colistin‐resistant S. Enteritidis isolates were also reported from turkeys (33.3%). In 2021, of the 12 Salmonella isolates from pigs with resistance to colistin, 41.7 % were serotyped as S. Enteritidis (n = 5), three isolates were S. Panama (25%), two isolates were S. Derby (16.7%) and one isolate S. Dublin and other S. Rissen. All nine colistin‐resistant isolates from calves were serotyped as S. Dublin.
Figure 7.
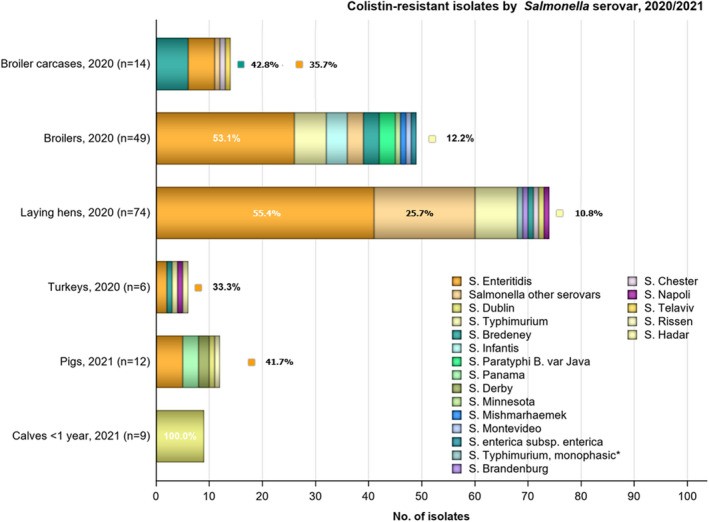
-
n: Total number of colistin‐resistant isolates reported by the MSs; predominant serovars are expressed as a percentage.*: Monophasic S. Typhimurium includes antigenic formulas; †: serovar unspecified; salmonellas in the legend are listed according to their predominance within all the animal/carcase origins.
Notably, S. Enteritidis, S. Dublin and S. Panama are group D salmonellas (serogroup O9). Salmonella belonging to group D tend to show decreased susceptibility to colistin without having any known acquired or mutational colistin resistance mechanisms (Agersø et al., 2012; Ricci et al., 2020). This is exemplified by the proportion of colistin‐resistant isolates belonging to S. Enteritidis and S. Dublin in 2020 and 2021, respectively. Figure 7 presents the number of colistin‐resistant isolates detected from the animal/carcase origins by MSs and the predominant serovars accounting for this resistance. Serovars Kapemba, Napoli and Panama, are group D salmonella serovars; the other serovars listed do not belong to group D (serogroup O9).
Other Salmonella serovars
S. Bredeney accounted for 42.8% of the colistin‐resistant isolates from broiler carcases (6/14), all reported by Spain. Two of the Salmonella isolates recovered from pigs in 2021 were serotyped as S. Derby and three as S. Panama. Colistin resistance was reported in a diverse range of serovars from poultry, including serovars Brandenburg, Bredeney, Chester, Hadar, Infantis, Minnesota, Mishmarhaemek, Montevideo, Napoli, Paratyphi B., Telaviv, Typhimurium and its monophasic variant. Across all poultry data, several MSs reported some colistin‐resistant Salmonella isolates as ‘Other serovars’.
A very small number of isolates reported markedly elevated colistin MICs (i.e. MIC > 16 mg/L), including one S. Enteritidis, isolate from broilers and one S. Montevideo isolate from a broiler carcase in 2020, and 2 isolates from pigs in 2021: one S. Rissen isolate and one S. Derby isolate.
2.4.5. Complete susceptibility (CS) and multidrug resistance (MDR)
For 2021 data from Salmonella spp. isolates, the new antimicrobial substance included in the harmonised panel for the monitoring of AMR according to the Commission Implementing Decision (EU) 2020/1729 was included in the assessment of CS and MDR (see Appendix F).
CS is defined as complete susceptibility to the antimicrobial substances included in the harmonised panel for the monitoring of AMR selected for the CS and MDR analysis. MDR is defined as resistance to three or more antimicrobial classes among Salmonella isolates from the monitored food‐producing animals and derived meat thereof (see Appendix F). Data from countries submitting less than ten Salmonella isolates from carcases or of animal origin are excluded from some of the analyses described in this section.
In 2021 data from pigs and calves, substances included in CS and MDR analysis include amikacin/gentamicin (assessed together as aminoglycoside antimicrobial class), ampicillin, cefotaxime/ceftazidime (assessed together as third‐generation cephalosporin), chloramphenicol, ciprofloxacin/nalidixic acid (assessed together as quinolone antimicrobial class), meropenem, sulfamethoxazole, tetracycline/tigecycline (assessed together as tetracycline antimicrobial class) and trimethoprim.
For 2020 data from poultry and derived meat, among the substances included in the harmonised test panel laid out in Commission Implementing Decision (EU) 2013/652, the ones included in the assessment of CS and MDR were gentamicin (aminoglycoside antimicrobial class), ampicillin, azithromycin (macrolide antimicrobial class), cefotaxime/ceftazidime (assessed together as third‐generation cephalosporin), chloramphenicol, ciprofloxacin/nalidixic acid (assessed together as quinolone antimicrobial class), meropenem, sulfamethoxazole, tetracycline/tigecycline (assessed together as tetracycline antimicrobial class) and trimethoprim. Due to the presence of resistance to colistin considered as intrinsic in serogroup D of Salmonella spp., colistin was not included in the analysis of MDR and CS for Salmonella in 2020 and 2021.
Carcases of poultry
The levels of CS and MDR among Salmonella isolates from poultry carcases are shown in Figure 8. In 2020, overall MDR for all reporting countries was observed at high levels in Salmonella spp. recovered from carcases of broilers (51.2%) and moderate levels for turkey carcasses (19.1%) (Annex A). Across all countries submitting data on ten or more Salmonella isolates recovered from broiler carcases, the median MDR was 44.6%, with the highest levels of MDR reported from Austria (73.8%, N = 61), Belgium (78.6%, N = 28), Romania (81.8%, N = 22) and Spain (83.1%, N = 124) (Annex A). For turkey carcasses, the median MDR was 34.3%, with Hungary (43.5%, N = 46), Poland (42.1%, N = 19) and Spain (26.5%, N = 34), reporting high to very high levels of MDR (Annex A).
Figure 8.
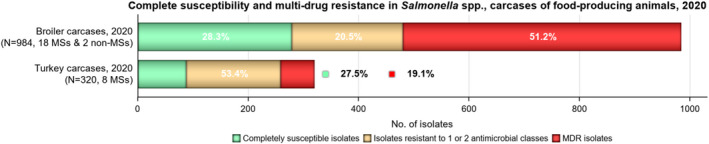
-
The MDR analysis of carcase isolates included the following antimicrobials: ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/nalidixic acid, gentamicin, meropenem, sulfamethoxazole, tetracycline, tigecycline and trimethoprim.MDR and complete susceptibility levels are also expressed as a percentage; N: total number of Salmonella spp. reported by MSs and non‐MSs. The ECOFFs used to determine microbiological resistance in 2020 data were from the Commission Implementing Decision (EU) 2013/652.
Overall CS, considering all reporting countries, was observed at moderate levels in carcasses of broilers and turkeys (28.3% and 27.5%, respectively) (Annex A). The overall median CS for broiler carcases was 22.0%, with results ranging from 0% (i.e. all isolates were resistant to at least one antimicrobial) to 90% (i.e. 90% of isolates tested were susceptible to all antimicrobial substances considered for the CS/MDR analysis). Belgium and Romania reported no isolates as CS, while countries with the highest proportion of isolates with CS include France (74.5%, N = 106) and Germany (56.5%, N = 23) (Annex A). For turkey carcasses, the overall median CS for countries reporting data for more than ten isolates was 12.6% and ranged from 5.3% (Poland) to 40.5% (France) (Annex A). The spatial distribution of CS across all reporting countries is visualised in Figure 9.
Figure 9.
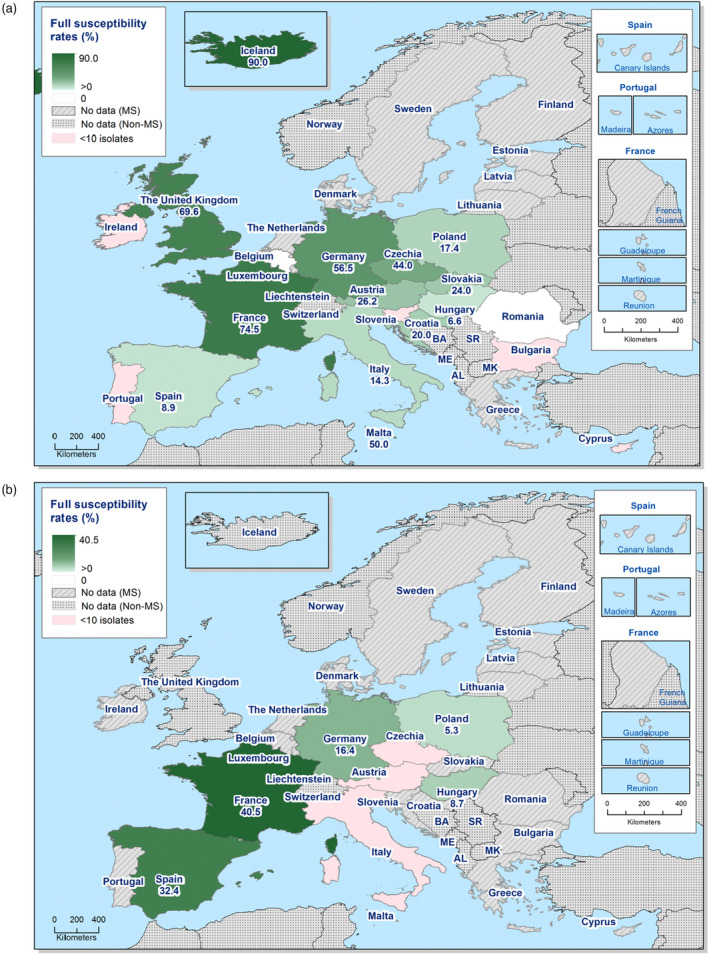
- The CS analysis of carcase isolates included the following antimicrobials: ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/nalidixic acid, gentamicin, meropenem, sulfamethoxazole, tetracycline/tigecycline and trimethoprim.
Differences in the prevalence of serovars and phage types of Salmonella in different countries and animal populations and their associated patterns of resistance likely explain some differences in the MDR and CS levels. The proportion of isolates which were completely susceptible and MDR among particular Salmonella serovars within the carcase origins are presented in Appendix C.
Food‐producing animals
The levels of CS and MDR among Salmonella isolates recovered from food‐producing animals are shown in Figure 10. In this figure, only MSs with ten or more isolates are included in the analysis. Annex A includes tables with overall and individual country MDR and CS. Overall MDR in all animal populations, considering all reporting counties, was observed at high levels in isolates from pigs (39.1%), calves (30.4%), broilers (41.8%) and turkeys (38.2%), and at a low level in isolates from laying hens (6.3%). Few countries reported zero MDR in any of the food‐producing animal groups. Across all MSs submitting data, in 2020, from broilers, the median MDR was 30.6%, with extremely high levels of MDR being reported by all isolates from Cyprus (100%, N = 16), 122 isolates from Austria (71.8%, N = 170) and 118 isolates from Slovenia (72.0%, N = 164). The median MDR for MSs with isolates from turkeys was 38.7%, with Hungary reporting the highest MDR, being detected in 118 isolates (69.4%, N = 170). When considering laying hens, the median MDR (1.1%) was much lower, with eleven countries reporting zero MDR. For 2021 data from pigs, the median MDR for MSs was 35.1%, with 15 isolates in Portugal (79.0%, N = 19), 23 isolates in Croatia (74.2%, N = 31) and 13 isolates in Slovenia (72.2%, N = 18) reporting extremely high MDR levels. For data from calves, the median MDR was 17.7% (Annex A).
Figure 10.
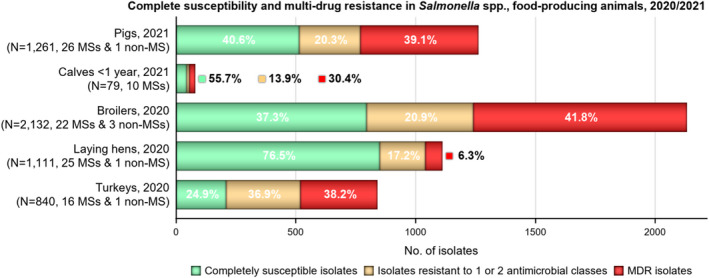
-
The MDR analysis of animal isolates included the following antimicrobials: amikacin/gentamicin (for pigs and calves) or gentamicin only (for poultry populations), ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/nalidixic acid, meropenem, sulfamethoxazole, tetracycline/tigecycline and trimethoprim.MDR and complete susceptibility are expressed as percentages; N: total number of Salmonella spp. reported by MSs and non‐MSs. Only MS with 10 or more isolates are included in the MDR analysis. The ECOFFs used to determine microbiological resistance in 2020 data were from the previous legislation (2013/652/EU) and the ECOFFs used for 2021 data are from the current legislation (2020/1729/EU).
Overall CS at the MS level was observed at high to very high levels for broilers (34.0%), turkeys (25.8%), pigs (40.5%) and calves (55.7%), and extremely high levels for laying hens (75.6%) (Annex A). However, the levels of CS varied widely between reporting countries, particularly in broiler, turkey and pig populations. This likely reflects the greater number of countries reporting data on these populations than from turkeys and calves. For 2020 MS data, the overall median percentage of isolates from broilers classified as CS was 35.1% with 131 isolates from France (78.4%, N = 167), and 13 isolates from Portugal (81.2%, N = 16) reporting the highest levels of CS, and Cyprus (0%, N = 16), Poland (15.4%, N = 208) and Hungary reporting the lowest percentage of CS in isolates (Annex A). For turkeys, the median CS was 24.6%, with eight isolates in Austria (80%, N = 10), and 69 isolates from France (73.4%, N = 94) reporting the highest levels of CS, and 14 isolates from Hungary the lowest level (8.2%, N = 170). For laying hens, the median CS was extremely high at 75.4%, with almost every country reporting over 60% CS. While for data from 2021, for pigs, the median CS was 42.7% with seven isolates from Greece (70.0%, N = 100), 39 isolates from Latvia (92.9%, N = 42) and 28 isolates from Luxembourg (75.7%, N = 37) reporting the highest levels of CS. For calves, the median CS was 50.0%, however only three countries submitted AMR data on more than ten isolates. The spatial distribution of CS across all reporting countries is visualised in Figure 11 (Annex A).
Figure 11.
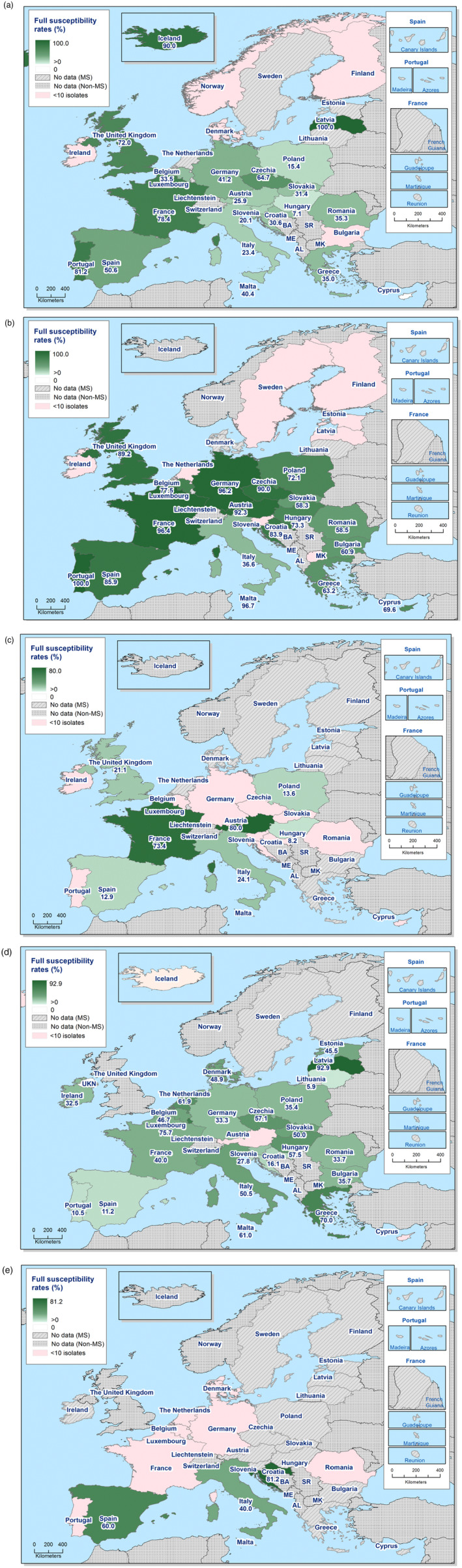
-
The ECOFF used to determine microbiological resistance in 2020 data were from the previous legislation (Commission Implementing Decision (EU) 2013/652) and the ECOFFs used for 2021 data are from the current legislation (Commission Implementing Decision (EU) 2020/1729).The CS analysis included the following antimicrobials: amikacin/gentamicin (for pigs and calves) or gentamicin only (for poultry populations), ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/nalidixic acid, meropenem, sulfamethoxazole, tetracycline/ tigecycline and trimethoprim.
It is of note, that the prevalence of particular serovars in different countries and animal populations, and their associated patterns of resistance, may account for the differences in the levels of MDR and CS among Salmonella spp. data. Notably, in laying hens, S. Enteritidis predominated (accounting for 25% of Salmonella isolates recovered from this poultry origin), with 79.5% of isolates exhibiting complete susceptibility reported from EU MSs and 92% from non‐EU MSs (including the Republic of North Macedonia and the United Kingdom), respectively. The proportions of isolates which were completely susceptible and MDR among particular Salmonella serovars within the animal origins are presented in Annex A.
2.4.6. High‐level resistance to ciprofloxacin (CIP) in Salmonella spp.
The distribution of ciprofloxacin‐resistant isolates displaying levels of microbiological resistance or clinical resistance, or high‐level resistance to ciprofloxacin within each of the animal/carcase categories is illustrated in Figure 12. Notably, the distribution of MICs provided is only for ciprofloxacin‐resistant isolates; the total number of Salmonella isolates monitored is provided in the legend. High‐level resistance to ciprofloxacin is considered in isolates with an MIC ≥ 4 mg/L. It is of note, that in 2021, according to the new implementing decision 2020/1729 the ciprofloxacin CBP was changed from > 1 mg/L to MIC > 0.06 mg/L, which aligns with the EUCAST ECOFF (MIC > 0.06 mg/L).
Figure 12.
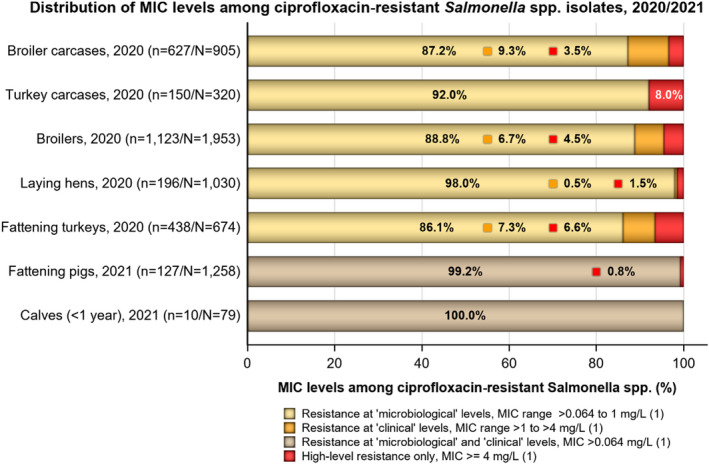
-
n: Total number of Salmonella spp. isolates exhibiting ciprofloxacin (CIP) resistance (MSs only); N: total number of Salmonella spp. reported by MSs.(1) In accordance with breakpoints stated in Decision 2013/652/EU (used for the analyses of poultry data) and Commission Implementing Decision (EU) 2020/1729 (used for the analysis of pigs and calves data).The proportion of isolates showing high‐level resistance is not included with those exhibiting ‘clinical’ or ‘microbiological’ resistance; similarly, the proportion of isolates showing ‘clinical’ resistance is not included with those displaying ‘microbiological’ resistance. Figure 12 excludes one isolate reported from laying hens (by the Republic of North Macedonia), which was ‘microbiologically’ resistant to ciprofloxacin.
Among Salmonella isolates displaying ciprofloxacin resistance, 3.5% of isolates from broiler carcases and 8% isolates from turkey carcases exhibited MICs of ≥ 4 mg/L. For poultry flocks, the highest proportions of Salmonella isolates displaying high‐level ciprofloxacin resistance originated from broilers (4.5%) and turkeys (6.6%) (Figure 12). A lower proportion of ciprofloxacin‐resistant isolates displayed MICs of ≥ 4 mg/L from laying hens (1.5%). Considering the total number of Salmonella isolates monitored from the different types of poultry by MSs in 2020, the highest proportions of isolates displaying ciprofloxacin MICs of ≥ 4 mg/L were noted in turkeys and turkey carcases; being detected in 3 Salmonella isolates (0.3%, N = 1,030), 22 isolates (2.4% N = 905), 51 isolates (2.6% N = 1,953), 12 isolates (3.8%, N = 320) and 29 isolates (4.3%, N = 674) reported from laying hens, broiler carcases, broilers, turkey carcases and turkeys, respectively (Figure 12).
In 2021, 127 Salmonella isolates from pigs, (10.1%, N = 1,258) recorded resistance to ciprofloxacin, with just a single isolate (S. Kentucky) from Malta displaying high‐level resistance to ciprofloxacin (and nalidixic acid). For calves, 10 Salmonella isolates (12.7%; N = 79) were resistant to ciprofloxacin, with none displaying high‐level resistance (Figure 12).
The serovars which displayed high‐level resistance to fluoroquinolones is of interest from both epidemiological and public/animal health perspectives. A detailed analysis on the high‐level resistance to ciprofloxacin in S. Kentucky and other Salmonella serovars is presented in Appendix A.
2.4.7. Phenotypic characterisation of third‐generation cephalosporin and carbapenem resistance in Salmonella spp.
According to Decision 2020/1729/EU and the previous legislation (2013/652/EU), any Salmonella isolate from food‐producing animals or derived meat showing resistance to cefotaxime or ceftazidime or meropenem (i.e. presumptive ESBL/AmpC/carbapenemase‐producing Salmonella) should be further tested with a second panel of harmonised antimicrobial substances to confirm the phenotypic resistance to third‐generation cephalosporins or carbapenems. Further phenotypic characterisation of those Salmonella isolates that exhibited resistance to third‐generation cephalosporins or carbapenems within each of the animal categories and for Salmonella isolates from humans is reported in Appendix B (Table B1). From 2021, whole genome sequencing (WGS) is authorised as an alternative method to conventional phenotypic testing for Salmonella isolates that show resistance to extended‐spectrum cephalosporins and carbapenems. MSs may choose to either undertake susceptibility testing of the antimicrobials included in panel 2 for the presumptive ESBL, AmpC or CP‐producing Salmonella or perform WGS and report this data. Information on WGS of these isolates can be found in chapter 5.
Salmonella spp. from food‐producing animals and derived carcases
Considering isolates from the animal sectors, a low percentage (1.0%, N = 6,219) of all Salmonella recovered from poultry flocks and derived meat in 2020 and from pigs and calves in 2021 by all MSs, demonstrated resistance to third‐generation cephalosporins and were subjected to further phenotypic characterisation. The proportions of Salmonella isolates exhibiting ESBL, AmpC or ESBL + AmpC phenotypes within the different animal species and production types are presented in Table 5. The overall percentage of presumptive ESBL, AmpC or ESBL + AmpC producers was from very low to low (range 0.1%–2.1%) in all animal/carcase matrices. The ESBL phenotype was more frequently detected than the AmpC phenotype among all animal categories. Considering the individual MSs reporting cephalosporin‐resistant isolates from poultry and derived meat, the proportion of presumptive ESBL, AmpC or ESBL + AmpC‐producers was observed at very low or low levels, although there were a few exceptions. Italy reported the highest number of isolates from broilers and laying hens, with 29 isolates from broilers and 2 isolates from laying hens exhibiting the ESBL phenotype. Of the ten isolates from pigs identified as either presumptive ESBL or ESBL + AmpC‐producers, most were from Romania (n = 6) followed by Hungary (n = 4). Notably, no Salmonella isolates recovered from turkey carcases exhibited resistance to third generation cephalosporins.
Table 5.
Summary of phenotypic characterisation of third‐generation cephalosporin resistance in non‐typhoidal Salmonella spp. from food‐producing animals, animal carcases and humans, reported in 2020/2021
| Matrix | Presumptive ESBL‐ and/or AmpC‐ producers (a) | Presumptive ESBL‐producers (b) | Presumptive AmpC‐producers (c) | Presumptive ESBL + AmpC‐producers (d) |
|---|---|---|---|---|
| n (%R) | n (%R) | n (%R) | n (%R) | |
| Humans – 2020 (N = 5,948, 15 MSs) | 45 (0.8) | 35 (0.6) | 10 (0.2) | 1 (0.02) |
| Humans – 2021 (N = 9,787, 14 MSs) | 88 (0.9) | 76 (0.8) | 12 (0.1) | 0 |
| Broiler carcasses – 2020 (N = 905, 18 MSs) | 3 (0.3) | 2 (0.2) | 1 (0.1) | 0 |
| Turkey carcasses – 2020 (N = 320, 8 MSs) | 0 | 0 | 0 | 0 |
| Broilers – 2020 (N = 1,953, 22MSs) | 41 (2.1) | 38 (1.9) | 3 (0.2) | 0 |
| Laying hens – 2020 (N = 1,030, 24 MSs) | 4 (0.4) | 2 (0.2) | 2 (0.2) | 0 |
| Fattening turkeys – 2020 (N = 674, 16 MSs) | 3 (0.4) | 3 (0.4) | 0 | 0 |
| Fattening pigs – 2021 (N = 1,258, 26 MSs) | 10 (0.8) | 10 (0.8) | 2 (0.2) | 2 (0.2) |
| Bovines < 1 year – 2021 (N = 79, 10 MSs) | 1(1.3) | 1(1.3) | 1(1.3) | 21 (1.3) |
N: Total number of isolates reported by the MSs; n: number of the isolates resistant; %R: percentage of resistant isolates; ESBL: extended‐spectrum β‐lactamase.
Isolates exhibiting only ESBL‐ and/or only AmpC‐ and/or combined ESBL + AmpC phenotype.
Isolates exhibiting an ESBL‐ and/or combined ESBL + AmpC‐phenotype.
Isolates exhibiting an AmpC and/or combined ESBL + AmpC‐phenotype.
Isolates exhibiting a combined ESBL + AmpC phenotype.
Salmonella serovars from food‐producing animals and carcases
When assessing the 2021 data by serovar, the ESBL or AmpC phenotype was detected in five serovars in pigs: S. Derby, S. Infantis, S. London, S. Kedougou and S. Rissen. Among Salmonella isolates from pigs, ten displayed an ESBL phenotype (two S. Derby, two S. Infantis, one S. London, one S. Kedougou and four S. Rissen from Hungary and Romania), and two displayed the ESBL + AmpC phenotype (one S. Derby from Hungary and one S. Rissen from Romania). In calves, a single Salmonella isolate displayed an ESBL + AmpC phenotype (S. Derby from Spain).
Considering the 2020 data on poultry, the ESBL or AmpC phenotype was associated with multiple isolates belonging to certain serovars, suggesting the possible clonal expansion of particular strains: namely, S. Infantis and S. Kentucky. Among both broilers and turkeys, presumptive ESBL‐producing Salmonella was identified more frequently than presumptive AmpC‐producing Salmonella and encompassed a greater number of serovars. The ESBL phenotype was identified in three different serovars from broilers (Infantis, Kentucky and Java) and three different serovars from turkeys (Agona, Derby and Infantis), while the AmpC phenotype was identified only different serovars from broilers in S. Infantis in broilers. Where presumptive ESBL, AmpC or ESBL + AmpC‐producers were identified from broilers (41/1,953 isolates), most were attributed to S. Infantis (29 isolates reported by Italy and three by Hungary) and S. Kentucky (seven isolates reported by Malta). All 29 S. Infantis isolates reported by Italy displayed an ESBL phenotype while all three S. Infantis isolates reported by Hungary, presented an AmpC phenotype. Conversely, only the ESBL phenotype was expressed in the seven S. Kentucky isolates reported by Malta and two S. Java isolates reported by Austria.
Three presumptive ESBL, AmpC or ESBL + AmpC‐producers were identified from turkeys (N = 674 isolates). These included a S. Infantis isolate and a S. Agona isolate from Italy, and a S. Derby isolate from Poland. All three isolates displayed an ESBL phenotype only. Among laying hens, two S. Infantis isolates reported by Italy were also identified as a presumptive ESBL only‐producer, and a S. Enteritidis and S. Bovismorbificans isolate reported by Hungary were identified as presumptive AmpC only‐producers. The ESBL phenotype was detected in S. Infantis isolates from Italy and Iceland (one isolate in each country) while the AmpC phenotype was also detected in a single S. Mbandaka isolate reported from a broiler carcase by France.
2.4.8. Carbapenem resistance in Salmonella spp. from food‐producing animals and carcases
Carbapenems are recognised as hpCIAs (WHO, 2019), and includes meropenem, an antimicrobial agent specified in the antimicrobial panel for monitoring and reporting AMR in Salmonella spp. (as stipulated by Commission Implementing Decision (EU) 2020/1729). This class of antimicrobials are not therapeutically used in food‐producing animals but are reserved for use in humans.
In 2020 and 2021, none of the Salmonella isolates recovered from any of the animal or carcase origins exhibited microbiological resistance to meropenem. This is consistent with data from animal or carcase origins in 2018 and 2019.
2.4.9. Resistance exhibited by dominant Salmonella serovars
The detailed reporting of results at the serovar level demonstrated the major contribution of a few serovars to the observed overall occurrence of resistance when considering aggregated data for Salmonella spp. The patterns of resistance associated with these different serovars have a marked influence on the overall resistance levels in Salmonella spp., as the proportion of completely susceptible and MDR isolates may vary significantly among serovars recovered from each of the carcase origins/food‐producing animal populations studied. The analysis of antimicrobial resistance at the serovar level is presented in Appendix C.
2.5. Comparison of resistance data in Salmonella from human and food‐producing animals
A comparison of human Salmonella data by serovar to that found in food‐producing animals for the years 2020–2021 can be found in Appendix D. Comparable AMR data are presented for serovars S. Typhimurium and its monophasic variant, S. Derby, S. Infantis, S. Enteritidis and S. Kentucky. The prevalence of particular Salmonella serovars within countries and animal populations, and their associated patterns of resistance, may explain some of the observed differences in the occurrence of AMR and MDR. The spread of resistant clones and the presence of resistance genes within these clones can be exacerbated by selective pressure from using antimicrobials in human and animal populations. However, it should be noted that relating the occurrence of AMR in human Salmonella isolates to that in isolates from food‐producing animals and derived meat should be done with caution because other sources of Salmonella occur, and such evaluations should be performed and interpreted considering the complex epidemiology of salmonellosis.
2.6. Discussion
The continuous AMR monitoring in Salmonella helps to identify new resistance mechanisms emerging in human and animal populations. The harmonised monitoring of Salmonella from food‐producing animals and carcases using phenotypic antimicrobial susceptibility testing, seeks to identify emerging issues such as MDR S. Kentucky with high resistance to fluoroquinolones and S. Infantis isolates exhibiting combined resistance to extended‐spectrum cephalosporins, fluoroquinolones and colistin (EFSA, 2019). In 2020 and 2021, the detection of resistant Salmonella isolates varied markedly between animal and carcase origins, by serovars and by reporting countries. These factors may introduce a source of variation to results when considering all reporting countries, and results should be interpreted cautiously. Further, the limited number of Salmonella isolates reported by some countries at serovar level, in recent years is not enough to perform a full statistical trend analysis of the level of resistance at the serovar level.
Under the new legislation (Commission Implementing Decision (EU) 2020/1729), MSs may perform WGS on Salmonella isolates from food‐producing animals displaying resistance to third‐generation cephalosporins or carbapenems as an alternative method to broth‐microdilution when further testing those isolates with the second panel of antimicrobial substances. Information on WGS data from Salmonella isolates can be found in chapter 5. Regarding data from humans, resistance predicted from WGS has been an accepted test method since 2019. WGS is increasingly recognised as a powerful tool for epidemiological surveillance of AMR in the ‘One Health’ context (WHO, 2020). WGS complements phenotypic methods by providing information on molecular determinants and mechanisms, genetic factors that facilitate transmission, and geographical distributions of resistance genes. Many studies on Enterobacteriaceae, including Salmonella, have described high concordance between WGS data and phenotypic data (McDermott et al., 2016; Hendriksen et al., 2019).
In 2021, information on AMR in Salmonella isolates from human clinical cases was reported by 24 MSs and two non‐MSs. No data was reported by the United Kingdom after 2019 due to its withdrawal from the EU on 30 January 2020. The effect of the COVID‐19 pandemic on the quantities of isolates reported by countries was not as pronounced in 2021 as for 2020 but the number of isolates were still one quarter (median) fewer compared with 2019, although more countries were able to report data for 2021 compared with 2020. In 2021, twenty‐one countries provided data as measured values (quantitative data), four as data interpreted with clinical breakpoints and one as predicted phenotypic resistance based on whole genome sequencing.
Of note, the comparison of AMR data reported for Salmonella isolates from pigs and calves in 2019 and 2021 should be made with caution because the legislation in place has changed and the requirements were different under the previous legislation (Commission Implementing Decision (EU) 2013/652) compared to the new one (Commission Implementing Decision (EU) /2020/1729). In 2019, it was mandatory to collect samples of carcasses of fattening pigs and bovine animals under 1 year of age, while in 2021 the sampling is taken from the caecal contents of pigs and calves. In 2019, far fewer MSs submitted data on pigs (N = 8) and calves (N = 3) compared to 2021 (N = 26, N = 10, respectively).
Occurrence of resistance to commonly used antimicrobials in veterinary medicine
Moderate to very high levels of resistance to ampicillin, sulfamethoxazole and tetracycline were generally reported by MSs among Salmonella isolates from all animal and carcase origins except laying hens. The highest resistance levels were observed in pigs (2021) and turkeys (2020). Resistance levels to sulfamethoxazole and tetracycline were generally higher than ampicillin in isolates from animal or carcase origins. This may be related to underlying genetic structures responsible for resistance and the proportion of Salmonella spp. carrying genetically‐linked resistance genes to these agents. Overall, high levels of resistance to antimicrobials used in veterinary medicine were also noted in Salmonella isolates from human cases. Considering individual serovars, monophasic S. Typhimurium generally showed the highest resistance to these antimicrobials for all the animal/carcase origins. The same observation was also noted among isolates from human cases, where extremely high levels of resistance to these antimicrobials were reported in monophasic S. Typhimurium and S. Kentucky in 2020 and 2021 (for S. Kentucky, very high in 2021).
Occurrence of resistance to highest‐priority critically important antimicrobials (hpCIAs) and last resort antimicrobials
Third‐generation cephalosporins and fluoroquinolones are categorised as hpCIAs because they are commonly used in treatment of gastrointestinal infections, including Salmonella infections, in humans (WHO, 2019). This sets the rationale for monitoring combined resistance to these antimicrobial classes within food‐producing animals.
From the monitoring of pigs and calves in 2021, the overall resistance levels to CIAs ranged from zero (no resistance to azithromycin and amikacin was observed in Salmonella isolates from calves) to moderate in pigs. Moderate levels of resistance to ciprofloxacin/nalidixic acid were observed in isolates from pigs and calves. From the monitoring of pigs in 2021, S. Rissen, S. Typhimurium and monophasic S. Typhimurium, showed the highest levels of resistance to ciprofloxacin and nalidixic acid. From the monitoring of poultry in 2020, highest levels of resistance were generally noted to ciprofloxacin/nalidixic acid and S. Infantis and S. Kentucky showed the highest resistance to ciprofloxacin and nalidixic acid across poultry origins. This likely reflects the spread of resistant clones belonging to these serovars. From human data reported in 2021, S. Infantis and S. Kentucky also showed the highest resistance to these substances. Resistance to ciprofloxacin/nalidixic acid, sulfamethoxazole and tetracycline are typical of a clone of S. Infantis which is prevalent in Europe in broilers (Nógrády et al., 2012) and S. Infantis is a serovar commonly reported in the monitoring by some countries. Ciprofloxacin resistance was observed at equally high levels among isolates from broilers, turkeys and their derived carcases and was generally very similar to nalidixic acid resistance. However, Salmonella isolates exhibiting ciprofloxacin resistance and nalidixic acid susceptibility, indicating the occurrence of plasmid‐mediated quinolone resistance (PMQR) mechanisms, were mostly evident in turkeys and their derived carcases.
Resistance to third‐generation cephalosporins, cefotaxime and ceftazidime in Salmonella isolates recovered from animal populations and derived meat was either not discerned or was generally detected at very low/low levels in most of the reporting MSs. Isolates that demonstrated resistance to third‐generation cephalosporins were subjected to supplementary testing with a further panel of antimicrobials to determine if they were presumptive ESBL, AmpC or ESBL + AmpC producers. Very small numbers of isolates were determined to be presumptive ESBL, AmpC or ESBL + AmpC producers, notably, no Salmonella isolates recovered from turkey carcases in 2020 exhibited resistance to third‐generation cephalosporins. In Salmonella spp. isolated from human cases the levels of resistance to cefotaxime and ceftazidime were also low, at 1.1%, ranging from 0.0% to 5.1%. In 2021, no Salmonella spp. recovered from human cases, or any carcase/animal origins were microbiologically resistant to meropenem.
Overall combined resistance to cefotaxime and ciprofloxacin in all animal/carcase origins was observed at very low or low levels, and in turkey carcases, no isolates displayed combined resistance. Notably, for poultry populations, 2020 data, where cefotaxime and ciprofloxacin MICs were interpreted using CBPs, none of the isolates exhibited ‘clinical’ resistance to these compounds, except for broilers at a very low level (0.4%). Note however that the CBP for ciprofloxacin changed in the new legislation and from 2021 corresponds to the ECOFF MIC > 0.06 mg/L. From human cases in 2021, combined resistance to cefotaxime and ciprofloxacin was very low overall (0.8%) but higher in S. Infantis (5.0%) and S. Kentucky (5.7%), with particularly high proportions among S. Infantis isolates from Italy (a similar observation for Italy was made in 2020). Italy also reported the highest proportion of combined resistance in S. Infantis in broiler flocks (20.7%), laying hens (12.5%) and fattening turkeys (3.7%) in 2020. For S. Kentucky from humans the results were based on altogether 105 isolates with very few isolates reported from the majority of countries, the highest number of isolates being from France, Germany and Malta (35, 23 and 18 isolates, respectively).
In 2021, S. Dublin accounted for all of the colistin‐resistant isolates observed in calves, while in pigs, S. Enteritidis was most often associated with colistin resistance. From the monitoring of poultry in 2020, colistin resistance was generally observed in S. Enteritidis isolates, with resistance observed in over half of the S. Enteritidis isolates recovered from broilers and laying hens. S. Enteritidis and S. Dublin are group D salmonellas (serogroup O9). This group shows decreased susceptibility to colistin without having any known acquired or mutational colistin resistance mechanisms and, therefore, shows a degree of intrinsic resistance to colistin (Agersø et al., 2012; Ricci et al., 2020). Various serovars from pigs displayed colistin‐resistance, including five isolates attributed to S. Enteritidis, three to S. Panama and two to S. Derby. In Salmonella spp. in isolates from human cases, levels of resistance to colistin ranged from 0.0% to 19.2% in 2021 with the highest proportion among the investigated serovars observed in S. Enteritidis (17.6%). Phenotypical testing for colistin is complicated, and EUCAST recommends performing testing using microbroth dilution or specific PCR. For that reason, colistin results are only available from a third of the reporting MSs. Because of the possible difference in intrinsic resistance to colistin in Salmonella by serogroup, EUCAST removed the Salmonella‐specific ECOFF until more data has been made available. A tentative ECOFF has however been suggested for S. Dublin where a MIC of ≤ 16 mg/L would be considered wild type (EUCAST, 2023). If that would be applied also on S. Enteritidis, which belongs to the same antigen O group as S. Enteritidis – O:9, fewer isolates would turn out non‐wild type to colistin, making it easier to identify isolates with acquired resistance. Further molecular characterisation of colistin‐resistant isolates obtained from the EU AMR monitoring to determine the underlying genetic mechanisms would assist in identifying the emergence and dissemination of colistin‐resistant Salmonella clones as well as identify colistin resistance plasmids occurring in Salmonella associated with livestock.
The ECOFF for tigecycline was changed under the new legislation from > 1 to > 0.5 mg/L, and resistance was reported separately for 2021 data from pig and bovine animals under 1 year of age and 2021 AMR data from poultry and meat derived thereof. The CBP for tigecycline was also changed to > 0.5 mg/L. Where tigecycline resistance was reported among the carcase/animal origins, most isolates displayed MICs that were one dilution above the ECOFF. Considering poultry, S. Infantis accounted for most of the resistant isolates recovered from broilers (70.3%) and all isolates from their derived carcases, as well as three tigecycline‐resistant isolates reported from turkeys. S. Bredeney accounted for most (83.8%) of the tigecycline‐resistant isolates recovered from turkeys. A low number of tigecycline‐resistant isolates were reported from calves (n = 8) with various serovars, while S. Rissen was the most common serovar reported (27.3%, n = 88) from pigs. Microbiological resistance to tigecycline may suggest clonal expansion of microbiologically‐resistant strains belonging to these serovars. MDR was often a feature of tigecycline‐resistant isolates from pigs and calves. In Salmonella spp. in isolates from humans, resistance to tigecycline was rare to low (overall 1.4%) among the nine countries reporting results for this last‐resort antimicrobial.
Determining the susceptibility to tigecycline is not straightforward as this compound can be inactivated by oxidation and exposure to light, which may lead to falsely‐elevated MIC values. In addition, upregulation of normal cell pathways or processes may also contribute to elevated tigecycline MIC values at levels above the ECOFF in Enterobacteriaceae (He et al., 2016). Two transferable plasmid‐mediated tigecycline resistance genes, tet(X3) and tet(X4) conferring higher levels of tigecycline resistance (MICs of ≥ 16 mg/L), have been reported in numerous Enterobacteriaceae from animals and meat (chicken and pork) in China (Bai et al., 2019; He et al., 2019). The potential for Salmonella to acquire such transferable tigecycline resistance genes is therefore highlighted, and the importance of monitoring tigecycline resistance through determination of MICs or by molecular investigation such as WGS is further underlined.
For the first time in 2021, amikacin, a member of the aminoglycoside class which is a high priority CIA for human medicine, was included in the harmonised panel for testing food‐producing animals and derived meat. The rationale for including amikacin, in addition to gentamicin, for harmonised monitoring is that amikacin improves the detection of 16S rRNA methyltransferase enzymes (RMTases) which confer resistance to aminoglycosides (EFSA, 2019). RMTases have been increasingly associated with carbapenemases, AmpC or ESBL enzymes and fluoroquinolone resistance in Enterobacteriaceae from human cases in Europe (Arca‐Suárez et al., 2022; Fournier et al., 2022). A small number of studies from outside of Europe have observed that the prevalence of RMTases in Enterobacteriaceae isolated from food‐producing animals is low (Yan et al., 2004; Wang et al., 2017; Belaynehe et al., 2019), and that the presence of these genes confers high‐level ampicillin resistance (MIC > 512 mg/L) in isolates (Belaynehe et al., 2019). For pigs, few Salmonella isolates were microbiologically resistant to amikacin (MIC > 4 mg/L) (n = 7), with one of those isolates also clinically resistant (MIC > 16 mg/L), while no isolates from calves were resistant to this antimicrobial. One S. monophasic Typhimurium isolate from Austria, from pigs, with amikacin resistance was MDR, also displaying resistance to ampicillin, nalidixic acid, ciprofloxacin, sulfamethoxazole, trimethoprim and tetracycline.
Multidrug resistance (MDR)
In 2020, MDR varied between reporting countries and animal/carcase origins, with overall MDR ranging from a low level of 6.1% in laying hens to the highest level of 53.6% in broiler carcases. In 2021, MDR was higher among Salmonella spp. from pigs (39.2%) compared to calves (30.4%). Resistance levels varied among serovars which may exhibit particular MDR patterns, so the relative contribution of individual serovars within the different animal origins and between countries should be considered when comparing the situation between reporting countries. For example, the overall lower level of MDR among isolates from laying hens in comparison to those reported from broilers and turkeys most likely reflects in part the predominance of S. Enteritidis, which accounted for 25.5% of Salmonella isolates from laying hens reported by MSs, and where 79.5% of S. Enteritidis isolates exhibited complete susceptibility. Additionally, only a limited number of antimicrobials are authorised for the treatment of laying hens in many EU countries, and this factor may also be reflected in overall AMR levels in Salmonella isolates from this sector. In Salmonella spp. strains from human cases, MDR was detected in 22.6%, ranging from 5.6% reported from Greece to 40.5% in Italy, respectively. The lowest rates of MDR were found in S. Enteritidis (1.9%) and the highest in S. Kentucky (54.8%) and in monophasic S. Typhimurium (78.4%), respectively.
Prevalence of particular Salmonella serovars and associated MDR patterns
In summary, the prevalence of particular Salmonella serovars within countries and animal populations and their associated patterns of resistance likely explain many of the observed differences in the overall levels of AMR and MDR. The spread of resistant clones and the occurrence of resistance genes within these clones can be exacerbated by selective pressure from using antimicrobials in human and animal populations. A detailed analysis of AMR at the serovar level, including possible underlying genetic structures responsible for resistance, is presented in Appendix C. Within a given MS, any attempt to relate the occurrence of AMR in human Salmonella isolates to that in isolates from food/food‐producing animals is complicated (see Appendix D), as much of the food consumed in a MS may have originated from other MSs or non‐member countries. Salmonella infections can also be associated with foreign travel, other types of animal contact (such as pets, including reptiles) or the environment. Additionally, human infections may result from human‐to‐human transmission. To improve the investigation of these relationships, human isolates from cases notified as having been acquired during travel outside of the reporting country were excluded from the analysis.
High‐level resistance to ciprofloxacin
In 2021, high‐level resistance to ciprofloxacin (MIC ≥ 4 mg/L) was detected in one isolate (S. Kentucky) from a pig sample from Malta, while in calves, there was none. In 2020, high‐level resistance to ciprofloxacin was also observed among isolates from poultry (see Appendix A). While many serovars (including Bredeney, Derby and Infantis) exhibited high‐level resistance among poultry, S. Kentucky accounted for most of the high‐level resistant Salmonella isolates recovered from the poultry origins. The same finding was also noted among isolates from human cases in 2021, where high‐level ciprofloxacin resistance was most commonly found in S. Kentucky (in 81.2% of S. Kentucky isolates) among the 13 countries reporting MIC data. S. Kentucky isolates exhibiting high‐level ciprofloxacin resistance are likely to belong to the multilocus sequence type (ST) 198 clone, which has shown epidemic spread in North Africa and the Middle East (Belaynehe et al., 2019). Notably, in 2020, the occurrence of this serovar exhibiting high‐level resistance in poultry was observed by eight MSs from most parts of Europe, suggesting further clonal expansion (S. Kentucky ST198‐X1). Furthermore, a very high proportion of the poultry S. Kentucky isolates displaying ciprofloxacin MICs of ≥ 4 mg/L were also multiresistant, primarily showing resistance to ampicillin, gentamicin, nalidixic acid, sulfamethoxazole and tetracycline. The same observation was also noted among S. Kentucky isolates from human cases. The sole S. Kentucky isolate showing high resistance to ciprofloxacin from pigs was resistant to nalidixic acid but no other antimicrobial substances.
Phenotypic characterisation of third‐generation cephalosporin and carbapenemase resistance
For data from animal/carcase origins, very small numbers of isolates were determined to be presumptive ESBL, AmpC or ESBL + AmpC producers. The highest number observed was in broiler flocks from 2020 (2.1%, N = 1,953). Notably, no Salmonella isolates recovered from turkey carcases in 2020 exhibited resistance to third‐generation cephalosporins. In 2021, for further testing third‐generation cephalosporin‐resistant isolates from pigs and calves, MSs could choose to undertake WGS as an alternative to broth‐microdilution, with some countries such as Italy submitting WGS data. More detailed information on the WGS results can be found in chapter 5. Note, in 2021, there were no human cases or animal Salmonella isolates reported with meropenem resistance, similarly for 2020 poultry data, indicating the absence of carbapenemase‐producers in the Salmonella isolates reported by MSs for these years.
Among poultry in 2020, the ESBL or AmpC phenotype was associated with multiple isolates belonging to certain serovars, suggesting the possible clonal expansion of particular strains: namely, S. Infantis and S. Kentucky. Among broilers and turkeys, presumptive ESBL‐producing Salmonella was identified more frequently than presumptive AmpC‐producing Salmonella and encompassed a greater number of serovars. Except for one MS, presumptive ESBL, AmpC or ESBL+AmpC producers were identified at very low or low levels. Italy, however, reported the ESBL phenotype in 29 Salmonella isolates (76.3% n = 38) from broilers and two (66.6%, n = 3) Salmonella isolates from turkeys; of which S. Infantis accounted for all those from broilers (n = 29) and half of those from turkeys (1/2). Additionally, some of these isolates also possessed an AmpC phenotype. The proportion of presumptive ESBL/AmpC‐producers attributed to S. Infantis within broilers and turkeys in Italy suggests clonal expansion and spread among these animal populations in this country. The findings in poultry are interesting because there are no authorised products for use in the poultry sector in the EU, which include third‐generation cephalosporins, and off‐label use of third‐generation cephalosporins in poultry is not permitted (Franco et al., 2015).
Considering the monitoring performed in 2021, the ESBL or ESBL + AmpC phenotype was detected in ten isolates representing five serovars among pig isolates: namely, S. Derby, S. Infantis, S. London, S. Rissen and S. Kedougou. These isolates from pigs were reported by just two countries, Romania (n = 6) and Hungary (n = 4). Presumptive ESBL‐producing Salmonella (n = 8) was more frequently reported than presumptive ESBL + AmpC producing Salmonella isolates (n = 2). In calves, only a single S. Derby isolate from Spain displayed an ESBL + AmpC phenotype.
In humans in 2021, presumptive ESBL‐producing Salmonella were identified in 0.8% of isolates tested, with the highest occurrence in Italy (3.5%). AmpC was less frequent (0.1%). Of note, there were no Salmonella isolates reported to be both AmpC‐ and ESBL‐producing nor carbapenemase producing. Of the 13 serovars and subspecies identified with an ESBL phenotype from humans in 2021, it was most commonly found in S. Infantis, monophasic S. Typhimurium and S. Typhimurium (5.2%, n = 27/517; 1.2%, n = 23/1867; 0.9%, n = 11/1,246, respectively). For human cases, the proportion of S. Kentucky with an ESBL phenotype decreased from 20.3% in 2017 to 3.8% in 2021, with three countries (France, the Netherlands and Sweden) reporting presumptive ESBL‐producing S. Kentucky in 2021. The introduction and spread of S. Kentucky with bla CTX‐M‐14b in Europe has recently been described by Coipan et al. (2020). AmpC‐type β‐lactamases were reported in five different serovars, most commonly in monophasic S. Typhimurium, S. Brandenburg and S. Goldcoast (0.3%, n = 6/1867; 1.8%, n = 2/110; 5.1%, n = 2/39, respectively). Of note, all human Salmonella isolates resistant to cefotaxime and/or ceftazidime identified in local or regional laboratories in Italy are submitted to the national surveillance system for strict monitoring of ESBL/AmpC. This may have resulted in an overestimation of such findings, although the high proportions of ESBL observed in isolates from Italian broilers and turkeys would seemingly confirm these results.
In conclusion, it is important to note that zoonotic Salmonella infections in humans tend to be self‐limiting diseases, rarely leading to clinical conditions, where a patient should receive antibiotic treatment. However, considering the relatively high number of people that each year fall ill with salmonellosis, the level of resistance to commonly used antimicrobials or antimicrobials used for critically ill patients such as the CIA needs to be continuously watched as these still may be of importance. In addition, the monitoring of the resistance levels in Salmonella from food‐producing animals and meat derived thereof allows the assessment and the evaluation of the occurrence of AMR in the EU and help to identify the achievements in the efforts to tackle AMR.
3. Antimicrobial resistance in Campylobacter spp.
3.1. Key findings
For 2021, 22 MSs and two non‐MS (Iceland and Norway) reported data on AMR in Campylobacter jejuni from human campylobacteriosis infections and 20 MSs and two non‐MS (Iceland and Norway) on AMR in Campylobacter coli. This is an increase in the number of countries reporting compared to 2019 and 2020.
In 2020, data related to the antimicrobial susceptibility of 3,382 C. jejuni isolates from broilers and 1,066 C. jejuni isolates from fattening turkeys were reported by 27 and 9 MSs, respectively. In relation to C. jejuni, antimicrobial susceptibility data from 1,198 isolates from calves (bovines less than 1 year old) and from 60 fattening pig isolates were reported in 2021 by 10 and 12 MSs, respectively.
Data related to the antimicrobial susceptibility of C. coli from 388 isolates from broilers and 567 isolates from fattening turkeys were reported in 2020 by 7 and 3 MSs, respectively. Data related to the antimicrobial susceptibility of C. coli from 443 isolates from calves and 3,546 isolates from pigs were reported in 2021 by 10 and 27 MSs, respectively.
Resistance rates differed greatly between reporting countries, between antimicrobials and between the two Campylobacter species.
Levels of resistance to ciprofloxacin ranged from high to extremely high in C. jejuni and C. coli isolates from humans in the EU and from very high to extremely high in C. jejuni and C. coli isolates from poultry, fattening pigs and calves. Resistance levels to ciprofloxacin in human C. jejuni isolates ranged from 27.6% to 100% among the EU countries. In two countries, all C. coli isolates tested from humans were resistant to ciprofloxacin. In 2021 for C. coli isolates, 14 out of 18 countries reporting more than 10 isolates found levels of ciprofloxacin resistance of > 70%. In relation to animal data, the highest levels of resistance to ciprofloxacin were observed in C. coli isolates from fattening turkeys in 2020 (80.4%) and from calves in 2021 (79.7%), followed by broilers (61.9%) in 2020 and fattening pigs (51.7%) in 2021. Overall, the levels of resistance to ciprofloxacin were higher for C. coli than for C. jejuni although the level of resistance to ciprofloxacin obtained from C. jejuni isolates from poultry in 2020 were also extremely high (77.9% in fattening turkeys and 72.8% in broilers).
Resistance to erythromycin was either not detected or detected at very low levels in C. jejuni from humans, poultry and calves, but was higher in C. coli isolates from humans (8.5%), calves (35.7%), fattening turkeys (21.5%), fattening pigs (12.3%) and broilers (4.4%).
Combined resistance to both ciprofloxacin and erythromycin, which are considered critically important antimicrobials for the treatment of campylobacteriosis, was generally rare to low in C. jejuni from humans, poultry, pigs and calves. The combined resistance was low to moderate in C. coli from humans and broilers, and moderate in C. coli isolated from fattening turkeys and calves. This finding may be a cause for public health concern.
The observed levels of resistance to gentamicin and ertapenem in C. coli isolated from calves in 2021 were 12.4% and 29.1%, respectively, which might be a cause for public health concern as they are recommended antimicrobials for treatment in severe invasive infections of Campylobacter in humans. Gentamicin resistance in C. coli from humans was observed at low levels except in one MS, while ertapenem is not (yet) included in the priority panel for Campylobacter monitoring of human isolates at EU level.
The prevalence of resistance to selected antimicrobials in C. coli from fattening pigs in 2021 has been estimated at country. Between‐country variability from low to extremely high levels was observed in the prevalences of ciprofloxacin resistant (ranging from 6.9% to 78.2%) and tetracycline resistant (ranging from 0.0% to 86.5%) C. coli from fattening pigs. Interestingly, a limited between‐country variation and notably lower levels of prevalence of resistance to erythromycin were found in C. coli from fattening pigs (below 10% for 21 MSs and 3 non‐MSs; ranging from 14.9% to 39.7% in six MSs). Noteworthy, the MS with the highest prevalence of resistance to erythromycin in C. coli from fattening pigs in 2021 had also the highest level of erythromycin occurrence of resistance in C. coli from humans.
Overall, complete susceptibility (CS) (i.e. defined in this report as susceptibility to ciprofloxacin, erythromycin, tetracycline and gentamicin) was higher in C. jejuni than in C. coli isolates. The overall CS observed from C. jejuni isolates was: 30.9% in humans in 2021, 23.0% in broilers in 2020, 16.8% in fattening turkeys in 2020 and 21.6% in calves in 2021 and 48.3% in fattening pigs in 2021. Regarding C. coli, the overall CS observed was moderate for humans (13.2%), broilers (13.7%) and fattening pigs (19.9%), while it was low for isolates from fattening turkeys (4.4%) and calves (6.3%).
Over the period 2013–2021, resistance to ciprofloxacin in C. jejuni from humans increased in 12 reporting countries (11 MSs and 1 non‐MS) and decreased in three (2 MSs and 1 non‐MS). Resistance to ciprofloxacin in C. coli from humans increased in three MSs and decreased in two countries (1 MS and 1 non‐MS) in the same period. Similar trends were observed in C. jejuni from broilers in the period between 2009 and 2020 where resistance to ciprofloxacin increased in 14 reporting countries (12 MSs and 2 non‐MSs) and decreased only in one MS. During the period 2009–2021 (2015–2021 for 1 MS), an increasing trend in resistance to ciprofloxacin was also observed in C. coli isolates from fattening pigs in four reporting countries (2 MSs and 2 non‐MSs).
Based on trend data, erythromycin resistance decreased in C. jejuni from humans in seven countries (5 MSs and 2 non‐MSs; period 2013–2021), from broilers in five MSs (over 2009–2020), from fattening turkeys in three MSs (period 2014–2020) and in C. coli from humans in five MSs (period 2013–2021), from broilers in one MS (period 2009–2020) and from fattening pigs in four countries (3 MSs and 1 non‐MS; period 2009–2021).
Although the period assessed for the trend and the countries providing data are slightly different for humans and animals, similar increasing and decreasing trends were often observed within a country in both humans and poultry, particularly regarding trends in increasing ciprofloxacin resistance.
3.2. Data on AMR in Campylobacter spp. addressed
Campylobacter bacteria are ubiquitous and can be found widespread in the environment and in animals. Campylobacter is frequently found in water, animals, biofilms and other environmental niches that can all be considered potential modes of transmission to humans (Garcıa and Percival, 2011; WHO, 2012, 2020; Garcia and Heredia, 2013; Kreling et al., 2020; Lopez‐Chavarrias et al., 2021). Birds are considered natural hosts for Campylobacter (Sopwith et al., 2008; Jokinen et al., 2011; Lopez‐Chavarrias et al., 2021). Campylobacter is frequently present in the intestines of poultry, cattle, sheep and pigs, and may contaminate the food processing environment and food products thus posing a public health risk to consumers (Dykes and Moorhead, 2001; Garcia et al., 2010a,b). Food‐producing animals are a major source of human campylobacteriosis through contamination of food products. However, wild birds, pets and environmental water may also play a role as potential modes of transmission (Moré et al., 2017; Szczepanska et al., 2017; EFSA, 2019). Campylobacter strains resistant to antibiotics may interfere with the treatment of human campylobacteriosis (Moore et al., 2006; Garcia and Heredia, 2013; Lopez‐Chavarrias et al., 2021).
The two main Campylobacter species responsible for human infections are C. jejuni, which is a predominant species in poultry, followed by C. coli (Jehanne et al., 2020), frequently found in pigs and in poultry, sometimes at higher rates than C. jejuni (Pergola et al., 2017). C. coli is often more resistant than C. jejuni to several important antimicrobials and may contain and transfer resistance genes to C. jejuni.
Campylobacter AMR data from human infections either derive from monitoring programs set up by national public health reference laboratories/services or is collected from primary or regional laboratories and integrated with the case information in the national surveillance of human Campylobacter infections. This report covers AMR data for C. jejuni and C. coli from human cases from 2021. Data from 2020 are presented in the 2019/2020 report (EFSA and ECDC, 2022).
In the framework of the most recent Commission Implementing Decision (EU) 2020/1729 the monitoring of AMR in Campylobacter spp. from food‐producing animals and meat derived thereof is focused on the species C. jejuni and C. coli. In accordance with Commission Implementing Decision (EU) 2020/1729, from 2021 onward, the AMR monitoring is mandatory, at biannual basis, in C. jejuni and C. coli from caecal samples from broilers, fattening turkeys, bovine animals under 1 year of age (where the national production of turkey meat and bovine meat is more than 10,000 tonnes per year) and fattening pigs at slaughter.
This chapter includes 2021 data on C. jejuni and C. coli from fattening pigs and calves resulting from mandatory monitoring in accordance with Commission Implementing Decision (EU) 2020/1729, as well as 2020 data from mandatory monitoring of AMR in C. jejuni and voluntary monitoring of C. coli in broilers and fattening turkeys in accordance with Commission Implementing Decision 2013/652/EU. In addition, the voluntary monitoring of AMR in Campylobacter isolates recovered from meat samples (of broilers, turkeys, bovine and pigs) at retail was performed in 2020 and 2021 and related data are also presented in this chapter and in the Annex B.
Detailed information on antimicrobial resistance data reporting including requirements, sample descriptions and codes for mandatory and voluntary reporting are presented in EFSA's manual for reporting AMR data within the framework of Directive 2003/99/EC and Commission Implementing Decision (EU) 2020/1729 (EFSA, 2021).
Further consideration on the data used and on the methodology applied in the analysis can be found in Appendix F – ‘Material and methods’.
3.3. Humans: occurrence of antimicrobial resistance in Campylobacter
3.3.1. Data reported
For 2021 AMR monitoring and reporting, 22 MSs and two non‐MS (Iceland and Norway) reported data on AMR isolated from Campylobacter jejuni from human cases of campylobacteriosis. The corresponding number for C. coli was 20 MSs and two non‐MS (Iceland and Norway). This is an increase in the number of countries reporting compared to 2019 and 2020. Lower reporting figures in 2020 are likely due to the impact of the COVID‐19 pandemic on referral of isolates and laboratory capacity. No data has been reported for 2020 and 2021 from the United Kingdom due to its withdrawal from the EU on 30 January 2020. Hungary reported Campylobacter AMR data for the first time for 2021.
Fifteen countries reported measured values, seven reported results interpreted as susceptible standard dosing regimen, susceptible increased exposure or resistant (SIR) according to the clinical breakpoints (CBPs) applied and two countries (Ireland and Sweden) reported results categorised as predicted wild type or predicted non‐wild type based on analysis of bacterial genomes (Appendix F – Table F.2). Not all countries reported results for all antimicrobials in the harmonised panel (ECDC, 2016).
Table F.2.
Antimicrobials reported, method used, type of data reported and interpretive criteria applied by MSs for human Campylobacter data in 2021
| Country | Gentamicin | Co‐amoxiclav | Ciprofloxacin | Erythromycin | Tetracyclines | Method used | Quantitative (Q) or categorical (SIR) | Interpretive criteria |
|---|---|---|---|---|---|---|---|---|
| Austria | ● | ● | ● | ● | DL | Q | Interpreted by ECDC. EUCAST ECOFF (CIP, ERY, GEN, TET), CA‐SFM CBP 2021 (AMC) | |
| Bulgaria | ● | ● | ● | ● | DD | SIR | No information available. | |
| Cyprus | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | ||
| Denmark | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. | |
| Estonia | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. | |
| Finland | ● | ● | ● | DD/DLG | Q | Interpreted by ECDC, as for Austria. | ||
| France | ● | ● | ● | ● | ● | DD | SIR | EUCAST CBP (CIP, ERY, TET), CA‐SFM CBP (AMC, GEN) |
| Germany | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. |
| Hungary | ● | ● | ● | No information | SIR | No information available. | ||
| Ireland | ● | ● | ● | WGS | PWT/PNWT | No information available. | ||
| Iceland | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | |||
| Italy | ● | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | |
| Lithuania | ● | ● | ● | DD | SIR | EUCAST CBP | ||
| Luxembourg | ● | ● | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. |
| Malta | ● | ● | ● | ● | ● | DLG/DL | Q | Interpreted by ECDC, as for Austria. |
| Netherlands | ● | ● | ● | DD/DL | SIR | EUCAST CBP | ||
| Norway | ● | ● | ● | ● | DLG | Q | Interpreted by ECDC, as for Austria. | |
| Poland | ● | ● | ● | ● | ● | No information | SIR | No information available. |
| Portugal | ● | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | |
| Romania | ● | ● | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. |
| Slovakia | ● | ● | ● | ● | ● | No information | SIR | No information available. |
| Slovenia | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | ||
| Spain | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. |
| Sweden | ● | ● | ● | ● | WGS | PWT/PNWT | Sequencing results interpreted by the laboratory with NCBI AMRFinder and CGE ResFinder and PointFinder |
MSs: Member States; AST: antimicrobial susceptibility testing; DD: disk diffusion; DL: dilution; DLG: dilution with gradient strip; WGS: whole genome sequencing; Q: quantitative data; SIR: susceptible standard dosing regimen, susceptible increased exposure, resistant (categorical data); PWT/PNWT: predicted wild type/predicted non‐wild type (categorical); ECDC: European Centre for Disease Prevention and Control; EUCAST: European Committee on Antimicrobial Susceptibility Testing; CA‐SFM: French Society for Microbiology; NCBI: National Center for Biotechnology Information, US; CGE: Center for Genomic Epidemiology, Denmark; ECOFF: epidemiological cut‐off; CBP: clinical breakpoint; CIP: ciprofloxacin; ERY: erythromycin; GEN: gentamicin; TET: tetracycline; AMC: amoxicillin/clavulanate.
The reported data represented 21.6% and 24.7% of the confirmed human cases with Campylobacter jejuni and Campylobacter coli, respectively, reported in the EU/EEA in 2021.
3.3.2. Occurrence of resistance
In 2021, reported data related to occurrence of resistance indicated that high to extremely high resistance levels to ciprofloxacin were observed in human Campylobacter jejuni isolates in the EU ranging from 27.6% reported by Ireland to 100% reported by Poland. The average level of ciprofloxacin resistance in EU was 64.5% for C. jejuni and 69.6% for C. coli; slightly higher than levels reported in 2020. Overall, Nordic countries reported low to high levels of resistance to ciprofloxacin ranging from 8.3% in Iceland to 49.1% in Denmark. The rest of the reporting countries obtained results that indicated very high to extremely high resistance levels to ciprofloxacin (Figure 13; Annex B, Table 1). In 2021, data related to occurrence of resistance to ciprofloxacin in C. coli isolates indicated that very high to extremely high resistance levels to ciprofloxacin were reported, apart from Ireland that reported high levels (Figure 13; Annex B, Table 2). Overall, resistance levels to ciprofloxacin were higher in C. coli than in C. jejuni. The highest levels of resistance to ciprofloxacin in C. coli isolates were reported by Portugal and Estonia (100%). Of note, in 2021, for those countries reporting more than 10 isolates of C. coli, 14 out of 18 found extremely high levels (> 70%) of ciprofloxacin resistance (Annex B, Table 2).
Figure 13.
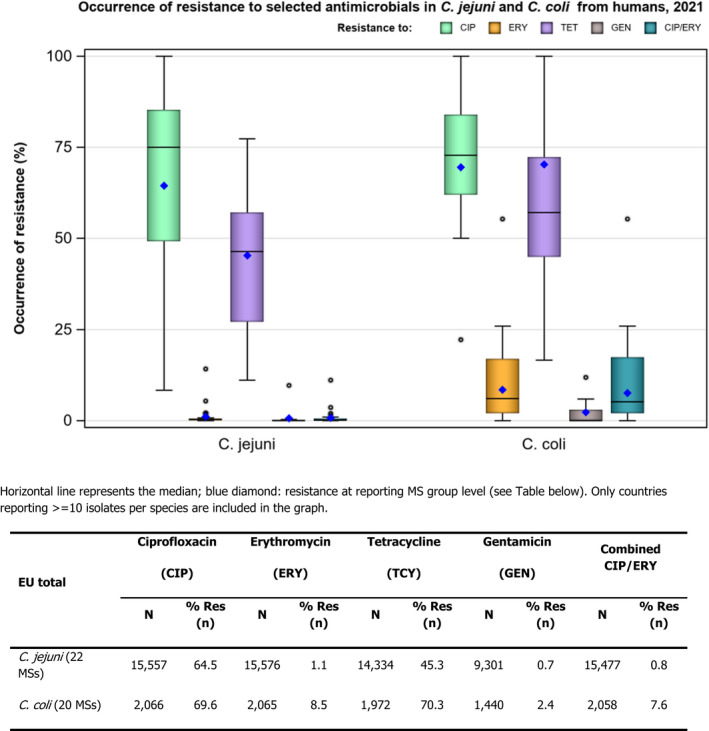
Box‐plot of the occurrence of resistance to a selection of antimicrobials in C. jejuni and C. coli isolates from humans, 2021
The level of resistance to erythromycin in human C. jejuni isolates in the EU was overall very low (1.1%) except for Spain where the results indicated a higher level of resistance (14.2%) (Figure 13; Annex B, Table 1). The level of resistance in human C. coli isolates to erythromycin in EU was overall low (8.5%) but highly variable between countries, ranging from 0% in Ireland and Slovenia to 55.3% in Portugal. Most of the countries, however, reported values between 1% and 26% (Figure 13; Annex B, Table 2).
The average levels of resistance in human isolates to tetracycline were high (45.3%) in C. jejuni (except in Finland, Ireland and Sweden where it was low) and extremely high (70.3%) in C. coli (except in Ireland where it was low). These levels of resistance to tetracycline were similar to those reported in 2020. The percentages of resistance to tetracycline in C. jejuni isolates ranged from 11.2% in Finland to 77.3% in Portugal. The percentages of resistance to tetracycline in C. coli isolates ranged from 16.7% in Ireland to 100% in Portugal (Figure 13; Annex B, Tables 1 and 2).
Resistance levels to gentamicin were overall low with an EU average of 0.7% and 2.4% in human C. jejuni and C. coli isolates, respectively. The highest levels were reported by Spain (9.6% and 11.9% in human C. jejuni and C. coli isolates, respectively) (Figure 13; Annex B, Tables 1 and 2).
Few countries reported resistance data in relation to co‐amoxiclav. The results indicate overall low levels (average EU level 6.6% and 9.2% in C. jejuni and C. coli isolates from humans, respectively) except for Germany that reported levels of 41.9% and 44.0% in C. jejuni and C. coli, respectively (Annex B, Tables 1 and 2).
3.3.3. Combined resistance to ciprofloxacin and erythromycin
Combined resistance to both ciprofloxacin and erythromycin, which are considered critically important for treatment of campylobacteriosis, was generally very low at EU level (0.8%) in C. jejuni and low (7.6%) in C. coli for 2021 (Figure 13). The levels of combined resistance to both ciprofloxacin and erythromycin in human C. jejuni isolates ranged from 0% to 11.1%; the highest level being reported by Spain. The levels of combined resistance to both ciprofloxacin and erythromycin in human C. coli isolates ranged from 0% to 55.3%; the highest level being reported by Portugal (Figure 14; Annex B, Tables 3 and 4).
Figure 14.
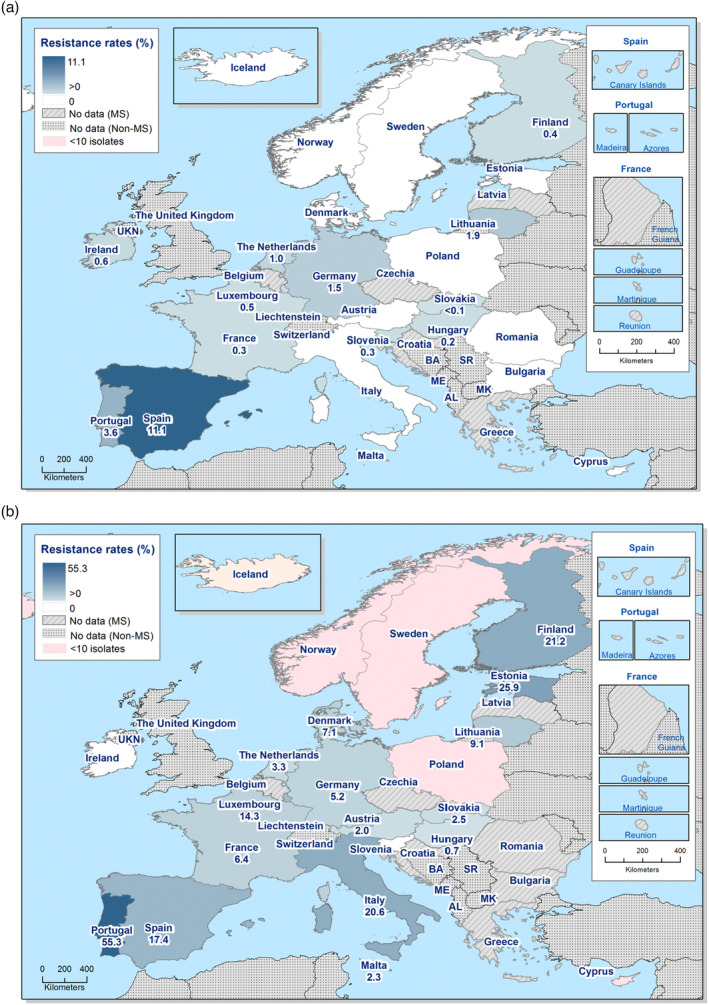
Spatial distribution of combined resistance to ciprofloxacin and erythromycin in (a) C. jejuni and (b) C. coli isolates from humans, 2021
3.3.4. Complete susceptibility and multidrug resistance
Multidrug resistance (MDR) in isolates tested for four antimicrobial classes (fluoroquinolones, macrolides, tetracyclines and aminoglycosides) was overall very low in C. jejuni (1%) and low in C. coli (9.9%) (Figure 15; Annex B, Tables 5 and 6). To note, the MDR analysis is based on data from fewer reporting countries as not all countries test gentamicin susceptibility. Complete susceptibility (CS) to the four antimicrobial classes was 30.9% in C. jejuni and 13.2% in C. coli (Figure 15; Annex B, Tables 5 and 6).
Figure 15.

- N: Total number of isolates reported.
The most common resistance pattern in C. jejuni isolates was complete susceptibility to the four antimicrobial classes in the harmonised panel (30.9%) while in C. coli it was resistance to both ciprofloxacin and tetracycline (33.9%). The second most common pattern in C. jejuni as resistance to both ciprofloxacin and tetracycline, observed in 27.7% of C. jejuni isolates while in C. coli it was tetracycline resistance alone (13.4%).
3.3.5. Temporal trends
Temporal trends were analysed for countries reporting data for at least 3 years over the period 2013–2021. Trends in antimicrobial resistance to C. jejuni and C. coli varied by country for selected antimicrobials (Table 6; Figures 16 and 17). As the number of Campylobacter isolates tested in humans is high, small changes in resistance may come out as significant. Statistically significant (p < 0.05) increasing trends of fluoroquinolone resistance were observed in C. jejuni isolates from eleven MSs and one non‐MS (United Kingdom) and in C. coli isolates from three MSs. Statistically significant (p < 0.05) decreasing trends of fluoroquinolone resistance were observed in C. jejuni isolates from two MSs (Finland and Portugal) and one non‐MS (Norway) and in C. coli isolates from one MS (France) and one non‐MS (UK) (Table 6; Figures 16 and 17). Tetracycline resistance increased significantly in six MSs and one non‐MS (UK) in C. jejuni isolates while four MSs and one non‐MS (Norway) observed a significant decrease in the same period. Erythromycin resistance in C. jejuni isolates from humans significantly increased in one country (Spain) while significantly decreased in five MSs and two non‐MSs (Norway and UK). Erythromycin resistance in C. coli isolates significantly decreased in five MSs (Table 6) and significantly increased in one non‐MS (UK). Results in relation to significantly increasing or decreasing trends at EU group level indicated that in C. jejuni a significant increase was noticed in the levels of resistance to ciprofloxacin and tetracycline during the period 2013–2021 while a significant decrease was observed in relation to resistance to erythromycin. Similarly for C. coli, a significant increase in resistance to tetracycline was observed at the EU level (but not to ciprofloxacin) and a significant decrease observed in resistance to erythromycin (Table 6; Figures 16 and 17).
Table 6.
Number of countries with significantly increasing or decreasing trends in resistance to selected antimicrobials for Campylobacter jejuni and C. coli in humans, 2013–2021
| Species | Ciprofloxacin | Erythromycin | Tetracycline | |||
|---|---|---|---|---|---|---|
| Incr. | Decr. | Incr. | Decr. | Incr. | Decr. | |
| C. jejuni (19 MS + 3 non‐MS) | 12 (AT, BG, DK, EE, FR, LT, MT, NL, PL, SI, SK, UK) | 3 (FI, NO, PT) | 1 (ES) | 7 (DK, FI, IT, MT, NO, SI, UK) | 7 (AT, DK, EE, NL, SI, SK, UK) | 5 (ES, FI, FR, LT, NO) |
| C. coli (14 MSs + 1 non‐MS) | 3 (NL, SI, SK) | 2 (FR, UK) | 1 (UK) | 5 (EE, ES, FR MT, SK) | 4 (FR, NL, SI, SK) | – |
Figure 16.

- Data from the United Kingdom included up to 2019. Trend at EU MS group level is excluding UK data.
Figure 17.

- Data from the United Kingdom included up to 2019. Trend at EU MS group level is excluding UK data.
3.3.6. High‐level resistance to erythromycin
High‐level resistance to erythromycin (MIC > 128 mg/L) was assessed as a potential indication for transferrable erythromycin resistance due to the presence of the erm(B) gene. The results indicated that 1.4% of the C. jejuni isolates (N = 3,102, 8 MSs + 1 non‐MS) showed MIC > 128 mg/L while for C. coli the percentage was higher, 4.8% (N = 480, 7 MSs + 1 non‐MS) (Figure 18). These results were similar to 2019 but higher than in 2020 (EFSA and ECDC, 2022). Similarly, in 0.5% (N = 2,447, 9 MSs) of C. jejuni and 17.5% (N = 200, 6 MSs + 1 non/MS) of C. coli tested with disk diffusion no inhibition zone could be observed (6 mm zone equals the disk size), which corresponds to a MIC of ≥ 128 mg/L for C. jejuni and 64 ‐≥ 128 mg/L for C. coli.
Figure 18.
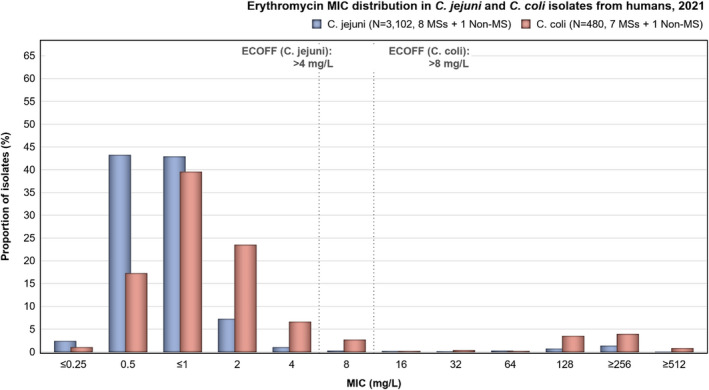
Erythromycin MIC distribution in C. jejuni and C. coli isolates from humans, 2021
3.4. Food‐producing animals and meat thereof: occurrence and prevalence of antimicrobial resistance in Campylobacter
3.4.1. Data reported
In the present report, the 2020 resistance data on Campylobacter from poultry are considered for comparison with the AMR data on Campylobacter isolates from pigs and calves reported in 2021.
In the year 2020, mandatory data on C. jejuni isolates recovered from caecal samples of broilers were reported by all 27 MSs and three non‐MSs (Norway, Switzerland and the United Kingdom) (N = 3,382 and N = 441, respectively). Data on C. jejuni isolates recovered from caecal samples of fattening turkeys were reported by nine MSs (Austria, France, Germany, Hungary, Italy, Poland, Portugal, Romania and Spain) and two non‐MSs (Norway and the United Kingdom) in 2020 (N = 1,066 and N = 174, respectively). In addition, seven MSs (Czechia, France, Ireland, Latvia, Luxembourg, the Netherlands and Slovenia) and one non‐MS (Switzerland) voluntarily reported data on C. coli isolates recovered from caecal samples of broilers (N = 388 and N = 68, respectively). Furthermore, three MSs (France, Germany and Spain) reported data on C. coli isolates recovered from caecal samples of fattening turkeys (N = 567). The complete overview of the data reported in 2020, including information on meat categories, is presented in Annex B (Table 7).
