Abstract
Objective:
Identification of unmet psychiatric needs, protective and risk factors for suicide are crucial for people with traumatic spinal cord injury (SCI). In this study, we aimed to explore depression, post-traumatic stress disorder (PTSD) status (non-PTSD, partial-PTSD, full-PTSD), resilience, suicidal ideation (SI) and to examine predictors and clinical correlates of current SI in traumatic SCI.
Method:
Sixty-three individuals with traumatic SCI who were at least 3 months post-injury were included in the study. The participants were evaluated in terms of PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (PCL-5), depression, SI, and resilience using the PCL-5, the Patient Health Questionnaire-9, the Brief Resilience Scale, and sociodemographic measures.
Results:
33% of our sample (n = 21) had SI over the past two weeks. 71.4% of the patients with SI (n = 15) had depression. A total of 52.4% of the patients with SI (n = 11) were diagnosed with full PTSD. Resilience was found to be significantly lower in individuals with depression and individuals with SI. While depression predicted SI in traumatic SCI, resilience stands as a protective factor against SI.
Conclusion:
SI is quite common in individuals with traumatic SCI and is accompanied by substantial psychiatric comorbidities such as depression and PTSD. Along with depression and PTSD, resilience – which has protective and predictive values and is inversely associated with SI – constitutes a significant psychotherapeutic intervention and screening area.
Keywords: Depression, Post-traumatic stress disorder (PTSD), Partial PTSD, Resilience, Suicidal ideation, Traumatic spinal cord injury, Rehabilitation
Introduction
Spinal cord injury (SCI) is a major traumatic event that is associated with devastating consequences for the physical, functional, and psychosocial well-being of patients and their caregivers. In addition to paralysis and reduced mobility in SCI, a substantial amount of psychiatric morbidity occurs, which can interfere with rehabilitation and long-term management of the patient. Many factors have been identified to contribute to psychiatric morbidity after SCI such as premorbid psychiatric disorders, perceived quality of life, coping style,1 trauma recency,2,3 the younger the age of trauma exposure,4 negative trauma-related appraisals.3 The risk of developing major depression,1 anxiety disorder,5,6 post-traumatic stress disorder (PTSD),1,4,7 and sleep disturbances8 as well as suicidal ideation (SI) and attempts,9,10 increases in individuals with SCI.
The total suicide rate among people with SCI is nearly five times greater11 and mortality due to suicide is 4.9 times higher than in the general population.12 The risk of suicide among people with SCI is higher in the early post-injury years, particularly the first 10.13 Different studies have predicted varied levels of risk.14 As SI is a significant predictor of subsequent suicide attempts,15 it is important to identify SI and factors that can increase the risk of suicide in individuals with SCI.
The presence of psychiatric disorders has been reported to be one of the more important risk factors for suicide among individuals with SCI,14 but the extent to which these disorders affect the risk of suicide is unclear, as is which psychiatric disorder has a greater effect on suicide. Depression is an established risk factor for SI,9 and it is twice as common in individuals with SCI compared with the general population.16 The prevalence of depression ranges from 25% to 45% in patients with SCI,3,17–19 and depression was found to be associated with poorer outcomes, such as longer hospital stays and increased medical complications.1
Traumatic stress reactions after SCI are common, and a significant proportion of these individuals develop PTSD.20,21 The lifetime prevalence of PTSD in individuals with SCI remains high; up to 29% continue to report symptoms 30 years after the injury.2 PTSD is best conceptualized as a dimensional disorder.22 Emergence of post-traumatic stress symptoms following trauma exposure that does not fulfill the diagnostic criteria of PTSD is known as subthreshold or partial PTSD.23 Partial PTSD was found to be a prevalent and clinically significant condition that is associated with depression, alcohol use problems, suicidal behavior,23 cause substantial functional impairment,24 and require intervention.25
Besides identifying negative factors in SCI, there has been also a growing interest in variables (e.g. self-efficacy, internal locus of control, resilience) that might ease the psychological adjustment process and prevent psychiatric problems in SCI.26 Resilience, which is defined as adaptability, sustainability, and recovery in the face of stress or trauma over the lifespan27 is a combination of state and trait factors.28 This dynamic process of resilience could provide a potential target for intervention in rehabilitation settings with its moderator role for depression, pain, and post-traumatic growth in individuals with SCI.29 In addition, it could also be a key consideration for the assessment of suicide risk in individuals with SCI because of its possible protective effects against suicide. Also, resilience might have a preventive role against the development of full PTSD therefore partial PTSD may reflect the resilience or represent a prodrome for delayed-onset PTSD.22
Promoting a better understanding of risk factors for suicide, and addressing protective factors against suicide in people with traumatic SCI is crucial. In this study, our main hypothesis was that psychiatric comorbidities might be associated with an increase in the frequency of SI while resilience might exist as a protective factor by correlating with a reduction in SI. We explored depression, PTSD status (non-PTSD, partial PTSD, and full PTSD), resilience, and SI in individuals with traumatic SCI. We also evaluated the clinical and sociodemographic factors involved and examined predictors and clinical correlates of current SI in association with PTSD and depression.
