Abstract
Burn injuries are frequent, horrifying, and life-threatening conditions that are still challenging to cure. Complications like scarring, keloid formation, and contractures are the main challenges for the treating surgeon. The Ayurvedic classics explain different treatment modalities for the management of burn wounds, like oral medicines, topical applications prepared with herbal medicines, ghee, oil, and typical wound dressing techniques like Patraadaana (wound covering with medicinal leaves), and fumigation therapy, etc. Here we report a case of accidental burn injury with a TBSA of 27% First degree (superficial) and 15% second degree (deep partial-thickness) burns with complaints of fever and burning sensation at the burn site. On the basis of the symptoms listed in the classical texts of Ayurveda, the case was diagnosed as Pramadadagdha (accidental burn). To properly manage the burn wound, an integrated therapy strategy was designed. Ropanaghrita (medicated ghee) was applied locally, followed by the application of Tinospora cordifolia leaves to cover the wound, fumigation therapy, and oral medications to hasten wound healing and reduce infection. In the first seven days, modern medicine was used as emergency care in addition to Ayurvedic management. Within 60 days of receiving treatment, the burn wound had entirely healed, and the patient was able to resume her regular work activities. In the current situation, the combined strategy produced encouraging burn management outcomes.
Keywords: Accidental burn, Total body surface area, Ropana ghrita, Patraadaana, Dhoopana
Abbreviations: TBSA, Total body surface area
1. Introduction
Burn injuries can occur from fire, moist heat, electrical source, chemical agents, radiations, etc [1]. In India, an estimated [6,7] million cases of mild to severe burns are reported each year [2,3]. Burn injuries are typically 86% thermal in origin, 4% electrical, and 3% chemical in nature. Burn injuries are more common in low- and middle-income people [4]. Standard guidelines for managing burns include fluid resuscitation, airway preservation, analgesics, broad-spectrum antibiotics, nutritional support, escharotomy, fasciotomy, skin grafting, and tetanus prophylaxis [5]. Topical applications, such as silver sulfadiazine, silver nitrate gel/solution, and fusidic acid, form the foundation of burn wound care. Dermatitis, renal failure, wound infection, and pneumonia are early complications, while scarring and contractures are late complications [6] Even after overcoming these early complications of burns with the utmost emergency care, the late complications remain. Acute respiratory distress syndrome and septicemia are the most challenging aspects of treating burn cases.
Burn injuries are discussed under Dagdhavrana in Ayurveda. The classification of burn injuries and treatment by Acharya Susrutha can be closely related to the degree of burn in modern science, with terms like Plushta (first-degree burn), Durdagdha (second-degree partial thickness burn), Samyakdagdha (second-degree full-thickness burns), and Atidagdha (third-degree burn, involving muscle and joints) [7]. Sixty therapeutic procedures are explained in the Ayurvedic classics for the management of wounds. Dressing of the burn wound with medicated ghee preparations and bandaging with Tinospora cordifolia leaves, as well as wound fumigation with medicinal drugs, were important treatments considered under local wound care [8]. Oral medicines like triphala guggulu, punernava mandoor, punernavadi kashaya, etc. were advised in the management of various symptoms of burn wounds.
Here, we report a case of accidental burn injury which was managed effectively with integrated approach, i.e., Ayurvedic and modern medicine treatment principles.
2. Patient information and clinical findings
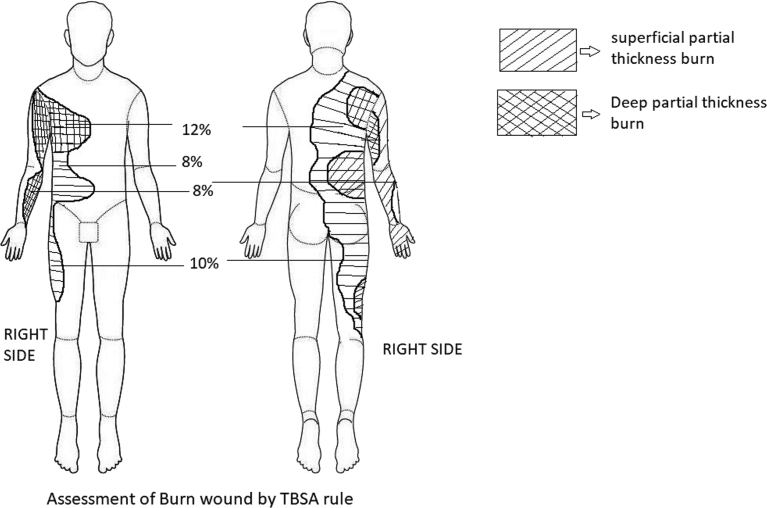
A 44-year-old female presented with burns over: the whole of the posterior side of the right arm; the whole right forearm with hand; more than two-thirds of the back; the right lateral sides of the chest and abdomen; part of the lower chest and upper abdomen over the anterior trunk; and the posterior and lateral areas of the right thigh with the right hip (Fig. 1, Fig. 2).