Table 7.
Occurrence of resistance (%) to selected antimicrobials in C. jejuni and C. coli from carcases, fresh meat, unspecified meat and meat preparations from broilers, using harmonised ECOFFs, in 2020 and 2021 (only MSs)
| Campylobacter species | Categories | Year | Number of isolates | Reporting Countries (N) | GEN | STR | CHL | ETP | NAL | CIP | ERY | TET | CIP/ERY |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C. jejuni | Carcases | 2020 | 361 | HR, DE, NL, RO (4) | 0 | 23.8 | 81.4 | 82.8 | 0.6 | 57.6 | 0.3 | ||
| 2021 | 67 | NL, RO (2) | 0 | 0 | 11.9 | 62.3 | 0 | 58.2 | 0 | ||||
| Fresh | 2020 | 343 | AT, BE, DE, LU, NL (5) | 0 | 22.2 | 73.5 | 74.9 | 0 | 58.6 | 0 | |||
| 2021 | 115 | BE, LU, NL (3) | 0 | 0 | 7.8 | 60.9 | 0 | 46.1 | 0 | ||||
| Meat preparations | 2020 | 35 | LU, NL (2) | 0 | 22.9 | 65.7 | 68.6 | 0 | 57.1 | 0 | |||
| 2021 | 25 | LU, NL (2) | 0 | 0 | 4.0 | 52.0 | 0 | 44.0 | 0 | ||||
| Meat unspecified | 2020 | 70 | IT (1) | 0 | 1.4 | 55.7 | 75.7 | 0 | 58.6 | 0 | |||
| 2021 | 8 | PT (1) | 0 | 0 | 25.0 | 87.5 | 12.5 | 100 | 12.5 | ||||
| C. coli | Carcases | 2020 | 76 | DE, LU, NL, RO (4) | 2.6 | 7.9 | 71.1 | 71.1 | 10.5 | 57.9 | 10.5 | ||
| 2021 | 52 | NL, RO (2) | 0 | 0 | 25.0 | 96.2 | 3.9 | 59.6 | 3.9 | ||||
| Fresh | 2020 | 99 | AT, BE, DE, LU, NL (5) | 1.0 | 16.2 | 84.9 | 84.9 | 0.6 | 67.7 | 10.1 | |||
| 2021 | 28 | BE, LU, NL (3) | 0 | 0 | 46.4 | 75.0 | 10.7 | 60.7 | 10.7 | ||||
| Meat preparations | 2020 | 17 | NL (1) | 0 | 17.7 | 70.6 | 70.6 | 0 | 35.3 | 0 | |||
| 2021 | 14 | NL (1) | 0 | 0 | 14.3 | 85.7 | 7.1 | 42.9 | 7.1 | ||||
| Meat unspecified | 2021 | 10 | PT (1) | 0 | 0 | 40.0 | 100 | 40.0 | 100 | 40.0 |
GEN: gentamicin; STR: streptomycin; NAL: nalidixic acid; CHL: chloramphenicol; ETP: ertapenem; CIP: ciprofloxacin; ERY: erythromycin; TET: tetracycline; CIP/ERY: combined ‘microbiological’ resistance to ciprofloxacin and erythromycin; CS: complete susceptibility to the four antimicrobial classes (ciprofloxacin/nalidixic acid; erythromycin; tetracycline and gentamicin/streptomycin); N: Total number of reporting Member States (MSs). Additional note: STR was not tested in 2021; however; CHL and ETP were first tested in 2021.
In 2021, 12 MSs (Bulgaria, Cyprus, Denmark, Germany, Ireland, Italy, Latvia, Lithuania, Luxemburg, Malta, the Netherlands and Portugal) and one non‐MS (Norway) reported mandatory data on C. jejuni isolates recovered from fattening pigs (N = 60 and N = 17, respectively). Ten MSs (Belgium, Croatia, Denmark, France, Germany, Italy, the Netherlands, Portugal, Romania and Spain) and two non‐MSs (Norway and Switzerland) reported data on C. jejuni isolates recovered from calves under 1 year of age (N = 1,198 and N = 270, respectively). Twenty‐six MSs (all MSs, save Czechia) and the United Kingdom (Northern Ireland), as well as three non‐MSs (Iceland, Norway and Switzerland) reported mandatory data on C. coli isolates recovered from fattening pigs (N = 3,546 and N = 624, respectively). Ten MSs (Belgium, Croatia, Denmark, France, Germany, Italy, the Netherlands, Portugal, Romania and Spain) reported data on C. coli isolates recovered from calves under 1 year of age (N = 443) in 2021 (Annex B, Tables 8 and 9).
The complete overview of the data (mandatory and voluntary) from food‐producing animal and meat derived thereof, reported in 2020 and 2021, is presented in Annex B (Tables 7–11).
Resistance data concerning food‐producing animals and meat derived thereof, reported in 2020 and 2021, are presented in the following sections. Additional tables on Campylobacter in food and food‐producing animals have been included in Annex B that is available as supporting documentation in Zenodo.
The new EU rules for the AMR monitoring in Campylobacter in place from 2021 (Commission Implementing Decision (EU) 2020/1729; see also EFSA, 2021) implemented changes to the harmonised panel of antimicrobials, consisting in the removal of streptomycin and nalidixic acid and in the inclusion of two new substances: ertapenem and chloramphenicol. Therefore, the mandatory antimicrobials to be reported for C. jejuni and C. coli from 2021 are: chloramphenicol, ciprofloxacin, ertapenem, erythromycin, gentamicin and tetracycline. Furthermore, in accordance with Commission Implementing Decision (EU) 2020/1729, the range of concentration (mg/L) has been reduced for gentamicin, and increased for erythromycin and ciprofloxacin. As this report presents both 2020 and 2021 data, the legislative requirements laid down in Decision 2013/652/EC have been applied for 2020 data, while 2021 data are reported in accordance with new AMR monitoring rules laid down in Commission Implementing Decision (EU) 2020/1729.
3.4.2. Occurrence of resistance in meat samples from broilers
Data reported during 2020 and 2021 indicate that the highest levels of resistance in C. jejuni and C. coli isolates recovered from broiler meat were noted for ciprofloxacin and nalidixic acid (overall percentages: 65.7%–84.9% in 2020, and 52%–100% in 2021), and for tetracycline (overall percentages: 35.3%–67.7% in 2020, and 42.9%–100% in 2021) considering the 1,001 isolates (809 C. jejuni and 192 C. coli) and 319 isolates (215 C. jejuni and 104 C. coli) reported from nine MSs in 2020 and from five MSs in 2021, respectively (Table 7). It can be noted that in both 2020 and 2021, the levels of resistance to the above‐mentioned antimicrobials were reported to be higher in carcases and fresh meat than in meat preparations. Resistance to gentamicin in C. jejuni isolates recovered from poultry meat was not observed in 2020 and 2021 and only low levels of resistance were reported in C. coli from broiler carcases and broiler fresh meat in 2020 (Table 7). Resistance to erythromycin in C. jejuni isolates from broiler meat was detected at low levels while a higher resistance to this antimicrobial was reported in C. coli isolates in both reporting years. Resistance to streptomycin was observed at low levels (data from 2020). Based on data reported for the first time in 2021, moderate to high levels of resistance to ertapenem were observed in particular for C. coli isolates (Table 7). This finding should interpreted with caution due to the very low number of MSs reporting data on broiler meat in 2021 (from one to three MSs reporting data on the different broiler meat categories). No resistance to chloramphenicol was observed in Campylobacter isolates from broiler meat, as reported for the first time in 2021 (Table 7).
3.4.3. Occurrence of resistance in poultry, pigs and calves
Comparison of resistance data between bacterial and animal species should be done with caution due to the dispersion of resistance rates between countries and because numbers of isolates and reporting countries vary, especially for voluntary monitoring and reporting. Data reported in 2021 for C. jejuni and C. coli isolates from legislative and non‐legislative categories are presented in Annex B, Tables 8–11.
In this Report, data on the occurrence of resistance in Campylobacter species in caecal samples from poultry (2020), pigs (2021) and calves under 1 year of age (2021) are presented in Table 8 and Figure 19. The detailed country‐level information on the occurrence of resistance is presented in Annex B (Tables 12–19).
Table 8.
Occurrence of resistance (%) to selected antimicrobials in C. coli and C. jejuni in caecal samples from poultry, pigs and calves using harmonised ECOFFs, 27 EU MSs and United Kingdom (Norther Ireland), 2020 and 2021
| Campylobacter species | Categories | Year | Number isolates | Reporting countries (N) | GEN | STR | CHL | ETP | NAL | CIP | ERY | TET | CIP/ERY |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C. jejuni | Broilers | 2020 | 3,382 | AT, BE, BG, CY, CZ, DE, DK, EE, EL, ES, FI, FR, HR, HU, IE, IT, LT, LU, LV, MT, NL, PL, PT, RO, SE, SI, SK (27) | 0.1 | 15.6 | 69.2 | 72.8 | 0.8 | 52.7 | 0.7 | ||
| Calves | 2021 | 1,198 | BE, DE, DK, ES, FR, IT, NL, PT, RO(10) | 0.5 | 0.1 | 1.0 | 54.7 | 1.0 | 68.8 | 0.8 | |||
| Fattening turkeys | 2020 | 1,066 | AT, DE, ES, FR, HU, IT, PL, PT, RO (9) | 0.1 | 11.4 | 71.0 | 77.9 | 0.8 | 58.5 | 0.8 | |||
| Fattening igs | 2021 | 60 | BG, CY, DK, DE, IE, IT, LV, LT, LU, MT, NL, PT (12) | 1.7 | 0.0 | 0.0 | 41.7 | 1.7 | 43.3 | 1.7 | |||
| C. coli | Broilers | 2020 | 388 | CZ, FR, IE, LV, LU, NL, SI (7) | 0.0 | 16.5 | 61.1 | 61.9 | 4.4 | 67.3 | 4.1 | ||
| Calves | 2021 | 443 | BE, DE, DK, ES, FR, IT, NL, PT, RO (10) | 12.4 | 3.4 | 29.1 | 79.7 | 35.7 | 90.5 | 32.7 | |||
| Fattening turkeys | 2020 | 567 | DE, ES, FR (3) | 0.2 | 11.5 | 80.2 | 80.4 | 21.5 | 89.2 | 21.2 | |||
| Fattening pigs | 2021 | 3,546 | AT, BE, BG, CY, DE, DK, EE, EL, ES, FI, FR, HR, HU, IE, IT, LV, LT, LU, MT, NL, PL, PT, RO, SE, SI, SK, XI (26+XI) | 2.6 | 0.5 | 1.3 | 51.7 | 12.3 | 69.3 | 9.3 |
GEN: gentamicin; STR: streptomycin; NAL: nalidixic acid; CHL: chloramphenicol; ETP: ertapenem; CIP: ciprofloxacin; ERY: erythromycin; TET: tetracycline; CIP/ERY: combined ‘microbiological’ resistance to ciprofloxacin and erythromycin; CS: complete susceptibility to the four antimicrobial classes (ciprofloxacin/nalidixic acid, erythromycin, tetracycline and gentamicin/streptomycin); N: Total number of reporting Member States (MSs); XI: Northern Ireland; Additional note: STR was not tested in 2021, however, CHL and ETP were first tested in 2021.
Figure 19.
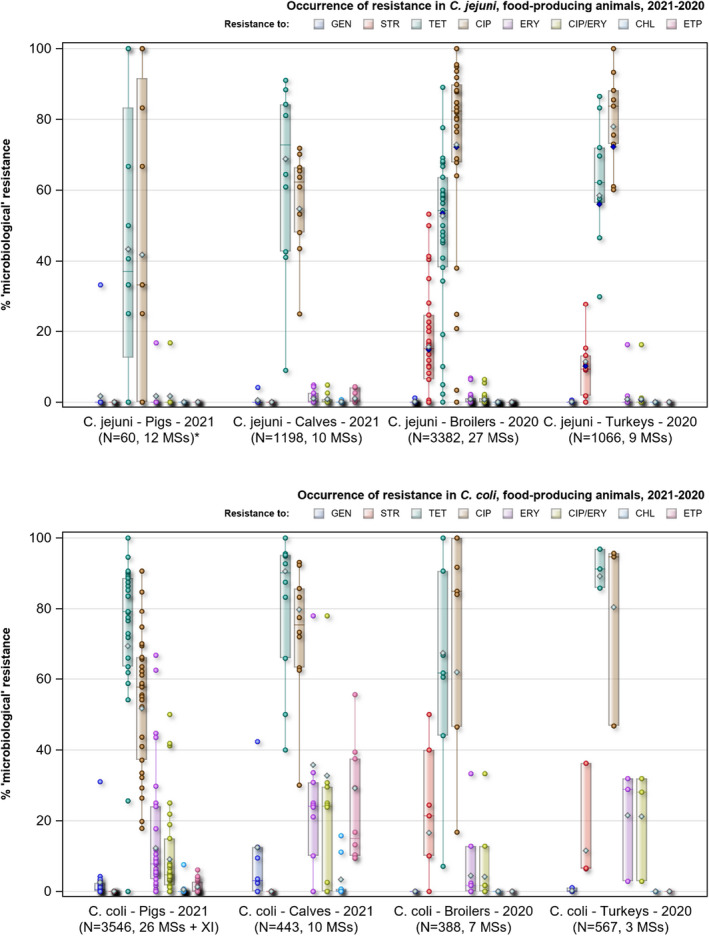
- GEN: gentamicin; STR: streptomycin; TET: tetracycline; CIP: ciprofloxacin; ERY: erythromycin; ETP: ertapenem CIP/ERY: combined ‘microbiological’ resistance to ciprofloxacin and erythromycin; N: Total number of isolates reported by all Member States (MSs); Horizontal line represents median; Light green diamond: resistance at reporting MS group level (excluding UK, 2020). Lower and upper box boundaries, 25th and 75th percentiles, line inside box median, diamond mean.
Based on the reported animal data, the level of resistance to tetracycline ranged from high to very high (43.3%–90.5%) in both C. jejuni and C. coli isolates from all the animal categories considered. The highest levels of resistance to tetracycline were observed in C. coli isolated from calves under 1 year of age (90.5%) in 2021 (data from 10 MSs) and from fattening turkeys (89.2%) in 2020 (data from three MSs). Overall, the levels of resistance to tetracycline were higher than those observed for the other selected antimicrobials in C. coli and C. jejuni isolates from calves and fattening pigs in 2021, and for C. coli isolated from poultry in 2020.
High levels of resistance were also observed to ciprofloxacin (range from 41.7% to 80.4%) and to nalidixic acid (range from 61.1% to 80.2%; data for 2020 only) in both C. jejuni and C. coli isolates. The highest levels of resistance to nalidixic acid and to ciprofloxacin were observed in C. coli isolated from fattening turkeys in 2020 (80.2% and 80.4%, respectively; data from three MSs). Likewise, a very high level of resistance to ciprofloxacin (79.7%) was obtained from C. coli isolated from calves in 2021. Overall, the levels of resistance to ciprofloxacin were higher for C. coli than for C. jejuni although the level of resistance to ciprofloxacin obtained from C. jejuni isolates from poultry in 2020 were also high (e.g. 77.9% in fattening turkeys, data from 9 MSs). The lowest levels of resistance to ciprofloxacin were in both C. jejuni and C. coli obtained from pig samples in 2021 (41.7% and 51.7%, respectively).
In relation to the levels of resistance to streptomycin, moderate overall levels (range from 11.4% to 16.5%) were reported for C. jejuni and C. coli from broilers and fattening turkeys in 2020. Due to recent changes in the legislation, no data in relation to this antimicrobial were reported for pigs and calves in 2021. However, high levels of resistance to streptomycin were reported in C. coli isolates from fattening pigs and calves in 2019 (overall, 70.0% and 65.7%, respectively).
Resistance to gentamicin in C. jejuni and C. coli isolates from broilers and fattening turkeys was either absent or extremely low in 2020 (0.0%–0.2%). In 2021, the overall levels of resistance to this antimicrobial for C. jejuni were 0.5% from calves and 1.7% from pig samples. Higher levels of resistance to gentamicin were observed in C. coli isolates from fattening pigs (2.6%) and especially from calves (12.4%) in 2021 (data from 10 MSs).
Resistance to erythromycin was detected at very low levels in C. jejuni isolates for the different animal categories (range from 0.8% to 1.7%). Notable higher levels of resistance were reported in C. coli isolates (range from 4.4% to 35.7%). The highest level of resistance to erythromycin was observed in C. coli isolates recovered from calves (35.7%), followed by fattening turkeys (21.5%), fattening pigs (12.3%) and broilers (4.4%).
Resistance to chloramphenicol in isolates from pigs and calves (2021) was either absent or extremely low in C. jejuni isolates from fattening pigs (0.0%) and calves (0.1%), and C. coli isolates from pigs (0.5%). A higher level resistance (but still low) to chloramphenicol was observed in C. coli isolated from calves (3.4%).
Resistance to ertapenem in isolates from pigs and calves (2021) was either absent or very low in C. jejuni isolates from fattening pigs (0.0%) and calves (1%), and C. coli from pigs (0.5%). It is noteworthy that a higher level of resistance to ertapenem was reported in C. coli isolated from calves (29.1%) in 2021 (see specific textbox on ‘further considerations on the occurrence of resistance to ertapenem in C. coli from calves’).
Further considerations on the detected levels of ertapenem resistance in C. coli from calves
No validated threshold for resistance to ertapenem has been recommended by EUCAST yet and no indication on the epidemiological cut‐off to be used for ertapenem in C. coli and C. jejuni was provided in Commission Implementing Decision (EU) 2020/1729.
An epidemiological cut‐off of 0.5 mg/L was used by EFSA as the threshold for resistance to ertapenem in both C. coli and C. jejuni isolates, in accordance with the critical concentrations indicated by the Société Française de Microbiologie in CA‐SFM 2018 (https://www.sfm-microbiologie.org/wp-content/uploads/2019/02/CASFM-V1_0-FEV_2018.pdf) and CA‐SFM 2019 (https://www.sfm-microbiologie.org/wp-content/uploads/2019/05/CASFM2019_V2.0_MAI.pdf). The choice of the epidemiological cut‐off has a direct impact on the threshold for considering an isolate as susceptible or resistant to a selected antimicrobial (as shown in the table below) and consequently on the interpretation of the results of the susceptibility testing.
Due to the lack of data, the epidemiological cut‐off used by EFSA in this analysis is still under discussion. Additional data will be available in the coming years because of the implementation of the harmonised AMR monitoring in accordance with Commission Implementing Decision (EU) 2020/1729 and these will allow a detailed evaluation and validation of the appropriate threshold for resistance to ETP in both C. coli and C. jejuni.
MIC distribution in ertapenem resistant and susceptible C. coli isolates from calves (ECOFF = 0.5 mg/L) reported in 2021 by 10 MSs.
| MIC | Number of isolates | % | ETP resistance |
|---|---|---|---|
| ≤ 0.125 | 133 | 30.0 | Susceptible |
| 0.25 | 78 | 17.6 | Susceptible |
| 0.5 | 103 | 23.2 | Susceptible |
| 1 | 103 | 23.2 | Resistant |
| 2 | 23 | 5.2 | Resistant |
| 4 | 3 | 0.7 | Resistant |
| Total | 443 |
At present, only few comparable data on the resistance to ertapenem in C. coli isolates from calves are available in the EU and further investigations are needed to interpret the unexpected level of ertapenem resistance (29.1%) reported in C. coli isolates from calves in 2021.
3.4.4. Combined resistance to ciprofloxacin and erythromycin
Macrolides such as erythromycin and fluoroquinolones such as ciprofloxacin are recognised as critically important antimicrobials (CIAs) for the treatment of Campylobacter infections in humans. Therefore, the occurrence of combined resistance to ciprofloxacin and erythromycin in Campylobacter spp. from food‐producing animals is of great importance to public health, since it might hamper the treatment of human campylobacteriosis (Friedrich, 2019; WHO, 2019).
Overall combined resistance to these antimicrobials was lower in C. jejuni isolates than in C. coli isolates for all animal species tested (Table 8; Figure 19). Very low levels of combined resistance to ciprofloxacin and erythromycin were reported in C. jejuni isolates from broilers (0.7%) and fattening turkeys (0.8%) in 2020 (Table 8; Figure 19; see also Annex B, Tables 22 and 24), and from calves (0.8%) and fattening pigs (1.7%) in 2021 (Table 8; Figure 19; see also Annex B, Tables 28 and 29). The highest levels of combined resistance were reported in C. coli isolates from calves (32.7%) in 2021 and from fattening turkeys (21.2%) in 2020, followed by fattening pigs (9.3%) in 2021 and broilers (4.1%) in 2020 (Table 8; Figure 19; see also Annex B, Tables 23, 25–27). The levels of combined resistance to ciprofloxacin and erythromycin observed in C. coli isolates from calves notably increased from 22.4% in 2019 to 32.7% in 2021. An increase was also observed in C. coli isolates from fattening pigs where the levels of combined resistance to ciprofloxacin and erythromycin increased from 8% in 2019 to 9.3% in 2021.
Combined resistance to ciprofloxacin and erythromycin in C. jejuni isolated from broilers was detected in seven MSs (Cyprus, Czechia, Italy, Lithuania, Portugal, Romania and Slovakia) out of 27 reporting data in 2020, ranging from 1.2% to 6.4%, with the highest level of combined resistance reported by Portugal (Figure 20a; Annex B, Table 22). Co‐resistance to ciprofloxacin and erythromycin detected in C. coli isolates from broilers was reported from four (Czechia, France, Latvia and the Netherlands) out of seven MSs reporting 2020 data. The levels of combined resistance ranged from 1.7% reported by the Netherlands to 33.3% reported by Latvia (Figure 21a; Annex B, Table 23). However, this last finding should be interpreted cautiously as only three C. coli isolates from broilers were reported by Latvia.
Figure 20.
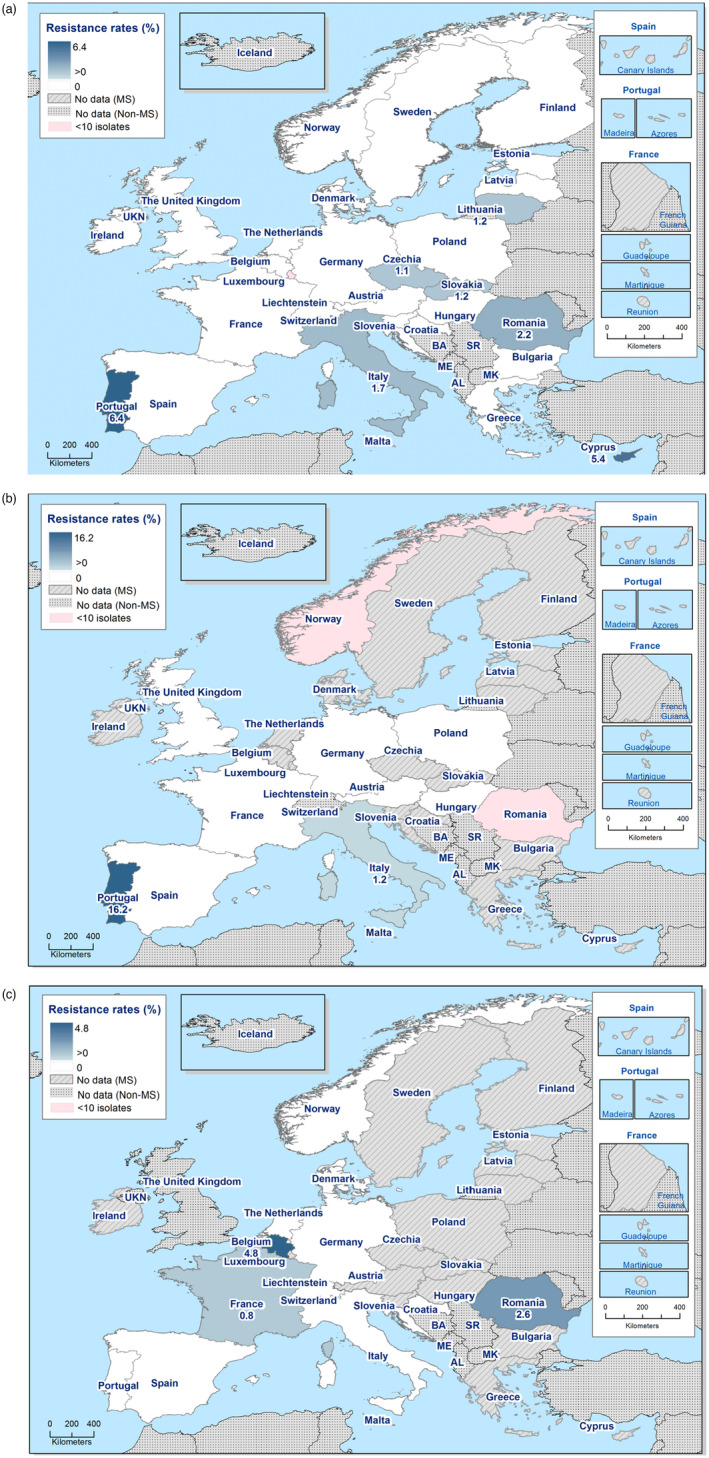
Spatial distribution of combined resistance to ciprofloxacin and erythromycin in Campylobacter jejuni isolates from (a) broilers (27 EU MSs and three non‐MSs, 2020); (b) fattening turkeys (nine EU MSs and two non‐MS, 2020); and (c) calves less than 1 year of age (10 EU MSs and two non‐MSs, 2021)
Figure 21.
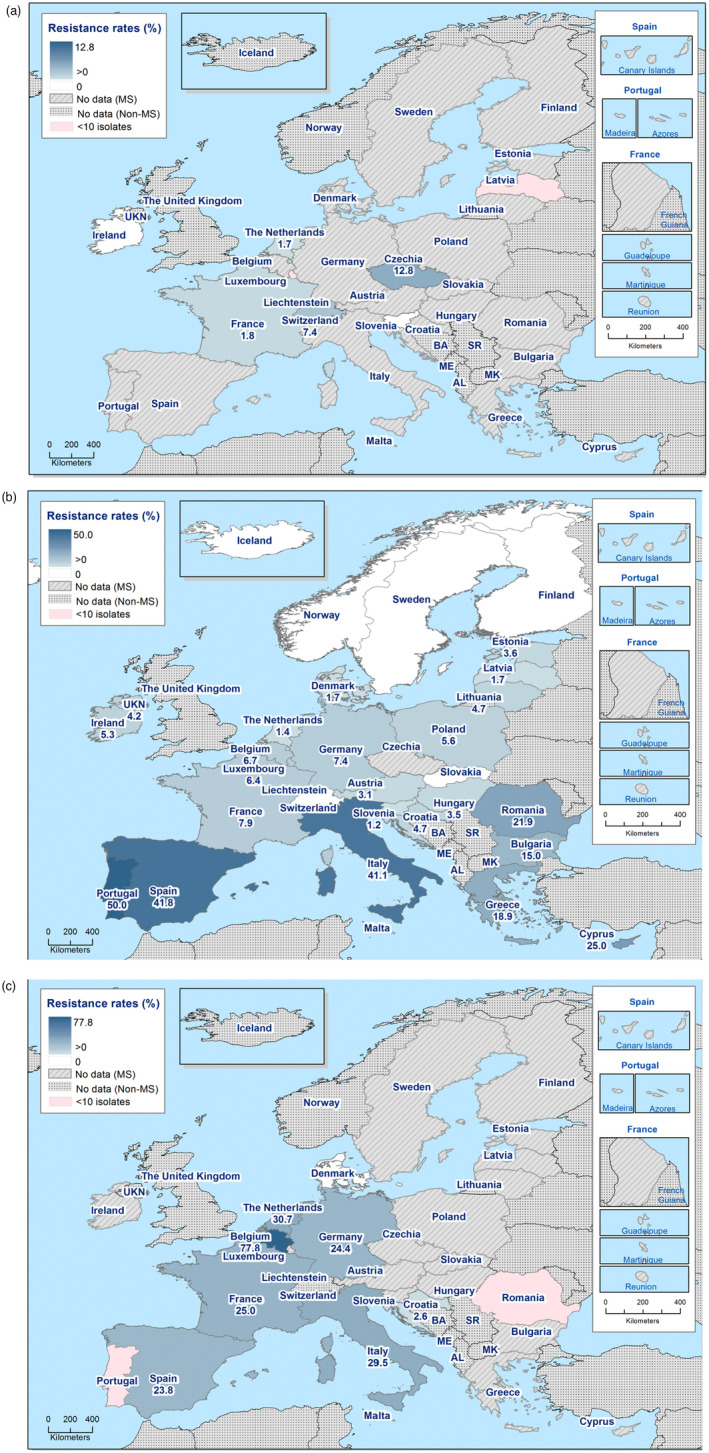
Spatial distribution of combined resistance to ciprofloxacin and erythromycin in Campylobacter coli isolates from (a) broilers (seven EU MSs and one non‐MS, 2020); (b) fattening pigs (26 EU MSs plus United Kingdom (Northern Ireland) and three non‐MSs, 2021) and (c) calves less than 1 year of age (10 EU MSs, 2021)
Combined resistance to ciprofloxacin and erythromycin in C. jejuni from fattening turkeys was detected only in Italy (1.2%) and Portugal (16.2%), out of nine reporting MSs in 2020 (Figure 20b; Annex B, Table 24). Data on combined resistance to ciprofloxacin and erythromycin in C. coli isolates from fattening turkeys in 2020 were reported by three MSs (France, Germany and Spain) with levels of co‐resistance ranging from 2.9% in France, up to 28.2% and 31.9% in Germany and Spain, respectively (see Annex B, Table 25).
Data on combined resistance to ciprofloxacin and erythromycin in C. jejuni isolated from fattening pigs were reported by 12 MSs (Bulgaria, Cyprus, Denmark, Germany, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, the Netherlands and Portugal) and Norway in 2021 (Annex B, Table 29). However, only one country (Lithuania) reported co‐resistance in 16.7% of pig isolates (N = 6) in 2021. These findings should be interpreted cautiously as only very few isolates were reported by each country (ranging from one to six isolates per country, except for Malta who reported 27 isolates). In 2021, combined resistance to ciprofloxacin and erythromycin in C. coli isolated from fattening pigs was detected in 26 MSs (all except Czechia), the United Kingdom (Northern Ireland) and three non‐EU countries (Iceland, Norway and Switzerland) (Figure 21b; Annex B, Table 26). All MSs reported combined resistance to these antimicrobials, except Finland, Malta, Slovakia and Sweden. The combined resistance levels ranged from 1.2% reported by Slovenia to 50% reported by Portugal in C. coli isolated in 2021. No combined resistance in C. coli isolated from fattening pigs was reported by the three non‐MSs who submitted data.
Data on combined resistance to both ciprofloxacin and erythromycin in C. jejuni isolated from calves under 1 year of age were reported by 10 MSs (Belgium, Croatia, Denmark, France, Germany, Italy, the Netherlands, Portugal, Romania and Spain) and two non‐EU countries (Norway and Switzerland) in 2021 (Figure 20c; Annex B, Table 28). Three out of the reporting countries found combined resistance to these antimicrobials with the following levels: 0.8% reported by France, 2.6% reported by Romania and 4.8% reported by Belgium. Data on combined resistance to ciprofloxacin and erythromycin in C. coli isolated from calves were reported by 10 MSs (Belgium, Croatia, Denmark, France, Germany, Italy, the Netherlands, Portugal, Romania and Spain) in 2021 (Figure 21c; Annex B, Table 27). Seven MSs reported combined resistance to both antimicrobials in C. coli isolates. The combined resistance levels in C. coli isolated from calves in 2021 ranged from 2.6% reported by Croatia to 77.8% reported by Belgium. No co‐resistant C. coli isolates from calves were reported by Denmark, Portugal and Romania.
The combined resistance to ciprofloxacin and erythromycin obtained from calves and pigs tested in 2021 is higher than those reported from these animal species in 2019. This observation is particularly relevant in C. coli isolated from calves and pigs in 2021 and could be partly explained by the higher number of reporting countries and isolates in 2021 (due to sampling frequency and changes in legislative requirement based on Commission Implementing Decision (EU) 2020/1729). The levels of resistance to erythromycin in C. coli isolates from calves increased from 21.5% in 2019 to 35.7% in 2021 and the levels of combined resistance to ciprofloxacin and erythromycin increased from 22.4% in 2019 to 32.7% in 2021 in C. coli isolates from calves, which might infer a public health concern.
The spatial distribution of combined resistance to both ciprofloxacin and erythromycin in C. jejuni and C. coli isolates from different animal categories is presented in Figures 20 and 21. Detailed data on combined resistance to ciprofloxacin and erythromycin in C. jejuni and C. coli isolates from food‐producing animals are presented in Annex B (Tables 22–29).
3.4.5. Prevalence of antimicrobial resistance in Campylobacter coli from fattening pigs
The prevalence of resistance to selected antimicrobials in C. coli from fattening pigs has been estimated at country level as the proportion of C. coli showing microbiological resistance to each selected antimicrobial as a percentage of all caecal samples cultured for C. coli. This prevalence of resistance is the product of the prevalence of C. coli in caecal samples from fattening pigs (Annex B, Table 20) and the occurrence of resistance in the C. coli isolates tested for susceptibility (Annex B, Table 12). Monitoring the prevalence of resistant C. coli in fattening pigs enables to address together both evolving temporal trends in the prevalence of C. coli in fattening pigs and in the occurrence of resistance in C. coli from fattening pigs, through a unique indicator. This indicator is primarily intended to follow up trends over time at the country level. The country‐level estimates of the prevalence resistance to selected antimicrobials in C. coli from caecal samples of fattening pigs are presented in Table 21 of Annex B.
The isolation method for Campylobacter has been now harmonised across the EU in accordance to the protocol of the EURL for Campylobacter (https://www.sva.se/en/about-us/eurl-campylobacter/). Therefore, the prevalence of C. coli in fattening pigs can be considered comparable between reporting countries. Similarly, the harmonised implementation of the antimicrobial susceptibility testing in C. jejuni and C. coli isolates allows comparability of the estimates of prevalence of resistance in C. coli from fattening pigs across the EU.
Although the sampling design for the monitoring of antimicrobial resistance in C. coli from fattening pigs is harmonised according to the Commission Implementing Decision 2020/1729, still differences in the intensity of sampling effort exist across the EU MSs, as shown in the numbers of tested samples included in Tables 20 and 21 of Annex B. To account for between‐country variation in the intensity of sampling effort, 95% confidence intervals have been calculated together with the estimated point prevalence of resistance as presented in Table 21 of Annex B, as well as in Figure 22a–c. It is to be noted that, according to Commission Implementing Decision (EU) 2020/1729, MSs having an annual national production less than 100,000 tonnes of pig meat are allowed, by derogation, to collect less samples (i.e. 150 instead of 300). Still, small countries may have difficulties to reach the minimum number of samples foreseen by derogation in the decision, due to the limited swine production.
Figure 22.
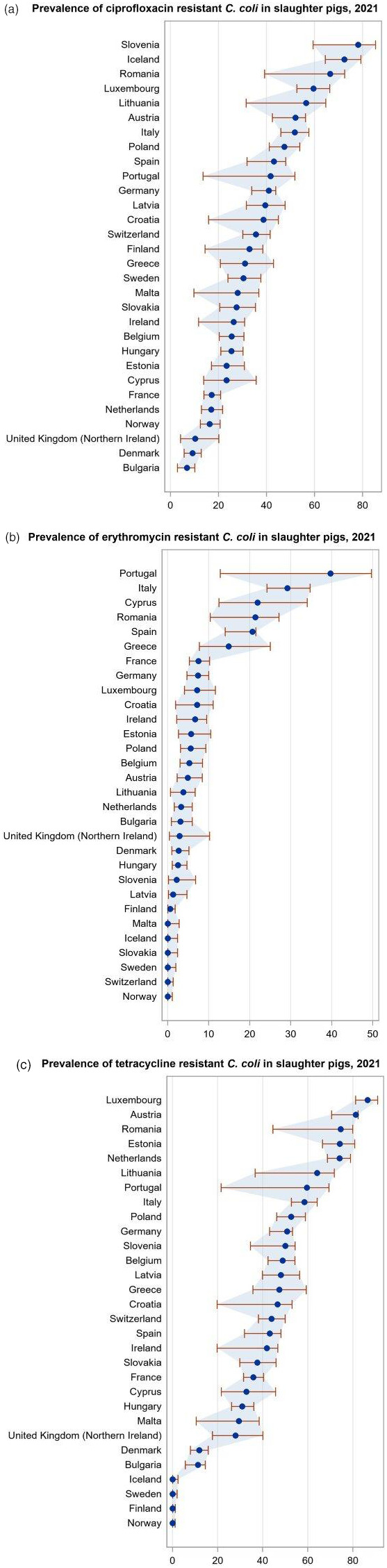
Prevalence of resistances to ciprofloxacin (a), erythromycin (b), tetracycline (c) and related 95% confidence intervals in C. coli from fattening pigs, per reporting country, 2021
The country‐level prevalence of resistance to ciprofloxacin, erythromycin and tetracycline in C. coli isolates from fattening pigs is presented in Figure 22, together with the 95% confidence intervals that provide an indication of the uncertainty around the point prevalence estimates. Between‐country variability from low to extremely high levels was observed in the prevalence of ciprofloxacin resistant (ranging from 6.9% to 78.2%; Figure 22a) and tetracycline resistant (ranging from 0.0% to 86.5%; Figure 22c) C. coli from fattening pigs. Interestingly, a limited between‐country variation and notably lower levels of prevalence of resistance to erythromycin were found in C. coli from fattening pigs, which have been estimated to be below 10% for 24 reporting countries (21 MSs and 3 non‐MSs), while ranging from 14.9% to 39.7% in the remaining six reporting MSs (Figure 22b). Noteworthy, the MS (Portugal) with the highest prevalence of resistance to erythromycin in C. coli from fattening pigs (39.7%) in 2021 had also the highest levels of erythromycin resistance (55.3%) and combined resistance to ciprofloxacin and erythromycin (55.3%) in C. coli from humans. It is also interesting to note that almost all the erythromycin‐resistant isolates (19 out of the 20 erythromycin‐resistant isolates) reported by Portugal, had very high MIC (≥ 256 mg/L).
3.4.6. Complete susceptibility and multidrug resistance
The observed overall complete susceptibility to the four antimicrobial classes (represented by susceptibility to ciprofloxacin/nalidixic acid, erythromycin, tetracycline and gentamicin) ranged from 4.4% in C. coli isolates from fattening turkeys to 48.3% in C. jejuni isolates from fattening pigs. Overall, the observed complete susceptibility was higher in C. jejuni than in C. coli isolates. The highest levels of complete susceptibility were observed from C. jejuni isolates from fattening pigs (48.3%), followed by broilers (23%), calves (21.6%) and fattening turkeys (16.8%). With regard to C. coli, the overall complete susceptibility observed was low for isolates from fattening turkeys (4.4%) in 2020 and calves (6.3%) in 2021, while it was higher for broilers (13.7%) in 2020 and pigs (19.9%) in 2021.
It is interesting to note that the overall complete susceptibility observed in C. coli from calves was higher (6.3%) in 2021 than the complete susceptibility reported in 2019 (1.5%).
Variability in the levels of complete susceptibility was detected between countries (Annex B, Tables 22–29). For example, overall complete susceptibility in C. jejuni isolated from broilers ranged from less than 5% in Greece, Latvia, Poland and Portugal to more than 75% in Finland, Sweden and Norway. Malta reported 100% of complete susceptibility in C. jejuni isolated from broilers, although from only two isolates. When interpreting the results, it is therefore important to account for the between country differences in the number of isolated reported (sample size).
The CS to the selected antimicrobial classes and the levels of MDR (defined as resistance to at least three antimicrobials among the four included in the harmonised panel tested: gentamicin, ciprofloxacin, erythromycin, tetracycline) among Campylobacter isolates recovered from these food‐producing animals by EU MSs are displayed in Figure 23.
Figure 23.
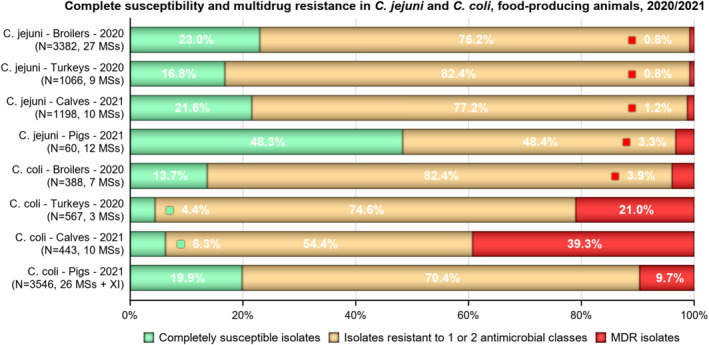
- N: Total number of isolates reported by the EU MSs. Complete susceptibility is defined as susceptibility to ciprofloxacin/nalidixic acid, erythromycin, gentamicin and tetracycline. MDR (multidrug resistance) is defined as resistance to at least three antimicrobial classes (including: GEN: gentamicin; CIP: ciprofloxacin; ERY: erythromycin; TET: tetracycline).
Overall, the levels of MDR observed were lower in C. jejuni than in C. coli isolates. MDR was observed at low levels in C. jejuni isolates from broilers and fattening turkeys (0.8%) in 2020, and from calves (1.2%) and pigs (3.3%) in 2021. The highest levels of MDR were reported in C. coli isolates from calves (39.3%), followed by fattening turkeys (21.0%) and fattening pigs (9.7%). A lower level of MDR was observed in C. coli isolates from broilers (3.9%) compared with the other monitored animal categories. Moreover, it is relevant to note that the MDR levels observed in pigs and calves (under 1 year of age) in 2021 were higher than the corresponding levels reported in 2019, particularly for isolates recovered from calves.
Detailed data on complete susceptibility and MDR in C. jejuni and C. coli isolates from different animal categories are presented in Annex B (Tables 22–29).
3.4.7. Temporal trends in resistance
Temporal trends in resistance in C. coli from pigs
Temporal trends showing resistance to selected antimicrobials in C. coli isolates from fattening pigs, for the period 2009–2021, are shown in Figure 24 and Table 9 (see also in Annex B, Table 30). Trends of resistance to selected antimicrobials in C. coli from fattening pigs were evaluated considering data from six MSs and two non‐MSs who reported at least three data points in the recent years and a minimum of 10 isolates per year. Countries reporting data with more than 1‐year gap over the period 2016–2020 were excluded from the trend analysis. Overall, seven MSs (Croatia, Denmark, Finland, France, Hungary, Luxembourg and Slovenia) were excluded from the trend analysis, because of the gap in reporting history (two or more missing data points over 2016–2021). A significant increasing trend of resistance to ciprofloxacin was observed in four countries (Germany, the Netherlands, Norway and Switzerland). No significantly increasing trend of resistance to erythromycin was observed in the reporting countries, while a significantly decreasing trend of resistance to erythromycin was found in Czechia, the Netherlands, Spain and Switzerland. A significantly increasing trend of resistance to tetracycline was observed in Estonia and Switzerland, while the results indicated significantly decreasing resistance in the Netherlands and Spain.
Figure 24.
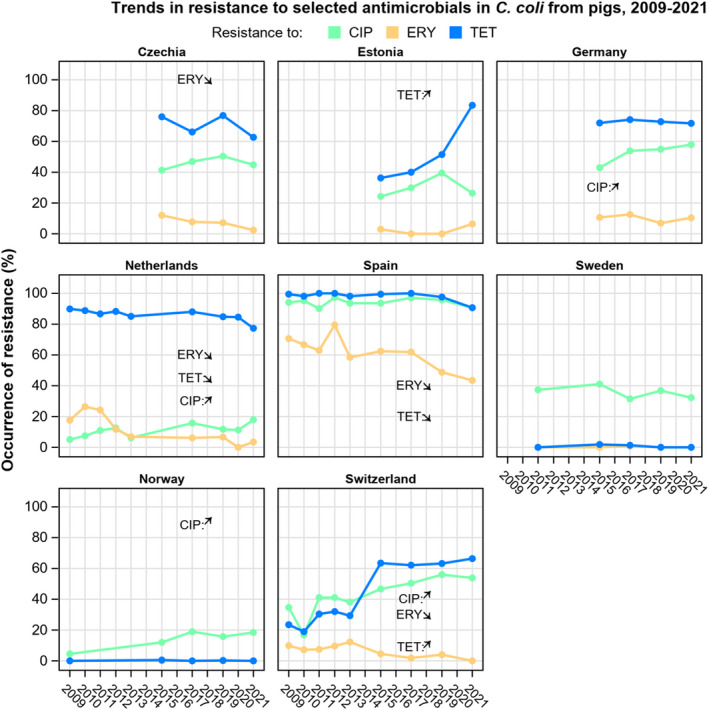
- CIP: ciprofloxacin; ERY: erythromycin; TET: tetracycline. Arrows indicate significant increasing (up) or decreasing (down) trend over the entire period. *The trend analysis was performed for different periods depending on the data availability. Czechia, Estonia, Germany and Sweden: the trend analysis was performed for the reporting period 2015–2021. The Netherlands, Spain, Norway and Switzerland: The trend analysis was performed for the reporting period 2009–2021.
Table 9.
Number of countries with significantly increasing or decreasing trends in resistance to selected antimicrobials for C. jejuni and C. coli from humans, 2013–2021, broilers, 2009–2020, fattening turkeys, 2014–2020 and pigs, 2009–2021
| Origin | Campylobacter species | Ciprofloxacin | Erythromycin | Tetracycline | |||
|---|---|---|---|---|---|---|---|
| Increase | Decrease | Increase | Decrease | Increase | Decrease | ||
| Humans | C. jejuni (19 MS + 3 non‐MS) | 12 (AT, BG, DK, EE, FR, LT, MT, NL, PL, SI, SK, UK) | 3 (NO, PT, FI) | 1 (ES) | 7 (DK, FI, IT, MT, NO, SI, UK) | 7 (AT, DK, EE, NL, SI, SK, UK) | 5 (ES, FI, FR, LT, NO) |
| C. coli (14 MSs + 1 non‐MS) | 3 (NL, SI, SK) | 2 (FR, UK) | 1 (UK) | 5 (EE, ES, FR, MT, SK) | 4 (FR, NL, SI, SK) | – | |
| Broilers | C. jejuni (24 MSs + 4 non‐MSs) | 14 (AT, DE, HR, CY, CZ, DK, FI, FR, NL, RO, SE, SK, CH, UK) | 1 (ES) | – | 5 (BG, NL, RO, SK, ES) | 12 (AT, HR, CZ, DK, DE, IE, LT, SK, SE, CH, UK) | 7 (BG, CY, FI, EL, IT, LV, ES) |
| C. coli (4 MSs + 1 non‐MS) | 2 (DE, NL) | – | 1 (CZ) | 1 (NL) | 3 (CZ, DE, CH) | – | |
| Turkeys | C. jejuni (8 MSs + 1 non‐MS) | 2 (DE, PL) | 2 (HU, IT) | – | 3 (DE, PL, ES) | 1 (HU) | 4 (DE, ES, FR, UK) |
| Pigs | C. coli (6 MSs + 2 non‐MSs) | 4 (DE, NL, CH, NO) | – | – | 4 (CZ, ES, NL, CH) | 2 (EE, CH) | 2 (ES, NL) |
MSs: Member States; AT: Austria; BE: Belgium; BG: Bulgaria; CY: Cyprus; CZ: Czechia; DE: Germany; DK: Denmark; EE: Estonia; EL: Greece; ES: Spain; FI: Finland; HU: Hungary; FR: France; IS: Iceland; IT: Italy; LU: Luxembourg; LV: Latvia; MT: Malta; NL: Netherlands; NO: Norway; PL: Poland; PT: Portugal; RO: Romania; SE: Sweden; SI: Slovenia; SK: Slovakia; UK: United Kingdom.
Temporal trends in resistance in C. jejuni and C. coli from broilers
The results from the analysis of temporal trends in resistance of C. jejuni isolated from broilers over the period 2009–2020 were obtained using data from 24 reporting MSs and 4 non‐MSs (Table 9; see also Annex B, Figure 1a and Table 30). Evaluation of temporal trends in resistance was performed for countries reporting data for at least 3 years (three data points). Countries reporting data with more than 1‐year gap over the period 2016–2020 were excluded from the trend analysis. Moreover, countries that reported only AMR data for years before 2015 were excluded from the analysis because the evaluation of the trend would not be representative of the current AMR situation. It is relevant to notice that between‐year oscillations in the occurrence resistance (%) may not be captured in the evaluation of the trend for the entire period (2009–2020) and that very recent decreasing or increasing trends may therefore be masked by the overall trend.
The analysis of temporal trends in resistance to ciprofloxacin in C. jejuni indicated that, over the period 2009–2020, a significant increase was reported in 12 MSs (Austria, Croatia, Cyprus, Czechia, Denmark, Finland, France, Germany, the Netherlands, Romania, Slovakia and Sweden) and two non‐MSs (Switzerland and the United Kingdom). On the other hand, a significant decrease in resistance to ciprofloxacin in C. jejuni was detected in Spain. A significant decrease in resistance to erythromycin was detected in five MSs (Bulgaria, the Netherlands, Romania, Slovakia and Spain), while a significant decrease in resistance to tetracycline was seen in seven MSs (Bulgaria, Cyprus, Finland, Greece, Italy, Latvia and Spain). Interestingly, a significant increase in resistance was detected for tetracycline in 10 MSs (Austria, Croatia, Czechia, Denmark, Germany, Hungary, Ireland, Lithuania, Slovakia and Sweden) and two non‐MSs (Switzerland and the United Kingdom).
The results from the analysis of temporal trends in resistance of C. coli isolated from broilers over the period 2009–2020 were obtained using data from four reporting MSs (Czechia, Germany, the Netherlands, Slovenia) and one non‐MS (Switzerland) (Table 9; see also Annex B, Figure 1b and Table 30). Temporal trends showed significant increases of resistance in C. coli isolated from broilers for ciprofloxacin (Germany, the Netherlands), erythromycin (Czechia) and tetracycline (Czechia, Netherlands, Switzerland). On the other hand, significant decreases were observed for erythromycin only in one MS (the Netherlands).
When interpreting the results, it is important to note that trend analyses may be driven by particularly high or low levels of resistance reported in one or few data points leading to unexpected findings (e.g. detection of significant increasing or decreasing trends where the observed data do not seem to show any clear trend over the entire period). This is the case, for example, of the detected significant increasing trend of resistance to ciprofloxacin in C. jejuni from broilers detected for Finland and of the increasing trend of resistance to tetracycline detected for Sweden (Annex B, Figure 1). For details on the methodology applied for trend analysis, see Appendix F – Materials and methods.
Temporal trends in resistance in C. jejuni from turkeys
Temporal trends of resistance to selected antimicrobials in C. jejuni isolates from fattening turkeys during the period of 2014–2020 are displayed in Figure 2 in Annex B (see also Table 30) and in Table 9. Evaluation of temporal trends in resistance could be performed for countries reporting data for at least 3 years (three data points). It is relevant to note that between‐year oscillations in the occurrence resistance may not be captured in the evaluation of the trend for the entire period (2014–2020) and that very recent decreasing or increasing trends may therefore be masked by the overall trend. Moreover, the results of these trends are based on very few data points, and therefore, more data and further analyses will be needed in the future for a more robust evaluation.
The results from the analysis of temporal trends in resistance of C. jejuni isolated from fattening turkeys over the period 2014–2020 were obtained using data from eight reporting MSs (Austria, France, Germany, Hungary, Italy, Poland, Portugal and Spain) and one non‐MS (the United Kingdom) (Table 9, see Annex B, Figure 2 and Table 30). Temporal trends showed significant increases of resistance in C. jejuni isolated from fattening turkeys for ciprofloxacin in two MSs (Germany and Poland) and tetracycline in one MS (Hungary). No significant increase to erythromycin was detected. On the other hand, significant decreases were observed for ciprofloxacin in two MSs (Hungary and Italy), for erythromycin in three MSs (Germany, Poland and Spain) and for tetracycline in three MSs (France, Germany, Spain) and one non‐MS (the United Kingdom).
Temporal trends in resistance in Campylobacter isolates from calves
Due to the scarcity of comparable historical data on C. jejuni and C. coli from calves (under 1 year of age), the temporal trends of resistance to selected antimicrobials was not analysed for this animal population. Comparable data will be available in the coming years thanks to the implementation of the monitoring requirements laid down in Commission Implementing Decision (EU) 2020/1729.
3.4.8. High‐level resistance to erythromycin
High‐level resistance to macrolides, streptogramin B and/or lincosamides in Campylobacter may be associated with the erm(B) gene encoding an rRNA methylase, as firstly described in a C. coli isolated from a swine in China (Qin et al., 2014). The erm(B) gene can be transferred by natural transformation between strains of Campylobacter (Wang et al., 2014). Erm(B) is detected more frequently in C. coli than in C. jejuni, but it may also be found on C. jejuni from poultry resistant to all clinically important antimicrobial agents (Liu et al., 2019). In Europe, erm(B) has been reported in C. coli from broilers and turkeys in Spain and from a broiler isolate in Belgium (Florez‐Cuadrado et al., 2018; Elhadidy et al., 2019; Mourkas et al., 2019). It was also detected in Australia, in faecal samples from two travellers returning from Southeast Asia (Wallace et al., 2020) and in patients in France (Jehanne et al., 2021). Importantly, in Campylobacter, the erm(B) gene is carried on plasmids, or more frequently on multidrug resistance islands (MDRI) which often contain genes coding for resistances to other families such as tetracycline and aminoglycosides (Florez‐Cuadrado et al., 2017). Another methylase, Erm(N) was recently described in human C. coli strains isolated in Canada (Greninger et al., 2020) and in France (Jehanne et al., 2021). The presence of transferable resistance genes, on either MDRI or plasmids in Campylobacter, represents a significant hazard, as acquisition of such genetic structures will confer multidrug resistance to isolates, which can be co‐selected and lead to therapeutic problems. Therefore, because erm(B) is more frequently reported among C. coli rather than C. jejuni in many published studies and to better detect the emergence of erm(B) in Campylobacter, it was decided the inclusion of C. coli in the monitoring programmes from 2021 onward (EFSA, 2019, Commission Implementing Decision (EU) 2020/1729). An increase of the tested concentrations of erythromycin (up to 512 mg/L instead of 128 mg/L) has been also implemented since 2021 according to Commission Implementing Decision (EU) 2020/1729. This amendment lead to a better screening of isolates which may carry erm(B), as it enables to differentiate erythromycin‐resistant isolates with an MIC < 128 mg/L, which have probably only mutations or alterations in target genes (L4, L22 CmeABC, CmeR genes and the binding site of CmeR) from those with a higher MIC (≥ 512 mg/L) that most likely have an erythromycin resistance phenotype consistent with either possession of transferable erm(B) or mutational resistance (Wang et al., 2014). Point mutations in 23SrRNA might also confer similar levels of high resistance against erythromycin as ermB‐mediated resistance in Campylobacter (Wei and Kang, 2018; Béjaoui et al., 2022).
The distribution of MIC values related to erythromycin resistance in Campylobacter spp. recovered from caecal samples of food‐producing animals following legislative requirements in 2020 and 2021 are shown in Figure 25. It is interesting to note that even though MIC values were reported at low and moderate levels (ECOFF ≤ 4 mg/L), several isolates displayed high MIC, particularly in C. coli isolates from fattening turkeys (2020 data) and calves (2021 data).
Figure 25.
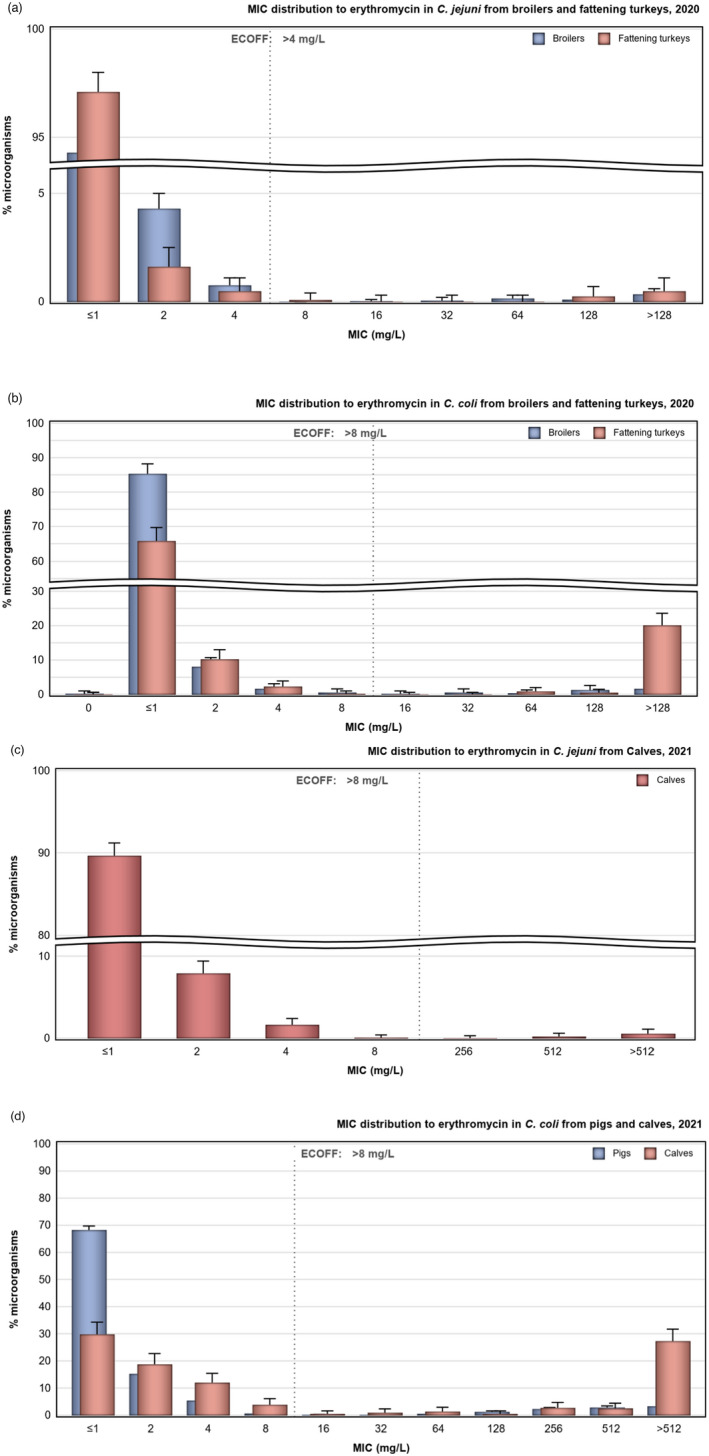
Distribution of MIC values related to erythromycin resistance in (a) C. jejuni from broilers and fattening turkeys, (b) C. coli from broilers and fattening turkeys, (c) C. jejuni from calves and (d) C. coli from fattening pigs and calves, in reporting EU MSs and non‐EU MSs, 2020 and 2021
Figure 26 (see also Annex B, Table 31) show data in relation to the erythromycin‐resistant isolates reported by MSs and non‐MSs displaying resistance below or equal to 128 mg/L (based on ecoff values for C. jejuni: MIC > 4 mg/L and for C. coli: MIC > 8 mg/L) in comparison to those displaying high‐level erythromycin resistance (MIC > 128 mg/L for 2020 data; 128 mg/L < MIC ≤ 512 mg/L and MIC > 512 mg/L for 2021 data) within each of the animal categories. As shown in Figure 26, a notable proportion of erythromycin‐resistant isolates displayed high MIC values (MIC > 128 mg/L for 2020 data; MIC > 512 mg/L for 2021 data) in both Campylobacter species, particularly in C. coli isolated from fattening turkeys (93.4% of isolates with MIC > 128 mg/L), fattening pigs (49.1% of isolates with MIC between 128 and 512 mg/L; 31.7% of isolates with MIC > 512 mg/L) and calves (25% of isolates with MIC between 128 and 512 mg/L; 66.7% of isolates with MIC > 512 mg/L). A very high level of erythromycin resistance was also observed in C. jejuni erythromycin‐resistant isolates from calves, although it is to be noted that only few C. jejuni isolates from calves (12) were resistant to erythromycin.
Figure 26.
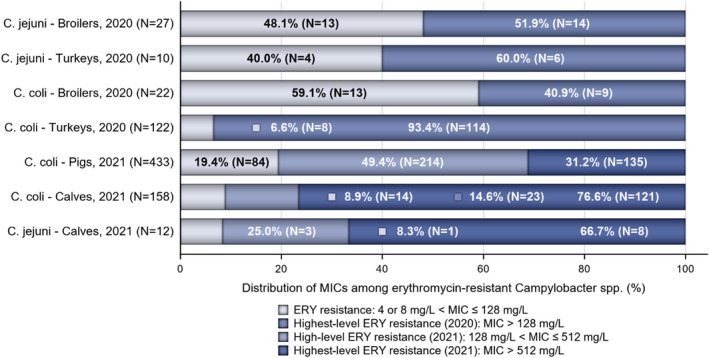
- N: Total number of C. jejuni or C. coli isolates exhibiting erythromycin resistance. ERY: erythromycin. ERY resistance in C. jejuni isolates: 4 mg/L < MIC ≤ 128 mg/L. ERY resistance in C. coli isolates: 8 mg/L < MIC ≤ 128 mg/L. For 2021 data, it is possible to discriminate between ERY‐resistant C. coli and C. jejuni isolates with MIC ranging from 128 mg/L to (equal) 512 mg/L and those with MIC above 512 mg/L.
Most high‐level erythromycin‐resistant C. jejuni isolates (MIC > 128 mg/L) from broilers were obtained from samples in Romania (seven isolates) and Cyprus (four isolates). Four of the six erythromycin high‐level resistant C. jejuni isolates from fattening turkeys were detected in Portugal, and nine of the 18 high‐level erythromycin‐resistant C. coli isolates from broilers were reported by Germany, followed by France and Switzerland (four isolates each), and the Netherlands (one isolate) in 2020. In 2021, a very high level of erythromycin resistance (MIC > 512 mg/L) was obtained in several C. coli isolates from calves reported by Belgium (54 isolates) and the Netherlands (42 isolates), followed by Italy and Germany (9 isolates each) and France (6 isolates). Several countries reported high‐level resistant isolates among the erythromycin‐resistant C. coli from fattening pigs obtained in 2021. The largest number of very high‐level resistant isolates (MIC > 512 mg/L) was reported by Germany (21 isolates), Spain (20 isolates) and Italy (18 isolates), followed by Romania (13 isolates), Ireland and Portugal (9 isolates each). Several additional countries (Austria, Belgium, Bulgaria, Croatia, Cyprus, Denmark, France, Greece, Hungary, Luxembourg, the Netherlands and Poland) reported less than 9 very high‐level resistant C. coli isolates from fattening pigs.
3.5. Comparison of human and animal data on Campylobacter spp.
In 2020–2021, quantitative human data were interpreted using EUCAST ECOFF values, where available, in the same way as for the animal and food data. Figure 27 illustrates the CBPs and ECOFFs used to interpret the MIC data reported for Campylobacter spp. from humans, animals and/or food. In the absence of CBPs from EUCAST (i.e. gentamicin), CBPs from the French Society for Microbiology (SFM) were applied (CASFM/EUCAST, 2020). For qualitative data interpreted with clinical breakpoints (S = susceptible, I = susceptible with increased exposure and R=resistant), I+R results were combined into one category. It can be observed that there is agreement across interpretive categories, with the exception of the EUCAST CBP for tetracycline in C. jejuni which is one dilution above the EUCAST ECOFF. For gentamicin, EUCAST lowered the ECOFF, in 2020, by one dilution compared to the ECOFF value listed in the Commission Implementing Decision (EU) 2020/1729 but then changed it back in 2022. For the comparison of 2021 data, the gentamicin criteria applied are thus the same for data from humans and animals.
Figure 27.
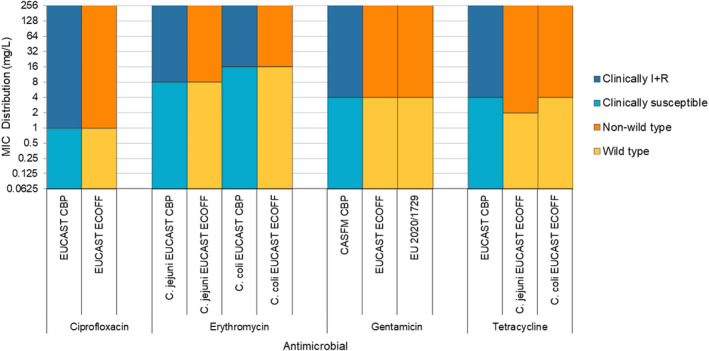
Comparison of clinical breakpoints (CBPs) and epidemiological cut‐off values (ECOFFs) used to interpret MIC data reported for Campylobacter spp. from humans, animals or food
The comparison of occurrence of resistance to selected antimicrobials and combined resistance to erythromycin and ciprofloxacin in C. jejuni and C. coli isolates between humans and food‐producing animals is presented in Figures 28 and 29, respectively.
Figure 28.
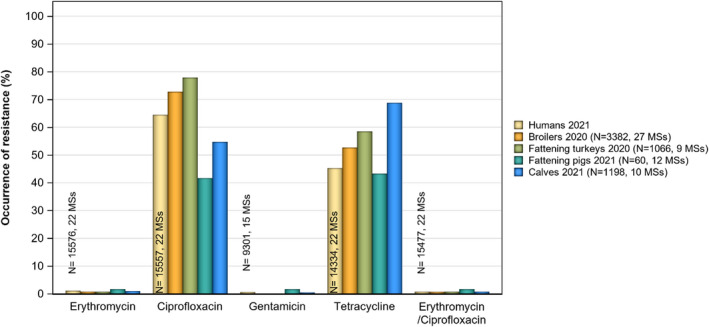
Comparison of C. jejuni occurrence of resistance between humans and animals
Figure 29.
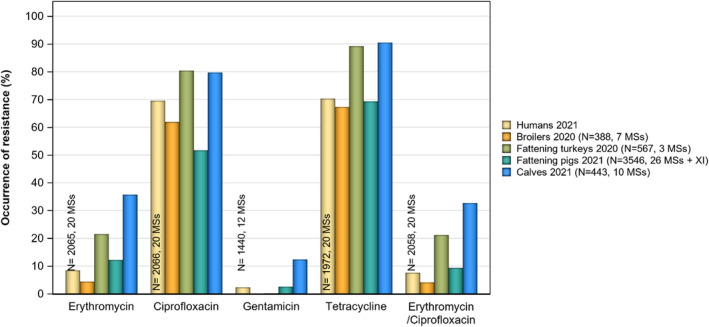
Comparison of C. coli occurrence of resistance between humans and animals
Human data submitted from MSs revealed that resistance to ciprofloxacin among C. jejuni isolates reported in 2020–2021 was detected in 61.2% (2020, 16 MSs) and in 64.5% (2021, 22 MSs) of human isolates. Similar levels of resistance to ciprofloxacin among C. coli isolates from humans were reported: 65.8% (2020, 15 MSs) and 69.6% (2021, 20 MSs). The levels of resistance to ciprofloxacin in food‐producing animals were estimated to be high to extremely high, ranging from 41.7% to 80.4%. The highest levels of resistance to ciprofloxacin were observed in C. coli isolated from fattening turkeys in 2020 (80.4%). Likewise, an extremely high level of resistance to ciprofloxacin (79.7%) was obtained from C. coli isolated from calves in 2021 and from broilers (61.9%) in 2020. Overall, the levels of resistance to ciprofloxacin were higher for C. coli than for C. jejuni, although the level of resistance to ciprofloxacin obtained from C. jejuni isolates from poultry in 2020 were also extremely high: 77.9% in fattening turkeys (data from 9 MSs) and 72.8% in broilers (data from 27 MSs). The lowest levels of resistance to ciprofloxacin were obtained from pig samples. The levels of resistance to ciprofloxacin among C. jejuni from human isolates and poultry isolates can be considered similar.
Overall resistance to erythromycin was reported at very low levels for C. jejuni (range from 0.8% to 1.7%) isolated from food‐producing animals. Similarly, overall resistance to erythromycin in human C. jejuni isolates was reported at 0.7% (2020) and 1.1% (2021). However, higher levels of resistance were observed in C. coli isolates from humans in 2021 (8.5%) and food‐producing animals (range from 4.4% to 35.7%). Overall, erythromycin resistance among animals was observed at the highest levels in C. coli isolates recovered from calves (35.7%, data from 2021), followed by fattening turkeys (21.5%, data from 2020), fattening pigs (12.3%, data from 2021) and broilers (overall, 4.4%, data from 2020).
Overall resistance to gentamicin was detected very low to low levels for C. jejuni (range from 0.1% to 1.7%) isolated from food‐producing animals. Similarly, overall resistance to gentamicin in human C. jejuni isolates was reported at 0.3% (2020) and 0.7% (2021). Higher levels of resistance to gentamicin were reported in C. coli isolates from humans and in fattening pigs and calves.
The overall levels of resistance to tetracycline were high to very high in C. jejuni isolates from both humans (43.7% in 2020 and 45.3% in 2021) and food‐producing animals (ranging from 43.3% in isolates from fattening pigs to 68.8% in isolates from calves in 2021). Very high to extremely high levels of resistance to tetracycline were detected in C. coli isolates from humans (74.0% in 2020 and 70.3% in 2021) and food‐producing animals (ranging from 67.3% in isolates from broilers in 2020 to 90.5% in isolates from calves in 2021).
Combined resistance to ciprofloxacin and erythromycin was reported at 0.8% in C. jejuni and in 7.6% of C. coli isolates from humans (in 2021). Similarly, combined resistance to these antimicrobials in food‐producing animals was overall lower in C. jejuni isolates than in C. coli isolates for all animal species tested (Table 8). Combined resistance to ciprofloxacin and erythromycin was reported in 0.7% of C. jejuni isolates from broilers and 0.8% of isolates from fattening turkeys in 2020 (Annex B, Tables 22 and 24) and in 0.8% of isolates from calves and 1.7% of pig isolates in 2021. Combined resistance to ciprofloxacin and erythromycin was reported in 4.1% of C. coli isolates from broilers and 21.2% of isolates from fattening turkeys in 2020 (Annex B, Tables 23 and 25) and in 32.7% of isolates from calves and 9.3% of pig isolates in 2021.
Information from MSs in relation to complete susceptibility to the four antimicrobials (ciprofloxacin/nalidixic acid, erythromycin, tetracycline and gentamicin) was reported at levels of 31.3% (2020) and 30.9% (2021) in C. jejuni isolates from humans and in C. coli isolates at levels of 12.5% (2020) and 13.2% (2021). Similarly, in food‐producing animals, the observed overall complete susceptibility was higher in C. jejuni than in C. coli isolates. The overall complete susceptibility observed from C. jejuni isolates was 23% in broilers in 2020, 16.8% in fattening turkeys in 2020 and 21.6% and 48.3% in calves and pigs, respectively, in 2021. Regarding C. coli, the overall complete susceptibility observed was low for isolates from fattening turkeys (4.4%) in 2020 and calves (6.3%) in 2021 while it was higher for broilers (13.7%) in 2020 and pigs (19.9%) in 2021.
It is also relevant to consider that all countries used EUCAST ECOFFs (MIC > 1 mg/L) to determine resistance to tetracycline in C. jejuni isolates from animals, whereas 7 of 22 MS reported SIR results using clinical breakpoints (MIC > 2 mg/L) regarding resistance to tetracycline in C. jejuni isolates from humans, and the gentamicin ECOFF was different between humans and animals in 2020 (1 mg/L for human isolates, and 2 mg/L for animal isolates) (Figure 27).
Table 9 presents countries with significantly increasing or decreasing trends in resistance to selected antimicrobials (ciprofloxacin, erythromycin and tetracycline) from human isolates (2013–2021) and isolates from food‐producing animals (2015–2021 or 2009–2020/2021). Factors such as time periods considered, data collected and antibiotic usage may explain the variability observed between countries.
3.6. Discussion
Campylobacter bacteria are ubiquitous and can be found widespread in the environment and animals including food‐producing animals which pose a risk to human health. Indeed, Campylobacter is an important food‐borne zoonotic agent. Moreover, Campylobacter strains resistant to antibiotics may interfere with the treatment of human campylobacteriosis (Moore et al., 2006; Garcia and Heredia, 2013) and represent an important public health concern. The main species responsible for human infections is C. jejuni, which is usually predominant in poultry, followed by C. coli (Jehanne et al., 2020). Because of this, the monitoring of AMR in Campylobacter spp. from food‐producing animals and food derived thereof focuses on these two species, as laid down in the Commission Implementing Decision (EU) 2020/1729.
In accordance with this Decision, from 2021 onwards, the AMR monitoring is mandatory, at biannual basis, in both C. jejuni and C. coli from caecal samples from broilers, fattening turkeys, bovine animals under 1 year of age (where the national production of turkey meat and bovine meat is more than 10,000 tonnes per year) and fattening pigs at slaughter.
In the framework of Commission Implementing Decision (EU) 2020/1729, the monitoring of AMR in C. jejuni and C. coli in food‐producing animals provides comparable data on the occurrence and enables to assess the trends of AMR in these Campylobacter species in animal productions. However, it must be highlighted that the number of MSs that report data on AMR in C. jejuni and C. coli from food‐producing animals and the number of isolates vary considerably, also due to differences in the national production of meat thereof.
Campylobacter monitoring programmes, surveillance programmes and epidemiological studies aim to improve the knowledge in relation to the prevalence of C. jejuni and C. coli in animal production and food of animal origin. Increasing the knowledge on the occurrence of resistance in these bacterial species will contribute to a better understanding of the epidemiology of human infections.
In 2020, information on AMR in Campylobacter isolates from human clinical cases was reported in fewer countries than in 2019. Some countries were unable to report any results due to the impact of the COVID‐19 pandemic on AMR surveillance and monitoring activities, and laboratory operations. Additionally, the pandemic affected the ability of countries to collect isolates and send them to national reference centres, thus reducing the number of isolates available for antimicrobial susceptibility testing compared to previous years. In 2021, more countries were again able to report Campylobacter AMR data from humans, with even some countries reporting quantitative data for the first time. This can be attributed, in part, to the return to regular activities post‐pandemic. The increased focus on and support for national surveillance of antimicrobial susceptibility for Salmonella and Campylobacter in humans via the HaDEA‐funded FWD AMR RefLabCap project has most likely also contributed (https://www.fwdamr-reflabcap.eu/about‐fwd‐amr‐reflabcap).
Resistance in bacteria isolated from humans has been associated with resistance in bacteria from food‐producing animals, and also with antimicrobial consumption in both humans and animals. In the third joint inter‐agency JIACRA report of the three EU agencies ECDC, EFSA and EMA, providing data from the respective networks on antimicrobial consumption and resistance in isolates from humans and animals, a statistically significant association was observed between resistance to fluoroquinolones, macrolides and tetracycline in Campylobacter spp. isolates from animals and isolates from humans in the EU (ECDC, EFSA, and EMA, 2021). This finding is biologically plausible as Campylobacter in meat products is a major source of food‐borne infections in humans.
Overall, the data obtained in 2020–2021 from C. jejuni and C. coli from human and animal origins showed high to extremely high levels of resistance to fluoroquinolones (in this report represented by ciprofloxacin), which are critically important antimicrobials (CIA) for the treatment of Campylobacter infections in humans. Moreover, increasing trends of resistance of C. jejuni to ciprofloxacin were detected from human isolates in 12 reporting countries and from isolates from broilers in 14 reporting countries (Table 9). The high level of ciprofloxacin resistance in Campylobacter is worrisome. Seen from a human perspective, high resistance levels point to a continued high use of fluoroquinolones in food‐producing animals and particularly in poultry production, where large numbers of animals could be affected by flock antimicrobial treatment. This might not only affect resistance levels in Campylobacter but also select for other resistant microorganisms as well (e.g. Salmonella), which are then passed from animals or the meat derived thereof to humans. In general, antibiotic treatment of human infections with Campylobacter is discouraged, since these infections tend to be self‐limiting diseases. In addition, the use of ciprofloxacin in the treatment of Campylobacter infections is not advised due to the risk of treatment failure unless prior testing can confirm susceptibility. As the use of ciprofloxacin is no longer advised for the treatment of human campylobacteriosis, even low levels of resistance to other critically important antimicrobials are a cause for concern in public health.
Resistance to quinolones and fluoroquinolones has been found to be mainly due to the C257T mutation on the gyrA gene (Elhadidy et al., 2020). Modifications in the expression of the efflux pump CmeABC may result in higher MIC values of various antimicrobials including ciprofloxacin. Highly resistant isolates bearing a transferrable ‘super’ efflux pump variant of CmeABC (RE‐CmeABC) were described in China (Yao et al., 2016), and their MIC values of ciprofloxacin, along with florfenicol, chloramphenicol, erythromycin and tetracycline, were found to be increased.
Considering that fluoroquinolones are no longer an option for treatment of severe Campylobacter infections in Europe, macrolides are now the main class of antibiotics used as first‐line treatment of human campylobacteriosis. Resistance to erythromycin, belonging to macrolides, was either not detected or detected at very low levels in C. jejuni from humans, poultry and calves, but was higher in C. coli isolates from humans (overall, 8.5%), calves (overall, 35.7%), fattening turkeys (overall, 21.5%), fattening pigs (overall, 12.3%) and broilers (overall, 4.4%). High variability can be observed between countries with some countries reporting high to extremely high levels of resistance to erythromycin in isolates from humans and food‐producing animals, e.g. 55.3% and 66.7% erythromycin resistance in C. coli isolates from humans and fattening pigs reported by Portugal and 77.8% resistance in C. coli isolates from calves reported from Belgium (no AMR data from humans reported). Interestingly, erythromycin resistance significantly decreased in C. jejuni from humans in seven countries (over the period 2013–2021), from broilers in five MSs (over 2009–2020) and from fattening turkeys in three MSs (period 2014–2020). Regarding C. coli, decreasing trends of resistance to erythromycin were observed in five MSs for humans, one MS for broilers and four reporting countries for pigs. Not enough comparable data on C. coli from calves was available for trend analysis. An increasing trend of resistance of C. jejuni to erythromycin has only been detected in humans in one MS (Spain), with no detection in animals. For C. coli, increasing trends were only registered in one non‐MS for humans and one MS for broilers (Czechia). However, it is to be noted that a high proportion of erythromycin‐resistant isolates displayed very high MIC values (MIC > 128 mg/L for 2020 data; MIC > 512 mg/L for 2021 data), particularly in C. coli isolated from fattening turkeys (93.4% of resistant isolates with MIC > 128 mg/L), calves (66.7% of resistant isolates with MIC > 512 mg/L; 25% of resistant isolates with MIC between 128 and 512 mg/L) and fattening pigs (31.7% of resistant isolates with MIC > 512 mg/L; 49.1% of resistant isolates with MIC between 128 and 512 mg/L).
Common mechanisms of resistance to macrolides are mutations in one or several copies of the ribosomal RNA genes, such as A2074G, A2074C and A2075G (Luangtongkum et al., 2009). In addition, the transferable erm(B) gene, encoding an rRNA methylase, usually present on multidrug resistance islands (MDRI) or plasmids in Campylobacter, may confer a high level of resistance to macrolides, lincosamides and/or streptogramin B antibiotics (Wang et al., 2014). Initially described in Asia, this emerging resistance mechanism has also been detected in patients and in animal isolates in Europe (Florez‐Cuadrado et al., 2017; Elhadidy et al., 2019; Jehanne et al., 2021). An increase of the tested concentrations of erythromycin (up to 512 mg/L instead of 128 mg/L) has been implemented since 2021 according to Decision (EU) 2020/1729, allowing for 2021 a better screening of isolates which may carry erm(B), as it enables differentiation of isolates with an MIC < 128 mg/L, which are likely to only have mutations or alterations in target genes (L4, L22 CmeABC, CmeR genes and the binding site of CmeR) from those with a higher MIC (≥ 512 mg/L) that have an erythromycin resistance phenotype more likely associated with possession of transferable erm(B), even though mutational resistance cannot be ruled out (Wang et al., 2014). Point mutations in 23SrRNA might also confer similar levels of high resistance against erythromycin as ermB‐mediated resistance in Campylobacter (Wei and Kang, 2018; Béjaoui et al., 2022).