Material and methods
This study was designed as a cross-sectional study with a cohort of people with traumatic SCI. The local ethics committee approved the study. A consecutive series of patients receiving inpatient rehabilitation at a tertiary physical medicine and rehabilitation clinic for traumatic SCI were interviewed between May 2018 and May 2019. The inpatient unit admits patients from a broad geographical region, both urban and rural areas. All patients with SCI of any severity received standard physical medicine and rehabilitation therapy. Participants were included if they 1) were 18–65 years of age, 2) had experienced abrupt traumatic onset SCI rather than the gradual progression of an illness, 3) complete or incomplete injury with ASIA Impairment Scale level either A or B or C, 4) were at least 3 months post-injury (to exclude problems that could be related to transient adjustment difficulties in the early phase of SCI), and 5) had adequate cognitive capacity to complete the questionnaires. The exclusion criteria were moderate to severe head injury at the time of SCI or the patient reporting unconsciousness for >15 min at the time of injury, severe vital organ dysfunction, SCI due to suicide attempt, and previous or current psychosis, intellectual disability, bipolar disorder, organic mental disorder, or dementia. The ASIA-D group which has a relatively milder severity was not included as it might interfere with the psychiatric outcomes. After explaining the purpose and content of the study, written informed consent was obtained from each participant. Eleven people with traumatic SCI were excluded because they did not meet the inclusion criteria (5 for the injury with ASIA-D, 3 for traumatic brain injury, 1 for not being medically stable, and 2 for not volunteering for the participation of the study). A total of 63 patients who met the inclusion criteria consented to participate in the study. Preliminary results of 40 patients in this study were presented with an e-poster at the 27th European Congress of Psychiatry, Warsaw, Poland.
Measures and procedure
The participants were assessed within the first 2 weeks of admission to inpatient rehabilitation to overcome the possible effects of hospital stay on outcome measures. Sociodemographic data on age, sex, years of education, current relationship and employment status, and injury-related data such as age at the time of injury, type of injury, time since injury was obtained from the participants. The level and the severity of the physical injury was assessed by a physiatrist according to the International Standards for Neurological Classification of SCI developed by the American Spinal Injury Association.30
PTSD symptoms
PTSD symptoms were assessed using the Turkish version of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (PCL-5).31 The PCL-5 consists of 20 self-report items and 4 scales in accordance with PTSD symptom clusters in DSM-5: re-experiencing (Criteria B), avoidance (Criteria C), negative alterations (Criteria D), and hyper-arousal (Criteria E).32 DSM-5 criteria require 1 B item, 1 C item, 2 D items, and 2 items to be fulfilled to diagnose full PTSD.33 Each item of the PCL-5 with a rating of at least 2 (moderate or higher) was considered a PTSD symptom. With .76 sensitivity and .69 specificity, a cutoff score of ≥47 was suggested for the diagnosis of PTSD for the Turkish version of the scale.31 Although there is no consistent definition for the diagnosis of partial PTSD, the most useful definition of partial PTSD according to DSM-5 was defined as meeting two or three of the DSM-5 Criteria.25
Resilience
The Turkish version of the Brief Resilience Scale (BRS) was used to measure resilience.34 The BRS was developed to assess the ability to rebound or recover from stress, which is defined as resilience.35 It consists of six items on a 5-point Likert scale, and higher scores indicate greater resilience.
Depression
To evaluate depressive symptomatology, the depression module from the Patient Health Questionnaire (PHQ) was used.36 This 9-item scale was shown to be reliable and valid for the criteria-based diagnosis of depression according to the Diagnostic and Statistical Manual of Mental Disorders as well as for the determination of depression severity.37 The total score can range from 0 to 27; scores of 5, 10, 15, and 20 serve as cutoff scores indicating mild, moderate, moderately severe, and severe depression.38 The PHQ-9 has been validated in an acute SCI rehabilitation sample.39
Suicidal ideation
The ninth item of the PHQ-9 (“Thoughts that you would be better off dead or of hurting yourself in some way”) was used to evaluate the current SI of the participants. The response options ranged from 0 (not at all) to 3 (nearly every day).37 The participants were coded as having SI if they scored at least 1.
