Abstract
Background and aim:
Femoral neck fractures are among the most frequent in mankind. Screw fixation is considered a suitable approach specially for undisplaced or slightly displaced fractures that occur to young patients. We conducted our study in order to evaluate both functional outcomes and complication rates of patients who received this treatment in our institution. A particular focus was given to the aseptic necrosis of the head, trying to identify if anamnestic, clinical or radiological data could play a significant role as prognostic factors.
Methods:
For each case who was treated with screw fixation due to a femoral neck fracture, we recorded data regarding, among the others, BMI and whether they used tobacco products or corticosteroids on a regular basis. Necrosis of the femoral head and mechanical complications were recorded. Functional outcome was evaluated using the Harris Hip Score.
Results:
74 cases were included in our study. The mean Harris Hip score was 89.5. Aseptic necrosis of the femoral head occurred in 9 cases (12.2%). Regular use of tobacco was associated with a higher risk to develop necrosis (p=0.007). The Body Mass Index was significantly higher in cases who had necrosis compared to the rest of our population (p=0.043) and was inversely proportional to the post-operative Harris hip score (p=0.001).
Conclusions:
While considering screw fixation to treat cases with femoral neck fractures, patient’s weight and use of tobacco should be considered as prognostic factors. (www.actabiomedica.it)
Keywords: Femoral Neck Fractures, Cannulated Screws, Avascular Necrosis, BMI, Tobacco
Introduction
Hip fractures represent a serious disease affecting old and younger people in western countries. According to recent epidemiologic studies, the total number of femoral neck fractures will increase in the next decades: from 1.6 million cases counted through the year 2000, it will rise up to 4.5 million in 2050 (1).
In the elderly the traumatic mechanism behind hip fractures usually consists in low-energy trauma since increased risks of osteoporosis and accidental falls are directly related to old age (2). On the other hand, younger people often develop femoral neck fractures after a quite high-energy trauma, even though a reduced bone quality can play a complementary role sometimes (3).
Surgical treatment changes depending on age, peculiarity and comorbidity of patients. However, specific characteristics of fracture represent the primary factors that define surgical strategy. Garden classified medial fractures of the femoral neck in four grades: I and II include non-displaced fractures whereas grade III and IV consist of partially and totally displaced fractures respectively. According to AAOS (American Academy of Orthopaedics Surgeons) evidence-based guideline, stable and non-displaced fractures deserve internal fixation. Instead, hip arthroplasty is defined as the most appropriate treatment for displaced (grade III/IV) fractures (4).
Especially in younger people, surgeons are mandated to pay close attention to preservation of the femoral head, in order to restore functional anatomy as much as possible. This goal is quite simple to achieve when the fracture is not displaced, in fact internal fixation (IF) has obtained global consensus for the treatment of stages I and II. On the other hand, for displaced femoral neck fractures an appropriate reduction with IF is more challenging and there is sufficient agreement between surgeons that hip arthroplasty should be the surgery of choice (5, 6).
Internal fixation of femoral neck fractures with cannulated screws is a minimally invasive procedure that allows the respect of patients’ anatomy, the preservation of native hips and an early rehabilitation (Figure 1). When it is well performed, patients can avoid hip replacement and all its major complications such as infections, dislocations and revision surgery.
Figure 1.
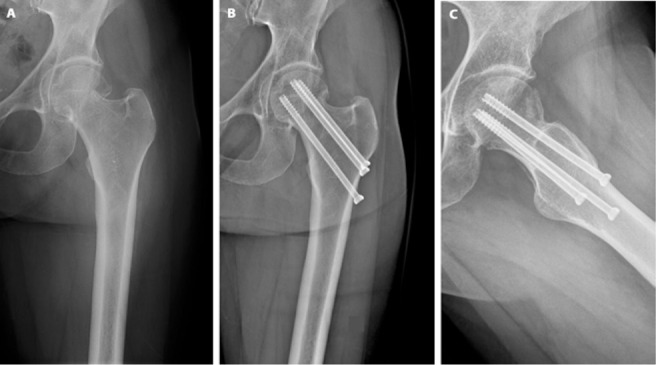
A transcervical fracture of the femoral neck (A) treated with closed reduction and fixation using three cannulated screws, anteroposterior (B) and inguinal view (C).