It should be noted that the level of resistance to tetracycline ranged from high to extremely high in humans and food‐producing animals based on data reported in 2020 and 2021. Levels were particularly high in C. jejuni and C. coli isolated from cattle (under 1 year of age) in 2021 and from C. coli isolated from fattening turkeys in 2020. Furthermore, increasing trends of resistance of C. jejuni to tetracycline were detected from human isolates in seven reporting countries and from broilers in 11 reporting countries (Table 9).
The prevalence of resistance to selected antimicrobials in C. coli from fattening pigs in 2021 has been estimated at country level as the proportion of C. coli showing microbiological resistance as a percentage of all caecal samples cultured for C. coli. Monitoring the prevalence of resistant C. coli in fattening pigs enables to address together both evolving temporal trends in the prevalence of C. coli in fattening pigs and in the occurrence of resistance in C. coli from fattening pigs, through a unique indicator. This indicator is primarily intended to follow up trends over time at the country level. However, it should be noticed that various factors, such as rearing conditions, feed, climate, etc., may also affect the C. coli true prevalence of resistance. Between‐country variability from low to extremely high levels was observed in the prevalence of ciprofloxacin resistant (ranging from 6.9% to 78.2%) and tetracycline‐resistant (ranging from 0.0% to 86.5%) C. coli from fattening pigs. Interestingly, a limited between‐country variation and notably lower levels of prevalence of resistance to erythromycin were found in C. coli from fattening pigs, which have been estimated to be below 10% for 24 reporting countries (21 MSs and 3 non‐MSs), while ranging from 14.9% to 39.7% in the remaining six reporting MSs. Noteworthy, the MS (Portugal) with the highest prevalence of resistance to erythromycin in C. coli from fattening pigs (39.7%) in 2021 had also the highest levels of erythromycin resistance (55.3%) and combined resistance to ciprofloxacin and erythromycin (55.3%) in C. coli from humans, suggesting that pigs could be a reservoir of erythromycin resistance for humans. This finding is of particular public health concern since, as commented above, macrolides, such as erythromycin and azithromycin, have become the first‐line treatment of human campylobacteriosis.
Another important aspect to highlight in this report is linked to the multidrug resistance (MDR) levels in isolates from humans and food‐producing animals. MDR in human isolates tested for four antimicrobial classes (fluoroquinolones, macrolides, tetracyclines and aminoglycosides) was overall very low in C. jejuni (1%) and low in C. coli (9.9%). MDR levels were generally low for C. jejuni isolated from the animal species considered; however, it was high in C. coli isolates from calves (39.3%) and fattening turkeys (21%).
The implementation of the Decision (EU) 2020/1729, the harmonisation of Campylobacter isolation methods and the monitoring in 2021–2027 of the resistance levels of C. jejuni and C. coli in food‐producing animals will improve our knowledge of the prevalence and occurrence of antimicrobial resistance of C. jejuni and C. coli isolated from animals in the reporting countries. Moreover, the modifications of the panel of antimicrobials and concentrations tested (EFSA, 2021) will enable a better detection of the emerging and threatening resistance mechanisms already mentioned (RE‐CmeABC, erm(B)) and other ones such as the cfr(C) gene, borne on a conjugative plasmid and conferring resistance to phenicols, lincosamides, pleuromutilins and oxazolidinones (Tang et al., 2017). These mechanisms (efflux pumps) and/or their genetic support (plasmids, MDRI) confer resistance to one or several families of antimicrobials of major importance for human treatment strategies (macrolides, fluoroquinolones or aminoglycosides) and could favour co‐selection of resistant clones or plasmids.
According to Commission Implementing Decision (EU) 2020/1729, two new substances, chloramphenicol and ertapenem, were added to the panel of antimicrobials and related findings were reported for the first time in 2021. Resistance to chloramphenicol in isolates from pigs and calves (2021) was either absent or extremely low in C. jejuni isolates from fattening pigs and calves (0%–0.1%) and C. coli isolates from pigs (0.5%). A higher (but still low) level resistance to chloramphenicol was observed in C. coli isolated from calves (3.4%). Similarly, ertapenem resistance in isolates from pigs and calves (2021) was either absent or very low in C. jejuni isolates from fattening pigs and calves (0.0%–1%) and C. coli from pigs (0.5%). It is noteworthy that an unexpected higher level of resistance to ertapenem was reported in C. coli isolated from calves (29.1%) in 2021. This finding is of public health concern as carbapenems, together with aminoglycocides, are the antimicrobial classes recommended for treatment of invasive Campylobacter infections in humans (EFSA, 2019; Dai et al., 2020). At present, only few comparable data on the resistance to ertapenem in C. coli from calves are available, and therefore, further investigations are needed to interpret this finding. Moreover, it should be noted that the epidemiological cut‐off for ertapenem used by EFSA in this analysis is still under discussion as there is not yet a validated threshold for resistance to ertapenem recommended by EUCAST. Also, no indication on the epidemiological cut‐off to be used for ertapenem in C. coli and C. jejuni was provided in Commission Implementing Decision (EU) 2020/1729. Additional data will be available in the coming years because of the implementation of the harmonised AMR monitoring in accordance with Commission Implementing Decision (EU) 2020/1729 and these will allow a detailed evaluation and validation of the appropriate threshold for resistance to ertapenem in both C. coli and C. jejuni.
Furthermore, WGS of isolates, particularly those with multidrug resistance, high‐level resistance to erythromycin or ciprofloxacin, or resistance to gentamicin or ertapenem is strongly encouraged to provide further evidence of involved antimicrobial resistance genes, their genetic origin (chromosome, plasmid, transposon, integrative and conjugative element, genomic islands) and their potential of horizontal transmission (Mourkas et al., 2019). WGS of isolates can also contribute to the detection of prevalent resistant lineages or subtypes (Webb et al., 2018; Mouftah et al., 2021) in the various sources and for comparison of animal and human isolates.
4. Antimicrobial resistance in indicator E. coli 14
The monitoring of AMR in commensal indicator E. coli collected from the intestinal flora of healthy food‐producing animals and food provides information on the reservoirs of resistant bacteria that could potentially be transferred between animal populations and humans. It also provides indirect information on the reservoirs of resistance genes that could be transferred to bacteria that are pathogenic to humans and/or animals. Such monitoring has relevance to both public health and animal health. The occurrence of AMR in indicator E. coli likely depends on several factors, including the selective pressure exerted by the use of antimicrobials in food‐producing animal populations; clonal spread of resistant organisms; dissemination of genetic elements, such as resistance plasmids; and the effects of co‐selection in bacteria exhibiting multidrug resistance (MDR).
4.1. Key findings
Resistance to ampicillin, sulfamethoxazole, trimethoprim or tetracycline was common and reported by most MSs at high or very high levels in all animal categories in 2020/2021. Resistance to quinolones was common in poultry, and very high or extremely high levels were reported by several MSs. Resistance to other antimicrobials was less common, and notably, meropenem resistance was not detected in any animal populations or meat categories in 2020/2021.
Large differences in the levels of resistance were observed between countries, and generally, lower levels were reported in northern Europe, although countries in southern and central Europe also reported low levels of resistance in isolates from bovines under 1 year of age (calves).
Complete susceptibility (CS) was more common in isolates from fattening pigs and calves than in those from broilers and fattening turkeys. Conversely, multidrug resistance (MDR) was more common in isolates from broilers and turkeys than in those from pigs and calves.
Marked differences in the levels of CS and MDR were observed between countries. The antimicrobials most often represented in the patterns of MDR isolates were tetracycline, ampicillin, sulfamethoxazole, trimethoprim and, additionally, quinolones in poultry.
The weighted summary key outcome indicator of complete susceptibility (KOICS), accounting for differences in the relative size of food animal populations in a country, varied widely between countries ranging from < 20% to > 80%. Lower KOICS were generally observed in countries in Eastern and Southern Europe and the highest in countries in the Northern part.
Resistance to highest priority critically important antimicrobials (hpCIA) was uncommon for colistin, azithromycin and third‐generation cephalosporins (cefotaxime or ceftazidime), and median levels ranged between rare and low in all animal categories. Ciprofloxacin resistance was more common, and median levels were very high in broilers, high in turkeys, low in calves and moderate in pigs. Combined resistance to third‐generation cephalosporins and fluoroquinolones was generally uncommon in all animal categories.
Statistically significant decreasing temporal trends in resistance to ampicillin, ciprofloxacin, cefotaxime, tetracycline and colistin, as well as increasing trends in CS and KOICS reveal progress towards lower levels of resistance in several countries and in the EU group as a whole. An improvement in the situation was most pronounced in poultry.
In 2021, MSs started to implement the new monitoring of AMR in indicator E. coli recovered from imported fresh meat sampled at border control posts. A number of MSs submitted E. coli isolates from imported pig meat and imported bovine meat. Similarly, 2021 was the first year MSs could choose to perform WGS as an alternative to supplementary testing of presumptive ESBL, AmpC or CP‐producing E. coli from routine monitoring.
4.2. Data on AMR in indicator E. coli addressed
Commission Implementing Decision (EU) 2020/1729 provides detailed requirements for the harmonised monitoring and reporting of AMR in zoonotic and commensal bacteria. In 2021, monitoring AMR in indicator E. coli isolates recovered from caecal contents of domestically produced fattening pigs 15 was mandatory, likewise, for MSs with consistent production of calves over a certain tonnage per annum, monitoring of indicator E. coli was mandatory. 16 For the first time in 2021, the monitoring of fresh meat from pigs and calves imported from third‐countries and sampled at border control posts (BCPs) was undertaken. In 2020, data were reported on indicator E. coli isolates from broiler and turkey flocks in accordance with Commission Implementing Decision (EU) 2013/652 (repealed on 17 November 2020). E. coli isolates from all animal origins exhibiting phenotypes suggestive of presumptive ESBL‐, AmpC‐ or CP‐producing E. coli are reported in this chapter and chapter 5.
In 2021, amikacin was added to the harmonised panel for the monitoring of AMR in indicator E. coli and was included in analyses of the occurrence of resistance, complete susceptibility (CS) and multidrug resistance (MDR). While amikacin is not used in food‐producing animals, it is commonly used in people to treat urinary tract infections, bacteraemia and intra‐abdominal infections caused by gram‐negative bacteria. The addition of amikacin to the harmonised panel is thought to improve the detection of 16S RNA methyltransferases (RMTases) (EFSA, 2019). RMTases have been increasingly found in association with carbapenemases, AmpC or ESBL enzymes and fluoroquinolone resistance in Enterobacteriaceae from human cases in Europe (Arca‐Suárez et al., 2022; Fournier et al., 2022).
The harmonised susceptibility testing of E. coli isolates derived from fresh meat imported from third countries improves our understanding of the dissemination of AMR through food and provides information that may help reduce the impact of AMR. In 2021, imported meat required for sampling was from pigs and calves. A limited number of countries reported data on isolates from meat samples collected at border control posts (BCPs), as only a small proportion of meat was imported into their country. In this chapter, reference to ‘fresh meat’ means fresh meat as defined in Annex I to Regulation (EC) No 853/2004 17 . Reference to ‘fresh imported meat’ refers to fresh meat that has been imported from a third country. BCPs are inspection posts designated and approved with EU legislation to carry out checks on animals and animal products arriving from third countries at a European Union border.
From 2021, whole genome sequencing (WGS) is authorised as an alternate method to conventional phenotypic testing for E. coli isolates obtained from routine monitoring that shows resistance to extended‐spectrum cephalosporins and carbapenems. MSs may choose to either undertake panel 2 testing of presumptive ESBL, AmpC or CP‐producing E. coli or perform WGS and report these data. WGS is authorised on a voluntary basis only, but technical conditions on the WGS technique have been imposed to ensure data comparability. The voluntary reporting of WGS data from 2021 on ESBL/AmpC/CP‐producing E. coli isolates will facilitate an understanding of the potential contribution of food‐producing animals and derived food to the burden of AMR in humans (EFSA, 2019). Information on WGS of these isolates can be found in chapter 5.
4.3. Antimicrobial resistance in poultry, porcine and bovine populations
4.3.1. Data reported
In 2021, 27 MSs and four non‐MSs reported data on indicator E. coli from pigs and 11 MSs and two non‐MSs submitted data on isolates from calves. For E. coli isolates recovered from fresh meat samples taken at BCPs, four MSs provided data from pig meat and six MSs on meat from bovine animals. Of those MSs, most submitted AMR data on fewer than 10 isolates. In 2020, 27 MSs and five non‐MSs reported data on isolates from broilers and 11 MSs and two non‐MSs data on isolates from turkeys.
Summary data on the occurrence of resistance 18 to commonly used antimicrobials in veterinary medicine (ampicillin, sulfamethoxazole and tetracyclines) as well as highest priority critically important antimicrobials (hpCIAs) (i.e. ciprofloxacin, cefotaxime and combined resistance to these two antimicrobials) are described in this chapter. Additionally, results from the analysis of MDR patterns and combined resistance to ciprofloxacin and cefotaxime 19 are reported here. Annex C presents detailed information on the occurrence of AMR, MDR and combined resistance in E. coli from pigs, calves (corresponding to 2021 data), as well as broilers and turkeys (corresponding to 2020 data), at the MS and MS‐group level. 20
Under the new legislation (Commission Implementing Decision (EU) 2020/1729), changes were made to the ECOFFs and clinical breakpoints for several antimicrobial substances included in the harmonised panel for testing of E. coli isolates. The substances include tigecycline, where the ECOFF changed from MIC > 1 to > 0.5 mg/L and the clinical breakpoint changed from MIC > 2 to > 0.5 mg/L. Also, the ECOFF for nalidixic acid changed from > 16 to > 8 mg/L. For ciprofloxacin, the clinical breakpoint changed from > 1 to > 0.5 mg/L. Therefore, for 2021 data from pigs, calves and meat from BCPS, the occurrence of resistance to tigecycline, nalidixic acid and ciprofloxacin is determined using the new ECOFFs and clinical breakpoints, and for 2020 data from poultry, tigecycline, nalidixic acid and ciprofloxacin resistance are analysed using the ECOFFs and clinical breakpoints from the previous legislation (Commission Implementing Decision (EU) 2013/652). Also, in 2021, a new substance, amikacin, was added to the harmonised panel with the ECOFF > 8 mg/L and the clinical breakpoint > 16 mg/L. See Appendix F – for more details on the changes to the harmonised panel of substances tested for E. coli isolates from the routine monitoring programme.
4.3.2. Occurrence of antimicrobial resistance
Since 2014, the antimicrobial substances included in the harmonised panel for the monitoring of AMR in E. coli from food‐producing animals have provided continuity of monitoring data and epidemiological tracing of isolates with resistance patterns of interest to public health. The antimicrobials included in the panel have been selected because they are either of public health importance, of epidemiological relevance or are commonly used in veterinary medicine. Antimicrobials such as ampicillin, sulfamethoxazole and tetracycline have been widely used for many years in veterinary medicine to treat infections in production animals. The WHO categorises ampicillin as a ‘critically important antimicrobial’ (CIA), while sulfamethoxazole and tetracycline are categorised as ‘highly important antimicrobials’ (WHO, 2019). A new substance, amikacin, was added to the harmonised panel in 2021.
Food‐producing animals
Resistance to ampicillin, sulfamethoxazole, trimethoprim and tetracycline was the most common resistance trait observed. Considering reporting MSs, median levels of resistance to these antimicrobials were high or very high in all animal populations except for calves, for which the median level of resistance to ampicillin was moderate (16.5%), and trimethoprim resistance was low (8.2%) (Figure 30; Annex C, Table 2). Large differences in resistance levels to ampicillin, sulfamethoxazole, trimethoprim and tetracycline between countries were however observed in all animal populations. For example, Cyprus (n = 22), Greece (n = 73), Portugal (n = 55) and Spain (n = 170) reported extremely high levels of resistance to tetracyclines in pigs (77.3%, 71.2%, 72.7% and 78.8%, respectively), while Finland (n = 170) and Sweden (n = 173) reported moderate resistance at 14.1% and 16.8%, respectively (Annex C, Table 2). In calves, Italy (n = 170) reported very high levels of resistance to ampicillin (60.6%), sulfamethoxazole (65.3%) and trimethoprim (56.5%) and extremely high resistance to tetracycline (74.7%). Belgium (n = 173) and France (n = 182) also reported very high levels of resistance to all four substances, while Denmark (n = 109) and Portugal (n = 53) reported low to moderate levels of resistance to these substances, and Sweden (n = 20) reported zero resistance to sulfamethoxazole and trimethoprim and just 5.0% resistance to ampicillin and tetracyclines, respectively (Annex C, Table 2).
Figure 30.
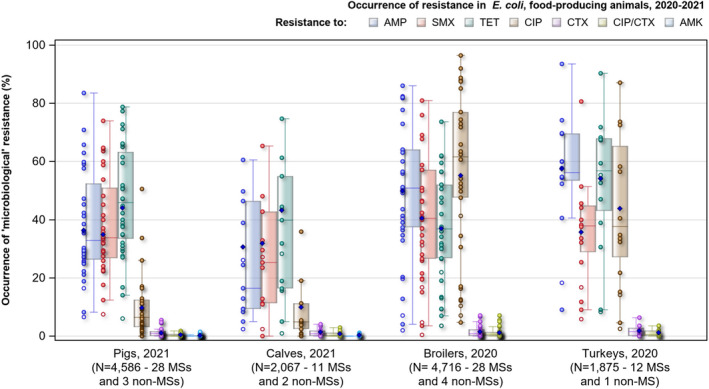
- N: Total number of isolates reported by Member States (MSs) and non‐Member States (non‐MSs); AMP: ampicillin; SMX: sulfamethoxazole; TET: tetracycline; CIP: ciprofloxacin, CTX: cefotaxime; CIP/CTX: combined ‘microbiological’ resistance to ciprofloxacin and cefotaxime; AMK: Amikacin; Horizontal lines represent median; Lower and upper box boundaries, 25th and 75th percentiles, respectively; Blue diamond: resistance at the reporting MS group level.
In poultry, resistance to ciprofloxacin and nalidixic acid was common, with very high median levels in broilers and high median levels in turkeys (Figure 30; Annex C, Tables 3 and 4). In contrast, in pigs and calves, median resistance levels to both these antimicrobials were low (Figure 30; Annex C, Tables 1 and 2). For both ciprofloxacin and nalidixic acid resistance, there were large differences between reporting countries. Most countries reported nalidixic acid resistance at lower levels than ciprofloxacin resistance. This was most notable for pigs and calves, and at the MS‐group level, nalidixic acid resistance was approximately half that for ciprofloxacin for both these animal populations. For chloramphenicol, the overall median resistance level for all reporting MSs was low to moderate for all animal populations (range 5.0–15.9%). However, some countries reported high to very high resistance, and one country (Romania) reported extremely high resistance in turkeys (74.2%, n = 31) (Annex C, Table 4). The overall median level of resistance to gentamicin was very low or low in all four animal populations (range 0.9–2.9%). Resistance to cefotaxime, ceftazidime, colistin and azithromycin were rare, very low or low in all four animal populations (Annex C). Meropenem resistance was not detected in any isolate of indicator E. coli. Overall resistance to tigecycline in E. coli isolates from pigs in the MSs was 0.4% (n = 4,013) with Hungary accounting for half of the resistant isolates (4.7%, n = 170), and in isolates from calves (n = 1,599), Belgium accounted for the majority of resistant isolates (5.2%, n = 173). Resistance to tigecycline was reported in a single isolate from a turkey in Portugal and from none in broilers. For amikacin, the new substance required for testing in 2021, overall median resistance in pigs was low (0.2%), with nine resistant isolates spread across seven countries. While for calves, amikacin resistance (0.3%) was detected in four E. coli isolates from Belgium (n = 2) and the Netherlands (n = 2).
Imported fresh meat
Four MSs contributed data on imported fresh pig meat sampled at BCPs, representing a total of 13 E. coli isolates. For ampicillin, sulfamethoxazole, trimethoprim and tetracycline, overall median resistance levels ranged from zero (trimethoprim) to high (tetracycline) for pig meat and bovine meat (Annex C, Tables 5 and 6). For E. coli isolates recovered from imported meat from bovine animals, six MSs contributed data, representing 110 isolates (Annex C, Table 6), most of them being submitted by the Netherlands (n = 79, 71.8%). The overall median resistance levels to ampicillin, sulfamethoxazole and trimethoprim was zero, and for tetracycline, the overall median resistance was low (2.4%). Among E. coli isolates tested in the Netherlands, resistance to ampicillin was not detected, while low to moderate resistance was detected for sulfamethoxazole (7.6%), trimethoprim (3.8%) and tetracycline (11.4%). Resistance to amikacin was not reported in either pig or bovine meat (Annex C, Tables 5 and 6).
Resistance to highest priority critically important antimicrobials (hpCIA)
Among the antimicrobials tested in the mandatory monitoring of indicator E. coli, ciprofloxacin (fluoroquinolones), cefotaxime and ceftazidime (third‐generation cephalosporins), colistin (polymyxins) and azithromycin (macrolides) are categorised by the WHO as hpCIA (WHO, 2019).
Food‐producing animals
Considering all reporting MSs, overall median colistin resistance was rare in pigs (0%), calves (0%) and broilers (0%) and very low in turkeys (1.8%) (Annex C). For broilers, just one country, Cyprus, reported moderate resistance to colistin in E. coli isolates (10.1%, n = 99), while for turkeys, Portugal reported high‐level resistance (23.9%, n = 142). For azithromycin, overall median levels of resistance in E. coli isolates for all reporting MSs were very low in calves (0.8%), broilers (0.5%) and low in pigs (1.3%) and turkeys (1.1%). E. coli resistance to both colistin and azithromycin was not observed in most countries, with only a small number of countries reporting resistance to both antimicrobials at either low or moderate levels (Annex C).
In contrast, very high levels of resistance to fluoroquinolones/quinolones were recorded in isolates from broilers (median: ciprofloxacin 52.7%; nalidixic acid 49.4%), and high levels in isolates from turkeys (median: ciprofloxacin 33.5%; nalidixic acid 22.9%) (Figure 30; Annex C, Tables 3 and 4). Including all reporting countries, overall median resistance to ciprofloxacin and nalidixic acid were reported at low levels in isolates from pigs (median 5.9% and 3.9%, respectively) and calves (median 4.7% and 3.1%, respectively). Large variations in resistance levels were observed at the individual reporting country level for each of the animal populations. For example, Spain reported very high resistance to ciprofloxacin (50.6%) and high resistance to nalidixic acid (27.1%) in 170 E. coli isolates recovered from pigs. While in broilers and turkeys, nearly all countries reported either high, very high or extremely high resistance to ciprofloxacin and nalidixic acid (Figure 31; Annex C). In all animal populations monitored, overall median resistance to third‐generation cephalosporins (cefotaxime or ceftazidime) was very low or low (range 0.2–1.1%) (Figure 30; Figure 31; Annex C).
Figure 31.
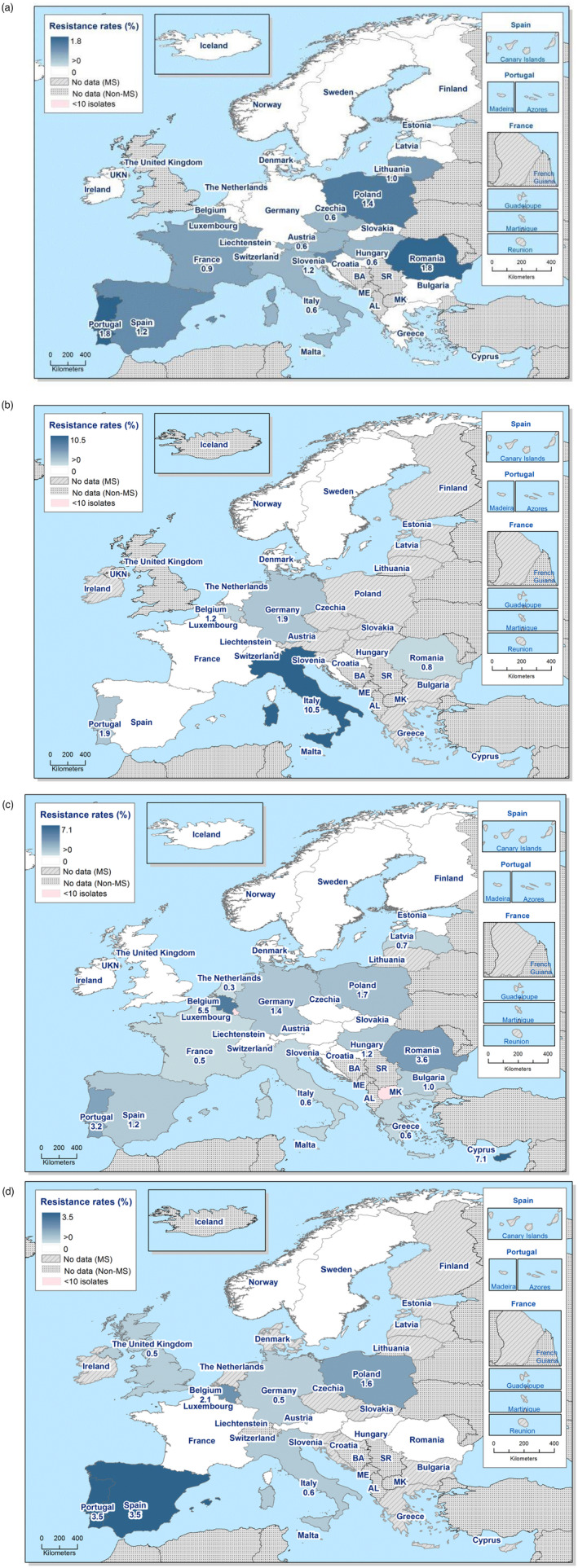
Spatial distribution of combined microbiological resistance to cefotaxime and ciprofloxacin in indicator Escherichia coli. (a) fattening pigs, 2021; (b) bovines under 1 year of age, 2021; (c) broilers, 2020; and (d) fattening turkeys, 2020, EU MSs and non‐MSs
Imported fresh meat
For colistin and azithromycin, resistance was not detected in E. coli isolates from pig meat (Annex C, Table 5). While in bovine meat, one isolate reported resistance to azithromycin, and no isolates were resistant to colistin (Annex C, Table 6). For ciprofloxacin, one E. coli isolate from pig meat was reported to be resistant (Sweden, n = 2) and two isolates from bovine meat (Italy, n = 21; the Netherlands, n = 79). For nalidixic acid, resistance was not detected in any isolates from pig meat; however, two isolates from bovine meat were resistant (Italy, n = 21; the Netherlands, n = 79) (Annex C). When considering cefotaxime and ceftazidime, resistance was not detected in E. coli isolates from pig meat, and just one isolate was resistant to both substances in isolates from bovine meat (Annex C, Table 6).
Combined resistance to ciprofloxacin and cefotaxime
Food‐producing animals
In most reporting countries, combined resistance to ciprofloxacin and cefotaxime was either not observed or discerned at low or very low levels in all four animal populations monitored (Figure 31; Annex C). Overall, the median of microbiological combined resistance to ciprofloxacin and cefotaxime was rare (pigs, calves) or very low (broilers and turkeys). Clinical combined resistance (i.e. defining resistance by the clinical breakpoint) was not generally observed in any of the animal origins, and where it was, fewer than 10 isolates were reported with combined resistance across all reporting countries by animal origin, except in broilers, where 24 isolates were observed as clinically resistant to both substances (Annex C). Overall, 98 E. coli isolates with microbiological combined resistance of which 41 also had clinical combined resistance were detected in the food‐producing animal populations monitored (Table 10). Isolates exhibiting combined resistance were more common in poultry than in pigs and calves.
Table 10.
Combined resistance to ciprofloxacin and cefotaxime in indicator E. coli from fattening pigs (pigs), bovines under 1 year of age (calves), broilers and fattening turkeys (turkeys) applying ECOFFs and clinical breakpoints, as issued by EUCAST for MSs and non‐MSs, 2020/2021
| Food‐producing animal population | ‘Microbiological’ combined resistance to CIP & CTX (using ECOFFs) | ‘Clinical’ combined resistance to CIP & CTX (using clinical breakpoints) | ||||
|---|---|---|---|---|---|---|
| No. of isolates | % Resistance | 95%CI | No. of isolates | % Resistance | 95%CI | |
| Pigs, 2021 (N = 4,586, 28 MSs, 3 non‐MSs) | 17 | 0.4 | 0.2, 0.6 | 6 | 0.1 | 0, 0.3 |
| Calves, 2021 (N = 2,067, 11 MSs, 2 non‐MSs) | 11 | 0.5 | 0 1.2 | 2 | 0.1 | 0, 0.5 |
| Broilers, 2020 (N = 4,716, 27 MSs, 5 non‐MSs) | 49 | 1.0 | 0, 4.2 | 24 | 0.5 | 0, 037 |
| Turkeys, 2020 (N = 1,875, 11 MSs, 2 non‐MSs) | 19 | 1.0 | 0.2, 1.7 | 8 | 0.4 | 0, 0.8 |
| Imported pig meat, 2021 (N = 13, 4 MSs) | 0 | 0 | 0 | 0 | 0 | 0 |
| Imported bovine meat, 2021 (N = 110, 6MSs) | 1 | 0.9 | 0, 5.0 | 1 | 0.9 | 0, 5.0 |
N: total number of E. coli isolates reported by MSs and non‐MSs; CIP: ciprofloxacin; CTX: cefotaxime; ECOFF: epidemiological cut‐off value.
Imported fresh meat
Microbiological combined resistance to ciprofloxacin and cefotaxime was not detected in any E. coli isolates recovered from imported pig meat, and only one isolate from imported bovine meat (reported by the Netherlands) exhibited combined resistance (Table 10).
4.3.3. Temporal trends in resistance
Temporal trends in resistance to ampicillin, ciprofloxacin, cefotaxime and tetracyclines in indicator E. coli from pigs, calves, broilers and turkeys were evaluated for countries having provided data for three or more years over the period 2009–2021 and for the MS‐group (including the United Kingdom). Ampicillin and tetracycline were considered in the temporal trend analysis, as they are the most used antimicrobials in food‐producing animals in Europe (EMA, 2021) and decreasing trends in resistance are believed to primarily reflect changes in usage. Resistance trends in the hpCIAs, ciprofloxacin and cefotaxime, have also been assessed, as the presence of such resistance in E. coli from food‐producing animals may impact human health. The statistical significance (p < 0.05) of trends was tested by logistic regression (see Appendix F – for details on methodological approach).
Sufficient data for assessing temporal trends were available from 31 countries for pigs, 30 for broilers and 11 countries each for calves and turkeys. Thus, 83 different animal/substance combinations were available and analysed for trends in resistance to ampicillin, ciprofloxacin, cefotaxime and tetracycline. For poultry data in 2020, 168 analyses were performed, and in total, 89 combinations had statistically significant (p < 0.05) decreasing trends, while 24 combinations had statistically significant increasing trends (Table 11). For pig and calf data in 2021, of the 162 analyses performed, 53 combinations had statistically significant (p < 0.05) decreasing trends, while 23 combinations had statistically significant increasing trends (Table 11). There were more decreasing than increasing trends and most noticeable was that a decrease in tetracycline resistance was observed in approximately half of the data sets for pig and calf data (24/43) and poultry data (23/42) (Table 11). It is of note that in several countries, levels of resistance were stable over time at low levels, and major changes cannot be expected.
Table 11.
Summary of trends in resistance to ampicillin, ciprofloxacin, cefotaxime and tetracyclines in indicator E. coli from fattening pigs (pigs) and bovines < 1 year of age (calves) for the period 2009–2021, and broilers, and fattening turkeys (turkeys) for the period 2009–2020, EU MSs and non‐MSs
| Animal population | Ampicillin | Ciprofloxacin | Cefotaxime | Tetracycline | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ↓ | ↑ | ↔ | ↓ | ↑ | ↔ | ↓ | ↑ | ↔ | ↓ | ↑ | ↔ | ↓ | ↑ | ↔ | |
| Pigs, 2021 (27 MSs, 4 non‐MSs) | 7 | 7 | 17 | 6 | 5 | 20 | 4 | 2 | 25 | 17 | 3 | 11 | 34 | 17 | 73 |
| Calves, 2021 (9 MSs, 2 non‐MSs) | 4 | 1 | 6 | 6 | 2 | 3 | 2 | 1 | 8 | 7 | 2 | 2 | 19 | 6 | 19 |
| Total, 2021 | 11 | 8 | 23 | 12 | 7 | 23 | 6 | 4 | 33 | 24 | 5 | 13 | 53 | 23 | 92 |
| Broilers, 2020 (26 MSs, 4 non‐MSs) | 15 | 6 | 9 | 18 | 10 | 2 | 20 | 2 | 8 | 15 | 2 | 13 | 68 | 20 | 32 |
| Turkeys, 2020 (10 MSs, 1 non‐MSs) | 7 | 1 | 4 | 4 | 1 | 7 | 2 | 1 | 9 | 8 | 0 | 4 | 21 | 3 | 24 |
| Total, 2020 | 22 | 7 | 13 | 22 | 11 | 9 | 22 | 3 | 17 | 23 | 2 | 17 | 89 | 24 | 55 |
↓: statistically significant decreasing trends; ↑: statistically significant increasing trends; ↔: stable trend.
Fattening pigs
Of the 31 countries reporting AMR data on indicator E. coli isolates from pigs between 2009 and 2021, a total of 34 decreasing and 17 increasing trends were registered (Table 11; Figure 32). In 13 countries, only decreasing trends were observed, notably Germany, the Netherlands and the Republic of North Macedonia, for all four antimicrobials and Cyprus, for three antimicrobials (ampicillin, ciprofloxacin, tetracycline). In contrast, two countries (Poland and Slovakia) reported only increasing trends in ampicillin and tetracycline, and for Poland, ciprofloxacin was observed to be also increasing. Most notable was that tetracycline resistance has decreased in 17 countries and increased in just three. Overall, four countries (Croatia, Estonia, Malta and Sweden) were observed to have no statistically significant change in trends. At the MS group level (including the UK), only decreasing trends were observed, especially in ampicillin and tetracycline.
Figure 32.
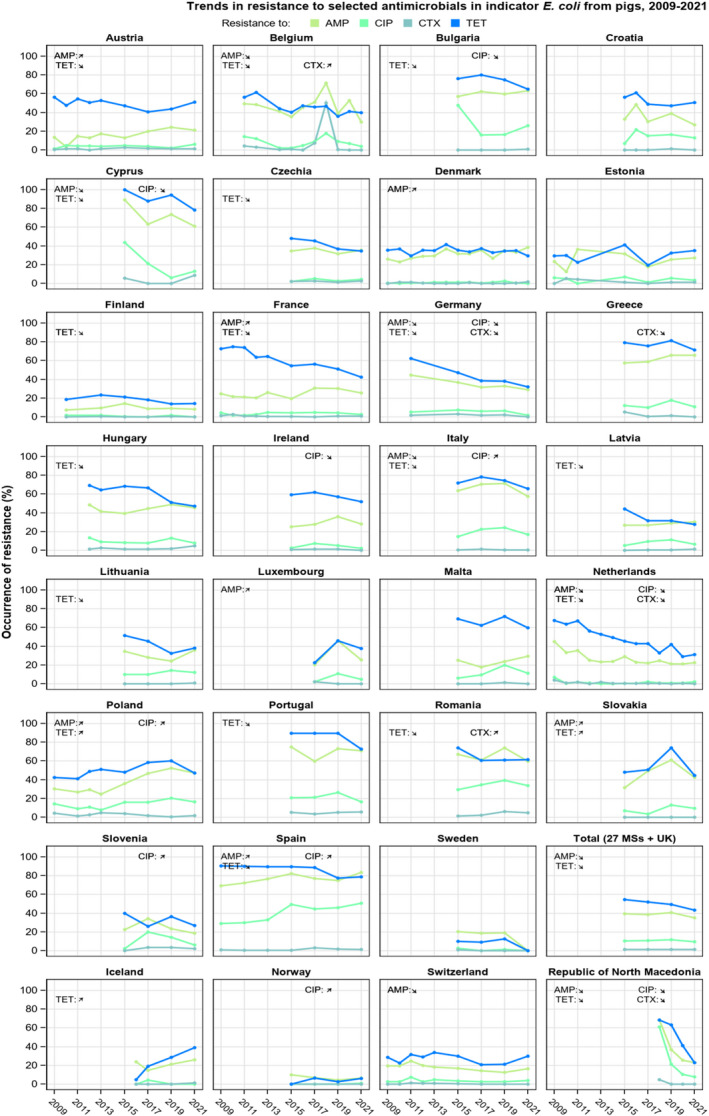
- (↘)(↗): indicates statistically significant trends over the study period.
Bovine animals under 1 year of age (calves)
In the 11 countries reporting data on indicator E. coli from calves between 2009 and 2021, a total of 19 decreasing and six increasing trends were observed (Table 11; Figure 33). In eight countries, only decreasing trends were recorded for one or more of the following substances: ampicillin, ciprofloxacin, cefotaxime or tetracycline. Germany and the Netherlands registered statistically significant decreasing trends in all four substances, while France and Switzerland recorded decreasing trends in three substances (ampicillin, ciprofloxacin and tetracycline). In contrast, two countries reported only increasing trends in resistance, with Belgium having increasing trends in all four substances, and Denmark having increasing trends in ciprofloxacin and tetracycline. Croatia was the only country observed to have no statistically significant change in trends. At the MS‐group level (including the UK), tetracycline was observed to have a decreasing trend in resistance.
Figure 33.
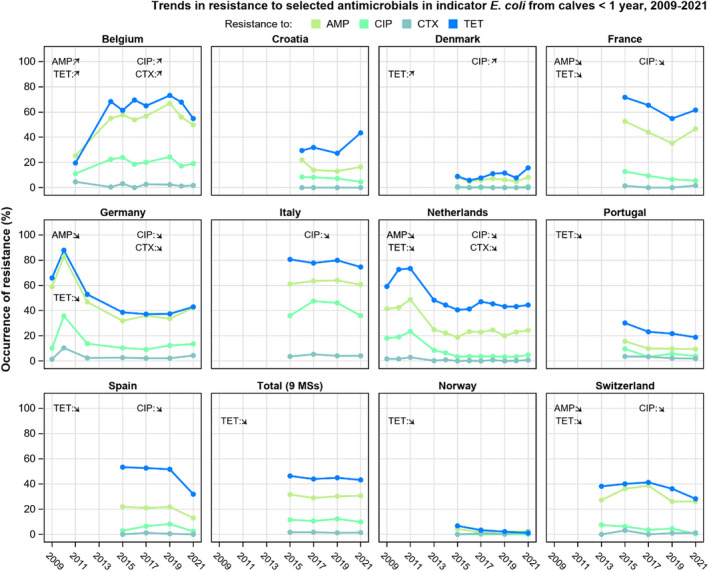
- (↘)(↗): indicates statistically significant trends over the study period.
Broilers
In the 30 countries reporting data on isolates from broilers, 68 decreasing and 20 increasing trends were registered (Table 11; Figure 34). In 16 countries, only decreasing trends were observed. Notably, in Ireland, Italy, Latvia, the Netherlands and Spain, resistance has decreased for all four antimicrobials and in Croatia, Estonia, France, Lithuania and Portugal for three antimicrobials. In contrast, in three countries, only increasing trends were observed. In the MS group, including also the United Kingdom, resistance to all four antimicrobials has decreased with statistical significance.
Figure 34.
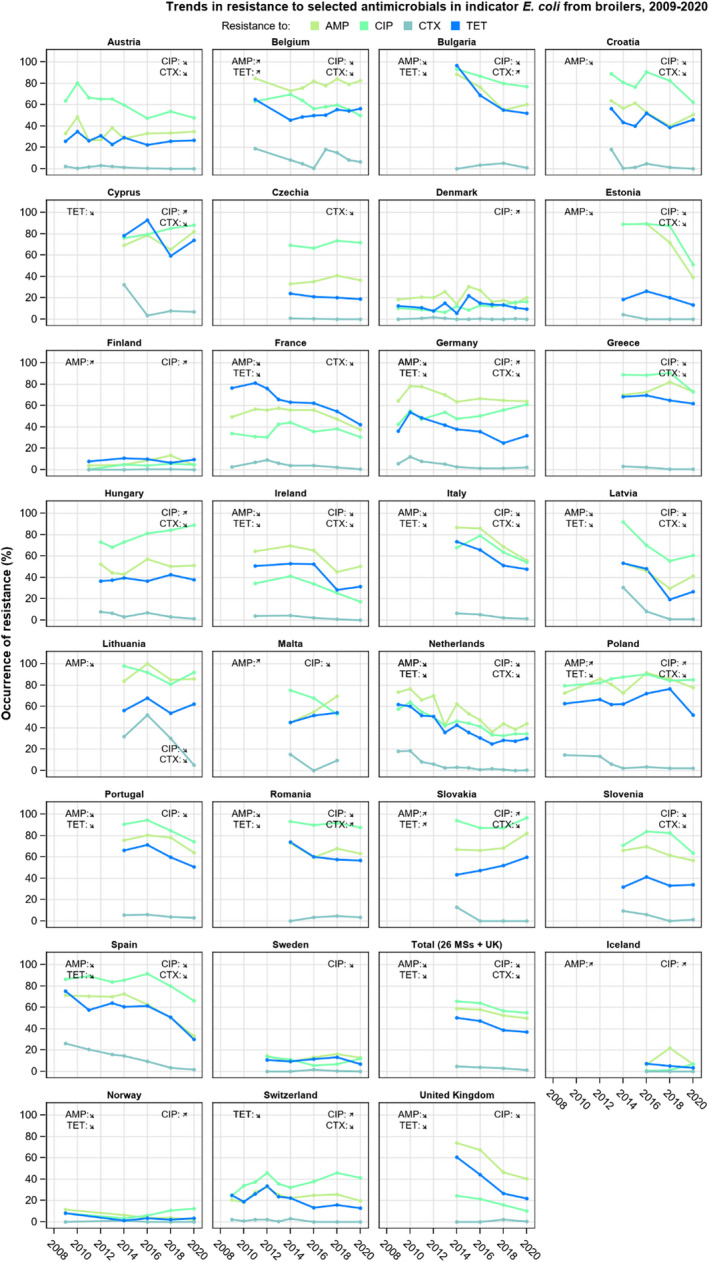
- (↘)(↗) indicates statistically significant trends over the study period.
Fattening turkeys (turkeys)
In the 12 countries reporting data on isolates from turkeys, there were 21 decreasing and three increasing trends were observed (Table 11; Figure 35). Eight countries reported only decreasing trends; in Spain, for all four antimicrobials and in France, Italy and Portugal, for three antimicrobials. At the MS‐group level, including also the United Kingdom, resistance to ampicillin and tetracycline has decreased with statistical significance.
Figure 35.
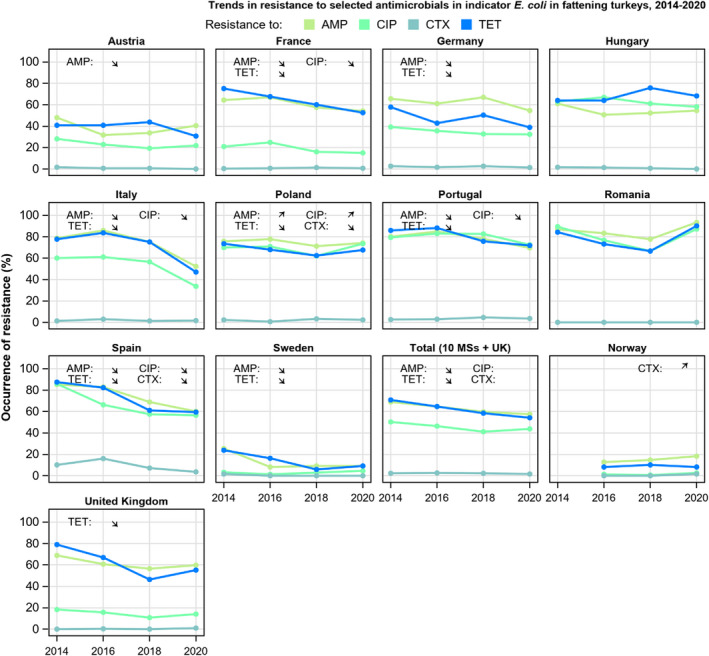
- (↘)(↗): indicates statistically significant trends over the study period.
4.3.4. Phenotypic characterisation of third‐generation cephalosporin and carbapenem resistance
A low number of indicator E. coli isolates from caecal samples from pigs and calves in 2021 and from broilers and turkeys in 2020 were phenotypically resistant to third‐generation cephalosporins (cefotaxime and/or ceftazidime) upon initial testing on panel 1 (Table 12). Further phenotypic characterisation of these isolates for presumptive production of ESBL‐ and/or AmpC‐enzymes on panel 2 showed that the total number of isolates exhibiting a phenotype of ESBL‐ and/or AmpC‐producers was low in all four animal populations (Table 12). In countries reporting presumptive ESBL‐ and/or AmpC‐producing isolates, the occurrence was generally very low or low, ranging from 0.6% to 8.7% in isolates from pigs, from 0.7% to 3.5% in isolates from calves, from 0.6% to 7.1% in isolates from broilers and from 0.6% to 6.3% in isolates from turkeys. Presumptive ESBL‐producers were more common than AmpC‐producers in all animal populations and isolates with a combined phenotype (ESBL + AmpC) were uncommon (Table 12).
Table 12.
Occurrence of resistance to third‐generation cephalosporins in indicator E. coli isolates from fattening pigs (pigs), bovines under 1 year of age (calves), pig meat from border control posts (BCP), bovine meat from BCPs, broilers and fattening turkeys (turkeys). EU MSs and non‐MSs, 2020/2021
| Animal category | No. of MSs/non‐MSs | N | Cefotaxime | Ceftazidime | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Pigs, 2021 | 28/3 | 4,586 | 46 | 1.0 | 43 | 0.9 |
| Calves, 2021 | 11/2 | 2,067 | 31 | 1.5 | 26 | 1.3 |
| Imported pig meat, 2021 | 4/0 | 13 | 0 | 0 | 0 | 0 |
| Imported bovine meat, 2021 | 6/0 | 110 | 1 | 0.9 | 1 | 0.9 |
| Broilers, 2020 | 27/5 | 4,716 | 58 | 1.2 | 54 | 1.1 |
| Turkeys, 2020 | 11/2 | 1,875 | 32 | 1.3 | 31 | 1.3 |
N: Total number of isolates tested by MSs and non‐MSs; n: Total number of isolates resistant; BCP: border control posts.
No indicator E. coli recovered from caecal samples by MSs and non‐MSs from the four animal populations in 2020/2021 showed microbiological resistance to carbapenems (meropenem) upon initial testing on panel 1 (Table 13).
Table 13.
Phenotypes of presumptive ESBL‐, AmpC‐ or CP‐ producing indicator E. coli subjected to supplementary testing (panel 2), EU MSs and non‐MSs, 2020/2021
| Animal category | ESBL and/or AmpC | ESBL (a) | AmpC (b) | ESBL + AmpC (c) | CP (d) |
|---|---|---|---|---|---|
| n (% R) | n (% R) | n (% R) | n (% R) | n (% R) | |
| Pigs, 2021 (N = 4,568) | 42 (0.9) | 31 (0.7) | 11 (0.2) | 0 | 0 |
| Calves, 2021 (N = 2,067) | 14 (0.7) | 8 (0.4) | 6 (0.3) | 0 | 0 |
| Imported pig meat, 2021 (N = 13) | 0 | 0 | 0 | 0 | 0 |
| Imported bovine meat, 2021 (N = 110) | 1 (0.9) | 1 (0.9) | 0 | 0 | 0 |
| Broilers, 2020 (N = 4,716) | 54 (1.1) | 45 (1.0) | 16 (0.3) | 7 (0.1) | 0 |
| Turkeys, 2020 (N = 1,875) | 30 (1.6) | 25 (1.3) | 8 (0.4) | 3 (0.2) | 0 |
ESBL: extended‐spectrum β‐lactamase; CP: carbapenemase; N: Total number of isolates reported by MSs and non‐MSs; n: number of isolates with this phenotype; % R: percentage of isolates from the total tested; ESBL: extended‐spectrum β‐lactamase; BCP: border control post.
All isolates showing clavulanate synergy with cefotaxime, ceftazidime or with both compounds, suggesting the presence of an ESBL (independently of the presence of other mechanisms).
Isolates with microbiological resistance to cefoxitin, suggesting the presence of an AmpC enzyme (independently of the presence of other mechanisms).
Isolates showing synergy with cefotaxime or ceftazidime and with microbiological resistance to cefoxitin, suggesting the presence of ESBL and AmpC enzymes in the same isolate. These isolates are also included in the ESBL and AmpC columns.
Isolates with microbiological meropenem resistance.
No E. coli isolates from imported pig meat (n = 13) displayed phenotypic resistance to third‐generation cephalosporins, while a single isolate from imported bovine meat (n = 110) was resistant to both cefotaxime and ceftazidime (Table 12). This isolate underwent supplementary testing (panel two) and exhibited a phenotype of ESBL producer (Table 13).
4.3.5. Colistin resistance
Colistin (polymyxin E) is an antimicrobial of the polymyxin group that has been used extensively in farm animals all over the world, including in Europe. In human medicine, the use of colistin has historically been limited, but an increased usage has been recorded to account for the need for last resort antimicrobials to treat infections caused by multidrug‐resistant Gram‐negative bacteria. Consequently, polymyxins are now among the five antimicrobials listed by the WHO as critically important and of highest priority for human medicine. The discovery of transferable genetic elements (e.g. mcr‐ genes) conferring resistance to colistin further underlines the importance of monitoring such resistance in food‐producing animals. The mandatory monitoring, in accordance with Commission Implementing Decision (EU) 2020/1729, is based on phenotypic susceptibility and molecular testing is required for inference regarding the underlying mechanisms of resistance and the possible presence of mcr‐ genes.
During the period 2020–2021, the phenotypic resistance to colistin in indicator E. coli for all animal origins was very low (1.1%, 143/13,239). While most countries did not detect colistin resistance in E. coli isolates from any animal origin, varying levels of resistance were reported in some countries. For example, few countries reported resistance to colistin in isolates from pigs (6/31) or calves (2/13), while more countries reported resistance in broilers (8/32) and turkeys (7/13). At the MS‐group level, median levels of colistin resistance were rare in isolates from pigs (0%), calves (0%) and broilers (0%), and low in isolates from turkeys (1.8%) (Annex C). At the country level, low to moderate to high levels of resistance were observed in some countries, up to 3.0% in pigs, 10.1% in broilers and 23.9% in turkeys (Annex C). Colistin resistance was not detected in E coli isolates from imported meat origins.
In pigs, statistically significant decreasing trends 21 were observed in three countries (Germany, Spain and the Republic of North Macedonia), and no country had increasing trends (Appendix E). Similarly, in calves, decreasing trends were observed in one MS (Italy), and no country had increasing trends. Trends for colistin resistance in broilers decreased in three countries (Italy, Portugal, Romania) and increasing trends were observed in Bulgaria and Cyprus (Appendix E). In turkeys, no statistically significant trends were observed (Appendix E). At the MS‐group level, decreasing trends in isolates from calves and broilers and no changes in trends in isolates from pigs and turkeys (Appendix E).
4.3.6. Multidrug resistance
Multidrug resistant isolates
Food‐producing animals
MDR is defined as microbiological resistance to three or more antimicrobial classes of the harmonised panel tested. In 2021, the median MDR observed in indicator E. coli isolates from pigs and all reporting MSs was 31.2% and 18.8% in isolates from calves, while, in 2020, the median MDR was assessed at 38.3% of E. coli isolates from broilers and in 49.5% of isolates from turkeys in the MSs. Large variations in MDR between reporting countries were observed, and ranged between 8.2 and 78.8% in pigs, 0–62.9% in calves, 2.4–85.2% in broilers and 4.6–90.3% in turkeys (Annex C).
Imported fresh meat
MDR was observed in two of the 13 E. coli isolates from imported pig meat, while for imported bovine meat, MDR was observed in four of 110 isolates, all reported by the Netherlands.
MDR patterns
Food‐producing animals
A wide variety of resistance patterns were observed in MDR isolates. The antimicrobials most often represented in the patterns of isolates from pigs and calves were ampicillin, sulfamethoxazole, trimethoprim and tetracycline. For MDR E. coli isolates from pigs, the combination of ampicillin, sulfamethoxazole, trimethoprim and tetracycline was found in 41.6% (564/1355) of all MDR patterns reported for all reporting countries, and one or more of these substances featured in every MDR pattern reported. For MDR E. coli isolates from calves, the combination of ampicillin, sulfamethoxazole, trimethoprim and tetracycline was found in 86.9% (483/539) of all MDR patterns reported for all reporting countries, and one or more of these substances featured in every MDR pattern reported. These antimicrobials, alone or in combination with other substances, were also common in resistance patterns of MDR isolates from broilers (41.5%) and turkeys (42.2%).
MDR patterns of isolates from poultry included (fluoro)quinolones (i.e. ciprofloxacin and nalidixic acid) at 75.9% for broilers and 73.8% for turkeys. In contrast, ciprofloxacin and/or nalidixic acid were not as common in MDR patterns for MDR E. coli isolates from pigs (17.0%, 231/1355) and calves (27.8%, 150/539). Resistance to third‐generation cephalosporins (i.e. cefotaxime and or ceftazidime) among MDR E. coli isolates was uncommon at 1.3% in pigs, 2.0% in calves, 3.0% in broilers and 3.8% in turkeys. Colistin was uncommon in the patterns of MDR E. coli isolates, with just three MDR isolates from pigs (0.2%) and two MDR isolates from calves (0.4%) featuring resistance to colistin across all reporting countries in 2021. While in 2020, colistin was more common in poultry data, with 2.7% of MDR isolates from broilers, and 9.5% of MDR isolates from turkeys reporting the presence of colistin in resistance patterns. In 2021, the occurrence of tigecycline resistance in MDR patterns was observed in just five isolates from pigs (0.4%) and in 11 isolates from calves (2.0%). While only one MDR isolate each for pigs and calves was observed to include amikacin, the new substance included in harmonised testing in 2021, in their resistance patterns.
Imported fresh meat
The resistance patterns of the two MDR E. coli isolates from imported pig meat featured sulfamethoxazole and tetracycline, along with other substances. One of the two isolates also featured resistance to ciprofloxacin (reported by Sweden). The resistance patterns for the four MDR E. coli isolates from imported bovine meat also featured one or more of the substances: ampicillin, sulfamethoxazole, trimethoprim or tetracycline. One of the isolates was resistant to six antimicrobial classes, including third‐generation cephalosporins and fluoroquinolones. No resistance to tigecycline or amikacin was recorded for either imported meat origin.
4.3.7. Completely susceptibility
Completely susceptible isolates
Food‐producing animals
The occurrence of resistance can also be addressed by considering the proportion of indicator E. coli isolates exhibiting susceptibility to all the 15 antimicrobials tested in the harmonised panel, using ECOFFs for interpretation. Considering all reporting MSs, the median CS in E. coli isolates was 38.3% from pigs, 54.1% from calves, 19.4% from broilers and 18.2% from turkeys (Annex C). For all animal populations, CS varied widely between reporting countries and ranged between 6.5% and 85.8% in pigs, 36.4–95.0% in calves, 1.0–82.9% in broilers and 3.2–79.6% in turkeys (Annex C). Typically, the highest levels of CS in all four animal populations were observed in isolates from the Nordic countries, with levels generally decreasing in a north‐to‐south gradient and, to a lesser extent, in a west‐to‐east gradient.
Imported fresh meat
Considering the four countries that reported data, CS for imported pig meat was 45.0% (n = 13). For imported bovine meat, the median CS was observed to be 95.2%.
Trends in complete susceptibility
Trends in complete susceptibility in indicator E. coli from pigs, calves, broilers and turkeys were assessed 22 for countries providing data for 3 or more years over the period 2014–2021 and also at the EU MS‐group level. In pigs, statistically significant difference in CS at the MS‐group level was not observed between 2015 and 2021 (Figures 36 and 37). In three countries (France, Germany and the Netherlands), the rate of completely susceptible isolates increased significantly, whereas it decreased in three countries Austria, Iceland and Slovakia. In calves, the level of complete susceptibility has also remained stable at the EU level, but an increase was observed in five countries (Belgium, France, Portugal, Spain and Switzerland) (Figures 36 and 37).
Figure 36.
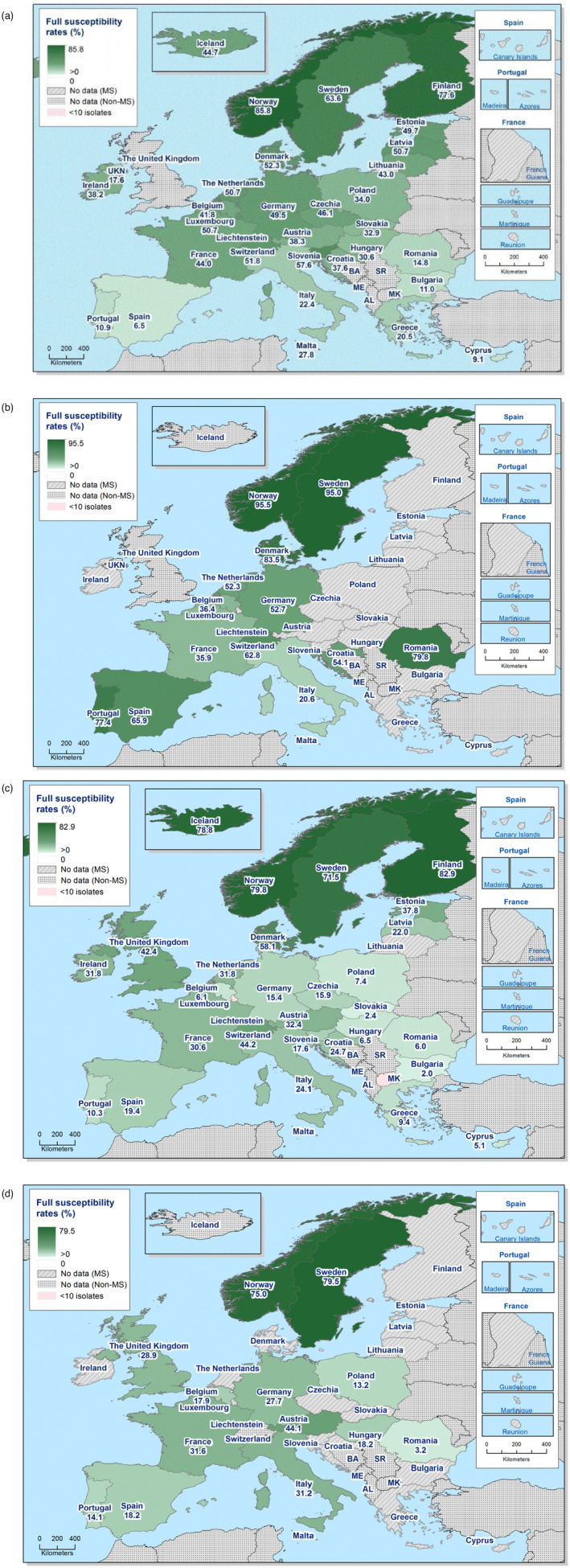
Spatial distribution of complete susceptibility to the antimicrobials tested in indicator E. coli. (a) fattening pigs (pigs) 2021; (b) bovines under 1 year of age (calves) 2021; (c) broilers 2020; (d) fattening turkeys (turkeys) 2020
Figure 37.
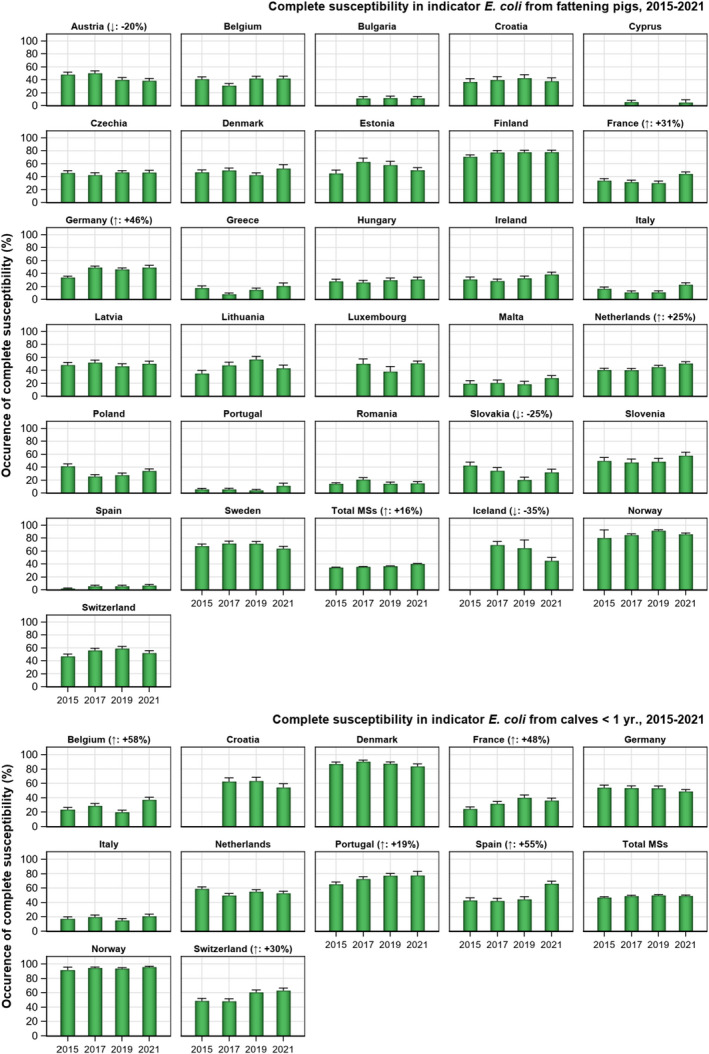
- (↓)/(↑): indicates statistically significant trends over the period 2015–2021.
In broilers, complete susceptibility increased between 2014 and 2020 at the MS‐group level (including the UK) as well as in 11 countries (Croatia, Estonia, France, Ireland, Italy, Latvia, the Netherlands, Portugal, Romania, Spain, the United Kingdom) and decreased in two countries (Belgium and Hungary) (Figures 36 and 38). In turkeys, the level of complete susceptibility has increased significantly at the MS‐group level (including the UK) as well as in seven individual countries (France, Hungary, Italy, Portugal, Spain, Sweden and the United Kingdom) (Figures 36 and 38).
Figure 38.
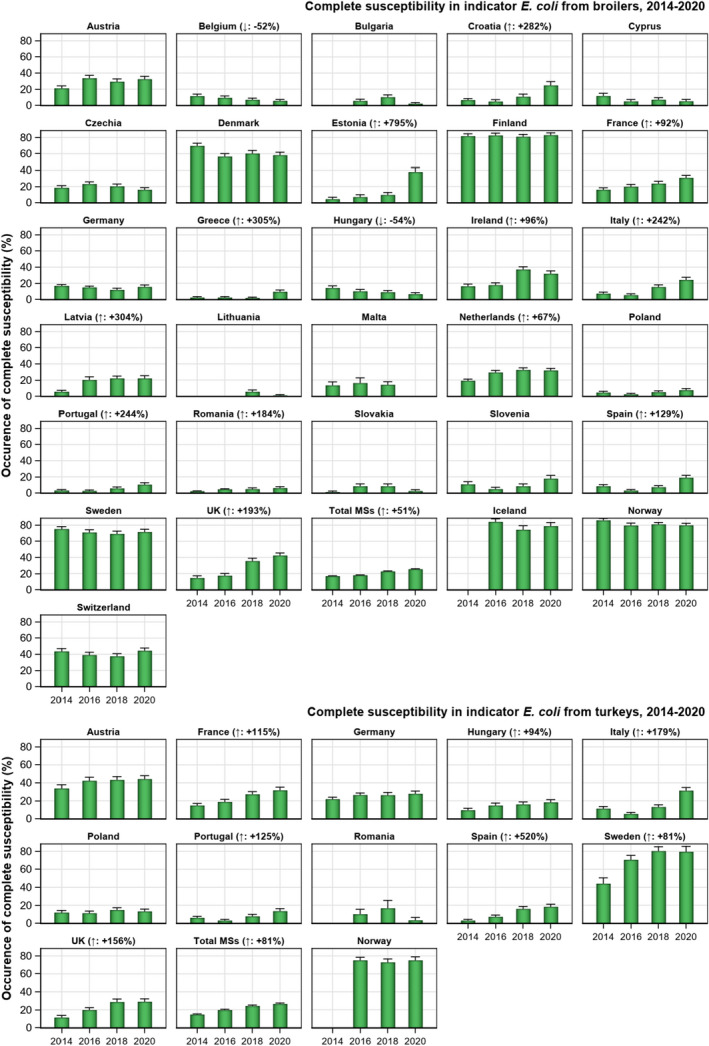
- (↓)/(↑): indicates statistically significant trends over the period 2014–2020.
4.3.8. Key Outcome Indicator of Complete Susceptibility (KOICS )
The occurrence of completely susceptible indicator E. coli isolates from the most important food‐producing animals (broilers, fattening turkeys, fattening pigs, bovines under 1 year of age) in a country is used as a key outcome indicator (KOICS) for the overall AMR situation in food‐producing animals. To account for differences in the relative size of food‐producing animal populations in a country, the KOICS was calculated as the weighted mean of the proportions of completely susceptible indicator E. coli isolates in each of the four animal populations monitored. For the calculation of the KOICS, the occurrence of CS in each animal population was weighted in relation to the relative size of the populations within a country using the ‘population correction unit’ (PCU). 23
KOICS was calculated using data reported in two consecutive years. KOIcs values were calculated from CS data on broilers and fattening turkeys reported in even‐numbered years and data on fattening pigs (pigs) and bovines under 1 year of age (calves) reported in the immediately preceding/following odd‐numbered years. CS data on broilers and pigs were included in the calculation for each country, while CS data on calves and turkeys were included in the calculation only in those countries reporting such data.
Marked variations in KOICS were observed among the 28 countries reporting consistently over the study period (Figure 39). In 2020–2021, levels of KOICS were < 20% in 10 countries, 20–40% in 12 countries, 40–60% in four countries, 60–80% in one country (Sweden) and >80% in three countries (Finland, Iceland, Norway). The lowest KOICS were generally observed in countries in Eastern and Southern Europe and the highest in countries in Northern Europe. KOICS has been stable at a high level over the period in some countries and in others at a low level. Statistically significant increasing trends in KOICS were registered in 17 countries and decreasing trends in three countries.
Figure 39.
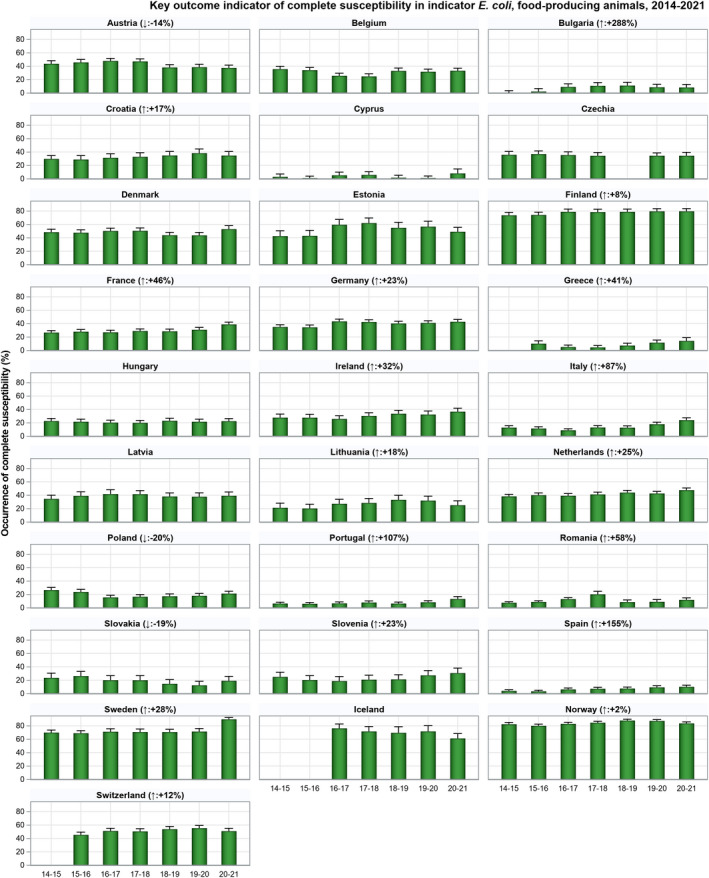
- (↓)/(↑): indicates statistically significant decreasing/increasing trends over the 2014–2021 period. Rates of change are given for statistically significant trends.
4.4. Discussion
Studying AMR in commensal indicator E. coli from the caecal contents of healthy food‐producing animals domestically produced provides information on the reservoirs of resistant bacteria that could potentially be transferred between animals and humans. Such monitoring is therefore relevant for both animal and public health. AMR exhibited by indicator E. coli is likely to depend on several factors, such as selective pressure from using antimicrobials in food‐producing animals, co‐selection of bacteria with multiple resistance, clonal spread of resistant bacteria and dissemination of genetic elements, such as plasmids, between bacteria.
Representative monitoring
The data on AMR in indicator E coli used in the present report were collected over the years 2014–2021 in accordance with Commission Implementing Decision (EU) 2013/652 (up until December 2020) and the replacement legislation, Commission Implementing Decision (EU) 2020/1729 which came into force on 1 January 2021. The new legislation enlarged the scope of the monitoring, with the inclusion of imported fresh meat from third countries, the addition of a new substance (amikacin) to the harmonised testing panel and the option for MSs to perform WGS as an alternative to the phenotypic testing in presumptive ESBL‐, AmpC‐ or CP‐producing E. coli. The AMR data are harmonised with respect to representative sampling design, laboratory methodologies, reporting and interpretation of resistance. In addition, as AMR data on indicator E. coli from pigs (2021) and broilers (2020) were reported by nearly all MSs and those from calves (11 MSs in 2021) and turkeys (11 MSs in 2020) were submitted by those MSs which are the main producers of meat derived thereof in the EU, AMR data can be considered representative.
General observations
At the MS‐group level, resistance to ampicillin, sulfamethoxazole, trimethoprim, and tetracycline was generally common in indicator E. coli and reported by most MSs at high or very high levels for all animal populations. Median levels of ampicillin resistance were very high in broilers and turkeys and high in pigs and calves. For sulfamethoxazole and trimethoprim, median levels were high in all four animal populations with the exception of calves, where the median level of trimethoprim resistance was moderate. In poultry, resistance to ciprofloxacin and nalidixic acid was also common, and several MSs reported very high or extremely high levels in both broilers and turkeys. In contrast, in pigs and calves, ciprofloxacin resistance was typically observed at moderate levels in most countries, with a few notable exceptions where resistance was high. In E. coli isolates from imported meat, very few isolates were observed to be resistant to any of the above‐mentioned substances. The frequent occurrence of resistance of isolates from animal origins to these substances likely reflects the widespread past and present use of these antimicrobials in food‐producing animals in a number of MSs. The observed differences between animal species likely reflect a diversity in the quantity of antimicrobials used in the different animal populations, but possibly also the mode of administration. In poultry, flock treatment is almost exclusively practised, whereas pigs and calves in some countries are typically treated individually.
Notable spatial differences were observed in the occurrence of resistance to most antimicrobials as well as in the occurrence of MDR, complete susceptibility and for the KOICS. Regarding pigs and broilers, the situation was generally more favourable in Northern Europe compared with Southern and Eastern Europe. Data on turkeys in the main producing MSs indicate a similar spatial distribution as that for pigs and broilers. In calves, the picture was more complex, and although the most favourable situation was registered in the Nordic countries (Norway, Denmark, Sweden), countries in Southern (Portugal, Romania) and Central Europe (Switzerland) also reported favourable situations in comparison to neighbouring countries in these regions.
Resistance to highest‐priority critically important antimicrobials (hpCIA)
Of the antimicrobials tested in the mandatory monitoring of indicator E. coli from caecal contents and imported fresh meat, ciprofloxacin (fluoroquinolones), cefotaxime and ceftazidime (third‐generation cephalosporins), colistin (polymyxin E) and azithromycin (macrolides) are categorised by the WHO as hpCIA (WHO, 2019). Bacteria resistant to these antimicrobials in food‐producing animals and derived meat is therefore of particular interest due to the risk of spread to humans along the food chain.
At the EU level, there were no major differences in occurrence of resistance to gentamicin, cefotaxime, ceftazidime, meropenem, tigecycline, azithromycin and colistin between the four animal populations monitored. Median levels were rare, very low, or low in all four categories, although individual countries reported considerably higher levels for some antimicrobials in some animal populations. Median levels of phenotypic resistance to third‐generation cephalosporins (cefotaxime and ceftazidime) at the EU group level were overall low in calves, broilers, and turkeys and very low in pigs. The highest level of resistance reported to third‐generation cephalosporins in each animal category was 5.5% in pigs, 4.1% in calves, 7.1% in broilers, and 7.4% in turkeys. In imported fresh meat, resistance to third‐generation cephalosporins was not reported in pork and only 1 isolate in beef. These findings relate to E. coli which are isolated using non‐selective culture methods. Within the mandatory monitoring, samples of caecal contents and fresh meat are also cultured on selective media to specifically detect the presence of E. coli resistant to third‐generation cephalosporins. The results of these analyses are presented in Chapter Error! Reference source not found.
Ciprofloxacin and nalidixic acid resistance in isolates from pigs and calves were recorded at low median levels at the EU level. In contrast, median levels of ciprofloxacin and nalidixic acid resistance were very high in broilers and high in turkeys. At the EU level, there were decreasing trends in resistance to ciprofloxacin in E. coli isolates from broilers and turkeys. Notably, a substantial proportion of isolates from all animal populations were resistant to ciprofloxacin but not to nalidixic acid, a resistance pattern which generally indicates the presence of transmissible genes mediating quinolone resistance. For isolates from imported fresh meat, one isolate from pig meat was observed to be resistant to ciprofloxacin, and two isolates from bovine meat.
Combined microbiological resistance to both ciprofloxacin and third‐generation cephalosporins was observed in only 96 of the 13,244 E. coli isolates from animal origins tested in 2020 and 2021, with 40 of these isolates demonstrating clinical resistance to both substances. The levels of microbiological co‐resistance were slightly higher in broilers (1.0%) and turkeys (1.0%) than in pigs (0.4%) and calves (0.6%). A single isolate from bovine meat was observed to have both microbiological and clinical resistance to ciprofloxacin and third‐generation cephalosporins.
Median levels of azithromycin resistance in all reporting countries were very low in calves and turkeys and low in pigs and broilers. Most countries reported no azithromycin resistance or single isolates only, but a few countries reported moderate levels, up to 9.1% for pigs, 9.4% for calves and 11.3% for broilers, and high level for turkeys, 22.6 %. A single isolate from imported bovine meat was resistant to azithromycin. Azithromycin is an azalide antimicrobial, a subgroup of the macrolides, not used in animals. Possibly, selection pressure exerted using other related macrolides, e.g., gamithromycin, in food‐producing animals may have favoured the emergence of azithromycin resistance.
Altogether only 142 of the 13,244 isolates tested in 2020 and 2021 showed phenotypic resistance to colistin. Median levels of colistin resistance in the EU group were rare for pigs and broilers, very low in calves and low in turkeys, although much higher levels were reported in individual countries. There was no colistin resistance reported in E. coli isolates from imported meat origins.
Of the 13,244 indicator E. coli isolates from pigs, calves, broilers, and turkeys phenotypically tested in 2020 and 2021, resistance to carbapenems (meropenem) was not detected. Similarly, meropenem resistance was not detected in the limited number of E. coli isolates derived from imported pig and bovine meats. Carbapenem resistance appears infrequent in commensal E. coli from these food‐producing animals in Europe. Still, further information on specific monitoring of carbapenem resistance is found in Chapter 5.
Complete susceptibility and multidrug resistance in all reporting countries
Considering all reporting countries, median levels of E. coli isolates susceptible to all antimicrobial classes tested were lower in broilers (24.4%) and turkeys (27.7%) than in pigs (41.8%) and calves (62.8%). Conversely, MDR isolates were more common in broilers (median 37.7%) and turkeys (median 47.6%) than in pigs (median 28.8%) and calves (median 18.8%). In all four animal populations, there were marked differences in levels of CS, as well as in MDR between countries. Generally, completely susceptible isolates from pigs, broilers, and turkeys were more common in Northern than in Southern and Eastern Europe, whereas the converse situation was observed for MDR. For calves, there was no obvious spatial pattern, and a favourable situation was reported in the Nordic countries (Norway, Denmark, Sweden) as well as in countries in southern Europe (Portugal, Romania).
Tetracycline, ampicillin, sulfamethoxazole, and trimethoprim were the antimicrobials most often represented in the patterns of MDR‐isolates, often in combination with other substances. Many of the MDR isolates from pigs and calves were resistant to all these antimicrobials, and they were also common in MDR‐isolates from broilers and turkeys. Additionally, quinolone resistance was common in MDR‐isolates from broilers (75.9%) and turkeys (73.8%) but less common in isolates from pigs (17%) and calves (27.8%). The frequent occurrence of these substances as a core component of MDR patterns in E. coli from poultry likely reflects an extensive usage in several countries over many years and that the genes conferring resistance to these substances often are linked on mobile genetic elements, resulting in co‐selection.
Key outcome indicator of complete susceptibility
An abundant and ubiquitous commensal bacterial species, E. coli, has been selected as a reporting organism because it is considered more relevant in representing the overall AMR situation, including transmissible AMR genes, than less abundant zoonotic bacterial species. The assumption underlying the choice of KOICS, as indicator, is that E. coli that is rarely, if ever, exposed to antimicrobials will tend to be fully susceptible (Martinez, 2014). As KOICS accounts for differences in the relative size of food animal populations in a country, it is relevant in the overall assessment of risks related to AMR in food‐producing animals. Marked variations in KOICS were registered from < 20% in ten MSs to > 80% in three countries (Norway, Finland, Iceland). To fully appreciate the situation within a country, the evaluation of KOICS should be complemented with data on resistance and CS available at the level of each animal population monitored so that any positive or negative trends occurring in one animal population of small relative size may not go unnoticed. The KOICS can be used to assess the development of AMR in relation to the total use of antimicrobials in food‐producing animals (Queenan et al., 2016; ECDC, EFSA, and EMA, 2017). Therefore, it is to be expected that a reduction in the use of antimicrobials in food‐producing animals would result in a noticeable improvement in this indicator.
Temporal trends in resistance
Overall, in several countries, there appear to be statistically significant trends toward reduction of resistance in indicator E. coli, notably in broilers and turkeys. Considering data from pigs and calves in 2021 and countries evaluated, there were 53 decreasing and 23 increasing trends in resistance to ampicillin, ciprofloxacin, cefotaxime, and tetracycline in the period 2009–2021. For poultry data in 2020, there were 89 decreasing and 24 increasing trends in resistance to the same four substances in the period 2009–2021. An improved situation was most pronounced in poultry, and in the EU group, there were significant decreases in resistance to ampicillin, ciprofloxacin, cefotaxime, tetracycline and colistin in both broilers and turkeys. For several antimicrobials, there are statistically significant associations between the use of antimicrobials in food‐producing animals and the occurrence of resistance in indicator E. coli from these animals (ECDC, EFSA, and EMA, 2021). The positive trends in several countries are, therefore, possibly due to the overall decline in sales of antimicrobials for use in animals since 2011, as documented in the ESVAC report (EMA, 2021).
For trends related to colistin resistance, there were four decreasing and no increasing trends between 2014 and 2021 for pigs and calves. While there were three decreasing and two increasing trends for broilers and no trends for turkeys for 2014–2020. As documented in the recent JIACRA III report (ECDC, EFSA, and EMA, 2021), there is a statistically significant association between consumption of polymyxins (colistin) in food‐producing animals and occurrence of colistin resistance in intestinal E. coli from these animals. The high occurrence of resistance in some animal populations in individual countries indicates large differences in the usage of colistin in Europe, which also was documented in the ESVAC report (EMA, 2021). However, at the EU group level, there were statistically significant decreasing trends in colistin resistance in isolates from broilers and calves. The decrease in resistance for broilers and calves is in accord with the 69.8% decrease in sales of polymyxins for food‐producing animals in the EU in the period 2011–2018, as reported in the ESVAC report (EMA, 2021). This shows that measures taken in individual countries to reduce the use of colistin, and thereby occurrence of resistance, are effective.