Statistics
Statistical analysis was performed using SPSS (Statistical Package for Social Science) version 21.0 software (IBM SPSS Statistics, New York, United States). The patients were divided into two groups based on the presence of SI. Demographic and injury characteristics were compared between the groups. Psychiatric comorbidities were evaluated and compared with the total and subscale scores of the given scales. In addition, participants who remained above the cut-off according to the measures (depression present/ not present, non-PTSD, partial PTSD, full-PTSD) were also compared categorically between SI groups. The Kolmogorov–Smirnov test was used for testing normality. As the continuous variables were not normally distributed, a Mann–Whitney U test was conducted to compare the characteristics of the two groups. Independent samples t-test was used to compare normally distributed variables. The Levene test was used to assess the homogeneity of the variances. The chi-square test was used to compare categorical variables. Due to the non-normally distributed data, correlation coefficients and their significance were calculated using the Spearmen test while investigating the associations between SI and other clinical variables. For all statistical analyses, the alpha level of significance was set at .05.
A binary logistic regression analysis was performed to determine the predictors of SI in individuals with traumatic SCI. For the multivariate analysis, logistic regression analysis was performed on the possible factors identified using univariate analyses. The Hosmer-Lemeshow test showed that the model fits the data well. A 5% type-1 error level was used to infer statistical significance.
Results
Characteristics
Sociodemographic and injury-related characteristics and results of the analyses of these data across patients with and without SI are summarized in Table 1.
Table 1.
Demographic and injury characteristics of participants.
| SI + n = 21 (33.3%) |
SI – n = 42 (66.7%) |
Total n = 63 |
Statistics | |
|---|---|---|---|---|
| Age (years) | 33.7 ± 12.5 | 38.4 ± 13.6 | 36.8 ± 13.3 | t(61) = 1.319, P = 0.192 |
Sex n (%)
|
9 (43%) 12 (57%) |
12 (29%) 30 (71%) |
21 (33%) 42 (67%) |
χ²=1.286, df =1, P =0.257 |
| Education (years) | 9 ± 3.3 | 8.7 ± 4.1 | 8.9 ± 3.8 | U = 451, P = 0.882 |
Relationship status
|
10(48%) 10(48%) 1 (4%) |
17 (40%) 23 (55%) 2 (5%) |
27 (43%) 33 (52%) 3 (5%) |
χ²=3.303, df =3, P =0.347 |
Current employment status
|
2 (5%) 19 (90%) |
5 (12%) 37 (88%) |
4 (6%) 59 (94%) |
χ²=0.134, df =2, P =0.935 |
| Age at the time of injury | 30 ± 13.3 | 34.8 ± 15 | 33 ± 15 | U = 357.5, P = 0.223 |
| Time since injury (month) min-max |
44.8 ± 58.5 3–228 |
42.1 ± 42.9 3–192 |
43 ± 48 3–228 |
U = 416.5, P = 0.721 |
Type of injury
|
8 (38%) - 7 (33%) 2 (10%) 3 (14%) 1 (5%) |
14 (33%) 1 (2%) 15 (35%) 4 (10%) 4 (10%) 4 (10%) |
22 (35%) 1 (2%) 22 (35%) 6 (9%) 7 (11%) 5 (8%) |
χ²=2.649, df =6, P =0.851 |
Type and level of injuryParaplegia
|
6 (29%) 7 (33%) 13(62%) 6 (29%) 2 (9%) 8 (38%) |
17(40%) 10 (24%) 27(64%) 7 (17%) 8 (19%) 15 (36%) |
23 (36%) 17 (27%) 40 (63%) 13 (21%) 10 (16%) 23 (37%) |
χ²=2.776, df =3, P =0.428 |
PTSD situation, depression and resilience
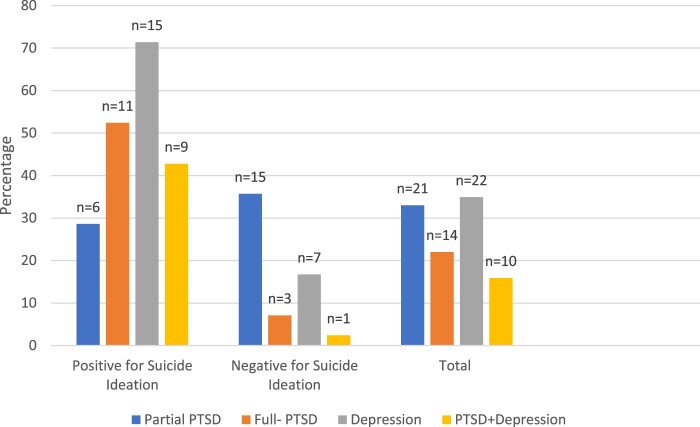
Psychiatric comorbidities among SI groups and total participants were given in Figure 1.