Nevertheless, many factors can condition mid-term and long-term results of this procedure, first of all the particular vascularization of femoral head which is a terminal type one: if vascular supply is disrupted during trauma, avascular femoral necrosis (AVN) will have more chance to develop (7). Fractures involving the femoral neck also have different biomechanical patterns: the inclination of the fracture line defines balance between compression forces and shear stress at the fracture site itself, according to the Pauwels classification. This factor can influence the process of fracture healing.
All these fracture-related elements, combined with patient-related factors, contribute to success or failure of the internal fixation and to determinate the onset of its possible complications like avascular necrosis with femoral head collapse, non-union and loosening. If they occur, the outcome inevitably gets poorer and chances of a reintervention increase, with consequent lower quality of patients’ life.
In this study we analyze fracture characteristics, appropriateness of reduction and fixation, comorbidity, complications, and functional outcome for a group of people younger than 70 years, who have undergone internal fixation with three screws for femoral neck fractures. The purpose of the work is to establish if, with an accurate pre-operative evaluation, surgeons can predict success or failure of fixation in order to reduce the eventuality of a complication or a reintervention.
Materials and methods
This single-center retrospective study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. This retrospective study did not require ethical approval since it involved only routine clinical follow-up and radiographic examination. All patients gave their written consent.
Our study consisted of a review of all the patients who were treated with screw fixation due to femoral neck fractures between January 2011 and December 2020.
For each patient we collected data regarding their age at surgery, gender, weight in kilograms and height in centimeters. These two latter were used to calculate each patient’s Body Mass Index (MBI). In order to investigate the effect of potential prognostic factors that could affect bone healing and femoral head vascularization, we evaluated whether cases did a regular use of tobacco (consisting of at least one cigarette per day on average) or corticosteroids before and after surgery. With the same aim, we reported all those cases who were diagnosed with diabetes mellitus at the moment of their hospitalization. X-rays of the affected hip and of the pelvic region as a whole were used not only to make diagnosis of medial fracture of the proximal femur, but also to classify the fracture according to both Garden and Pauwels classifications and assess the pre-operative Garden Index of the contralateral femoral neck.
Time between radiographic diagnosis and surgery, calculated in hours, was recorded for each case.
Surgery was performed placing the patient supine on a fracture table for closed reduction. Reduction was achieved by pulling the affected limb in the direction of its long axis in order to distract the fragments and regain length. Slight internal rotation was added in order to achieve a more correct reduction of the fracture and better expose the trochanteric region during the intervention. Once these maneuvers were carried out, antero-posterior and lateral view X-ray images were acquired to confirm a proper reduction had been achieved. Using a percutaneous approach to the trochanteric region, 3 parallel wires in an inverted triangle configuration were introduced from the lateral subtrochanteric surface towards the apex of the femoral head. Finally, bone was drilled using the wires as a guide and screws were introduced over these latter. The whole procedure is performed under fluoroscopic guidance and both antero-posterior and lateral view X-ray images were acquired at the end of the surgical intervention. Post-operative X-rays were used to calculate the Garden index of the treated femur but also the angle between the screws’ main axis and the one of the femoral shaft. Gradual and progressive weight bearing was allowed since the first days after the intervention; total weight bearing was attained within one month.
In the month that came after surgery, follow-up consisted of serial office visits, clinical evaluations and X-ray images. Particular attention was given to the onset of symptoms or radiological signs that could be attributable to the outbreak of avascular necrosis of the femoral head . Cases who developed necrosis were recorded and the time between surgery and diagnosis was calculated. The same approach was applied for mechanical issues or any major complication that could be attributable to the implant of the three cannulated screws.
Functional outcomes were assessed using the Harris Hip Score. For those who did not suffer from necrosis, we recorded each patient’s score at their latest clinical evaluation. For those cases who had necrosis and therefore underwent further surgery with total hip replacement, the attributed score was the one they had in their last office visit before THA.
Statistics
Statistical analysis was performed using Stata SE 13 (StataCorp LLC, College Station, TX). Statistical significance was set at 0.05 for all endpoints.
The Fisher exact test was used in order to evaluate whether cases who used to make regular use of tobacco before the fracture had a significantly higher tendency to develop avascular necrosis of the femoral head after surgery. The same test was used to assess if grade 3 fractures according to the Garden classification or type 3 fractures according to the Pauwels classification had a significantly higher risk of post-operative AVN. We also subdivided our population in two groups: those who developed AVN and those who did not. T-student tests were performed comparing groups’ BMI, surgical delay and differential Garden Index before and after surgery, trying to understand if these three variables differed from one group to the other.