For levels of CS and considering all animal populations and countries evaluated, there were altogether 27 increasing and five decreasing trends in the period 2014–2021. As for resistance to individual antimicrobials, the improved situation was most pronounced in poultry and in the EU‐group there were increasing trends in CS for broilers, turkeys and pigs but no change for calves. There were significant increases in KOICS in 17 of the 28 reporting countries and trends towards decreasing values in four countries.
Statistically significant decreasing trends in resistance to ampicillin, ciprofloxacin, cefotaxime, tetracycline and colistin, as well as statistically significant trends towards higher levels of complete susceptibility and KOICS reveal progress towards reduced resistance in several countries and in the EU MS‐group as a whole. It should, however, be noted that in some countries, levels of resistance to individual antimicrobials are consistently stable at low levels, as well as CS and KOICS are at high levels, and major changes cannot be expected.
5. Extended‐spectrum β‐lactamase (ESBL)‐, AmpC‐ and/or carbapenemase (CP)‐producing Salmonella and Escherichia coli
All ESBL‐, AmpC‐ or CP‐producers prevalence and occurrence tables from the 2020 and 2021 monitoring, as well as the tables on occurrence of resistance (panel 1 and panel 2) mentioned in this chapter can be found in Annex D and the Salmonella spp., E. coli or ESBL Microsoft Excel® documents available on Zenodo at: https://doi.org/10.5281/zenodo.7544221. Materials and methods are included in the Appendix F.
5.1. Key findings
The occurrence of presumptive ESBL, AmpC or ESBL + AmpC‐producing Salmonella spp. was generally low in 2020.
Starting in 2021, MSs could use whole genome sequencing (WGS) as an alternative method to broth microdilution when carrying out the specific monitoring of ESBL‐/AmpC‐/CP‐producing E. coli and for the second panel of harmonised antimicrobials when further testing E. coli and Salmonella isolates showing resistance to cefotaxime or ceftazidime or meropenem. Four MSs opted to use this method: Italy, Germany, Finland and Czechia. Finland and Italy reported both phenotypic and genotypic results selecting the WGS results to be used in the analysis. Italy reported WGS data for the routine monitoring of Salmonella spp., E. coli and the specific monitoring of E. coli. Germany reported data for the routine and specific monitoring of ESBL‐/AmpC‐/CP‐producing E. coli, and Finland and Czechia also reported data for this specific monitoring.
In 2021, three E. coli isolates with the carbapenemase phenotype were detected in the specific monitoring of ESBL‐/AmpC‐/CP‐producing E. coli. Two isolates from bovine meat and one isolate from pig were detected by Hungary. Those isolates were confirmed as CP‐producers harbouring the bla NDM‐5 gene, responsible for the carbapenemase phenotype, by the EURL‐AR during the confirmatory testing exercise.
Furthermore, within the specific monitoring of CP‐producing microorganisms using selective media for CP‐producers, three isolates from bovine meat and one isolate from pig meat were reported by Hungary (presence of CP‐encoding genes pending of confirmation). Additionally, two isolates from fattening pigs were detected in Spain carrying the bla OXA‐48 gene.
WGS revealed additional 26 E. coli isolates from Italy (21 from pigs and five from bovine animals under 1 year of age) and three isolates from Czechia (all from fattening pigs) carrying CP‐encoding genes under the carbapenemase monitoring. These included bla OXA‐181 (4 isolates from calves and 20 from fattening pigs), bla OXA‐48 (one isolate from a fattening pig) and bla NDM‐5 (one isolate from a bovine animal) detected in the Italian isolates, and bla NDM‐5 (three isolates from fattening pigs) reported by Czechia.
WGS also revealed the presence of three different AmpC‐genes in E. coli isolates from the four MSs. These included: bla CMY‐113 detected in one isolate from a fattening pig in Italy. bla DHA‐1 detected in one, three and three isolates in a bovine animal, fattening pigs and pig meat, respectively, from Italy. bla CMY‐2 identified in pigs (24 isolates from Italy, 9 from Czechia two from Germany and 1 from Finland), in calves (seven isolates from Italy and one isolate from Germany), in bovine meat (seven isolates from Italy and three from Czechia) and pig meat (three isolates from Czechia and four from Italy).
A variety of ESBL‐encoding genes were identified in the four MSs reporting WGS. The most frequently reported gene in the majority of animal populations and meat categories was bla CTX‐M‐1, identified in 250 isolates from fattening pigs, 202 isolates from bovine animals under 1 year of age, 21 isolates from bovine meat and 33 isolates from pig meat. Followed by bla CTX‐M‐15 identified in 193 isolates from calves, 81 from fattening pigs, 8 from bovine meat and 6 from pig meat.
The prevalence of ESBL/AmpC‐producing E. coli in food‐producing animals is still high compared to previous years for some countries. Statistically significant decreasing trends are, however, observed in many countries for several animal categories, as well as at the level of the reporting MS‐group (plus the United Kingdom) for broilers and turkeys.
Statistically significant decreasing trends in the key outcome indicator of ESBL‐ and/or AmpC‐producing E. coli (KOIESC) were observed in 17 MSs and two reporting countries. In nine MSs and two reporting countries, a statistically significant increasing trend is registered, and in the remaining countries, no statistically significant trend is seen.
5.2. Data on ESBL‐, AmpC‐ and/or CP‐producing Salmonella and Escherichia coli addressed
The occurrence of ESBL‐, AmpC‐ or CP‐producing bacteria in the intestinal flora of animals is undesirable, as it might lead to the dissemination of resistant bacteria from animals and food to humans. Bacteria from animals with such resistance should also be considered as a reservoir of resistance genes which may be transferable to other bacteria including food‐borne zoonoses, such as Salmonella spp., further adding to the potential public health consequences. No statistically significant associations between resistance to third‐generation cephalosporins among indicator E. coli from animals and invasive E. coli from humans were observed in the latest JIACRA report (ECDC, EFSA, EMA, 2021). Nevertheless, the epidemiology of ESBL‐, AmpC‐ and CP‐producing E. coli is complex. Through continued improvement of monitoring system to study their prevalence in healthy animals and food derived thereof a fuller epidemiological picture can emerge.
Routine monitoring of ESBL‐/AmpC‐/CP‐producing indicator E. coli and Salmonella spp. and the specific monitoring of ESBL‐/AmpC‐/CP‐producing E. coli in caecal samples of animals and their meat products is mandatory. Monitoring in fattening pigs and bovine animals under 1 year of age, as well as pig meat and bovine meat gathered at retail was mandatory in 2021, whereas monitoring in caecal samples of broilers, fattening turkeys and fresh broiler meat sampled at retail was mandatory in 2020. From 2021, MSs were also able to submit fresh meat samples from pigs and bovine animals that were recovered at border control posts. In 2021, the specific monitoring was carried out by 11 MSs and two non‐MSs for bovine animals under 1 year, by 26 MSs, the United Kingdom (Northern Ireland) and three non‐MSs for fattening pigs, 23 MSs and one non‐MSs for meat from pigs, and by 26 MSs and one non‐MSs for meat from bovine animals under 1 year. In 2020, the monitoring was performed by 27 MSs and four non‐MSs for broilers and broiler meat, and 11 MSs and 2 non‐MS for fattening turkeys.
Until 2020, isolates were categorised as presumptive ESBL‐, AmpC‐ or CP‐producers based predominantly on the phenotype exhibited by the isolates. Phenotypic categorisation is performed in accordance with the criteria described in the Materials and Methods, Appendix F. Most, but not all, isolates resistant to extended spectrum cephalosporins (ESC) were therefore classified into these categories. However, not all classified isolates, in particular those exhibiting an AmpC phenotype, necessarily carry any transferable genes. From 2021, whole genome sequencing (WGS) was authorised as an alternative method to the phenotypic testing for E. coli and Salmonella isolates that show resistance to extended spectrum cephalosporins and carbapenems in the first panel of antimicrobials or for the specific monitoring of ESBL‐/AmpC‐/CP‐producing E. coli. Countries who identify ESBL‐, AmpC‐ or CP‐producers based on genotypic results using WGS no longer need to report the phenotypic results. In 2021, Czechia, Germany, Italy and Finland reported WGS results and selected those results for the analysis for the specific monitoring of E. coli. Genotypic results for samples isolated from bovine meat (Czechia, Germany and Italy), bovines (Germany and Italy), meat from pigs (Czechia, Germany and Italy) and pigs (Czechia, Germany, Finland and Italy). The reporting of WGS data will facilitate an understanding of the potential contribution of food‐producing animals and food derived thereof to the burden of AMR in humans (EFSA, 2019).
5.3. Food‐producing animals and derived meat: routine antimicrobial resistance monitoring. Presumptive ESBL/AmpC/CP producers and related WGS data
In 2020 and 2021, third‐generation cephalosporin resistance was identified in Salmonella spp. from broilers, fattening turkeys and laying hens, pigs and bovine animals under 1 year of age, and from carcases (meat) of broilers, as well as in indicator E. coli isolates from broiler meat, broilers, turkey meat, fattening turkeys, pig meat, fattening pigs and bovine meat and animals under 1 year of age, within the framework of the routine monitoring. 24 Some samples collected from fattening pigs, bovines under 1 year of age and their derived meat products in 2021 were subjected to whole genome sequencing according to the updated legislation.
ESC resistance and ESBL/AmpC/CP phenotypes and genotypes in Salmonella spp.
The proportion of ESC‐resistant Salmonella spp. isolates (tested with panel 2) collected within the routine monitoring was generally very low or low in 2020 and 2021 (ranging between 0.2% and 2.1% of the investigated isolates, depending on the animal population, see Annex C2 and C3). The occurrence of ESC‐resistant Salmonella isolates in a specific animal population can be greatly affected by the situation in certain countries regarding the prevalence of different Salmonella serovars. As an example, considering all reported isolates, about two‐thirds of the ESC‐R Salmonella isolates from broilers derived from one single MS in 2020 (see chapter 2, Salmonella for further details). At the reporting MS‐group level, the occurrence of presumptive ESBL‐ and/or AmpC‐producing Salmonella spp. was 2.1% in broilers, 0.4% in turkeys, 0.4% in laying hens, 0.8% in fattening pigs and 1.3% in bovine animals under 1 year of age. Detailed data per country and matrix can be found in Annex D2 and D3.
Italy was the only country to report WGS results in Salmonella spp. isolates in 2021. One monophasic S. Typhimurium from fattening pigs harbouring the bla SHV‐12 gene and one S. Ngor isolate from bovine animals under 1 year of age presenting the bla CTX‐M‐3 were reported.
ESC resistance and ESBL/AmpC/CP phenotypes and genotypes in indicator E. coli
The proportion of ESC‐resistant indicator E. coli isolates (tested with panel 2) collected within the routine monitoring was generally low in 2020 and 2021 (ranging between 0.5% and 1.5% of the investigated isolates, depending on the animal population). Among the reporting MSs, the occurrence of ESC resistance varied from 0% to 5.9% in fattening pigs, from 0% to 4.1% in bovines under 1 year of age, from 0% to 7.1% in broilers and from 0% to 6.4% in fattening turkeys (see chapter 4, E. coli, for further details). When only considering the isolates of indicator E. coli with ESBL/AmpC‐production, similar variations in occurrences are observed. At the MS‐group level, the occurrence of presumptive ESBL, AmpC or ESBL + AmpC‐producers in indicator E. coli was 1.1% in broilers, 1.6% in turkeys, 0.9% in fattening pigs and 0.7% in bovine animals under 1 year of age. For all matrices, the ESBL phenotype was more frequent than the AmpC phenotype. Detailed data per matrix and country can be found in Annex D2 and D3.
Only, two MSs, Italy and Germany, reported ESBL genes identified in the routine monitoring of indicator E. coli from fattening pigs and bovine animals under 1 year of age. Germany reported bla CTX‐M‐1 (n = 3), bla CTX‐M‐32 (n = 1) and bla SHV‐12 (n = 1), in isolates from calves, while Italy reported bla SHV‐12 in an isolate from a pig and bla CTX‐M in seven isolates from bovine animals under 1 year of age.
5.4. Food‐producing animals and derived meat: specific monitoring of presumptive ESBL/AmpC‐producing E. coli and related WGS data
5.4.1. Prevalence and occurrence of presumptive ESBL/AmpC/CP producers
The specific monitoring 25 of ESBL/AmpC/CP‐producers employs culture of samples on selective media (containing cefotaxime at 1 mg/L, as recommended by EUCAST), which can detect very low numbers of resistant isolates present within a sample. The prevalence of presumptive ESBL or AmpC‐producing and genotypic results for E. coli for all matrices tested in 2020 and 2021 is shown in Figure 41. Detailed prevalence and occurrence data per country and matrix can be found in Annex D2 and D3.
Figure 41.
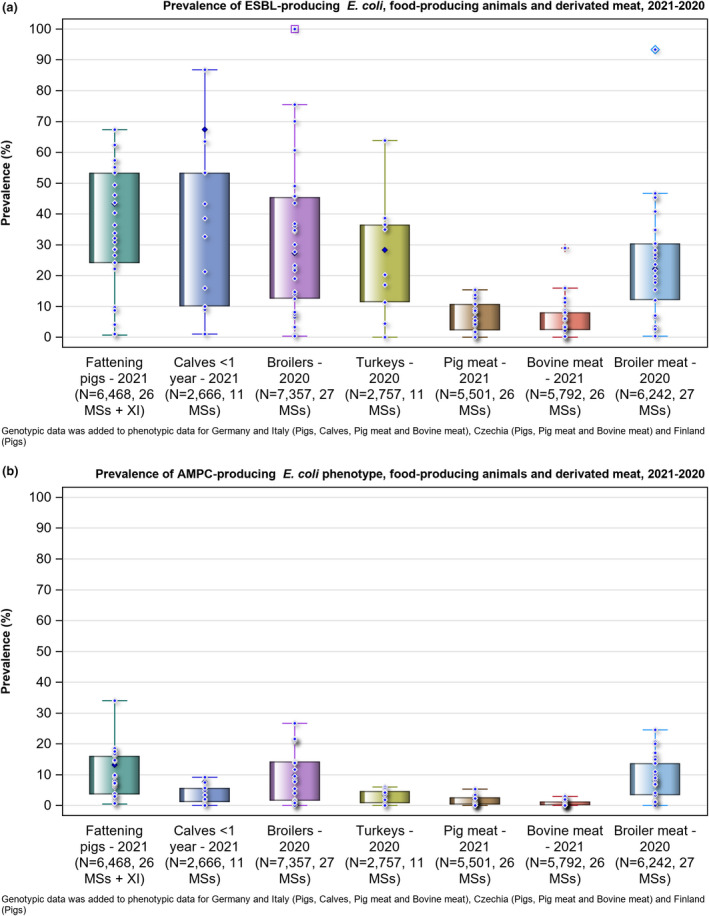
- N: number of samples tested; Diamond with white outline is the data (one data point per country); Diamond with black outline is Total EU. Outliers (> 1.5 IQR from 75th percentile) are spotted using a different symbol for each matrix (for example square for Pig meat 2021)
Regarding food‐producing animals, marked variations in the prevalence of presumptive E. coli ESBL and/or AmpC‐producers 26 were observed between the MSs for the period 2020–2021, when considering MIC results, as it ranged from 8.3% (Sweden) to 77.1% (Spain) in fattening pigs, from 5.8% (Denmark) to 59.1% (Belgium) in bovine animals under 1 year of age, from 0.3% (Finland) to 96.6% (Slovakia) in broilers and from 0% (Sweden) to 70.4% (Spain) in fattening turkeys (Annex D2 and D3). Important differences among the reporting countries were also evident when assessing the prevalence of ESBL or AmpC producers separately (Annex D2 and D3). The prevalence of ESBL and/or AmpC producers based on genotypic data also varied in the MSs that selected WGS instead of phenotypic results for the analysis in 2021. These results ranged from 64.2% (Germany) to 90.3% (Italy) in calves, and between 6.5% (Finland) and 80.7% (Italy) in fattening pigs.
Regarding meat, the prevalence of presumptive E. coli ESBL and/or AmpC‐producers 23 in meat varied markedly between the MSs, ranging from 0.3% (Finland) to 96.7% (Malta) in broiler meat, from 0% (Cyprus, Finland and Sweden) to 90.5% (Malta) for pig meat and from 0% (Finland) to 30.7%% (Hungary) for bovine meat at retail (Annex D2 and D3). The differences among reporting countries were also evident when the prevalence of ESBL or AmpC producers was considered separately (Annex D2 and D3). The prevalence of ESBL and/or AmpC producers based on genotypic data did not vary greatly in the MSs that performed WGS instead of phenotypic testing in 2021. These results ranged from 2.2% (Germany) to 7.4% (Czechia) in bovine meat, and 4.9%(Germany) to 8.2% (Czechia) in pig meat (Annex D3).
WGS‐based ESBL, AmpC and/or CP results.
Four MSs provided WGS data on ESBL and AmpC genes identified in the specific monitoring of ESBL‐/AmpC‐/CP‐producing E. coli isolates. WGS results were reported for isolates from fattening pigs (243 isolates in Italy, 164 by Germany, 152 by Czechia and 20 by Finland), bovines under 1 year of age (280 isolates by Italy and 193 by Germany), bovine meat (13 isolates by Italy, 10 by Germany and 22 by Czechia) and pig meat (23 isolates by Italy, 23 by Germany and 24 by Czechia) in 2021. The majority of the genes identified encoded for ESBLs, followed by AmpC genes. This is in line with the phenotypic findings, where the number of presumptive ESBL‐producing isolates largely outnumbered the AmpC‐producing E. coli isolates in all animal and food groups. Generally, ESBL genes were more commonly identified in samples from animals compared to samples from meat. A summary of CP‐ producers that were identified in 2020 and 2021 is available in Section 5.5.
ESBL genes were reported by four MSs (Czechia, Germany, Finland and Italy) (Table H.1, Appendix H; Figure 40). The most frequently reported gene in the majority of animal populations and meat categories was bla CTX‐M‐1. This gene was reported in 92pig isolates from Italy (37.9%, N = 243), 94 pig isolates from Germany (57.3%, N = 164), and 64 pig isolates from Czechia (42.1%, N = 152). This gene was also identified in 99 calf isolates from Italy (35.4%, N = 280) and 103 calf isolates from Germany (35.2%, N = 193). The second most commonly identified gene was bla CTX‐M‐15, which was detected in 133 bovine isolates from Italy (47.5%, N = 280) and 60 bovine isolates from Germany (31.1%, N = 193) as well as in 36 pig isolates from Italy (14.8%, N = 243), 25 pig isolates from Germany (15.2%, N = 164), 18 pig isolates from Czechia (31.6, N = 152) and 2 pig isolates from Finland (10%, N = 20)
AmpC genes and point mutations in the AmpC promoter region were also reported by the four MSs (Czechia, Germany, Finland and Italy) (Table H2, Appendix H; Figure 40). The most common AmpC gene identified across all MSs was bla CMY‐2.This gene was mainly detected in pigs, specifically, in 24 isolates from Italy, nine isolates from Czechia, two isolates from Germany and one isolate from Finland. However, the point mutations in the AmpC promotor were the mechanism most frequently detected in all MSs reporting WGS, except for Italy where this mechanism was not reported. In particular, the C‐42T mutation that is responsible for the AmpC phenotype was frequently detected in Czechia (in 46 isolates from pigs, three isolates from pig meat and two isolates from bovine meat), in Germany (22 isolates from pigs, three isolates from pig meat and one isolate from calves). Sixteen isolates from pigs in Finland had the C‐42T mutation and one had the T‐32A mutation.
Table H.1.
ESBL genes detected in E. coli isolates from the specific monitoring of ESBL‐/AmpC‐/CP‐ producers in food‐producing animals and meat derived thereof, by country, in 2021
| ESBL encoding genes | Bovines under 1 year old | Bovine meat | Fattening pigs | Pig meat | ||||
|---|---|---|---|---|---|---|---|---|
| E. coli | N | n | N | n | N | n | N | n |
| Italy * | ||||||||
| bla CTX‐M‐1 | 310 | 99 | 301 | 5 | 301 | 92 | 305 | 5 |
| bla CTX‐M‐2 | 310 | 1 | 301 | 0 | 301 | 0 | 305 | 0 |
| bla CTX‐M‐3 | 310 | 0 | 301 | 0 | 301 | 1 | 305 | 0 |
| bla CTX‐M‐8 | 310 | 0 | 301 | 0 | 301 | 4 | 305 | 1 |
| bla CTX‐M‐14 | 310 | 4 | 301 | 0 | 301 | 9 | 305 | 0 |
| bla CTX‐M‐15 | 310 | 133 | 301 | 5 | 301 | 36 | 305 | 2 |
| bla CTX‐M‐27 | 310 | 1 | 301 | 0 | 301 | 3 | 305 | 0 |
| bla CTX‐M‐32 | 310 | 1 | 301 | 0 | 301 | 3 | 305 | 1 |
| bla CTX‐M‐55 | 310 | 11 | 301 | 0 | 301 | 13 | 305 | 1 |
| bla CTX‐M‐65 | 310 | 1 | 301 | 0 | 301 | 3 | 305 | 1 |
| bla SHV‐12 | 310 | 11 | 301 | 1 | 301 | 20 | 305 | 4 |
| Germany | ||||||||
| bla CTX‐M‐1 | 299 | 103 | 418 | 4 | 382 | 94 | 466 | 16 |
| bla CTX‐M‐2 | 299 | 1 | 418 | 0 | 382 | 0 | 466 | 0 |
| bla CTX‐M‐3 | 299 | 2 | 418 | 1 | 382 | 2 | 466 | 0 |
| bla CTX‐M‐8 | 299 | 0 | 418 | 0 | 382 | 3 | 466 | 0 |
| bla CTX‐M‐9 | 299 | 0 | 418 | 0 | 382 | 1 | 466 | 0 |
| bla CTX‐M‐14 | 299 | 2 | 418 | 2 | 382 | 4 | 466 | 1 |
| bla CTX‐M‐15 | 299 | 60 | 418 | 2 | 382 | 25 | 466 | 2 |
| bla CTX‐M‐27 | 299 | 0 | 418 | 0 | 382 | 1 | 466 | 0 |
| bla CTX‐M‐32 | 299 | 6 | 418 | 0 | 382 | 2 | 466 | 0 |
| bla CTX‐M‐55 | 299 | 6 | 418 | 0 | 382 | 2 | 466 | 1 |
| bla CTX‐M‐65 | 299 | 4 | 418 | 0 | 382 | 1 | 466 | 0 |
| bla SHV‐12 | 299 | 5 | 418 | 0 | 382 | 2 | 466 | 0 |
| bla TEM‐52 | 299 | 1 | 418 | 0 | 382 | 2 | 466 | 0 |
| bla TEM‐207 | 299 | 1 | 418 | 0 | 382 | 0 | 466 | 0 |
| Czechia | ||||||||
| bla CTX‐M‐1 | – | – | 298 | 12 | 302 | 64 | 294 | 12 |
| bla CTX‐M‐3 | – | – | 298 | 1 | 302 | 1 | 294 | 0 |
| bla CTX‐M‐8 | – | – | 298 | 0 | 302 | 3 | 294 | 0 |
| bla CTX‐M‐14 | – | – | 298 | 1 | 302 | 1 | 294 | 1 |
| bla CTX‐M‐15 | – | – | 298 | 1 | 302 | 18 | 294 | 2 |
| bla CTX‐M‐27 | – | – | 298 | 0 | 302 | 5 | 294 | 0 |
| bla CTX‐M‐32 | – | – | 298 | 1 | 302 | 0 | 294 | 1 |
| bla CTX‐M‐55 | – | – | 298 | 1 | 302 | 3 | 294 | 1 |
| bla CTX‐M‐125 | – | – | 298 | 0 | 302 | 1 | 294 | 0 |
| bla SHV‐12 | – | – | 298 | 0 | 302 | 1 | 294 | 1 |
| bla TEM‐52 | – | – | 298 | 0 | 302 | 0 | 294 | 1 |
| bla TEM‐126 | – | – | 298 | 0 | 302 | 1 | 294 | 0 |
| Finland | ||||||||
| bla CTX‐M‐15 | – | – | 309 | 0 | 307 | 2 | 313 | 0 |
N = number of samples tested by each country; n = the number of isolates carrying the gene.
–: No data reported for this animal category or derived meat, by the MS.
Please note that Italy reported additional information only at family level (CTX‐M) for 7 isolates from bovines under 1 year of age and 4 isolates from fattening pigs. These isolates have not been included in the table.
Figure 40.
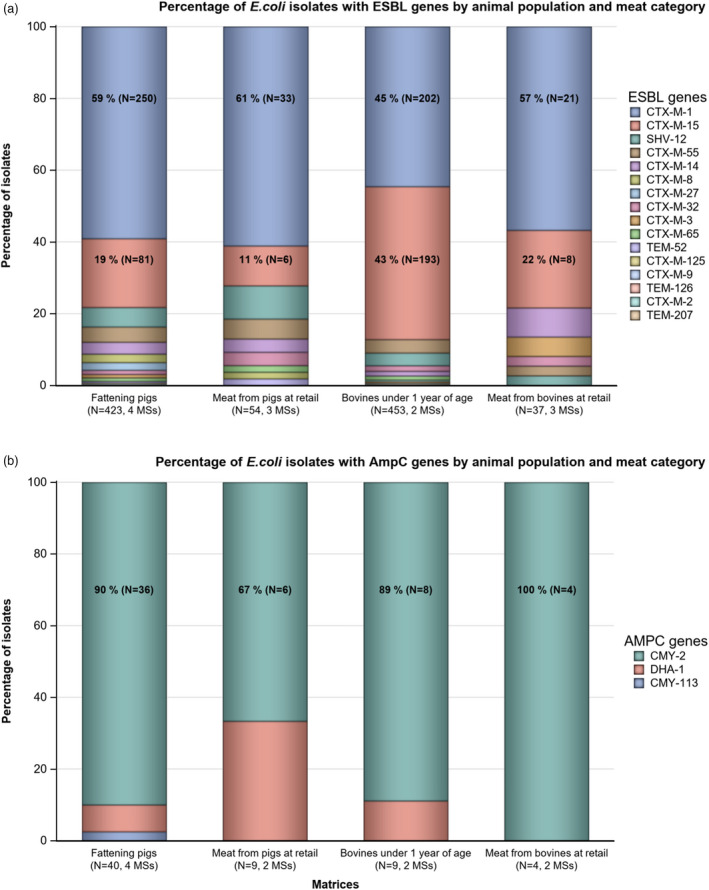
-
ESBL: extended‐spectrum β‐lactamase; AmpC: AmpC β‐lactamase; N: Total number of isolates harbouring an ESBL or AmpC gene.The breakdown of AmpC genes does not include point mutations in the AmpC promotor, only the genes listed in the legend.These figures incorporate data from countries that supplied WGS results to be used for analysis instead of MIC values. This excludes countries that provided MIC results as well as WGS results voluntarily.
Table H.2.
AmpC genes detected in E. coli isolates from the specific monitoring of ESBL‐/AmpC‐/CP‐ producers in food‐producing animals and meat derived thereof, by country, in 2021
| AmpC encoding genes | Bovines under 1 year old | Bovine meat | Fattening pigs | Pig meat | ||||
|---|---|---|---|---|---|---|---|---|
| E. coli | N | n | N | n | N | n | N | n |
| Italy* | ||||||||
| bla CMY‐2 | 310 | 7 | 301 | 1 | 301 | 26 | 305 | 4 |
| bla CMY‐113 | 310 | 0 | 301 | 0 | 301 | 1 | 305 | 0 |
| bla DHA‐1 | 310 | 1 | 301 | 0 | 301 | 3 | 305 | 3 |
| Germany | ||||||||
| bla CMY‐2 | 299 | 1 | 418 | 0 | 382 | 2 | 466 | 0 |
| Czechia | ||||||||
| bla CMY‐2 | – | – | 298 | 2 | 302 | 5 | 294 | 2 |
| Finland | ||||||||
| bla CMY‐2 | – | – | 309 | 0 | 307 | 1 | 313 | 0 |
N = the number of samples tested by each country; n = the number of isolates carrying the gene.
–: No data reported for this animal category or derived meat, by the MS.
*: Please, note that Italy reported the presence of an AmpC phenotype/genotype for 28 isolates from fattening pigs, three isolates from bovines under 1 year of age, one isolate from pig meat and one isolate from bovine meat. These isolates have not been included in the table.
5.4.2. Relative abundance (occurrence) of presumptive ESBL/AmpC producers
As only one isolate per sample is further investigated, the relative abundance of E. coli with an ESBL or AmpC phenotype when both are present in the sample influences the probability of detecting either phenotype. In the animal populations/food matrices monitored, at the reporting MS‐group level and in most of the countries, the detection of presumptive ESBL‐producing E. coli exceeded that of presumptive AmpC‐producing E. coli (Figures 41, 42, 43, 44, 45, 46; Annex D). Nevertheless, the occurrence of the different phenotypes varied considerably among the reporting MSs for certain matrices. After excluding the MSs with less than 10 presumptive isolates tested, the occurrence of the ESBL phenotype ranged from 12% (Sweden) to 100% (Bulgaria and Malta) in fattening pigs; from 29.4% (Sweden) to 89.6% (Belgium) in broilers; 16.7% (Denmark) to 97.6% (Croatia) in bovines under 1 year of age; and from 27.6% (Sweden) to 93.3% (Malta) in meat from broilers (Annex D2 and D3). For the other matrices, the difference in occurrence of the ESBL phenotype was less pronounced and ranged between 66.7% (Hungary) and 91.7% (Spain) in fattening turkeys; between 61.9% (Slovenia) and 92.6% (Austria) in meat from pigs and between 53.3% (Denmark) and 100% (Belgium and Romania) in meat from bovine animals. Bovine animals under 1 year of age and fattening turkeys are, however, only investigated by some MSs, as it is not mandatory for those with small production. Furthermore, the overall occurrence of presumptive ESBL/AmpC 27 producers in samples of meat from pigs and meat from bovines, as well as in pigs and bovines, is low.
Figure 42.
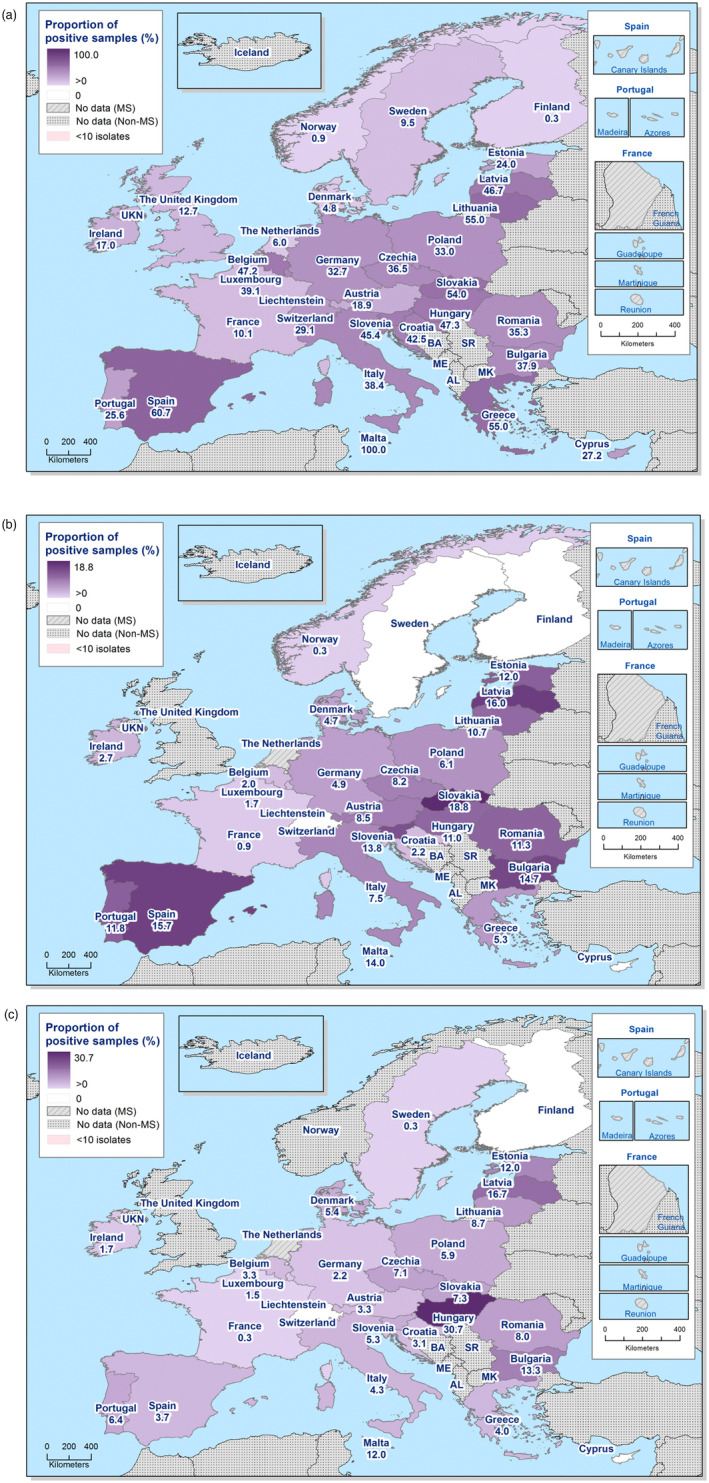
Spatial distribution of the prevalence of presumptive ESBL and/or AmpC‐producing E. coli from (a) meat from broilers in 2020, (b) meat from pigs in 2021 and (c) meat from bovines in 2021, EU MSs and non‐MSs, 2020/2021
Figure 43.
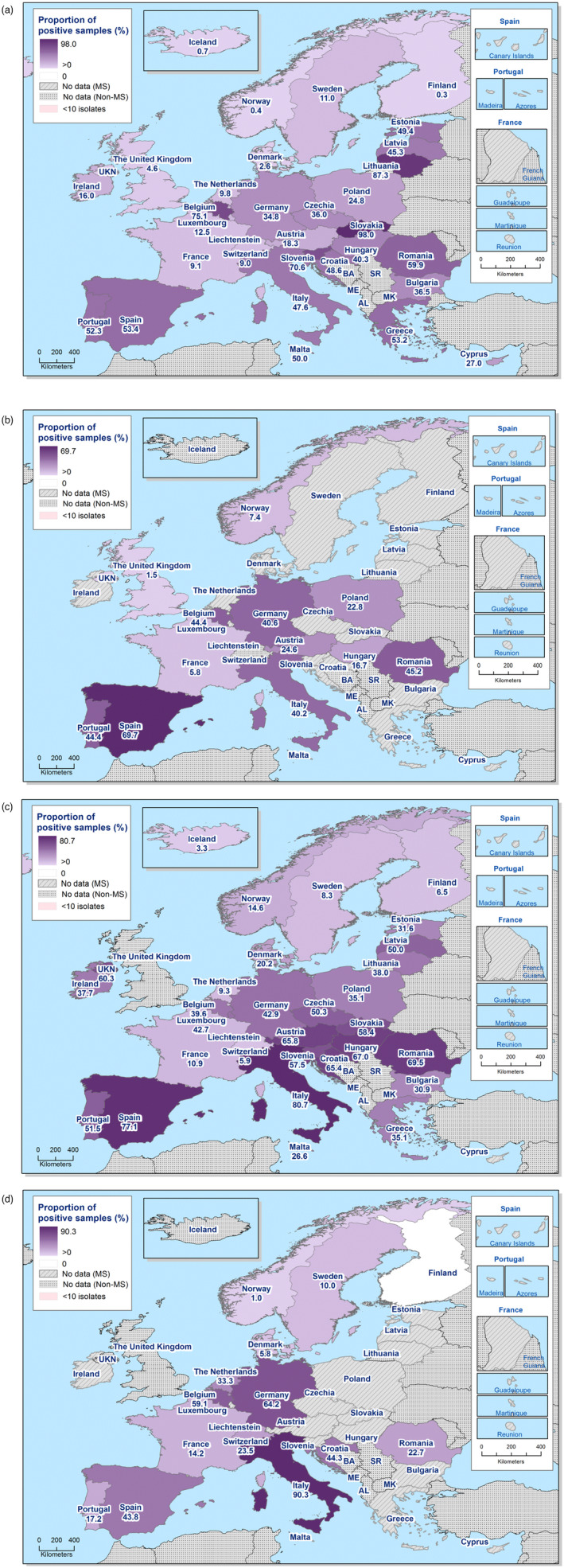
Spatial distribution of the prevalence of presumptive ESBL and/or AmpC‐producing E. coli from (a) broilers in 2020, (b) fattening turkeys in 2020, (c) fattening pigs in 2021 and (d) bovines under 1 year of age in 2021, EU MSs and non‐MSs, 2020/2021
Figure 44.
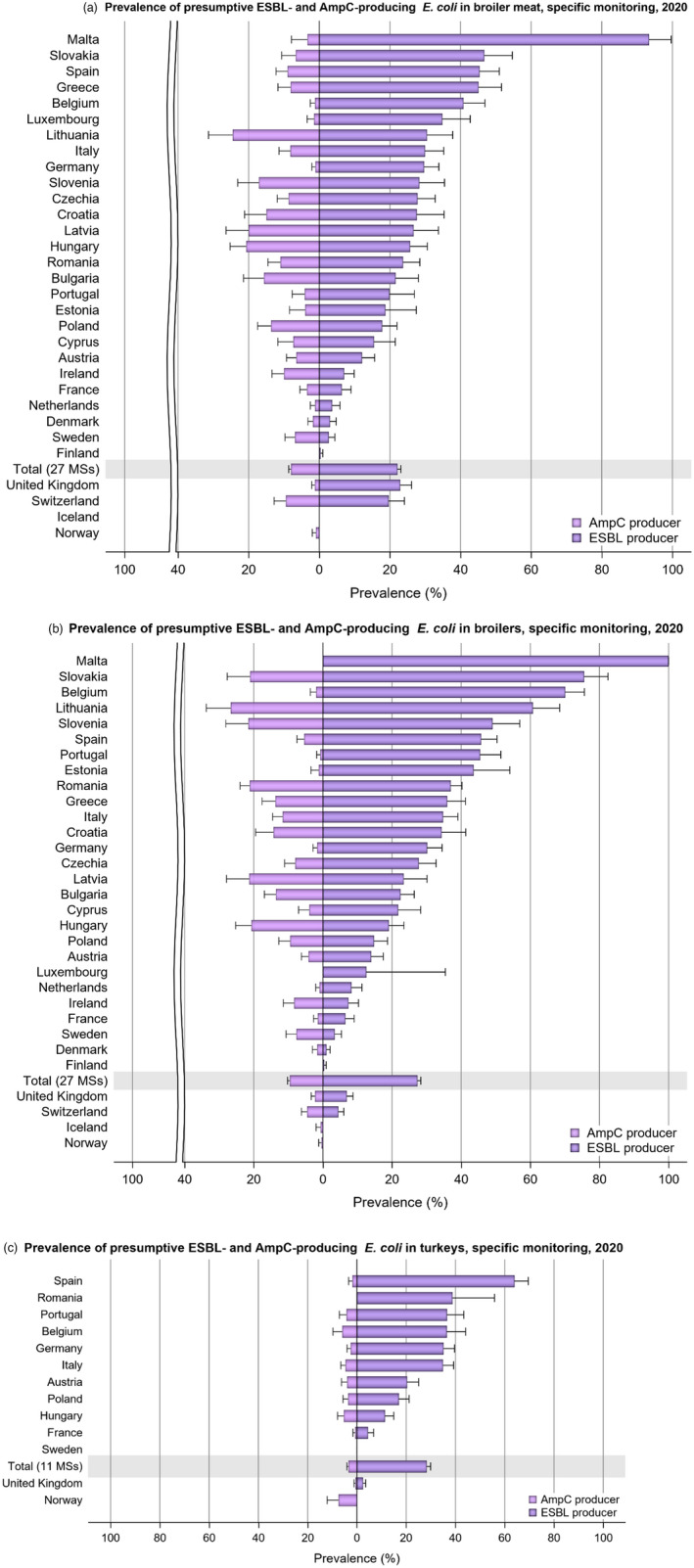
- The upper bounds of the 95% confidence interval of the prevalence of ESBL‐ and/or AmpC‐producing E. coli are also indicated.
Figure 45.
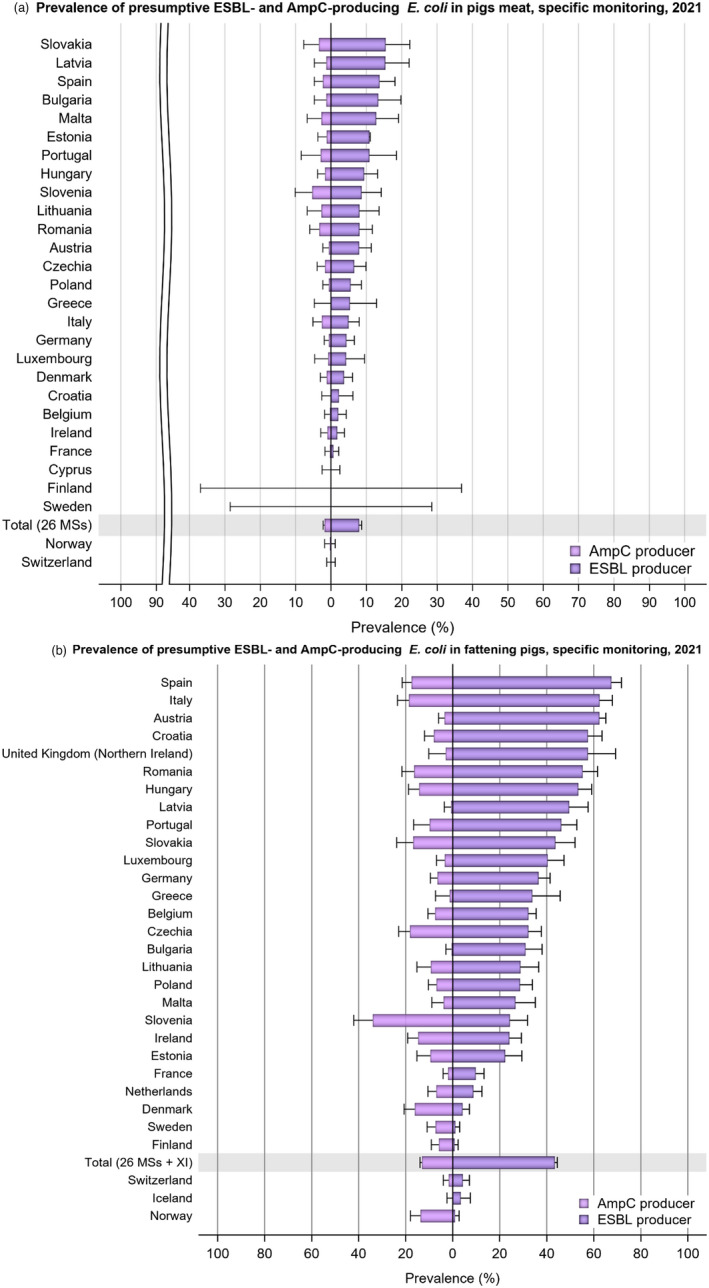
-
Prevalence was assessed using genotypic data reported by Czechia, Finland, Germany and Italy.The upper bounds of the 95% confidence interval of the prevalence of ESBL‐ and/or AmpC‐producing E. coli are also indicated. Please note the different scales used for the x‐axis in the subfigures to improve the visibility of the variations among countries.
Figure 46.
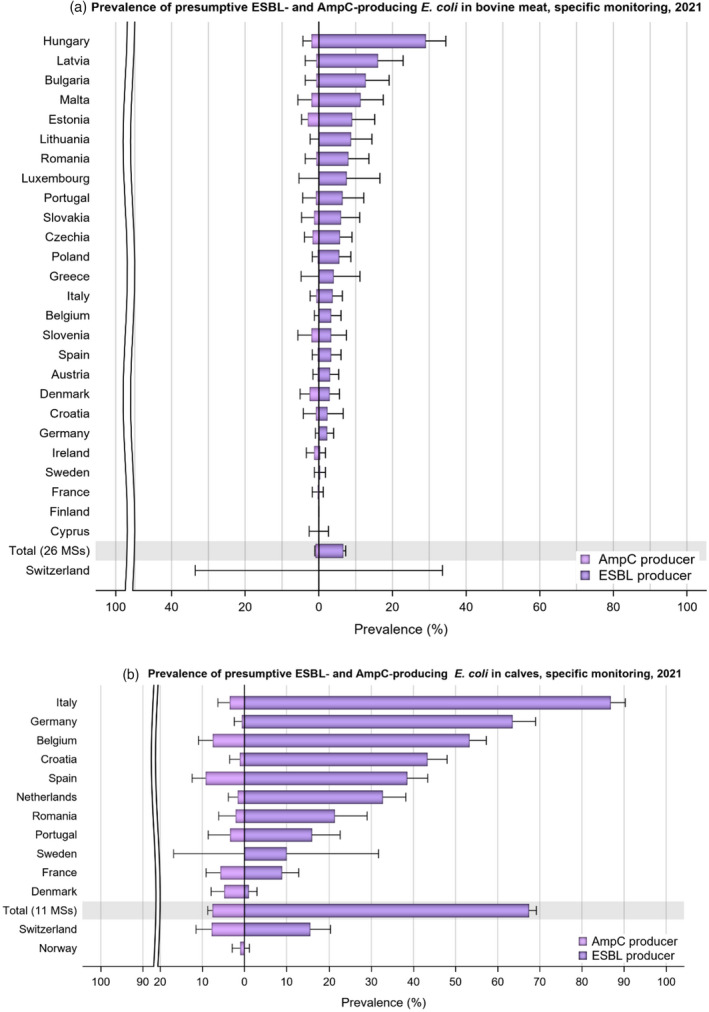
-
Prevalence was assessed using genotypic data reported by Czechia, Finland, Germany and Italy.The upper bounds of the 95% confidence interval of the prevalence of ESBL‐ and/or AmpC‐producing E. coli are also indicated. Please note the different scales used for the x‐axis in the subfigures to improve the visibility of the variations among countries.
5.4.3. Temporal trends in prevalence of presumptive ESBL/AmpC/CP producers
The temporal trend in the prevalence of presumptive ESBL‐producing E. coli in each separate animal population and meat category since the start of the harmonised mandatory monitoring is presented at both reporting country and MS‐group levels in Figures 47 and 48.
Figure 47.
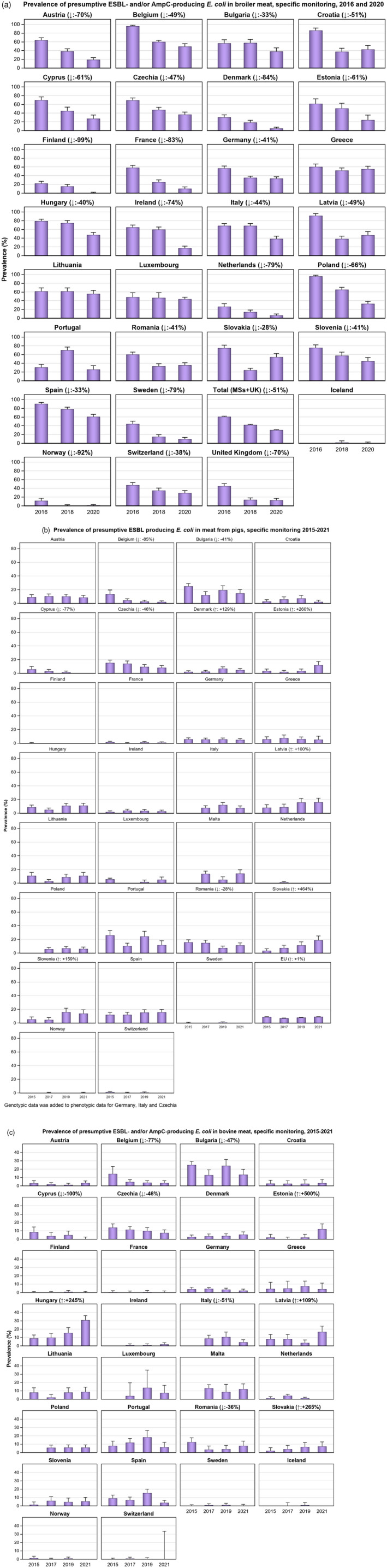
-
Prevalence was assessed using genotypic data reported by Czechia, Germany and Italy in 2021.The upper bounds of the 95% confidence interval of the prevalence of ESBL‐ and/or AmpC‐producing E. coli are also indicated.Prevalence was assessed using genotypic data reported by Czechia, Germany and Italy in 2021.
Figure 48.
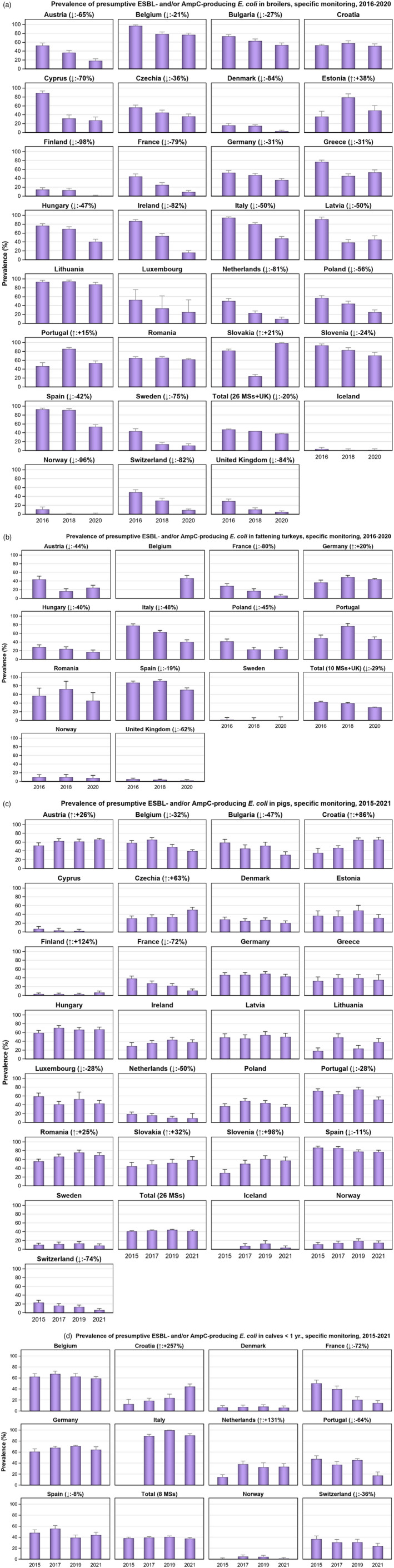
- The upper bounds of the 95% confidence interval of the prevalence of ESBL‐ and/or AmpC‐producing E. coli are also indicated.
The prevalence of presumptive ESBL‐producing E. coli at the MS‐group level in broilers and meat from broilers has gradually decreased to reach 38.0% in broilers and 30.6% in meat from broilers in 2020. Likewise, the prevalence in fattening turkeys has decreased from over 40% in 2016 to 30.7% in 2020. These decreasing trends are statistically significant and generally paralleled with statistically significant decreases observed in most reporting countries.
The prevalence of presumptive ESBL‐producing E. coli at the MS‐group level assessed in meat from pigs (7.9%) and meat from bovine animals (6.2%) in 2021 is comparable with that assessed in the same meat categories in the previous years. Statistically significant increases have been seen in 2021 for pig meat (Denmark, Estonia, Latvia, Slovakia and Slovenia) and bovine meat (Estonia, Hungary, Latvia and Slovakia).
Likewise, the prevalence of presumptive ESBL‐producing E. coli assessed in fattening pigs and bovine animals under 1 year of age in 2021 is comparable with that assessed in the previous years. Statistically significant decreasing trends are demonstrated for fattening pigs in seven reporting countries. For bovine animals under 1 year of age, statistically significant decreasing trends were identified in four reporting countries, namely France, Portugal, Spain and Switzerland.
A decreasing trend in prevalence is observed in many of the reporting countries, and certain MSs report a considerable improvement over the study period. This, however, is not uniform and some MSs have reported consistently high or very high prevalence over the study period. Detailed data on the prevalence assessed by country, animal population and meat category for 2020 and 2021 monitoring are presented in Figures 47 and 48, as well as in Annex D. For the 2015–2018 period, complementary data can be found in previous published reports.
5.4.4. Key outcome indicator of prevalence of ESBL and/or AmpC producers
The proportion of samples from broilers, fattening turkeys, fattening pigs and bovines under 1 year, weighted by PCU, that are identified as positive for presumptive ESBL and/or AmpC‐producing E. coli in the framework of the specific monitoring for ESBL‐/AmpC‐/CP‐producing E. coli according to Commission Implementing Decision 2020/1729/EU has been retained as a summary indicator.
One of the most medically relevant forms of AMR is mediated by plasmid‐encoded ESBL genes (EFSA BIOHAZ, 2011; Maslikowska et al., 2016). In contrast, the AmpC β‐lactamases in E. coli can be due to both upregulation and thus overexpression of chromosomally encoded existing ampC genes or to enzyme production by plasmid‐encoded transferable genes. There are many different enzymes that can destroy the β‐lactam ring (Pimenta et al., 2014), with a corresponding variety of genes and plasmids (Chong et al., 2011). The observation that ESBL‐carrying isolates from humans are often more related to chicken isolates than are susceptible isolates indicates that a proportion of ESBL and/or AmpC‐encoding isolates from agricultural settings may be of importance in human health‐care situations (Törneke et al., 2015). Plasmids carrying ESBL encoding genes can be transferred rapidly between E. coli strains (Händel et al., 2015) and selection can be driven by the use of many β‐lactam antimicrobials (Cavaco et al., 2008).
To account for differences in the relative size of food animal populations in a country, a weighted key outcome indicator of the prevalence of ESBL‐ and/or AmpC‐producing E. coli (KOIESC) was calculated. The indicator is the weighted mean of the prevalence of ESBL‐ and/or AmpC‐producing E. coli in each of the four animal populations monitored. For the calculation of the mean, the value for each population was weighted in relation to the relative size of the populations within a country using the ‘population correction unit’ (PCU). PCU is a technical unit of measurement used as an indicator of animal population size and was developed by the EMA, primarily to estimate sales of antimicrobials corrected by the animal population in individual countries. The data sources and methodology for the calculation of PCU are comprehensively described in EMA's report ‘Sales of veterinary antimicrobial agents in 31 European countries in 2019 and 2020’ (EMA, 2021). For each country, KOIESC was calculated using data reported for two consecutive years. Thus, values for 2014–2015 were calculated from data for broilers and fattening turkeys reported in 2014 and on data for fattening pigs and bovines under 1 year of age reported in 2015. Likewise, values for 2015–2016 were calculated from data reported for fattening pigs and bovines under 1 year of age in 2015 and on data for broilers and fattening turkeys reported in 2016, and so on.
A positive development manifested by a decreasing trend in the KOIESC is seen in 18 countries (17 MSs and 1 non‐MS). Still, in some of these countries, decreases are observed starting from very high or extremely high levels. For seven MSs, the trends in KOIESC are not statistically significant in any direction, over the period of study. Still, two MSs show a statistically significant increasing trend in their KOIESC which is at a very high level in 2021 (Figure 49).
Figure 49.
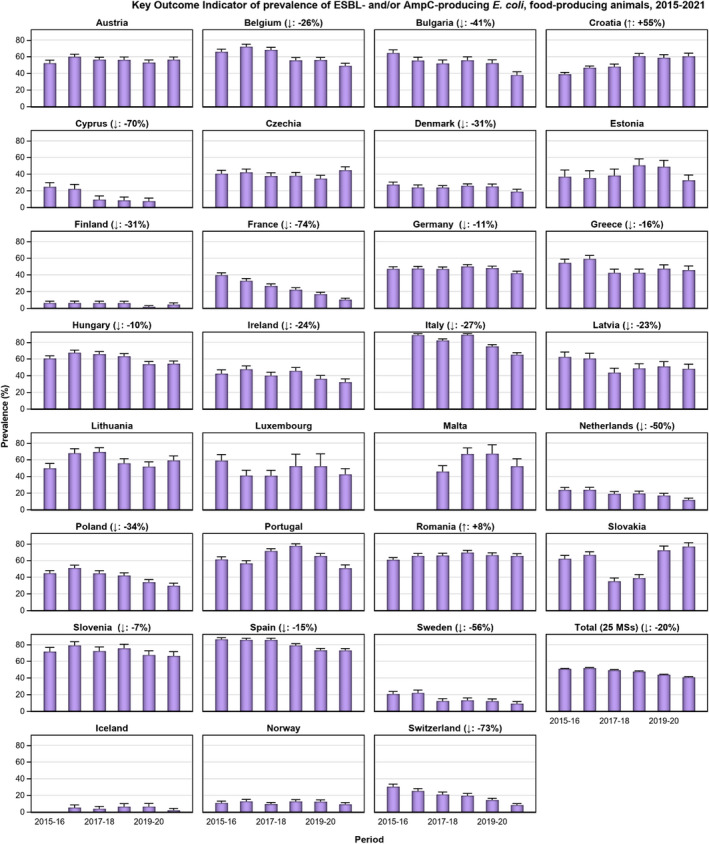
-
(↓)/(↑): indicates statistically significant decreasing/increasing trends over the 2014–2021 period.Rates of change are shown for the statistically significant decreasing/increasing trends observed.
5.4.5. Discussion
As the classification of the isolates as being presumptive ESBL‐, AmpC‐ or ESBL + AmpC‐producers is based on the phenotype observed, not all classified isolates (in particular those exhibiting an AmpC phenotype), necessarily carry any transferable genes. Molecular investigations would be needed to show whether the isolates carry any transferable genes encoding resistance to ESC. From 2021, WGS has been authorised as an alternative method to phenotypic testing, only four MSs reported and selected the molecular results for ESBL‐, AmpC‐ and CP‐producers to be used in the analysis. Italy, Germany, Czechia and Finland performed WGS on E. coli and Salmonella isolates from fattening pigs, bovines under 1 year old, as well as from bovine and pig meat. Italy and Finland performed both phenotypic and genotypic testing on E. coli isolates, although they indicated to use the genotypic results in the analysis of ESBL‐, AmpC‐ or ESBL + AmpC‐ producers. The combination of results reported by Finland, however, suggests that the prevalence of ESBL‐ and AmpC‐producing E. coli isolates is low in fattening pigs, while no ESBL and/or AmpC producers have been detected in pig and bovine meat samples.
In all monitored animal populations and meat categories, the ESBL‐producing phenotype was more common than the AmpC‐producing phenotype at the reporting MS‐group level and in most of the reporting countries. This was also the case in the molecular data where the vast majority of genes identified were ESBLs, followed by AmpC genes. The prevalence of the different phenotypes did, however, vary considerably among the MSs and in some countries, the AmpC phenotype was dominant, such as broiler populations in Hungary and Lithuania or turkeys from Norway. As only one isolate per sample is to be further investigated, the relative abundance of bacteria with an ESBL and/or AmpC phenotype present in the sample will influence the probability of detecting either phenotype.
Based on the WGS findings, bla CTX‐M‐1 and bla CTX‐M‐15 were the most commonly reported ESBL‐encoding genes and bla CMY‐2 was the most identified AmpC‐encoding gene. The CTX‐Ms are the largest groups of ESBLs, with bla CTX‐M‐15 becoming one of the predominant genotypes. bla CTX‐M‐1 has persisted in Europe suggesting the possible spread of epidemic plasmids (Bevan et al., 2017). bla CMY‐2 is one of the most prevalent AmpC genes and has been isolated in numerous species across the globe. Among others, a recent study in China detected bla CMY‐2 mediated resistance of food animal‐derived E. coli to third‐generation cephalosporins (Zheng et al., 2022).
Overall, the specific monitoring highlighted that presumptive ESBL‐, AmpC‐ or ESBL + AmpC‐producing E. coli were frequently observed in the caecal samples tested, which are representative of all investigated animal populations monitored. However, a statistically significant decrease in the prevalence of ESBL and/or AmpC‐producing E. coli has been observed in both broilers and turkeys over the period 2016–2020. Notably, since 2012, the off‐label use of extended spectrum cephalosporins in poultry has been discontinued (EMA/CVMP, 2018). This has likely contributed to the decreased occurrence of resistance in these species.
Similar to the caecal samples of healthy broilers collected at slaughter, a statistically significantly decreased prevalence of presumptive ESBL‐, AmpC‐ or ESBL + AmpC‐producing E. coli in broiler meat has been observed. The prevalence assessed in meat was statistically lower, but still comparable to, that observed in broilers.
Conversely, the prevalence of ESBL‐producing E. coli in meat of pigs and bovine animals was much lower than that assessed in fattening pigs and bovine animals under 1 year of age at slaughter. The range of the prevalence of these phenotypes in pig and bovine meat among the MSs also tended to be narrower than that observed in these animals at slaughter. The findings suggest that many of these animals are carrying ESBL‐producing E. coli in their intestinal content, but that the bacteria do not contaminate the carcases during the slaughter process; alternatively, that the bacteria contaminate the carcases but are somehow removed later in the process. This may be impacted by the differences in the slaughter process applied to broilers compared with those applied to pigs and bovine animals.
5.5. Monitoring of carbapenemase (CP)‐producing E. coli
5.5.1. Specific E. coli ESBL/AmpC/CP‐producers monitoring
The specific monitoring of ESBL/AmpC‐producing E. coli on selective media (including cefotaxime) enables the detection of isolates with some mechanisms of carbapenem resistance.
In 2021, Hungary detected the CP‐phenotype in an isolate from pig meat and two isolates from bovine meat collected at retail, although molecular data was not provided for these isolates. Those isolates were confirmed as CP‐producers harbouring the bla NDM‐5 gene, responsible for the carbapenemase phenotype, by the EURL‐AR during the confirmatory testing exercise. In addition, within the 2020 ESBL‐/AmpC‐ producers monitoring, Austria detected one isolate with a CP phenotype from broilers. This isolate harboured the metallo‐β‐lactamase resistance gene bla VIM‐1, as well as the β‐lactamase genes bla TEM‐1C and bla TEM‐1B (EFSA and ECDC, 2022).
5.5.2. Specific CP‐producers monitoring
In 2020 (EFSA and ECDC, 2022) and 2021, specific monitoring of CP‐producing microorganisms using selective media for CP‐producers, in accordance with a protocol developed by the EURL on AMR, 28 , 29 was performed by a number of countries (Annex D4; see Appendix F, Materials and methods). In the 2 years combined, 23 countries (20 MSs and 3 non‐MSs) investigated 5,089 samples from fattening pigs; 2,214 samples from bovines under 1 year of age; 6,088 samples from broilers; 2,250 samples from fattening turkeys, 4,843 samples of meat from pigs, 4,688 samples of meat from bovines and 4,456 samples of meat from broilers.
For 2020, the Netherlands also reported data on additional specific monitoring of CP‐producing E. coli in broilers, fattening pigs, bovines under 1 year, laying hens and dairy cows using a different isolation protocol. All these samples (n = 1,408) were negative (EFSA and ECDC, 2022).
In 2021, suspected CP‐producing E. coli isolates were detected in two samples from fattening pigs (Spain), three samples from bovine meat (Hungary) and one sample of meat from pigs (Hungary) (Annex D4) in the specific monitoring of CP‐producing E. coli (some of the isolates seems to proceed from the same samples positive in the specific E. coli ESBL/AmpC/CP‐producers monitoring, see Section 5.5.1 above). The isolates from fattening pigs reported by Spain carried the bla OXA‐48 gene. For the isolates reported by Hungary, the presence of CP‐encoding genes is pending of confirmation.
Only two out of the four MSs, which reported and selected WGS results for the analysis, detected CP resistance genes in 29 E. coli isolates from fattening pigs and bovine animals under 1 year of age (Czechia and Italy) (Figure 50; Appendix H, Table H.3). Among them, the CP gene bla OXA‐181 was identified in 20 E. coli isolates from fattening pigs and four isolates from bovines under 1 year of age from Italy; and bla OXA‐48 was identified in an isolate from a fattening pig in Italy; bla NDM‐5, was identified in three E. coli isolates from fattening pigs in Czechia and in an E. coli isolate from a bovine under 1 year of age in Italy.
Figure 50.
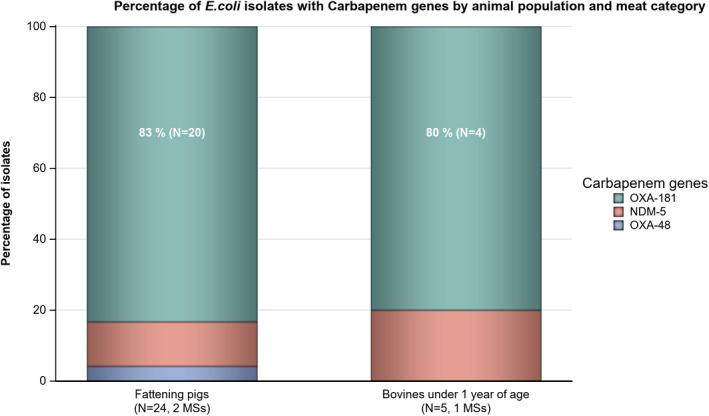
-
N = Total number of isolates harbouring a CP‐encoding gene.These figures incorporate data from countries that provided WGS results to be used for analysis instead of MIC values. This excludes countries that provided MIC results as well as WGS results voluntarily.
Table H.3.
CP‐encoding genes detected in E. coli isolates from the specific monitoring of CP‐ producers in food‐producing animals and meat derived thereof, by country, in 2021
| CP encoding genes | Bovines under 1 year of age | Fattening pigs | ||
|---|---|---|---|---|
| E. coli | N | n | N | n |
| Italy | ||||
| bla NDM‐5 | 310 | 1 | 301 | 0 |
| bla OXA‐181 | 310 | 4 | 301 | 20 |
| bla OXA‐48 | 310 | 0 | 301 | 1 |
| Czechia | ||||
| bla NDM‐5 | – | – | 302 | 3 |
N = the number of samples tested by each country; n = the number of isolates carrying the gene.
–: No data reported for this animal category, by the MS.
5.5.3. Discussion
Among all samples and isolates investigated within the harmonised monitoring in 2020 and 2021, by phenotypic methods, 14 E. coli with elevated MIC to meropenem were detected. Of these, four (one from broilers, one from pig meat, two from meat from bovines) where detected within the specific monitoring of ESBL/AmpC‐producing E. coli on selective media and 10 (three from broilers, one from fattening turkey, two from fattening pigs and one from pig meat, and three from bovine meat) within the specific monitoring of CP‐producing microorganisms using selective media for CP‐producers. Countries using WGS detected CP genes in 29 E. coli isolates (24 from fattening pigs, five from bovine animals under 1 year) within the specific CP‐producing E. coli monitoring.
Although the total number of suspected CP‐producing E. coli isolated within the monitoring is still low, there has been an increase in numbers compared with the previous years (EFSA and ECDC, 2022), probably also facilitated by the use of WGS.
The occurrence of CP‐producing E. coli among farm animals and meat derived thereof in several countries is of concern. Due to the public health importance of CP‐producing E. coli and/or Salmonella, both as pathogens and as vectors for resistance mechanisms, there is a need to follow up possible further developments in this area for farm animals and food derived thereof. WGS seems to have detected more CP‐producing E. coli isolates than phenotypic methods, even though only four MSs reported molecular data. WGS being authorised as an alternative method to phenotypic testing will hopefully strengthen the detection rates.
In 2021, a high variety of CP genes were detected in different countries: bla OXA‐48 in Spain (confirmed by the MSs) and Italy, in both countries isolates from fattening pigs. bla OXA‐181 in Italy, in isolates from fattening pigs and bovines (Carfora et al., 2022). bla NDM‐5 in Czechia, in isolates from fattening pigs, in Italy from a bovine isolate and Hungary (confirmed by the EURL‐AR) from pig and bovine meat isolates collected at retail. In 2020, bla VIM‐1 was detected in Austria from poultry. The CP‐encoding genes bla OXA‐181 and bla NDM‐5 were the most frequently reported in 2021. The gene bla OXA‐181 belongs to class D carbapenemases, and the first report of its isolation from porcine E. coli was in Italy (Pulss et al., 2017). Prior to which it was mainly identified in human isolates and rarely in animals. The gene bla NDM‐5 belongs to the New Delhi metallo‐beta‐lactamases (NDMs), which are a class of carbapenemase genes that have previously been identified in E. coli. This gene was previously isolated in E. coli isolates from dairy cows in Algeria, as well as in dogs and humans (Yaici et al., 2016). Based on nucleotide similarity of the plasmids containing CP genes and others identified in human animal sources, it has been suggested that specific antimicrobial resistance plasmids have been circulating among E. coli strains across vertebrate species barriers, which could increase the risk of dissemination of carbapenem resistance in animal reservoirs.
Apart from isolates detected within the harmonised monitoring in the EU (shown in this report, as well as in EFSA and ECDC, 2022; Diaconu et al., 2020; Garcia‐Graells et al., 2020; Bortolaia et al., 2021; Carfora et al., 2022), CP‐producing Enterobacterales has also been reported, not only in companion animals (Rincon‐Real et al., 2022), farm animals and food derived thereof but also from vegetables from many parts of the world including Europe (Zurfluh et al., 2015; Touati et al., 2017; Brouwer et al., 2018; Köck et al., 2018; Liu et al., 2018; Irrgang et al., 2019, 2020). In addition, a number of closely related but non identical plasmids carrying the carbapenem resistance gene bla VIM‐1 has been found in isolates from livestock in Germany (Pauly et al., 2021). Consequently, the concern of animals becoming a reservoir for CP‐producing Enterobacterales has been raised (Taggar et al., 2020). Carbapenems are not authorised for use in animals in the EU, and the spill‐over of resistant genes and/or bacteria from humans has been suggested as potential source of CP Enterobacteraceae in the food production (Irrgang et al., 2020). However, the spread of the same or related CP‐encoding genes in isolates from different farms in certain regions could point to horizontal/vertical transmission of these isolates within the food chain (Carfora et al., 2022). Furthermore, as CP‐producing Enterobacterales are probably still emerging among the investigated animal species in Europe, potential actions to preserve this situation can hopefully still be effective, ensuring that farm animals do not become an important source of such bacteria for humans.
6. Antimicrobial resistance in methicillin‐resistant Staphylococcus aureus (MRSA)
6.1. Key findings
The monitoring of MRSA in 2020 and 2021 provided useful information on the occurrence of MRSA in livestock and food. The situation continues to develop and evolve and there is a clear requirement for the continued monitoring and appropriate molecular characterisation of MRSA isolates recovered from livestock and food.
Molecular characterisation is necessary to fully evaluate the significance of MRSA isolates. There are limitations to the analyses which can be performed when spa‐typing is used as the only technique to characterise isolates. Isolates from the same spa‐type may have very divergent sources and characteristics. For the assessment of the risk for humans, determination of the production of the PVL toxin seems relevant as well as the presence of the immune evasion cluster.
Where typing data were available, most MRSA isolates were associated with spa‐types that are assigned to livestock associated (LA‐)MRSA in both reporting years. However, spa‐types associated with community acquired (CA‐) and hospital acquired (HA‐)MRSA were also reported, as well as mecC‐MRSA. The occasional detection of lineages of CA‐ and HA‐MRSA primarily associated with humans is not surprising, since the sporadic interchange of strains between humans and animals may be expected.
All spa‐types of clonal complex 398 and other clonal complexes reported in 2020/2021 in animals and food are provided in Tables 14 and 15 of the present chapter. Changes in the reported occurrence of different MRSA lineages may be assessed against this list in the future.
Isolates that could not be assigned to the clonal complex 398 were more frequent in isolates from food than in isolates from animals. This may point to contamination at slaughter or during processing with strains of non‐animal origin. Many of the observed types have however repeatedly been reported in animals making it difficult to assign them unequivocally to human sources.
An important observation from the 2021 monitoring was the detection of rifampicin resistance in dairy cows and bovine meat.
A relevant observation from the 2020 monitoring was the occurrence of a vancomycin‐resistant t011 isolate in meat from sheep. The isolate lacks the typical vancomycin resistance genes and it is likely, that the increased MIC of 4 mg/L was due to multiple point mutations as described in the literature.
Table 14.
spa‐types of CC398 and their detection in animals and food 2020/2021
| Spa‐type | Year | Animals (number of isolates) | Tot | Food (number of isolates) | Tot |
|---|---|---|---|---|---|
| t011 | 2021 | calves (65), dairy (10), cattle (2) | 77 | bovine meat (8), pig meat (24) | 32 |
| 2020 | broilers (2), turkeys (2) | 4 | broiler meat (4), meat from sheep (1) | 5 | |
| t034 | 2021 | calves (6), dairy cows (2) | 8 | Pig meat (26), bovine meat (5) | 31 |
| 2020 | 0 | broiler meat (4), meat from sheep (2) | 6 | ||
| t1451 | 2021 | Calves (1) | 1 | Bovine meat (1) | 1 |
| 2020 | 0 | Sheep meat (1) | 1 | ||
| t1456 | 2021 | Calves (1) | 1 | 0 | |
| t2346 | 2021 | Calves (1) | 1 | 0 | |
| t2370 | 2021 | Calves (1) | 1 | 0 | |
| t3423 | 2021 | Calves (1) | 1 | 0 | |
| t5210 | 2021 | Calves (1) | 1 | 0 | |
| t6228 | 2021 | Calves (1) | 1 | 0 | |
| t899* | 2021 | 0 | Bovine meat (1), pig meat (6) | 7 | |
| t2741 | 2021 | 0 | Pig meat (9) | 9 | |
| t4677 | 2021 | 0 | Pig meat (1) | 1 | |
| t2576 | 2021 | 0 | Pig meat (1) | 1 | |
| 2020 | Sheep meat (1) | 1 | |||
| t19979 | 2020 | 0 | Sheep meat (1) | 1 | |
| t1793 | 2021 | 0 | Pig meat (1) | 1 | |
| t9013 | 2021 | 0 | Pig meat (1) | 1 | |
| t571 | 2021 | 0 | Pig meat (1) | 1 |
Calves are bovine animals below 1 year of age.
t899 is sometimes also attributed to CC9 as it is a hybrid strain.
Table 15.
spa‐types of other clonal complexes and their occurrence in animals and food in 2020/2021
| spa‐type | Clonal complex (sequence type) | Year | Animals | Food | ||
|---|---|---|---|---|---|---|
| Population (number of isolates) | Tot | Matrix (number of isolates) | Tot | |||
| t002 | 5* | 2021 | 0 | Bovine meat (2) | 2 | |
| t008 | 8* | 2021 | 0 | Bovine meat (2) | 2 | |
| t037 | 8 | 2021 | Dairy cows (3), cattle (2) | 5 | 0 | |
| t095 | 45 | 2021 | 0 | Bovine meat (7), Pig meat (11) | 18 | |
| t174 | 1 | 2021 | 0 | Bovine meat (1) | 1 | |
| t223 | 22* | 2020 | 0 | Sheep meat (2) | 2 | |
| t311 | 5* | 2021 | 0 | Bovine meat (2) | 2 | |
| t386 | 1 | 2021 | Calves (1) | 1 | 0 | |
| t359 | 97* | 2021 | 0 | Bovine meat (1) | 1 | |
| t559 | 1* | 2021 | 0 | Bovine meat (1) | 1 | |
| t728 | 45 | 2021 | 0 | Pig meat (1) | 1 | |
| t843 | 130* | 2021 | 0 | Bovine meat (1) | 1 | |
| t1154 | 5 | 2020 | 0 | Sheep meat (1) | 1 | |
| t1346 | 8 | 2021 | 0 | Bovine meat (1) | 1 | |
| t1430 | 9* | 2021 | 0 | Bovine meat (1), pig meat (3) | 4 | |
| t2112 | 97* | 0 | Bovine meat (1) | 1 | ||
| t15010 | 97 | 2020 | 0 | Sheep meat (1) | 1 | |
The CC associated with the spa‐type is based on information from the literature and not from data reported by countries.
6.2. Data on MRSA addressed
Periodic monitoring of methicillin‐resistant Staphylococcus aureus (MRSA) in food‐producing animals and food allows for the identification of trends in the diffusion and evolution of potentially zoonotic MRSA in food‐producing and other animals. In conjunction with systematic surveillance of MRSA in humans, the transmission of MRSA from food‐producing animals to the human population may be analysed (EFSA, 2009a,b, 2012). To this end, in addition to determining the occurrence of MRSA in the different food chains, representative isolates should optimally be characterised with respect to their molecular subtype and AMR. The monitoring of MRSA in animals and food in Europe is voluntary and only a limited number of countries reported MRSA occurrence data in 2020 and 2021. Some countries additionally reported data on spa‐ and/or sequence types and/or antimicrobial susceptibility.
MRSA is commonly found on the skin and mucosa of humans and animals and can cause serious infections in both groups. Strains of MRSA can be divided into three broad categories: community‐associated (CA‐), healthcare‐associated (HA‐) and livestock‐associated (LA‐) MRSA. These categories differ in their epidemiology, although the separation between the types is not strict. HA‐MRSA and CA‐MRSA comprise strains that predominantly affect humans, and these strains are much less frequently reported from food‐producing animals. LA‐MRSA has been detected in most farm animal species including those covered by the antimicrobial resistance monitoring according to Decision 2020/1729/EU (2021 data) and Decision 2013/652/EU (2020 data).
Among humans, LA‐MRSA are predominantly carried by people with repeated occupational contact with colonised livestock. The proportion of MRSA carried by humans in the European Union that belong to livestock associated strains has been estimated to be small (3.9%); however, higher proportions were observed in five countries (Belgium, Denmark, the Netherlands, Slovenia and Spain) (Kinross et al., 2017). Although frequently detected in food, MRSA is generally not considered to be transmitted by food‐borne routes to humans, and detection often involves selective culture techniques, which may detect very low levels of contamination (Pauly et al., 2019).
Isolates of LA‐MRSA in Europe predominantly belong to clonal complex (CC) 398, although other livestock‐associated clonal lineages have been reported. Although the severity of LA‐MRSA infection in humans is usually less than those caused by other MRSA strains, there is still potential for the infections to become life threatening. Risk of transmission of LA‐MRSA in the hospital environment is considered less likely than with HA‐MRSA strains although public health surveillance in the Netherlands (2003–2014) and Denmark (1999–2011) detected distinct LA‐MRSA strains disseminating into the community, sometimes in the absence of livestock contact (Kinross et al., 2017).
A variant of the methicillin resistance gene mecA, termed mecC, was first identified in 2011 in MRSA from humans and cattle in Europe (García‐Álvarez et al., 2011; Shore et al., 2011). It has subsequently been detected in ruminants, pigs and companion animals, with reports also from wild animals (Paterson et al., 2014; Bengtsson et al., 2017). In hindsight, mecC MRSA isolates have been found in isolates dating back to the pre‐antibiotic era (Larsen et al., 2022). The mecC gene shares 70% identity with mecA at the DNA level (García‐Álvarez et al., 2011). Risk factors for mecC MRSA carriage in humans include contact to animals and the presence of an underlying disease (Lozano et al., 2020). mecC‐MRSA strains have been negative for Panton–Valentine leukocidin (PVL) toxin – a virulence factor typically associated with CA‐MRSA. However, some isolates have carried genes belonging to the immune evasion cluster (IEC) (Lozano et al., 2020). Carriage of these IEC genes is considered an adaptation to enable S. aureus colonisation and infection of humans and is not usually a feature of animal S. aureus strains (Cuny et al., 2015).
Antimicrobial susceptibility in European invasive Staphylococcus aureus isolates from humans is reported by 29 MSs to the European Antimicrobial Resistance Surveillance Network (EARS‐Net) hosted by ECDC. MRSA typing data are not reported and, therefore, when there may be possible links to the animal reservoir of LA‐MRSA, these cannot easily be detected with current monitoring procedures, at least at the European level. The EU/EEA (excluding the United Kingdom) population‐weighted mean proportion of MRSA among invasive S. aureus infections reported to EARS‐Net decreased significantly from 18.4% in 2017 to 15.8% in 2021, with significantly decreasing trends reported by 11 of the reporting EU/EEA countries (excluding the United Kingdom). Nevertheless, MRSA continues to be an important human pathogen in the EU/EEA, as levels of MRSA remain high in several countries and combined resistance to another antimicrobial group was common (WHO/ECDC, 2022).
Technical specifications for a baseline survey on the prevalence of MRSA in pigs (EFSA, 2022 )
The technical specifications for a baseline survey on the prevalence of MRSA in pigs were recently published by EFSA following a request received from the European Commission to provide scientific and technical assistance in the preparation of a EU wide baseline survey protocol for a EU coordinated monitoring programme on the prevalence of MRSA in pigs (EFSA, 2022). The baseline survey aims to estimate the prevalence of MRSA in batches of fattening pigs at slaughter at the European and national level, with a 95% level of confidence and a level of precision of 10% considering an expected prevalence of 50%. An additional objective of the baseline survey it to assess the genetic diversity and antimicrobial resistance of MRSA in pigs. This will include detailed characterisation of MRSA strains and lineages, virulence and host‐adaptation factors, and other genetic markers associated with animal hosts, such as phages. This will facilitate the comparison of AMR in humans and animals.
