Highlights
-
•
Cognitive and affective responses differentiated vaccine-hesitant from vaccine-inclined.
-
•
Five subgroups of vaccine-hesitant individuals were identified with latent profile analysis.
-
•
Each subgroup has a unique profile feature that requires distinct messaging strategy.
-
•
Group membership was predicted by gender, political orientation, and purity and fairness beliefs.
Keywords: COVID-19, Vaccine hesitancy, Audience segmentation, Audience targeting
Abstract
COVID-19 has caused tremendous consequences in the U.S., and combating the pandemic requires a significant number of Americans to receive COVID-19 vaccines. Guided by prominent health communication theories, this project took a formative evaluation approach and employed a national sample (N = 1041) in the U.S. to explore the potential differences between vaccine-inclined vs. -hesitant individuals and to generate profiles of hesitant individuals as the foundation for audience segmentation and message targeting. Five distinct profiles emerged in the sample. Characteristics of each profile were described, and appropriate messaging strategies were identified to target each group. Theoretical and practical implications were discussed.
Winning the battle against COVID-19 in the U.S. requires a significant number of Americans to vaccinate themselves against COVID-19. A poll in July 2021 showed that three in ten American adults remain unvaccinated, with a significant portion of them indicating that they want to “wait and see” [27]. Urgent research attention is needed to focus on possible interventions to address vaccine hesitancy so that herd immunity can be achieved. Health messaging is an important means to build vaccine confidence. To date, vaccine-promoting messages have mainly focused on their effectiveness and safety, primarily highlighting gains and losses (e.g., [25], [26]). However, given how individuals’ vaccine hesitancy could arise due to a variety of reasons, such messages often fail to address their specific concerns. Indeed, the U.S. Centers for Disease Control and Prevention [11] and others (e.g., [43]) have observed that pro-vaccine communications are often ineffective and may backfire and called for more nuanced and tailored messaging to address vaccine hesitancy. Moreover, the one-strategy-fits-all approach means that individuals with heterogeneous characteristics are benefiting from pro-vaccine messaging disproportionally, which may further exacerbate health disparity (e.g., [31]).
Designing and implementing tailored health campaigns requires both a thorough understanding of the nature of the problem to be solved and how the target audience approaches the problem and the proposed solution. However, health experts often lack the perspective of the target audience, given that they differ substantially in topic knowledge, perceptions, values, and level and type of involvement. Formative evaluation research can potentially close the gap and provide insights into guiding the development of effective campaign messages [4]. A key purpose of formative evaluation research is to utilize information about how the target audience approaches the problem and how they might react to persuasive messages to identify substantial subgroups. This allows the development of suitable message appeals and presentation styles and the selection of appropriate communication channels and sources for each subgroup [4]. This project thus utilizes the formative evaluation approach to understand what psychological factors vaccine-inclined and -hesitant individuals differ on and to use the psychological features of vaccine-hesitant individuals to identify potential segments in such a way that the between-segments differences would be maximized and within-segments differences minimized, which serves as the basis for efficient message targeting.
Informed by the literature on vaccine hesitancy and leading theories of intention and behavioral formation and change [7], [20], [35], [44], potential predictors of COVID-19 vaccination intention were identified and tested. The significant predictors (i.e., what separated the vaccine-hesitant from the vaccine-inclined) were then used as input data in latent profile analysis (LPA) for audience segmentation. To facilitate easier targeting, demographic, political, and sociocultural background variables were analyzed as potential proxies that predict the audience segments. Message strategies were discussed for each segment based on their distinct characteristics.
Vaccine hesitancy
Vaccination has been one of the most successful public health measures, but it has also been perceived to be unsafe and unnecessary by a growing number of people. Individuals’ attitudes toward vaccination could be mapped on a continuum ranging from active demand for vaccines to complete refusal of all vaccines [18]. Vaccine-hesitant individuals are in the middle of the continuum [18], [37]. These individuals may choose to accept some vaccines while rejecting others; they may delay vaccines or accept them based on the recommended schedule but still have serious doubts in doing so [18], [19]. A new systematic literature review [10] suggested defining vaccine hesitancy as a state of indecisiveness regarding a vaccination decision. In other words, vaccine-hesitant people constitute a highly heterogeneous group, within which hesitancy levels can vary substantially across individuals [30]. As long as an individual is not completely sure about their vaccination decision, they still experience some level of indecisiveness, which indicates vaccine hesitancy. For the purpose of this exploratory study, we thus consider any individual who is less than 100% decided to receive COVID-19 vaccines at the measurement moment hesitant; those who are 100% committed to receiving the vaccine are considered inclined. This allows us to identify potential segments that reflect widely varying levels of hesitancy among individuals who are still making up their minds regarding COVID-19 vaccine decisions.
Identifying antecedents of vaccine hesitancy
To explore the potential antecedents that contribute to individuals’ vaccine hesitancy, we consulted a number of leading theories of intention and behavior formation and change that have been widely applied to a variety of health domains for intervention design purposes. Example theories include the reasoned action approach [20], the Integrated Behavior Model [44], the Protection Motivation Theory [35], and the Health Belief Model [7]. These theories suggest a number of psychological variables, such as emotional responses, behavioral beliefs, control beliefs, risk perceptions, and efficacious beliefs, should be taken into consideration to explain vaccination intention, a direct predictor of vaccination behavior. According to these theories, such identified variables are candidates for consideration for the development of messaging strategies aiming to change vaccination intention and, subsequently, behavior. Background factors are assumed to exert their influence on intention through the above-mentioned antecedents. Although vaccine hesitancy should be considered in historic, political, and sociocultural contexts [18], [19], these background factors cannot be modified with communication strategies. Knowledge and skills to perform the behavior, salience of the behavior, environmental constraints, and habit are expected to have a direct impact on behavior or to moderate the intention-behavior relationship rather than having main effects on intention. Therefore, these factors were not included in the LPA.
Affective responses to COVID-19 vaccines
Affective responses to vaccines contribute to vaccine hesitancy and declines in vaccine uptake [13], [18]. The fact that COVID-19 vaccines have gone through an unusually rapid development process sparked many fears over vaccine safety [9], [13]. These fears are further coupled with anger, sadness, and disgust [23], which are likely fueled by controversies and disagreements over vaccines between polarized groups. On the other hand, the prospect of effective and safe vaccines offers at least a glimpse of hope for the end of the pandemic and the return to normalcy, which can elicit other positive emotions such as happiness and calm [29].