Pearson correlation tests were used to evaluate if there was a linear correlation between post-operative functional outcome, assessed with the Harris Hip Score, and pre-operative factors such as patients’ BMI or surgical delay.
Results
74 patients who suffered from femoral neck fracture were treated with screw fixation between January 2011 and December 2020. They were 35 males and 39 females, with a mean age at surgery of 55.7 (22-70) years. Mean height and weight in our population were 171cm (154-192) and 68kg (44-94) respectively, while the average BMI was 23.1 (18-33). 19 cases (26%) were smokers, whereas the remaining 55 (74%) were not habitual smokers. 4 patients (5%) were affected by type II diabetes mellitus, while 8 patients (11%) were under corticosteroid treatment when fracture occurred.
Femoral neck fractures were classified according to the Pauwels classification as follows: 16 (22%) type 1, 42 (56%) type 2 and 16 (22%) type 3 fractures. According to the Garden classification, fractures were grade 1 in 23 cases, grade 2 in 37 and grade 3 in the remaining 14. All those cases who had a grade 3 fracture at the moment of their hospitalization were successfully reduced intra-operatively, reaching a grade 2 conformation. The mean Garden index of the contralateral proximal femur was 168.9 (126-188).
On average, surgery was performed 29.7 (2-96) hours after the diagnosis of fracture. Screws were placed with a mean angle of 134.2 (122-152) degrees with the main axis of the femoral shaft. After surgery, the mean Garden index of the treated femur was 168.1 (148-180) degrees. The mean variation between pre-operative and post-operative Garden index was 5 (0-26) degrees. The mean follow-up was 58.3 (13-134) months.
Only 1 case (1.3%) showed radiographic signs of aseptic loosening and, since the fracture had already reached complete healing, a prompt removal of the three screws could be carried out without further complications or negative effects on the patient’s functional results. The rest of our patients did not show any other major mechanical complication attributable to the implant of the three cannulated screws. One other case was found with a non-union of the bone segments despite the implant of the screws.
Through their post-operative intercourse, 9 of our 74 patients (12%) developed avascular necrosis of the femoral head. Time from surgery to the diagnosis of necrosis ranged from 3 to 50 months. The necrosis-free survival in our population was 91.9% after 1 year, 90.5% after 2 years and 87.8% after 5 years (Fig. 2). At the moment of diagnosis, necrosis implied hip pain and a remarked functional impairment, with a mean Harris Hip Score of 62.7 (40-92). For those who did not develop avascular necrosis, the mean Harris Hip score was 93.3 (62-100). The mean post-operative Harris Hip Score in our whole population was 89.5 (40-100).
Figure 2.
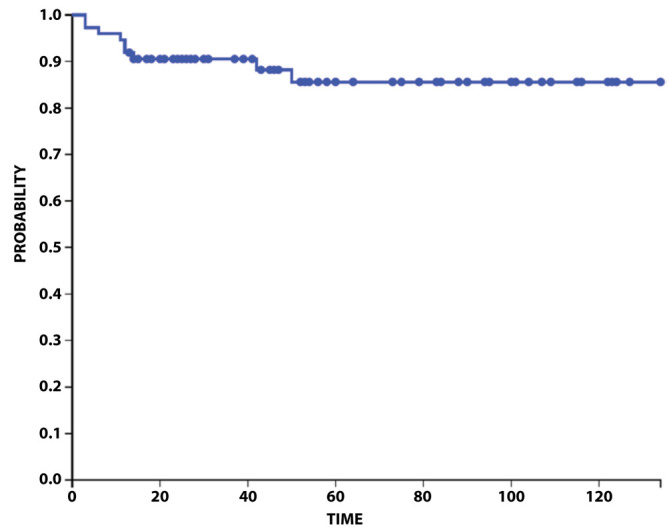
Kaplan-Meier curve that describes the necrosis-free survival in our whole population.
Cases who made regular use of tobacco were exposed to a significantly higher risk of post-operative avascular necrosis of the femoral head (p=0.007). Furthermore, cases who developed necrosis had a significantly higher Body Mass Index compared to the rest of our population (p=0.043). The BMI also had a significant direct correlation with the post-operative Harris Hip Score: on average, the higher the index is, the lower the post-operative functional score came to be (p=0.001). In light of these results, in our population BMI played a prognostic role both in terms of avascular necrosis and post-operative functional results.