Figure 1.
Psychiatric comorbidities among SI groups and total participants.
There was no statistically significant difference between individuals with depression in terms of age (t(61) = 0.675, p = 0.502), sex(χ² = 0.873, df = 1, P = 0.350), education (U = 413.5, P = 0.581), and employment status (χ² = 0.428, df = 2, P = 0.807). Regarding the trauma-related parameters, no difference was observed between depressed individuals and those without depression in terms of age at the time of injury (U = 373, P = 0.260), time since injury (U = 426.5, P = 0.724), type of injury (χ² = 4.188, df = 6, P = 0.651), and type and level of spinal injury (χ² = 2.946, df = 3, P = 0.400).
The mean resilience score according to the BRS was 21.06 ± 4.7. BRS scores differed significantly between patients with or without SI (U = 223.5, P = 0.001) and between depressed and non-depressed participants (U = 273.5, P = 0.01). There was no statistical difference between the PTSD groups in terms of resilience (χ²(2) = 3.891, P = 0.143).
Suicidal ideation
Of the participants, 21 (33%) had SI over the past two weeks according to PHQ-9 item 9. Demographic and injury characteristics of participants according to SI and the statistical results are given in Table 1. 71.4% of the patients with SI (n = 15) had depression. A total of 52.4% of the patients with SI (n = 11) were diagnosed with full PTSD and 78.6% of the full PTSD sample had current SI. In the partial PTSD group, the SI rate was 28.6% (n = 6). Psychiatric comorbidity rates of the participants with or without SI were given in Figure 1.
Four of the participants (6.3%) had attempted suicide (a total of 5 attempts) after the traumatic event, while 3 of them still had SI. Two patients (3.2%) with a history of suicide attempts prior to the traumatic event had no current SI.
Table 2 shows psychometric evaluations related to PTSD, depression, and resilience among SI groups. Intercorrelation analysis for variables predicting SI was given in Table 3.
Table 2.
Psychometric evaluations related to PTSD, depression, and resilience among SI groups.
| SI + | SI - | Statistics | |
|---|---|---|---|
| PCL-Total Re-experience Avoidance Negative alteration Hyperarousal |
40 ± 17.9 8.7 ± 4.6 4.8 ± 2.9 14.2 ± 6.6 12.3 ± 6.1 |
20.5 ± 13.7 4.7 ± 3.6 2.1 ± 2.2 8.1 ± 6 5.5 ± 4.4 |
U = 179, P < 0.001 U = 224.5, P = 0.002 U = 199, P < 0.001 U = 220.5, P = 0.001 U = 161, P < 0.001 |
| Brief Resilience Scale (BRS) | 18.4 ± 3.7 | 22.4 ± 4.6 | U = 223.5, P = 0.001 |
| PHQ-9 total item 9 score |
13 ± 4.7 1.3 ± 0.6 |
6 ± 4.2 0 |
U = 122.5, P < 0.001 |
Values are mean ± SD
Table 3.
Correlation analysis for variables predicting SI.
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Suicide ideation (PHQ- item 9) | – | .608** | −.409** | .501** |
| 2. PHQ-total | – | −.328** | .701** | |
| 3. BRS | – | −.333** | ||
| 4. PCL total | – |
**significant at the 0.01 level
Predictors of suicidal ideation
Binary logistic regression analysis was performed to determine which independent variables were significantly associated with SI. The selection of the independent variables (BRS, total PHQ-9, and total PCL scores) for the binary logistic regression analysis was based on significance from the univariate analysis (SI present/not present) (P < 0.05).
The combined predictor variables correctly distinguished between those who reported some degree of SI and those who did not (82.5% of all possible pairs). Cox & Snell R2 = .395; Nagekerke R2 = .548.
Results of the multiple binary logistic regression
The likelihood ratio test (χ² (2) = 31.609, P < .001) indicated that the logistic model was more effective than an intercept-only model. Table 4 summarizes the results of the logistic regression. The Hosmer-Lemeshow test showed that the model fits the data well (χ²(8) = 1.951, P = .982). Logistic regression analysis revealed that BRS score (OR = 0.821, P = .044, 95% CI = 0.678-.995), and total PHQ-9 score (OR = 1.39, P = .000, 95% CI = 1.163-1.66) were significantly associated with SI.
Table 4.