Behavioral beliefs and control and efficacy beliefs of COVID-19 and vaccines
Behavioral beliefs that precede COVID-19 vaccine intention are cognitive appraisals of the potential outcomes of receiving a vaccine or not. The factors include the threat of COVID-19 (severity, susceptibility, and overall seriousness), COVID-19 precaution and vaccine response efficacy, and severity and susceptibility of the potential side effects of COVID-19 vaccines. Control beliefs and efficacy beliefs represent another category of constructs that determines behavioral intention, which pertains to individuals’ perceived ability to enact a behavior. This category involves COVID-19 precaution and vaccine self-efficacy.
Proxies of vaccine-hesitant subgroups
To gain insights into audience beliefs and emotions that can inform message design and targeting, determinants of vaccine hesitancy should be identified, vaccine-hesitant individuals be segmented into subgroups, and their distinct characteristics be revealed. From a practical point of view, however, because the audience’s beliefs and emotions are normally unknown to message designers, and their assessments might be costly in terms of time, financial resources, and labor, it can be demanding and less effective to identify the target audience based on their psychological states in practice. To allow practitioners to bypass such burdens and to target receivers without having to measure all the psychological factors, it is important to identify “proxy” variables, which are more easily known and can be collected more cost-effectively and efficiently, that predict audience segments. The demographic variables, including gender and race, are ready candidates for such potential proxies. In addition, political and sociocultural background variables, including political orientation [21] and moral values (e.g., purity and fairness beliefs, [3], [24]), are also likely predictors of audience segments.
In sum, based on the review above, we proposed the following research questions:
RQ1: On what psychological characteristics (i.e., affective responses, behavioral beliefs, and control and efficacy beliefs) are vaccine-inclined and -hesitant individuals significantly different?
RQ2: What subgroups among vaccine-hesitant individuals can be identified based on their psychological characteristics?
RQ3: How, if at all, are demographic, political, and sociocultural background characteristics associated with membership of the subgroups?
Method
Participants and procedure
Participants were sampled from the general U.S. population who do not identify as a healthcare worker or a resident/staff of a long-term care facility (N = 1,041)1. The sample was recruited through a national paid opt-in online panel comprised of individuals who registered with Qualtrics. Data were collected between December 22, 2020, and January 4, 20212. The nature and possible consequences of the study were fully explained at the beginning of the online survey. Consented participants responded to a set of demographic questions, followed by a battery of questions assessing their cognitive and affective responses to COVID-19 and (potential) COVID-19 vaccines. Toward the end of the questionnaire, participants responded to several scales measuring individual differences and reported their intention to vaccinate against COVID-19. Table 1 presents the demographic information of the sample.
Table 1.
Sample characteristics.
| n | % | |
|---|---|---|
| Sex | ||
| Female | 514 | 49.38 |
| Male | 510 | 48.99 |
| Non-binary | 17 | 1.63 |
| Race/Ethnicity | ||
| White | 688 | 66.09 |
| Black or African American | 125 | 12.01 |
| Hispanic/Latino | 126 | 12.10 |
| Asian or Pacific Islander | 75 | 7.20 |
| American Indian or Alaska Native | 6 | 0.58 |
| Other/Prefer not to answer | 21 | 2.02 |
| Household Income | ||
| Less than $25,000 | 230 | 22.12 |
| $25,000-$49,999 | 273 | 26.25 |
| $50,000-$99,999 | 329 | 31.63 |
| $100,000-$149,999 | 124 | 11.92 |
| $150,000 and above | 84 | 8.08 |
| Education | ||
| Less than high school | 25 | 2.40 |
| High school diploma or equivalent | 230 | 22.09 |
| Some college, no degree | 228 | 21.90 |
| Associate’s degree | 124 | 11.91 |
| Bachelor’s degree | 254 | 24.40 |
| Master’s degree | 145 | 13.93 |
| Doctoral or professional degree | 35 | 3.36 |
| M | SD | |
| Age | 45.52 | 16.74 |
Measures
The uni-dimensionality of multi-item scales was established with confirmatory factor analysis (CFA). Descriptives of all variables and their correlations are summarized in Table 2. All items were measured on a 7-point Likert scale ranging from “Strongly disagree” to “Strongly agree” unless stated otherwise.
Table 2.
Means, standard deviations, reliability coefficients, and correlations.
| Variable | M | SD | α | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|---|
| 1. Sadness | 2.57 | 1.76 | 0.81 | |||||
| 2. Fear | 3.20 | 1.96 | 0.89 | 0.65*** | ||||
| 3. Anger | 2.95 | 1.97 | 0.88 | 0.62*** | 0.47*** | |||
| 4. Calm | 3.88 | 1.91 | 0.90 | −0.34*** | −0.40*** | −0.35*** | ||
| 5. Hope | 4.81 | 1.92 | 0.90 | −0.35*** | −0.31*** | −0.44*** | 0.72*** | |
| 6. Happiness | 4.26 | 2.04 | 0.91 | −0.41*** | −0.37*** | −0.45*** | 0.80*** | 0.83*** |
| 7. Disgust | 2.32 | 1.66 | 0.77 | 0.66*** | 0.51*** | 0.75*** | −0.30*** | −0.43*** |
| 8. COVID Severity | 6.17 | 1.35 | 0.90 | −0.07* | 0.07* | −0.23*** | 0.16*** | 0.35*** |
| 9. COVID Self Susceptibility | 5.62 | 1.51 | 0.88 | −0.05 | 0.04 | −0.14*** | 0.07* | 0.25*** |
| 10. COVID Other Susceptibility | 5.91 | 1.33 | 0.85 | −0.01 | 0.04 | −0.09** | 0.11*** | 0.26*** |
| 11. Self-Protection Efficacy | 5.93 | 1.15 | 0.77 | −0.11*** | −0.05 | −0.10** | 0.09** | 0.15*** |
| 12. Other Protection Efficacy | 5.62 | 1.28 | 0.74 | −0.09** | −0.01 | −0.15*** | 0.17*** | 0.21*** |
| 13. COVID Response Efficacy | 5.72 | 1.22 | 0.75 | −0.08** | −0.00 | −0.16*** | 0.18*** | 0.24*** |
| 14. COVID Seriousness | 5.79 | 1.46 | 0.85 | −0.05 | 0.07* | −0.27*** | 0.17*** | 0.36*** |