We could also verify that cases who suffered from necrosis had significantly longer surgical delay (expressed as the time gap between radiographic diagnosis of fracture and surgical intervention) compared to those who did not develop such a complication (p=0.043). Moreover, we could unveil an inverse correlation between surgical delay and post-operative Harris Hip Score (p=0.048). Early intervention therefore seems to play a positive prognostic role, reducing the risk of necrosis and maximizing the post-operative functional outcome.
Our results also suggest that the grade of intra-operative reduction may represent another prognostic factor. In fact, those who developed AVN had a significantly higher differential between their pre-operative and post-operative Garden indexes compared to those who did not develop necrosis (p=0.019).
Screw angle did not vary significantly between those who did and did not develop AVN after our intervention (p=0.181).
Radiographic presentation of fractures and anamnestic factors for cases who had and had not avascular necrosis of their femoral head are summarized in Table 1.
Table 1.
Our cases, divided on the basis of post-operative diagnosis of Avascular Necrosis (AVN), with their radiographic presentation and anamnestic characteristics.
| Cases who developed AVN | Cases who did not develop AVN | |
|---|---|---|
| Number | 9 | 65 |
| Garden Class. | ||
| Grade 1 | 3 (33%) | 20 (31%) |
| Grade 2 | 3 (33%) | 34 (52%) |
| Grade 3 | 3 (33%) | 11 (17%) |
| Pauwels Class. | ||
| Type 1 | 2 (22%) | 14 (22%) |
| Type 2 | 4 (44%) | 38 (58%) |
| Type 3 | 3 (33%) | 13 (20%) |
| Garden Index Differential | 9.7 (4-14) | 5.0 (0-26) |
| Mean Screw Angle | 133.8 (122-152) | 136.9 (128-148) |
| Smokers | 6 (67%) | 13 (20%) |
| Diabetes | 1 (11%) | 3 (5%) |
| Steroid Ther. | 2 (22%) | 6 (9%) |
| MEAN BMI | 24.3 | 22.8 |
| Surgical Delay | 33.7 | 29.0 |
In our population, the difference between pre-operative and post-operative Garden Index was significantly higher in those cases who later developed necrosis of their femoral head (p=0.019).
Still correlating pre-operative X-rays and clinical outcomes, necrosis rate was higher for patients who had grade 3 fractures according to the Garden classification. In fact, necrosis was developed by 27.2% of this subpopulation, whereas its prevalence in the rest of our cases was only 10%. However, although this difference may suggest an increased risk of necrosis for grade 3 fractures, the size of our population did not furnish enough statistical significance to firmly prove this association. Similarly, in our cases Pauwels type 3 fractures had a higher risk to develop avascular necrosis of the femoral head (23%) compared to the other types of fracture (10.3%), even though it was not possible to demonstrate statistical significance for our endpoints (Fig. 3).
Figure 3.
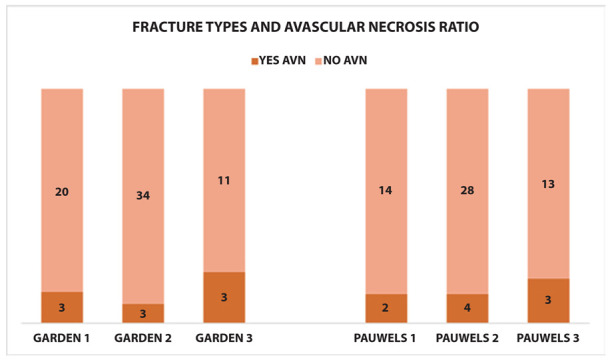
Graphic distribution of avascular necrosis (AVN) sorted for fracture type according to both Garden and Pauwels classification.
Discussion
Internal fixation of femoral neck fracture with three screws is a minimally invasive surgical procedure: following an external reduction operation, three cannulated screws are inserted with a percutaneous technique. Risks connected to surgery are reduced as compared to hip arthroplasty, since bleeding is minimalized, and the procedure is shorter. The main advantage of internal fixation is the possibility to preserve the femoral head and avoid arthroplasty with its possible complications, maintaining the native hip and therefore, especially for young people, supporting high functional requests.
However, the outcome of patients treated with internal fixation with cannulated screws is not always positive. This surgical option can present some complications such as avascular necrosis of the femoral head, non-union at the fracture site and screw loosening. When they occur, patients usually complain of hip pain and difficulty to carry out their everyday activities; in these circumstances, a reintervention is usually needed.