Backward logistic regression analysis.
| Predictors of SI | SE | Wald χ2 | P | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Step1 | PHQ-9 | .098 | 7.202 | .007 | 1.302 | [1.07–1.57] |
| BRS | .096 | 3.207 | .073 | 0.842 | [0.69–1.01] | |
| PCL | .028 | 1.7 | .192 | 1.037 | [0.98–1.09] | |
| Step2 | PHQ-9 | .091 | 13.143 | .000 | 1.39 | [1.16-1.66] |
| BRS | .098 | 4.049 | .044 | 0.821 | [0.67-0.99] |
SE: Standard Error, P: statistical significance, OR: odds-ratio, CI: Confidence Interval
Overall, depression (total PHQ-9 score) was closely associated with an increased risk of SI while the growth of resilience (BRS score) was related to a decrease in SI (Table 4).
Discussion
The present study examined the prevalence and risk factors of depression, PTSD symptoms, and SI in individuals with traumatic SCI. The predictors and clinical correlates of SI were also evaluated. We found that 22% of our sample was diagnosed with full PTSD, and 33% of patients had partial PTSD. PTSD rates in the SCI population were reported to range between 14% and 40%.2,7,20,40 This wide range of prevalence rates may be explained by several reasons. For instance, some studies included war veterans with SCI, with whom PTSD prevalence is higher.40 Time since trauma and the use of various tools to assess PTSD status in patients with SCI may have also contributed to differences in prevalence rates. Only two other studies evaluated PTSD symptomatology dimensionally by examining partial PTSD with SCI; the prevalence rates reported were 42% and 20%.7,41 This difference in prevalence rates may be related to similar causes that were mentioned for full PTSD or the definition used for partial PTSD.
Psychiatric comorbidity is considered a major risk factor for suicide among individuals with SCI and it is high in those with SI.14 In our study, more than half of the patients (52.4%) with SI were diagnosed with full PTSD, 71.4% with depression and nearly half of them (42.8%) both PTSD and depression. Comorbidity between PTSD and major depressive disorder is common, with approximately half the people with PTSD also presenting with a diagnosis of major depressive disorder across different samples.42 It is unclear whether this high comorbidity is due to symptom overlap or is a trauma-related phenomenon in this group of patients. Research has shown that patients diagnosed with both depression and PTSD are at greater risk for suicide attempts than people with only PTSD.42 In this study, the main difference in terms of SI was observed in the full PTSD group with depression. In the logistic regression analysis, depression along with resilience predicted SI in patients with traumatic SCI. Also, significant correlations were obtained between PTSD and depression ratings and this high correlation might be obfuscating whether PTSD or depression is driving SI. Our findings suggest that in a subgroup of individuals with SCI, full PTSD is highly comorbid with depression, and that this group might be at higher risk for suicide. Furthermore, these findings suggest that this high comorbidity may be a distinct trauma-related condition beyond the overlap of symptom clusters. Therefore, these patients should be routinely screened for depression and PTSD and intervened when necessary, because of the frequency of both conditions and their strong relationship with SI.
Although 28.6% had SI, the partial PTSD group did not differ significantly from the full PTSD and non-PTSD groups in terms of SI. Even if partial PTSD was shown to be similar to full PTSD in terms of chronicity and disability in previous research,43 this group might be associated with a lower risk of suicide and depression. Partial PTSD has been stated as an expression of individuals with higher resilience.22 However, no statistical difference in resilience between PTSD groups in our study suggests that partial PTSD might be related to insufficient recovery from full PTSD.
In recent years, resilience started to gain more attention in suicide studies. Previous research has shown that low resilience predicted suicidality at all ages44 and was associated with increased suicide attempts in different clinical populations.45 It has been shown to moderate depressive symptoms46 and was found to be associated with less pain interference, higher functionality, shorter length of stay during rehabilitation, and better long-term health in individuals with SCI.47 In our study, resilience was found to be significantly lower in individuals with depression and individuals with SI and emerged as an important factor predicting SI. Resilience was proposed to modify the risk of suicidality with its “buffering effect” in previous work.48 Also, resilience factors such as social support was shown to reduce the impact of both PTSD and partial PTSD on suicidal behavior risk in trauma victims.49 This indicates presence and the severity of psychiatric comorbidities are not enough for the assessment of suicide risk. Therefore, resilience seems to be a helpful and essential tool for determining the risk of suicide. Because resilience is a dynamic process and different aspects of resilience can be affected across the life span or after adverse life events,47 time since trauma and cross-sectional evaluation of resilience should be taken into account. Improving resilience can reduce the risk of depression and SI in patients with SCI, and considering its overall health effects, resilience enhancement should become part of the standard of care of individuals with SCI.