| 15. Vaccine Susceptibility | 4.51 | 1.53 | 0.89 | 0.29*** | 0.35*** | 0.31*** | −0.36*** | −0.37*** |
| 16. Vaccine Severity | 4.55 | 1.65 | 0.94 | 0.28*** | 0.38*** | 0.35*** | −0.43*** | −0.45*** |
| 17. Vaccine Self-Efficacy | 5.07 | 1.31 | 0.72 | −0.24*** | −0.21*** | −0.26*** | 0.35*** | 0.38*** |
| 18. Vaccine Response Efficacy | 5.02 | 1.66 | 0.95 | −0.28*** | −0.26*** | −0.43*** | 0.50*** | 0.65*** |
| 19. Political Orientation | 4.03 | 1.61 | 0.89 | 0.11*** | 0.06 | 0.20*** | −0.07* | −0.18*** |
| 20. Purity | 3.23 | 1.48 | 0.85 | 0.33*** | 0.29*** | 0.43*** | −0.27*** | −0.43*** |
| 21. Fairness | 4.55 | 1.68 | 0.84 | −0.20*** | −0.16*** | −0.33*** | 0.46*** | 0.57*** |
| 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|
| −0.41*** | ||||||||
| 0.28*** | −0.24*** | |||||||
| 0.18*** | −0.20*** | 0.47*** | ||||||
| 0.22*** | −0.18*** | 0.42*** | 0.69*** | |||||
| 0.11*** | −0.09** | 0.35*** | 0.18*** | 0.22*** | ||||
| 0.20*** | −0.12*** | 0.34*** | 0.16*** | 0.26*** | 0.54*** | |||
| 0.24*** | −0.12*** | 0.43*** | 0.18*** | 0.28*** | 0.54*** | 0.67*** | ||
| 0.31*** | −0.23*** | 0.71*** | 0.35*** | 0.38*** | 0.25*** | 0.32*** | 0.40*** | |
| −0.38*** | 0.32*** | −0.12*** | 0.02 | 0.04 | 0.02 | −0.05 | −0.05 | −0.14*** |
| −0.46*** | 0.37*** | −0.18*** | −0.08* | −0.05 | −0.01 | −0.06 | −0.07* | −0.21*** |
| 0.36*** | −0.28*** | 0.20*** | 0.19*** | 0.18*** | 0.17*** | 0.18*** | 0.17*** | 0.18*** |
| 0.62*** | −0.46*** | 0.40*** | 0.30*** | 0.30*** | 0.18*** | 0.25*** | 0.27*** | 0.41*** |
| −0.16*** | 0.19*** | −0.29*** | −0.15*** | −0.15*** | −0.06* | −0.09** | −0.16*** | −0.30*** |
| −0.37*** | 0.46*** | −0.29*** | −0.22*** | −0.21*** | −0.12*** | −0.12*** | −0.14*** | −0.31*** |
| 0.56*** | −0.30*** | 0.44*** | 0.25*** | 0.25*** | 0.17*** | 0.24*** | 0.30*** | 0.47*** |
| 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|
| 0.79*** | |||||
| −0.23*** | −0.33*** | ||||
| −0.46*** | −0.56*** | 0.42*** | |||
| 0.14*** | 0.20*** | −0.12*** | −0.23*** | ||
| 0.49*** | 0.57*** | −0.38*** | −0.55*** | 0.22*** | |
| −0.43*** | −0.49*** | 0.34*** | 0.69*** | −0.32*** | −0.46*** |
Note. * p <.05, ** p <.01, *** p <.001.
Vaccination hesitancy
Participants indicated their likelihood (in percentage) of getting vaccinated once a COVID-19 vaccine becomes available for the general public on a 0–100 scale (0% = not likely at all, 100% = absolutely). Those who reported a 100% intention were considered vaccine-inclined (n = 291); otherwise vaccine-hesitant (n = 736).
Affective responses to COVID-19 vaccine
This set of variables was assessed by asking participants to indicate the extent to which they had the following feelings about COVID-19 vaccines on a 1–7 scale (1 = none of this feeling, 7 = a lot of this feeling): (1) sad, depressed (Sadness), (2) scared, afraid (Fear), (3) annoyed, irritated (Anger), (4) calm, relaxed (Calm), (5) hopeful, optimistic (Hope), (6) happy, glad (Happiness), and (7) disgusted, grossed out (Disgust).
Perceived COVID-19 severity
This variable was measured with two items, which were “COVID-19 would be harmful to me” and “COVID-19 would be dangerous to me.”.
Perceived susceptibility (of self and cared others) to COVID-19
These were assessed with two sets of Likert-scale items asking about the perceived likelihood of oneself and their cared others contracting COVID-19. The items were “There is a chance that I/someone I cared about could contract COVID-19” and “It’s possible that I/someone I cared about could get COVID-19.”.
Perceived efficacy to protect (self and cared others) from COVID-19
The variables were captured with two sets of Likert-scale items: “I have the ability to protect myself/the people I care about against COVID-19” and “I know what to do to protect myself/the people I care about from COVID-19.”.
Perceived COVID-19 precaution response efficacy
Participants rated on a 1–7 scale the extent to which they agree with the following two statements: “If we take precautions against COVID-19, we will be safe” and “There are steps that anyone can take that will protect us from COVID-19.”.
Perceived COVID-19 seriousness
This variable pertains to one’s perception of the threat posed by COVID-19 on the general community. It was assessed by asking participants to indicate to what extent they perceive COVID-19 is a national problem and a problem in the place where they live (1 = not at all serious, 7 = extremely serious).
Perceived severity of vaccine side effects
Participants responded to three items asking about the extent to which they believe COVID-19 vaccines can have serious side effects (e.g., “The COVID-19 vaccine could have dangerous side effects”) on a 1–7 scale.
Perceived susceptibility to vaccine side effects
Participants were asked to indicate their perceived chance of being affected by the side effects of COVID-19 vaccines with three items. A sample item was “There is a chance that I could be affected by the side effects of COVID-19 vaccines.”.
Perceived Self-efficacy to receive vaccine
This variable was measured with three Likert-scale items. One sample item was “I would have the ability to get the vaccine when it becomes publicly available.”.
Perceived vaccine response efficacy
Participants indicated the extent to which they perceived COVID-19 vaccines are effective with three items, including “I believe the COVID-19 vaccines are effective in preventing COVID-19 or its complications.”.
Political orientation
This variable was measured with two 7-point semantic differential items, including extremely liberal/extremely conservative and left-wing/right-wing.
Purity belief
Purity belief was assessed with four Likert-scale items. Sample items included “Vaccine might contain chemical compounds,” and “Injection of vaccines violates my standards of purity.”.
Fairness belief
Fairness belief was measured with three items, including “It is fair that everyone should get vaccinated” and “Everyone is equally responsible to get vaccinated.”.