We selected different factors that, in our opinion, could influence the future outcome of internal fixation with three cannulated screws (CS). Success or failure could be a result of - among the others - fracture-related factors like the degree of displacement expressed by Garden’s classification, and the orientation of the fracture line according to Pauwels. We also analyzed the possible association between complications of IF with CS and patient-related factors such as diabetes, obesity, addiction to smoking alongside surgery-related elements like the timing between diagnosis of fracture and surgical treatment, and the restoration of Garden Index.
The AAOS evidence-based guideline express a dichotomy of treatment of femoral neck fracture in the elderly based on the displacement of femoral head, proposing internal fixation for non-displaced fracture exclusively (Stage I-II of Garden classification), and hemiarthroplasty (HA) or total hip arthroplasty (THA) for displaced fracture (Stage III-IV) (4). However, at the moment literature is not clear about surgical management of displaced fractures in younger people and there is no global consensus on preferring HA or THA for stage III and IV. Tseng et al. in their meta-analysis found that there isn’t any difference in mortality between osteosynthesis and arthroplasty for displaced fractures but osteosynthesis has a higher revision rate (8). Heetveld at al.’s review confirms that revision is less likely to be necessary with primary arthroplasty, but internal fixation seems to be associated with lower morbidity and lower early mortality rates compared to HA or THA. Failure and revision rate of osteosynthesis is about 40% at 80 years or more, but there is no sufficient evidence about preferring one treatment or the other in younger people. Although the same authors affirm that internal fixation should be avoided in patients with osteoarthritis or rheumatoid arthritis, it is unquestionable that this approach, if performed with an acceptable reduction, leads to a number of advantages also for displaced neck fractures in those patients that can tolerate the risk and the possibility of a revision (9).
In our analysis we found a higher rate of avascular necrosis and revision surgery in patients with displaced femoral neck fractures. In fact, this complication was developed by 21,4% of cases with grade III of Garden fractures, whereas only 10% of non-displaced fractures progressed in necrosis. However, the assertion was not statistically significant due to the small size of the population of our study.
Pauwels classification analyzes the angle between fracture line and the horizontal line identifying three grades in which the distribution of compression forces and shear stress changes. The vertical orientation of fracture line (grade III) was frequently correlated to the probability of developing non-union because of the prevalence of shear forces at the fracture site that can lead to displacement and varus collapse. In 1998, Parker and Dynan’s study didn’t find any difference in union rate between vertical and transverse fractures surgically treated with a good reduction and a stable synthesis [10]. Liporace et al. in 2008 reiterate the importance to obtain an excellent reduction avoiding varus displacement and the relevance of proper placement of the screws. In their case series of 76 patients with Pauwels III fracture treated with internal fixation they found a non-union rate with implant failure that ranged from 9 to 18%, despite the good quality of reduction and fixation and the prevalence of young people in the cohort. Therefore, in contrast to Parker and Dynan, they underlined that Pauwels III fractures can be challenging because the prevalence of shear forces can condition final results of treatment (11).
In a review of literature about Pauwels classification in 2016, the authors admitted that, for displaced vertical fractures, the risk of non-union and necrosis increases. Authors focused on the still unsolved but important problem of investigating an ideal construct of fixation in order to maintain an appropriate reduction when shear forces act to displace the fracture (12).
In our analysis we didn’t find any case of non-union in Pauwels III fractures, so deducting that good reduction and stable fixation have been achieved. Like displaced fractures (Garden III), also vertical fractures developed avascular necrosis with double incidence if compared with horizontal fractures (20% to 10%). But, also for this parameter, our population was too small to deduce a significant statistical value from this data.
Vascularization of the femoral head originates from lateral and medial circumflex arteries, with a minority contribution by the obturator artery through the round ligament. In case of a femoral neck fracture, a partial or total disruption of terminal intracapsular vessels can occur, predisposing to avascular necrosis of the femoral head that remains ischemic until reduction is achieved. The grade of urgency with which internal fixation of femoral head fractures has to be performed is still controversial in literature. The ideal timing between fracture diagnosis and surgery has not been defined yet. Some authors sustain the importance of early treatment, within 6 to 24 hours, which has the objective of an early restoration of blood flow to the femoral head reducing the future risk of avascular necrosis (13). This assertion has been denied by other different studies that didn’t find any difference in necrosis rate between patients treated with early reduction and patients undergone delayed treatment (11, 14, 15).