Findings regarding the effect of injury severity (level and completeness of lesion) on psychopathology are inconsistent in the literature. In some studies, paraplegia was associated with PTSD,2,50 while in others, tetraplegia was found to be associated with more severe PTSD.51 We found no significant association between injury severity and SI status, depression, or PTSD. Further research is required on the effect of the physical impact of injury on psychopathology level.
Studies related to PTSD in civilian populations are relatively few in the literature. One of the strengths of this study is that we evaluated a homogeneous civilian group with traumatic SCI with well-established scales. While addressing risk factors for SI, we also evaluated a significant protective factor. We also approached post-traumatic stress symptoms from a spectrum perspective by including partial PTSD in the assessment.
One of the major limitations of the study is the difficulty in establishing a cause–effect relationship because of the cross-sectional design. We included SCI with a traumatic origin for this study. It is difficult to distinguish whether the traumatic injury or spinal cord lesions caused trauma-related consequences from the present findings. The sample size, the single-center recruitment, the inclusion of inpatient SCI for rehabilitation purposes and the exclusion of the individuals with ASIA-D level injury reduce the generalizability of the findings. Individuals with severe mental illness (e.g. psychosis, bipolar disorder, etc.) were excluded from our study which limits the prediction of psychiatric adversities that may develop after traumatic spinal cord injury in individuals with a history of severe mental illness. Along with the risks brought by severe mental illness, it might be necessary to be more careful in terms of psychiatric adversity and SI during the rehabilitation processes of individuals with both traumatic SCI and severe mental illnesses. Since the stepwise regression model sometimes could lead to misleading results due to overfitting, our results should be interpreted with caution. Longitudinal follow-up studies are needed to understand the dynamic nature of factors such as PTSD, depression, SI, and resilience in traumatic SCI.
This study primarily highlights the risk factors for suicide as well as protective elements against suicide in individuals with traumatic SCI. Depression and PTSD are common psychiatric morbidities in individuals with traumatic SCI and are substantial factors predicting SI. Depression was highly prevalent in a group of SCI patients with SI and full PTSD. Whether this comorbidity is a co-occurrence or a trauma-related phenomenon is unclear, but the need to address both psychopathologies simultaneously is obvious. Therefore, they constitute a significant psychotherapeutic intervention and screening area. In addition, our results support the clinical importance of resilience in this patient group, as its protective and predictive values were associated with SI. Enhancing resilience can reduce or prevent SI in individuals with traumatic SCI, and a more detailed understanding of its effects on mental health outcomes could have a beneficial effect on the rehabilitation practice of these individuals.
Funding Statement
None.
Disclaimer statements
Contributors None.
Conflicts of interest Authors have no conflict of interests to declare.
References
- 1.Craig A, Tran Y, Middleton J.. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2009;47(2):108–14. [DOI] [PubMed] [Google Scholar]
- 2.Radnitz CL, Hsu L, Willard J, Perez-Strumolo L, Festa J, Lillian LB, et al. Posttraumatic stress disorder in veterans with spinal cord injury: trauma-related risk factors. J Trauma Stress 1998;11(3):505–20. [DOI] [PubMed] [Google Scholar]
- 3.Schönenberg M, Reimitz M, Jusyte A, Maier D, Badke A, Hautzinger M.. Depression, posttraumatic stress, and risk factors following spinal cord injury. Int J Behav Med 2014;21(1):169–76. [DOI] [PubMed] [Google Scholar]
- 4.Pollock K, Dorstyn D, Butt L, Prentice S.. Posttraumatic stress following spinal cord injury: a systematic review of risk and vulnerability factors. Spinal Cord 2017;55(9):800–11. [DOI] [PubMed] [Google Scholar]
- 5.Craig A, Hancock K, Dickson H.. A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Spinal Cord 1994;32(10):675–9. [DOI] [PubMed] [Google Scholar]
- 6.Kennedy P, Rogers BA.. Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil 2000;81(7):932–7. [DOI] [PubMed] [Google Scholar]