The technical specifications published by EFSA (EFSA, 2022) define the target populations, the sample size for the baseline survey (20 pigs per batch), the sample collection requirements, the analytical methods (for isolation, identification, phenotypic susceptibility testing and further genotypic testing of MRSA isolates), the data reporting requirements and the plan of analysis. As indicated in the technical specifications, the samples are to be analysed according to the laboratory protocols available on the European Union Reference Laboratory (EURL‐AR) website. Generalised linear models will be used to estimate proportion (with 95% confidence intervals) of batches of slaughter pigs tested positive to MRSA. The necessary data to be reported by the EU Member States to support the baseline survey are presented in three data models. The results of the baseline survey should be reported using the EFSA data collection framework. EFSA will therefore update the reporting guidance and the data models. Consecutively, an updated reporting tool for reporting AMR data will be created and new reporting tools for MRSA prevalence and pig population data will be available.
6.3. Food and animals: MRSA
This section summarises the occurrence of MRSA and its susceptibility to antimicrobials in various food categories, in food‐producing animals excluding clinical investigations, and during clinical investigations in food‐producing and other animals in 2020/2021. Additional tables on MRSA in food and food‐producing animals have been included in Annex E that is available as supporting documentation in zenodo (https://doi.org/10.5281/zenodo.7544221).
In 2021, five MSs (Austria, Belgium, Finland, Germany and the Netherlands) and two non‐MSs (Norway and Switzerland) provided data on the occurrence of MRSA in food and animals. In addition, Belgium, Germany and Switzerland also reported isolate‐based data on antimicrobial susceptibility of MRSA. In 2020, data on the occurrence of MRSA were reported by six MSs (Austria, Belgium, Finland, Germany, the Netherlands and Slovakia) and one non‐MS (Norway). Out of the six MSs reporting occurrence data in 2020, Austria, Belgium and Germany also reported isolate‐based data on the susceptibility of MRSA. It is important to note that monitoring of MRSA in food and animals is not harmonised in the EU. Therefore, findings and related comparison between reporting countries should be interpreted with caution, as differences exist in the sensitivity of the methods used for the isolation of MRSA from food and animals, as well as in the sampling strategies and types of samples collected. The sampling stage can influence MRSA prevalence rates and should be taken into consideration when interpreting the results discussed below.
6.3.1. Food: monitoring of MRSA
In both 2021 and 2020, a low number of countries reported data on the occurrence of MRSA in food (N = 4 and N = 4, respectively). In 2021, Austria, Germany, the Netherlands and Finland provided data (see Annex E, Table 1a). MRSA was investigated in meat from bovine animals (Austria, Germany and the Netherlands) and meat from pigs (Austria, Germany and Finland). The Netherlands also provided data on MRSA found in meat from broilers, turkeys, sheep, ducks and deer. In 2020, MRSA was investigated in meat from broilers (Austria and the Netherlands), and meat from pigs (Slovakia and the Netherlands). Moreover, data on meat from bovines and from turkeys was reported by the Netherlands, and data on meat from sheep by Germany. The Netherlands reported few negative samples from unspecified meat and meat from deer. Germany reported investigations on soft cheese with no positive MRSA findings (see Annex E, Table 1b). Monitoring results on the occurrence of MRSA in food reported in 2021 and 2020 are presented in Figure 51.
Figure 51.
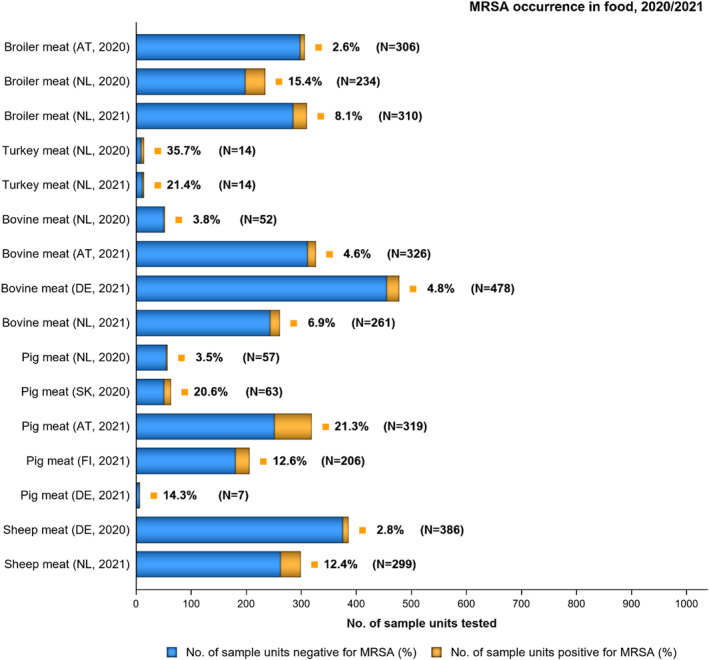
-
N: Total number of sample units tested; AT: Austria; DE: Germany; FI: Finland; NL: the Netherlands; SK: Slovakia; CH: Switzerland.• Broiler meat (AT, 2020): spa‐types: t011 (4 isolates) t034 (4).•Bovine meat (DE, 2021): spa‐types: t1346 (1 isolate), t002 (2), t008 (2), t311 (2), t2112 (1), t174 ST41110 (1), t011 (4), t034 (4), t359 (1), t559 (1), t843 mecC positive (1), t899 (1), t1430 (1), t1451 (1).•Pig meat (FI, 2021): spa‐types: t728 St45 (1 isolate), t034 ST398 (14), t899 ST398 (1), t2741 ST398 (9), t4677 ST398 (1).•Pig meat (DE, 2021) spa‐types: t1430 (1 isolate).•Sheep meat (DE, 2020) spa‐type: t011 (1 isolate), t034 (2), t1451 (1), t2576 (1), t19979 ST 398 (1), t223 (2), t267 (1), t1154 ST5 (1) t15010 ST97 (1).
The highest occurrence of MRSA was observed in meat from turkeys (35.7% in 2020; 21.4% in 2021), though it should be noted that only 14 samples were tested in each year by only one MS (Netherlands). In meat from pigs and broilers, occurrence differed between countries with occurrence in pig meat ranging from 3.5% in the Netherlands (2020) to 20.6% and 21.3% in Slovakia (2020) and Austria (2021), respectively. In broiler meat, the proportion of positive samples ranged from 2.6% in Austria (2020) to 15.4% in the Netherlands (2020). Occurrence of MRSA in broiler meat reported by the Netherlands decreases in 2021 (8.1%) compared with 2020 (15.4%). Occurrence of MRSA was overall lower in bovine meat ranging from 3.8% (Netherlands, 2020) to 6.9% in the Netherlands (2021). Meat from sheep was found to be MRSA positive in 2.8% of samples from Germany (2020) and 12.4% in the Netherlands (2021).
6.3.2. Animals: monitoring of MRSA
6.3.2.1. Monitoring of MRSA in healthy animals
MRSA occurrence data from animals were reported by five MS (Belgium, Germany, Finland, the Netherlands and Slovakia) and Norway in 2020 (see Annex E, Table 2b) and by five countries, 3 MS (Belgium, Finland and the Netherlands) and two non‐MS (Norway, Switzerland) in 2021 (see Annex E, Table 2a). The data originated from different frameworks, including a voluntary monitoring, surveillance, control programs and specific surveys, the latter being restricted to fur animals in Finland. The voluntary monitoring performed over 2020/2021 examined turkeys, laying hens, broilers, calves (under 1 year), dairy cows, meat production cattle, fattening pigs, wild boars and wild freshwater fish. Fur animals surveyed included foxes, mink and racoon dogs.
In 2020 and 2021, MRSA were most frequently detected in pigs (Figure 52). Among the different populations studied at farm level were herds of fattening pigs in the Netherlands (79.0% in 2020) and Switzerland (53.6% in 2021). At slaughter 18.0% of pigs were positive in Slovakia in 2020. In contrast, MRSA was not detected at all in 643 samples (2020) or 763 samples (2021) in the framework of the national control and eradication programme in pigs in Norway (see Annex E, Table 2a,b). High detection rates for MRSA in pigs except for Norway confirm the results of previous years.
Figure 52.
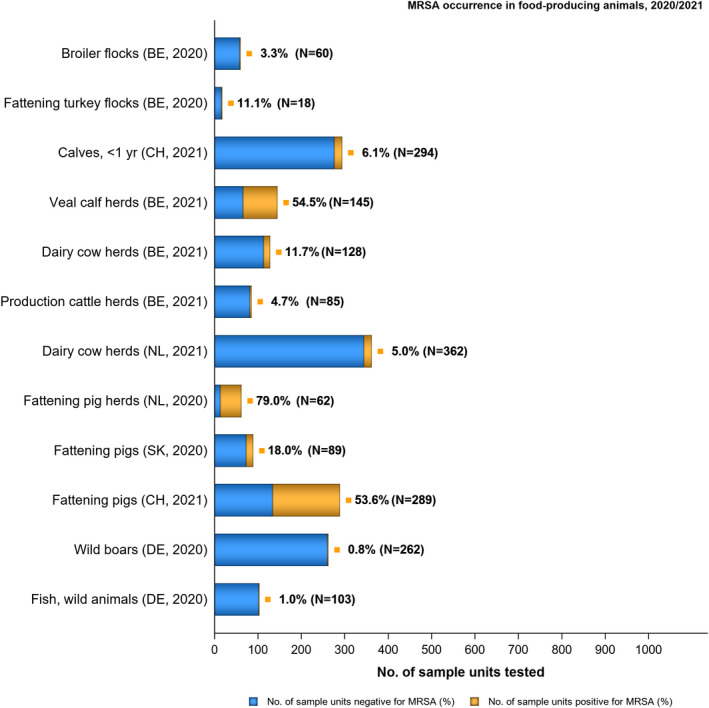
-
N: Total number of sample units tested; BE: Belgium; CH: Switzerland; DE: Germany; NL: the Netherlands; NO: Norway; SK: Slovakia.• Broiler flocks, BE 2020: spa‐types: t011 CC398 (2 isolates).• Fattening turkey flocks, BE 2020: spa‐types: t011 CC398 (2 isolates).• Fattening pigs, SK 2020: data were reported as suspect sampling.• Veal calf herds, BE 2021: spa‐types: t386 ST1 (1), t011 (65), t034 (6), t1451 (1), t1456 (1), t2346 (1), t2370 (1), t3423 (1), t5210 (1), t6228 (1).• Dairy cow herds, BE 2021: spa‐types: t037 ST239 (3 isolates), t011 (10), t034 (2).• Production cattle herds, BE 2021: spa‐types: t037 ST239 (2 isolates), t011 (2).
MRSA were detected in turkeys (11.1%) and broilers (3.3%) in Belgium in 2020, but not in laying hens in Belgium in 2020. Low detection rates in broiler flocks and laying hen flocks have been observed frequently. In broilers, this contrasts with higher detection rates in broiler meat indicating that cross contamination at slaughter my play a relevant role here. Turkeys were more frequently positive on farm than broilers, in 2020 as well as in previous years.
Very few MRSA were found in wild boars and wild freshwater fish in Germany (0.8% and 1.0%) (Figure 52) see also Annex E, Table 2b. In Finland, no MRSA were detected in samples from farmed fur animals: racoon dogs (1 sample in 2020 and 10 samples in 2021), mink (15 samples in 2020 and 47 samples in 2021) and foxes (11 samples in 2020 and 2 samples in 2021). Absence of MRSA in farmed mink in Finland contrasts with a considerable proportion of positive samples in Denmark in 2018 (EFSA and ECDC, 2020)
In 2020, no cattle were tested for MRSA. However, in 2021, 4.7% of meat production cattle, 11.7% of dairy herds and 54.5% of veal calf herds in Belgium, were found positive for MRSA. A higher occurrence of MRSA in calves than in dairy cows has been reported previously (Graveland et al., 2010; Tenhagen et al., 2014; Schnitt et al., 2020).
6.3.2.2. Monitoring of MRSA in animals following clinical investigations
Typically, clinical investigations differ from monitoring studies in food‐producing animals: selective culture methods are typically not used, and the sampling is biased. These data therefore do not allow occurrence to be inferred and cannot be extrapolated at the population level. However, it is still considered relevant to report the range of animal species/populations which were affected, and the lineages of MRSA detected. Slovakia and the Netherlands reported on clinical animal data on MRSA in 2020 and 2021 (see Annex E, Tables 3 and 4a,b).
In 2020, Slovakia reported data following clinical investigations for MRSA in 46 animals of various species with no positive finding (see Annex E, Tables 3 and 4a). These included dogs (23 samples), cats (9), dairy cows (5), goats (2), horses (2), rabbits (2), guinea pigs, squirrels and falcons (1). The Netherlands reported data, predominantly on cats, dogs and horses in 2020. The highest rate of MRSA findings was in horses (5.4%) followed by cats (0.8%) and dogs (0.4%). One individual finding of MRSA in a caged bird was reported by the Netherlands. The bird species was not reported. No molecular data was provided by the two countries. In 2021, the Netherlands reported data on clinical isolates from cats (0.8%), dogs (0.1%) and horses sampled in farms (1.9%, see Annex E, Table 4b).
6.3.3. Animals and food: results of molecular typing of isolates
In 2021, molecular characterisation was reported for 124 of 1329 MRSA isolates recovered from food. Among those, 74 originated from Austria, 24 originated from Germany and 26 from Finland. Molecular characterisation was also reported by one MS (Belgium) for 98 of 358 MRSA isolates recovered from food‐producing animals (see Annex E, Table 9a). In 2020, typing data were only reported for 19 isolates from food and for four isolates from food‐producing animals, all of which originated from MSs (Austria, Belgium and Germany) (see Annex E, Table 9b). Over both years, most MRSA isolates from food and animals were assignable to the clonal complex 398 (food: 99 of 143, 69.2%; animals: 96/102, 94%). Results of molecular typing of isolates from animals and food are presented in Figure 53; Tables 14 and 15.
Figure 53.
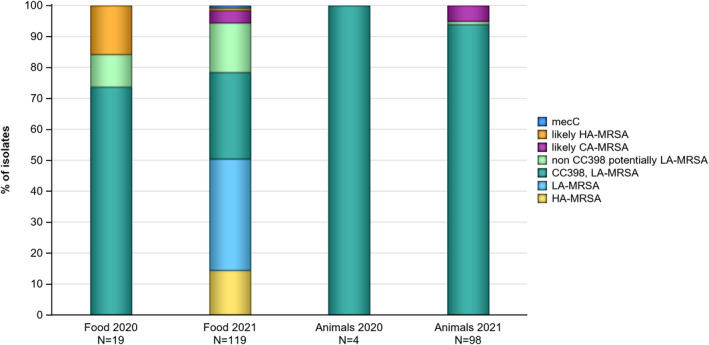
-
N = number of reported isolates with typing data, mecC: MRSA harbouring the mecC gene, HA‐MRSA: hospital acquired MRSA, CA‐MRSA: community acquired MRSA, LA‐MRSA: livestock associated MRSA, CC: clonal complex.Inferred MRSA types recovered from animals in 2020 were derived from broiler flocks (2 isolates) and fattening turkey flocks (2 isolates). In 2021 these were recovered from veal calves (79 isolates), dairy cows (15 isolates) and cattle (4 isolates).Inferred MRSA types recovered from food in 2020 were derived from broiler meat (8 isolates) and meat from sheep (11). In 2021 these were recovered from bovine meat (21 isolates) and pig meat (27 isolates). Eight bovine meat isolates and 1 pig meat isolate were identified at border in imported meat from border control posts in 2021. Four bovine meat isolates (t898 ST399, t588 ST402, t034 ST4562, t311 St5/CC5) and 1 pig meat isolate (t588 ST400) were excluded from the graph as it was unclear whether they were LA, HA or CA.
Among the CC398 isolates, most isolates with spa‐typing data in both years were from spa‐types t011 and t034. In 2021, t011 and t034 accounted for 92.4% (85/92)of CC398 isolates from animals and for 74.1% (63/85) of CC398 isolates from food. In 2020, t011 and t034 accounted for 11 of 14 CC398 isolates from food (78.6%) and for all four CC398 isolates from animals. All isolates from animals reported in 2020 were from t011.
In 2021, spa‐types that were assignable to CC398 but were not t011 and t034 included two isolates from pig and bovine meat that were spa‐type t899. Spa‐type t899 can be associated with different clonal lineages, including CC398 and CC9. LA‐MRSA CC9/CC398 displaying spa‐type t899 is a mosaic strain, consisting of a CC398 chromosomal backbone having acquired the CC9 region containing the staphylococcal protein A gene (Guardabassi et al., 2009; Larsen et al., 2016; Tegegne et al., 2021b; Ceballos et al., 2022) Other CC398 associated spa‐types in food in 2021 included one isolate of t1451 from bovine meat, one isolate of t2741 from pig meat and one t4677 from pig meat.
In 2020, three isolates from sheep meat reported by Germany were from less frequently observed spa‐types (t1451, t2576 and t19979) of CC398. Spa‐type t1451 had also been observed in one isolate from a veal calf in 2021. Spa‐type t19979 is a comparatively new variant but was confirmed as an ST398 by Germany.
In 2021 and 2020, most spa‐types of isolates from animals and food that were assignable to CC398 have already been observed in the EU‐baseline in breeding pigs in 2008 (EFSA, 2009a) demonstrating a remarkable persistence in the food‐producing animal population. This applies to t011, t034, t899, t1451, t1456, t2346 and t2370. Most other spa‐types assigned to this clonal complex have likewise been observed previously as exemplified below:
t3423 was previously identified in MRSA isolated from a pig and a veal calf on Belgium farms, as well as in a surgical site infection in a horse from the United Kingdom (Verhegghe et al., 2013; Nemeghaire et al., 2014; Bortolami et al., 2017).
t5210 was previously identified in multiple farm workers and a rabbit on a rabbit farm in Italy (Agnoletti et al., 2014).
t6228 was previously identified in dairy farms in Belgium (Nemeghaire et al., 2014).
t2741 has been described as a dominant spa‐type in Finnish fattening pigs (Heikinheimo et al., 2016).
t2576 was previously described in a bovine clinical isolate from a dairy farm in Germany and a pork meat sample in a supermarket from the Czech Republic (Feßler et al., 2010; Tegegne et al., 2021a).
t1793 was identified in pig meat from Austria. This spa‐type has previously been identified in a slaughter pig from Denmark (Guardabassi et al., 2007).
t9013 was identified in pig meat from Austria. It has been identified in human MRSA isolates that were suspected to be livestock associated in Germany (Köck et al., 2013)
t571 was identified in pig meat from Austria. This spa‐type belonging to CC398 has been isolated from pigs and a veal calf in Germany (Cuny et al., 2013).
While this list does not claim full coverage, it clearly indicates that these spa‐types persist in animal production (including at slaughter and meat).
Spa‐type t19979 is a recent strain as indicated by the high spa‐type number and has not been reported in animals, food or farmers before 2020.
In 2021, Austria reported spa‐types for 74 isolates from pig and bovine meat, Germany reported spa‐types for 24 isolates recovered from imported pig and bovine meat from border control posts, and Finland reported for 26 isolates recovered from pig meat. Switzerland provided information on clonal complex for three MRSA isolates from pig and bovine meat. In 2020, molecular typing data were reported for eight isolates from broiler meat from Austria and 11 isolates from sheep meat from Germany.
Isolates that were not assigned to the CC398 included a range of spa‐types that could be or were assigned to a number of different CC (see Annex E, Table 9a,b). The highest proportion of such isolates was observed in meat from sheep in 2020 (5 of 11, 45.5%), bovine meat in 2021 (20 of 38, 52.6%) and pig meat in 2021 (15 isolates).
In 2021, the following isolates were from spa‐types not assignable to CC398 (see also Table 15).
Spa‐type t002 was reported in imported bovine meat from border control posts by Germany in 2021. This spa‐type has repeatedly been observed in turkey meat and in turkeys (Richter et al., 2012; Vossenkuhl et al., 2014; Tegegne et al., 2021b).
Germany reported spa‐type t008 from imported bovine meat from border control posts. This spa‐type has been identified as one of the most prevalent in European human populations (Asadollahi et al., 2018). It belongs to CC8 which has been suggested to have made a jump from humans to bovines (Resch et al., 2013).
mecC‐MRSA spa‐type t843 was reported by Germany from cattle meat. The isolate was confirmed to carry the mecC gene. The association of this spa‐type with CC130 has previously been observed in cattle (Mališová et al., 2020; Cui et al., 2021; Silva et al., 2021).
t037 was reported in dairy cows and cattle from Belgium. This spa‐type has been previously described in chickens from Belgium (Jungwhan Chon, 2017). This isolate was confirmed to belong to ST239. MRSA isolates with ST239 and t037 were previously identified in human infections from patients in Iran (Ghasemzadeh‐Moghaddam et al., 2022).
t174 was reported in cattle meat from Germany. This spa‐type has previously been isolated from pigs in Italy (Normanno et al., 2015). This isolate was confirmed to belong to ST41110.
t311 was described in isolates from cattle meat in Germany. t311 has previously been described in an isolate from a cow with mastitis in Germany (Wu et al., 2020).
t386 was isolated from veal calves in Belgium. This isolate was confirmed to belong to ST1 and CC1. T386 has been identified in methicillin susceptible S. aureus isolated from chicken samples in Gabon and in MRSA isolated from a hedgehog in Spain (Lozano et al., 2016; Silva et al., 2020).
t359 was isolated from cattle meat in Germany. t359 has previously been described in MRSA isolates from clinical human samples in Kuwait (Boswihi et al., 2018).
t588 was described in bovine and pig meat samples from Austria. has been identified in a Spanish pig farmer who was suggested to have been infected by MRSA transmitted from his pigs (Lozano et al., 2011).
t728 was isolated from pig meat in Finland. t095 was isolated from bovine and cattle meat in Austria. Both spa‐types were confirmed to belong to ST45 and CC45. CC45 is widely spread in human populations and an isolate harbouring t359‐ST45 was previously identified in an Irish maternity hospital (Cuny et al., 2015; Broderick et al., 2021).
t898 was described in bovine meat from Austria. This spa‐type has previously been identified in an environmental sample on a pig farm (Golob et al., 2022).
t1430 was described in isolates from pig and cattle meat in Germany. This spa‐type was previously described in broiler farms from Germany (Kittler et al., 2019).
In 2020 five isolates, all from sheep meat reported by Germany, were from spa‐types not assignable to CC398.
Two isolates were spa‐type t223. This spa‐type is frequently assigned to the MLST‐type ST22 in clinical isolates from humans in Iran and was also identified in Kuwait and Palestine (Goudarzi et al., 2020). This spa‐type has also been identified in community and healthcare environments in Norway and Sweden (Di Ruscio et al., 2018).
One isolate (t15010) was identified as MLST‐type ST97. This MLST‐type is frequently observed among S. aureus from cattle and has also been observed in pigs, e.g. in Italy. Despite not being related to the CC398 it is considered as a livestock associated strain by some authors (Feltrin et al., 2016; Boswihi et al., 2019).
A second spa‐type that frequently occurs in ST97 is t267. This spa‐type has been found in bovine milk as well as a PVL positive strain in humans (Käppeli et al., 2019; McManus et al., 2021) underlining that it could be both, of animal and human origin.
One other isolate (t1154) was identified as MLST‐type ST5. ST5 isolates are frequently observed in humans but have also been reported in turkeys (Richter et al., 2012; Vossenkuhl et al., 2014), although with different spa‐types. Spa‐type 1154 belonging to ST5 have been identified in clinical samples from humans (Viana et al., 2021).
6.4. Temporal trends of MRSA occurrence
Isolation of MRSA from food‐producing animals and the farm environment
In 2018, the European Union Reference Laboratory‐Antimicrobial Resistance (EURL‐AR) published revised recommendations for the isolation of MRSA from food‐producing animals and the farm environment (known as 1‐step (1‐S) method) (EURL (European Union Reference Laboratory for Antimicrobial Resistance), 2018). The revised recommendations were based on a study of Danish and Norwegian pig herds which confirmed that the 1‐S method resulted in a lower proportion of false‐negative results than the 2‐step (2‐S) method (comprising of a pre‐enrichment step and a selective enrichment step) used prior to 2017 (Larsen et al., 2017). For broiler meat, it has been shown that the 1‐S method may improve sensitivity but decrease the specificity (Pauly et al., 2019). Direct comparison of the data obtained using the different protocols should be performed with caution.
In 2021, occurrence data was obtained using the 1‐S method by 2/3 reporting countries in food‐producing animals (Belgium, Norway, Switzerland) and 3/4 reporting countries in food (Austria, Finland, the Netherlands). Belgium used the 2‐S method in animals and Germany described their method as ‘other’ in food. In 2020, the 2‐S method was used by Belgium (animals) and Germany (animals and food), while Austria, the Netherlands and Norway used the 1‐S method.
Considering the monitoring performed in 2019/2020 and 2021 and for previous years, comparable longitudinal data were available for the animal species and food items, as presented in the following sections.
Based on the limited number of available data no statistical trend analyses were carried out. Therefore, changes in occurrence are reported here only descriptively.
6.4.1. Temporal trends of MRSA occurrence in various types of meat
Four countries reported comparable data over time on MRSA from broiler meat (Figure 54; Annex E, Table 5). Over the last 4 years, the Netherlands consistently provided data on broiler meat. The proportion of positive samples decreased slightly over time from 20.2% in 2018 (no data before that date) to 8.1% in 2021. Austria provided similar data in 2018 (1.0%) and 2020 (2.6%). Both countries used the 1‐S method. Germany and Switzerland used the 2‐S method. Germany last provided data in 2018 (16.4%), which was a higher proportion than seen in 2016 (13.0%) but lower than 2013 and before, when detection rates were between 22% and 26%. Samples of broiler meat in Switzerland rarely contained MRSA in 2016 (3.0%) and 2018 (1.3%).
Figure 54.
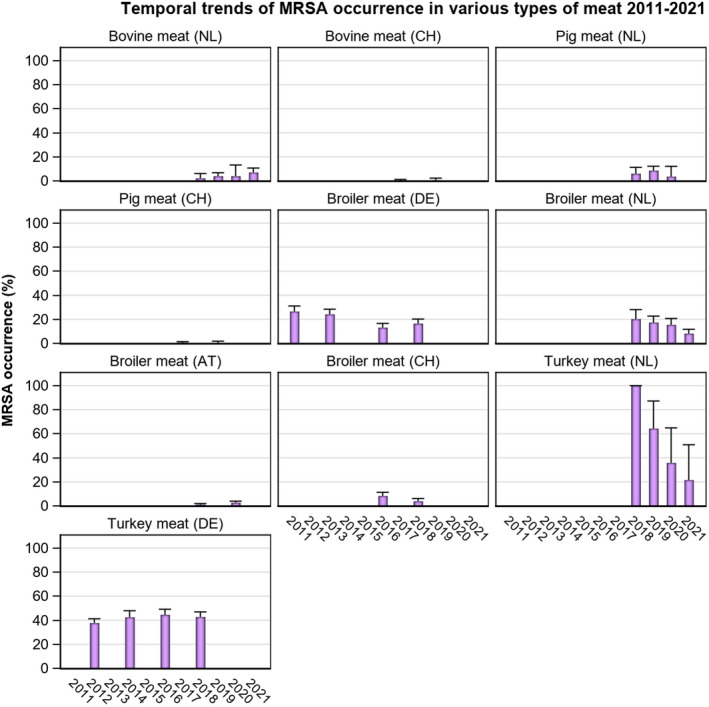
-
AT: Austria; CH: Switzerland; DE: Germany; NL: the Netherlands.The 2‐S method of isolation was used by CH and DE from 2011 to 2018; while the 1‐S method was used by the NL from 2018 to 2021, as well as CH in 2019.Bovine meat (CH): In 2019, spa‐types were not reported; however, both isolates were confirmed to belong to CC398 using the sau1‐hsdS1 CC398 PCR reaction (Stegger et al., 2011).Pig meat (CH): In 2017, spa‐type: t011 (1 isolate), t002 (1). PVL status of the t002 isolate was not reported. In 2019, spa‐type was not reported; however, the isolate was confirmed to belong to CC398 using the sau1‐hsdS1 CC398 PCR reaction (Stegger et al., 2011).Broiler meat (AT): In 2018, spa‐types: t011 (2 isolates), t034 (1 isolate). In 2020, spa‐types: t011 (4 isolates), t034 (4 isolates).Broiler meat (CH): In 2016, spa‐types: t034 (3 isolates), t153 (1), t1430 (3), t2123 (2). PVL status of the t153 isolate was not reported.In 2018, spa‐types: t034 CC398 (1 isolate), t1430 (1), t571 CC398 (1), t13177 (1).*spa‐types were not provided for Bovine meat (NL), Pig meat (NL), Broiler meat (DE), Turkey meat (DE and NL).
The Netherlands provided MRSA data from turkey meat in 2018–2021. However, the number of collected samples was very low (45 over the 3 years) not allowing a meaningful analysis of trends. Germany last reported on MRSA in turkey meat in 2018 with 42.7% positive samples. This was in the range of results reported between 2009 and 2017 for fresh turkey meat from Germany (39.9%–44.5%). While the Netherlands used the 1‐S method throughout, Germany used the 2‐S method.
The Netherlands reported data on pig meat in 2018–2020, with results ranging from 3.5% (2020) to 8.4% (2019) and 2018 in between (5.9%), i.e. without a clear trend. Slovakia reported on different kinds of pig meat over the years precluding straightforward comparison of data. Switzerland reported data in 2017 and 2019, with very low detection rates (0.7% and 0.3%). While the Netherlands used the 1‐S method throughout, Switzerland changed from 2‐S to 1‐S in 2019. Austria used the 1‐S method and reported an increase from 15.7% (2019) to 21.3% (2021), although much fewer samples were collected in 2021.
The Netherlands reported on bovine meat in 2018–2021. The number of positive samples have slowly increased from 2.1% (2018), to 3.8% (2019/2020), to 6.9% (2021). Austria also reported a small increase in MRSA positive bovine meat from 2.6% (2019) to 4.6% (2021). In Switzerland, reporting in 2017 and 2019, MRSA were only detected in two samples of fresh bovine meat in 2019 (0.6%). As in pig meat, the Netherlands and Austria used the 1‐S method throughout, while Switzerland changed from 2‐S to 1‐S in 2019.
6.4.2. Temporal trends of MRSA occurrence in various animals
As monitoring of MRSA is not mandatory and methodology is not harmonised, comparable data over time are only available for some populations in a few reporting countries. These are presented in Figures 55 and 56 (as well as in Annex E, Figure 1 and Table 6).
Figure 55.
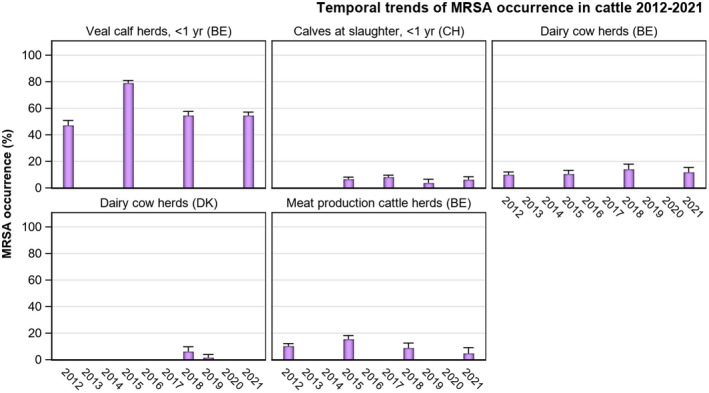
-
BE: Belgium; CH: Switzerland; DK: Denmark. The 2‐S method of isolation was used by Belgium and Switzerland from 2012 to 2018; while the 1‐S method was used by Denmark since 2018 and by Switzerland since 2019.*spa‐types not reported.Veal calf herds < 1(BE): In 2012, spa‐types: t011 (40 isolates), t1451 (3), t1456 (1), t1985 (3), t3423 (1), untypable (1).In 2015, spa‐types: t011 (64 isolates), t034 (15), t037 (8), t044 (3), t1451 (3), t1580 (7), t1985 (8), t2287 (2), t3423 (5), untypable (1). The t044 isolates were PVL‐negative. In 2018, spa‐types: t011 CC398 (65 isolates), t034 CC398 (8), t1451 CC398 (1), t1580 CC398 (2), t3423 CC398 (1), t3479 CC398 (1), t9433 CC398 (1). In 2021, spa‐types: t386 (1), t011 (65), t034 (6), t1451 (1), t1456 (1), t2346 (1), t2370 (1), t3423 (1), t5210 (1), t6228 (1)Veal calf herds < 1(CH): In 2015, spa‐types: t011 (11 isolates), t034 (6) and t008 (2). The t008 isolates were PVL‐positive.In 2017, spa‐types: t011 (14 isolates), t034 (7), t127 (1), t17339 (2). PVL status of the t127 isolate was not reported. In 2019, spa‐types were not reported; however, all 11 isolates were confirmed to belong to CC398 using the sau1‐hsdS1 CC398 PCR reaction (Stegger et al., 2011).Dairy cow herds (BE): In 2012, spa‐types: t011 (8 isolates), t037 (1), t388 (1), t1456 (1), t6228 (2), untypable (1). In 2015, t011 (4 isolates), t034 (1), t1580 (1), t1985 (2), t2383 (1), untypable (1). In 2018, spa‐types: t011 CC398 (8 isolates), t034 CC398 (1), t223 (3), t1257 (1). The t223 isolates were PVL‐negative; TSST status was not determined. The PVL status of the t1257 isolate was not reported. In 2021, spa‐types: t037 (3), t011 (10), t034 (2).Dairy cow herds (DK): In 2018, spa‐types: t034 (7 isolates), t267 CC97 (1). In 2019, spa‐types: t127 CC1 (1 isolate), t843 CC130 (1). The t127 isolate was PVL‐negative, as well as negative for the human IEC gene scn. spa‐type t843 was confirmed to carry the mecC gene.Meat production cattle herds (BE): In 2012, spa‐types: t011 (16 isolates), t121 (1), t1456 (1), t1985 (1). In 2015, spa‐types: t011 (9 isolates), t034 (2), t1451 (1), t1580 (2), t2287 (1), t3423 (1). In 2018, spa‐types: t011 CC398 (5 isolates), t1451 CC398 (1), t223 (2), t223 ST22 (1). All three t223 isolates were PVL‐negative. One t223 isolate was confirmed to belong to ST22, harbour the tst gene and IEC genes (chp, sak and scn) from WGS data. In 2021, spa‐types: t037 (2), t011 (2).
Figure 56.
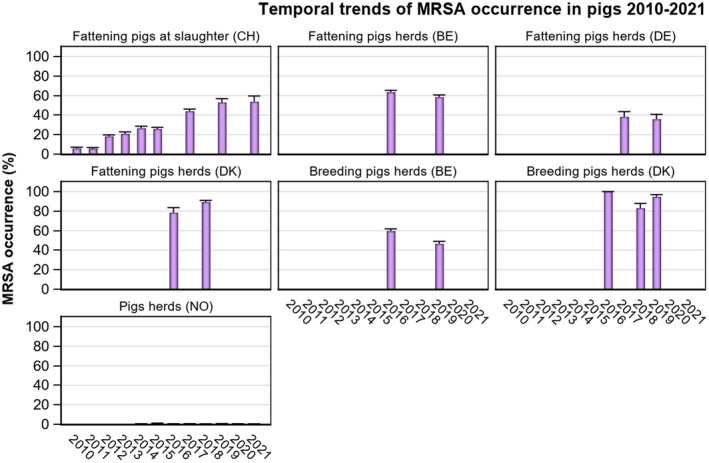
-
BE: Belgium; CH: Switzerland; DE: Germany; DK: Denmark; NO: Norway.Note: The 2‐S method of isolation was used by Belgium and Germany from 2016 to 2019, as well as by Denmark in 2016, in Switzerland from 2010 to 2017 and in Norway from 2014 to 2017. The 1‐S method was used by Switzerland in 2019 and 2021, by Denmark in 2018 and 2019, and by Norway in 2018–2021.All isolates tested by Norway in 2018, 2020 and 2021 (n = 716 in 2018, n = 641 in 2020 and n = 763 in 2021) were MRSA negative; extremely low % positive MRSA isolates (range: 0.1%–0.5%) were reported in the other years. Norway is the only country with a control programme in place for MRSA in pigs.Fattening pigs (CH): In 2010, spa‐types: t034 ST398 (17 isolates), t011 ST398 (1), t208 ST49 (5). In 2011, spa‐types: t034 ST398 (19 isolates), t011 ST398 (1), t208 ST49 (1), t2279 ST1 (1). In 2012, spa‐types: t034 CC398 (61 isolates), t011 CC398 (9), t208 ST49 (2). In 2013, spa‐types: t034 (63 isolates), t011 (10). In 2014, spa‐types: t034 (57 isolates), t011 (19), t208 (1), t899 (1), t2741 (1). In 2015, spa‐types: t034 (48 isolates), t011 (23), t032 (1), t571 (1), t899 (1), t1145 (1), t1250 (1), t4475 (1). In 2017, spa‐types: t034 (63 isolates), t011 (61), t899 (2), t1451 (3), t2330 (1), t2876 (1). In 2019, spa‐types were not reported; however, 159/160 isolates were confirmed to belong to CC398 using the sau1‐hsdS1 CC398 PCR reaction (Stegger et al., 2011). The remaining isolate did not survive cryo‐conservation, therefore typing could not be performed.Fattening pigs (BE): In 2016, spa‐types: t011 CC398 (71 isolates), t1451 (1), t1456 (1), t1456 CC398 (1), t1580 (5), t1985 (8), t1985 CC398 (3), t034 (7), t034 CC398 (2), t037 (1), t898 (1), unspecified (11). In 2019, spa‐types: t011 CC398 (67 isolates), t034 CC398 (11), t1451 CC398 (2), t1457 CC398 (1), t2346 CC398 (1), t2370 CC398 (2), t2383 CC398 (1), t3041 CC398 (1), t3119 CC398 (1), unspecified (18).Fattening pigs (DE): No molecular typing results available.Fattening pigs (DK): In 2016, spa‐types not reported. In 2018, spa‐types: t011 CC398 (22 isolates), t034 CC398 (85), t571 CC398 (3), t898 CC398 (1), t2383 CC398 (1), t2974 CC398 (1), t3423 CC398 (1), t4652 CC398 (1), t9266 CC398 (1). Prevalence data for fattening pig herds (not raised under controlled housing conditions) from 2018 are not included.Breeding pigs (BE): In 2016, spa‐types: t011 CC398 (55 isolates), t1451 (2), t1456 (1), t1456 CC398 (3), t1580 (1), t1985 (5), t1985 CC398 (1), t034 (1), t034 CC398 (4), t4659 CC398 (1), unspecified (17). In 2019, spa‐types: t011 CC398 (57 isolates), t034 CC398 (18), t108 CC398 (2), t779 CC398 (1), t2346 CC398 (1), t2582 CC398 (1), t2922 CC398 (1), t3119 CC398 (2).Breeding pigs (DK): In 2016, spa‐types not reported. In 2018, spa‐types: t011 CC398 (6 isolates), t034 CC398 (24), t1250 CC398 (2), t1793 CC398 (1), t3171 CC398 (1). In 2019, spa‐types t011 CC398 (10), t034 CC398 (57), t1928 CC398 (1), t4652 CC398 (1) were identified in isolates from multiplier pig herds.Pig herds (NO): In 2014, spa‐type: t011 CC398 (1). In 2015, spa‐type: t034 CC398 (2), t177 CC1 (2). In 2016, spa‐type: t034 CC398 (1). In 2017, spa‐types: t091 CC7 (1 isolate), t843 CC130 (1), t6292 CC425 (1). The t091 isolate was PVL‐negative, spa‐types t843 and t6292 were confirmed to carry the mecC gene. In 2019, spa‐type: t034 CC398 (1).
Belgium provided data on MRSA in broiler flocks using the 2‐S method in 2014, 2017 and 2020 (Figure 55). While sampling details changed between the years, the proportion of positive holdings or flocks was very low in all 3 years with only two herds positive in 2014 (2.5%), 2017 (2.5%) and 2020 (3.3%). Spa‐type was t011 of CC398 in five positive samples and t1985 (likewise CC398) in one isolate in 2014.
Flocks/holdings of laying hens investigated in the same years in Belgium using the 2‐S method were also rarely positive for MRSA (see Annex E, Figure 1). Six herds (2.4%) were positive in 2014, three (1.3%) in 2017 and none in 2020. Among the 9 isolates collected in 2014 and 2017, 3 were t011 CC398 and 6 were spa‐type t037 (ST239).
Investigations in turkey flocks were repeatedly reported from Germany (2012, 2014 and 2018). In contrast to chicken flocks, these were more frequently positive with 12.8, 21.9 and 17.2% positive over the years (see Annex E, Figure 1). Investigations were carried out using the 2‐S method.
Switzerland reported on bovines < 1 year of age at slaughter in 2015, 2017, 2019 and 2021 with results ranging between 6.1% (2021) and 8.1% (2017) without a clear trend (Figure 55). In contrast to 2015 and 2017, Switzerland used the 1‐S method in 2019. In Belgium, MRSA in herds of calves under 1 year of age was investigated in 2012, 2015, 2018 and 2021 using the 2‐S method. Results varied widely with 78.9% in 2015 and 47.1% in 2012. The last investigations in 2018 and 2021 resulted in an occurrence in between the two (54.5%).
Data on MRSA in dairy cows using the 2‐S method were provided by Belgium in 2012, 2015, 2018 and 2021 (Figure 55) with values ranging between 9.9% (2012) and 10.2% (2021). Denmark reported on dairy cows in 2018 and 2019 using the 1‐S method, with occurrence seemingly lower in 2019 (1.5%) than in 2018 (6.1%).
Meat production cattle herds were reported by Belgium in 2012, 2015, 2018 and 2021 using the 2‐S isolation method with values ranging between 15.4% (2015) and 4.7% (2021) (Figure 55).
Considering the monitoring of pigs (Figure 56), MRSA occurrence data for Swiss fattening pigs at slaughter were reported from 2010 to 2015, as well as in 2017, 2019 and 2021. Generally, occurrence has increased annually, rising from 5.9% in 2010 to 53.6% in 2021; and from 2015 to 2017, a marked increase was observed from 25.7% to 44.0%, respectively. Notably, spa‐types associated with CC398 have shown a steady increase in occurrence; and where molecular typing data were available, all isolates in 2017 and 2019 were those associated with CC398, with most belonging to spa‐types t011 and t034 in 2017 (associated spa‐types were not provided in 2019). Molecular typing data was not available for 2021 isolates. It should be noted however, that from 2010 to 2017, the 2‐S method of isolation was used in comparison to the 1‐S method in 2019. It is important to note that all isolates tested by Norway (641 in 2020 and 763 in 2021) were MRSA negative as it is the only country with a control programme in place for MRSA in pigs. MRSA occurrence data from Belgian fattening pig herds using the 2‐S method was reported in 2016 (63.3%) and 2019 (58.3%) with a similar number of herds tested in both years. Belgium also reported MRSA occurrence data from breeding pig herds in 2016 (59.5%) and 2019 (46.4%). In both populations the occurrence tended to be lower in 2019 than in 2016. All MRSA isolates recovered from these production types over these years were spa‐types associated with CC398 (LA‐MRSA), except for a single isolate of spa‐type t037 reported from fattening pigs in 2016 (categorised as HA‐MRSA) in Belgium. Denmark reported results from a national survey on the occurrence of MRSA in breeding pig herds in 2016, 2018 and 2019. However, the number of tested herds in 2016 (n = 6) was too low for a meaningful comparison of the results between the years and populations studied differed slightly between years with multiplier herds sampled in 2019 and a census on breeding pig herds carried out in 2018. Spa‐typing data were reported in 2018 and 2019: All reported spa‐types were those associated with CC398 (LA‐MRSA). To note, Denmark used the 2‐S method in 2016 but changed to 1‐S in 2018. Norway is the only reporting country with a systematic surveillance and control programme that has been in operation since 2013. From 2014 to 2017 and again in 2019, very low levels of occurrence were reported as 0.1%, 0.5%, 0.1%, 0.4% and 0.1%, respectively. No pig herds tested positive for MRSA in 2018 and 2020 despite the large number of tested herds (641 in 2020). Since 2018, Norway has used the 1‐S method of isolation, replacing the 2‐S method that was in use until 2017.
MRSA occurrence data obtained from horse premises in Denmark were reported in 2018 and 2019 using the 1‐S method, with similar levels seen in both years (8.1 and 10.8%). In both years, most isolates were spa‐types associated with LA‐MRSA, except for t843 in 2018/2019 and t3256 in 2019; all three isolates were confirmed to belong to CC130 and carry the mecC gene.
6.5. Summary data on the occurrence and susceptibility of MRSA
Determination of the susceptibility of MRSA isolates to antimicrobials, including those of medical importance, such as linezolid and vancomycin, provides valuable information on the MRSA situation in animals and food. The importance of monitoring AMR patterns among different lineages is underlined by the potential for multiple resistance genes harboured by less virulent strains to spread to other S. aureus strains (Sahibzada et al., 2017).
In 2021, data on the antimicrobial susceptibility of MRSA isolates were reported by Belgium, Germany and Switzerland. In 2020, such data were provided by Austria, Belgium and Germany (see Annex E, Table 7a,b). All countries used a broth dilution method and applied EUCAST epidemiological cut‐offs (ECOFFs) to determine the susceptibility of isolates, and as expected, all MRSA isolates were resistant to penicillin and cefoxitin.
6.5.1. Susceptibility data of MRSA isolates from meat and food‐producing animals (excluding clinical investigations)
Figures 57 and 58 (see also Annex E, Table 7a,b) present the overall resistance to selected antimicrobials within food‐producing animal and the meat origins in 2020 and 2021.
Figure 57.
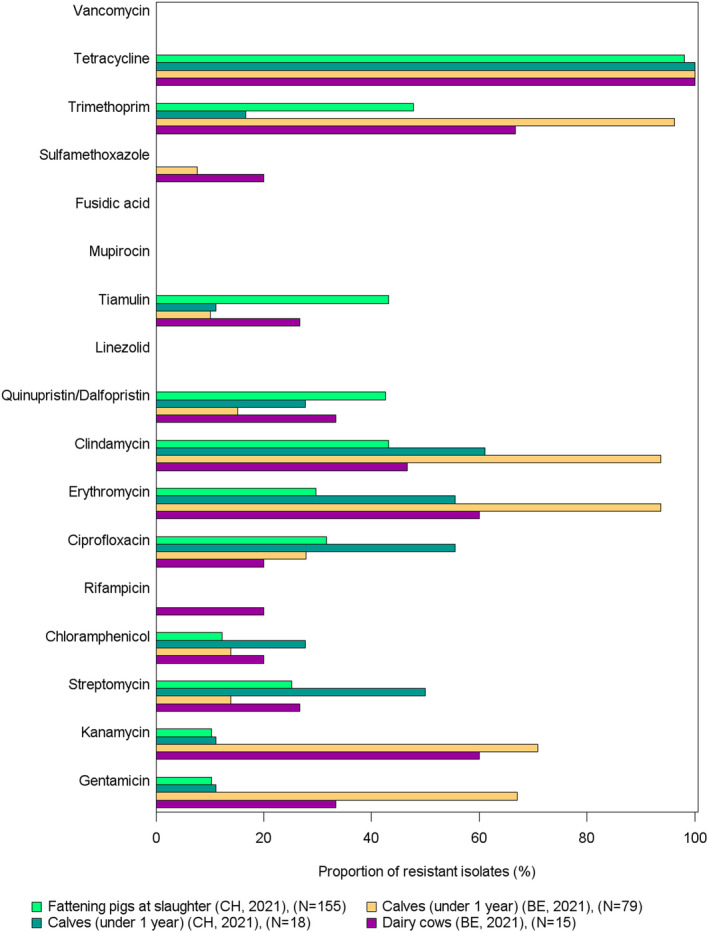
- BE: Belgium; CH: Switzerland. N: number of tested isolates. All isolates were resistant to Penicillin and Cefoxitin.
Figure 58.
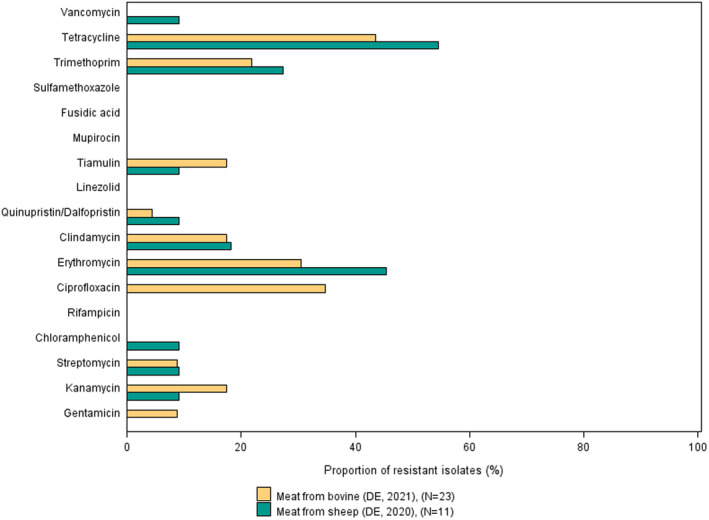
- DE: Germany. N: number of tested isolates. All isolates were resistant to Penicillin and Cefoxitin. Eight bovine meat samples and 1 pig meat sample from DE were from imported meat at border control posts.
In 2020 and 2021, extremely high levels of tetracycline resistance were reported in isolates from most reported animal populations (see Figure 57; see also Annex E, Table 7a,b). This is in line with a very high proportion of isolates from animals that can be assigned to the CC398, which are typically resistant to tetracycline (Crombé et al., 2012). All isolates from food‐producing animals were reported to be resistant to tetracycline, except for three isolates out of 155 from pigs reported by Switzerland in 2021. In 2020, only Belgium provided susceptibility data for only a few animal isolates (two isolates from broiler flocks and two from fattening turkeys) and all were resistant to tetracycline.
Resistance to other antimicrobials was more heterogenous among the animal populations. High heterogeneity was observed in the 155 isolates from fattening pigs from Switzerland in 2021. Moderate to high resistance levels were reported for aminoglycosides (gentamicin 10.3%, kanamycin 10.3%, streptomycin 25.2%) and chloramphenicol (12.3%), clindamycin (43.2%), quinupristin/dalfopristin (42.6%), tiamulin (43.2%) and trimethoprim (47.7%).
Susceptibility data was reported for calves under 1 year of age in Switzerland (18 isolates), and Belgium (79 isolates). Isolates from Swiss calves displayed very high resistance to streptomycin, ciprofloxacin, erythromycin and clindamycin (50%, 55.6%, 55.6% and 61.1%, respectively). Extremely high levels of resistance were detected for erythromycin (93.7%) and clindamycin (93.7%) in isolates from Belgium calves. Moreover, isolates from Belgium calves also displayed very high resistance to gentamicin (67.1%), kanamycin (70.9%) and trimethoprim (96.2%).
Belgium also reported susceptibility data for MRSA isolated from dairy cows (15 isolates) and bovine meat production animals (4 isolates). Isolates from meat production animals displayed very high to extremely high resistance to kanamycin (60%), erythromycin (60%), trimethoprim (66.7%) in dairy cows, and to gentamicin (50%), kanamycin (100%), streptomycin (50%), rifampicin (50%), erythromycin (50%), sulfamethoxazole (50%) and trimethoprim (50%). However, cautious interpretation of these results is advised due to the small sample size.
In 2021, two MRSA isolates from meat production animals and three isolates from dairy cows were resistant to rifampicin, an important antimicrobial for human use. No isolates were resistant to other antimicrobials of specific importance to the control of MRSA in humans, including vancomycin and mupirocin. Two isolates were resistant to rifampicin, and another three to mupirocin (Figure 57; Annex E, Table 7a).
Germany reported susceptibility data for 23 isolates from bovine meat and a single isolate from pig meat in 2021, several which were from imported meat at border control posts. Germany also reported susceptibility data for 11 isolates from sheep meat in 2020. Austria reported on 8 isolates from broiler meat in 2020 (Figure 58; see also Annex E, Table 7a,b). Isolates from bovine meat showed a lower frequency of resistance to gentamicin, kanamycin, streptomycin, erythromycin, clindamycin, quinupristin/dalfopristin, trimethoprim and tetracycline than those from bovine animals.
Resistance data on eight isolates from broiler meat were reported by Austria in 2020 (Annex E, Table 7b). Five of those isolates were also resistant to erythromycin and clindamycin. However, cautious interpretation of these results is advised due to the small sample size of eight isolates.
Only six of the 11 isolates from sheep meat in 2020 and 10 of the 23 isolates from bovine meat in 2021 from Germany were resistant to tetracycline (Figure 58; see also Annex E, Table 7a,b). This is in line with the high proportion of non‐CC398 strains (n = 5) among these isolates. All non‐CC398 strains were susceptible to tetracycline. Resistance in more than one of the isolates was only observed for three antimicrobials: erythromycin (5 isolates), clindamycin (2) and trimethoprim (3). However, interpretation of the results needs caution on account of the limited number of isolates. Interestingly, one of the isolates from sheep meat was resistant to vancomycin, an antimicrobial of utmost importance for the treatment of MRSA infections in the medical field. Whole genome sequencing revealed that the isolate did not carry a specific vancomycin‐resistance gene. This is in accordance with the limited MIC value of 4 mg/l, i.e. one dilution step above the cut off.
6.5.2. Meat and food‐producing animals: multidrug resistance in MRSA isolates (excluding clinical investigations)
MRSA are typically resistant to penicillins and cephalosporins. Moreover, most isolates also show resistance to three or more substances and can be considered multi‐drug resistant (MDR). Overall, MDR patterns displayed substantial variability (Annex E, Table 8a). In 2021, 98% (289/295) of MRSA isolates reported in bovine animals, pigs and meat thereof from Switzerland, Germany and Belgium displayed MDR patterns. All MDR isolates were resistant to penicillin and cefoxitin.
All isolates from pigs (155/155) and calves (18/18) reported by Switzerland were MDR. The most common MDR pattern in pig isolates (27) displayed resistance to erythromycin, clindamycin, quinupristin/dalfopristin, tiamulin, trimethoprim and tetracycline. In contrast, the most common MDR pattern observed in calve isolates (4) included streptomycin, erythromycin, clindamycin and tetracycline. One‐hundred percent (79/79) of isolates from calves, dairy cows (15/15) and meat production bovine animals (4/4) from Belgium were MDR. Twenty‐eight of the MDR calf isolates were resistant to gentamicin, kanamycin, erythromycin, clindamycin, trimethoprim and tetracycline. Three isolates from dairy cows and two from meat production animals displayed resistance to kanamycin, streptomycin, chloramphenicol, rifampicin, erythromycin, sulfamethoxazole and tetracycline. Germany reported that 73.9% (17/23) of isolates from bovine meat were MDR. The most commonly reported MDR pattern included penicillin, cefoxitin and ciprofloxacin. This was the only MDR pattern identified without tetracycline resistance.
The most commonly described MDR pattern in isolates from 2020 included penicillin, cefoxitin and tetracycline (18/23 isolates). These were isolated from turkeys, broilers, broiler meat and sheep meat reported by Belgium, Austria and Germany (Annex E, Table 8b). Only five sheep meat isolates from Germany did not display resistance to tetracycline.
6.6. Discussion
The monitoring of MRSA in animals and food was voluntary in 2020 and 2021 and only a limited number of countries reported data on the occurrence of MRSA. Moreover, sampling and laboratory techniques are not fully harmonised across countries. Therefore, comparisons across countries should be done with prudence.
Recently, EFSA has published the technical specifications for a baseline survey to assess the prevalence of MRSA and the associated antimicrobial resistance in fattening pigs at the EU level (EFSA, 2022). The survey will also investigate the genetic diversity of the MRSA isolates, including lineages/strains and virulence factors. The timing of these surveys is planned to be harmonised between MSs to optimise the comparability of results. This will allow scientists to gain an overview of the current situation of MRSA in European pig populations.
Food: occurrence of MRSA
The monitoring of MRSA in various food products performed by MSs in 2020/2021 indicates that MRSA can be detected in different types of food. Imported meat may also play a role. However, occurrence varies between types of food and countries. While the numbers of investigated samples differed, MRSA were detected in all reported meat categories.
It should be underlined that the laboratory techniques used to detect MRSA employ selective bacterial culture and therefore, very low levels of contamination in food can be detected (Pauly et al., 2019). Although a previous report has cautiously suggested that some strains of LA‐MRSA may be adapted to colonise and infect humans and reported poultry meat as a possible source of MRSA for humans (Larsen et al., 2016), food is not generally considered to be a significant source of MRSA infection or colonisation of humans (EFSA, 2009a; FSA (Food Standards Agency), 2017). Nevertheless, MRSA is still frequently detected in animal food products and are considered to be a public health concern (da Silva et al., 2020; Titouche et al., 2022)
Animals: occurrence of MRSA
In 2020 and 2021 MRSA were reported in animals in the framework of monitoring programs, surveys and as a result of clinical investigations. While monitoring results and surveys will typically allow for an estimation of the occurrence of MRSA in the investigated animal population, this is not valid for clinical investigations due to the sampling bias associated with the clinical conditions. The comparison of the occurrence of MRSA in the animal populations is always hampered by the lack of precision and harmonisation of the definition of the animal populations. As AMR tends to differ between different animal populations of the same animal species, these differences need to be considered, when comparing the results from different reporting countries (Mesa Varona et al., 2020).
Another potential confounder could include the sampling strategy. Norway has been investigating pig herds in the framework of the control programme for several years, which could increase the likelihood of detecting positive herds even if they are rare.
The location of sampling could also influence the detection of MRSA, as Broens et al., 2011 found that batches of pigs at slaughter were more frequently positive than pigs at farm, potentially due to contamination of pigs during transport. Therefore, prevalence estimates should not be directly compared for the two sampling locations.
An additional aspect to be considered are differences in the types and numbers of samples collected. Sampling of nasal swabs is a frequent approach, but the numbers of samples tested may differ between countries with a likely effect on the prevalence estimate. Frequently, for the convenience of sample collection, dust from the housing environment is sampled despite concerns over the sensitivity of testing these samples (EFSA, 2012).
The occurrence of MRSA appears stable in veal calves and dairy cows from Belgium between 2012 and 2021, with a higher rate of detection in calves. Stable levels of MRSA have also been observed in calves from Switzerland between 2015 and 2021. In contrast, the occurrence of MRSA isolates detected in meat production animals in Belgium has slowly been reducing.
No MRSA was isolated in pigs from Norway in 2020 and 2021. This is in line with the low levels of MRSA identified in the previous years. These findings might be explained by the annual comprehensive surveillance programme of MRSA that Norway has implemented in their pig populations. In contrast, the occurrence of MRSA in pigs from Switzerland has slowly been increasing since 2010, with the occurrence in 2021 (53.6%) being only slightly higher than 2019 (52.8%). Kittler et al., 2019 suggested that the increase observed in Swiss pigs could be due to clonal complex 398 with the spa‐type t011, however, molecular data was not available for the isolates submitted and so this cannot be confirmed.
Occurrence of MRSA in flocks of broilers and laying hens in Belgium was very low in 2020, as it had been in previous years. The reason for this rare occurrence is not known yet as it contrasts with the regular detection of MRSA in broiler meat. MRSA were more often observed in turkey flocks from Germany, which was also previously reported for turkey carcases elsewhere (Vossenkuhl et al., 2014; El‐Adawy et al., 2016).
Typing findings of MRSA in animals and food
Some countries additionally reported data on spa‐type/clonal complex and antimicrobial susceptibility of the MRSA isolates from animals and food. The number of reported isolates was higher in 2021 than in 2020.
Among the isolates from animals with available typing results in 2020 and 2021, only six isolates reported in 2021 could not be assigned to CC398. This underlines the fact that CC398 widely dominates the MRSA from animals in the reporting countries. These six isolates originated from bovine animals. Remarkably, all isolates were from Belgium and five of the six isolates were assigned to CC8, a major clonal complex worldwide, including both hospital and community associated strains (Aires‐de‐Sousa, 2017; Turner et al., 2019). The identification of this CC in bovine animals could be due to the emergence of the bovine adapted strain belonging to CC8 which has been suggested to have made a jump from humans to bovines (Resch et al., 2013). The other non‐CC398 isolate was an ST1/CC1 of spa‐type t386, that has been identified in methicillin susceptible S. aureus isolated from chicken samples in Gabon and in MRSA isolated from a hedgehog in Spain (Lozano et al., 2016; Silva et al., 2020). The origin of such isolates is debatable. This spa‐type does not seem to be established in the food‐producing animal populations, the clonal complex has been described as being livestock associated. This particular isolate might have originated from people handling the animals as exchange of bacterial strains between animals and humans is likely for strains that can colonise several species. In 2020, typing information on isolates from animals was only provided for four isolates (two isolates from broiler flocks, and two from turkey flocks). These were all from the predominant spa‐type t011.
The livestock associated lineage of CC398 was also the most prevalent MRSA type detected in food with 68.5% of 124 typed isolates assignable to that CC in 2021 and 73.7% of 19 isolates in 2020. Remarkably, the proportion of non‐CC398 isolates in food is higher than in animals, which may indicate contamination at slaughterhouses or processing plants. This is in line with the literature and requires further targeted investigations (Tenhagen et al., 2014; Vossenkuhl et al., 2014). Isolates from broiler meat in Austria in 2020 were, however, all attributed to the CC398.
Isolates of other CCs (CC1, CC5, CC8, CC45, CC97, CC130) and of spa‐types assignable to other CCs were observed in a veal calf, dairy cows, cattle, meat from bovines and pigs in 2021. Interestingly, isolates from meat at border inspection posts were all non CC398. CC1 is commonly isolated in humans and is considered to be community‐associated, but has also been widely reported in livestock as well as wildlife in Europe (Silva et al., 2020). MRSA isolates belonging to CC5 have previously been observed in turkeys; however, this clonal complex is also a major HA‐MRSA lineage worldwide. CC45 was identified in a single MRSA isolate from pig meat. This CC is another widely disseminated clonal complex that is primarily associated with isolates from humans, suggesting potential contamination of the meat (Cuny et al., 2015). CC97 isolates have previously been associated with bovines (Käppeli et al., 2019) and pigs in Italy (Feltrin et al., 2016), but they have also been observed in human cases unrelated to animal production (Monecke et al., 2011; Boswihi et al., 2020). Therefore, their origin in food is doubtful. Isolates of CC130 harbouring the mecC gene have been observed in horses, cattle and sheep before (Paterson et al., 2014; Haenni et al., 2015; Giacinti et al., 2017; Islam et al., 2017). However, they are also a medical concern (Lozano et al., 2020).
Further typing data would in many cases provide useful additional information to aid classification and help assess the origin and significance of the MRSA isolates. For example, possession of the IEC genes (chp, sak and scn) is considered an adaptation facilitating colonisation and infection of humans and is not usually a feature seen in animal strains (Cuny et al., 2015; Larsen et al., 2016). Similarly, the presence of the PVL toxin is a virulence feature typically associated with most CA‐MRSA strains; other genetic factors can be associated with particular strains or may suggest a particular host preference (e.g. lukM has been associated with certain animal strains, particularly those affecting ruminants). Some genomic factors that seem to be associated with MRSA strains that shifted from human hosts to animals included the vwb gene, an animal specific virulence factor that is associated with clotting of animal plasma, and a novel staphylococcal cassette chromosome mec island (Resch et al., 2013; Yu et al., 2021).
Antimicrobial resistance in MRSA from animals and food
Antimicrobial resistance of MRSA differed substantially between the different origins of the bacteria. In line with the literature, MRSA of CC398 were mostly resistant to tetracycline and lower resistance rates to tetracycline were only observed if MRSA of other CCs were involved, e.g. in meat from a pig in Germany in 2021 and meat from sheep in Germany 2020. Here, all five non‐CC398 isolates were susceptible to tetracycline. Resistance to important medical drugs for the treatment and control of MRSA was overall extremely low. However, resistance to vancomycin was observed in an isolate from sheep meat in Germany in 2020, and resistance to rifampicin was detected in isolates from dairy cows and bovine meat from Belgium in 2021.
The occurrence of these types of resistance is worrisome as vancomycin is one of the preferred drugs of choice to treat MRSA infections, and rifampicin is often used in combination with vancomycin to treat implant associated S. aureus infections (Guo et al., 2021; Maraolo et al., 2021). Interestingly the rifampicin resistant isolates all belonged to ST239, which has been associated with high rates of rifampicin resistance previously (Guo et al., 2021). The vancomycin resistant isolate did not harbour one of the typical vancomycin resistance genes, which is in line with the limited increase in the MIC (4 mg/L). These moderate increases are typically caused by multiple point mutations rather than by specific vancomycin resistance genes like vanA or vanB (McGuinness et al., 2017). Fortunately, resistance to other medically important drugs for the control of MRSA such as mupirocin was not observed in 2020/2021. Mupirocin is an important component of the decolonisation therapy used prior to surgery in MRSA positive patients.
Temporal trends of MRSA occurrence in various types of meat and food‐producing animals
In 2018, the recommended method for the isolation of MRSA was revised by the EURL‐AR from the 2‐S method (which comprised a pre‐enrichment step and a selective enrichment step) to the 1‐S method (whereby the selective enrichment step is omitted). Therefore, and because of the limited number of reported samples, direct comparisons of longitudinal data obtained using different protocols should be performed with caution. In line with these limitations, we did not perform statistical trend analyses but only presented changes over time descriptively.
The Netherlands reported an incremental annual increase in the occurrence of MRSA isolated from meat from bovines under 1 year old between 2018 and 2021. This might be due to contamination of the meat by workers and the environment of the slaughterhouses, or perhaps the bovine population has been exposed to MRSA via farmers. A recent review suggested that MRSA isolation in dairy cows from the Netherlands might be due to exposure to pigs or pig farmers (Lam et al., 2020). Pig populations and pig farmers in the Netherlands have been shown to have a high prevalence of MRSA (Dierikx et al., 2016). We do not have 2021 data on MRSA occurrence in fattening pigs from Netherlands and the isolation of MRSA seemed to decrease from 2019 to 2020; however, this could be linked to a small sample size in 2020. Low rates of MRSA isolation in the pig population could also be due to the 69.6% reduction in antimicrobial usage by Dutch farmers (those raising broilers, pigs and veal calves) between 2009 and 2019 (Mallioris et al., 2022). However, a recent review noted that despite a decrease in antimicrobial usage in European animal production in recent years, the occurrence of MRSA in farm animals has not decreased. It was suggested that this is most likely due to other reservoirs of MRSA such as farm workers and veterinarians (Crespo‐Piazuelo and Lawlor, 2021).
Similarly, Austria has also reported an increase in MRSA detected in samples from pig and bovine meat in 2021 compared to 2019. Without data on MRSA isolation in live pigs and bovines it is difficult to say whether this might be due to an increase of MRSA colonisation in farm animals or whether this could be due to contamination at the slaughterhouses. The occurrence of MRSA isolated from fattening pigs reported by Switzerland also increased annually from 2010 to 2021, with a marked increase noted from 2015 to 2017. This increase most likely represents the dissemination of particular livestock‐associated spa‐types in Swiss fattening pig populations; and where molecular typing data were available, all isolates in 2017 and 2019 were those associated with CC398, with most belonging to spa‐types t011 and t034 in 2017. A longitudinal study carried out by Kraemer et al. (2017) also supports these trends, in which MRSA occurrence of pig farms in Western Switzerland were reported to increase from 7.3% in 2008 to 31% in 2015.
The complete epidemiological data should however be considered when evaluating trends apparent in this chapter, because the summary data reported to EFSA may not include full details of any changes to methodology or monitoring procedures. A detailed longitudinal study illustrated that pigs are intermittently and repeatedly colonised, and that colonisation may also occur during transportation and while being in the lairage (Bangerter et al., 2016). The detection of intermittent, repeated colonisation suggests that the number of animals sampled as part of a batch, including whether individual animals are sampled to represent a herd or batch, is likely to influence the batch or herd occurrence obtained. These factors should therefore be taken into consideration when comparing trends, as the Swiss annual MRSA monitoring examines a single pig from a herd at slaughter.
Abbreviations
- %
Percentage
- % f
Percentage frequency of isolates tested
- % Res
Percentage of resistant isolates
- AMC
Antimicrobial consumption
- AMR
Antimicrobial resistance
- AMS
Antimicrobial stewardship
- AST
Antimicrobial susceptibility test
- CA‐MRSA
Community associated MRSA
- CASFM
Comité de l'Antibiogramme de la Société Française de Microbiologie
- CBP
Clinical breakpoints
- CC
Clonal complex
- CI
Confidence interval
- CIA
Critically important antimicrobial
- CLSI
Clinical and Laboratory Standards Institute
- CS
Complete susceptibility
- CP
Carbapenemase producer
- DD
Disc diffusion method
- DL
Dilution/dilution method
- DLG
Dilution with gradient step
- EARS‐Net
European Antimicrobial Resistance Surveillance Network
- ECDC
European Centre for Disease Prevention and Control
- ECOFF
Epidemiological cut‐off value
- EEA
European Economic Area
- EFTA
European Free Trade Association
- EMA
European Medicines Authority
- ESBL
extended spectrum beta‐lactamase
- ESC
extended spectrum cephalosporins
- EUCAST
European Committee on Antimicrobial Susceptibility Testing
- EURL‐AR
EU Reference Laboratory for Antimicrobial Resistance
- EUSR
European Union Summary Report
- FWD
Food‐ and Waterborne Diseases and Zoonoses
- HaDEA
European Health and Digital Executive Agency
- HA‐MRSA
Hospital associated MRSA
- hpCIA
Highest‐priority critically important antimicrobials
- I
Intermediate
- IEC
Immune evasion cluster
- IPC
Infection, prevention, and control
- KOIESC
Key outcome indicator of ESBL‐ and/or AmpC‐producing E. coli
- LA‐MRSA
Livestock associated MRSA
- MDR
Multi‐drug resistant
- MDRI
Multi‐drug resistant islands
- MIC
Minimum inhibitory concentration
- MLST
Multi‐locus sequence typing
- MRSA
Methicillin‐resistant Staphylococcus aureus
- MS
Member State
- NA
Not applicable/not available
- NCP
National Control Programme
- NRL
National Reference Laboratory
- NTS
Non‐typhoidal Salmonellas
- OECD
Organisation for Economic Cooperation and Development
- PCR
Polymerase chain reaction
- PMQR
Plasmid‐mediated quinolone resistance
- PVL
Panton valentine leukocidin
- Q
Quantitative
- QRDR
Quinolone resistance‐determining regions
- R
Resistant
- RCs
Reporting countries
- res1–res9
Resistance to one antimicrobial substance/resistance to nine antimicrobial substances of the common set for Salmonella
- S
Susceptible
- SIR
Susceptible, intermediate, resistant
- ST
Sequence type
- SYN
Synergy
- TESSy
The European Surveillance System
- WGS
Whole genome sequencing
- WHO
World Health Organization
Antimicrobial substances
- AMC
Amoxicillin/clavulanate
- AMK
Amikacin
- AMP
Ampicillin
- AZM
Azithromycin
- CLA
Clavulanate
- CTZ/CAZ
Ceftazidime
- CHL
Chloramphenicol
- CIP
Ciprofloxacin
- CLI
Clindamycin
- COL
Colistin
- CTX
Cefotaxime
- ERT/ETP
Ertapenem
- ERY
Erythromycin
- CFT
Cefoxitin
- FUS
Fusidic acid
- GEN
Gentamicin
- KAN
Kanamycin
- LZD
Linezolid
- MEM
Meropenem
- MUP
Mupirocin
- NAL
Nalidixic acid
- PEN
Penicillin
- PEF
Pefloxacin
- QD
Quinupristin/Dalfopristin
- RIF
Rifampicin
- SMX
Sulfonamides
- STR
Streptomycin
- SUL
Sulfonamides
- SXT
Trimethoprim‐sulfamethoxazole
- TET/TCY
Tetracycline
- TIA
Tiamulin
- TIG
Tigecycline
- TMP
Trimethoprim
MSs of the EU and other reporting countries
- AT
Austria
- BE
Belgium
- BG
Bulgaria
- HR
Croatia
- CY
Cyprus
- CZ
Czechia
- DK
Denmark
- EE
Estonia
- FI
Finland
- GR
France
- DE
Germany
- EL
Greece
- HU
Hungary
- IE
Ireland
- IT
Italy
- LV
Latvia
- LT
Lithuania
- LU
Luxembourg
- MT
Malta
- NL
Netherlands
- PL
Poland
- PT
Portugal
- RO
Romania
- SK
Slovakia
- SI
Slovenia
- ES
Spain
- SE
Sweden
Non‐MSs reporting
- AL
Albania
- IS
Iceland
- MK
Republic of North Macedonia
- NO
Norway
- CH
Switzerland
- UK
United Kingdom
Definitions
| ‘Antimicrobial‐resistant isolate’ | In the case of quantitative data, an isolate was defined as ‘resistant’ to a selected antimicrobial when its minimum inhibitory concentration (MIC) value (in mg/L) was above the cut‐off value or the disc diffusion diameter (in mm) was below the cut‐off value. The cut‐off values, used to interpret MIC distributions (mg/L) for bacteria from animals and food, are shown in Appendix F ‘Material and methods’, Tables F.5–F.7. |
| In the case of qualitative data, an isolate was regarded as resistant when the country reported it as resistant using its own cut‐off value or break point. | |
| ‘Level of antimicrobial resistance’ | The percentage of resistant isolates among the tested isolates. |
| ‘Reporting MS group’ | Member States (MSs) that provided data and were included in the relevant table for antimicrobial resistance data for the bacteria–food/animal category–antimicrobial combination. |
| Terms used to describe the levels of antimicrobial resistance | Rare: < 0.1% |
| Very low: 0.1%–1.0% | |
| Low: > 1.0–10.0% | |
| Moderate: > 10.0% to 20.0% | |
| High: > 20.0% to 50.0% | |
| Very high: > 50.0% to 70.0% | |
| Extremely high: > 70.0% |
Table F.5.
Panel of antimicrobial substances included in AMR monitoring, thresholds for interpreting resistance and concentration ranges tested in Salmonella spp. and indicator commensal E. coli (first panel) based on Commission Implementing Decision (EU) 2020/1729 and EFSA Technical Report 2021
| Antimicrobial |
Salmonella EU surveillance 2021 EUCAST ECOFF* |
E. coli EU surveillance 2021 EUCAST ECOFF* |
Concentration range, mg/L (no. of wells) |
|---|---|---|---|
| Amikacin (a) | > 4 | > 8 | 4–128 (6) |
| Ampicillin | > 8 | > 8 | 1–32 (6) |
| Azithromycin (b) | > 16 | > 16 | 2–64 (6) |
| Cefotaxime | > 0.5 | > 0.25 |
0.25–4 (5) (c) 0.25–64 (9) (d) |
| Ceftazidime | > 2 | > 0.5 |
0.25–8 (6) (c) 0.25–128 (10) (d) |
| Chloramphenicol | > 16 | > 16 | 8–64 (4) |
| Ciprofloxacin | > 0.06 | > 0.06 | 0.015–8 (10) |
| Colistin | > 2 | > 2 | 1–16 (5) |
| Gentamicin (e) | > 2 | > 2 | 0.5–16 (6) |
| Meropenem | > 0.125 | > 0.125 | 0.03–16 (10) |
| Nalidixic acid | > 8 | > 8 | 4–64 (5) |
| Sulfamethoxazole | > 256 | > 64 | 8–512 (7) |
| Tetracycline | > 8 | > 8 | 2–32 (5) |
| Tigecycline | > 0.5 | > 0.5 | 0.25–8 (6) |
| Trimethoprim | > 2 | > 2 | 0.25–16 (7) |
AMR: antimicrobial resistance; ECOFFs: epidemiological cut‐off values; EUCAST: European Committee on Antimicrobial Susceptibility Testing.
EUCAST epidemiological cut‐off values. ‘>’ than the ECOFF, criteria used to determine microbiological resistance.
EUCAST epidemiological cut‐off (ECOFF) value for Salmonella is tentative.
EUCAST epidemiological cut‐off (ECOFF) value for E. coli is tentative.
Range to be used when the substance is tested in panel 1.
Range to be used when the substance is tested in panel 2.
EUCAST epidemiological cut‐off (ECOFF) value for Salmonella is 1 mg/L.
Table F.7.
Panel of antimicrobial substances, EUCAST ECOFFs and concentration ranges used for testing Salmonella spp. and indicator commensal E. coli isolates resistant to cefotaxime, ceftazidime or meropenem (second panel)
| Antimicrobial |
Salmonella EU surveillance 2021 EUCAST ECOFF* |
E. coli EU surveillance 2021 EUCAST ECOFF* |
Concentration range, mg/L (no. of wells) |
|---|---|---|---|
| Cefepime (a) | > 0.125 | > 0.125 | 0.06–32 (10) |
| Cefotaxime | > 0.5 | > 0.25 |
0.25–4 (5) (b) 0.25–64 (9) (c) |
| Cefotaxime + clavulanic acid | > 0.5 | > 0.25 | 0.06–64 (11) |
| Cefoxitin | > 8 | > 8 | 0.5–64 (8) |
| Ceftazidime | > 2 | > 0.5 |
0.25–8 (6) (b) 0.25–128 (10) (c) |
| Ceftazidime + clavulanic acid | > 2 | > 0.5 | 0.125–128 (11) |
| Ertapenem (d) | > 0.06 | > 0.06 | 0.015–2 (8) |
| Imipenem | > 1 | > 0.5 | 0.12–16 (8) |
| Meropenem | > 0.125 | > 0.125 | 0.03–16 (10) |
| Temocillin | > 16 | > 16 | 0.5–128 (9) |
AMR: antimicrobial resistance; ECOFFs: epidemiological cut‐off values; EUCAST: European Committee on Antimicrobial Susceptibility Testing.
EUCAST epidemiological cut‐off values. ‘>’ than the ECOFF, criteria used to determine microbiological resistance.
EUCAST epidemiological cut‐off (ECOFF) value for E. coli is 0.25 mg/L.
Range to be used when the substance is tested in panel 1.
Range to be used when the substance is tested in panel 2.
EUCAST epidemiological cut‐off (ECOFF) value for E. coli is tentative 0.03 mg/L.
Appendix A – High‐level resistance to ciprofloxacin among certain Salmonella serovars recovered from poultry origins as well as a single isolate from a fattening pig
High‐level resistance to ciprofloxacin in S. Kentucky
Considering individual serovars, in 2020, S. Kentucky accounted for most of the Salmonella isolates recovered from the poultry origins which exhibited MICs to ciprofloxacin of ≥ 4 mg/L. Within each of the poultry origins, the highest number of Salmonella isolates exhibiting high‐level resistance to this antimicrobial were attributed to S. Kentucky; this serovar accounted for 86.4%, 91.7%, 76.5%, 100% and 93.1% of the total number of isolates displaying MICs of ≥ 4 mg/L from broiler carcases, turkey carcases, broilers, laying hens and turkeys, respectively. Additionally, in 2021, only a single isolate recovered from a fattening pig also displayed high‐level ciprofloxacin resistance and was serotyped as S. Kentucky. No Salmonella spp. isolates from calves displayed high‐level resistance to ciprofloxacin.
S. Kentucky isolates exhibiting high‐level ciprofloxacin resistance are likely to belong to the multilocus sequence type (ST) 198 clone, which has shown epidemic spread, first in Africa, then the Middle East, Asia and finally Europe (Le Hello et al., 2011, 2013; Hawkey et al., 2019). Notably in 2018, the occurrence of this serovar exhibiting high‐level resistance was observed by many MSs from most parts of Europe, suggesting further clonal expansion (S. Kentucky ST198‐X1) within poultry populations. In view of reported MIC values, most of the S. Kentucky isolates exhibiting high‐level ciprofloxacin resistance in 2020/2021 displayed MICs of ≥ 8 mg/L. Additionally, a very high proportion of the poultry S. Kentucky isolates displaying ciprofloxacin MICs of ≥ 4 mg/L were also multiresistant, primarily showing resistance to ampicillin, gentamicin, nalidixic acid, sulfamethoxazole and tetracycline (AMP‐CIP‐GEN‐NAL‐SMX‐TET). The single isolate from the fattening pig showing high resistance to ciprofloxacin, was also resistant to nalidixic acid (with an MIC > 64 mg/L for nalidixic acid), sulfamethoxazole, tetracycline and trimethoprim.