In a recent review and meta-analysis, the authors evaluated non-union rate and avascular necrosis rate in patients sorted in three groups based on a specific timing of intervention (within 6, 12 and 24 hours from diagnosis), thereby comparing early and delayed treatment. The incidence of complications was the same for both early and delayed surgical intervention, corroborating the idea that no statistically significant correlation exists between surgical timing and the future onset of femoral head necrosis (16). In our analysis, although no chi-square test could indicate a proper end-point for surgical timing, a t-student test testified that cases who later developed avascular necrosis had a significantly higher mean diagnostic delay compared to the rest of our population.
Appropriateness of intraoperative reduction and fixation of femoral neck fractures can be evaluated calculating the Garden alignment index, or rather the angle of the compression trabeculae related to the longitudinal axis of the femoral shaft. If the angle is between 155° and 180°, anatomical reduction has been achieved; otherwise, if the measurement falls outside of this range the risk of avascular necrosis increases (17). For each patient we assessed the value of Garden Index before fracture from the contralateral femur and post-reduction (18). Through a t-student test we observed that the mean differential between pre-operative and post-operative Garden Indexes was significantly higher in those patients that developed AVN: the more final reduction is close to the anatomical structure of native hip, the less future complications are probable. This assessment corroborates the thesis that a more anatomical reduction decreases risk of AVN therefore surgeons must always attempt to obtain it.
For each patient of our cohort we investigated comorbidities, in particular obesity and diabetes, and whether they made or not regular use of tobacco. We found that almost all the patients which developed avascular necrosis presented at least one of the above-mentioned associated factors, regardless of Garden and Pauwels grade. Particularly, the regular use of tobacco in our patients seems to be strictly related to the onset of post-operative osteonecrosis, also in non-displaced fractures and in absence of other comorbidities.
According to the data of our population, a high Body Mass Index also seems to have a correlation with avascular necrosis especially if summed up with grade 3 of Pauwels or Garden. Obesity was also associated with poorer Harris Hip Score in follow-up.
In our opinion, recent literature lacks a large number of studies verifying the connection between smoke, obesity and diabetes with failure and complications of internal fixation of femoral head fractures. However, studies have been carried out in order to analyze association of tobacco with avascular necrosis and delay in fractures healing in general. Chassanidis et al. underlined the role of tobacco in the expression of BMP-2 and BMP-6, involved in promotion of terminal differentiation in osteoblasts. In smokers’ periosteal cells, the genic expression of BPM decreases; consequently, they have an increased risk of delayed healing and non-union of fractures (19). Furthermore, the negative influence of smoking on bone healing has been confirmed in a wide review of literature conducted in 2021 (20).
In our records we found the only case of non-union in a smoker patient with a grade II of Pauwels hip fracture and no other risk factors associated.
Wen et al. in 2017 published a meta-analysis in which they showed that current smokers and former smokers have a greater risk to develop avascular necrosis of femoral head than non-smokers (21). In an animal study Chang et al. demonstrated that inhalation of smoke interferes with expression of VEGF and angiogenesis in the early phases of bone healing, leading to delayed fractures union (22). The arrest of angiogenesis in patients with hip fracture could act on a disadvantaged substratum because of the probable disruption of blood supply to the femoral head. Therefore, the action of tobacco intensifies the vascular damage and impedes the attempts of flow restoration and fracture healing, leading to increased probability of avascular necrosis and non-union, as confirmed by our records.
The link between obesity and bone metabolism, for its part, has been widely studied. In obese people serum level of vitamin D are lower than in normal weight people. If 25(OH)D decreases, serum level of PTH increases, leading to a negative result on cortical bone mineralization. Obesity also plays a role in type-II-diabetes-related bone disease, along with insulin resistance and hyperinsulinemia which can have adverse effects on femoral neck strength (23). High body weight increases shear stresses at the fracture line; especially in case of vertical lines (Pauwels III), the displacement forces of overweight cases are considerable and complications like nonunion and avascular necrosis are therefore more probable (24).