Data analysis strategy
All analyses were conducted in R [34]. To address RQ1, general linear models (GLMs) were estimated to identify the psychological variables that differentiate vaccine-inclined and -hesitant individuals and provide insight into variables that should be included in the LPA for generating vaccine-hesitant segments. Participants’ sex, age, race, and income were entered as controlled covariates in all models. Assuming α = 0.05, two-tailed, a sample size of N = 1,041 yields a statistical power of 0.90 to detect an effect size of f = 0.10, which is considered a small effect size. LPA was conducted with the “tidyLPA” package [36] to address RQ2. All affective and cognitive factors on which vaccine-hesitant and -inclined individuals differed significantly were used as indicators. We assessed fit statistics for 1- through 10-profile models using the following indicators: (1) sample-size-adjusted Bayesian information criterion (SABIC), (2) Akaike information criterion (AIC), (3) approximate weight of evidence (AWE), (4) Entropy, and (5) bootstrapped likelihood ratio test (BLRT). For the three information criteria (i.e., SABIC, AIC, and AWE), lower values indicate superior fit [2], [5], [38]. Entropy indicates how well individuals were classified into the latent profiles, with higher values suggesting a better classification of individuals [14]. BLRT provides an indication of the superiority of a k-class model over the k-1-class model where a significant p-value suggests that the k-class model significantly improves the fit in comparison to the k-1-class model [32]. Multiple logistic regression was conducted to address RQ3.
Results
Factors differentiating vaccine-hesitant and -inclined individuals
GLM results showed that controlling for sex, age, race, and income, vaccine-inclined and -hesitant individuals were significantly different from each other on all the 18 emotional and cognitive variables (i.e., behavioral beliefs) at p <.001, with effect sizes (i.e., Cohen’s d) ranging from 0.24 to 1.04. Estimated marginal means and effect sizes are presented in Table 3. Vaccine-hesitant individuals reported experiencing higher levels of negative emotions (sadness, fear, anger, and disgust) about COVID-19 and lower levels of positive emotions (calm, hope, and happiness) about vaccines compared to vaccine-inclined individuals. In comparison to vaccine-inclined individuals, vaccine-hesitant individuals also perceived lower levels of COVID-19 severity, susceptibility, efficacy to protect self and cared others, response efficacy, seriousness, vaccine self-efficacy, vaccine response efficacy, and higher levels of severity and susceptibility of vaccine side effects.
Table 3.
Estimated marginal means.
| Hesitant (n = 736) |
Inclined (n = 291) |
Cohen’s d | |
|---|---|---|---|
| M (SE) | M (SE) | ||
| Sadness | 2.44 (0.41) | 1.67 (0.42) | 0.39 |
| Fear | 2.74 (0.45) | 1.56 (0.45) | 0.55 |
| Anger | 2.85 (0.46) | 1.74 (0.46) | 0.51 |
| Calm | 3.26 (0.43) | 4.48 (0.43) | 0.78 |
| Hope | 3.93 (0.41) | 5.79 (0.41) | 0.94 |
| Happiness | 3.41 (0.44) | 5.41 (0.44) | 0.95 |
| Disgust | 2.28 (0.38) | 1.28 (0.39) | 0.55 |
| COVID severity | 6.00 (0.31) | 6.75 (0.31) | 0.51 |
| COVID susceptibility of self | 5.74 (0.36) | 6.36 (0.36) | 0.37 |
| COVID susceptibility of cared others | 5.96 (0.32) | 6.58 (0.32) | 0.42 |
| Efficacy to protect self from COVID | 6.00 (0.28) | 6.32 (0.28) | 0.24 |
| Efficacy to protect cared others from COVID | 5.66 (0.31) | 6.19 (0.31) | 0.37 |
| COVID response efficacy | 5.78 (0.29) | 6.35 (0.29) | 0.42 |
| COVID seriousness | 5.97 (0.34) | 6.74 (0.34) | 0.48 |
| COVID vaccine side effect susceptibility | 4.65 (0.34) | 3.35 (0.35) | 0.80 |
| COVID vaccine side effect severity | 4.90 (0.35) | 3.27 (0.36) | 0.96 |
| COVID vaccine self-efficacy | 4.45 (0.29) | 5.45 (0.29) | 0.71 |
| COVID vaccine response efficacy | 4.35 (0.35) | 6.10 (0.35) | 1.04 |
Profiles of vaccine-hesitant individuals
To address RQ2, all 18 variables in Table 3 were used as input data for the LPA analyses. Table 4 presents the fit indices of the 10 estimated models. SABIC, AIC, and BLRT all suggested that adding an additional class improved fit compared to the previous model, but the improvement became marginal after the 5- or 6-profile model. AWE, however, increased when a sixth class was added to the 5-profile model, favoring a 5-profile solution. The highest entropy value was achieved by the 4- and 5-profile models. Based on the fit statistics and the considerations of parsimony and interpretability, a 5-profile model was selected as the best-fitting model3.
Table 4.
Fit indices.
| Class | SABIC | AIC | AWE | Entropy | BLRT p-value |
|---|---|---|---|---|---|
| 1 | 49308.13 | 49256.85 | 49766.04 | 1 | NA |
| 2 | 47300.93 | 47222.58 | 48001.83 | 0.87 | 0.01 |
| 3 | 46253.58 | 46148.16 | 47197.17 | 0.89 | 0.01 |
| 4 | 45722.36 | 45589.87 | 46908.65 | 0.90 | 0.01 |
| 5 | 45271.56 | 45112.01 | 46700.58 | 0.90 | 0.01 |
| 6 | 45103.30 | 44916.68 | 46775.09 | 0.88 | 0.01 |
| 7 | 44739.49 | 44525.81 | 46653.99 | 0.89 | 0.01 |
| 8 | 44550.71 | 44309.96 | 46707.93 | 0.89 | 0.01 |
| 9 | 44449.17 | 44181.36 | 46849.15 | 0.88 | 0.01 |
| 10 | 44378.18 | 44083.30 | 47020.89 | 0.88 | 0.01 |
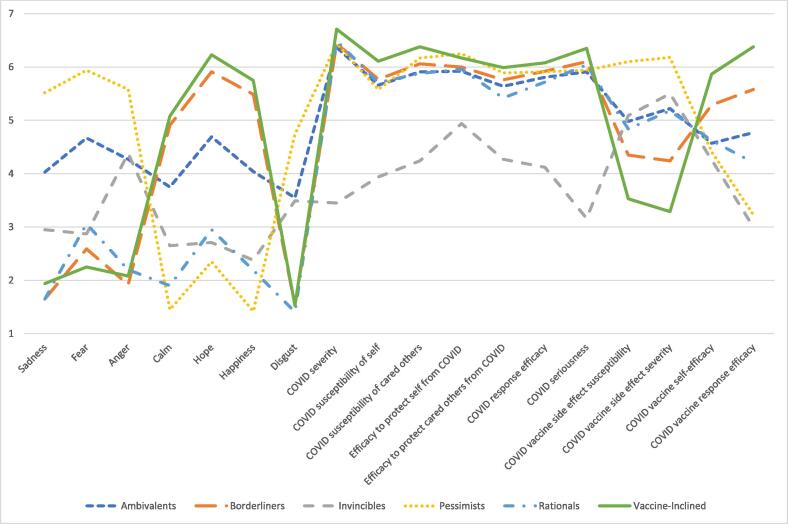