Figure A.1 presents the overall AMR levels among MDR S. Kentucky isolates from poultry which exhibited high‐level ciprofloxacin resistance.
Figure A.1.
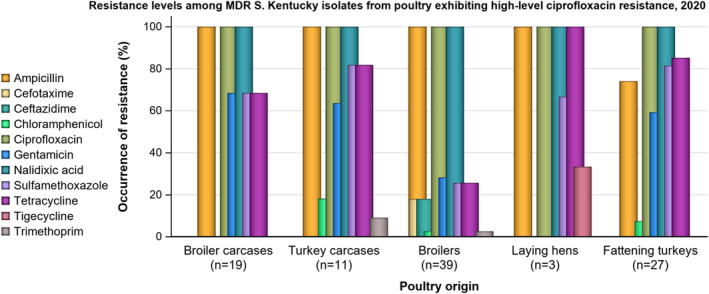
-
n: Total number of S. Kentucky isolates exhibiting high‐level ciprofloxacin resistance.NB: A single S. Kentucky isolate recovered from a fattening pig in 2021 with high‐level ciprofloxacin resistance was also resistant to nalidixic acid only and susceptible to all the other antimicrobials tested. None of the S. Kentucky isolates reported in poultry exhibited either azithromycin or colistin resistance.
In 2021, S. Kentucky was the 21st most commonly reported serovar in humans, with 145 cases reported in EU/EEA countries. From the monitoring of human cases in 2021, high to extremely high levels of resistance were noted to gentamicin (27.9%), sulfonamides (51.6%), ampicillin (62.9%), tetracyclines (58.1%), ciprofloxacin (78.1%) and nalidixic acid (79.7%); consistent with the multiresistance patterns observed in isolates from the monitoring of poultry in 2020, and the possible dissemination of the S. Kentucky ST198 strain within Europe. Furthermore, of 6,162 Salmonella isolates from humans where ciprofloxacin MIC data was available, 76 of these (1.2%) exhibited MICs of ≥ 4 mg/L, of which S. Kentucky accounted for 56 (73.7%).
Hawkey et al. (2019) recently documented that MDR S. Kentucky ST198 is a globally disseminated clone, capable of rapid spread and accumulation of resistance determinants to last‐line antimicrobials. Acquisition of Salmonella genomic island 1 (SGI1) and plasmids, as well as mutations in the Quinolone Resistance‐determining regions (QRDR), were the only genetic features found during this study to explain the global epidemiological success of the MDR S. Kentucky ST198 lineage which is highly resistant to ciprofloxacin. Coipan et al. (2020) describe how a clone of this lineage, with an ESBL‐gene (bla CTX‐M‐14b) incorporated on the chromosome, has emerged in Europe. In contrast to plasmid‐mediated resistance, chromosomal‐mediated resistance is most likely to be maintained also without antibiotic pressure, especially if it incurs no fitness cost for the bacteria.
High‐level resistance to ciprofloxacin among other Salmonella serovars
In 2020, while S. Kentucky generally accounted for an important number of the Salmonella isolates exhibiting high‐level resistance to ciprofloxacin, there was also a significant contribution from S. Infantis in broilers and broiler carcases, many other serovars exhibiting resistance by this definition were noted among the poultry origins (namely S. Newport, S. Derby and S. Bredeney). Figure A.2 shows the number of isolates exhibiting high‐level resistance to ciprofloxacin by serovar within each of the poultry origins. Considering ciprofloxacin MICs among the serovars presented in Figure A.2 (excluding S. Kentucky), MICs of 4 mg/L were reported in S. Derby (from turkeys), S. Infantis and S. Newport (from broiler carcases), S. Bredeney (from turkey carcases), S. Infantis and S. Newport (from broilers).
Figure A.2.
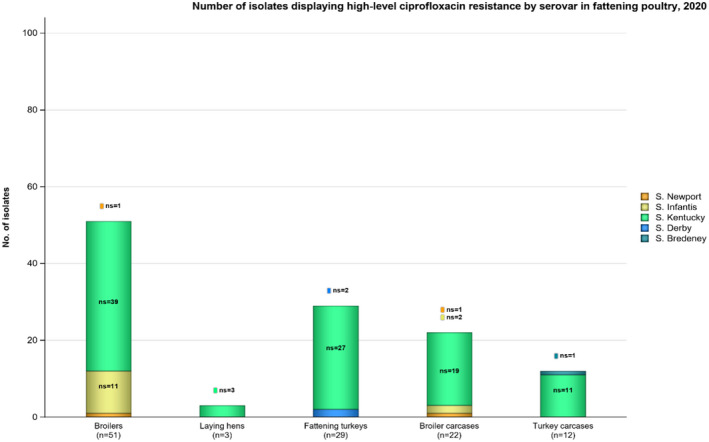
- n: Total number of Salmonella isolates exhibiting high‐level ciprofloxacin resistance; ns: number of isolates by serovar exhibiting high‐level ciprofloxacin resistance; In addition, a single S. Kentucky isolate displaying high‐level ciprofloxacin resistance was also recovered from a fattening pig in 2021.
Appendix B – Cefotaxime, ceftazidime and ciprofloxacin resistance in Salmonella spp. recovered from each of the animal/carcase origins and humans considering all reporting MSs in 2020/2021
Table B.1.
Occurrence of resistance to third‐generation cephalosporins and fluoroquinolones in non‐typhoidal Salmonella spp. from food‐producing animals, animal carcases and humans, reported by MSs in 2020/2021
| Human/animal category | No. of MSs | N | Cefotaxime | Ceftazidime | Ciprofloxacin/pefloxacin | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Humans – 2020* | See footnote below | – | 0.8 (a) | – | 0.8% (b) | – | 14.1% (c) | |
| Humans – 2021* | – | 1.1% (d) | – | 1.1% (e) | – | 14.9% (f) | ||
| Broiler carcases – 2020 | 18 MSs | 905 | 3 | 0.1% | 1 | 0.1% | 627 | 69.3% |
| Turkey carcases – 2020 | 8 MSs | 320 | 0 | 0% | 0 | 0% | 150 | 46.9% |
| Broilers – 2020 | 22 MSs | 1,953 | 39 | 2.0% | 40 | 2.1% | 1,123 | 57.5% |
| Laying hens – 2020 | 24 MSs | 1,030 | 4 | 0.4% | 4 | 0.4% | 196 | 19.0% |
| Fattening turkeys – 2020 | 16 MSs | 674 | 3 | 0.5% | 3 | 0.5% | 438 | 65.0% |
| Fattening pigs – 2021 | 26 MSs + XI | 1,258 | 11 | 0.9% | 11 | 0.9% | 127 | 10.1% |
| Calves (< 1 year) – 2021 | 10 MSs | 79 | 2 | 2.5 | 1 | 1.3 | 10 | 12.7% |
N: Total number of isolates tested/reported by MSs; n: Total number of isolates resistant; MSs: Member states.
In most countries using disk diffusion methods, ciprofloxacin has been replaced by pefloxacin for screening for fluoroquinolone resistance, as recommended by EUCAST.
N = 7,101, 19 MSs.
N = 6,000, 16 MSs.
N = 6,906, 20 MSs.
N = 11,572, 22 MSs.
N = 10,385, 21 MSs.
N = 11,725, 23 MSs.
Appendix C – Occurrence of antimicrobial resistance at the Salmonella serovar level
In carcases of food‐producing animals
Breakdown of the most prevalent serovars
The detailed reporting of results at the serovar level clearly demonstrated the major contribution of a few serovars to the observed occurrence of resistance in Salmonella spp. Figure C.1 illustrates the relative contribution of some of the most dominant serovars recovered from each of the carcase origins considering all reporting countries (including non‐MSs). In broiler carcases, six serovars (Infantis, Enteritidis, Agona, Montevideo, Indiana and Chester) accounted for 76.3% of Salmonella isolates; while in turkey carcases, Bredeney, Hadar, Indiana, monophasic Typhimurium and Kentucky accounted for 57.5% of Salmonella spp. isolated from this origin. Other serovars represented about 30% of the Salmonella isolates reported in both broiler and turkey carcases.
Figure C.1.
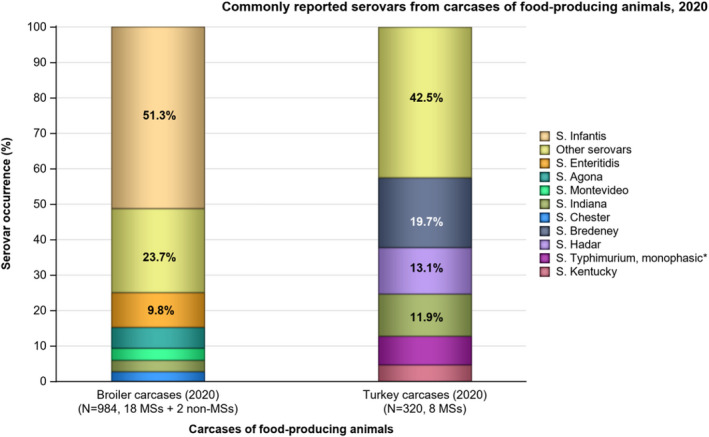
- *Monophasic S. Typhimurium includes antigenic formulas; serovars in the legend are listed according to their predominance within all the carcase origins.
Complete susceptibility and multidrug resistance
Patterns of resistance associated with these different serovars have a marked influence on the overall resistance levels in Salmonella spp., and Figure C.2 summarises the proportion of completely susceptible and MDR isolates among particular serovars recovered from each of these carcase origins considering all reporting countries (including non‐MSs). Large contributions of a few resistant serovars to the overall level of MDR among Salmonella spp. were evident within some of the carcase origins; notably S. Infantis (79.2%, 400/505) in broiler carcases (see Figure C.6).
Figure C.2.
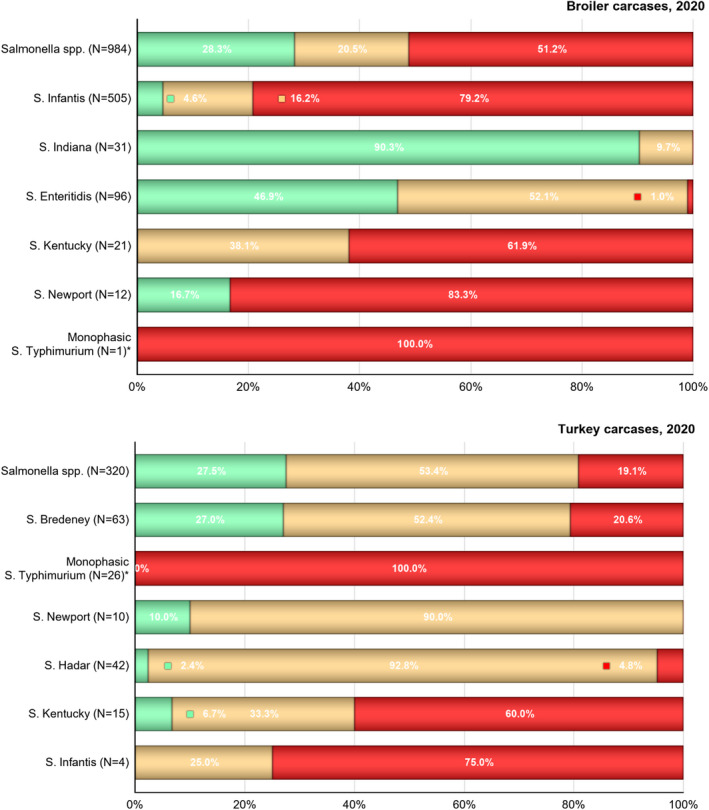
-
N: Total number of Salmonella spp. or total number of particular serovars recovered from the carcase monitoring.*Monophasic S. Typhimurium includes antigenic formulas. The ECOFF used to determine resistance to tigecycline was MIC > 1 mg/L.
Figure C.6.
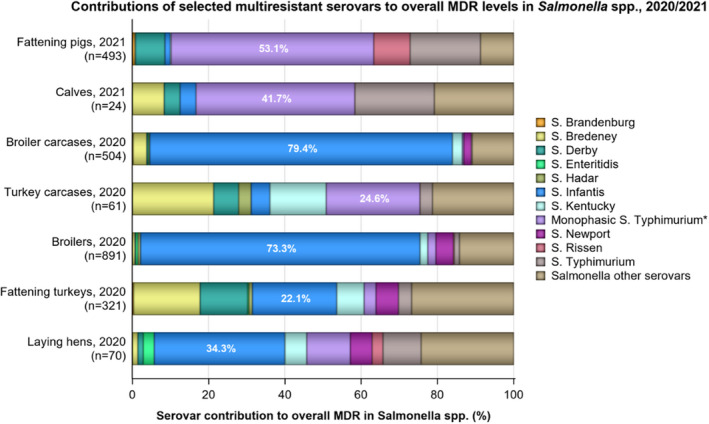
- n: Total number of Salmonella isolates exhibiting MDR; serovars contributing the highest levels of MDR to overall MDR levels in Salmonella spp. are illustrated with a percentage; *monophasic S. Typhimurium includes antigenic formulas; serovars in the legend are listed according to their predominance within all the animal/carcase origins.
In food‐producing animal populations
Breakdown of the most prevalent serovars
Considering all reporting countries (including non‐MSs), the relative contribution of some of the most dominant serovars recovered from each of the food‐producing animal populations is illustrated in Figure C.3. In pigs, six serovars (Derby, monophasic Typhimurium, Typhimurium, Rissen, Infantis and Brandenburg) accounted for 82.2% of Salmonella spp., while in calves, serovars monophasic Typhimurium, Typhimurium, Dublin, Bredeney, Stanleyville and Enteritidis accounted for 62.0% of the total Salmonella spp. recovered from this origin. Additionally, in broilers, six serovars (Infantis, Enteritidis, Kedougou, Montevideo, Mbandaka and Newport) accounted for 59.8% of Salmonella isolates, while in laying hens five serovars (Enteritidis, Kentucky, Infantis, Typhimurium and Mbandaka) accounted for 55.4% of isolates; and in turkeys, serovars Derby, Anatum, Infantis, Bredeney, Kedougou and Senftenberg accounted for 56.5% of Salmonella isolates.
Figure C.3.
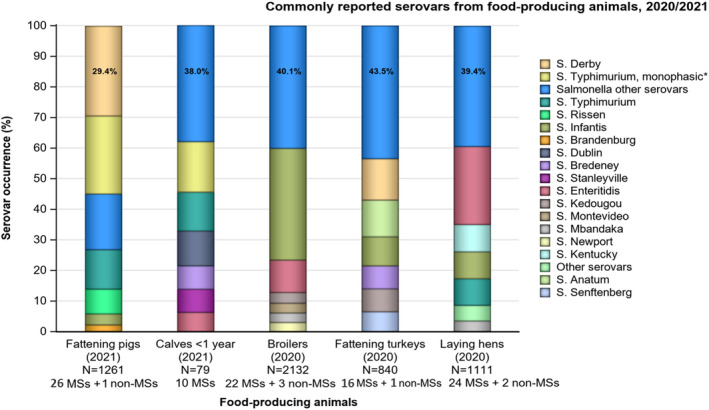
- *Monophasic S. Typhimurium includes antigenic formulas; serovars in the legend are listed according to their predominance within all the animal origins.
Complete susceptibility and multidrug resistance
In 2021, the ECOFF used to determine microbiological resistance of Salmonella isolates to tigecycline was changed from > 1 to > 0.5 mg/L (EFSA, 2021). Therefore, in this report, complete susceptibility (CS) and multidrug resistance (MDR) to tigecycline for 2021 data (i.e. pigs and calves) is determined using the new ECOFF (MIC > 0.5 mg/L). While for 2020 data from poultry populations and derived meat, tigecycline resistance is analysed using the previous ECOFF (i.e. MIC > 1 mg/L).
The patterns of resistance associated with these different serovars influenced the overall resistance levels in Salmonella isolates, and Figures C.4 and C.5 summarise the proportion of completely susceptible and MDR isolates among particular serovars recovered from each of these food‐producing animal populations considering all reporting countries (including non‐MSs).
Figure C.4.
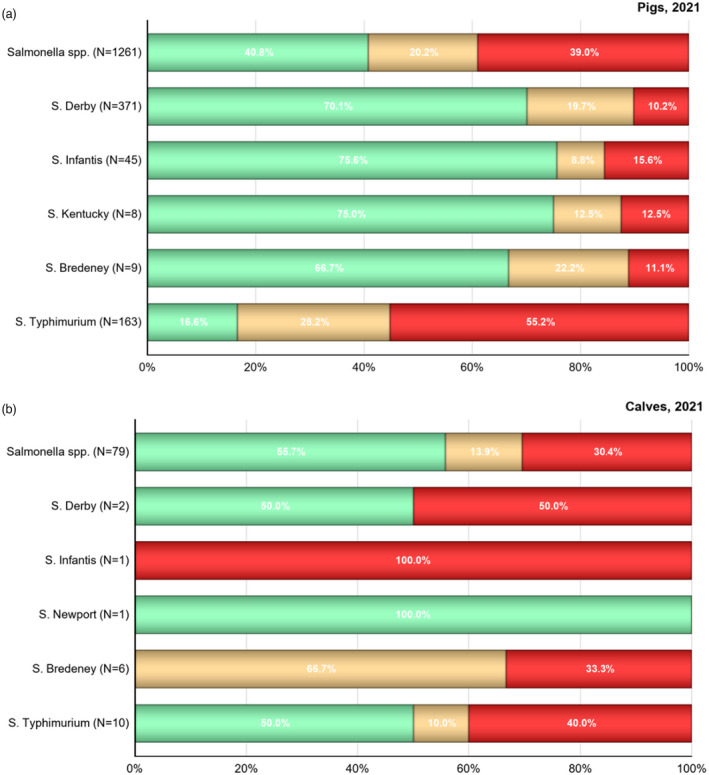
-
N: Total number of isolates recovered; *monophasic S. Typhimurium includes antigenic formulas.The MDR analysis of animal isolates included the following antimicrobials: ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/nalidixic acid, gentamicin/amikacin, meropenem, sulfamethoxazole, tetracycline/tigecycline and trimethoprim. In 2021, amikacin was also included in the analysis of pigs and calves, for the MDR analysis it was considered together with gentamicin for the aminoglycosides antimicrobial class The ECOFF used to determine resistance to tigecycline for pig and calf data was MIC > 0.5 mg/L, while for poultry data was MIC > 1 mg/L.
Figure C.5.
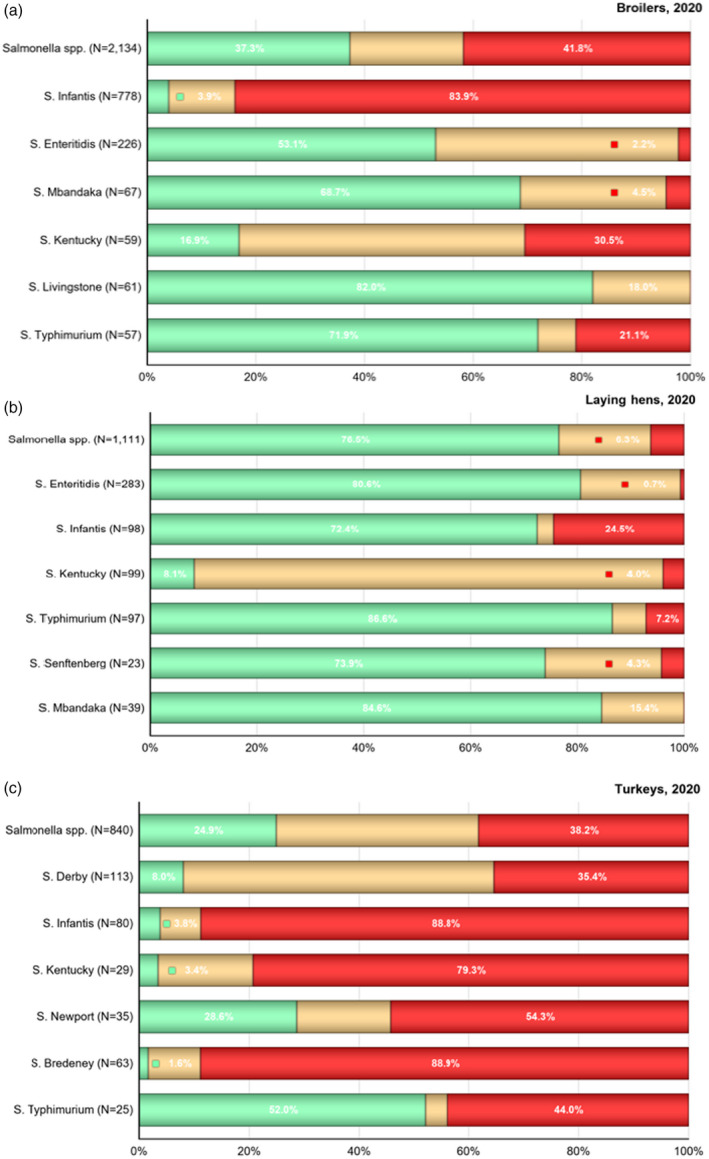
- N: Total number of isolates recovered; *monophasic S. Typhimurium includes antigenic formulas. The MDR analysis of animal isolates included the following antimicrobials: ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/nalidixic acid, gentamicin, meropenem, sulfamethoxazole, tetracycline, tigecycline and trimethoprim. The ECOFF used to determine resistance to tigecycline for poultry data was MIC > 1 mg/L while for pig and calf data MIC > 0.5 mg/L.
High proportions of MDR isolates were reported in the different food‐producing animal populations. For instance, 55.2% of the S. Typhimurium isolated in pigs were MDR. Similarly, the S. Infantis isolates from broilers were largely MDR (83.9%) (see Figures C.4 and C.5). Like in broilers, S. Infantis were the lead serovar contributing with MDR in laying hens (24.5%); while in turkeys, MDR isolates were mainly S. Infantis (88.8%), Bredeney (88.9%) and Kentucky (79.3%).
On the human side, 22.6% of 6,867 isolates were MDR, while 60.0% were susceptible to all tested antimicrobials (Annex A, Table 16). Furthermore, the most common MDR pattern in human Salmonella isolates was AMP‐SXT‐TET found in 209 isolates. This is also confirmed in Annex A, Table 1 where the human isolates showed the most resistant to ampicillin (25.3%, N = 11,832), sulfamethoxazole (26.8%, N = 6,872) and tetracycline (26.2%, N = 10,949). Only a few isolates (0.8%, N = 11,532) showed microbiological and clinical resistance to ciprofloxacin and cefotaxime (Annex A, Table 8).
Resistance exhibited by particular serovars
S. Derby was the most common serovar detected in fattening pigs (2021) and turkeys (2020), accounting for 29.4% and 14% of Salmonella isolates recovered from these animal origins, respectively (see Figure C.3). While multidrug resistance was not frequently observed among S. Derby isolates from pigs (10.2%, see Figure C.6), it was detected at high levels in the 2020 isolates from turkeys (35.4%, Figure C.5). Among S. Derby isolates recovered from these animal/carcase origins, different core resistance patterns predominated. In pigs, the most common resistance pattern in MDR S. Derby was AMP‐SXT‐TET, and was seen in isolates reported by Denmark, Estonia, Germany, Poland and Slovenia. Five of the MDR isolates from pigs were resistant to up to five classes of antimicrobials.
One of the two S. Derby isolated in calves was multidrug resistant. This isolate was reported by Spain with the pattern GEN‐CHL‐AMP‐CTX‐NAL‐CIP‐SMX‐TMP‐TET, including a third‐generation cephalosporin (see Figure C.4). The most frequently reported resistance pattern among MDR S. Derby isolates from turkeys was AMP‐NAL‐CIP‐SMX‐TMP‐TET (32/93, 34.4%).
In human isolates, 10.1% (N = 148) of S. Derby were MDR (Annex A, Table 22), with the predominant MDR pattern being AMP‐SXT‐TET. This is confirmed in Table 7 where human isolates showed mainly resistance to ampicillin (10.3%, N = 261), sulfamethoxazole (32.4%, N = 148) and tetracycline (19.3%, N = 259).
Under the new legislation (2020/1729/EU), the ECOFF used to determine microbiological resistance of Salmonella isolates to nalidixic acid changed from > 16 to > 8 mg/L, while the clinical breakpoint for ciprofloxacin changed from > 1 to 0.06 mg/L. In this report, the occurrence of resistance to nalidixic acid for 2021 data (i.e. pigs and calves) is determined using the new ECOFF (MIC > 8 mg/L), and for 2020 poultry and meat derived data, nalidixic acid resistance is analysed using the previous ECOFFs (MIC > 16 mg/L). Quinolone resistance (ciprofloxacin/nalidixic acid) was reported in the single MDR S. Derby isolate from a calf and in seven MDR isolates from pigs, while tigecycline resistance was observed in six isolates originating from pigs. Resistance to third‐generation cephalosporin was detected in the single MDR S. Derby isolated from a calf in Spain and in two isolates from pigs reported by Hungary and Romania. Moreover, the pig isolate from Hungary and the isolate from a calf exhibited an ESBL phenotype. Only a single isolate from a turkey (Poland) was determined to be resistant to third‐generation cephalosporins. This S. Derby isolate exhibited an ESBL phenotype. Where third‐generation cephalosporin resistance was reported in this turkey isolate, it did not display resistance to ciprofloxacin (MIC > 0.064 mg/L).
Recent studies on S. Derby originating from the pork and poultry sectors in France identified four major host‐specific lineages, corresponding to multilocus sequence typing (MLST) profiles ST39, ST40, ST71 and ST682 (Sévellec et al., 2018, 2020). The lineages ST39, ST40 and ST682 were associated with pork, and ST71 with poultry. While ST71 and ST682 isolates were generally devoid of resistance genes, ST40 isolates commonly harboured several resistance genes, with Clade 2 of this lineage characterised by SGI1 and the pattern of resistance to streptomycin, sulfonamides and tetracycline. Additionally, the presence of a resistance gene for fosfomycin was detected in all genomes from ST39 (Sévellec et al., 2020).
Monophasic S. Typhimurium was the main serovar recovered in calves and the second most frequently reported in pigs, accounting for 16.5% and 26.1% of Salmonella isolates recovered from these origins, respectively (see Figure C.3). The proportion of all Salmonella isolates showing MDR in calves and pigs was largely influenced by the occurrence of multidrug resistance monophasic S. Typhimurium, which accounted for 41.7% (10/24) and 53.1% (262/493), of the MDR Salmonella isolates recovered from these animal origins, respectively (Figure C.4). Similarly, this serovar contributed with the highest level of overall MDR among Salmonella isolates recovered from turkey carcases (24.6%, see Figure C.3).
Monophasic S. Typhimurium isolates were MDR in the majority of the carcasses/animal origins with resistance to ampicillin, sulfamethoxazole and tetracycline (AMP‐SMX‐TET) seen as the most frequent pattern in calves and pigs. This pattern with the addition of chloramphenicol was the second leading pattern in isolates from calves (AMP‐CHL‐SMX‐TET); however, in pig isolates the second leading pattern was an addition of ciprofloxacin and nalidixic acid to the core resistance pattern (AMP‐NAL‐CIP‐SMX‐TET).
Monophasic S. Typhimurium has spread widely among European pig populations. There are particular MDR patterns associated with monophasic S. Typhimurium and because this serovar is prevalent in many countries, these patterns greatly influenced the overall resistance figures. This is exemplified by the resistance pattern to ampicillin, sulfamethoxazole and tetracycline (AMP‐SMX‐TET) which occurred as the main MDR pattern in 159/493 (32.2%) monophasic S. Typhimurium isolates from pigs. This resistance pattern (together with resistance to streptomycin) is typical of the European clone of monophasic S. Typhimurium (Hopkins et al., 2010). The genes conferring resistance to these antimicrobials are commonly found in association together with IS26 mobile genetic elements, responsible for their integration at different chromosomal locations, in recently described European strains of monophasic S. Typhimurium (Sun et al., 2020). It is noteworthy that multidrug resistance in the European clone of monophasic S. Typhimurium appears to have originated from integration of MDR plasmids into the chromosome, facilitated by the presence of these IS26 mobile genetic elements (Sun et al., 2020).
Resistance to five or more classes of antimicrobials was observed among 31 monophasic S. Typhimurium isolates from pigs, with nine of them exhibiting resistance to six antimicrobial classes. No isolates from other animals/carcase origins showed such multi‐drug resistance. In human isolates, 78.4% (N = 1,235) of monophasic S. Typhimurium were MDR (Annex A, Table 19), with the predominant MDR pattern being AMP‐SXT‐TET (found in 187 isolates). This is confirmed in Table 4 where human isolates showed mainly resistance to ampicillin (88.2%, N = 1,958), sulfamethoxazole (85.2%, N = 1,236) and tetracycline (84.5%, N = 1,913). A few of these isolates (1.2%, N = 1,957) showed microbiological and clinical resistance to ciprofloxacin and cefotaxime (Annex A, Table 11). Notably, isolates from food‐producing animals, resistance to quinolones (ciprofloxacin/nalidixic acid) was only reported in pig isolates, accounting for 13.7% (36/262) of all MDR monophasic S. Typhimurium isolated from this origin. Similarly, tigecycline resistance was only reported in isolates from pigs (21/262). Resistance to third‐generation cephalosporins was rare in this serovar with a single isolate from a pig reported by Italy exhibiting resistance to cefotaxime/ceftazidime, its phenotype was confirmed by the presence of the bla SHV‐12 gene.
From the monitoring of human monophasic S. Typhimurium cases reported to ECDC in 2021, out of 1,867 isolates for which data were available, 23 had an ESBL phenotype and six had an AmpC phenotype, with genes encoding different types of CTX‐M enzymes as well as CMY‐2 enzymes detected.
S. Typhimurium was the second most frequently reported serovar from calves (2021), the third most commonly reported serovar from pigs (2021) and fourth in laying hens (2020); accounting for 12.7%, 12.9% and 7.7% of Salmonella isolates recovered from these origins, respectively (Figure C.3). Among S. Typhimurium isolates recovered from calves and pigs, MDR was also frequently observed: 40.0% and 55.2%, respectively (Figure C.4). MDR S. Typhimurium represented 44.0% of Salmonella spp. isolated from turkeys. Notably, the proportion of all Salmonella isolates showing MDR in calves and pigs was greatly influenced by the occurrence of multiresistant S. Typhimurium, which come second after monophasic Typhimurium in all the MDR Salmonella isolates recovered from these animal origins (see Figure C.6). The most frequent MDR pattern among S. Typhimurium isolates from pigs was AMP‐SXT‐TET with an addition of CHL to this pattern as the second most commonly encountered. Moreover, of the five MDR S. Typhimurium isolates recovered from calves, four different resistance patterns were noted, with the pattern TGC‐SMX‐TET observed in two isolates.
Mobile genetic elements which could account for this resistance pattern in S. Typhimurium isolates have previously been described. Salmonella genomic island 1 (SGI1), known to contain a multidrug resistance region located on a complex class 1 integron designated In104, confers pentavalent resistance (the ampicillin, chloramphenicol, streptomycin, sulfamethoxazole, tetracycline resistance phenotype – AMP‐CHL‐STR‐SMX‐TET) and has widely been documented in a range of Salmonella serovars.
In pigs, (fluoro)quinolone resistance (ciprofloxacin/nalidixic acid) was encountered in 23.1% of the 91 MDR S. Typhimurium isolates. However, only a single isolate from a calf showed this resistance. Tigecycline resistance among multiresistant S. Typhimurium isolates was reported in three isolates from calves and in 13.2% of the 91 pig isolates. While a single isolate from a calf was resistant to at least five classes of antimicrobials, 23.1% (21/91) MDR S. Typhimurium from pigs showed resistance to five or more antimicrobial classes. No MDR S. Typhimurium isolates recovered from any of the animal/carcase origins displayed resistance to third‐generation cephalosporins.
In human isolates, 23% (N = 871) of the serovar S. Typhimurium were MDR (Annex A, Table 18), with the predominant MDR pattern being AMP‐SXT‐TCY (found in 18 isolates and the addition of CHL to this pattern in 14 isolates). The human isolates showed mainly resistance to ampicillin (35.5%, N = 1,382), sulfamethoxazole (28.8%, N = 872) and tetracycline (28%, N = 1,330) (Annex A, Table 3). A few of the isolates (0.9%, N = 1,353) showed microbiological and clinical resistance to ciprofloxacin and cefotaxime (Annex A, Table 10). Additionally, of 1,246 human S. Typhimurium isolates for which data were available to ECDC in 2021, 11 isolates exhibited an ESBL phenotype and 1 isolates exhibited an AmpC phenotype; genes encoding different types of CTX‐M enzymes, as well as CMY‐2 enzymes, were detected.
Multiresistant S. Rissen isolates were recovered from pigs, broilers and laying hens, as well as carcases of broilers (see Figures C.2 and C.5). In 2021, S. Rissen isolates were detected mainly in pigs, representing 8.1% of the total Salmonella isolates from pigs (see Figure C.3), while only a single S. Rissen isolate was detected in calves. The majority of the S. Rissen isolated from pigs were MDR (93%, 44/47). A wide range of MDR patterns were observed in S. Rissen isolates from pigs with the leading pattern of resistance to ampicillin, chloramphenicol, sulfamethoxazole, tetracycline and trimethoprim (AMP‐CHL‐SMX‐TET‐TMP) being detected in five isolates. García‐Fierro et al. (2016) previously identified a dominant S. Rissen clone in pigs, pork and humans in Spain, which was shown to carry genes conferring resistance to ampicillin, chloramphenicol, streptomycin, sulfonamides, tetracycline and trimethoprim (AMP‐CHL‐STR‐SMX‐TET‐TMP) at varying frequencies, mostly on integrons. S. Rissen is also a common serovar in pigs, chicken, pork and man in some parts of Asia. (Pornsukarom et al., 2015) demonstrated that S. Rissen isolates originating from Thai pig farms were frequently multidrug resistant to most of the antimicrobials listed above.
A single S. Rissen isolate recovered from a broiler carcase also exhibited resistance to ampicillin, chloramphenicol, sulfamethoxazole, trimethoprim and tetracycline (AMP‐CHL‐SMX‐TMP‐TET). In broilers, where 2/7 (28.8%) S. Rissen isolates exhibited MDR, four different combinations were noted (the most common being the pattern: AMP‐CTX‐CHL‐CIP‐GEN‐SXT‐TMP‐TET). Resistance to six antimicrobial classes was also observed among isolates from broilers; however, 22 isolates from pigs showed resistance to at least five classes of antimicrobials with one isolate reported by Romania exhibiting resistance to seven antimicrobial classes. The core pattern of resistance AMP‐SXT‐TET‐TMP was noted in the only two MDR S. Rissen isolates recovered from laying hens (N = 12). Tigecycline resistance was not a feature of any of the MDR S. Rissen isolates recovered from these animal/carcase origins. Resistance to quinolones (ciprofloxacin/nalidixic acid) was reported in 51.1% (24/47) of isolates from pigs, while 16 of such isolates showed resistance to tigecycline. Four isolates reported by Romania displayed resistance to third‐generation cephalosporins (CTX‐CAZ), and all exhibited an ESBL phenotype; one of which has in addition an AmpC phenotype.
Considering S. Infantis, this serovar was most frequently recovered from broilers and their derived carcases, accounting for 36.4% and 50.3% of Salmonella isolates recovered from these origins, respectively (see Figures C.1 and C.3). Additionally, this serovar was the second most frequently reported in turkeys (9.5%), and the third most frequently reported in laying hens (8.8%). While MDR was common among S. Infantis isolates from broilers and turkeys as well as their derived carcases, (84.0%, 88.8%, 79.8% and 75.0%, respectively), isolates recovered from laying hens (N = 98) were less frequently MDR (24.5%). Notably, the proportion of all Salmonella isolates showing MDR in broilers and their derived carcases was greatly influenced by the occurrence of multiresistant S. Infantis, which accounted for 84% (653/777) and 79.8% (399/500) of the MDR Salmonella isolates from these origins, respectively (see Figures C.2 and C.5). Similarly, this serovar contributed the highest levels of multiresistance to overall MDR among Salmonella isolates recovered from laying hens, turkeys and turkey carcases (as did monophasic S. Typhimurium in turkey carcases).
Although a wide range of different MDR patterns were reported among S. Infantis isolates from poultry, the most frequent core MDR pattern was AMP‐CIP‐NAL‐SXT‐TET. This resistance pattern is typical of a major European clone of S. Infantis which is prevalent among broilers (Nógrády et al., 2012). Where MDR was detected, this resistance profile (resistance to only ampicillin, ciprofloxacin, nalidixic acid, sulfamethoxazole and tetracycline) accounted for 26.8%, 95.6%, 95.5%, 83.7%, 81.9% of MDR patterns, respectively. Previous scientific publications in Europe highlight the involvement of plasmids, which appear to be responsible for resistance in many European MDR S. Infantis isolates (Nógrády et al., 2012; Franco et al., 2015). In Australia, a S. Infantis strain harbouring a SGI1 homologue with an integron related to In104 and conferring resistance to streptomycin, sulfamethoxazole and trimethoprim was identified (Levings et al., 2005). Resistance to five antimicrobial classes was noted among isolates from all poultry origins, with the exception of turkey carcases where all isolates displayed the core resistance pattern as described above (CIP‐NAL‐SMX‐TET). Resistance to six antimicrobial classes was noted among isolates from broilers and turkeys, as well as a single isolate from laying hens; while four isolates from broilers also displayed resistance to seven antimicrobial classes. Additionally, tigecycline resistance was observed among some MDR isolates from poultry, with the exception once more of turkey carcases. Multiresistant S. Infantis was also reported from pig carcases; of only five MDR isolates, four different combinations were noted, of which resistance to sulfamethoxazole and tetracycline was a feature of all five isolates.
Resistance to third‐generation cephalosporins was detected in 34 S. Infantis isolates recovered from broilers, 30 originating from Italy (all displaying an ESBL phenotype, with 6/30 also exhibiting an AmpC phenotype) and 4 from Hungary (2 exhibiting an ESBL phenotype and 2 exhibiting an AmpC phenotype). Additionally, Italy reported resistance to this antimicrobial class in 7/12 S. Infantis isolates from turkeys and in 1/11 isolates from laying hens. An ESBL phenotype was identified in the isolate from laying hens and seven isolates from turkeys, as well as an AmpC phenotype in two of the seven isolates from turkeys. For information on ESBL‐carrying S. Infantis, please see the specific text box within the discussion. Where third‐generation cephalosporin resistance was reported, 32/34 isolates from broilers and all seven isolates from turkeys, as well as the single isolate from laying hens, displayed resistance to ciprofloxacin.
While high‐level resistance to ciprofloxacin (MIC ≥ 4 mg/L) was mostly observed among S. Kentucky isolates from poultry, 19.8% (50/252) of isolates displaying resistance by this definition were attributed to S. Infantis. Particular MDR patterns are associated with S. Infantis and because this serovar was prevalent in many countries, these patterns greatly influenced the overall resistance figures. Moreover, resistance to third‐generation cephalosporins, as well as high‐level resistance to ciprofloxacin, further underline the significance of this multiresistant serovar.
In 2021, the serovar S. Infantis represented only 3.6% of Salmonella isolated from pigs. Seven isolates from pigs showed seven different MDR patterns. Three out of the seven isolates from pigs showed resistance to quinolones. Only one MDR isolate from a pig was resistant to tigecycline. Resistance to third‐generation cephalosporins was detected in 1/7 MDR isolates from pigs. Only one S. Infantis isolate from a calf was MDR with the pattern CIP‐ NAL‐SMX‐TET‐ TGC, showing quinolone and tigecycline resistance.
In human isolates, 38.1% (N = 336) of the serovar S. Infantis were MDR (Table 20), with the predominant MDR patterns being CIP‐NAL‐SXT‐TET (found in eight isolates) and CIP‐NAL‐TET‐SMX (found in six isolates). The human isolates showed resistance to nalidixic acid (33.3%, N = 438), ciprofloxacin (33.9%, N = 528), sulfamethoxazole (40.5%, N = 36), co‐trimoxazole (30.3%, N = 188) and tetracycline (34.1%, N = 499) (Annex A, Table 5). Combined microbiological resistance to ciprofloxacin and cefotaxime was reported in 5.0% while clinical resistance to these two antimicrobials was 4.8% (N = 525) (Table 12).
MDR and ESBL‐producing S. Infantis.
In 2020, the proportion of all Salmonella isolates showing MDR in broilers and their derived carcases was greatly influenced by the occurrence of multiresistant S. Infantis, which accounted for 73% and 79.4% of the MDR Salmonella isolates from these origins, respectively. Additionally, this serovar accounted for 22% and 5% of the MDR isolates in turkeys and their derived carcases, respectively. In human cases from 2020 and 2021, 45.3% and 38.1% of S. Infantis were MDR, with four and five countries reporting S. Infantis with an ESBL phenotype, respectively, and most frequently reported by Italy. All ESBL‐carrying S. Infantis in 2021 except one were also ciprofloxacin‐resistant.
Over the last decade, multiresistant S. Infantis has increasingly been reported from food‐producing animals and humans in Italy. Subsequently, an S. Infantis clone harbouring a pESI‐like megaplasmid and carrying the ESBL gene bla CTX‐M‐1 (mediating cefotaxime resistance), as well as the resistance genes tet(A), sul1, dfrA1 and dfrA14 (conferring resistance to tetracycline, sulfamethoxazole and trimethoprim, respectively), was identified from food‐producing animals and humans in Italy (Franco et al., 2015). This MDR clone was mainly detected among the Italian broiler chicken industry, where it is thought to have disseminated through the food chain to humans (Franco et al., 2015). A proportion of the Italian isolates of MDR S. Infantis also possessed the streptomycin resistance gene aadA1.
The pESI megaplasmid (pESI = ‘plasmid for emerging S. Infantis;’ Tate et al., 2017) was first reported among S. Infantis isolates from Israel; and while these isolates were susceptible to extended‐spectrum cephalosporins, this megaplasmid also conferred resistance to tetracycline, sulfamethoxazole and trimethoprim (Aviv et al., 2014). Additionally, a S. Infantis clone harbouring the pESI‐like megaplasmid, but carrying the ESBL gene bla CTX‐M‐65, has been reported in the United States (Tate et al., 2017), as well as Switzerland (Hindermann et al., 2017). In the US, this genotype has been associated with travel to South America (Tate et al., 2017; Brown et al., 2018). In 2019, three countries (Denmark, Germany and Spain) together reported 11 domestically acquired cases of S. Infantis with bla CTX‐M‐65 (the majority of cases in Germany), and in 2020, two countries (Spain and the Netherlands) reported one case each. The majority of the bla CTX‐M‐65 isolates were resistant to ciprofloxacin, nalidixic acid, chloramphenicol, gentamicin, sulfamethoxazole, tetracycline and trimethoprim, in addition of being ESBL‐producing. In 2021, only Germany reported S. Infantis with bla CTX‐M‐65 (5 isolates).
In contrast, S. Enteritidis isolates exhibited much lower multiresistance. This serovar was the most frequently reported in laying hens and the second most commonly reported in broilers and broiler carcases, accounting for 25.5%, 10.6% and 10.7% of Salmonella spp. recovered from these poultry origins, respectively (see Figures C.1 and C.3). While complete susceptibility was observed at 46.9% in S. Enteritidis isolates from broiler carcases; in isolates recovered from broilers and laying hens, the majority of isolates exhibited complete susceptibility (53.1% and 92%, respectively). Notably, a greater number of countries reported S. Enteritidis data from broilers and laying hens in comparison to those reporting data from broiler carcases, which may reflect the overall reported levels of complete susceptibility. S. Enteritidis belongs to group D Salmonella (serogroup O9) which tend to show elevated colistin MICs, a phenomenon considered to reflect slightly decreased intrinsic susceptibility of wild‐type isolates belonging to Group D (Agersø et al., 2012). This is exemplified by the proportion of colistin‐resistant isolates attributed to S. Enteritidis (from laying hens, broilers and broiler carcases) in comparison to other serovars belonging to different serogroups. In 2021, S. Enteritidis were recovered in 6.3% of Salmonella isolates originating from calves (see Figure C.3). No S. Enteritidis was reported in pigs in 2021. In human isolates, only 1.9% (N = 1,722) of the serovar S. Enteritidis were MDR (Annex A, Table 17), with the predominant MDR patterns being AMP‐CIP‐TET (found in four isolates). However, the highest proportions of resistance in these isolates were reported to nalidixic acid (24.8%, N = 1,793), ciprofloxacin (22.6%, N = 3,103) and colistin (17.6%, N = 574) (Annex A, Table 2).
S. Kentucky was the second most commonly reported serovar in laying hens and the tenth in turkeys, as well as the eighth most frequently reported in broilers, accounting for 8.9%, 3.5% and 2.8% of Salmonella spp. recovered from these poultry origins, respectively (see Figure C.3). MDR was observed at an extremely high level in S. Kentucky isolates from turkeys (79.3%) while the proportion of isolates with MDR recovered from broilers was high (30.5%) but low for and laying hens (4% MDR). MDR was also frequent among S. Kentucky isolates recovered from carcases of turkeys and broilers (60% and 61.9%, respectively), although the total number of isolates available for analysis from these carcase origins was relatively low (N = 15 and N = 21, respectively).
A wide range of different MDR patterns were reported among S. Kentucky isolates from broilers, laying hens and turkeys. Among all poultry origins (including carcases of broilers and turkeys), the most frequent core pattern of resistance was AMP‐CIP‐NAL‐GEN‐SXT‐TET. Where MDR was detected, this resistance pattern accounted for 64.9%, 75.6%, 80% and 83.3% of the multiresistant S. Kentucky isolates recovered from broilers, turkeys, broiler carcases and turkey carcases, respectively. In 2021, eight isolates of S. Kentucky were recovered from pigs (0.6%). One isolate of them showed the resistance pattern TGC‐NAL‐CIP‐SMX‐TMP‐TET demonstrating resistance to tigecycline and to quinolones. No S. Kentucky was reported in calves in 2021.
In human isolates, 54.8% (N = 62) of the serovar S. Kentucky were MDR (Annex A, Table 21), with the predominant MDR pattern being AMP‐CIP‐NAL‐GEN‐SXT‐TET (found in 5 isolates). The human isolates showed most resistant to gentamicin (27.9%, N = 104), ampicillin (62.9%, N = 105), nalidixic acid (79.7%, N = 74), ciprofloxacin (78.1%, N = 105), sulfamethoxazole (51.6%, N = 62) and tetracycline (58.1%, N = 86) (Annex A, Table 6). Microbiological resistance to CIP and CTX was reported in 5.7%, while clinical resistance to CIP and CTX was reported in 4.8% (N = 105) of the isolates (Annex A, Table 13).
Considering isolates exhibiting high‐level resistance to ciprofloxacin (MIC ≥ 4 mg/L), S. Kentucky accounted for most of the Salmonella isolates recovered from poultry in 2020 and from humans in 2021 which exhibited resistance by this definition (180/252 and 56/76, respectively). Additionally, a single S. Kentucky isolate recovered from a pig carcase displayed high‐level resistance to ciprofloxacin. Resistance to third‐generation cephalosporins was detected in five S. Kentucky isolates recovered from broilers by Malta (4 isolates) and the Netherlands (1 isolate), as well as an isolate recovered from laying hens by Hungary. An ESBL phenotype was reported in the five isolates from broilers, while an AmpC phenotype was reported in the single isolate from laying hens. Where third‐generation cephalosporin resistance was reported in these S. Kentucky isolates, resistance to ciprofloxacin was also observed. The detection of third‐generation cephalosporin resistance and high‐level resistance to ciprofloxacin, underline the significance of this serovar.
Coipan et al. (2020) recently described the introduction and spread of a highly ciprofloxacin‐resistant S. Kentucky with the ESBL‐gene bla CTX‐M‐14b among humans in Europe. Cases were identified in eight countries in the period 2013–2018. While the clone seems to have originated in Egypt, the study pointed to a potential establishment of the clone in Malta. Germany and the Netherlands reported human cases of S. Kentucky bla CTX‐M‐14b to TESSy in 2019 and the Netherlands also in 2020. Additionally, in 2019 and 2020, Malta reported three S. Kentucky isolates, one with an ESBL phenotype and two with a combined ESBL + AmpC phenotype; genotyping was not performed. In 2021, France (1), the Netherlands (2) and Sweden (1) reported human cases of ESBL S. Kentucky. Genotyping was confirmed to be bla CTX‐M‐14b in two of the isolates, bla CTX‐M not further specified in one and the fourth lacking genotype information. Medialdea Carrera et al. (2020) were able to confirm a link between Maltese isolates of ESBL‐producing S. Kentucky from poultry and at least one human case in 2019.
S. Newport isolates recovered from turkeys in 2020 displayed very high levels of MDR, where 58.8% (30/51) of isolates were multiresistant. Notably, the level of MDR among turkeys was greatly influenced by one MS, with Hungary (N = 39) reporting 30 multiresistant isolates. While a relatively low number of S. Newport isolates were available for analysis from broiler and turkey carcases (N = 26 and N = 27, respectively), a greater proportion of isolates from broiler carcases were multiresistant in comparison to those from turkey carcases (84.6% and 18.5%, respectively). The level of MDR among broiler carcases was again strongly influenced by the results of one MS, with Poland (N = 22) reporting 22 multiresistant isolates. In 2021, S. Newport isolates were recovered in a single calf. No isolates from pigs were reported as S. Newport. In 2020, out of 165 S. Newport isolates from humans, one had a presumptive AmpC phenotype. Similarly in 2021, one isolate from a human case had a presumptive AmpC phenotype.
Among MDR S. Newport isolates recovered from turkeys and their derived carcases, the most frequent pattern of resistance was AMP‐CIP‐NAL‐TET; followed by the same pattern but without nalidixic acid resistance. In broiler carcases, the combination AMP‐CIP‐NAL‐SXT‐TET predominated. This pattern was also the second most frequently reported in broilers, although the combination CHL‐CIP‐NAL‐SXT‐TET was most frequently noted.
S. Bredeney represents about 25% of Salmonella isolates recovered from turkey carcases in 2020, being the most frequently recovered serovar from this origin (see Figure C.1). In 2021, this serovar was the fourth most reported (7.6%) in calves (see Figure C.3). Multidrug resistance was extremely high in this serovar in 2020, especially among isolates recovered from turkeys (88.9%), while only 20.6% of Bredeney isolates from turkey carcases were MDR (see Figure C.2). One isolate from a calf reported by Italy showed quinolone resistance (NAL‐CIP‐SMX‐TET), while tigecycline resistance was reported by Poland in one isolate from a pig (AMP‐TGC‐SMX‐TMP‐TET). Interestingly, multidrug resistance was observed at an extremely high level among S. Bredeney isolates from turkeys in 2020 (82%); while a low level was noted among S. Bredeney isolates from turkey carcases (4.7%). Notably, among isolates reported from turkeys (N = 50), the level of MDR was greatly influenced by one MS, with Hungary (N = 31) reporting 31 multiresistant isolates. In 2020, out of 29 S. Bredeney isolates from humans, two AmpC‐producers were identified, both by Spain and carrying bla CMY‐2.
Among MDR S. Bredeney isolates recovered from turkeys, the most frequent pattern of resistance was to AMP‐CIP‐NAL‐TET‐TGC (34.1%); followed by the same pattern but with the addition of trimethoprim (24.4%). This second core pattern was also the most commonly noted among turkey carcases (40%). While a wide range of different resistance patterns were noted among S. Bredeney isolates from turkeys, tigecycline resistance among MDR isolates from this animal origin was observed at 68.3% (all MDR isolates displaying tigecycline‐resistance originated from Hungary).
Multiresistant serovars
Considering all reporting countries (including non‐MSs), the contributions of particular multiresistant serovars to overall MDR levels in Salmonella spp. from each of the animal/carcase categories are illustrated in Figure C.6. Overall, the figure shows that monophasic S. Typhimurium and S. Infantis were the lead serovars contributing with multidrug resistance among all Salmonella spp. isolated from carcass/animal origins in 2020/2021.
Appendix D – Comparison of human Salmonella data by serovar to that in food‐producing animals
In 2020/2021 the quantitative human data were interpreted using EUCAST ECOFF values (categorised into wild‐type and non‐wild type), when available, in the same way as for the animal and food data. For 2021 data, this resulted in one dilution difference (e.g. defining a higher number of samples to be of the non‐wild type) compared to Commission Implementing Decision (EU) 2020/1729 regarding ampicillin (Figure D.1). Also, for 2021 data, the clinical breakpoint for ciprofloxacin for animal data was changed from > 1 to > 0.064 mg/L with the new Implementing Decision and now aligns with the EUCAST ECOFF (> 0.064 mg/L). For tigecycline, the applied ECOFF was changed from > 1 to > 0.5 mg/L, and the clinical breakpoint changed from > 2 mg/L to NA. Where ECOFFs do not exist, EUCAST or Clinical and Laboratory Standards Institute (CLSI) CBPs were applied. Notably, for sulfamethoxazole/sulfonamides, there is no EUCAST interpretative criterion for Salmonella and therefore a threshold of > 256 mg/L was applied to both the human and animal data. For qualitative data interpreted with clinical breakpoints (S = susceptible, I = susceptible with increased exposure* and R = resistant), I+R results were combined into one category, except for tetracycline where only R was used. When aligning susceptible isolates with wild‐type isolates and I+R isolates with non‐wild‐type isolates, there is generally close concordance across categories (Figure D.1). An exception is meropenem where the EUCAST CBP is substantially higher (+4 dilutions) than the ECOFF.
Figure D.1.
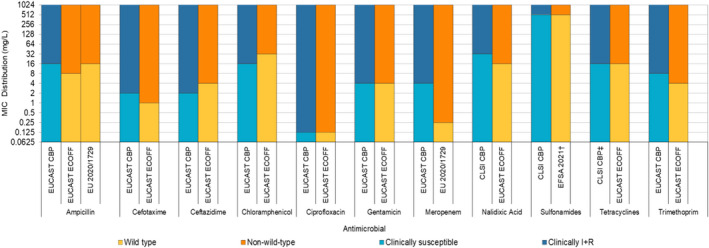
- *EUCAST has changed the definitions of SIR from 2019 (EUCAST, 2019 – http://www.eucast.org/newsiandr/). For Intermediate (I), the new definition ‘susceptible, increased exposure’ is used when there is a high likelihood of therapeutic success because exposure to the agent is increased by adjusting the dosing regimen or by its concentration at the site of infection. †EFSA Manual for reporting 2021 antimicrobial resistance data within the framework of Directive 2003/99/EC and Decision 2020/1729/EU. ‡Only R category included.
It is of note that the countries reporting data on particular Salmonella serovars from human cases are not always the same as those reporting corresponding serovar data within the animal categories. Additionally, the number of isolates reported from human cases and from the animal origins varied, both at the MS and MS‐group level. Further, Salmonella isolates have been derived from different scenarios, for human data is from clinical cases while animal data comes from healthy animals at slaughter. All of these factors mentioned above may introduce a source of variation to results when comparing overall percentage resistance to particular antimicrobials and MDR levels among human and animal isolates. The panel of nine antimicrobial classes comprising the MDR analysis of human isolates includes ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/pefloxacin/nalidixic acid, gentamicin, meropenem, sulfonamides/sulfamethoxazole, tetracyclines and trimethoprim/trimethoprim‐sulfamethoxazole (co‐trimoxazole) and does not include tigecycline. Not all MSs use the full panel when resistance testing clinical Salmonella isolates; most use a selected number of antimicrobials that reflect local or national prescribing habits and or treatment guidelines. For animal isolates, the MDR analysis included the same nine antimicrobial classes, as well as tigecycline (glycylcycline class). Tigecycline was not included in the MDR analysis of human isolates, and has been addressed together with Tetracycline from the MDR analysis of animal isolates as tigecycline has very limited effect on MDR outputs and therefore, negligible effect on human and animal comparisons.
Comparison of 2021 human data to that in poultry and their derived carcases from 2020
S. Infantis was the fourth most common serovar identified in human cases in 2021, with 1,076 cases reported in the EU/EEA. For most countries, the number of S. Infantis isolates tested were low and testing results were therefore excluded from the analysis. All countries reported AST results for ampicillin, gentamicin, chloramphenicol, cefotaxime/ceftazidime and meropenem. Resistance to ampicillin in S. Infantis from humans was, on average, 15.7%, and ranged from 0 to 65.6%. The highest levels of resistance were noted to sulfonamides (40.5%), tetracyclines (34.1%), ciprofloxacin/pefloxacin (33.9%) and co‐trimoxazole (30.3%), reported by altogether nine MSs (Austria, Belgium, France, Germany, Italy, Malta, Netherlands, Slovakia and Spain). Resistance levels varied markedly between these countries. At the reporting MS‐group level for S. Infantis from poultry in 2020, generally very high or extremely high resistance to ciprofloxacin, nalidixic acid, sulfamethoxazole and tetracycline was reported, with the exception of laying hens where much lower resistance levels to these antimicrobials were noted. Figure D.2 presents the resistance levels to these four antimicrobials considering all reporting MSs.
Figure D.2.
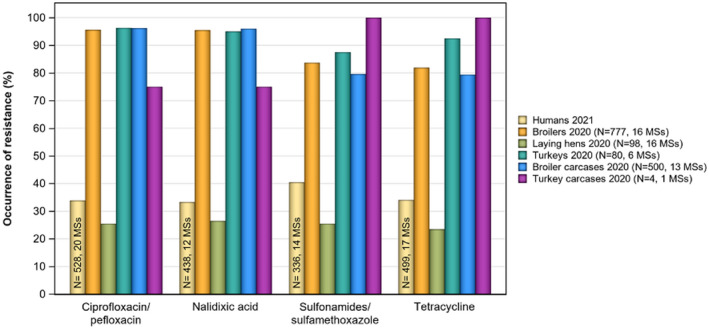
- N: Total number of isolates reported by MSs.
With the exception of laying hens, MDR among S. Infantis was reported at higher levels in isolates from poultry compared to those from humans considering all reporting countries. In human isolates, overall MDR was observed at 38.1% (14 MSs); while 79.8%, 88.8%, 84% and 75% of isolates from broiler carcases (13 MSs and 1 non‐MS), turkeys (6 MSs), broilers (16 MSs) and turkey carcases (1 MS) were MDR, respectively. At the reporting MS‐group level for S. Infantis isolates recovered from laying hens, MDR was noted at a much lower level of 24.5% (16 MSs). Notably, only four S. Infantis isolates were reported by one MS in turkey carcases and only 80 isolates were reported by six MSs in turkeys; comparative assessment of AMR data to that in humans at the country level was therefore not considered for these categories. Comparative data for nalidixic acid resistance among isolates from both broilers and humans was available for six MSs. Considering only the 4 MSs reporting a similar number of S. Infantis isolates from both broilers and humans and where more than ten isolates were reported, a higher occurrence of nalidixic acid resistance as well as ciprofloxacin/pefloxacin resistance was noted in isolates from broilers in comparison to those from humans by Austria, Belgium, Italy and Spain. Also concerning sulfamethoxazole resistance and tetracycline resistance, Austria, Belgium, Italy and Spain registered a higher occurrence of resistance in isolates from broilers compared to isolates from humans.
When applying the same considerations to AMR data for S. Infantis from both broiler carcases and humans (i.e. where a similar number and ten or more isolates were reported), apparent differences in the levels of nalidixic acid resistance were noted by Austria, Belgium and Spain; with a higher occurrence of resistance in isolates from broiler carcases compared to those from humans. This was also the case for resistance to ciprofloxacin/pefloxacin, sulfamethoxazole and tetracycline. Although comparable AMR data for S. Infantis from both laying hens and humans was available, a much lower number of isolates were reported from laying hens, with only 3 MSs (Italy, Poland and Spain) reporting data on ten or more isolates from this poultry origin. Italy and Spain reported a lower occurrence of resistance to nalidixic acid, ciprofloxacin, sulfamethoxazole and tetracyclines among isolates from laying hens in comparison to isolates from humans.
S. Enteritidis was the most common Salmonella serovar identified in human cases in 2021, with 28,453 cases reported in the EU/EEA. While MDR was uncommon among S. Enteritidis isolates (from both humans and poultry), the highest levels of resistance in S. Enteritidis from humans were noted to ciprofloxacin/pefloxacin (22.6%), nalidixic acid (24.8%) and colistin (17.6%). Colistin resistance among S. Enteritidis is not uncommon, since this serovar belongs to group D salmonellas (serogroup O9) which tend to show decreased intrinsic susceptibility to colistin (Agersø et al., 2012; Ricci et al., 2020). Figure D.3 presents the resistance levels to these antimicrobials considering all reporting MSs.
Figure D.3.
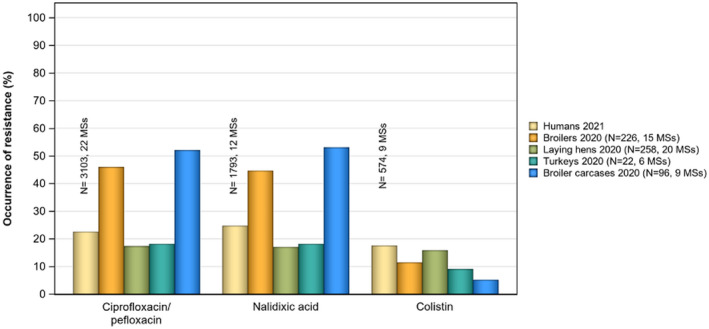
-
N: Total number of isolates reported by MSs.NB. S. Enteritidis was not reported from turkey carcases.
Only 22 S. Enteritidis isolates were reported by six MSs in turkeys; a comparative assessment of AMR data to that in humans at the country level was therefore not considered for this category. Considering data available for broiler carcases, Poland and Slovakia were the only countries to report on ten or more S. Enteritidis isolates from this poultry origin. A much higher occurrence of nalidixic acid and ciprofloxacin/pefloxacin resistance was reported among isolates from broiler carcases in Slovakia in comparison to those from humans; however, for ciprofloxacin/pefloxacin, a considerably lower number of isolates were available from broiler carcases than from humans (N = 42 and N = 527, respectively). Similarly, France, Poland and Slovakia were the only countries to report on 10 or more S. Enteritidis isolates from broilers in 2020, while also reporting data from humans in 2021. While nalidixic acid and ciprofloxacin/pefloxacin resistance was not detected among broiler isolates from France, and low resistance levels to these antimicrobials were 9.7% among human isolates, a much lower number of isolates were available from broilers in comparison to humans (N = 18 and N = 155, respectively). In Poland, extremely high occurrence of nalidixic acid and ciprofloxacin/pefloxacin resistance was reported among broiler isolates in 2020 (75.8% and 76.9%, respectively) and even higher levels in isolates collected from humans in 2021 (95.5%).
In isolates from human cases from all reporting MSs, resistance to ciprofloxacin/pefloxacin was reported at 22.6% (N = 3,143) and to nalidixic acid at 24.8% (N = 1,793); while in laying hens (N = 258), ciprofloxacin and nalidixic acid resistance were reported at levels of 17.1% and 17.1%, respectively. Considering data available in laying hens, Belgium, Cyprus, France, Hungary, Italy, Poland and Spain reported on ten or more S. Enteritidis isolates from both poultry in 2020 and humans in 2021. In four of those Member States (Belgium, Cyprus, France and Hungary), the ciprofloxacin/pefloxacin resistance among laying hen isolates, which ranged from none detected to low or moderate, was lower than that observed in isolates from humans which ranged from 6.5 to 26.4%. This was also the case for Poland, although resistance levels here were considerably higher, 31.3% from laying hens and from humans, 95.5%. In Spain, the resistance levels were similarly lower in isolates from laying hens, (16.0%), than from humans (32.2%). Conversely, in Italy (60.5%), ciprofloxacin/pefloxacin resistance in laying hen isolates was greater than that reported in human isolates (41.7% vs. 14.7%).
Considering S. Kentucky, the 21st most commonly reported serovar from human cases in 2021, with 145 cases reported in the EU/EEA, very high levels of resistance were noted to ampicillin (62.9%), ciprofloxacin/pefloxacin (78.1%), nalidixic acid (79.7%), gentamicin (27.9%), sulfonamides (51.6%) and tetracyclines (58.1%). Figure D.4 presents the resistance levels to these antimicrobials in human and poultry isolates considering all reporting MSs. Resistances to the most commonly used antimicrobials for treatment of human Salmonellosis, cefotaxime, ceftazidime and azithromycin, were notably lower (5.7%, 6.2% and 3.9%), respectively.
Figure D.4.
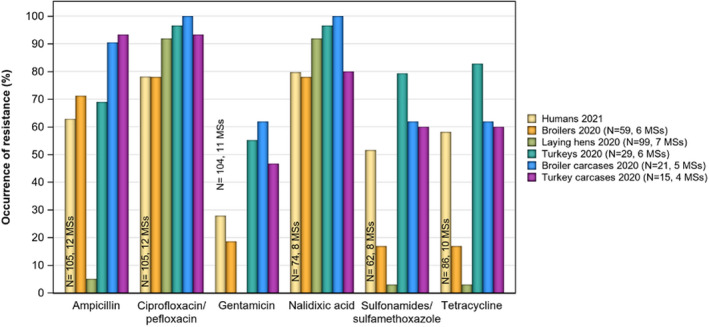
- N: Total number of isolates reported by MSs.
The number of S. Kentucky isolates recovered from broilers and turkeys and their derived carcases was relatively low (N = 59, N = 21, N = 29 and N = 15, respectively). While for laying hens, a higher number of isolates were recovered (N = 99). Overall, high and very high level of MDR was noted among isolates from broiler flocks (30.5%) and turkey flocks (79.3%), an overall low level was reported among isolates from laying hen flocks (4.0%). Because only 21 S. Kentucky isolates were reported by five MSs in broiler carcases and only 15 isolates were reported by four MSs in turkey carcases; comparative assessment of AMR data to that in humans at the country level was therefore not considered for these categories. Although comparable AMR data for S. Kentucky from both laying hens and humans were available, only Malta reported data for altogether 86 isolates from laying hens and 23 isolates from broilers in 2020 and 18 isolates from humans in 2021. Due to these low numbers of reported isolates comparison of data was not performed on MS level.
Comparison of 2021 human data to that in pigs and calves, and their derived carcases
S. Typhimurium was the second most common Salmonella serovar identified in human cases in 2021, with 5,861 cases reported in the EU/EEA. Considering all reporting MSs, the highest levels of resistance in S. Typhimurium from humans were observed for ampicillin (35.5%), sulfonamides (28.8%), tetracyclines (28.0%) and co‐trimoxazole (30.7%); as was the case for S. Typhimurium isolates from pigs (n = 163). In calves, just 10 S. Typhimurium isolates from four MSs were reported. Figure D.5 presents the resistance levels to these compounds considering all reporting MSs.
Figure D.5.
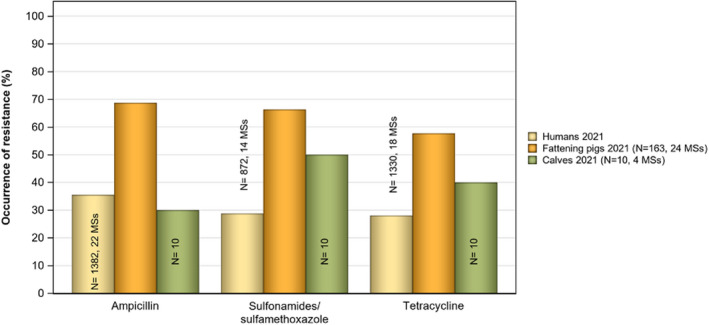
- N: Total number of isolates reported by MSs.
Considering all reporting countries, MDR levels in S. Typhimurium were reported at 23.0%, 55.8% and 50% in isolates from humans (14 MSs), pigs (24 MSs) and calves (4 MSs), respectively. While 871 isolates were included in the MDR analysis from humans, a much lower number of isolates were available from pigs (n = 163) and calves (n = 10). Assessment of human and animal S. Typhimurium AMR data at the country level was not performed, as where comparable data were available, a much lower number of isolates were reported from animals in comparison to humans by given MSs; such small sample sizes are subject to high statistical variation.
Monophasic S. Typhimurium was the third most common serovar reported from human cases in 2021, with 4,826 registered cases in the EU/EEA. Considering all reporting MSs, the highest levels of resistance in monophasic S. Typhimurium from humans were observed for ampicillin (88.2%), sulfonamides (85.2%) and tetracyclines (84.5%); as was also the case for isolates from pigs and calves. Notably, this resistance pattern (together with resistance to streptomycin) is typical of monophasic S. Typhimurium (Hopkins et al., 2010). Figure D.6 presents resistance levels to these compounds considering all reporting MSs.
Figure D.6.
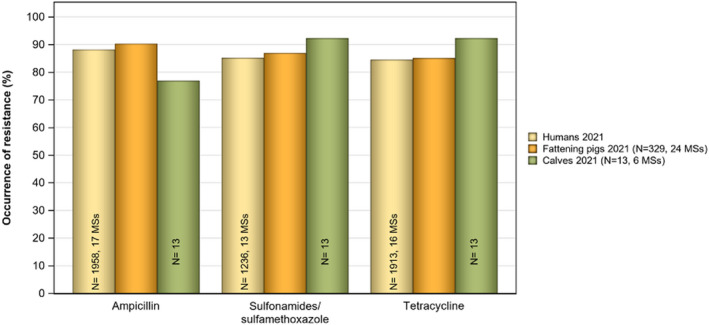
- N: Total number of isolates reported by MSs.
Considering all reporting countries, MDR levels in monophasic S. Typhimurium were reported at 78.4%, 79.6% and 76.9% in isolates from humans (13 MSs), pigs (24 MSs) and calves (6 MSs), respectively. In total, 1,235 isolates were included in the MDR analysis from humans, while a much lower number of isolates were available from pigs (n = 329) and calves (n = 13). Assessment of human and animal monophasic S. Typhimurium AMR data at the country level was not performed, as where comparable data were available, a much lower number of isolates were reported from animals.
S. Derby was the fifth most common serovar reported from human cases in 2021, with 490 cases registered by EU/EEA countries. While MDR was not as frequently observed among human/animal S. Derby isolates in comparison to S. Typhimurium and its monophasic variant, resistance to sulfonamides and tetracycline was relatively common in S. Derby isolates from human cases (32.4% and 19.3%, respectively). This was also observed among S. Derby isolates from the animal origins. Figure D.7 presents resistance levels to these compounds considering all reporting MSs. Assessment of human and animal S. Derby AMR data at the country level was not performed due to the low number of isolates reported by MSs from human cases and within the animal categories.
Figure D.7.
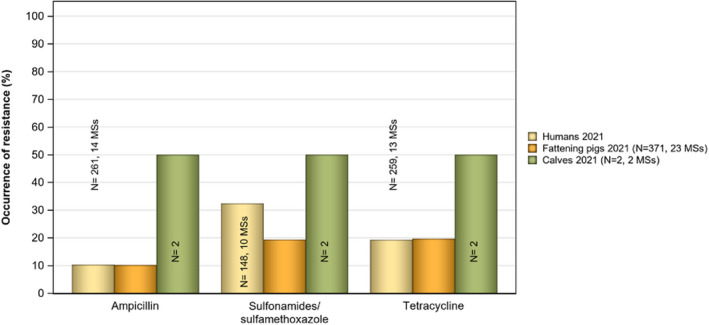
- N: Total of isolates reported by MSs.
Within a given MS, attempts to relate the occurrence of AMR in human Salmonella isolates to that in isolates from food/food‐producing animals is complicated, as much of the food consumed in a MS may have originated from other MSs or non‐member countries. Salmonella infections can also be associated with foreign travel, other types of animal contact (such as pet reptiles) or the environment. Additionally, some human infections may result from human‐to‐human transmission and, although known travel‐associated isolates from human cases were excluded from the analysis, a large proportion of cases lacked information on travel status. Such circumstances may influence the human AMR data at the reporting MS level. Furthermore, the local medical and diagnostic practices and policies for referral to clinical laboratories may vary between countries, which may result in reporting of various clinical or regional subsets of isolates from humans
Appendix E – Trends in colistin resistance in indicator E. coli from fattening pigs, calves under 1 year of age and broilers
The statistical significance (p < 0.05) of trends in colistin resistance in indicator E. coli from fattening (pigs), bovines under 1 year of age (calves), broilers and fattening turkeys was analysed by logistic regression for countries reporting data for 3 years or more in the period 2014–2020 for broilers and turkeys and 2014–2021 for pigs and calves (see Appendix F – for details on methodology). The temporal trend analyses are presented in Figures E.1, E.2, E.3–E.4 below.
Figure E.1.
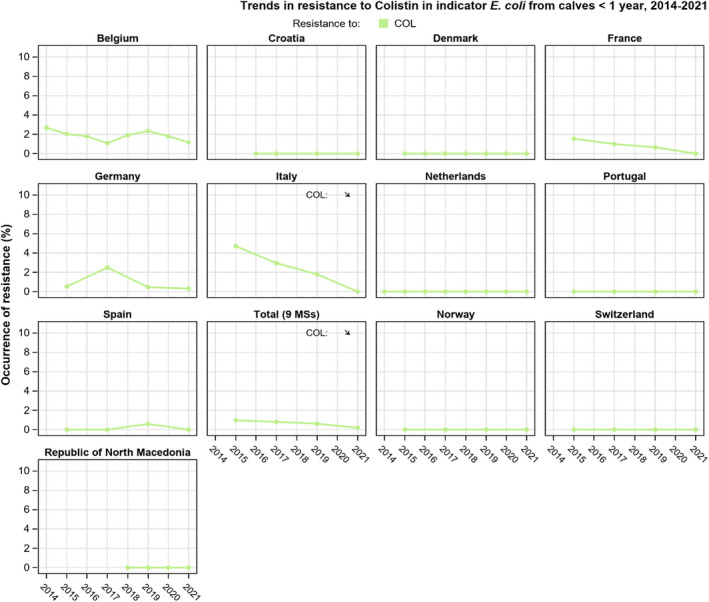
- Statistically significant increase (↑) or decrease (↓) indicated (p < 0.05).
Figure E.2.
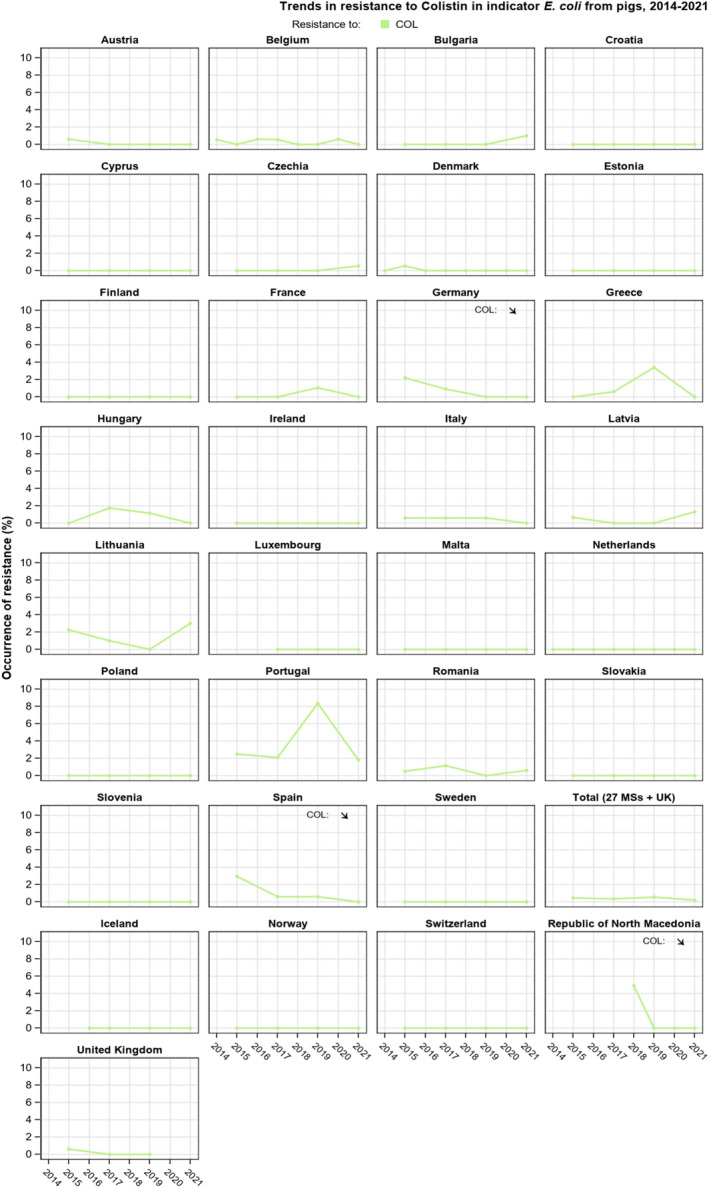
- Statistically significant increase (↑) or decrease (↓) indicated (p < 0.05).
Figure E.3.
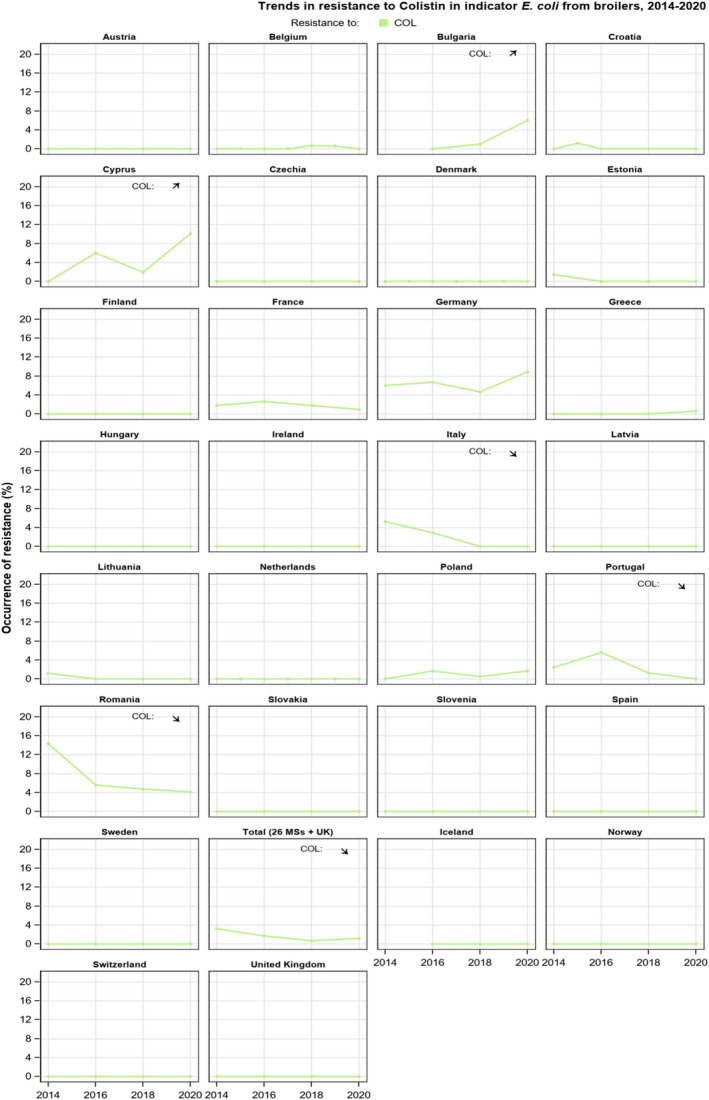
- Statistically significant increase (↑) or decrease (↓) indicated (p < 0.05).
Figure E.4.
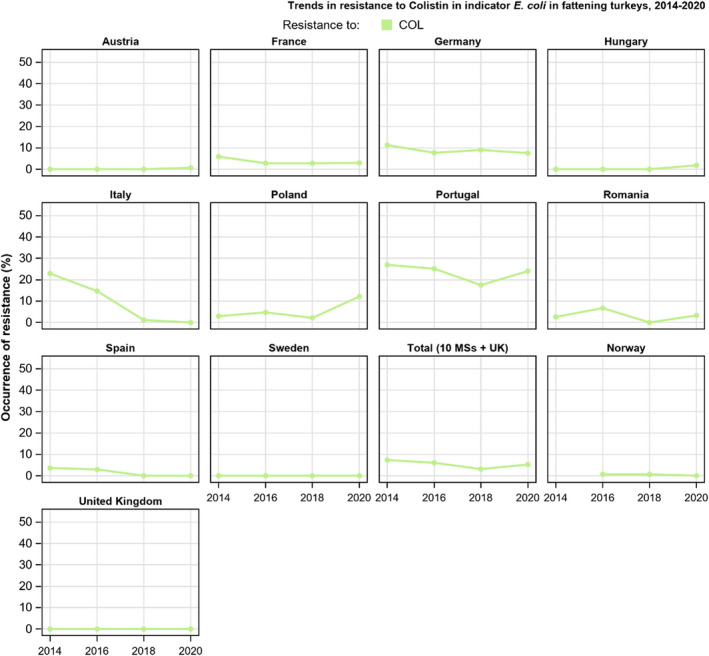
- Statistically significant increase (↑) or decrease (↓) indicated (p < 0.05).