In conclusion, we are aware that in everyday practice surgeons use to consider Garden and Pauwels classification as the more significant parameters to evaluate for choosing the best treatment in younger people. Alongside these fundamental considerations, the quality of reduction and fixation must not be underestimated. In parallel, during the decisional process, surgeons should also take into consideration patients-related factors like weight and in particular the use of tobacco which - as our study shows - can play an important role in determining fracture healing, the incidence of complications and patients’ functional outcome.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018 Aug;49(8):1458–1460. doi: 10.1016/j.injury.2018.04.015. doi: 10.1016/j.injury.2018.04.015. Epub 2018 Apr 20. PMID: 29699731. [DOI] [PubMed] [Google Scholar]
- Rapp K, Büchele G, Dreinhöfer K, Bücking B, Becker C, Benzinger P. Epidemiology of hip fractures: Systematic literature review of German data and an overview of the international literature. Z Gerontol Geriatr. 2019 Feb;52(1):10–16. doi: 10.1007/s00391-018-1382-z. doi: 10.1007/s00391-018-1382-z. Epub 2018 Mar 28. PMID: 29594444; PMCID: PMC6353815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia Y, Zhang W, Zhang Z, Wang J, Yan L. Treatment of femoral neck fractures: sliding hip screw or cannulated screws? A meta-analysis. J Orthop Surg Res. 2021 Jan 14;16(1):54. doi: 10.1186/s13018-020-02189-1. DOI:10.1186/s13018-020-02189-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brox WT, Roberts KC, Taksali S, et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on Management of Hip Fractures in the Elderly. J Bone Joint Surg Am. 2015 Jul 15;97(14):1196–9. doi: 10.2106/JBJS.O.00229. doi: 10.2106/JBJS.O.00229. PMID: 26178894; PMCID: PMC6948785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zielinski SM, Meeuwis MA, Heetveld MJ, et al. Dutch femoral neck fracture investigator group. Adherence to a femoral neck fracture treatment guideline. Int Orthop. 2013 Jul;37(7):1327–34. doi: 10.1007/s00264-013-1888-3. doi: 10.1007/s00264-013-1888-3. Epub 2013 Apr 18. PMID: 23595233; PMCID: PMC3685653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samsami S, Saberi S, Sadighi S, Rouhi G. Comparison of Three Fixation Methods for Femoral Neck Fracture in Young Adults: Experimental and Numerical Investigations. J Med Biol Eng. 2015;35(5):566–579. doi: 10.1007/s40846-015-0085-9. doi: 10.1007/s40846-015-0085-9. Epub 2015 Oct 1. PMID: 26500470; PMCID: PMC4609309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EO, Soultanis K, Soucacos PN. Vascular anatomy and microcirculation of skeletal zones vulnerable to osteonecrosis: vascularization of the femoral head. Orthop Clin North Am. 2004 Jul;35(3):285–91, viii. doi: 10.1016/j.ocl.2004.03.002. doi: 10.1016/j.ocl.2004.03.002. PMID: 15271536. [DOI] [PubMed] [Google Scholar]
- Tseng FJ, Chia WT, Pan RY, et al. Comparison of arthroplasty vs. osteosynthesis for displaced femoral neck fractures: a meta-analysis. J Orthop Surg Res. 2017 Sep 15;12(1):131. doi: 10.1186/s13018-017-0629-5. doi: 10.1186/s13018-017-0629-5. PMID: 28915928; PMCID: PMC5602948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heetveld MJ, Rogmark C, Frihagen F, Keating J. Internal fixation versus arthroplasty for displaced femoral neck fractures: what is the evidence? J Orthop Trauma. 2009 Jul;23(6):395–402. doi: 10.1097/BOT.0b013e318176147d. doi: 10.1097/BOT.0b013e318176147d. PMID: 19550224. [DOI] [PubMed] [Google Scholar]
- Parker MJ, Dynan Y. Is Pauwels classification still valid? Injury. 1998 Sep;29(7):521–3. doi: 10.1016/s0020-1383(98)00118-1. doi: 10.1016/s0020-1383(98)00118-1. PMID: 10193494. [DOI] [PubMed] [Google Scholar]
- Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008 Aug;90(8):1654–9. doi: 10.2106/JBJS.G.01353. doi: 10.2106/JBJS.G.01353. PMID: 18676894. [DOI] [PubMed] [Google Scholar]