Table 5 summarizes the estimated means on all variables for the five profiles of vaccine-hesitant individuals (see also Fig. 1). Profile 1 included 22.04% of the vaccine-hesitant individuals in the sample (n = 162). Individuals classified into this group reported the highest levels of risk perceptions and efficacious beliefs. They also expressed relatively high levels of negative emotions and positive emotions simultaneously and had medium levels of concern over the side effects of COVID-19 vaccines. This group was labeled “the Ambivalents,” which had an average vaccination intention of 54.32% (SD = 30.07). Profile 2 was the largest group (35.24%) and consisted of n = 259 individuals. This group expressed the highest levels of positive emotions and the lowest levels of negative emotions. Admitting to the relatively high severity and susceptibility of COVID-19, this group had the strongest faith in COVID-19 vaccines and expressed the lowest levels of concern over the side effects of COVID-19 vaccines. We called this group “the Borderliners.” The average vaccination intention of this group was 76.00% (SD = 23.91). Profile 3 contained 15.24% of the sample (n = 112). This group did not perceive COVID-19 to be a severe threat, and at the same time, did not believe in their abilities to protect themselves or their cared ones. Their responses to all 18 variables were generally around the mid-point of the scales. This group was labeled “the Invincibles” and had an average vaccination intention of 17.78% (SD = 25.29). Profile 4 included 11.29% of the sample (n = 83). Although only expressing medium levels of risk perceptions of COVID-19, this group reported the most intense negative emotions and the lowest levels of positive emotions. They were also extremely concerned over the side effects of COVID-19 vaccines and had the lowest levels of efficacy regarding COVID-19 vaccines. We labeled this group “the Pessimists,” which reported a 22.75% vaccination intention on average (SD = 30.03). The last group, Profile 5, comprised 16.19% of the sample (n = 119). This group reported relatively low levels of emotional responses, including both negative and positive emotions; individuals in this group also perceived themselves to be extremely susceptible to COVID-19 but reported a medium level of risk perceptions relative to other groups, including their perceived severity and seriousness of COVID-19, as well as a medium level of efficacy beliefs, such as their perceived self-efficacy to protect themselves and their cared others from COVID-19 and the efficacy of COVID-19 vaccines. We labeled this group “the Rationals.” The average vaccination intention of this group was 41.29% (SD = 31.66).
Table 5.
Estimated means of five vaccine-hesitant profiles.
| Class 1 |
Class 2 |
Class 3 |
Class 4 |
Class 5 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | M | SE | M | SE | |
| Sadness | 4.03 | 0.20 | 1.65 | 0.08 | 2.95 | 0.27 | 5.52 | 0.19 | 1.65 | 0.20 |
| Fear | 4.67 | 0.18 | 2.59 | 0.15 | 2.87 | 0.31 | 5.94 | 0.18 | 3.06 | 0.28 |
| Anger | 4.27 | 0.15 | 1.92 | 0.10 | 4.38 | 0.24 | 5.58 | 0.41 | 2.20 | 0.20 |
| Calm | 3.75 | 0.23 | 4.91 | 0.11 | 2.65 | 0.33 | 1.45 | 0.12 | 1.90 | 0.15 |
| Hope | 4.69 | 0.19 | 5.91 | 0.08 | 2.71 | 0.33 | 2.35 | 0.29 | 2.95 | 0.27 |
| Happiness | 4.04 | 0.22 | 5.49 | 0.11 | 2.38 | 0.33 | 1.42 | 0.14 | 2.19 | 0.20 |
| Disgust | 3.55 | 0.22 | 1.53 | 0.07 | 3.49 | 0.23 | 4.74 | 0.54 | 1.41 | 0.10 |
| COVID severity | 6.37 | 0.26 | 6.44 | 0.07 | 3.45 | 0.29 | 6.44 | 0.12 | 6.49 | 0.12 |
| COVID susceptibility of self | 5.66 | 0.23 | 5.77 | 0.09 | 3.94 | 0.25 | 5.58 | 0.25 | 5.71 | 0.18 |
| COVID susceptibility of cared others | 5.91 | 0.25 | 6.06 | 0.09 | 4.24 | 0.23 | 6.17 | 0.19 | 5.88 | 0.15 |
| Efficacy to protect self from COVID | 5.92 | 0.20 | 6.00 | 0.07 | 4.94 | 0.19 | 6.25 | 0.18 | 5.96 | 0.14 |
| Efficacy to protect cared others from COVID | 5.64 | 0.25 | 5.76 | 0.08 | 4.27 | 0.15 | 5.89 | 0.24 | 5.42 | 0.18 |
| COVID response efficacy | 5.81 | 0.23 | 5.92 | 0.07 | 4.12 | 0.17 | 5.91 | 0.21 | 5.72 | 0.17 |
| COVID seriousness | 5.91 | 0.21 | 6.10 | 0.07 | 3.16 | 0.32 | 5.94 | 0.18 | 6.04 | 0.17 |
| COVID vaccine side effect susceptibility | 4.98 | 0.17 | 4.35 | 0.10 | 5.09 | 0.20 | 6.10 | 0.23 | 4.84 | 0.13 |
| COVID vaccine side effect severity | 5.22 | 0.17 | 4.24 | 0.11 | 5.50 | 0.22 | 6.18 | 0.24 | 5.18 | 0.12 |
| COVID vaccine self-efficacy | 4.57 | 0.10 | 5.29 | 0.08 | 4.26 | 0.11 | 4.41 | 0.19 | 4.62 | 0.14 |
| COVID vaccine response efficacy | 4.77 | 0.15 | 5.58 | 0.08 | 3.00 | 0.26 | 3.23 | 0.40 | 4.21 | 0.18 |
Fig. 1.
Five vaccine-hesitant profiles.
Proxies predicting profile membership
RQ3 concerned the correlates of subgroup membership among the vaccine-hesitant individuals. Results from multiple logistic regression (see Table 6) showed that females were more likely to be rationals (b = 0.42, OR = 1.52) and less likely to be borderliners (b = -0.33, OR = 0.72) compared to males. Different race groups had a similar likelihood of falling into each class. Conservatives were more likely to be Invincibles (b = 0.23, OR = 1.27) and less likely to be Rationales (b = -0.13, OR = 0.87) compared to their liberal counterparts. Moreover, participants who held the belief that vaccines might contain chemical compounds and metals and, therefore, injection of vaccines violate their standards of purity and decency were more likely to be Ambivalents (b = 0.35, OR = 1.42), Pessimists (b = 0.32, OR = 1.38), and Invincibles (b = 0.17, OR = 1.19) and less likely to be Borderliners (b = -0.54, OR = 0.59) or Rationals (b = -0.26, OR = 0.77). In addition, participants who held the belief that it is fair that everyone should get vaccinated were more likely to be Borderliners (b = 0.53, OR = 1.69) and Ambivalents (b = 0.34, OR = 1.40). They were also less likely to be Pessimists (b = -0.36, OR = 0.70), Rationales (b = -0.21, OR = 0.81), and Invincibles (b = -0.70, OR = 0.50).