At the MS‐group level, statistically significant decreasing trends were observed in isolates from broilers and calves and no change in trends for pigs and turkeys. In calves, decreasing trend in colistin resistance was observed in one MS (Italy) and no others reported an increase (Figure E.1). In pigs, decreasing trends were reported in two MSs (Germany and Spain) and one non‐MS (The Republic of North Macedonia), while no countries reported an increasing trend (Figure E.2). In 2020, the trends for colistin resistance in broilers decreased in three MSs (Italy, Portugal, Romania) and increased in two MSs (Bulgaria and Cyprus) (Figure E.3). In isolates from turkeys, there were no reported statistically significant increasing or decreasing trends in colistin resistance (Figure E.4).
Appendix F – Materials and methods
Antimicrobial susceptibility data from humans available in 2021
Data reported to The European Surveillance System (TESSy)
EU MSs report results from antimicrobial susceptibility testing of Salmonella spp. and Campylobacter spp. isolated from clinical cases to ECDC on an annual basis. Data can be submitted to ECDC and The European Surveillance System (TESSy) either as results interpreted with clinical breakpoints via the case‐based reporting of Salmonella and Campylobacter infections or as measured values (inhibition zone diameters or minimum inhibitory concentrations (MIC)) through the isolate‐based reporting in TESSy. From 2019 MSs can also submit data as phenotypes predicted from sequencing of the bacterial genome sequencing via the isolate‐based reporting. The reporting of quantitative data via the isolate‐based reporting is the preferred route, as stipulated in the EU protocol for harmonised monitoring of AMR in human Salmonella and Campylobacter isolates (ECDC, 2016, 2021).
| Salmonella spp.: For 2021, 24 MSs, plus Iceland and Norway provided data on antimicrobial resistance (AMR) in human Salmonella isolates. Twenty‐one countries reported measured values and four reported results interpreted as susceptible standard dosing regimen, susceptible increased exposure or resistant (SIR) according to the clinical breakpoints (CBPs) applied. One country reported results categorised as predicted wild type or predicted non‐wild type based on analysis of bacterial genomes (Table F.1). | Campylobacter spp.: For 2021, 22 MSs, plus Iceland and Norway provided AMR data from human isolates. Fifteen countries reported measured values, seven reported results interpreted as susceptible standard dosing regimen, susceptible increased exposure or resistant (SIR) according to the clinical breakpoints (CBPs) applied and two countries (Ireland and Sweden) reported result categorised as predicted wild type or predicted non‐wild type based on analysis of bacterial genomes (Table F.2). |
Table F.1.
Antimicrobials reported, methods used, type of data reported and interpretive criteria applied by MSs for human Salmonella AST data in 2021
| Country | Gentamicin | Chloramphenicol | Ampicillin | Cefotaxime | Ceftazidime | Meropenem | Tigecycline | Nalidixic acid | Ciprofloxacin/pefloxacin | Azithromycin | Colistin | Sulfonamides | Trimethoprim | Trimethoprim‐sulfa | Tetracyclines | Method used | Quantitative (Q) or categorical (SIR or PWT/PNWT) | Interpretive criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Austria | ● | ● | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | ● | DD | Q | Interpreted by ECDC. EUCAST ECOFFs for all except CLSI CBP for SUL | ||
| Belgium | ● | ● | ● | ● | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. | ||||||
| Bulgaria | ● | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria except for MEM where EUCAST CBP were used. | |||||||||
| Cyprus | ● | ● | ● | ● | ● | ● | ● | ● | DL/DLG | Q | Interpreted by ECDC, as for Austria, except for CTX, MEM and SXT where EUCAST CBP were used. | |||||||
| Denmark | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. MIC ECOFF for TGC according to EFSA reporting manual 2021. | |
| Estonia | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. | ||
| Finland | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | ||||||
| France | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. MIC ECOFF for TGC according to EFSA reporting manual 2021. | |
| Germany | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. | ||||
| Greece | ● | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | |||
| Hungary | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | DD | SIR | EUCAST CBP except CLSI CBP for NAL, SUL and TET | |||||
| Iceland | ● | ● (a) | ● | DD | Q | Interpreted by ECDC, as for Austria. | ||||||||||||
| Italy | ● | ● | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | ● | ● | DD/DL | Q | Interpreted by ECDC, as for Austria. | |
| Latvia | ● | ● | ● | ● | DD | SIR | No recent information on guidelines used. | |||||||||||
| Lithuania | ● | ● | ● | ● | ● | ● | ● | ● | ● | DL/DD | SIR | EUCAST CBP | ||||||
| Luxembourg | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | DD/DLG | Q | Interpreted by ECDC, as for Austria. | |||||
| Malta | ● | ● | ● | ● | ● | ● (a) | DL/DLG/DD | Q | Interpreted by ECDC, as for Austria, except for CTX and MEM where EUCAST CBP were used. | |||||||||
| Netherlands | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | DL | Q | Interpreted by ECDC, as for Austria. MIC ECOFF for TGC according to EFSA reporting manual 2021. | |
| Norway | ● | ● | ● | ● | ● | ● (a) | ● | DD | Q | Interpreted by ECDC, as for Austria. | ||||||||
| Poland | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | DD/DLG/DL | Q | Interpreted by ECDC, as for Austria. MIC ECOFF for TGC according to EFSA reporting manual 2021. | |
| Portugal | ● | ● | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | ||
| Romania | ● | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | |||
| Slovakia | ● | ● | ● | ● | ● | ● | ● | ● | DD/DL | SIR | EUCAST CBP except CLSI CBP for NAL, SUL and TET. | |||||||
| Slovenia | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | ● | DD/DLG | Q | Interpreted by ECDC, as for Austria. | ||||
| Spain | ● | ● | ● | ● | ● | ● | ● | ● (a) | ● | ● | ● | DD | Q | Interpreted by ECDC, as for Austria. | ||||
| Sweden | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | WGS | PWT/PNWT | Sequencing results interpreted by the laboratory with NCBI AMRFinder and CGE ResFinder and PointFinder |
AST: antimicrobial susceptibility testing; CBP: clinical breakpoint; DD: disk diffusion; DL: dilution; DLG: dilution with gradient strip; WGS: whole genome sequencing; Q: quantitative data; SIR: susceptible standard dosing regimen, susceptible increased exposure, resistant (categorical data); PWT/PNWT: predicted wild type/predicted non‐wild type (categorical); ECDC: European Centre for Disease Prevention and Control; ECOFF: epidemiological cut‐off; CLSI: Clinical and Laboratory Standards Institute; EUCAST: European Committee on Antimicrobial Susceptibility Testing; NCBI: National Center for Biotechnology Information, US; CGE: Center for Genomic Epidemiology, Denmark; MIC: minimum inhibitory concentration; AZM: azithromycin; CTX: cefotaxime; GEN: gentamicin; MEM: meropenem; NAL: nalidixic acid; SUL: sulfonamides; TET: tetracycline.
Pefloxacin used in disk diffusion.
Harmonised testing
Most laboratories follow the ‘EU protocol for harmonised monitoring of antimicrobial resistance in human Salmonella and Campylobacter isolates’ on the antimicrobial panel to be tested (ECDC, 2016, 2021). The antimicrobials tested, the method used (dilution, disk diffusion, gradient strip, WGS), the type of data provided, and the interpretive criteria applied are presented in Table F.1 for Salmonella and in Table F.2 for Campylobacter. For Salmonella, eight MSs, plus Iceland and Norway used only disk diffusion methods (DDs) for their antimicrobial susceptibility tests (AST), seven MSs used dilution methods (DLs) and another eight MSs used various combinations of DD/DL or dilution with gradient strip (DLG) methods. One country used sequencing and bioinformatics tools to predict phenotypic resistance from the genome (Table F.1). For Campylobacter, ten MSs used only disk diffusion methods (DDs) for their AST, six MSs and Norway used dilution methods (DLs or DLG), two MSs used a combination of the two. Two countries (Ireland and Sweden) used sequencing and bioinformatics tools to predict phenotypic resistance from the genome. Three MSs did not provide the methodology (Table F.2). All data on measured MIC or zone mm values were results of AST performed at the national public health reference laboratories, with the exception of Italy for Salmonella where two regional laboratories also contributed, and Finland for Campylobacter where the quantitative data had been collected from regional laboratories. Data interpreted with clinical breakpoints were normally from local or regional laboratories and reported together with the information on the clinical case. In these cases, AST had primarily been performed with the purpose of treatment of the case rather than AMR monitoring. For this reason, the number of tests per antimicrobial varied.
Salmonella test panel
The national public health laboratories within the Food‐ and Waterborne Diseases and Zoonoses (FWD) network has agreed on a panel of priority antimicrobials and optional antimicrobials to test for and report to ECDC (ECDC, 2016, 2021). Compared with earlier recommendations, a second beta‐lactam (ceftazidime) and a carbapenem (meropenem) were added. For 2021, all MS reported results on meropenem and all but four for ceftazidime. Three last‐line antimicrobials – azithromycin, colistin and tigecycline – are also included in the priority list. For colistin, however, the methodology is complicated due to chemical properties of the substance and a joint EUCAST and Clinical and Laboratory Standards Institute (CLSI) subcommittee confirmed that broth microdilution is so far the only valid method for colistin susceptibility testing (CLSI and ECDC, 2016). Disk diffusion does not work because of poor diffusion of the large colistin molecule in the agar and tested gradient strips also underestimate colistin MIC values, again most likely due to poor diffusion in the agar (Matuschek et al., 2018). Therefore, only countries performing broth microdilution (or those predicting resistance from WGS) should report on colistin resistance. Nine MSs reported AST results for azithromycin, tigecycline and colistin for 2021.
Due to the problems in detecting low‐level fluoroquinolone resistance in Salmonella spp. using disk diffusion, nalidixic acid was, for a long time, used as a marker for fluoroquinolone resistance. After the discovery that plasmid‐mediated fluoroquinolone resistance is often not detected using nalidixic acid, EUCAST studied alternative disks and concluded that pefloxacin was an excellent surrogate marker (except for isolates having the aac(6′)‐Ib‐cr gene as the only resistance determinant) (Skov and Monnet, 2016). Since 2014, EUCAST has recommend this agent for screening of low‐level fluoroquinolone resistance in Salmonella with disk diffusion (EUCAST, 2014) and, since June 2016, this is also reflected in the EU protocol. In 2021, all countries reporting measured values for disk diffusion tested with pefloxacin instead of ciprofloxacin, except for Latvia where this information is unknown. Eleven countries reported the combination drug co‐trimoxazole (trimethoprim–sulfamethoxazole) in addition to, or instead of, testing the substances separately, partly because this combination is used for clinical treatment and partly because no EUCAST interpretive criterion exists for sulfamethoxazole for Salmonella.
Campylobacter test panel
The antimicrobials included in the 2021 report followed the panel of antimicrobials from the EU protocol for harmonised monitoring of AMR in human Salmonella and Campylobacter isolates (ECDC, 2016, 2021). The priority panel for Campylobacter includes ciprofloxacin, erythromycin, tetracyclines and, since June 2016, gentamicin. Gentamicin is recommended for screening of invasive isolates and was added to the priority panel after a EUCAST ECOFF became available for disk diffusion for C. jejuni. Co‐amoxiclav (combination drug with amoxicillin and clavulanic acid) was included from the list of optional antimicrobials. In 2021, all reporting countries except Iceland tested the isolates against the three main antimicrobials ciprofloxacin, erythromycin and tetracycline (although some countries tested less than 10 isolates). In relation to C. jejuni isolates, sixteen reporting countries also tested for gentamicin and thirteen tested for co‐amoxiclav. With regards to C. coli isolates, thirteen reporting countries also tested these isolates for gentamicin and six tested for co‐amoxiclav (Annex B, Tables 1 and 2)
Analyses of antimicrobial resistance testing
Harmonised interpretation of data with animal and food data
Data reported as measured values were interpreted by ECDC based on the EUCAST ECOFF values, when available. For MIC data, the same criteria as used by EFSA were applied (Tables F.5 and F.6) except for when EUCAST had changed the ECOFF after the regulation for animal and food AMR monitoring had been implemented, e.g. as for ampicillin in 2021 for Salmonella enterica (MIC lowered with 1 dilution). Where EUCAST had removed the ECOFF (colistin, tigecycline and trimethoprim‐sulfamethoxazole for Salmonella), the same criteria were applied as recommended by EFSA (EFSA, 2021). For zone diameter data, corresponding EUCAST disk diffusion ECOFF values were applied with a few exceptions (Tables F.1 and F.2). Regarding data reported as SIR values, the categories of ‘susceptible, increased exposure’ (I) and ‘clinically’ resistant (R) were combined into one group, except for tetracycline and Salmonella. Alignment of the susceptible category with the ‘wild type’ category based on epidemiological cut‐off values (ECOFFs) and of the I+R category with the ECOFF‐based ‘non‐wild type’ category provides better comparability and more straightforward interpretation of the data for most antimicrobial agents included (Figure 27 in Section 3.5 and Figure D.1 in Appendix D of the 2020/2021 EUSR‐AMR). For Salmonella, this procedure results in good concordance (± 1 dilution) across categories with the exception of meropenem where the MIC for non‐susceptible category is substantially higher (+4 dilutions) than the ECOFF. For Campylobacter, there was full concordance across interpretive categories with this procedure, except for the EUCAST CBP for C. jejuni for tetracyclines, which is one dilution step higher than the EUCAST ECOFF.
Table F.6.
Panel of antimicrobial substances included in AMR monitoring, thresholds for interpreting resistance and concentration ranges tested in C. jejuni and C. coli based on Commission Implementing Decision (EU) 2020/1729 and EFSA Technical Report 2021
| Antimicrobial |
C. jejuni EU surveillance 2021 EUCAST ECOFF* |
C. coli EU surveillance 2021 EUCAST ECOFF* |
Concentration range, mg/L (no. of wells) |
|---|---|---|---|
| Chloramphenicol | > 16 | > 16 | 2–64 (6) |
| Ciprofloxacin | > 0.5 | > 0.5 | 0.12–32 (9) |
| Ertapenem | > 0.5 | > 0.5 | 0.125–4 (6) |
| Erythromycin | > 4 | > 8 | 1–512 (10) |
| Gentamicin (a) | > 2 | > 2 | 0.12–16 (7) |
| Tetracycline | > 1 | > 2 | 0.5–64 (8) |
AMR: antimicrobial resistance; ECOFFs: epidemiological cut‐off values; EUCAST: European Committee on Antimicrobial Susceptibility Testing.
As these values are based on Commission Implementing Decision 2020/1729, no values for STR and NAL are presented.
EUCAST epidemiological cut‐off values. ‘>’ than the ECOFF, criteria used to determine microbiological resistance.
The updated EUCAST epidemiological cut‐off (ECOFF) value for both species is at 1 mg/L.
Separation by species or serovar
As resistance levels differ substantially between Salmonella serovars, results are presented separately for selected serovars of importance in humans. The serovars presented in the report are S. Enteritidis, S. Typhimurium, monophasic S. Typhimurium, S. Infantis, S. Kentucky and S. Derby. AMR data on the 10 most common serovars in human cases in the last years are also available in the ECDC Surveillance Atlas for Infectious Diseases (https://atlas.ecdc.europa.eu/public/index.aspx). For Campylobacter, resistance levels differ quite substantially between the two most important Campylobacter species, C. jejuni and C. coli, and data are therefore presented by species. The proportion of resistant isolates is only shown when at least 10 isolates were reported from a MS.
Exclusion of travel‐associated cases
To better assess the impact from food consumed within each reporting country on the AMR levels found in human isolates, cases known to have travelled outside of the country during the incubation period were excluded from the analysis. However, as several countries had not provided any information on travel status of their cases, cases with unknown travel status were also included in addition to domestically acquired cases. The exception to this is Denmark and Finland, where it has been agreed that cases of unknown travel status have been excluded from analyses for Salmonella spp. and for Denmark also for Campylobacter spp. The proportions of travel‐associated, domestic and cases with unknown travel status among the tested isolates are presented in Tables F.3 and F.4.
Table F.3.
Proportion of tested Salmonella spp. isolates from human cases associated with travel, domestic cases and cases with unknown travel information by country, 2021
| Country | Total Salmonella tested | Travel‐ associated | Domestic | Unknown |
|---|---|---|---|---|
| N | % | % | % | |
| Austria | 1,052 | 0 | 0 | 100 |
| Belgium | 781 | 4.4 | 19 | 76.7 |
| Bulgaria | 2 | 0 | 0 | 100 |
| Cyprus | 75 | 0 | 0 | 100 |
| Denmark | 383 | 10.4 | 89.6 | 0 |
| Estonia | 136 | 4.4 | 64 | 31.6 |
| Finland | 170 | 1.8 | 98.2 | 0 |
| France | 883 | 5.7 | 14.3 | 80.1 |
| Germany | 2,996 | 0.3 | 99.7 | 0 |
| Greece | 249 | 0 | 0 | 100 |
| Hungary | 534 | 0 | 100 | 0 |
| Italy | 693 | 0 | 0 | 100 |
| Latvia | 8 | 0 | 100 | 0 |
| Lithuania | 224 | 2.2 | 97.8 | 0 |
| Luxembourg | 116 | 0 | 0 | 100 |
| Malta | 205 | 0 | 0 | 100 |
| Netherlands | 645 | 5.1 | 0 | 94.9 |
| Poland | 75 | 0 | 0 | 100 |
| Portugal | 278 | 0 | 1.8 | 98.2 |
| Romania | 25 | 0 | 0 | 100 |
| Slovakia | 780 | 0 | 100 | 0 |
| Slovenia | 185 | 4.9 | 21.1 | 74.1 |
| Spain | 1,003 | 0.1 | 75.9 | 24 |
| Sweden | 659 | 6.1 | 90.7 | 3.2 |
| Total (25 MSs) | 12,157 | 1.9 | 55.9 | 42.2 |
| Iceland | 55 | 12.7 | 54.5 | 32.7 |
| Norway | 222 | 9.9 | 65.3 | 24.8 |
MSs: Member States; N: number of isolates tested.
Table F.4.
Proportion of tested Campylobacter jejuni and Campylobacter coli isolates from human cases associated with travel, domestic cases and cases with unknown travel information by country in 2021
| Country | Total C. jejuni and C. coli tested | Travel‐ associated | Domestic | Unknown |
|---|---|---|---|---|
| N | % | % | % | |
| Austria | 473 | 1.1 | 92.6 | 6.3 |
| Bulgaria | 22 | 0 | 0 | 100 |
| Cyprus | 32 | 0 | 0 | 100 |
| Denmark | 331 | 9.7 | 90.3 | 0 |
| Estonia | 214 | 1.4 | 36.4 | 62.1 |
| Finland | 1,042 | 0 | 0 | 100 |
| France | 7,931 | 0 | 0 | 100 |
| Germany | 1,547 | 0.1 | 99.9 | 0 |
| Hungary | 586 | 0 | 100 | 0 |
| Ireland | 202 | 0 | 0 | 100 |
| Italy | 139 | 0 | 23.7 | 76.3 |
| Lithuania | 230 | 0 | 99.6 | 0.4 |
| Luxembourg | 208 | 0 | 0 | 100 |
| Malta | 244 | 0 | 0 | 100 |
| Netherlands | 1,408 | 0 | 0 | 100 |
| Poland | 78 | 0 | 79.5 | 20.5 |
| Portugal | 325 | 0 | 100 | 0 |
| Romania | 2 | 0 | 100 | 0 |
| Slovakia | 1,287 | 0.1 | 99.9 | 0 |
| Slovenia | 855 | 0.1 | 4.8 | 95.1 |
| Spain | 571 | 0 | 60.2 | 39.8 |
| Sweden | 281 | 11 | 83.6 | 5.3 |
| Total (23 MSs) | 18,008 | 0.4 | 30.6 | 69 |
| Iceland | 54 | 31.5 | 48.1 | 20.4 |
| Norway | 296 | 9.1 | 56.8 | 34.1 |
MSs: Member States; N: number of isolates tested.
Temporal trends in resistance
Temporal trends in the proportion of resistant human isolates to selected antimicrobials over the period 2013–2021 were analysed by country and for the EU MSs group. The statistical significance was assessed with logistic regression in R 4.2.1 and a p‐value of < 0.05 was considered to be significant. Only countries testing at least ten isolates per year and for at least 3 years in the 6‐year period were included. As the number of isolates reported by country was markedly lower in almost all countries in 2020 compared to previous years as an effect of the pandemic, it may have affected on the power of the statistical test. For Salmonella, the antimicrobials analysed were ciprofloxacin/pefloxacin/nalidixic acid, cefotaxime, ampicillin and tetracycline. For Campylobacter, the corresponding antimicrobials were ciprofloxacin, erythromycin and tetracycline (Annex B, Tables 1 and 2).
Within the framework of the temporal trend analyses covering data from 2013 to 2021, all EU/EEA countries reporting data during the period have been included. From 1 February 2020, the United Kingdom withdrew and became a ‘third‐ country’ in relation to the EU, with final withdrawal effective after a transition period ending on 31 December 2020. The withdrawal of the UK from the EU has an impact on the AMR data reported at the EU level as no data from 2020 onwards has been reported by the United Kingdom. In this report, data at the EU level are reported in accordance with the membership of the EU, whether before 2020 (EU including the UK) or in 2020–2021 (EU without the UK). In relation to trend analysis at country level for the 2021 report, UK data are referred to as from a non‐EU MS and the UK was excluded for the trend analysis for the EU MSs group.
Maps for critically important antimicrobials resistance
For Salmonella, the proportions of human isolates resistant to both of the critically important antimicrobials for treatment of severe Salmonella infections (WHO, 2019), fluoroquinolones (ciprofloxacin/pefloxacin) and third‐generation cephalosporins (cefotaxime), were presented in blue shaded maps to provide an overview of the geographical distribution of resistance in the EU/EEA. Combined ‘microbiological resistance’ was presented for Salmonella spp. and selected serovars (tables with combined resistance are also available in Annex A). For Campylobacter, the proportions of human isolates resistant to both critically important antimicrobials for treatment of severe Campylobacter infections (WHO, 2019), fluoroquinolones (ciprofloxacin) and macrolides (erythromycin), were presented in maps to provide an overview of the geographical distribution of this combined resistance in the EU/EEA. Combined ‘microbiological’ resistance (using EUCAST ECOFFs and EUCAST CBPs) were presented for C. jejuni and C. coli.
Analysis of multidrug resistance
Multidrug resistance (MDR) of human Salmonella spp. to nine antimicrobial classes was analysed, these classes being harmonised between ECDC and EFSA for better comparison between the two sectors. Multidrug resistance of an isolate was defined as resistance or non‐susceptibility to at least three different antimicrobial classes (Magiorakos et al., 2012). The antimicrobials included were ampicillin, cefotaxime/ceftazidime, chloramphenicol, ciprofloxacin/pefloxacin/nalidixic acid, gentamicin, meropenem, sulfonamides/sulfamethoxazole, tetracyclines and trimethoprim/trimethoprim‐sulfamethoxazole (co‐trimoxazole). Resistance to nalidixic acid, ciprofloxacin and pefloxacin were addressed together, as they belong to the same class of antimicrobials: quinolones. Isolates that were non‐wild type or I+R to any of these antimicrobials were classified as microbiologically resistant to the class of quinolones. The same method was applied to the two third‐generation cephalosporins cefotaxime and ceftazidime. Trimethoprim and co‐trimoxazole were also addressed together, as a few countries had only tested for susceptibility to the combination. This approach was considered appropriate because among the countries that provided data on both trimethoprim alone and the combination co‐trimoxazole, the proportion of resistant or non‐susceptibles corresponded closely between the two. Multidrug resistance of a C. jejuni or C. coli isolate was defined as resistance or non‐susceptibility to at least three different antimicrobial classes (Magiorakos et al., 2012). The antimicrobials in the MDR analysis were harmonised between EFSA and ECDC and included ciprofloxacin, erythromycin, gentamicin and tetracycline.
Analysis of ESBL, AmpC and carbapenemase‐production in Salmonella
All countries reported results from AST of third‐generation cephalosporins in 2021. Those which reported findings of ESBL and/or AmpC or non‐wild type results to third‐generation cephalosporins and ampicillin, were contacted by mail to provide further details on phenotypic and/or genotypic results. Of the 16 MSs and one non‐MS reporting such isolates, all except two could provide further information.
Antimicrobial susceptibility data from animals and food in 2020–2021
Data reported under Directive 2003/99/EC, Commission Implementing Decision (EU) 2013/652 and Commission Implementing Decision (EU) 2020/1729
EU MSs reported mandatory data collected following AMR monitoring programs during 2020 and 2021. ‘Directive 2003/99/EC requires Member States to ensure that monitoring provides comparable data on the occurrence of antimicrobial resistance (‘AMR’) in zoonotic agents and, in so far as they present a threat to public health, other agents’. ‘Directive 2003/99/EC also requires Member States to assess the trends and sources of AMR in their territory and to transmit a report every year covering data collected in accordance with that Directive to the Commission.’ Furthermore, some non‐EU countries reported AMR data and both, some EU and non‐EU reporting countries (RCs) also reported voluntary data from samples that were not included in the mandatory programs per reporting year.
The Commission Implementing Decision 2013/652/EU 30 lays down detailed rules for the harmonised monitoring and reporting of AMR in zoonotic and commensal bacteria applicable until 31 December 2020. The Commission Implementing Decision (EU) 2020/1729 31 of 17 November 2020 lays down new rules for antimicrobial resistance monitoring performed in 2021 onwards. This Decision specifies harmonised rules for the period 2021–2027 for the monitoring and reporting of AMR to be carried out by Member States in accordance with EU Regulations.
The Commission Implementing Decision (EU) 2020/1729 determines specific technical requirements for AMR testing and reporting in relation to sampling in food‐producing animals and derived meat (at retail and at border control posts). The Commission Implementing Decision (EU) 2020/1729 indicates that the monitoring and reporting of AMR shall cover the following bacteria: (a) Salmonella spp.; (b) Campylobacter coli (C. coli); (c) Campylobacter jejuni (C. jejuni); (d) Indicator commensal Escherichia coli (E. coli); (e) Salmonella spp. and E. coli producing the following enzymes: (i) Extended Spectrum β‐Lactamases (ESBL); (ii) AmpC β‐Lactamases (AmpC); (iii) Carbapenemases (CP). Therefore, during 2021, AMR data were collected from the bacteria listed above. It seems relevant to notice that the collection of AMR data from Campylobacter coli isolates was not compulsory in 2020. Despite this, some countries reported AMR data related to Campylobacter coli.
Countries can also report AMR data from other agents of public health importance such as methicillin‐resistant Staphylococcus aureus (MRSA). According to Commission Implementing Decision(EU) 2020/1729 the monitoring and reporting of AMR may also cover indicator commensal Enterococcus faecalis (E. faecalis) and Enterococcus faecium (E. faecium).
A scientific report published by EFSA in 2012 included technical specifications on the harmonised monitoring and reporting of antimicrobial resistance in methicillin‐resistant Staphylococcus aureus (MRSA) in food‐producing animals and food (EFSA, 2012). Detailed rules were specified for harmonised monitoring and reporting on the prevalence of resistant microorganisms in food‐producing animals and food, in particular as regards the microorganisms to be included, the origin of the isolates of the microorganisms, the number of isolates to be tested, the antimicrobial susceptibility tests to be used, the specific monitoring of MRSA and ESBL‐ or AmpC‐producing bacteria and the collection and reporting of the data. Comparison between human data and data from food‐producing animals and food sector was ensured by involvement of ECDC.
The Commission Implementing Decision (EU) 2020/1729 specifies that the monitoring and reporting of AMR shall cover the following food‐producing animal populations and food: (a) broilers; (b) laying hens; (c) fattening turkeys; (d) bovine animals under 1 year of age; (e) fattening pigs; (f) fresh meat from broilers; (g) fresh meat from turkeys; (h) fresh meat from pigs; (i) fresh meat from bovine animals. This European Commission Decision indicates the sampling frequency for MSs to carry out the AMR monitoring and reporting in accordance with the following rotational system: (a) In the years 2021, 2023, 2025 and 2027: in fattening pigs, bovine animals under 1 year of age, pig meat and bovine meat. (b) In the years 2022, 2024 and 2026: in laying hens, broilers, fattening turkeys and fresh meat derived from broilers and turkeys.
Therefore, following relevant EU legislation AMR data presented in this Report were collected from poultry populations and derived meat thereof in 2020 and from pigs and from bovines under 1 year of age in 2021.
The Commission Implementing Decision (EU) 2013/652 and the Commission Implementing Decision(EU) 2020/1729 lay down detailed rules for sampling design and sample size as well as for antimicrobial susceptibility testing for the different bacteria. These European Commission Decisions indicate the analytical methods for detection and antimicrobial susceptibility testing that shall be performed by the laboratories referred to in Article 3(2). AMR testing shall be performed by using the broth microdilution method according to the reference method ISO 20776‐1:2019.
For AMR testing, isolates were obtained through harmonised national programs. The broth microdilution testing method was widely used for susceptibility testing following EU legislation.
On November 17, 2020, the European Commission laid down the new technical specifications in Commission Implementing Decision (EU) 2020/1729 and repealed Commission Implementing Decision(EU) 2013/652. The new legislation came into effect on 1 January 2021, and updates technical specifications for harmonised AMR monitoring and reporting to include the monitoring of AMR in derived meat sampled at border control posts, the testing of new substances. The new legislation also authorises WGS as an alternate method to phenotypic testing for AMR monitoring. The new rules apply until December 2027.
Resulting quantitative 32 isolate‐based data were reported to EFSA and considered for this report. Resistance was interpreted using EUCAST ECOFF values (see text box below for further information). The antimicrobials incorporated in this report were selected based on their public health relevance and as representatives of different antimicrobial classes. Data on methicillin resistant Staphylococcus aureus (MRSA) and other microorganisms apart from those required by legislation were reported on a voluntary basis.
Harmonised representative sampling and monitoring
Representative sampling and AMR monitoring should be performed following the current legislation and the technical specifications published by EFSA (EFSA, 2012, 2014, 2019, 2020). Regulation (EC) No 2073/2005 33 Article 4 indicates that: ‘Food business operators shall perform testing as appropriate against the microbiological criteria set out in Annex I, when they are validating or verifying the correct functioning of their procedures based on HACCP principles and good hygiene practice.’
Salmonella spp.
The Commission Implementing Decision (EU) 2020/1729 lays down new rules for antimicrobial resistance monitoring performed in 2021 onwards. The Commission Implementing Decision (EU) 2020/1729 determines specific technical requirements for AMR testing and reporting in relation to sampling in food‐producing animals and derived meat (at retail and at border control posts). In 2021, MSs collected representative Salmonella spp. isolates for AMR monitoring from samples of caecal content taken at slaughter from bovines under 1 year of age where the production of meat of those bovines in the MSs was more than 10,000 tonnes per year sampled for testing and verification of compliance, in accordance with point 2.1.3 of chapter 2 of Annex I of Regulation (EC) No 2073/2005. Also in 2021, representative Salmonella isolates for AMR monitoring were obtained by MSs from samples of caecal content fattening pigs sampled for testing and verification of compliance, in accordance with point 2.1.4 of chapter 2 of Annex I of Regulation (EC) No 2073/2005. In compliance with EU legislation and EFSA guidelines, MSs sampled the caecal contents of fattening pigs and of bovines under 1 year of age at the slaughterhouse. MSs employed a two‐stage stratified sampling design (with slaughterhouses as primary sampling units and carcases as secondary units) based on proportional allocation of the number of samples to the annual throughput of the slaughterhouse. Moreover, samples of fresh meat from pigs and calves were collected at retail and at the border control posts.
In 2020, representative Salmonella isolates for monitoring AMR were collected by MSs from the populations of broilers, laying hens and fattening turkeys sampled following the Salmonella National Control Programmes (NCPs), set up in accordance with Article 5(1) of Regulation (EC) No 2160/2003. 34 Moreover, carcasses of broilers and fattening turkeys were sampled for testing and verification of compliance, in accordance with paragraph 2.1.5 of chapter 2 of Annex 1 of Regulation (EC) No 2073/2005. For the purposes of sampling design and representativeness, no more than one isolate per Salmonella serovar from the same epidemiological unit (herd/holding/flock of birds) per year should be included in the AMR monitoring program. Moreover, samples of fresh meat from broilers and fattening turkeys were collected at retail. In most MSs, the isolates tested for AMR formed a representative subsample of the total Salmonella isolates available at the National Reference Laboratory (NRL) and/or other laboratories involved. The sampling was performed in such way as to ensure geographical representativeness and even distribution over the year. However, when sampling from low prevalence areas, all the Salmonella isolates available should be tested for susceptibility.
Campylobacter spp.
The Commission Implementing Decision (EU) 2020/1729 lays down new rules for antimicrobial resistance monitoring performed in 2021 onwards. The Commission Implementing Decision (EU) 2020/1729 determines specific technical requirements for AMR testing and reporting in relation to sampling in food‐producing animals and derived meat (at retail and at border control posts).
In 2021, MSs collected at least 170 isolates of the nationally most prevalent species of Campylobacter (C. coli and C. jejuni) from samples obtained from pigs and bovines under 1 year of age following regulations and technical requirements for AMR testing. The sample collection was approximately evenly distributed over the year 2021. One representative caecal sample (single or pooled) per epidemiological unit (e.g. batch of animals sent to the slaughterhouse), was gathered to account for clustering. Isolates were recovered from caecal samples (single or pooled), in accordance with EFSA's recommendations (EFSA, 2014, 2019, 2021). Moreover, samples of meat from pigs and bovines under 1 year of age were collected at retail and at the border control posts.
Regarding AMR testing of C. coli and C. jejuni isolated from different animal species (depending on the year), the Commission Implementing Decision (EU) 2020/1729 specifies where the isolates shall be obtained from (referred to in point 1(b)(i) to (iv)) or, for Member States making use of the derogation referred to in the second paragraph of point 3(1)(b), all isolates obtained from these samples. MSs shall test at least 170 isolates of the nationally most prevalent species of Campylobacter (among C. coli and C. jejuni) obtained from samples referred to in point 1(b)(i) to (iii) or, for Member States making use of the derogation referred to in the second paragraph of point 3(1)(b), all isolates obtained from these samples. By way of derogation, where Member States have a national annual production of less than 100 000 tonnes of broiler meat, they may decide to test a minimum of 85 isolates instead of 170 isolates. Similarly, by way of derogation, where Member States have a national annual production of less than 100 000 tonnes of pig meat, they may decide to test a minimum of 85 isolates instead of 170 isolates.
In 2020, MSs collected C. jejuni isolates as part of their national monitoring programme of AMR according to the provisions of Commission Implementing Decision (EU) 2013/652, based on representative random sampling of broilers/fattening turkeys at the slaughterhouse. A two‐stage stratified sampling design was applied considering slaughterhouses as primary sampling units and carcasses as secondary units, with proportional allocation of the number of samples to the annual throughput of the slaughterhouse. In 2021, MSs collected C. jejuni isolates as part of their national monitoring programme of AMR according to the provisions of Commission Implementing Decision (EU) 2013/652, based on representative random sampling of fattening pigs and bovines under 1 year of age. Moreover, reporting countries can collect AMR data from other animal species than the required each year on voluntary basis.
Campylobacter coli caecal samples gathered at slaughter from fattening pigs and bovines under 1 year of age were collected in compliance with new legislation in 2021 and on voluntary basis in 2020. One representative caecal sample (single or pooled) per epidemiological unit (batch of carcases deriving from the same herd), was gathered to account for clustering. Isolates were recovered from caecal contents samples (single or pooled), in accordance with EFSA's recommendations (EFSA, 2012, 2014, 2019, 2020). The sample collection was approximately evenly distributed over the year 2021.
Indicator commensal E. coli
Routine monitoring of indicator E. coli
Indicator E. coli isolates were collected by MSs as part of their national monitoring programme of AMR according to the provisions of the Commission Implementing Decision (EU) 2020/1729. In 2021, MSs collected indicator E. coli isolates based on random sampling of caecal samples gathered at slaughter from fattening pigs and calves under one year of age where the production of bovine meat in the MSs is more than 10,000 tonnes slaughtered per year as specified in Annex Part A paragraph 1(c)(iv). One representative caecal sample (single or pooled) per epidemiological unit (herds), was gathered to account for clustering. Isolates were recovered from caecal samples (single or pooled), in accordance with regulations and EFSA's recommendations (EFSA, 2012, 2014, 2019, 2020).
As per Regulations, from 2021 MSs shall test at least 170 isolates obtained from samples referred to in points 1(c)(v). By way of derogation, where MSs have a national annual production of less than 100,000 tonnes of pig meat, less than 100,000 tonnes of broiler meat or less than 100,000 tonnes of turkey meat, they may test a minimum of 85 isolates instead of 170 isolates for each specific animal population (depending on the mandatory testing every year).
In 2020, MSs collected indicator commensal E. coli isolates as part of their national monitoring programme of AMR according to the provisions of Commission Implementing Decision (EU) 2013/652, based on representative random sampling of broilers and fattening turkeys at the slaughterhouse. A two‐stage stratified sampling design was applied in the reporting countries, with slaughterhouses as primary sampling units and carcasses as secondary units, accounting for proportional allocation of the number of samples to the annual throughput of the slaughterhouse. Only one representative caecal sample (single or pooled) per epidemiological unit (batch of carcasses deriving from the same flock), was gathered to account for clustering. Isolates were recovered from caecal contents samples (single or pooled), in accordance with EFSA's recommendations (EFSA, 2014, 2019). The sample collection was approximately evenly distributed over the year 2020.
In 2021, MSs collected indicator commensal E. coli isolates as part of their national monitoring programme of AMR according to the provisions of Commission Implementing Decision (EU) 2020/1729, based on representative random sampling of fattening pigs and bovines under 1 year of age. Samples and isolates were obtained as previously indicated in accordance with EU legislation and EFSA's recommendations (EFSA, 2014, 2019, 2020). The sample collection was approximately evenly distributed over the year 2021.
Specific monitoring of E. coli ESBL/AmpC/carbapenemase producers
In 2021, MSs collected caecal samples from fattening pigs and bovines under 1 year of age at slaughter, where the production of meat of those bovines in the MSs was more than 10,000 tonnes slaughtered per year and samples of fresh pig meat and bovine meat gathered at retail and at the border control posts. In 2020, MSs obtained caecal samples from broilers and from fattening turkeys at slaughter, in those MSs where the production of turkey meat in the MS was more than 10,000 tonnes slaughtered per year. Moreover, samples of fresh meat from broilers and fattening turkeys were collected at retail and at the border control posts. Only one representative caecal sample (single or pooled) per epidemiological unit (batch of carcases deriving from the same herd/flock), was collected to account for clustering. Isolates were recovered from caecal contents samples (single or pooled), in accordance with relevant Regulations and EFSA's recommendations (EFSA, 2014, 2019, 2020). The sample collection as described above was approximately evenly distributed over the years 2020 and 2021. The same sampling design was used to collect indicator E. coli isolates, whether dedicated to the routine monitoring of AMR or the specific monitoring of ESBL‐/AmpC‐/carbapenemase‐producing E. coli. EUSR on AMR in zoonotic and indicator bacteria from humans, animals and food in 2020–2021.
Epidemiological cut‐off values (ECOFFs) and clinical breakpoints (CBPs).
Epidemiological cut‐off values (ECOFFs) and clinical breakpoints (CBPs)
A microorganism is defined as ‘clinically’ resistant when the degree of resistance shown is associated with a high likelihood of therapeutic failure. The microorganism is categorised as resistant by applying the appropriate CBP in a defined phenotypic test system, and this breakpoint may alter with legitimate changes in circumstances (for example alterations in dosing regimen, drug formulation, patient factors). A microorganism is defined as wild type for a bacterial species when no acquired or mutational resistance mechanisms are present to the antimicrobial in question. A microorganism is categorised as wild type for a given bacterial species presenting a lower MIC to the antimicrobial in question than the appropriate ECOFF in a defined phenotypic test system. This cut‐off value will not be altered by changing circumstances (such as alterations in frequency of antimicrobial administration). Wild‐type microorganisms may or may not respond clinically to antimicrobial treatment. A microorganism is defined as non‐wild type for a given bacterial species by the presence of an acquired or mutational resistance mechanism to the antimicrobial in question. A microorganism is categorised as non‐wild type for a given bacterial species by applying the appropriate ECOFF value in a defined phenotypic test system; non‐wild‐type organisms are considered to show ‘microbiological’ resistance (as opposed to ‘clinical’ resistance). CBPs and ECOFFs may be the same, although it is often the case that the ECOFF is lower than the CBP. EUCAST has defined CBPs and ECOFFs.
Clinical breakpoints (clinical resistance)
The clinician, or veterinarian, choosing an antimicrobial agent to treat humans or animals with a bacterial infection requires information that the antimicrobial selected is effective against the bacterial pathogen. Such information will be used, together with clinical details such as the site of infection, ability of the antimicrobial to reach the site of infection, formulations available and dosage regimes, when determining an appropriate therapeutic course of action. The in vitro susceptibility of the bacterial pathogen can be determined and CBPs used to ascertain whether the organism is likely to respond to treatment. CBPs will take into account the distribution of the drug in the tissues of the body following administration and assume that a clinical response will be obtained if the drug is given as recommended and there are no other adverse factors which affect the outcome. Conversely, if the CBP indicates resistance, then it is likely that treatment will be unsuccessful. Frequency of dosing is one factor that can affect the antimicrobial concentration achieved at the site of infection. Therefore, different dosing regimens can lead to the development of different CBPs, as occurs in some countries for certain antimicrobials where different therapeutic regimes are in place. Although the rationale for the selection of different CBPs may be clear, their use makes the interpretation of results from different countries in reports of this type problematic, as the results are not directly comparable between those different countries.
Epidemiological cut‐off values (microbiological resistance)
For a given bacterial species, the pattern of the MIC distribution (i.e. the frequency of occurrence of each given MIC plotted against the MIC value) can enable the separation of the wild‐type population of microorganisms from those populations that show a degree of acquired resistance. The wild‐type susceptible population is assumed to have no acquired or mutational resistance and commonly shows a normal distribution. When bacteria acquire resistance by a clearly defined and efficacious mechanism, such as the acquisition of a plasmid bearing a gene which produces an enzyme capable of destroying the antimicrobial, then the MIC commonly shows two major subpopulations, one a fully susceptible normal distribution of isolates and the other a fully resistant population which has acquired the resistance mechanism. Resistance may be achieved by a series of small steps, such as changes in the permeability of the bacterial cell wall to the antimicrobial or other mechanisms which confer a degree of resistance. In this case, there may be populations of organisms which occur lying between the fully susceptible population and more resistant populations. The ECOFF value indicates the MIC or zone diameter above which the pathogen has some detectable reduction in susceptibility. ECOFFs are derived by testing an adequate number of isolates to ensure that the wild‐type population can be confidently identified for a given antimicrobial. The clinical breakpoint, which is set to determine the therapeutic effectiveness of the antimicrobial, may fail to detect emergent resistance. Conversely, the ECOFF detects any deviation in susceptibility from the wild‐type population, although it may not be appropriate for determining the likelihood of success or failure for clinical treatment.
MRSA
MRSA Isolates may have been collected by reporting countries using different monitoring approaches, either by active surveillance and monitoring of animals and foods or, in some cases, by passive monitoring (for example based on diagnostic submission of samples from clinical cases of disease in animals, or from foods sampled as part of investigatory work).
Harmonised antimicrobial susceptibility testing
Routine monitoring antimicrobial susceptibility
MSs followed Commission Implementing Decision (EU) 2020/1729 and recommendations from EFSA regarding the use of epidemiologic cut‐off values for AMR monitoring. MSs tested antimicrobials and interpreted the results using the ECOFFs and concentration ranges shown in Tables F.5 and F.6 to determine the susceptibility of the following microorganisms: Salmonella spp., C. coli, C. jejuni and indicator commensal E. coli. Under the new legislation (Commission Implementing (EU) 2020/1729), changes were made to the ECOFFs and clinical breakpoints for several antimicrobial substances included in the harmonised panel for testing of Salmonella spp., and E. coli. The substances with changes to ECOFFs and or clinical breakpoints included tigecycline, nalidixic acid and ciprofloxacin (Table F.5). For 2021 data from pigs, calves and meat from BCPS, the occurrence of resistance to tigecycline, nalidixic acid and ciprofloxacin is determined using the new ECOFFs and clinical breakpoints, and for 2020 data from poultry, tigecycline, nalidixic acid and ciprofloxacin resistance are analysed using the ECOFFs and clinical breakpoints from the previous legislation (Decision 2013/652/EU). Also, in 2021, a new substance, amikacin, was added to the harmonised panel for both Salmonella spp. and E. coli. While for Campylobacter spp., no changes were made to ECOFFs and clinical breakpoints for the substances included in the harmonised panel. However, two new substances were added (chloramphenicol and ertapenem) and two substances were removed (nalidixic acid and streptomycin).
Presumptive ESBL‐ AmpC‐ or carbapenemase‐producing E. coli isolates identified through selective plating, as well as randomly selected isolates of Salmonella spp. and E. coli that, after testing with the first panel of antimicrobials in accordance with Commission Implementing Decision (EU) 2020/1729 were found to be resistant to cefotaxime, ceftazidime or meropenem, should be further tested with a second panel of antimicrobial substances (Table F.7) or further investigated using WGS. The second panel includes cefoxitin, cefepime and clavulanic acid in combination with cefotaxime and ceftazidime for the detection of presumptive ESBL‐ and AmpC‐ producing isolates. Moreover, the second panel contains imipenem, meropenem and ertapenem to phenotypically verify presumptive carbapenemase‐ producers.
Specific monitoring of ESBL‐/AmpC‐/carbapenemase‐producing E. coli
For the specific monitoring of ESBL‐/AmpC‐/carbapenemase‐producing E. coli, the isolation method used an initial non‐selective pre‐enrichment step, followed by inoculation on MacConkey agar containing a third‐generation cephalosporin in a selective concentration (cefotaxime 1 mg/L), in accordance with the most recent version of the detailed protocol for standardisation of the EU Reference Laboratory for Antimicrobial Resistance (EURL‐AR). 35 Following this protocol, also presumptive carbapenemase‐producing isolates can be recovered. If available, one presumptive ESBL/AmpC/carbapenemase‐producing E. coli isolate obtained from each positive caecal sample and meat sample was tested for its antimicrobial susceptibility to the first panel of antimicrobials (Table F.5). This step was performed to confirm the microbiological resistance to cefotaxime (expected as the antimicrobial is present in the isolation medium at a concentration higher than the ECOFF), as well as to identify possible resistance to cefotaxime and/or ceftazidime and/or meropenem. In a second step, the isolate should be tested using the second panel of antimicrobials (Table F.7) to infer the presumptive ESBL/AmpC/carbapenemase‐producing phenotypes according to the β‐lactams resistance phenotypes obtained (Figure F.1).
Figure F.1.
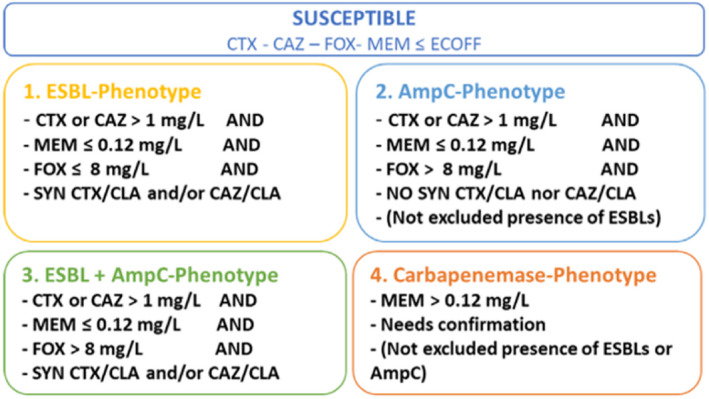
Phenotypes inferred based on the resistance to the b‐lactams included in Panel 2
Specific monitoring of carbapenemase‐producing microorganisms
This monitoring programme has been implemented and reported on a voluntary basis. For the specific monitoring of carbapenemase‐producing microorganisms, isolation required the use of non‐selective pre‐enrichment and subsequent selective plating on carbapenem‐containing media, in accordance with the most recent version of the detailed protocol of the EURL‐AR. The microbial species was identified using appropriate methods. If available, one presumptive carbapenemase‐producing isolate (primarily E. coli, but also Salmonella) obtained from each positive caecal sample and meat sample should be tested for its antimicrobial susceptibility to the first panel of antimicrobials (Table F.5) to confirm the microbiological resistance to meropenem and to identify possible resistance to other antimicrobials such as cefotaxime and/or ceftazidime. In a second step, the isolate should be tested against the second panel of antimicrobials (Table F.7) to infer the presumptive carbapenemase‐producer phenotype according to the β‐lactam resistance phenotypes obtained (Figure F.1). The EUCAST epidemiological cut‐off values applied for the antimicrobial susceptibility testing (Tables F.5, F.6–F.7) are based on Commission Implementing Decision (EU) 2020/1729. For some antimicrobials, these values have been changed compared to the previous legislation. For example, the panel of antimicrobials included in AMR monitoring for Salmonella spp. and indicator commensal E. coli indicates that for these microorganisms the EUCAST ECOFF has changed in relation to nalidixic acid from > 16 to > 8 and in relation to tigecycline from > 1 to > 0.5 based on the new legislation (Table F.5).
Data validation
Validation against business rules
The reported data were first checked for usability against a series of ‘business rules’, which were automatically applied in the EFSA data collection system once a file was sent. This automatic data validation process refers to the first validation of incoming data. Quality checks are related to a specific business only.
Scientific data validation
The scientific validation of the data collected by the MSs/non‐MSs and submitted to EFSA consisted of the reviewing the data and making comparisons between data reported for the same antimicrobials when tested by different panels. Special attention was given to carbapenems, colistin, azithromycin, tigecycline and to possible discrepancies between results for antimicrobials present in both panels (i.e. cefotaxime, ceftazidime, meropenem). MSs were contacted by EFSA asking for clarifications. If necessary, MSs were asked to confirm the MIC results and the species identification of the reported isolates.
Reference testing
To ensure the quality of data submitted, a reference testing exercise was run by the EURL‐AR in close collaboration with the MSs. The exercise consisted in retesting the AST of the isolates received using both Panel 1 and Panel 2 of antimicrobials, as well as whole genome sequencing (WGS) analyses of the isolates (WGS analyses on‐going by the time of drafting the present report). Based on the data submitted to EFSA, a selection of approximately 277 isolates was made. The selection of these isolates was based on different criteria:
Isolates representing the categorisations presumptive ESBLs‐, AmpC and ESBL + AmpC producers.
Salmonella spp. and E. coli isolates showing high resistance to Amikacin (MIC > 128 mg/L).
Isolates having genes reported at low frequency identified in their genome.
Isolates having multiple genes identified as belonging to the same family.
MSs sent the selected isolates to the EURL‐AR, where they were retested. EFSA, EURL‐AR and MSs liaised together to address possible discrepancies found.
Analyses of antimicrobial resistance data
Data are reported in separate sections dedicated to each microorganism. Clinical investigation data were not accounted for in this report.
Overview tables of the resistance data reported
Data generated from the antimicrobial susceptibility testing and reported as quantitative at the isolate level by MSs have been described in the overview tables included in the Annexes A–E published on the EFSA Knowledge Junction community on Zenodo (https://doi.org/10.5281/zenodo.7544221). The tables also display complete susceptibility, multidrug resistance and co‐resistance. These analyses are described in Section 2.4.
Minimum inhibitory concentration distributions
For each combination of microorganism, antimicrobial and food category/animal population were tested, MIC distributions were tabulated in frequency tables, giving the number of isolates tested that have a given MIC at each test dilution (mg/L) of the antimicrobial. Isolate‐based dilution results allowed MIC distributions reported:
for Salmonella for amikacin, ampicillin, azithromycin, cefepime, cefotaxime, cefotaxime and clavulanic acid, ceftazidime, ceftazidime and clavulanic acid, cefoxitin, chloramphenicol, ciprofloxacin, colistin, ertapenem, gentamicin, imipenem, meropenem, nalidixic acid, sulfamethoxazole, temocillin, tetracycline, tigecycline and trimethoprim;
for Campylobacter for chloramphenicol, ciprofloxacin, ertapenem, erythromycin, gentamicin, nalidixic acid and tetracycline;
for indicator E. coli for amikacin, ampicillin, azithromycin, cefepime, cefotaxime, cefotaxime and clavulanic acid, ceftazidime, ceftazidime and clavulanic acid, cefoxitin, chloramphenicol, ciprofloxacin, colistin, ertapenem, gentamicin, imipenem, meropenem, nalidixic acid, sulfamethoxazole, temocillin, tetracycline, tigecycline and trimethoprim;
for MRSA for cefoxitin, chloramphenicol, ciprofloxacin, clindamycin, erythromycin, fusidic acid, gentamicin, kanamycin, linezolid, mupirocin, penicillin, quinupristin/dalfopristin, rifampicin, streptomycin, sulfamethoxazole, tetracycline, tiamulin, trimethoprim and vancomycin.
Epidemiological cut‐off values and the occurrence of resistance
ECOFFs, as listed in Commission Implementing Decision (EU) 2020/1729, have been used in this report to interpret the isolate based reported MIC data and determine non‐wild‐type organisms also termed ‘microbiologically’ resistant organisms (i.e. displaying a decreased susceptibility), and to ensure that results from different MSs are comparable. From this point onwards in this report, ‘microbiologically’ antimicrobial resistant organisms are referred to as ‘resistant’ for brevity. This report also incorporates re‐evaluation of the historical data accounting for the revised EU legislation, which included the revised ECOFFs. Under the new legislation, the ECOFF used to determine microbiological resistance of Salmonella isolates to tigecycline changed from > 1 to > 0.5 mg/L. Therefore, in this report, the occurrence of resistance to tigecycline for 2021 data (i.e. pigs and calves) is determined using the new ECOFF (MIC > 0.5 mg/L), and for 2020 poultry and carcase data, tigecycline resistance is analysed using the old ECOFF (i.e. MIC > 1 mg/L). To note for tigecycline testing is the instability of the substance in aged (> 12 hours old) Mueller‐Hinton broth medium used in MIC‐testing, which may result in elevated MIC values for some isolates (Bradford et al., 2005). The reported instability of tigecycline during testing, coupled with the lower ECOFF, may result in elevated reporting of resistance to tigecycline in Salmonella and E. coli isolates with MICs within one dilution range of the ECOFF.
Starting in 2021, new legislative requirements listed in Commission Implementing Decision (EU) 2020/1729, require MSs to test target bacterial isolates for new substances. For Salmonella spp., and E. coli, the new substance to be tested is amikacin. For Campylobacter spp., the new substances are chloramphenicol and ertapenem. Nalidixic acid and streptomycin were removed from the harmonised panel for Campylobacter spp.
The occurrence of resistance to a number of antimicrobials was determined for Salmonella, Campylobacter and indicator commensal E. coli isolates and are tabulated at the production‐type level in this report. The occurrence of resistance (i.e. resistance levels) in reporting MS groups was calculated as totals (the total number of resistant isolates out of the total number of tested isolates across reporting MSs) and in the E. coli chapter, also as weighted means to account for the animal population sizes. Data description Throughout the report, level or occurrence of AMR means the percentage of resistant isolates as a proportion of the isolates tested of that microorganism. MSs reporting group means the MSs that provided data and were included in the relevant table of antimicrobial resistance for that bacterium– food or animal category–antimicrobial combination. Terms used to describe the levels or occurrence of antimicrobial resistance are ‘rare’: < 0.1%, ‘very low’: 0.1%–1.0%, ‘low’: > 1%–10.0%, ‘moderate’: > 10.0%–20.0%, ‘high’: > 20.0%–50.0%, ‘very high’: > 50.0%–70.0%, ‘extremely high’: > 70.0%. Although these terms are applied to all antimicrobials, the significance of a given level of resistance depends on the particular antimicrobial and its importance in human and veterinary medicine.
Temporal trends in resistance
Trend graphs were generated for data meeting the minimum criteria for inclusion, e.g. ten or more isolates reported and with three or more time points. Additional criteria, where applicable, are indicated in the specific chapters. Temporal trends show the resistance to different antimicrobials overtime, by plotting the level of resistance for each year of sampling and for diverse species such as humans and different food‐producing animals. Graphs were created for those countries for which resistance data were available for three or more years in the 2009–2020 period. When historical data was available the trends could cover the full period, otherwise, the time period could be different. To assess the statistical significance of temporal trends, the proportions of resistance were modelled using logistic regression. Logistic regression models used resistance as the outcome variable (with resistant (1)/non‐resistant (0)) and year as a covariate. This analysis was carried out using the PROC LOGISTIC of SAS 9.2. for each country reporting at least 10 total tested isolates, where there were 3 years or more of available data to use in the model. The PROC LOGISTIC function uses a logit transformation to model the proportions against year and provides estimates for both intercepts and slope. Models where the likelihood ratio test suggested it to be meaningful and resulting in a p‐value associated with slope of < 0.05 were significant (linear model fit). It is important to note that between‐year fluctuations in the occurrence resistance (%) may not be captured in the evaluation of the linear trend over the entire time period (2009–2021) and that very recent decreasing or increasing trends may therefore be masked by the overall trend. Also, when interpreting the results, it is important to note that trend analyses may be driven by particularly high or low levels of resistance reported in one or few data points leading to unexpected findings (e.g. detection of significant increasing or decreasing trends where the observed data do not show any clear trend over the entire period). The withdrawal of the UK from the EU has an impact on the AMR data reported at the EU level in 2020. In this report, data at the EU level are reported in accordance with the membership of the EU, whether before 2020 (EU including the UK) or after 2020 (EU without the UK).
Spatial analysis of resistance through maps
MS‐specific AMR levels for selected bacterium–food category/animal population combinations were plotted in blue shaded maps for 2020 and 2021, using ArcGIS 9.3. In the maps, resistance levels are presented with colours reflecting the continuous scale of resistance to the antimicrobial of interest among reporting MSs; so, there might be some apparent discrepancies between the colours and resistance levels between maps.
Resistance in Salmonella serovars of public health importance
In this report, AMR in tested Salmonella isolates were aggregated to give a value for Salmonella spp. for each country and food/animal category. In addition, the most prevalent Salmonella serovars were also reported separately for particular food/animal category. Additional tables have been included in this report to describe the occurrence of AMR among selected Salmonella serovars of public health importance or of high prevalence in animals. To present a complete overview of the animal populations and food categories in which specific Salmonella serovars of public health importance have been recovered, all the data reported (derived even from fewer than four reporting countries and less than 10 isolates tested) have been included.
Analysis of multidrug resistance, complete susceptibility and co‐resistance data
The analysis of MDR and co‐resistance data is important considering the emergence of multiresistant bacteria. The intention is to focus mainly on multi/co‐resistance patterns involving critically important antimicrobials (WHO, 2019), such as cephalosporins, fluoroquinolones and macrolides, and to summarise important information in the EU Summary Report. The occurrence of the isolates of a serotype/resistance pattern of interest is studied both at the MS level and at the EU level (by grouping data for all MSs and where also relevant for MSs and other reporting countries), as the overall picture for all MSs might show a more definite pattern of emergence and spread.
Analysis of MDR and complete susceptibility
For the analysis of MDR and complete susceptibility, a multiresistant isolate is one defined as resistant to at least three of the antimicrobial substances. In contrast, a completely susceptible isolate is one defined as non‐resistant (MIC < ECOFF) to these antimicrobial substances. For indicator E. coli and Salmonella spp., all substances from the harmonised test panel laid out in Commission Implementing Decision (EU) 2020/1729 will be included in the assessment of MDR, which is consistent with the approach taken in the 2019–2020 EUSR on AMR. The substances included will be amikacin/gentamicin (assessed together as aminoglycoside antimicrobial class for 2021 data), ampicillin, azithromycin (macrolide antimicrobial class), cefotaxime/ceftazidime (assessed together as third‐generation cephalosporin), chloramphenicol, ciprofloxacin/nalidixic acid (assessed together as quinolone antimicrobial class), meropenem, sulfamethoxazole, tetracycline/tigecycline (assessed together as glycylcycline antimicrobial class) and trimethoprim. For C. coli and C. jejuni, the substances included will be ciprofloxacin, erythromycin (macrolide antimicrobial class), gentamicin and tetracycline.
Key Outcome Indicators
To support EU countries in their progress to reduce use of antimicrobials and AMR a list of key outcome indicators has been jointly published by ECDC, EFSA and EMA (ECDC, EFSA, and EMA, 2017). Two of these key outcome indicators (KOI) are included in the report: (1) The key outcome indicator of complete susceptibility (KOICS) in indicator E. coli; and (2) the key outcome indicator of the prevalence of ESBL‐ and/or AmpC‐producing E. coli (KOIESC). KOICS is the proportion of fully susceptible indicator E. coli isolates, weighted by the size of the populations of the most important production animals (broilers, fattening turkeys, fattening pigs, calves) and is used as an indicator (KOICS) for the overall AMR situation in food‐producing animals. KOIESC is the weighted mean of the prevalence of ESBL‐ and/or AmpC‐producing E. coli in each of the four animal populations monitored. The KOICS and KOIESC account for differences in the relative size of food animal populations in a country and are therefore relevant in evaluation of risks related to resistance in food animals. These KOIs are displayed in bar charts showing changes in KOI over the years. The statistical significance of the trends was analysed using a simple linear regression over time. The F‐test was used to assess the overall significance of the models (p‐value < 0.05).
Combined resistance patterns of interest
The term combined resistance is used in this report to indicate phenotypic resistance to two or more different classes of antimicrobials, exhibited by the same bacterial isolate. In Salmonella and E. coli isolates, co‐resistance to cefotaxime (CTX) and ciprofloxacin (CIP) was estimated, as these two antimicrobials are of particular interest in human medicine. In 2021, co‐resistance was addressed using both ECOFFs (CTX > 0.25 mg/L and CIP > 0.064 mg/L) and CBPs (CTX > 2 mg/L and CIP > 0.064 mg/L) for E. coli. In C. jejuni and C. coli isolates, co‐resistance to ciprofloxacin and erythromycin (ERY) was estimated, as these two antimicrobials are of particular interest in human medicine in the treatment of severe campylobacteriosis. The interpretive ECOFFs used to address co‐resistance to ciprofloxacin and erythromycin were, for C. jejuni, CIP > 0.5 mg/L and ERY > 4 mg/L and, for C. coli, CIP > 0.5 mg/L and ERY > 8 mg/L. These values may be considered as very similar to CBPs.
Identification of presumptive ESBL, AmpC and/or carbapenemase producers
Definition of ESBL, AmpC, ESBL + AmpC, CP‐phenotypes
The categorisation of isolates resistant to third‐generation cephalosporins and/or carbapenems in presumptive ESBL, AmpC or carbapenemase producers was carried out based on the EUCAST guidelines for detection of resistance mechanisms and specific resistances of clinical and/or epidemiological importance (EUCAST, 2017).
For the occurrence and prevalence tables, as well as the violet shaded maps and graphics shown in Section ‘ESBL/AmpC/CP producers monitoring’, presumptive ESBL producers were considered as those exhibiting an ESBL and/or ESBL + AmpC phenotype and presumptive AmpC producers, those with an AmpC and ESBL + AmpC phenotype (see below).
For the present report, the terms:
‘Presumptive ESBL/AmpC producers’ refers to those isolates who present an ESBL and/or and AmpC and/or an ESBL + AmpC phenotype (presumptive ESBL producers and/or presumptive AmpC producers).
‘Presumptive ESBL producers’ refers to those isolates with MICs > 1 mg/L for cefotaxime and/or ceftazidime and a synergy test positive for any of these antimicrobials and susceptibility to meropenem (MEM ≤ 0.125 mg/L, see CP phenotype). These isolates may also harbour other resistance mechanisms (e.g. AmpC‐encoding genes).
‘Presumptive ESBL‐cefotaximase producers’ refers to those presumptive ESBL producers with MICs > 1 mg/L for cefotaxime and a synergy test positive for cefotaxime only. These isolates may also harbour other resistance mechanisms.
‘Presumptive ESBL‐ceftazidimase producers’ refers to those presumptive ESBL producers with MICs > 1 mg/L for ceftazidime and synergy test positive for ceftazidime only. These isolates may also harbour other resistance mechanisms. ‘Presumptive AmpC producers’ refers to isolates with MICs > 1 mg/L for cefotaxime and/or ceftazidime and cefoxitin MIC > 8 mg/L together with susceptibility to meropenem (MEM ≤ 0.125 mg/L, see CP phenotype). No distinction between acquired AmpC and natural AmpC was made. These isolates may also harbour other resistance mechanisms (e.g. ESBL‐encoding genes).
‘Presumptive ESBL + AmpC producers’ refers to isolates with the ESBL + AmpC phenotype described above. ‘Presumptive carbapenemase‐producers (CP‐producers)’ refers to those isolates with the CP phenotype described above.
Data on ESBL/AmpC/CP genes
From 2021, MSs and non‐MSs can choose to report whole genome sequencing (WGS) data for characterisation of presumptive ESBL‐, AmpC‐, CP‐producing E. coli and Salmonella spp. isolates from the routine monitoring (when further testing to the second panel of antimicrobials was performed, if resistant isolates to cefotaxime, ceftazidime and meropenem were detected in the first panel) or from the specific ESBL‐, AmpC‐, CP‐producing E. coli monitoring. Definitions for genotypic interpretation of AMR data for 2021 are listed below:
Positive isolate is an isolate where at least one ESBL‐ or AmpC‐ or CP‐ gene was detected using WGS.
Negative isolate is an isolate where no ESBL‐ or AmpC‐ or CP‐ genes are detected using WGS.
It is important to highlight that genotypic complete susceptibility is not the same as phenotypic complete susceptibility because not all genes that are detected are phenotypically expressed.
For the analysis, in relation to genotypic data the following definitions are applied:
genotypic prevalence will be defined using the following formula:
genotypic occurrence will be defined as the proportion (%) of ESBL‐ or AmpC‐ or CP‐ producing E. coli or Salmonella positive isolates (associated with at least one ESBL‐, AmpC‐ or CP‐ gene) divided by the total number of ESBL‐ or AmpC‐ or CP‐ isolates tested.
Bar charts were also used to present the WGS data.
The list of ESBL‐, AmpC‐ and CP‐ encoding genes used for the analysis of the ESBL‐, AmpC‐ and CP‐ producing isolates can be consulted in the catalogue browser https://github.com/openefsa/catalogue-browser/wiki.
Data on methicillin‐resistant Staphylococcus aureus (MRSA)
The occurrence of MRSA and its susceptibility to antimicrobials in various food categories (including meat samples from various species) and food‐producing animals was reported by few MSs. MRSA occurrence data reported from clinical investigations of food‐producing and companion animals in 2020–2021 were also reported. Details of the antimicrobials selected are provided in the section on MRSA. For further information on reported MIC distributions and the number of resistant isolates, refer to the submitted and validated MS data published on the EFSA website. The methods for collecting and testing samples for MRSA are not harmonised between MSs and, as a result, MSs may use differing procedures. Due to the variety of methods employed by MSs, these are explained in detail within the section on MRSA to enable readers to better follow the procedures carried out by individual countries.
Appendix G – Additional information and supporting data
List of Annexes
The annexes are available on the EFSA Knowledge Junction community on Zenodo at: https://doi.org/10.5281/zenodo.7544221
The annexes contain the following information:
Annex A. Data reported on antimicrobial resistance in Salmonella spp.
The annex contains tables on antimicrobial resistance data:
-
–
Antimicrobial resistance in Salmonella spp. from humans, 2020–2021;
-
–
Occurrence of resistance to selected antimicrobials in Salmonella spp. from animal carcases, 2020–2021;
-
–
Occurrence of resistance to selected antimicrobials in Salmonella spp. from animals, 2020–2021;
-
–
Occurrence of resistance (%) to selected antimicrobials in specific Salmonella serovars.
Annex B. Data reported on antimicrobial resistance in Campylobacter spp.
The annex contains tables and figures showing antimicrobial resistance data:
– Antimicrobial resistance in Campylobacter spp. from humans, 2021 and trends for 2016–2021 period;
– Data reported on antimicrobial resistance and occurrence of resistance to selected antimicrobials in C. jejuni and C. coli from food‐producing animals and derived meat, for 2020/2021 and trends of resistance in broilers (2009–2020) and in fattening turkeys (2014–2020).
Annex C. Data reported on AMR in indicator Escherichia coli from food‐producing animals and derived meat
The annex contains tables on data reported on AMR in indicator Escherichia coli from food‐producing animals and derived meat (data from poultry from 2020 and data from calves and pigs from 2021).
Annex D. Data on presumptive ESBL‐, AmpC‐ and/or carbapenemase‐producing microorganisms and their resistance occurrence (routine and specific monitorings)
The annex contains tables with the data reported on presumptive ESBL‐, AmpC‐ and/or carbapenemase‐producing microorganisms for poultry (2020), pigs and cattle (2021) and meat thereof, and their resistance occurrence (routine and specific monitorings):
– ESBL‐, AmpC‐producers prevalence and occurrence tables – pigs and cattle and meat thereof, 2021;
– ESBL‐, AmpC‐, carbapenemase‐producers prevalence and occurrence tables – poultry 2020;
– Specific carbapenemase‐producing E. coli monitoring 2020–2021;
– Occurrence of antimicrobial resistance in poultry isolates collected in 2020;
– ESBL‐, AmpC‐producers prevalence maps – pigs and cattle and meat thereof, 2021; ESBL‐, AmpC‐ producers, carbapenemase‐producers prevalence maps – poultry 2020.
Annex E. Data reported on antimicrobial resistance in MRSA from food‐producing animals and derived meat
The annex contains tables 2020 and 2021 data reported on the prevalence, genetic diversity and antimicrobial resistance of MRSA from food‐producing animals and derived meat.
Annex F. WGS data reported complementary to MIC values
The annex contains tables with WGS data additionally to the MICs reported for the routine monitoring, when further testing to the second panel of antimicrobials was performed (when resistant isolates to cefotaxime, ceftazidime and meropenem were detected in the first panel) as well as for the specific ESBL‐/AmpC‐/CP‐producing E. coli monitoring.
Supporting data
All tables produced for the European Union Summary Report on Antimicrobial Resistance in Zoonotic and Indicator Bacteria from Humans, Animals and Food in 2020/2021 are available on the EFSA Knowledge Junction community on Zenodo at: https://doi.org/10.5281/zenodo.7544221.
The aggregated dataset submitted on the negative results for extended‐spectrum ?‐lactamases (ESBL) and carbapenemase‐producers is also available on the Knowledge Juntion at: https://doi.org/10.5281/zenodo.7660134
The 2021 prevalence of MRSA aggregated dataset is also available on the Knowledge Junction at: https://doi.org/10.5281/zenodo.7636225
Country datasets
All country datasets containing the tables on the occurrence of antimicrobial resistance per each country are available on the EFSA Knowledge Junction community on Zenodo – please see below the list and corresponding link to the datasets.
The countries that submitted datasets on the 2020/2021 monitoring years are: the 27 EU Member States, the four non‐EU Member States, and Albania and Republic of North Macedonia as pre‐accession countries.
Appendix H – ESBL‐, AmpC‐ and CP‐ encoding genes identified during the specific monitoring of ESBL‐/AmpC‐/CP – producing E. coli isolates using whole genome sequencing (WGS)
In total four MSs, Italy, Germany, Czechia and Finland, provided genotypic data on ESBL‐, AmpC‐ and CP‐ producing E. coli isolates detected in the specific monitoring of ESBL‐/AmpC‐/CP‐ isolates (Tables H.1, H.2–H.3).
A variety of ESBL genes were identified in all the 4 MSs providing WGS data (Table H.1). The most frequently ESBL gene reported in the majority of animal populations and meat categories was bla CTX‐M‐1 . This gene was detected in pigs in 64 isolates from Czechia (21.2%, N = 302), 92 isolates from Italy (31%, N = 301) and 94 isolates from Germany (25%, N = 381). It was also detected in calves in 99 isolates from Italy (32.0%, N = 310) and 103 isolates from Germany (34.4%, N = 299). The detection of bla CTX‐M‐1 in meat samples was much lower being identified in 12 isolates from bovine meat (4%, N = 298) and 12 isolates of pig meat (4.1%, N = 294) in Czechia, 16 isolates (3.4%, N = 466) of pig meat and 4 bovine meat isolates (1% %, N = 418) from Germany and in 5 isolates of bovine meat (1.7%, N = 301) and 5 isolates from pig meat (1.6 %, N = 305) from Italy.
The second most frequently ESBL gene identified was bla CTXM‐15 , being detected in bovines in 133 isolates from Italy (42.9%, N = 310) and 60 isolates from Germany (20.1%, N = 299), in pigs in 36 isolates from Italy (12.0%, N = 301), 25 isolates from Germany (6.5%, N = 382), 18 isolates from Czechia (6.0%, N = 302) and two isolates from Finland (0.7%, N = 307). As well as in bovine meat: five isolates from Italy(1.7%, N = 301), two isolates from Czechia (0.7%, N = 298) and two isolates from Germany (0.5%, N = 418); and in pig meat in two isolates in each country Germany (0.4%, N = 466), Italy (0.7%, N = 305) and Czechia (0.7%, N = 294). In general ESBL‐encoding genes were more commonly detected in food‐producing animals than in their derived food products, although the number of samples tested was higher in the derived meat than in animals.
Three AmpC genes were also identified in E. coli isolates in all MSs reporting WGS data, Czechia, Germany, Italy and Finland, including bla CMY‐2, bla CMY‐113 and bla DHA‐1 (Table H.2). Among these, the bla CMY‐2 gene was the only one identified in all four countries. This included 7 isolates from calves (2.3%, N = 310), 1 isolate from bovine meat (0.33%, N = 301), 4 isolates from pig meat (1.31%, N = 305) and 24 isolates from fattening pigs (8.0%, N = 301) in Italy. This gene was also detected in 2 isolates from bovine meat (0.67%, N = 298), 2 isolates from pig meat (0.68%, N = 294), 3 isolates from bovine meat (1.0%, N = 298) and 9 isolates from fattening pigs (3.0%, N = 302) from Czechia. In Germany, two isolates from pigs (0.5% N = 382) and one isolate from bovine animals (0.2%, N = 418) presented this gene, while only 1 isolate from a fattening pig (0.33%, N = 307) in Finland was identified to carry this gene. However, most of the AmpC‐producing E. coli isolates detected presented a point mutation in the AmpC promotor.
Four CP‐encoding genes were identified in the specific CP‐producing E. coli monitoring, including bla OXA‐181, bla OXA‐48, bla NMD‐4 and bla NMD‐5, in bovines under 1 year old and fattening pigs from Italy and Czechia (Table H.3). The most frequently identified gene was bla OXA‐181 detected in 20 pig isolates (6.6%, N = 301) and 1.3% of calf isolates from Italy, followed by bla NMD‐5 detected in three pig isolates from Czechia (1.0%, N = 302) and a bovine isolate from Italy. bla OXA‐48 was identified in a pig isolate from Italy.
Several MSs also reported data on WGS additionally to the MICs reported for the routine monitoring, when further testing to the second panel of antimicrobials (if resistant isolates to cefotaxime, ceftazidime and meropenem were detected in the first panel) as well as for the specific E. coli ESBL/AmpC/CP‐producers monitoring. These data can be consulted in the Annex E.
Supporting information
Plain Language Summary
Suggested citation: EFSA (European Food Safety Authority) and ECDC (European Centre for Disease Prevention and Control) , 2023. The European Union Summary Report on Antimicrobial Resistance in zoonotic and indicator bacteria from humans, animals and food in 2020/2021. EFSA Journal 2023;21(3):7867, 232 pp. 10.2903/j.efsa.2023.7867
Requestor European Commission
Question number EFSA‐Q‐2021‐00768
Declarations of interest If you wish to access the declaration of interests of any expert contributing to an EFSA scientific assessment, please contact interestmanagement@efsa.europa.eu.
Acknowledgements EFSA and ECDC wish to thank the members of the Scientific Network for Zoonoses Monitoring Data (EFSA) and the Food‐ and Waterborne Diseases and Zoonoses Network (ECDC) who provided the data and reviewed the report and the members of the Scientific Network for Zoonoses Monitoring Data, for their endorsement of this scientific output. Also, the contribution of EFSA staff members: Raquel García‐Fierro, Pierre‐Alexandre Beloeil, Giusi Amore, Valentina Rizzi, Beatriz Guerra Roman, Anca‐Violeta Stoicescu, Alexandra Papanikolau, Kenneth Mulligan, and the contributions of ECDC staff members: Therese Westrell and Hanna Merck, and the contributions of ECDC and EFSA contractor: AUSVET Europe (Angus Cameron, Skye Badger, Hester Tang, Ana Belen García, Céline Faverjon, Angela Fanelli, Alison Hillman, Anders Dalsgaard, Ute Wolff Sönksen) SOLADIS (Florian Kroell, Frédéric Chavanel, Thomas Briére, Omraam Agbohouto, Catherine Pahon) and EFOR‐CVO‐SOLADIS Group (Patrick Etiévant). Also, the support from the EURL‐AR, specifically, Jette Sejer Kjeldgaard, Birhte S. Rosenqvist Lund, Jacob Dyring Jensen and Rene S. Hendriksen for the confirmatory testing are gratefully acknowledged.
Map disclaimer The designations employed and the presentation of material on the maps included in this report do not imply the expression of any opinion whatsoever on the part of the European Food Safety Authority and of the European Centre for Disease Prevention and Control concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries.
Copyright for non‐EFSA content: EFSA may include images or other content for which it does not hold copyright. In such cases, EFSA indicates the copyright holder and users should seek permission to reproduce the content from the original source.
EFSA may include images or other content for which it does not hold copyright. In such cases, EFSA indicates the copyright holder and users should seek permission to reproduce the content from the original source.
Approved: 31 January 2023
The Plain Language Summary is available under the Supporting Information section with the link.
Notes
Regulation (EC) No. 178/2002 of the European Parliament and of the Council of 28 January 2002 laying down the general principles and requirements of food law, establishing the EFSA and laying down procedures in matters of food safety. OJ L 31, 1.2.2002, p. 1–24.
Directive 2003/99/EC of the European Parliament and of the Council of 17 November 2003 on the monitoring of zoonoses and zoonotic agents, amending Council Decision 90/424/EEC and repealing Council Directive 92/117/EEC. OJ L325/31, 12.12.2003, p. 31–40.
Commission Implementing Decision (EU) 2020/1729 of 17 November 2020 on the monitoring and reporting of antimicrobial resistance in zoonotic and commensal bacteria and repealing Implementing Decision 2013/652/EU. OJ L 387, 19.11.2020, p. 8–21.
Commission Implementing Decision (EU) 2013/652 of 12 November 2013 on the monitoring and reporting of antimicrobial resistance in zoonotic and commensal bacteria. OJ L 303, 14.11.2013, p. 26–39.
Commission Implementing Decision (EU) 2018/945 of 22 June 2018 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions. OJ L 170, 6.7.2018, p. 1–74.
Decision No. 1082/2013/EU of the European Parliament and of the Council of 22 October 2013 on serious cross‐border threats to health and repealing Decision No. 2119/98/EC. OJ L 293, 5.11.2013, p. 1–15.
https://health.ec.europa.eu/funding/eu4health-programme-2021-2027-vision-healthier-european-union_en.
Regulation (EU) 2021/522 of the European Parliament and of the Council of 24 March 2021 establishing a Programme for the Union's action in the field of health (‘EU4Health Programme’) for the period 2021‐2027, and repealing Regulation (EU) No 282/2014. OJ L 107, 26.3.2021, p. 1‐29
Additional information on Materials and methods can be found in Appendix F. and links to supporting data for this chapter (Annex A–E) are provided in Appendix G.
The epidemiological cut‐off (ECOFF) values separate the naive, susceptible wild‐type bacterial populations from isolates that have developed reduced susceptibility to a given antimicrobial agent (Kahlmeter et al., 2003). The ECOFFs may differ from breakpoints used for clinical purposes, which are set out against a background of clinically relevant data, including therapeutic indication, clinical response data, dosing schedules, pharmacokinetics and pharmacodynamics. The use of harmonised methods and ECOFFs ensures the comparability of data over time at the country level and facilitates the comparison of resistance between MSs.
Additional information on Materials and methods can be found in Appendix F and links for supporting data for this chapter are provided in Appendix G.