- Shen M, Wang C, Chen H, Rui YF, Zhao S. An update on the Pauwels classification. J Orthop Surg Res. 2016 Dec 12;11(1):161. doi: 10.1186/s13018-016-0498-3. doi: 10.1186/s13018-016-0498-3. PMID: 27955672; PMCID: PMC5154085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Li B, Zhang Z, Yu X, Li Q, Liu L. Early versus delayed hip reduction in the surgical treatment of femoral head fracture combined with posterior hip dislocation: a comparative study. BMC Musculoskelet Disord. 2021 Dec 20;22(1):1057. doi: 10.1186/s12891-021-04968-1. doi: 10.1186/s12891-021-04968-1. PMID: 34930251; PMCID: PMC8690980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duckworth AD, Bennet SJ, Aderinto J, Keating JF. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Joint Surg Br. 2011 Jun;93(6):811–6. doi: 10.1302/0301-620X.93B6.26432. doi: 10.1302/0301-620X.93B6.26432. PMID: 21586782. [DOI] [PubMed] [Google Scholar]
- Longstaff LM, Jain R, Schemitsch EH. Fixation of subcapital hip fractures in patients sixty years of age or less. J Bone Joint Surg Am. 2003 Aug;85(8):1616. doi: 10.2106/00004623-200308000-00039. author reply 1616-7. doi: 10.2106/00004623-200308000-00039. [DOI] [PubMed] [Google Scholar]
- Papakostidis C, Panagiotopoulos A, Piccioli A, Giannoudis PV. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome. Injury. 2015 Mar;46(3):459–66. doi: 10.1016/j.injury.2014.12.025. doi: 10.1016/j.injury.2014.12.025. Epub 2015 Jan 3. PMID: 25616675. [DOI] [PubMed] [Google Scholar]
- Jo S, Lee SH, Lee HJ. The Correlation between the Fracture Types and the Complications after Internal Fixation of the Femoral Neck Fractures. Hip Pelvis. 2016 Mar;28(1):35–42. doi: 10.5371/hp.2016.28.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agar A, Utkan A. The Effect of Anatomical Reduction on Functional Outcomes in Femoral Neck Fracture: A Novel Modified Garden Index. Cureus. 2021 Nov 24;13(11):e19863. doi: 10.7759/cureus.19863. doi: 10.7759/cureus.19863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassanidis CG, Malizos KN, Varitimidis S, et al. Smoking affects mRNA expression of bone morphogenetic proteins in human periosteum. J Bone Joint Surg Br. 2012 Oct;94(10):1427–32. doi: 10.1302/0301-620X.94B10.28405. doi: 10.1302/0301-620X. 94B10.28405. PMID: 23015573. [DOI] [PubMed] [Google Scholar]
- Xu B, Anderson DB, Park ES, Chen L, Lee JH. The influence of smoking and alcohol on bone healing: Systematic review and meta-analysis of non-pathological fractures. EClinicalMedicine. 2021 Oct 31;42:101179. doi: 10.1016/j.eclinm.2021.101179. doi: 10.1016/j.eclinm.2021.101179. PMID: 34765953; PMCID: PMC-8571530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z, Lin Z, Yan W, Zhang J. Influence of cigarette smoking on osteonecrosis of the femoral head (ONFH): a systematic review and meta-analysis. Hip Int. 2017 Sep 19;27(5):425–435. doi: 10.5301/hipint.5000516. doi: 10.5301/hipint.5000516. Epub 2017 May 29. PMID: 28574127. [DOI] [PubMed] [Google Scholar]
- Chang CJ, Jou IM, Wu TT, Su FC, Tai TW. Cigarette smoke inhalation impairs angiogenesis in early bone healing processes and delays fracture union. Bone Joint Res. 2020 May 16;9(3):99–107. doi: 10.1302/2046-3758.93.BJR-2019-0089.R1. doi: 10.1302/2046-3758.93.BJR-2019-0089.R1. PMID: 32435462; PMCID: PMC7229299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou J, He C, He W, Yang M, Luo X, Li C. Obesity and Bone Health: A Complex Link. Front Cell Dev Biol. 2020;8:600181. doi: 10.3389/fcell.2020.600181. Published 2020 Dec 21. doi:10.3389/fcell.2020.600181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L, Jang K, Moon YJ, Wagle S, Kim KM, Lee KB. Leptin ameliorates ischemic necrosis of the femoral head in rats with obesity induced by a high-fat diet. Sci Rep. 2015;5:9397. doi: 10.1038/srep09397. DOI: https://doi.org/10.1038/srep09397. [DOI] [PMC free article] [PubMed] [Google Scholar]