Table 6.
Multiple logistic regressions predicting profile membership.
| Rationals |
Ambivalents |
Pessimists |
Invincibles |
Borderliners |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | OR | B | OR | B | OR | B | OR | B | OR | |
| Gender (female & non-binary) | 0.42† | 1.52 | 0.09 | 1.10 | 0.40 | 1.49 | −0.41 | 0.66 | −0.33† | 0.72 |
| Race | ||||||||||
| Asian/PI | 0.02 | 1.02 | 0.20 | 1.23 | −1.43 | 0.24 | 0.26 | 1.30 | 0.08 | 1.08 |
| Black/AA | 0.11 | 1.11 | 0.06 | 1.06 | −0.55 | 0.58 | 0.15 | 1.16 | 0.17 | 1.19 |
| Hispanic/Latino | −0.33 | 0.72 | 0.31 | 1.36 | 0.10 | 1.11 | 0.00 | 1.00 | −0.15 | 0.86 |
| Other | 0.60 | 1.83 | −0.34 | 0.71 | 0.32 | 1.38 | 0.22 | 1.25 | −0.60 | 0.55 |
| Political orientation | −0.13* | 0.87 | −0.02 | 0.98 | −0.06 | 0.94 | 0.23** | 1.27 | 0.05 | 1.05 |
| Purity | −0.26** | 0.77 | 0.35*** | 1.42 | 0.32*** | 1.38 | 0.17† | 1.19 | −0.54*** | 0.59 |
| Fairness | −0.21** | 0.81 | 0.34*** | 1.40 | −0.36** | 0.70 | −0.70*** | 0.50 | 0.53*** | 1.69 |
Note. Asian/PI = Asian or Pacific Islander; Black/AA = Black or African American. Regression coefficients are unstandardized. Reference group for gender is male; reference group for race is White. For each regression model, the dependent variable is membership in the column profile versus membership in all other profiles (i.e., membership in column profile = 1, non-membership in column profile = 0). *** p <.001 ** p <.01 * p <.05 † p <.10.
Discussion
Our data revealed a significant portion of vaccine-hesitant individuals. Based on the psychological characteristics that differentiated vaccine-inclined and -hesitant individuals, five subgroups were identified through LPA, with each representing a meaningful, interpretable profile that has implications for message design and targeting. Group membership was predicted by gender, political orientation, and purity and fairness beliefs.
Factors that differentiate vaccine-inclined from vaccine-hesitant
Results showed that vaccine-inclined and -hesitant individuals held drastically different cognitive responses to the pandemic and COVID-19 vaccines. Compared to vaccine-inclined individuals, vaccine-hesitant ones reported lower levels of COVID-19 severity and seriousness, susceptibility of both self and cared ones to COVID-19, efficacy to protect themselves and cared ones from COVID-19, response efficacy, and self-efficacy in getting vaccinated, and higher levels of perceived severity of and susceptibility to the sides effects of COVID-19 vaccines. Research on COVID-19 vaccine hesitancy has consistently identified individuals’ concerns over the safety of vaccines as primary causes for vaccine hesitancy [22], [29]. In addition, consistent with previous findings, the lack of knowledge of the SARS-CoV-2 virus and the vaccines may have contributed to individuals’ perceptions that the virus is mild as well as their low self-efficacy of protecting themselves and others from the virus, which further fueled their hesitancy to receive COVID-19 vaccination [17], [22].
Not surprisingly, such cognitive perceptions were coupled with emotional responses. Our data showed that vaccine-hesitant individuals reported experiencing higher levels of negative emotions as well as lower levels of positive emotions compared to vaccine-inclined individuals. As Chou and Budenz [13] pointed out, the COVID-19 pandemic and the subsequent dramatic societal changes have heightened the public’s emotional responses collectively. Research on individuals’ emotional responses to health crises has consistently revealed that negative emotions individuals experience during health crises could trigger maladaptive coping strategies [16], [28]. Therefore, it is possible that participants who experienced greater negative emotions tended to utilize maladaptive coping strategies to reduce their negative emotions, which might further contribute to unrealistic risk perceptions and ultimately prevent them from taking protective measures to control the danger [13], [28].
Message design strategies
The purpose of the LPA lies in segmenting vaccine-hesitant individuals into heterogeneous subgroups and selecting message design strategies for each subgroup accordingly. The basic message strategy lies in that messages should move vaccine-hesitant individuals’ responses in the direction of the vaccine-inclined group, which in turn moves their vaccine intention toward 100%. In this section, we discuss messaging strategies that can be applied to each subgroup.
First, the profile for the Borderliners is very similar to the descriptive statistics from the vaccine-inclined group in our data. Indeed, this group, on average, reported the highest vaccination intention among the five groups, further supporting the correspondence between the psychological variables and hesitancy level. It is plausible that they had not made up their minds simply because there were no COVID-19 vaccines available for them at the time of data collection. Their intention would likely increase to 100%, and they will drop out of the target audience as soon as vaccines become available.
Second, the differences in behavioral beliefs were not as substantial between the Rationals and the inclined group. The major differences seemed to be the disconnection between the appraisals and emotions: Relatively high levels of risk perceptions were not coupled with stronger negative emotions, neither were efficacy appraisals and positive emotions. It is thus likely that the Rationals are not motivated and undecided due to the lack of an affective push despite the knowledge of the pros and cons (see [15]). As indicated by the relatively low average vaccination intention of this group, such a mismatch between emotions and cognitions can be a powerful driver of hesitancy. Accordingly, messages should appeal to their emotions. The use of audio-visual messages with high sensation value [33], empathy-arousing features [39], interactive web features [42], and immersive virtual environments [1] should also be effective.
Third, Ambivalents’ affective responses were closely associated with cognitive appraisals—they experienced high levels of negative and positive emotions due to risk perceptions and efficacy beliefs, respectively. Their indecision can be attributed to the concern over the potential side effects of COVID-19 vaccines and their belief that vaccines contain chemical compounds and metals; therefore injection of vaccines violates their standards of purity and decency. It might have become more challenging to persuade this group when data on the cases and severity of the side effects from COVID-19 vaccines were disclosed since April 2021 after the vaccines became available for the general public (16 years and older). For this group, the only effective message will probably be more data and scientific evidence on the vaccine purity and side effects and more certainty that alleviates their concerns. On the promising side, among all vaccine-hesitant individuals in our sample, those in this group reported the second highest vaccination intention, suggesting that their concerns – although alarming – are unlikely to completely close the door to consideration of COVID-19 vaccines.