In this chapter, fattening pigs are referred to as ‘pigs’; bovines under 1 year of age are referred to as ‘calves’; fattening turkeys are referred to as ‘turkeys’.
Commission Implementing Decision (EU) 2020/729 sets out the sampling frequency of bacterial isolates/ food‐producing animal/ food combinations based on a rotational system. In even years (e.g. 2020, 2022) AMR monitoring is carried out in poultry flocks (broilers, laying hens, fattening turkeys) and in meat derived from broilers and turkeys. In odd years (e.g. 2021, 2023), AMR monitoring is carried out in fattening pigs and calves under 1 year of age, and in pig meat and bovine meat. MSs can voluntarily report data from species other than those required for that year, and in 2021, a small number of MSs voluntarily reported AMR data from E. coli isolates collected from flocks of broilers and fattening turkeys (turkeys) in 2021.
‘Fresh meat’ means meat that has not undergone any preserving process other than chilling, freezing or quick freezing, including meat that is vacuum‐wrapped or wrapped in a controlled atmosphere. Regulation (EC) No 853/2004 of the European Parliament and of the Council laying down specific hygiene rules for on the hygiene of foodstuffs. OJ L 139/55, 30.4.2004.
In the following sections, the occurrence of resistance refers to microbiological resistance (i.e. determined by the ECOFF value) unless otherwise stated. The level of resistance is described as either ‘rare’: < 0.1%, ‘very low’: 0.1%–1.0%, ‘low’: > 1%–10.0%, ‘moderate’: > 10.0%–20.0%, ‘high’: > 20.0%–50.0%, ‘very high’: > 50.0%–70.0%, ‘extremely high’: > 70.0%. The significance of a given level of resistance depends on the antimicrobial substance and its relative relevance in human and veterinary medicine. The small sample size from some reporting countries should be considered when interpreting results.
Ciprofloxacin and cefotaxime are first‐line agents that are critically important for treating human infections caused by Enterobacteriaceae.
Annex C is available on the EFSA Knowledge Junction community on Zenodo at: https://doi.org/10.5281/zenodo.6257446.
Trends in colistin resistance were analysed by logistic regression for countries reporting data for three years or more in the period 2014–2021 (see Appendix E – for details).
The statistical significance (p < 0.05) of trends was tested by logistic regression (see Appendix F – for details on methodology).
PCU is a technical unit of measurement used as an indicator of animal population size and was developed by the EMA primarily to estimate sales of antimicrobials corrected by the animal population in individual countries. The data sources and methodology for the calculation of PCU are comprehensively described in EMA's report ‘Sales of veterinary antimicrobial agents in 31 European countries in 2019–2020 (EMA, 2021).
All Salmonella and indicator E. coli isolates tested with the harmonised panel of antimicrobial substances (Panel 1) and exhibiting microbiological resistance to cefotaxime, ceftazidime or meropenem were subsequently subjected to further testing using a supplementary panel of substances (Panel 2) to obtain more detailed phenotypic characterisation (see Appendix F, materials and methods).
The method is described in Appendix F and protocols are available at: https://www.eurl-ar.eu/protocols.aspx.
E. coli isolates exhibiting an ESBL‐, AmpC‐ or ESBL+AmpC‐producing phenotype.
E. coli isolates exhibiting an ESBL+AmpC‐producing phenotype.
Commission Implementing Decision (EU) 2013/652 of 12 November 2013 on the monitoring and reporting of antimicrobial resistance in zoonotic and commensal bacteria.
Commission Implementing Decision (EU) 2020/1729 of 17 November 2020 on the monitoring and reporting of antimicrobial resistance in zoonotic and commensal bacteria and repealing Commission Implementing Decision 2013/652.
‘Quantitative data’ derived from dilution methods consisted of the number of isolates having a specific MIC value (measured in mg/L) relative to the total number of isolates tested, for each antimicrobial agent and specific food/animal category.
Commission Regulation (EC) No 2073/2005 of 15 November 2005 on microbiological criteria for foodstuffs. OJ L 338, 22.12.2005, p. 1–26.
Regulation (EC) No 2160/2003 of the European Parliament and of the Council of 17 November 2003 on the control of Salmonella and other specified food‐borne zoonotic agents. OJ L 325, 12.12.2003, p. 1–15.
Available online: www.eurl-ar.eu.
Contributor Information
European Food Safety Authority (EFSA), Email: zoonoses@efsa.europa.eu.
European Centre for Disease Prevention and Control (ECDC), Email: FWD@ecdc.europa.eu.
References
- Agersø Y, Torpdahl M, Zachariasen C, Seyfarth A, Hammerum AM and Nielsen EM, 2012. Tentative colistin epidemiological cut‐off value for Salmonella spp. Foodborne Pathogens and Disease, 9(4), 367–369. 10.1089/fpd.2011.1015 [DOI] [PubMed] [Google Scholar]
- Agnoletti F, Mazzolini E, Bacchin C, Bano L, Berto G, Rigoli R, Muffato G, Coato P, Tonon E and Drigo I, 2014. First reporting of methicillin‐resistant Staphylococcus aureus (MRSA) ST398 in an industrial rabbit holding and in farm‐related people. Veterinary Microbiology, 170(1–2), 172–177. 10.1016/j.vetmic.2014.01.035 [DOI] [PubMed] [Google Scholar]
- Aires‐de‐Sousa M, 2017. Methicillin‐resistant Staphylococcus aureus among animals: current overview. Clinical Microbiology and Infection, 23(6), 373–380. 10.1016/j.cmi.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Anyanwu MU, Nwobi OC, Okpala COR and Ezeonu IM, 2022. Mobile tigecycline resistance: an emerging health catastrophe requiring urgent one health global intervention. Frontiers Microbiology, 13, 808744. 10.3389/fmicb.2022.808744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arca‐Suárez J, Rodiño‐Janeiro BK, Pérez A, Guijarro‐Sánchez P, Vázquez‐Ucha JC, Cruz F, Gómez‐Garrido J, Alioto TS, Álvarez‐Tejado M, Gut M, Gut I, Oviaño M, Beceiro A, Bou G and GEMARA‐SEIMC/REIPI Enterobacterales Study Group , 2022. Emergence of 16S rRNA methyltransferases among carbapenemase‐producing Enterobacterales in Spain studied by whole‐genome sequencing. International Journal of Antimicrobial Agents, 59(1), 106456. 10.1016/j.ijantimicag.2021.106456 [DOI] [PubMed] [Google Scholar]
- Asadollahi P, Farahani NN, Mirzaii M, Khoramrooz SS, van Belkum A, Asadollahi K, Dadashi M and Darban‐Sarokhalil D, 2018. Distribution of the most prevalent Spa types among clinical isolates of methicillin‐resistant and ‐susceptible Staphylococcus aureus around the world: a review. Frontiers in Microbiology, 9. 10.3389/fmicb.2018.00163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aviv G, Tsyba K, Steck N, Salmon‐Divon M, Cornelius A, Rahav G, Grassl GA and Gal‐Mor O, 2014. A unique megaplasmid contributes to stress tolerance and pathogenicity of an emergent Salmonella enterica serovar Infantis strain. Environmental Microbiology, 16(4), 977–994. 10.1111/1462-2920.12351 [DOI] [PubMed] [Google Scholar]
- Bai L, du P, du Y, Sun H, Zhang P, Wan Y, Lin Q, Fanning S, Cui S and Wu Y, 2019. Detection of plasmid‐mediated tigecycline‐resistant gene tet(X4) in Escherichia coli from pork, Sichuan and Shandong Provinces, China, February 2019. Eurosurveillance, 24(25), 1900340. 10.2807/1560-7917.ES.2019.24.25.1900340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangerter PD, Sidler X, Perreten V and Overesch G, 2016. Longitudinal study on the colonisation and transmission of methicillin‐resistant Staphylococcus aureus in pig farms. Veterinary Microbiology, 183, 125–134. 10.1016/j.vetmic.2015.12.007 [DOI] [PubMed] [Google Scholar]
- Béjaoui A, Gharbi M, Bitri S, Nasraoui D, Ben Aziza W, Ghedira K, Rfaik M, Marzougui L, Ghram A and Maaroufi A, 2022. Virulence profiling, multidrug resistance and molecular mechanisms of Campylobacter Strains from chicken carcasses in Tunisia. Antibiotics, 11, 830. 10.3390/antibiotics11070830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belaynehe KM, Won HG, Yoon IJ and Yoo HS, 2019. Prevalence and molecular characteristics of 16s rRNA methylase gene rmtB in amikacin resistant Escherichia coli isolated from South Korea. Korean Journal of Veterinary Research, 59, 157–160. [Google Scholar]
- Bengtsson B, Persson L, Ekström K, Unnerstad HE, Uhlhorn H and Börjesson S, 2017. High occurrence of mecC ‐MRSA in wild hedgehogs (Erinaceus europaeus) in Sweden. Veterinary Microbiology, 207, 103–107. 10.1016/j.vetmic.2017.06.004 [DOI] [PubMed] [Google Scholar]
- Bevan ER, Jones AM and Hawkey PM, 2017. Global epidemiology of CTX‐M β‐lactamases: temporal and geographical shifts in genotype. Journal of Antimicrobial Chemotherapy, 72(8), 2145–2155. 10.1093/jac/dkx146 [DOI] [PubMed] [Google Scholar]
- Bortolaia V, Ronco T, Romascu L, Nicorescu I, Milita NM, Vaduva AM, Leekitcharoenphon P, Kjeldgaard JS, Hansen IM, Svendsen CA, Mordhorst H, Guerra B, Beloeil PA, Hoffmann M and Hendriksen RS, 2021. Co‐localization of carbapenem (blaOXA‐162) and colistin (mcr‐1) resistance genes on a transferable IncHI2 plasmid in Escherichia coli of chicken origin. Journal of Antimicrobial Chemotheraphy, 76, 3063–3065. 10.1093/jac/dkab285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bortolami A, Williams NJ, McGowan C, Kelly PG, Archer DC, Corrò M, Pinchbeck G, Saunders CJ and Timofte D, 2017. Environmental surveillance identifies multiple introductions of MRSA CC398 in an Equine Veterinary Hospital in the UK, 2011–2016. Scientific Reports, 7(1), 5499. 10.1038/s41598-017-05559-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boswihi SS, Udo EE, Monecke S, Mathew B, Noronha B, Verghese T and Tappa SB, 2018. Emerging variants of methicillin‐resistant Staphylococcus aureus genotypes in Kuwait hospitals. PLoS One, 13(4), e0195933. 10.1371/journal.pone.0195933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boswihi SS, Udo EE, Mathew B, Noronha B, Verghese T and Tappa SB, 2019. Livestock‐associated methicillin‐resistant Staphylococcus aureus in patients admitted to Kuwait Hospitals in 2016‐2017. Frontiers in Microbiology, 10, 2912. 10.3389/fmicb.2019.02912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boswihi SS, Udo EE and AlFouzan W, 2020. Antibiotic resistance and typing of the methicillin‐resistant Staphylococcus aureus clones in Kuwait hospitals, 2016–2017. BMC Microbiology, 20(1), 314. 10.1186/s12866-020-02009-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford PA, Petersen PJ, Young M, Jones CH, Tischler M and O'Connell J, 2005. Tigecycline MIC testing by broth dilution requires use of fresh medium or addition of the biocatalytic oxygen‐reducing reagent oxyrase to standardize the test method. Antimicrobial Agents and Chemotherapy, 49(9), 3903–3909. 10.1128/AAC.49.9.3903-3909.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broderick D, Brennan GI, Drew RJ and O'Connell B, 2021. Epidemiological typing of methicillin resistant Staphylococcus aureus recovered from patients attending a maternity hospital in Ireland 2014–2019. Infection Prevention in Practice, 3(1), 100124. 10.1016/j.infpip.2021.100124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broens EM, Graat EA, van der Wolf P, van de Giessen A and de Jong MC, 2011. Transmission of methicillin resistant Staphylococcus aureus among pigs during transportation from farm to abattoir. The Veterinary Journal, 189(3), 302–305. 10.1016/j.tvjl.2010.08.003 [DOI] [PubMed] [Google Scholar]
- Brouwer MSM, Rapallini M, Geurts Y, Harders F, Bossers A, Mevius DJ, Wit B and Veldman KT, 2018. Enterobacter cloacae complex isolated from Shrimps from Vietnam carrying bla IMI‐1 resistant to carbapenems but not cephalosporins. Antimicrobial Agents and Chemotherapy, 62(7), e00398‐18. 10.1128/AAC.00398-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown AC, Chen JC, Watkins LKF, Campbell D, Folster JP, Tate H, Wasilenko J, van Tubbergen C and Friedman CR, 2018. CTX‐M‐65 extended‐spectrum β‐lactamase–producing Salmonella enterica serotype infantis, United States. Emerging Infectious Diseases, 24(12), 2284–2291. 10.3201/eid2412.180500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos J, Cristino L, Peixe L and Antunes P, 2016. MCR‐1 in multidrug‐resistant and copper‐tolerant clinically relevant Salmonella 1,4,[5],12:i:‐ and S. Rissen clones in Portugal, 2011 to 2015. Eurosurveillance, 21(26), 30270. 10.2807/1560-7917.ES.2016.21.26.30270 [DOI] [PubMed] [Google Scholar]
- Carfora V, Diaconu EL, Ianzano A, Di Matteo P, Amoruso R, Dell'Aira E, Sorbara L, Bottoni F, Guarneri F, Campana L, Franco A, Alba P and Battisti A, 2022. The hazard of carbapenemase (OXA‐181)‐producing Escherichia coli spreading in pig and veal calf holdings in Italy in the genomics era: risk of spill over and spill back between humans and animals. Frontiers Microbiology, 13, 1016895. 10.3389/fmicb.2022.1016895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnevali C, Morganti M, Scaltriti E, Bolzoni L, Pongolini S and Casadei G, 2016. Occurrence of mcr‐1 in colistin‐resistant Salmonella enterica isolates recovered from humans and animals in Italy, 2012 to 2015. Antimicrobial Agents and Chemotherapy, 60(12), 7532–7534. 10.1128/AAC.01803-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASFM/EUCAST , 2020. CASFM/EUCAST: French Society for Microbiology v1.2. French Society for Microbiology. Available online: https://www.sfm-microbiologie.org/wp-content/uploads/2020/10/CASFM2020_Octobre2020_V1.2.pdf [Accessed: 19 January 2023]. [Google Scholar]
- Cavaco LM, Abatih E, Aarestrup FM and Guardabassi L, 2008. Selection and persistence of CTX‐M‐producing Escherichia coli in the intestinal flora of pigs treated with amoxicillin, ceftiofur, or cefquinome. Antimicrobial Agents and Chemotherapy, 52(10), 3612–3616. 10.1128/AAC.00354-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceballos S, Lozano C, Aspiroz C, Ruiz‐Ripa L, Eguizábal P, Campaña‐Burguet A, Cercenado E, López‐Calleja AI, Castillo J, Azcona‐Gutiérrez JM, Torres L, Calvo J, Martin C, Navarro M, Zarazaga M, Torres C and The Study Group of Clinical la‐Mrsa , 2022. Beyond CC398: characterisation of other tetracycline and methicillin‐resistant Staphylococcus aureus genetic lineages circulating in spanish hospitals. Pathogens, 11(3), 307. 10.3390/pathogens11030307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chon J, 2017. Methicillin‐resistant Staphylococcus aureus (MRSA) in food‐ producing and companion animals and food products. In: Sung K (ed). Frontiers in Staphylococcus aureus . IntechOpen, Rijeka. 10.5772/66645 [DOI] [Google Scholar]
- Chong Y, Ito Y and Kamimura T, 2011. Genetic evolution and clinical impact in extended‐spectrum β‐lactamase‐producing Escherichia coli and Klebsiella pneumoniae . Infection, Genetics and Evolution, 11(7), 1499–1504. 10.1016/j.meegid.2011.06.001 [DOI] [PubMed] [Google Scholar]
- CLSI and ECDC , 2016. Recommendations for MIC determination of colistin (polymyxin E) as recommended by the joint CLSI‐EUCAST Polymyxin Breakpoints Working Group. 22 March 2016. Clinical and Laboratory Standards Institute and European Committee on Antimicrobial Susceptibility Testing. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/General_documents/Recommendations_for_MIC_determination_of_colistin_March_2016.pdf
- Coipan CE, Westrell T, van Hoek A, Alm E, Kotila S, Berbers B, de Keersmaecker SCJ, Ceyssens PJ, Borg ML, Chattaway M, McCormick J, Dallman TJ and Franz E, 2020. Genomic epidemiology of emerging ESBL‐producing Salmonella Kentucky blaCTX‐M‐14b in Europe. Emerging Microbes & Infections, 9(1), 2124–2135. 10.1080/22221751.2020.1821582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo‐Piazuelo D and Lawlor PG, 2021. Livestock‐associated methicillin‐resistant Staphylococcus aureus (LA‐MRSA) prevalence in humans in close contact with animals and measures to reduce on‐farm colonisation. Irish Veterinary Journal, 74(1), 21. 10.1186/s13620-021-00200-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crombé F, Willems G, Dispas M, Hallin M, Denis O, Suetens C, Gordts B, Struelens M and Butaye P, 2012. Prevalence and antimicrobial susceptibility of methicillin‐resistant Staphylococcus aureus among pigs in Belgium. Microbial Drug Resistance, 18(2), 125–131. 10.1089/mdr.2011.0138 [DOI] [PubMed] [Google Scholar]
- Crump JA, Sjölund‐Karlsson M, Gordon MA and Parry CM, 2015. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of invasive Salmonella infections. Clinical Microbiology Reviews, 28(4), 901–937. 10.1128/CMR.00002-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui C, Ba X and Holmes MA, 2021. Prevalence and characterization of mecC MRSA in bovine bulk tank milk in Great Britain, 2017–18. JAC‐Antimicrobial Resistance, 3(1), dlaa125. 10.1093/jacamr/dlaa125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuny C, Layer F, Köck R, Werner G and Witte W, 2013. Methicillin susceptible Staphylococcus aureus (MSSA) of clonal complex CC398, t571 from infections in humans are still rare in Germany. PLoS ONE, 8(12), e83165. 10.1371/journal.pone.0083165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuny C, Wieler LH and Witte W, 2015. Livestock‐associated MRSA: the impact on humans. Antibiotics, 4(4), 521–543. 10.3390/antibiotics4040521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva AC, Rodrigues MX and Silva NCC, 2020. Methicillin‐resistant Staphylococcus aureus in food and the prevalence in Brazil: a review. Brazilian Journal of Microbiology, 51(1), 347–356. 10.1007/s42770-019-00168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai L, Sahin O, Grover M and Zhang Q, 2020. New and alternative strategies for the prevention, control, and treatment of antibiotic‐resistant Campylobacter . Translational Research, 223, 76–88. 10.1016/j.trsl.2020.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- di Ruscio F, Bjørnholt JV, Larssen KW, Leegaard TM, Moen AE and de Blasio BF, 2018. Epidemiology and spa‐type diversity of meticillin‐resistant Staphylococcus aureus in community and healthcare settings in Norway. Journal of Hospital Infection, 100(3), 316–321. 10.1016/j.jhin.2017.12.019 [DOI] [PubMed] [Google Scholar]
- Diaconu EL, Carfora V, Alba P, Di Matteo P, Stravino F, Buccella C, Dell'Aira E, Onorati R, Sorbara L, Battisti A and Franco A, 2020. Novel IncFII plasmid harbouring blaNDM‐4 in a carbapenem‐resistant Escherichia coli of pig origin, Italy. Journal of Antimicrobial Chemotheraphy, 75, 3475–3479. 10.1093/jac/dkaa374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierikx CM, Hengeveld PD, Veldman KT, de Haan A, van der Voorde S, Dop PY, Bosch T and van Duijkeren E, 2016. Ten years later: still a high prevalence of MRSA in slaughter pigs despite a significant reduction in antimicrobial usage in pigs the Netherlands. Journal of Antimicrobial Chemotherapy, 71(9), 2414–2418. 10.1093/jac/dkw190 [DOI] [PubMed] [Google Scholar]
- Dykes GA and Moorhead SM, 2001. Survival of Campylobacter jejuni on vacuum or carbon dioxide packaged primal beef cuts stored at −1.5°C. Food Control, 12(8), 553–557. [DOI] [PubMed] [Google Scholar]
- ECDC , 2016. EU Protocol for Harmonised Monitoring of Antimicrobial Resistance in Human Salmonella and Campylobacter isolates – June 2016. European Centre for Disease Prevention and Control, Stockholm: Available online: https://www.ecdc.europa.eu/sites/default/files/documents/antimicrobial-resistance-Salmonella-Campylobacter-harmonised-monitoring.pdf [Google Scholar]
- ECDC , 2021. EU Protocol for Harmonised Monitoring of AMR in Human Salmonella and Campylobacter Isolates. Annex 1. EUCAST Clinical Breakpoints and Epidemiological Cut‐Off Values for the Priority List of Antimicrobials to be Tested for Salmonella enterica as of 31 August 2021. European Centre for Disease Prevention and Control. Available online: Stockholm. https://www.ecdc.europa.eu/sites/default/files/documents/antimicrobial-resistance-Salmonella-Campylobacter-harmonised-monitoring-Annex-Aug-2021.pdf [Google Scholar]
- ECDC, EFSA and EMA , 2017. ECDC/EFSA/EMA second joint report on the integrated analysis of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food‐producing animals, EFSA Journal 2017;15(7), e04872. 10.2903/j.efsa.2017.4872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC, EFSA and EMA , 2021. Third Joint Inter‐Agency Report on Integrated Analysis of Consumption of Antimicrobial Agents and Occurrence of Antimicrobial Resistance in Bacteria from Humans and Food‐Producing Animals in the EU/EEA, JIACRA III. 2016–2018. Parma; European Centre for Disease Prevention and Control European Food Safety Authority and European Medicines Agency, Stockholm; Amsterdam. 10.2903/j.efsa.2021.6712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA , 2008. Report from the Task Force on Zoonoses Data Collection including guidance for harmonized monitoring and reporting of antimicrobial resistance in commensal Escherichia coli and Enterococcus spp. from food animals, EFSA Journal 2008;6(4):141, 44 pp. 10.2903/j.efsa.2008.141r [DOI] [Google Scholar]
- EFSA , 2009a. Analysis of the baseline survey on the prevalence of methicillin‐resistant Staphylococcus aureus (MRSA) in holdings with breeding pigs, in the EU, 2008, EFSA Journal 2009;7(11):1376. 10.2903/j.efsa.2009.1376. [DOI] [Google Scholar]
- EFSA , 2009b. Assessment of the Public Health significance of meticillin resistant Staphylococcus aureus (MRSA) in animals and foods, EFSA Journal 2009;7(3):993, 73 pp. 10.2903/j.efsa.2009.993. [DOI] [Google Scholar]
- EFSA , 2012. Technical specifications on the harmonised monitoring and reporting of antimicrobial resistance in methicillin‐resistant Staphylococcus aureus in food‐producing animals and food, EFSA Journal 2012;10(10):2897, 56 pp. 10.2903/j.efsa.2012.2897 [DOI] [Google Scholar]
- EFSA , 2014. Technical specifications on randomised sampling for harmonised monitoring of antimicrobial resistance in zoonotic and commensal bacteria. EFSA Journal 2014;12(5):3686, 33 pp. 10.2903/j.efsa.2014.3686 [DOI] [Google Scholar]
- EFSA , 2019. Technical specifications on harmonised monitoring of antimicrobial resistance in zoonotic and indicator bacteria from food‐producing animals and food, EFSA Journal 2019;17(6):5709. 10.2903/j.efsa.2019.5709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA , 2020. Technical specifications on a randomisation of sampling for the purpose of antimicrobial resistance monitoring from food‐producing animals and food as from 2021, EFSA Journal 2020;18(12):6364, 31 pp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA , 2021. Manual for Reporting 2021 Antimicrobial Resistance Data Within the Framework of Directive 2003/99/Ec and Decision 2020/1729/Eu, EFSA Supporting Publications, 18(5). 10.2903/sp.efsa.2021.EN-6652 [DOI] [Google Scholar]
- EFSA , 2022. Technical specifications for a baseline survey on the prevalence of methicillin‐resistant Staphylococcus aureus (MRSA) in pigs, EFSA Journal 2022;20(10):7620. 10.2903/j.efsa.2022.7620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA and ECDC , 2021. The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2018/2019, EFSA Journal 2021;19(4):e06490. 10.2903/j.efsa.2021.6490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA and ECDC , 2022. The European Union Summary Report on Antimicrobial Resistance in zoonotic and indicator bacteria from humans, animals and food in 2019–2020, EFSA Journal 2022;20(3):7209, 197 pp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA BIOHAZ , 2011. Scientific Opinion on the public health risks of bacterial strains producing extended‐spectrum β‐lactamases and/or AmpC β‐lactamases in food and food‐producing animals, EFSA Journal 2011;9(8):2322. 10.2903/j.efsa.2011.2322. [DOI] [Google Scholar]
- el‐Adawy H, Ahmed M, Hotzel H, Monecke S, Schulz J, Hartung J, Ehricht R, Neubauer H and Hafez HM, 2016. Characterization of Methicillin‐Resistant Staphylococcus aureus Isolated from Healthy Turkeys and Broilers Using DNA Microarrays. Frontiers in Microbiology, 7. 10.3389/fmicb.2016.02019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhadidy M, Miller WG, Arguello H, Álvarez‐Ordóñez A, Dierick K and Botteldoorn N, 2019. Molecular epidemiology and antimicrobial resistance mechanisms of Campylobacter coli from diarrhoeal patients and broiler carcasses in Belgium. Transboundary and Emerging Diseases, 66(1), 463–475. 10.1111/tbed.13046 [DOI] [PubMed] [Google Scholar]
- Elhadidy M, Ali MM, el‐Shibiny A, Miller WG, Elkhatib WF, Botteldoorn N and Dierick K, 2020. Antimicrobial resistance patterns and molecular resistance markers of Campylobacter jejuni isolates from human diarrheal cases. PLoS One, 15(1), e0227833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMA , 2021. Surveillance of Veterinary Antimicrobial Consumption, 2021. Sales of veterinary antimicrobial agents in 31 European countries in 2019 and 2020. Trends from 2010 to 2020. EMA/58183/2021. 11th ESAVC Report. Luxembourg: European Medicines Agency. Available online: https://www.ema.europa.eu/en/documents/report/sales-veterinary-antimicrobial-agents-31-european-countries-2019-2020-trends-2010-2020-eleventh_en.pdf
- EMA and EFSA (European Medicines Agency and European Food Safety Authority) , 2017. EMA and EFSA Joint Scientific Opinion on measures to reduce the need to use antimicrobial agents in animal husbandry in the European Union, and the resulting impacts on food safety (RONAFA) EFSA Journal 2017;15(1):4666, 245 pp. 10.2903/j.efsa.2017.4666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMA/CVMP , 2018. Opinion Following an Article 35 Referral for All Veterinary Medicinal Products Containing Systemically Administered (Parenteral and Oral) 3rd and 4th Generation Cephalosporins Intended for Use in Food Producing Species. European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/veterinary/referrals/cephalosporins [Accessed: 19 January 2023]. [Google Scholar]
- EUCAST , 2014. Screening for Fluoroquinolone Resistance in Salmonella spp. with Pefloxacin 5 lg. Tentative Quality Control Criteria for Users and Disk Manufacturers. European Committee for Antimicrobial Susceptibility Testing; Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/QC/Tentative_QC_criteria_for_pefloxacin_5__g.pdf [Google Scholar]
- EUCAST , 2017. The EUCAST Guidelines for Detection of Resistance Mechanisms and Specific Resistances of Clinical and/or Epidemiological Importance. Version 2. European Committee for Antimicrobial Susceptibility Testing; Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Resistance_mechanisms/EUCAST_detection_of_resistance_mechanisms_170711.pdf [Google Scholar]
- EUCAST , 2019. New definitions of S, I and R from 2019. Available online: https://www.eucast.org/newsiandr/ Accessed 20 February 2023.
- EUCAST , 2023. EUCAST: clinical breakpoints and dosing of antibiotics. Available online: https://www.eucast.org/clinical_breakpoints/ [Accessed: 22 April 2022].
- European Commission , 2022. AMR One Health Network meeting of 25–26 January 2022 MINUTES. European Commission: Directorate General for Health and Food Safety. [Google Scholar]
- EURL (European Union Reference Laboratory for Antimicrobial Resistance) , 2018. Laboratory Protocol, Isolation ofmethicillin‐resistant Staphylococcus aureus (MRSA) from food‐producing animals and farm environment. Technical University of Denmark. [Google Scholar]
- FSA (Food Standards Agency) , 2017. Risk Assessment on Meticillin‐ResistantStaphylococcus aureus(MRSA), witha focus on Livestock‐associated MRSA in the UK Food Chain. Available online: https://www.food.gov.uk/sites/default/files/media/document/mrsa_risk_assessment_feb17_0.pdf
- Feltrin F, Alba P, Kraushaar B, Ianzano A, Argudín MA, di Matteo P, Porrero MC, Aarestrup FM, Butaye P, Franco A and Battisti A, 2016. A livestock‐associated, multidrug‐resistant, methicillin‐resistant Staphylococcus aureus clonal complex 97 lineage spreading in dairy cattle and pigs in Italy. Applied and Environmental Microbiology, 82(3), 816–821. 10.1128/AEM.02854-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fessler A, Scott C, Kadlec K, Ehricht R, Monecke S and Schwarz S, 2010. Characterization of methicillin‐resistant Staphylococcus aureus ST398 from cases of bovine mastitis. Journal of Antimicrobial Chemotherapy, 65(4), 619–625. 10.1093/jac/dkq021 [DOI] [PubMed] [Google Scholar]
- Florez‐Cuadrado D, Ugarte‐Ruiz M, Meric G, Quesada A, Porrero MC, Pascoe B, Sáez‐Llorente JL, Orozco GL, Domínguez L and Sheppard SK, 2017. Genome Comparison of Erythromycin Resistant Campylobacter from Turkeys Identifies Hosts and Pathways for Horizontal Spread of erm(B) Genes. Frontiers in Microbiology, 8, 2240. 10.3389/fmicb.2017.02240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florez‐Cuadrado D, Moreno MA, Ugarte‐Ruíz M and Domínguez L, 2018. Antimicrobial resistance in the food chain in the European Union. Advances in Food and Nutrition Research, 86, 115–136. 10.1016/bs.afnr.2018.04.004 [DOI] [PubMed] [Google Scholar]
- Fournier C, Poirel L, Despont S, Kessler J and Nordmann P, 2022. Increasing trends of association of 16S rRNA methylases and carbapenemases in enterobacterales clinical isolates from Switzerland, 2017–2020. Microorganisms, 10(3), 615. 10.3390/microorganisms10030615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco A, Leekitcharoenphon P, Feltrin F, Alba P, Cordaro G, Iurescia M, Tolli R, D'Incau M, Staffolani M, di Giannatale E, Hendriksen RS and Battisti A, 2015. Emergence of a clonal lineage of multidrug‐resistant ESBL‐producing Salmonella Infantis transmitted from broilers and broiler meat to humans in Italy between 2011 and 2014. PLoS One, 10(12), e0144802. 10.1371/journal.pone.0144802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedrich MJ, 2019. Antimicrobial resistance on the rise in zoonotic bacteria in Europe. Journal of the American Medical Association, 321(15), 1448. [DOI] [PubMed] [Google Scholar]
- Garcia S and Heredia NL, 2013. Campylobacter. In: Labbé RG and García S (eds). Guide to Foodborne Pathogens. John Wiley & Sons, Chichester. pp. 188–196. [Google Scholar]
- Garcıa AB and Percival SL, 2011. Zoonotic infections: the role of biofilms. Biofilms and Veterinary Medicine, 6, 69. [Google Scholar]
- Garcia AB, Steele WB, Reid SW and Taylor DJ, 2010a. Risk of carcase contamination with Campylobacter in sheep sent for slaughter into an abattoir in Scotland. Preventive Veterinary Medicine, 95(1–2), 99–107. [DOI] [PubMed] [Google Scholar]
- Garcia AB, Steele WB and Taylor DJ, 2010b. Prevalence and carcass contamination with Campylobacter in sheep sent for slaughter in Scotland. Journal of Food Safety, 30(1), 237–250. [DOI] [PubMed] [Google Scholar]
- García‐Álvarez L, Holden MT, Lindsay H, Webb CR, Brown DF, Curran MD, Walpole E, Brooks K, Pickard DJ, Teale C, Parkhill J, Bentley SD, Edwards GF, Girvan EK, Kearns AM, Pichon B, Hill RL, Larsen AR, Skov RL, Peacock SJ, Maskell DJ and Holmes MA, 2011. Meticillin‐resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: a descriptive study. The Lancet Infectious Diseases, 11(8), 595–603. 10.1016/S1473-3099(11)70126-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García‐Fierro R, Montero I, Bances M, González‐Hevia MÁ and Rodicio MR, 2016. Antimicrobial drug resistance and molecular typing of Salmonella enterica Serovar Rissen from different sources. Microbial Drug Resistance, 22(3), 211–217. 10.1089/mdr.2015.0161 [DOI] [PubMed] [Google Scholar]
- Garcia‐Graells C, Berbers B, Verhaegen B, Vanneste K, Marchal K, Roosens NHC, Botteldoorn N and De Keersmaecker SCJ, 2020. First detection of a plasmid located carbapenem resistant blaVIM‐1 gene in E. coli isolated from meat products at retail in Belgium in 2015. International Journal of Food and Microbiology, 324, 108624. 10.1016/j.ijfoodmicro.2020.108624 [DOI] [PubMed] [Google Scholar]
- Ghasemzadeh‐Moghaddam H, Azimian A, Bayani G, Dashti V, Nojoomi S, Shirazi N, Solati A and Belkum AV, 2022. High prevalence and expression of antiseptic resistance genes among infectious t037/ST239 methicillin‐resistant Staphylococcus aureus (MRSA) strains in North Khorasan Province, Iran. Iranian Journal of Basic Medical Sciences, 25(6), 775–780. 10.22038/IJBMS.2022.63780.14055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacinti G, Carfora V, Caprioli A, Sagrafoli D, Marri N, Giangolini G, Amoruso R, Iurescia M, Stravino F, Dottarelli S, Feltrin F, Franco A, Amatiste S and Battisti A 2017. Prevalence and characterization of methicillin‐resistant Staphylococcus aureus carrying mecA or mecC and methicillin‐susceptible Staphylococcus aureus in dairy sheep farms in central Italy. Journal of Dairy Science, 100(10), 7857–7863. 10.3168/jds.2017-12940 [DOI] [PubMed] [Google Scholar]
- Golob M, Pate M, Kušar D, Zajc U, Papić B, Ocepek M, Zdovc I and Avberšek J, 2022. Antimicrobial resistance and molecular characterization of methicillin‐resistant Staphylococcus aureus from two pig farms: longitudinal study of LA‐MRSA. Antibiotics, 11(11), 1532. 10.3390/antibiotics11111532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudarzi M, Razeghi M, Chirani AS, Fazeli M, Tayebi Z and Pouriran R, 2020. Characteristics of methicillin‐resistant Staphylococcus aureus carrying the toxic shock syndrome toxin gene: high prevalence of clonal complex 22 strains and the emergence of new spa types t223 and t605 in Iran. New Microbes and New Infections, 36, 100695. 10.1016/j.nmni.2020.100695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graveland H, Wagenaar JA, Heesterbeek H, Mevius D, van Duijkeren E and Heederik D, 2010. Methicillin resistant Staphylococcus aureus ST398 in veal calf farming: human MRSA carriage related with animal antimicrobial usage and farm hygiene. PLoS One, 5(6), e10990. 10.1371/journal.pone.0010990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greninger AL, Addetia A, Starr K, Cybulski RJ, Stewart MK, Salipante SJ, Bryan AB, Cookson B, Gaudreau C, Bekal S and Fang FC, 2020. International spread of multidrug‐resistant Campylobacter coli in men who have sex with men in Washington State and Québec, 2015–2018. Clinical Infectious Diseases, 71(8), 1896–1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guardabassi L, Stegger M and Skov R, 2007. Retrospective detection of methicillin resistant and susceptible Staphylococcus aureus ST398 in Danish slaughter pigs. Veterinary Microbiology, 122(3–4), 384–386. 10.1016/j.vetmic.2007.03.021 [DOI] [PubMed] [Google Scholar]
- Guardabassi L, O'Donoghue M, Moodley A, Ho J and Boost M, 2009. Novel Lineage of Methicillin‐Resistant Staphylococcus aureus, Hong Kong. Emerging Infectious Diseases, 15(12), 1998–2000. 10.3201/eid1512.090378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Wang B, Rao L, Wang X, Zhao H, Li M and Yu F, 2021. Molecular characteristics of rifampin‐sensitive and ‐resistant isolates and characteristics of rpoB gene mutations in methicillin‐resistant Staphylococcus aureus . Infection and Drug Resistance, 14, 4591–4600. 10.2147/IDR.S336200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haenni M, Châtre P, Dupieux C, Métayer V, Maillard K, Bes M, Madec JY and Laurent F, 2015. mecC ‐positive MRSA in horses. Journal of Antimicrobial Chemotherapy, 70, 3401–3402. 10.1093/jac/dkv278 [DOI] [PubMed] [Google Scholar]
- Händel N, Otte S, Jonker M, Brul S and ter Kuile B, 2015. Factors that affect transfer of the IncI1 β‐lactam resistance plasmid pESBL‐283 between E. coli strains. PLoS One, 10(4), e0123039. 10.1371/journal.pone.0123039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkey J, le Hello S, Doublet B, Granier SA, Hendriksen RS, Fricke WF, Ceyssens PJ, Gomart C, Billman‐Jacobe H, Holt KE and Weill FX, 2019. Global phylogenomics of multidrug‐resistant Salmonella enterica serotype Kentucky ST198. Microbial Genomics, 5(7). 10.1099/mgen.0.000269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindermann D, Gopinath G, Chase H, Negrete F, Althaus D, Zurfluh K, Tall BD, Stephan R and Nüesch‐Inderbinen M, 2017. Salmonella enterica serovar infantis from food and human infections, Switzerland, 2010–2015: poultry‐related multidrug resistant clones and an emerging ESBL producing clonal lineage. Frontiers Microbiology, 8, 1322. 10.3389/fmicb.2017.01322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He F, Xu J, Wang J, Chen Q, Hua X, Fu Y and Yu Y, 2016. Decreased susceptibility to tigecycline mediated by a mutation in mlaA in Escherichia coli strains. Antimicrobial Agents and Chemotherapy, 60(12), 7530–7531. 10.1128/AAC.01603-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He T, Wang R, Liu D, Walsh TR, Zhang R, Lv Y, Ke Y, Ji Q, Wei R, Liu Z, Shen Y, Wang G, Sun L, Lei L, Lv Z, Li Y, Pang M, Wang L, Sun Q, Fu Y, Song H, Hao Y, Shen Z, Wang S, Chen G, Wu C, Shen J and Wang Y, 2019. Emergence of plasmid‐mediated high‐level tigecycline resistance genes in animals and humans. Nature Microbiology, 4(9), 1450–1456. 10.1038/s41564-019-0445-2 [DOI] [PubMed] [Google Scholar]
- Heikinheimo A, Johler S, Karvonen L, Julmi J, Fredriksson‐Ahomaa M and Stephan R, 2016. ‘New dominant spa type t2741 in livestock‐associated MRSA (CC398‐MRSA‐V) in finnish fattening pigs at slaughter. Antimicrobial Resistance & InfectionControl, 5(1), 6. 10.1186/s13756-016-0105-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriksen RS, Bortolaia V, Tate H, Tyson GH, Aarestrup FM and McDermott PF, 2019. Using Genomics to Track Global Antimicrobial Resistance. Frontiers in Public Health, 7. Available online: https://www.frontiersin.org/articles/10.3389/fpubh.2019.00242 [Accessed: 1 September 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins KL, Kirchner M, Guerra B, Granier SA, Lucarelli C, Porrero MC, Jakubczak A, Threlfall EJ and Mevius DJ, 2010. Multiresistant Salmonella enterica serovar 4,[5],12:i:‐ in Europe: a new pandemic strain? Euro Surveillance: Bulletin Europeen Sur Les Maladies Transmissibles = European Communicable Disease Bulletin, 15(22), 19580. [PubMed] [Google Scholar]
- Irrgang A, Tenhagen BA, Pauly N, Schmoger S, Kaesbohrer A and Hammerl JA, 2019. Characterization of VIM‐1‐producing E. coli isolated From a German fattening pig farm by an improved isolation procedure. Frontiers in Microbiology, 10, 2256. 10.3389/fmicb.2019.02256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irrgang A, Pauly N, Tenhagen BA, Grobbel M, Kaesbohrer A and Hammerl AJA, 2020. Spill‐over from public health? First detection of an OXA‐48‐producing Escherichia coli in a German pig farm. Microorganisms, 8(6), 855. 10.3390/microorganisms8060855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam MZ, Espinosa‐Gongora C, Damborg P, Sieber RN, Munk R, Husted L, Moodley A, Skov R, Larsen J and Guardabassi L, 2017. Horses in Denmark are a reservoir of diverse clones of methicillin‐resistant and ‐susceptible Staphylococcus aureus . Frontiers in Microbiology, 8. 10.3389/fmicb.2017.00543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jehanne Q, Pascoe B, Bénéjat L, Ducournau A, Buissonnière A, Mourkas E, Mégraud F, Bessede E, Sheppard SK and Lehours P, 2020. Genome‐wide identification of host‐segregating single‐nucleotide polymorphisms for source attribution of clinical Campylobacter coli isolates. Applied and Environmental Microbiology, 86(24), e01787‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jehanne Q, Bénéjat L, Ducournau A, Domingues‐Martins C, Cousinou T, Bessède E and Lehours P, 2021. Emergence of erythromycin resistance methyltransferases in Campylobacter coli strains in France. Antimicrobial Agents and Chemotherapy, 65(11), e01124‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokinen C, Edge TA, Ho S, Koning W, Laing C, Mauro W, Medeiros D, Miller J, Robertson W, Taboada E, Thomas JE, Topp E, Ziebell K and Gannon VP, 2011. Molecular subtypes of Campylobacter spp., Salmonella enterica, and Escherichia coli O157: H7 isolated from faecal and surface water samples in the Oldman River watershed, Alberta, Canada. Water Research, 45(3), 1247–1257. [DOI] [PubMed] [Google Scholar]
- Kahlmeter G, Brown DF, Goldstein FW, MacGowan A, Mouton JW, Osterlund A, Rodloff A, Steinbakk M, Urbaskova P and Vatopoulos A, 2003. European harmonization of MIC breakpoints for antimicrobial susceptibility testing of bacteria. Journal of Antimicrobial Chemotherapy, 52(2), 145–148. 10.1093/jac/dkg312 [DOI] [PubMed] [Google Scholar]
- Käppeli N, Morach M, Corti S, Eicher C, Stephan R and Johler S, 2019. Staphylococcus aureus related to bovine mastitis in Switzerland: clonal diversity, virulence gene profiles, and antimicrobial resistance of isolates collected throughout 2017. Journal of Dairy Science, 102(4), 3274–3281. 10.3168/jds.2018-15317 [DOI] [PubMed] [Google Scholar]
- Kieffer N, Aires‐de‐Sousa M, Nordmann P and Poirel L, 2017. High rate of MCR‐1–producing Escherichia coli and Klebsiella pneumoniae among pigs, Portugal. Emerging Infectious Diseases, 23(12), 2023–2029. 10.3201/eid2312.170883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinross P, Petersen A, Skov R, van Hauwermeiren E, Pantosti A, Laurent F, Voss A, Kluytmans J, Struelens MJ, Heuer O, Monnet DL and European Human LA‐MRSA Study Group , 2017. Livestock‐associated meticillin‐resistant Staphylococcus aureus (MRSA) among human MRSA isolates, European Union/European Economic Area countries, 2013. Eurosurveillance, 22(44). 10.2807/1560-7917.ES.2017.22.44.16-00696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kittler S, Seinige D, Meemken D, Müller A, Wendlandt S, Ehricht R, Monecke S and Kehrenberg C, 2019. Characteristics of methicillin‐resistant Staphylococcus aureus from broiler farms in Germany are rather lineage‐ than source‐specific. Poultry Science, 98(12), 6903–6913. 10.3382/ps/pez439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köck R, Schaumburg F, Mellmann A, Köksal M, Jurke A, Becker K and Friedrich AW, 2013. Livestock‐associated methicillin‐resistant Staphylococcus aureus (MRSA) as causes of human infection and colonization in Germany. PLoS One, 8(2), e55040. 10.1371/journal.pone.0055040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köck R, Daniels‐Haardt I, Becker K, Mellmann A, Friedrich AW, Mevius D, Schwarz S and Jurke A, 2018. Carbapenem‐resistant Enterobacteriaceae in wildlife, food‐producing, and companion animals: a systematic review. Clinical Microbiology and Infection, 24(12), 1241–1250. 10.1016/j.cmi.2018.04.004 [DOI] [PubMed] [Google Scholar]
- Kraemer JG, Pires J, Kueffer M, Semaani E, Endimiani A, Hilty M and Oppliger A, 2017. Prevalence of extended‐spectrum β‐lactamase‐producing Enterobacteriaceae and methicillin‐resistant Staphylococcus aureus in pig farms in Switzerland. Science of The Total Environment, 603–604, 401–405. 10.1016/j.scitotenv.2017.06.110 [DOI] [PubMed] [Google Scholar]
- Kreling V, Falcone FH, Kehrenberg C and Hensel A, 2020. Campylobacter sp.: pathogenicity factors and prevention methods – new molecular targets for innovative antivirulence drugs? Applied Microbiology and Biotechnology, 104(24), 10409–10436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam TJGM, Heuvelink AE, Gonggrijp MA and Santman‐Berends IMGA, 2020. Antimicrobial use in dairy cattle in the Netherlands. Journal of Animal Science, 98(Suppl 1), S9–S14. 10.1093/jas/skaa143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen J, Stegger M, Andersen PS, Petersen A, Larsen AR, Westh H, Agersø Y, Fetsch A, Kraushaar B, Käsbohrer A, Feβler AT, Schwarz S, Cuny C, Witte W, Butaye P, Denis O, Haenni M, Madec JY, Jouy E, Laurent F, Battisti A, Franco A, Alba P, Mammina C, Pantosti A, Monaco M, Wagenaar JA, de Boer E, van Duijkeren E, Heck M, Domínguez L, Torres C, Zarazaga M, Price LB and Skov RL, 2016. Evidence for human adaptation and foodborne transmission of livestock‐associated methicillin‐resistant Staphylococcus aureus . Clinical Infectious Diseases, 63(10), 1349–1352. 10.1093/cid/ciw532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen J, Sunde M, Islam MZ, Urdahl AM, Barstad AS, Larsen AR, Grøntvedt CA and Angen Ø, 2017. Evaluation of a widely used culture‐based method for detection of livestock‐associated meticillin‐resistant Staphylococcus aureus (MRSA), Denmark and Norway, 2014 to 2016. Eurosurveillance, 22(28). 10.2807/1560-7917.ES.2017.22.28.30573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen J, Raisen CL, Ba X, Sadgrove NJ, Padilla‐González GF, Simmonds MSJ, Loncaric I, Kerschner H, Apfalter P, Hartl R, Deplano A, Vandendriessche S, Černá Bolfíková B, Hulva P, Arendrup MC, Hare RK, Barnadas C, Stegger M, Sieber RN, Skov RL, Petersen A, Angen Ø, Rasmussen SL, Espinosa‐Gongora C, Aarestrup FM, Lindholm LJ, Nykäsenoja SM, Laurent F, Becker K, Walther B, Kehrenberg C, Cuny C, Layer F, Werner G, Witte W, Stamm I, Moroni P, Jørgensen HJ, de Lencastre H, Cercenado E, García‐Garrote F, Börjesson S, Hæggman S, Perreten V, Teale CJ, Waller AS, Pichon B, Curran MD, Ellington MJ, Welch JJ, Peacock SJ, Seilly DJ, Morgan FJE, Parkhill J, Hadjirin NF, Lindsay JA, Holden MTG, Edwards GF, Foster G, Paterson GK, Didelot X, Holmes MA, Harrison EM and Larsen AR, 2022. Emergence of methicillin resistance predates the clinical use of antibiotics. Nature, 602(7895), 135–141. 10.1038/s41586-021-04265-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Hello S, Hendriksen RS, Doublet B, Fisher I, Nielsen EM, Whichard JM, Bouchrif B, Fashae K, Granier SA, Jourdan‐da Silva N, Cloeckaert A, Threlfall EJ, Angulo FJ, Aarestrup FM, Wain J and Weill FX, 2011. International spread of an epidemic population of Salmonella enterica serotype kentucky ST198 resistant to ciprofloxacin. The Journal of Infectious Diseases, 204(5), 675–684. 10.1093/infdis/jir409 [DOI] [PubMed] [Google Scholar]
- Le Hello S, Bekhit A, Granier SA, Barua H, Beutlich J, Zając M, Münch S, Sintchenko V, Bouchrif B, Fashae K, Pinsard JL, Sontag L, Fabre L, Garnier M, Guibert V, Howard P, Hendriksen RS, Christensen JP, Biswas PK, Cloeckaert A, Rabsch W, Wasyl D, Doublet B and Weill FX, 2013. The global establishment of a highly‐fluoroquinolone resistant Salmonella enterica serotype Kentucky ST198 strain. Frontiers in Microbiology, 4. 10.3389/fmicb.2013.00395 [Accessed: 1 September 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levings RS, Lightfoot D, Partridge SR, Hall RM and Djordjevic SP, 2005. The genomic island SGI1, containing the multiple antibiotic resistance region of Salmonella enterica serovar typhimurium DT104 or variants of it, is widely distributed in other S. enterica serovars. Journal of Bacteriology, 187(13), 4401–4409. 10.1128/JB.187.13.4401-4409.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Liao X, Yang Y, Sun J, Li L, Liu B, Yang S, Ma J, Li X, Zhang Q and Liu Y, 2013. Spread of oqxAB in Salmonella enterica serotype Typhimurium predominantly by IncHI2 plasmids. Journal of Antimicrobial Chemotherapy, 68(10), 2263–2268. 10.1093/jac/dkt209 [DOI] [PubMed] [Google Scholar]
- Liu B‐T, Zhang XY, Wan SW, Hao JJ, Jiang RD and Song FJ, 2018. Characteristics of carbapenem‐resistant Enterobacteriaceae in ready‐to‐eat vegetables in China. Frontiers in Microbiology, 9, 1147. 10.3389/fmicb.2018.01147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D, Liu W, Lv Z, Xia J, Li X, Hao Y, Zhou Y, Yao H, Liu Z, Wang Y, Shen J, Ke Y and Shen Z, 2019. Emerging erm (B)‐mediated macrolide resistance associated with novel multidrug resistance genomic islands in Campylobacter . Antimicrobial Agents and Chemotherapy, 63(7), e00153‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez‐Chavarrias V, Ugarte‐Ruiz M, Barcena C, Olarra A, Garcia M, Saez JL, de Frutos C, Serrano T, Perez I, Moreno MA, Dominguez L and Alvarez J, 2021. Monitoring of antimicrobial resistance to aminoglycosides and macrolides in Campylobacter coli and Campylobacter jejuni from healthy livestock in Spain (2002–2018). Frontiers in Microbiology, 12. 10.3389/fmicb.2021.689262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano C, Aspiroz C, Ara M, Gómez‐Sanz E, Zarazaga M and Torres C, 2011. Methicillin‐resistant Staphylococcus aureus (MRSA) ST398 in a farmer with skin lesions and in pigs of his farm: clonal relationship and detection of lnu(A) gene. Clinical Microbiology and Infection, 17(6), 923–927. 10.1111/j.l469-0691.2010.03437.x [DOI] [PubMed] [Google Scholar]
- Lozano C, Gharsa H, Ben Slama K, Zarazaga M and Torres C, 2016. ‘Staphylococcus aureus in animals and food: methicillin resistance, prevalence and population structure. A review in the African continent. Microorganisms, 4(1), E12. 10.3390/microorganisms4010012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano C, Fernández‐Fernández R, Ruiz‐Ripa L, Gómez P, Zarazaga M and Torres C, 2020. Human mecC‐carrying MRSA: clinical implications and risk factors. Microorganisms, 8(10), 1615. 10.3390/microorganisms8101615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luangtongkum T, Jeon B, Han J, Plummer P, Logue CM and Zhang Q, 2009. Antibiotic resistance in Campylobacter: emergence, transmission and persistence. Future Microbiology, 4(2), 189–200. 10.2217/17460913.4.2.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luk‐in S, Pulsrikarn C, Bangtrakulnonth A, Chatsuwan T and Kulwichit W, 2017. Occurrence of a novel class 1 integron harboring qnrVC4 in Salmonella Rissen . Diagnostic Microbiology and Infectious Disease, 88(3), 282–286. 10.1016/j.diagmicrobio.2017.03.016 [DOI] [PubMed] [Google Scholar]
- Magiorakos A‐P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson‐Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT and Monnet DL, 2012. Multidrug‐resistant, extensively drug‐resistant and pandrug‐resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clinical Microbiology and Infection, 18(3), 268–281. 10.1111/j.1469-0691.2011.03570.x [DOI] [PubMed] [Google Scholar]
- Mališová L, Jakubů V, Musílek M, Kekláková J and Žemličková H, 2020. Phenotype and genotype characteristics of Staphylococcus aureus resistant to methicillin/oxacillin carrying gene mecC in the Czech Republic from 2002 to 2017. Microbial Drug Resistance, 26(8), 918–923. 10.1089/mdr.2019.0319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallioris P, Dohmen W, Luiken REC, Wagenaar JA, Stegeman A and Mughini‐Gras L, 2022. Factors associated with antimicrobial use in pig and veal calf farms in the Netherlands: A multi‐method longitudinal data analysis. Preventive Veterinary Medicine, 199, 105563. 10.1016/j.prevetmed.2021.105563 [DOI] [PubMed] [Google Scholar]
- Maraolo AE, Giaccone A, Gentile I, Saracino A and Bavaro DF, 2021. Daptomycin versus vancomycin for the treatment of methicillin‐resistant Staphylococcus aureus bloodstream infection with or without endocarditis: a systematic review and meta‐analysis. Antibiotics, 10(8), 1014. 10.3390/antibiotics10081014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez JL, 2014. General principles of antibiotic resistance in bacteria. Drug Discovery Today: Technologies, 11, 33–39. 10.1016/j.ddtec.2014.02.001 [DOI] [PubMed] [Google Scholar]
- Maslikowska JA, Walker SA, Elligsen M, Mittmann N, Palmay L, Daneman N and Simor A, 2016. Impact of infection with extended‐spectrum β‐lactamase‐producing Escherichia coli or Klebsiella species on outcome and hospitalization costs. Journal of Hospital Infection, 92(1), 33–41. 10.1016/j.jhin.2015.10.001 [DOI] [PubMed] [Google Scholar]
- Matuschek E, Åhman J, Webster C, Kahlmeter G, 2018. Antimicrobial susceptibility testing of colistin ‐ evaluation of seven commercial MIC products against standard broth microdilution for Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter spp. Clin Microbiol Infect, 24(8), 865–870. 10.1016/j.cmi.2017.11.020 [DOI] [PubMed] [Google Scholar]
- McDermott PF, Tyson GH, Kabera C, Chen Y, Li C, Folster JP, Ayers SL, Lam C, Tate HP and Zhao S, 2016. Whole‐genome sequencing for detecting antimicrobial resistance in nontyphoidal Salmonella. Antimicrobial Agents Chemotheraphy, 60, 5515–5520. 10.1128/AAC.01030-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuinness WA, Malachowa N and DeLeo FR, 2017. Vancomycin resistance in Staphylococcus aureus . The Yale Journal of Biology and Medicine, 90(2), 269–281. [PMC free article] [PubMed] [Google Scholar]
- McManus BA, Aloba BK, Earls MR, Brennan GI, O’Connell B, Monecke S, Ehricht R, Shore AC and Coleman DC, 2021. Multiple distinct outbreaks of Panton‐Valentine leucocidin‐positive community‐associated meticillin‐resistant Staphylococcus aureus in Ireland investigated by whole‐genome sequencing. Journal of Hospital Infection, 108, 72–80. 10.1016/j.jhin.2020.11.021 [DOI] [PubMed] [Google Scholar]
- Medialdea CR, Melillo T, Rocco G and Borg M, 2020. Investigation of an outbreak of ESBL‐producing Salmonella Kentucky in humans linked to poultry in Malta, 2013–2020. 24‐27 November 2020. In Proceedings of the European Scientific Conference on Applied Infectious Disease Epidemiology (ESCAIDE). ECDC. Available online: https://www.escaide.eu/sites/default/files/documents/Escaide2020-abstract-book.pdf
- Mesa Varona O, Chaintarli K, Muller‐Pebody B, Anjum MF, Eckmanns T, Norström M, Boone I and Tenhagen BA, 2020. Monitoring antimicrobial resistance and drug usage in the human and livestock sector and foodborne antimicrobial resistance in six European countries. Infection and Drug Resistance, 13, 957–993. 10.2147/IDR.S237038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monecke S, Coombs G, Shore AC, Coleman DC, Akpaka P, Borg M, Chow H, Ip M, Jatzwauk L, Jonas D, Kadlec K, Kearns A, Laurent F, O'Brien FG, Pearson J, Ruppelt A, Schwarz S, Scicluna E, Slickers P, Tan HL, Weber S and Ehricht R, 2011. A field guide to pandemic, epidemic and sporadic clones of methicillin‐resistant Staphylococcus aureus . PLoS One, 6(4), e17936. 10.1371/journal.pone.0017936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore JE, Barton MD, Blair IS, Corcoran D, Dooley JS, Fanning S, Kempf I, Lastovica AJ, Lowery CJ, Matsuda M, McDowell D, McMahon A, Millar BC, Rao JR, Rooney PJ, Seal BS, Snelling WJ and Tolba O, 2006. The epidemiology of antibiotic resistance in Campylobacter . Microbes and infection, 8(7), 1955–1966. [DOI] [PubMed] [Google Scholar]
- Moré E, Ayats T, Ryan PG, Naicker PR, Keddy KH, Gaglio D, Witteveen M and Cerdà‐Cuéllar M, 2017. Seabirds (Laridae) as a source of Campylobacter spp., Salmonella spp. and antimicrobial resistance in South Africa. Environmental Microbiology, 19(10), 4164–4176. [DOI] [PubMed] [Google Scholar]
- Mouftah SF, Cobo‐Díaz JF, Álvarez‐Ordóñez A, Elserafy M, Saif NA, Sadat A, el‐Shibiny A and Elhadidy M, 2021. High‐throughput sequencing reveals genetic determinants associated with antibiotic resistance in Campylobacter spp. from farm‐to‐fork. PLos One, 16(6), e0253797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mourkas E, Florez‐Cuadrado D, Pascoe B, Calland JK, Bayliss SC, Mageiros L, Méric G, Hitchings MD, Quesada A, Porrero C, Ugarte‐Ruiz M, Gutiérrez‐Fernández J, Domínguez L and Sheppard SK, 2019. Gene pool transmission of multidrug resistance among Campylobacter from livestock, sewage and human disease. Environmental Microbiology, 21(12), 4597–4613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemeghaire S, Argudín MA, Haesebrouck F and Butaye P, 2014. Epidemiology and molecular characterization of methicillin‐resistant Staphylococcus aureus nasal carriage isolates from bovines. BMC Veterinary Research, 10(1), 153. 10.1186/1746-6148-10-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nógrády N, Király M, Davies R and Nagy B, 2012. Multidrug resistant clones of Salmonella infantis of broiler origin in Europe. International Journal of Food Microbiology, 157(1), 108–112. 10.1016/j.ijfoodmicro.2012.04.007 [DOI] [PubMed] [Google Scholar]
- Normanno G, Dambrosio A, Lorusso V, Samoilis G, di Taranto P and Parisi A, 2015. Methicillin‐resistant Staphylococcus aureus (MRSA) in slaughtered pigs and abattoir workers in Italy. Food Microbiology, 51, 51–56. 10.1016/j.fm.2015.04.007 [DOI] [PubMed] [Google Scholar]
- OECD , 2022. Antimicrobial resistance in the EU/EEA. A one health response. OECD. Available online: https://www.oecd.org/health/Antimicrobial-Resistance-in-the-EU-EEA-A-One-Health-Response-March-2022.pdf [Accessed: 11 August 2022]. [Google Scholar]
- Olaitan AO, Morand S and Rolain J‐M, 2014. Mechanisms of polymyxin resistance: acquired and intrinsic resistance in bacteria. Frontiers in Microbiology, 5. Available online: https://www.frontiersin.org/articles/10.3389/fmicb.2014.00643 [Accessed: 1 September 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan Y, Awan F, Zhenbao M, Zhang X, Zeng J, Zeng Z and Xiong W, 2020. Preliminary view of the global distribution and spread of the tet(X) family of tigecycline resistance genes. Journal of Antimicrobial Chemotherapy, 75(10), 2797–2803. 10.1093/jac/dkaa284 [DOI] [PubMed] [Google Scholar]
- Paterson GK, Morgan FJ, Harrison EM, Peacock SJ, Parkhill J, Zadoks RN and Holmes MA, 2014. Prevalence and properties of mecC methicillin‐resistant Staphylococcus aureus (MRSA) in bovine bulk tank milk in Great Britain. Journal of Antimicrobial Chemotherapy, 69(3), 598–602. 10.1093/jac/dkt417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauly N, Wichmann‐Schauer H, Ballhausen B, Torres Reyes N, Fetsch A and Tenhagen BA, 2019. Detection and quantification of methicillin‐resistant Staphylococcus aureus in fresh broiler meat at retail in Germany. International Journal of Food Microbiology, 292, 8–12. 10.1016/j.ijfoodmicro.2018.11.025 [DOI] [PubMed] [Google Scholar]
- Pauly N, Hammerl JA, Schwarz S, Grobbel M, Meemken D, Malorny B, Tenhagen BA, Käsbohrer A and Irrgang A, 2021. Co‐occurrence of the bla VIM‐1 and bla SHV‐12 genes on an IncHI2 plasmid of an Escherichia coli isolate recovered from German livestock. Journal of Antimicrobial Chemotherapy, 76(2), 531–533. 10.1093/jac/dkaa436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pergola S, Franciosini MP, Comitini F, Ciani M, de Luca S, Bellucci S, Menchetti L and Casagrande Proietti P, 2017. Genetic diversity and antimicrobial resistance profiles of Campylobacter coli and Campylobacter jejuni isolated from broiler chicken in farms and at time of slaughter in central Italy. Journal of Applied Microbiology, 122(5), 1348–1356. [DOI] [PubMed] [Google Scholar]
- Pimenta AC, Fernandes R and Moreira IS, 2014. Evolution of drug resistance: insight on TEM β‐lactamases structure and activity and β‐lactam antibiotics. Mini Reviews in Medicinal Chemistry, 14(2), 111–122. [DOI] [PubMed] [Google Scholar]
- Pornsukarom S, Patchanee P, Erdman M, Cray PF, Wittum T, Lee J and Gebreyes WA, 2015. Comparative phenotypic and genotypic analyses of Salmonella Rissen that originated from food animals in Thailand and United States. Zoonoses and Public Health, 62(2), 151–158. 10.1111/zph.12144 [DOI] [PubMed] [Google Scholar]
- Pulss S, Semmler T, Prenger‐Berninghoff E, Bauerfeind R and Ewers C, 2017. First report of an Escherichia coli strain from swine carrying an OXA‐181 carbapenemase and the colistin resistance determinant MCR‐1. International Journal of Antimicrobial Agents, 50(2), 232–236. 10.1016/j.ijantimicag.2017.03.014 [DOI] [PubMed] [Google Scholar]
- Qin S, Wang Y, Zhang Q, Zhang M, Deng F, Shen Z, Wu C, Wang S, Zhang J and Shen J, 2014. Report of ribosomal RNA methylase gene erm (B) in multidrug‐resistant Campylobacter coli . Journal of Antimicrobial Chemotherapy, 69(4), 964–968. [DOI] [PubMed] [Google Scholar]
- Queenan K, Häsler B and Rushton J, 2016. A one health approach to antimicrobial resistance surveillance: is there a business case for it? International Journal of Antimicrobial Agents, 48(4), 422–427. 10.1016/j.ijantimicag.2016.06.014 [DOI] [PubMed] [Google Scholar]
- Resch G, François P, Morisset D, Stojanov M, Bonetti EJ, Schrenzel J, Sakwinska O and Moreillon P, 2013. Human‐to‐bovine jump of Staphylococcus aureus CC8 is associated with the loss of a β‐hemolysin converting prophage and the acquisition of a new staphylococcal cassette chromosome. PLoS One, 8(3), e58187. 10.1371/journal.pone.0058187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricci V, Zhang D, Teale C and Piddock LJV 2020. The O‐antigen epitope governs susceptibility to colistin in Salmonella enterica . mBio, 11(1), e02831‐19. 10.1128/mBio.02831-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter A, Sting R, Popp C, Rau J, Tenhagen BA, Guerra B, Hafez HM and Fetsch A, 2012. Prevalence of types of methicillin‐resistant Staphylococcus aureus in turkey flocks and personnel attending the animals. Epidemiology and Infection, 140(12), 2223–2232. 10.1017/S095026881200009X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rincón‐Real AA and Suárez‐Alfonso MC, 2022. Carbapenem resistance in critically important human pathogens isolated from companion animals: a systematic literature review. Osong Public Health and Research Perspectives, 13, 407–423. 10.24171/j.phrp.2022.0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahibzada S, Abraham S, Coombs GW, Pang S, Hernández‐Jover M, Jordan D and Heller J, 2017. Transmission of highly virulent community‐associated MRSA ST93 and livestock‐associated MRSA ST398 between humans and pigs in Australia. Scientific Reports, 7(1), 5273. 10.1038/s41598-017-04789-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnitt A, Lienen T, Wichmann‐Schauer H, Cuny C and Tenhagen BA, 2020. The occurrence and distribution of livestock‐associated methicillin‐resistant Staphylococcus aureus ST398 on German dairy farms. Journal of Dairy Science, 103(12), 11806–11819. 10.3168/jds.2020-18958 [DOI] [PubMed] [Google Scholar]
- Sévellec Y, Vignaud ML, Granier SA, Lailler R, Feurer C, le Hello S, Mistou MY and Cadel‐Six S, 2018. Polyphyletic nature of Salmonella enterica serotype derby and lineage‐specific host‐association revealed by genome‐wide analysis. Frontiers in Microbiology, 9, 891. 10.3389/fmicb.2018.00891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sévellec Y, Granier SA, Le Hello S, Weill FX, Guillier L, Mistou MY and Cadel‐Six S, 2020. Source attribution study of sporadic Salmonella derby cases in France. Frontiers in Microbiology, 11. 10.3389/fmicb.2020.00889 [Accessed: 20 September 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore AC, Deasy EC, Slickers P, Brennan G, O'Connell B, Monecke S, Ehricht R and Coleman DC, 2011. Detection of Staphylococcal cassette chromosome mec Type XI carrying highly divergent mecA, mecI, mecR1, blaZ, and ccr genes in human clinical isolates of clonal complex 130 methicillin‐resistant Staphylococcus aureus . Antimicrobial Agents and Chemotherapy, 55(8), 3765–3773. 10.1128/AAC.00187-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva V, Capelo JL, Igrejas G and Poeta P, 2020. Molecular epidemiology of Staphylococcus aureus lineages in wild animals in Europe: a review. Antibiotics, 9(3). 10.3390/antibiotics9030122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva V, Gabriel SI, Borrego SB, Tejedor‐Junco MT, Manageiro V, Ferreira E, Reis L, Caniça M, Capelo JL, Igrejas G and Poeta P, 2021. Antimicrobial resistance and genetic lineages of Staphylococcus aureus from wild rodents: first report of mecC‐positive methicillin‐resistant S. aureus (MRSA) in Portugal. Animals, 11(6), 1537. 10.3390/ani11061537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skov RL and Monnet DL, 2016. Plasmid‐mediated colistin resistance (mcr‐1 gene): three months later, the story unfolds. Eurosurveillance, 21(9). 10.2807/1560-7917.ES.2016.21.9.30155 [DOI] [PubMed] [Google Scholar]
- Sopwith W, Birtles A, Matthews M, Fox A, Gee S, Painter M, Regan M, Syed Q and Bolton E, 2008. Identification of potential environmentally adapted Campylobacter jejuni strain, United Kingdom. Emerging Infectious Diseases, 14(11), 1769–1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegger M, Lindsay JA, Moodley A, Skov R, Broens EM and Guardabassi L, 2011. Rapid PCR detection of Staphylococcus aureusclonal complex 398 by targeting the restriction‐modification system carrying sau1‐hsdS1. Journal of Clinical Microbiology, 49, 732–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun H, Wan Y, Du P and Bai L, 2020. The epidemiology of monophasic Salmonella Typhimurium . Foodborne Pathogens and Disease, 17(2), 87–97. 10.1089/fpd.2019.2676 [DOI] [PubMed] [Google Scholar]
- Szczepanska B, Andrzejewska M, Spica D and Klawe JJ, 2017. Prevalence and antimicrobial resistance of Campylobacter jejuni and Campylobacter coli isolated from children and environmental sources in urban and suburban areas. BMC Microbiology, 17(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taggar G, Attiq Rheman M, Boerlin P and Diarra MS, 2020. Molecular epidemiology of carbapenemases in enterobacteriales from humans, animals, food and the environment. Antibiotics, 9(10), 693. 10.3390/antibiotics9100693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y, Fang L, Xu C and Zhang Q, 2017. Antibiotic resistance trends and mechanisms in the foodborne pathogen, Campylobacter . Animal Health Research Reviews, 18(2), 87–98. [DOI] [PubMed] [Google Scholar]
- Tate H, Folster JP, Hsu CH, Chen J, Hoffmann M, Li C, Morales C, Tyson GH, Mukherjee S, Brown AC, Green A, Wilson W, Dessai U, Abbott J, Joseph L, Haro J, Ayers S, McDermott P and Zhao S, 2017. Comparative analysis of extended‐spectrum‐β‐lactamase CTX‐M‐65‐producing Salmonella enterica serovar infantis isolates from humans, food animals, and retail chickens in the United States. Antimicrobial Agents and Chemotherapy, 61(7), e00488‐17. 10.1128/AAC.00488-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tegegne HA, Koláčková I, Florianová M, Gelbíčová T, Madec JY, Haenni M and Karpíšková R, 2021a. Detection and molecular characterisation of methicillin‐resistant Staphylococcus aureus isolated from raw meat in the retail market. Journal of Global Antimicrobial Resistance, 26, 233–238. 10.1016/j.jgar.2021.06.012 [DOI] [PubMed] [Google Scholar]
- Tegegne HA, Koláčková I, Florianová M, Wattiau P, Gelbíčová T, Boland C, Madec JY, Haenni M and Karpíšková R, 2021b. Genomic insights into methicillin‐resistant Staphylococcus aureus spa Type t899 isolates belonging to different sequence types. Applied and Environmental Microbiology, 87(6), e01994‐20. 10.1128/AEM.01994-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenhagen B‐A, Vossenkuhl B, Käsbohrer A, Alt K, Kraushaar B, Guerra B, Schroeter A and Fetsch A, 2014. Methicillin‐resistant Staphylococcus aureus in cattle food chains – prevalence, diversity, and antimicrobial resistance in Germany. Journal of Animal Science, 92(6), 2741–2751. 10.2527/jas.2014-7665 [DOI] [PubMed] [Google Scholar]
- Titouche Y, Akkou M, Houali K, Auvray F and Hennekinne JA, 2022. Role of milk and milk products in the spread of methicillin‐resistant Staphylococcus aureus in the dairy production chain. Journal of Food Science, 87(9), 3699–3723. 10.1111/1750-3841.16259 [DOI] [PubMed] [Google Scholar]
- Törneke K, Torren‐Edo J, Grave K and Mackay DK, 2015. The management of risk arising from the use of antimicrobial agents in veterinary medicine in EU/EEA countries – a review. Journal of Veterinary Pharmacology and Therapeutics, 38(6), 519–528. 10.1111/jvp.12226 [DOI] [PubMed] [Google Scholar]
- Touati A, Mairi A, Baloul Y, Lalaoui R, Bakour S, Thighilt L, Gharout A and Rolain JM, 2017. First detection of Klebsiella pneumoniae producing OXA‐48 in fresh vegetables from Béjaïa city, Algeria. Journal of Global Antimicrobial Resistance, 9, 17–18. 10.1016/j.jgar.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Trio Presidency of the Council of the European Union , 2022. Declaration on Antimicrobial Resistance. Trio Presidency of the Council of the EU, France, Czech Republic and Sweden. Available online: https://solidarites-sante.gouv.fr/IMG/pdf/220306_declaration_trio_en_final.pdf [Accessed: 11 August 2022]. [Google Scholar]
- Turner NA, Sharma‐Kuinkel BK, Maskarinec SA, Eichenberger EM, Shah PP, Carugati M, Holland TL and Fowler VG Jr, 2019. Methicillin‐resistant Staphylococcus aureus: an overview of basic and clinical research. Nature Reviews Microbiology, 17(4), 203–218. 10.1038/s41579-018-0147-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhegghe M, Pletinckx LJ, Crombé F, Vandersmissen T, Haesebrouck F, Butaye P, Heyndrickx M and Rasschaert G, 2013. Methicillin‐resistant Staphylococcus aureus (MRSA) ST398 in pig farms and multispecies farms. Zoonoses and Public Health, 60(5), 366–374. 10.1111/zph.12007 [DOI] [PubMed] [Google Scholar]
- Viana AS, Nunes Botelho AM, Moustafa AM, Boge CLK, Pires Ferreira AL, da Silva Carvalho MC, Guimarães MA, Costa BSS, de Mattos MC, Maciel SP, Echevarria‐Lima J, Narechania A, O'Brien K, Ryan C, Gerber JS, Carvalho BTF, Figueiredo AMS and Planet PJ, 2021. Multidrug‐resistant methicillin‐resistant Staphylococcus aureus associated with bacteremia and monocyte evasion, Rio de Janeiro, Brazil. Emerging Infectious Diseases, 27(11), 2825–2835. 10.3201/eid2711.210097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vossenkuhl B, Brandt J, Fetsch A, Käsbohrer A, Kraushaar B, Alt K and Tenhagen BA, 2014. Comparison of spa Types, SCCmec types and antimicrobial resistance profiles of MRSA isolated from Turkeys at Farm, Slaughter and from retail meat indicates transmission along the production chain. PLoS One, 9(5), e96308. 10.1371/journal.pone.0096308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace RL, Bulach D, Valcanis M, Polkinghorne BG, Pingault N, Stylianopoulos A, Givney RC, Glass K and Kirka MD, 2020. Identification of the first erm (B)‐positive Campylobacter jejuni and Campylobacter coli associated with novel multidrug resistance genomic islands in Australia. Journal of Global Antimicrobial Resistance, 23, 311–314. [DOI] [PubMed] [Google Scholar]
- Wang Y, Zhang M, Deng F, Shen Z, Wu C, Zhang J, Zhang Q and Shen J, 2014. Emergence of multidrug‐resistant Campylobacter species isolates with a horizontally acquired rRNA methylase. Antimicrobial Agents and Chemotherapy, 58(9), 5405–5412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Zhang A, Yang Y, Lei C, Jiang W, Liu B, Shi H, Kong L, Cheng G, Zhang X, Yang X and Wang H, 2017. Emergence of Salmonella enterica serovar Indiana and California isolates with concurrent resistance to cefotaxime, amikacin and ciprofloxacin from chickens in China. International Journal of Food Microbiology, 262, 23–30. 10.1016/j.ijfoodmicro.2017.09.012 [DOI] [PubMed] [Google Scholar]
- Wang Y, Liu F, Xu X, Huang H, Lyu N, Ma S, Chen L, Mao M, Hu Y, Song X, Li J, Pan Y, Wang, A , Zhang G, Zhu B and Gao GF, 2021. Detection of plasmid‐mediated tigecycline resistance gene tet(X4) in a Salmonella enterica serovar llandoff isolate. Infectious Microbes & Diseases, 3(4), 198–204. 10.1097/IM9.0000000000000077 [DOI] [Google Scholar]
- Webb AL, Selinger LB, Taboada EN and Inglis GD, 2018. Subtype‐specific selection for resistance to fluoroquinolones but not to tetracyclines is evident in Campylobacter jejuni isolates from beef cattle in confined feeding operations in Southern Alberta, Canada. Applied and Environmental Microbiology, 84(7), e02713‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei B and Kang M, 2018. Molecular basis of macrolide resistance in Campylobacter strains isolated from Poultry in South Korea. Biomed Research International, 2018, 4526576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization) , 2012. The evolving threat of antimicrobial resistance: options for action. World Health Organization. Available online: https://apps.who.int/iris/handle/10665/44812 [Google Scholar]
- WHO , 2019. Critically Important Antimicrobials for Human Medicine. 6th Revision. World Health Organisation. Available online: https://apps.who.int/iris/bitstream/handle/10665/312266/9789241515528-eng.pdf?ua=1 [Google Scholar]
- WHO , 2020. GLASS Whole‐Genome Sequencing for Surveillance of Antimicrobial Resistance. World Health Organisation. Geneva. Available online: https://www.who.int/publications-detail-redirect/9789240011007 [Accessed: 20 June 2022]. [Google Scholar]
- WHO/ECDC , 2022. Antimicrobial resistance surveillance in Europe 2022–2020 data.
- WHO (World Health Organization) , 2019. Ten health issues WHO will tackle this year. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 [Accessed: 13 June 2022].
- Wu D, Wang H, Zhu F, Jiang S, Sun L, Zhao F, Yu Y and Chen Y, 2020. Characterization of an ST5‐SCCmec II‐t311 methicillin‐resistant Staphylococcus aureus strain with a widespread cfr‐positive plasmid. Journal of Infection and Chemotherapy, 26(7), 699–705. 10.1016/j.jiac.2020.02.018 [DOI] [PubMed] [Google Scholar]
- Yaghoubi S, Zekiy AO, Krutova M, Gholami M, Kouhsari E, Sholeh M, Ghafouri Z and Maleki F, 2022. Tigecycline antibacterial activity, clinical effectiveness, and mechanisms and epidemiology of resistance: narrative review. European Journal of Clinical Microbiology & Infectious Diseases, 41(7), 1003–1022. 10.1007/s10096-020-04121-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaici L, Haenni M, Saras E, Boudehouche W, Touati A and Madec JY, 2016. blaNDM‐5‐carrying IncX3 plasmid in Escherichia coli ST1284 isolated from raw milk collected in a dairy farm in Algeria. Journal of Antimicrobial Chemotherapy, 71(9), 2671–2672. 10.1093/jac/dkw160 [DOI] [PubMed] [Google Scholar]
- Yan J‐J, Wu JJ, Ko WC, Tsai SH, Chuang CL, Wu HM, Lu YJ and Li JD, 2004. Plasmid‐mediated 16S rRNA methylases conferring high‐level aminoglycoside resistance in Escherichia coli and Klebsiella pneumoniae isolates from two Taiwanese hospitals. The Journal of Antimicrobial Chemotherapy, 54(6), 1007–1012. 10.1093/jac/dkh455 [DOI] [PubMed] [Google Scholar]
- Yao H, Shen Z, Wang Y, Deng F, Liu D, Naren G, Dai L, Su CC, Wang B, Wang S, Wu C, Yu EW, Zhang Q and Shen J, 2016. Emergence of a potent multidrug efflux pump variant that enhances Campylobacter resistance to multiple antibiotics. mBio, 7(5), e01543‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu F, Cienfuegos‐Gallet AV, Cunningham MH, Jin Y, Wang B, Kreiswirth BN and Chen L, 2021. ‘Molecular evolution and adaptation of livestock‐associated methicillin‐resistant Staphylococcus aureus (LA‐MRSA) sequence type 9. mSystems, 6(3), e0049221. 10.1128/mSystems.00492-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X‐R, Sun YH, Chang MX and Jiang HX, 2022. Plasmid and chromosomal copies of blaCMY‐2 mediate resistance to third‐generation cephalosporins in Escherichia coli from food animals in China. Veterinary Microbiology, 271, 109493. 10.1016/j.vetmic.2022.109493 [DOI] [PubMed] [Google Scholar]
- Zurfluh K, Poirel L, Nordmann P, Klumpp J and Stephan R, 2015. ‘First detection of Klebsiella variicola producing OXA‐181 carbapenemase in fresh vegetable imported from Asia to Switzerland. Antimicrobial Resistance and Infection Control, 4(1), 38. 10.1186/s13756-015-0080-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Plain Language Summary