- 7.Chung MC, Preveza E, Papandreou K, Prevezas N.. The relationship between posttraumatic stress disorder following spinal cord injury and locus of control. J Affect Disord 2006;93(1–3):229–32. [DOI] [PubMed] [Google Scholar]
- 8.Budh CN, Hultling C, Lundeberg T.. Quality of sleep in individuals with spinal cord injury: a comparison between patients with and without pain. Spinal Cord 2005;43(2):85–95. [DOI] [PubMed] [Google Scholar]
- 9.McCullumsmith CB, Kalpakjian CZ, Richards JS, Forchheimer M, Heinemann AW, Richardson EJ, et al. Novel risk factors associated with current suicidal ideation and lifetime suicide attempts in individuals with spinal cord injury. Arch Phys Med Rehabil 2015;96(5):799–808. [DOI] [PubMed] [Google Scholar]
- 10.Nam H, Kim H, Ha TH, Shin H-I.. Suicidal ideation in Korean persons with spinal cord injury. Spinal Cord 2013;51(10):789–93. [DOI] [PubMed] [Google Scholar]
- 11.Hartkopp A, Brønnum-Hansen H, Seidenschnur A-M, Biering-Sorensen F.. Suicide in a spinal cord injured population: its relation to functional status. Arch Phys Med Rehabil 1998;79(11):1356–61. [DOI] [PubMed] [Google Scholar]
- 12.DeVivo MJ, Black K, Richards JS, Stover S.. Suicide following spinal cord injury. Spinal Cord 1991;29(9):620–7. [DOI] [PubMed] [Google Scholar]
- 13.Savic G, DeVivo M, Frankel H, Jamous M, Soni B, Charlifue S.. Suicide and traumatic spinal cord injury—a cohort study. Spinal Cord 2018;56(1):2–6. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy P, Garmon-Jones L.. Self-harm and suicide before and after spinal cord injury: a systematic review. Spinal Cord 2017;55(1):2–7. [DOI] [PubMed] [Google Scholar]
- 15.Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, Keyes KM, Hasin DS, Grant BF, et al. Estimating risk for suicide attempt: Are we asking the right questions?: passive suicidal ideation as a marker for suicidal behavior. J Affect Disord 2011;134(1-3):327–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giannini MJ, Bergmark B, Kreshover S, Elias E, Plummer C, O'Keefe E.. Understanding suicide and disability through three major disabling conditions: intellectual disability, spinal cord injury, and multiple sclerosis. Disabil Health J 2010;3(2):74–8. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS.. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil 2011;92(3):411–8. [DOI] [PubMed] [Google Scholar]
- 18.Arango-Lasprilla JC, Ketchum JM, Starkweather A, Nicholls E, Wilk AR.. Factors predicting depression among persons with spinal cord injury 1 to 5 years post injury. NeuroRehabilitation 2011;29(1):9–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saunders LL, Krause J, Focht KL.. A longitudinal study of depression in survivors of spinal cord injury. Spinal Cord 2012;50(1):72–7. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy P, Duff J.. Post traumatic stress disorder and spinal cord injuries. Spinal Cord 2001;39(1):1–10. [DOI] [PubMed] [Google Scholar]
- 21.Cao Y, Li C, Newman S, Lucas J, Charlifue S, Krause JS.. Posttraumatic stress disorder after spinal cord injury. Rehabil Psychol 2017;62(2):178. [DOI] [PubMed] [Google Scholar]
- 22.Schnurr P. A guide to the literature on partial PTSD. PTSD Res Q 2014;25(1):1–3. [Google Scholar]
- 23.Kim JI, Oh S, Park H, Min B, Kim JH.. The prevalence and clinical impairment of subthreshold PTSD using DSM-5 criteria in a national sample of Korean firefighters. Depress Anxiety 2020;37(4):375–85. [DOI] [PubMed] [Google Scholar]
- 24.Bergman HE, Przeworski A, Feeny NC.. Rates of subthreshold PTSD among US military veterans and service members: A literature review. Mil Psychol 2017;29(2):117–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLaughlin KA, Koenen KC, Friedman MJ, Ruscio AM, Karam EG, Shahly V, et al. Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biol Psychiatry 2015;77(4):375–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Driver S, Warren AM, Reynolds M, Agtarap S, Hamilton R, Trost Z, et al. Identifying predictors of resilience at inpatient and 3-month post-spinal cord injury. J Spinal Cord Med 2016;39(1):77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jalilianhasanpour R, Williams B, Gilman I, Burke MJ, Glass S, Fricchione GL, et al. Resilience linked to personality dimensions, alexithymia and affective symptoms in motor functional neurological disorders. J Psychosom Res 2018;107:55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB.. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018;8(6):e017858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Min J-A, Lee C-U, Hwang S-I, Shin J-I, Lee B-S, Han S-H, et al. The moderation of resilience on the negative effect of pain on depression and post-traumatic growth in individuals with spinal cord injury. Disabil Rehabil 2014;36(14):1196–202. [DOI] [PubMed] [Google Scholar]