Fourth, almost all the affective responses and cognitive appraisals of the Pessimists were in the opposite direction to the inclined group: high in negative emotions, low in positive emotions and efficacy, and extremely concerned with the side effects. Their negative emotions and hesitancy might be further strengthened by new waves of cases due to COVID variants and breakthrough cases. More effective strategies might lie in appeals to positive emotions such as hope. There is some evidence that hope can be aroused by a positive prospect highlighted by similar success stories (e.g., the success of the Smallpox vaccine [40].
Finally, the Invincibles do not see COVID-19 as a severe threat, consequently, the need to protect themselves or their loved ones, which suggests this group is probably high in unrealistic optimism [8]. Given the cognitive biases such as confirmation bias [45] and egocentrism [41], self-referencing messages (i.e., messages focusing on what might happen to the audience themselves) might result in biased processing and attitude polarization. There has been evidence that other-benefiting strategies might be more efficacious [6]. That is, messages delivered to this group should highlight how vaccination behaviors would benefit others who are innocent and helpless because they cannot receive the vaccine due to medical or religious reasons or there are no vaccines available for them (e.g., children under 5). It is worth noting that to the extent that the Invincibles and the Pessimists had the lowest vaccination intention, these two groups might require greater and more sustained effort to change. Practitioners should set realistic expectations regarding the timeline and effect size of interventions targeting these individuals.
The results of the LPA provided valuable insights for us to segment the audience and design the most effective messaging strategies for each class. However, it would be costly for practitioners to measure all 18 psychological variables in order to segment the target audience. To allow practitioners to target receivers easily, we identified a set of “proxy” variables as a rough estimate of the profiles based on which message targeting can take place. Results showed that 1) male participants who held a strong fairness belief but a weak purity belief were more likely to be Borderliners. 2) Conservatives were more likely to be Invincibles compared to liberals. 3) Pessimists were associated with a strong purity belief and a weak fairness belief. 4) Strong purity belief was consistently associated with Ambivalents. And 5) female and non-binary participants who held weak fairness and purity beliefs tended to be Rationals.
Strengths, limitations, & future research
To our best knowledge, this is the first study that used psychological data for audience analysis and segmentation for COVID-19 vaccine messages. The project employed a national sample of the general population in the U.S. with a large sample size. Despite these strengths, this project suffered from a few limitations. To begin with, vaccine hesitancy is a dynamic status that is subject to change over time. This study utilized a cross-sectional sample, which limited our ability to examine this phenomenon dynamically or observe the potential changes over time. Future research could benefit from obtaining longitudinal data to further examine this question. Relatedly, this project only collected data before COVID-19 vaccines became available to the general population. Given that the U.S. public’s affective and cognitive appraisals might be different after vaccines became widely available, results need to be interpreted and generalized with caution. In addition, only survey data were collected, and no in-depth information from interviews or focus groups was obtained. Our proposed message strategies hence are speculative. In other words, the proposed strategies are “predictions” based on the literature on persuasion and health communication, and they need to be empirically tested in future studies. Last but not least, future research could also benefit from testing potential moderators, such as individual differences and sociocultural contexts, as well as the role played by media channels in vaccine hesitancy.
Conclusions
Employing a general U.S. population sample, this project revealed that vaccine-inclined individuals differ substantially from vaccine-hesitant ones in their cognitive and emotional responses to the pandemic and COVID-19 vaccines. Our data further showed that the vaccine-hesitant individuals could be classified into five heterogeneous groups, with each class having a unique, interpretable profile feature. Different messaging strategies are needed in communicating with vaccine-hesitant individuals based on their unique profiles.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Data can be accessed here: https://osf.io/sq26c/?view_only=b78712f38550448cb10d256acaac8889.
The U.S. Food and Drug Administration issued emergency use authorization (EUA) for the Pfizer-BioNTech, Moderna, and Johnson and Johnson COVID-19 vaccines, respectively, on December 11, 2020, December 18, 2020, and February 27, 2021. Although data of the study were collected after the first EUA was issued, it should be noted that the COVID-19 vaccines were only available for healthcare workers and people of 65 years and older in some states and remained unavailable for the general population by the time the data were collected.
Given that the COVID-19 vaccines had been made available to individuals 65 years of age and older in several states at the time of data collection, we repeated the analysis dropping participants who were 65 years of age and older (n = 110). Fit indices again favored a 5-profile solution. Characteristics of the five profiles were similar to those generated using the entire sample.
Contributor Information
Yanmengqian Zhou, Email: alisonzhou@lsu.edu.
Ruobing Li, Email: ruobing.li@stonybrook.edu.
Lijiang Shen, Email: lus32@psu.edu.
Data availability
Data will be made available on request.
References
- 1.Ahn S.J., Fox J. In: Encyclopedia of health and risk message design and processing. Parrott R., editor. Oxford University Press; 2017. Immersive virtual environments, avatars, and agents for health. [Google Scholar]
- 2.Akaike H. Factor analysis and AIC. Psychometrika. 1987;52(3):317–332. doi: 10.1007/BF02294359. [DOI] [Google Scholar]
- 3.Amin A.B., Bednarczyk R.A., Ray C.E., Melchiori K.J., Graham J., Huntsinger J.R., et al. Association of moral values with vaccine hesitancy. Nat Hum Behav. 2017;1(12):873–880. doi: 10.1038/s41562-017-0256-5. [DOI] [PubMed] [Google Scholar]
- 4.Atkin CK, Freimuth V. Guidelines for formative evaluation research in campaign design. In: Rice RE, Atkin C.K, editors, Public communication campaigns, Sage; 2013. 4th ed. p. 53-68.
- 5.Banfield J.D., Raftery A.E. Model-based Gaussian and non-Gaussian clustering. Biometrics. 1993;49(3):803–821. doi: 10.2307/2532201. [DOI] [Google Scholar]
- 6.Banker S., Park J. Evaluating prosocial COVID-19 messaging frames: evidence from a field study on Facebook. Judgm Decis Mak. 2020;15(6):1037–1043. doi: 10.2139/ssrn.3684901. [DOI] [Google Scholar]
- 7.Becker M.H. The health belief model and sick role behavior. Health Educ Monogr. 1974;2(4):409–419. [Google Scholar]
- 8.Boutebal S.E., Yahi S., Madani A. Impact of unrealistic optimism on the risk of contamination during the home confinement of COVID-19 in Algeria. Ind J Public Health Res Dev. 2020;12(1):413–425. doi: 10.21203/rs.3.rs-50930/v1. [DOI] [Google Scholar]
- 9.Bunch L. A tale of two crises: Addressing Covid-19 vaccine hesitancy as promoting racial justice. HEC Forum 2021;33(1-2):143–154. https://doi.org/10.1007/s10730-021-09440-0. [DOI] [PMC free article] [PubMed]
- 10.Bussink-Voorend D., Hautvast J.L., Vandeberg L., Visser O., Hulscher M.E. A systematic literature review to clarify the concept of vaccine hesitancy. Nat Hum Behav. 2022;1–15 doi: 10.1038/s41562-022-01431-6. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. How to tailor COVID-19 vaccine information to your specific audience. Retrieved from http://dx.doi.org/10.1136/archdischild-2020-319910.
- 13.Chou W.Y.S., Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 14.Clark SL, Muthén B. Relating latent class analysis results to variables not included in the analysis; 2009. Retrieved from https://www.statmodel.com/download/relatinglca.pdf.
- 15.Damasio A., Carvalho G.B. The nature of feelings: evolutionary and neurobiological origins. Nat Rev Neurosci. 2013;14:143–152. doi: 10.1038/nrn3403. [DOI] [PubMed] [Google Scholar]
- 16.Dillard J.P., Yang C., Li R. Self-regulation of emotional responses to Zika: spiral of fear. PLoS One. 2018;13(7):e0199828. doi: 10.1371/journal.pone.0199828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J.A. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dubé E., Gagnon D., Nickels E., Jeram S., Schuster M. Mapping vaccine hesitancy—country-specific characteristics of a global phenomenon. Vaccine. 2014;32(49):6649–6654. doi: 10.1016/j.vaccine.2014.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fishbein M, Ajzen, I. Predicting and changing behavior: The reasoned action approach. Psychology Press; 2010.
- 21.Fridman A., Gershon R., Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLoS One. 2021;16(4):e0250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffith J., Marani H., Monkman H. COVID-19 vaccine hesitancy in Canada: Content analysis of tweets using the theoretical domains framework. J Med Internet Res. 2021;23(4):e26874. doi: 10.2196/26874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu T., Wang S., Luo W., Zhang M., Huang X., Yan Y., et al. Revealing public opinion towards COVID-19 vaccines with Twitter data in the United States: spatiotemporal perspective. J Med Internet Res. 2021;23(9):e30854. doi: 10.2196/30854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karimi-Malekabadi F, Reimer NK, Atari M, Trager J, Kennedy B, Graham J, Dehghani M. Moral values predict county-level COVID-19 vaccination rates in the United States. [DOI] [PubMed]
- 25.Kelly B.J., Hornik R.C. Effects of framing health messages in terms of benefits to loved ones or others: an experimental study. Health Commun. 2016;31(10):1284–1290. doi: 10.1080/10410236.2015.1062976. [DOI] [PubMed] [Google Scholar]
- 26.Kim J., Choe Y.J., Lee J., Park Y.J., Park O., Han M.S., et al. Role of children in household transmission of COVID-19. Arch Dis Child. 2021;106(7):709–711. doi: 10.1136/archdischild-2020-319910. [DOI] [PubMed] [Google Scholar]
- 27.Kirzinger A, Sparks G, Hamel L, Lopes L, Kearrney A, Stokes M, Brodie M. 2021. KFF COVID-19 Vaccine Monitor: July 2021. KFF. Retrieved from https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-july-2021/.
- 28.Li R. Fear of COVID-19: What causes fear and how individuals cope with it. Health Commun. 2021 doi: 10.1080/10410236.2021.1901423. [DOI] [PubMed] [Google Scholar]
- 29.Lyu J.C., Le Han E., Luli G.K. COVID-19 vaccine-related discussion on Twitter: topic modeling and sentiment analysis. J Med Internet Res. 2021;23(6):e24435. doi: 10.2196/24435. https://preprints.jmir.org/preprint/24435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 31.Magesh S., John D., Li W.T., Li Y., Mattingly-App A., Jain S., et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw Open. 2021;4(11):e2134147. doi: 10.1001/jamanetworkopen.2021.34147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McLachlan G.J., Peel D. Wiley; 2000. Finite mixture models. [Google Scholar]
- 33.Morgan S.E., Palmgreen P., Stephenson M.T., Hoyle R.H., Lorch E.P. Associations between message features and subjective evaluations of the sensation value of antidrug public service announcements. J Commun. 2003;53(3):512–526. doi: 10.1111/j.1460-2466.2003.tb02605.x. [DOI] [Google Scholar]
- 34.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; 2019. URL https://www.R-project.org/.
- 35.Rogers R.W. A protection motivation theory of fear appeals and attitude change1. J Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 36.Rosenberg J.M., Beymer P.N., Anderson D.J., Van Lissa C.J., Schmidt J.A. tidyLPA: An R package to easily carry out latent profile analysis (LPA) using open-source or commercial software. J Open Source Software. 2018;3(30):978. doi: 10.21105/joss.00978. [DOI] [Google Scholar]
- 37.Salmon D.A., Dudley M.Z., Glanz J.M., Omer S.B. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine. 2015;33:D66–D71. doi: 10.1016/j.amepre.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 38.Sclove S.L. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52(3):333–343. doi: 10.1007/BF02294360. [DOI] [Google Scholar]
- 39.Shen L. Features of empathy-arousing strategies messages. Health Commun. 2019;34(11):1329–1339. doi: 10.1080/10410236.2018.1485078. [DOI] [PubMed] [Google Scholar]
- 40.Shen L, Li S, Sweeney K, Lee D. (November 2021). Re-explicating hope as a discrete emotion and its role in persuasion. Paper presented at NCA Conference. Seattle, WA.
- 41.Shen L., Zhou Y. Epistemic egocentrism and processing of vaccine misinformation (vis-à-vis scientific evidence): the case of vaccine-autism link. Health Commun. 2021;36(11):1405–1416. doi: 10.1080/10410236.2020.1761074. [DOI] [PubMed] [Google Scholar]
- 42.Sundar S.S., Jia H., Waddell T.F., Huang Y. In: The handbook of the psychology of communication technology. Sundar S.S., editor. Wiley Blackwell; 2015. Toward a theory of interactive media effects (TIME): Four models for explaining how interface features affect user psychology; pp. 47–86. [Google Scholar]
- 43.Yale Institute of Global Health. Vaccine message guide. Retrieved from https://medicine.yale.edu/yigh/resources/Covid-19_Guide_v3_416091_40906_v1.pdf.
- 44.Yzer M. The integrative model of behavior prediction as a tool for designing health messages. In Cho H (Ed.). Designing messages for health campaigns: Theory and practice (pp. 21-40). Sage.
- 45.Zhou Y Shen L. Confirmation bias and the persistence of misinformation on climate change. Commun Res. https://doi.org/10.1177%2F00936502211028049.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.