- 30.Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the International Standards for Neurological Classification of spinal cord injury. J Spinal Cord Med 2011;34(6):547–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boysan M, Guzel Ozdemir P, Ozdemir O, Selvi Y, Yilmaz E, Kaya N.. Psychometric properties of the Turkish version of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, (PCL-5). Psychiatry Clin Psychopharmacology 2017;27(3):300–10. [Google Scholar]
- 32.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL.. The posttraumatic stress disorder Checklist for DSM-5 (PCL-5): development and initial Psychometric evaluation. J Trauma Stress 2015;28(6):489–98. [DOI] [PubMed] [Google Scholar]
- 33.AmericanPsychiatricAssociation . Diagnostic and statistical manual of mental disorders (DSM-5®). Arlington (VA: ): American Psychiatric Pub; 2013. [Google Scholar]
- 34.Doğan T. Kısa psikolojik sağlamlık ölçeği’nin Türkçe uyarlaması: Geçerlik ve güvenirlik çalışması. The J Happiness Well-Being 2015;3(1):93–102. [Google Scholar]
- 35.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J.. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008;15(3):194–200. [DOI] [PubMed] [Google Scholar]
- 36.Spitzer RL, Kroenke K, Williams JB.. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA 1999;282(18):1737–44. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Spitzer RL, Williams JB.. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Poritz JMP, Mignogna J, Christie AJ, Holmes SA, Ames H.. The Patient Health Questionnaire depression screener in spinal cord injury. J Spinal Cord Med 2018;41(2):238–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bombardier CH, Kalpakjian CZ, Graves DE, Dyer JR, Tate DG, Fann JR.. Validity of the Patient Health questionnaire-9 in assessing major depressive disorder during inpatient spinal cord injury rehabilitation. Arch Phys Med Rehabil 2012;93(10):1838–45. [DOI] [PubMed] [Google Scholar]
- 40.Ullrich PM, Smith BM, Poggensee L, Evans CT, Stroupe KT, Weaver FM, et al. Pain and post-traumatic stress disorder symptoms during inpatient rehabilitation among operation enduring freedom/operation Iraqi freedom veterans with spinal cord injury. Arch Phys Med Rehabil 2013;94(1):80–5. [DOI] [PubMed] [Google Scholar]
- 41.Otis C, Marchand A, Courtois F.. Risk factors for posttraumatic stress disorder in persons with spinal cord injury. Top Spinal Cord Inj Rehabil 2012;18(3):253–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Flory JD, Yehuda R.. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues Clin Neurosci 2015;17(2):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jeon HJ, Suh T, Lee HJ, Hahm BJ, Lee JY, Cho SJ, et al. Partial versus full PTSD in the Korean community: prevalence, duration, correlates, comorbidity, and dysfunctions. Depress Anxiety 2007;24(8):577–85. [DOI] [PubMed] [Google Scholar]
- 44.Liu DW, Fairweather-Schmidt AK, Roberts RM, Burns R, Anstey KJ.. Does resilience predict suicidality? A lifespan analysis. Arch Suicide Res 2014;18(4):453–64. [DOI] [PubMed] [Google Scholar]
- 45.Roy A, Sarchiapone M, Carli V.. Low resilience in suicide attempters. Arch Suicide Res 2007;11(3):265–9. [DOI] [PubMed] [Google Scholar]
- 46.Catalano D, Chan F, Wilson L, Chiu C-Y, Muller VR.. The buffering effect of resilience on depression among individuals with spinal cord injury: a structural equation model. Rehabil Psychol 2011;56(3):200. [DOI] [PubMed] [Google Scholar]
- 47.McDonald SD, Pugh Jr M, Mickens MN.. Resilience after spinal cord injury: a scoping review. Am J Phys Med Rehabil 2020;99(8):752–63. [DOI] [PubMed] [Google Scholar]
- 48.Johnson J, Wood AM, Gooding P, Taylor PJ, Tarrier N.. Resilience to suicidality: the buffering hypothesis. Clin Psychol Rev 2011;31(4):563–91. [DOI] [PubMed] [Google Scholar]
- 49.Panagioti M, Gooding PA, Taylor PJ, Tarrier N.. Perceived social support buffers the impact of PTSD symptoms on suicidal behavior: implications into suicide resilience research. Compr Psychiatry 2014;55(1):104–12. [DOI] [PubMed] [Google Scholar]
- 50.Hatcher MB, Whitaker C, Karl A.. What predicts post-traumatic stress following spinal cord injury? Br J Health Psychol 2009;14(Pt 3):541–61. [DOI] [PubMed] [Google Scholar]
- 51.Boyer B, Tollen L, Kafkalas C.. A pilot study of posttraumatic stress disorder in children and adolescents with spinal cord injury. SCI Psychosocial Process 1998;11(1):75–81. [Google Scholar]