Fig. 1.
Assessment of burn wound.
Fig. 2.
Initial stage(A)(B)(C).
The incident was caused by the flame from a gas explosion while cooking. For five days, the patient was treated conservatively at an Modern medicine hospital, receiving intravenous antibiotics and anti-inflammatory drugs as well as wound care (application of Silverex ointment) (Table 1). She was discharged as her complaints had subsided and was advised to rest at home. She approached our hospital as symptoms like fever and intense pain at the burn site were aggravated due to a lack of definitive care and negligence by the patient. The general examination revealed that she was moderately built and well-nourished. The systemic examination revealed that she was conscious, well-oriented, and without any co-morbidities. Her vital signs showed a pulse rate of 108 beats per minute, blood pressure of 100/70 mm of Hg, a respiratory rate of 24 per minute, and a body temperature of 99.8 °F. The local examination revealed second-degree partial-thickness burns on the posterior side of the right arm (centre with red, white, and eschar) and first-degree burns (periphery with pink color) over the right forearm and hand. Second-degree partial-thickness burns (red, white, and eschar) were seen over the scapular region and first-degree burns (pink color) on more than two-thirds of the back. Second-degree partial-thickness burns were seen from the right axillary region to the right hip, which are second-degree partial-thickness burns seen on the lower chest and upper abdomen over the anterior trunk. A second-degree partial-thickness burn was seen in the posterior and lateral areas of the right thigh. The haematology and urine reports revealed haemoglobin of 9.2 gm%, WBC count of 13,700 cells/cumm, Neutrophils - 58%, Lymphocytes - 28%, Eosinophil −12%, and Monocytes - 2%, ESR of 160 mm/hr, Platelet count of 428,000 cells/cumm, BT - 3 min, CT - 6 min, RBS 184 mg/dl, blood urea 18 mg/dl, serum creatinine 0.9 mg/dl, and RBC count of 3.57 million/cumm. The patient was catheterized to observe the urine output.
Table 1.
Time line
| 25/03/2021 | Patient met with accidental burn injury and received emergency care in modern hospital. |
| 1/4/2021 | Symptoms aggravated due to lack of definitive care and negligence by the patient. |
| 04/04/2021 to 31/05/2021 | Integrated approach (Ayurveda and Modern medicine) was initiated and patient responded well with treatment. |
2.1. Diagnosis
The diagnosis was established based on the signs, symptoms, and clinical examination. It was diagnosed as an accidental burn injury with a TBSA of 27% for the first degree (superficial with a pink colour appearance) and 15% for the second degree (deep partial-thickness burn with eschar) burn. In Ayurveda, it was diagnosed as Plushta and Durdagdha, and treatment was planned accordingly.
2.2. Therapeutic intervention
The treatment protocol was designed with an integrated approach, i.e., Modern medicine and Ayurveda. The prognosis and probable complications, risks were informed to the patient and their relatives; later, treatment was initiated after obtaining high-risk consent. The patient was initially treated by a modern medicine specialist with standard treatments like fluid therapy, intravenous antibiotics, and anti-inflammatory drugs. According to the “4-2-1″ fluid replacement rule, the fluid requirement was 2400 ml. As the patient was taking fluids orally (1500 ml), a 900 ml fluid deficit was present, and it was substituted by 1000 ml of crystalloids (900 ml replacement + 100 ml to overcome insensible loss) [9].
Local burn wound care was done with ropana ghrita application over the burn site followed by bandaging with T. cordifolia leaves (Fig. 3) twice daily. As a measure for infection control, fumigation was done twice daily at the burn site and the patient's room with powders of medicinal drugs like Commifora mukul, Neem leaves, etc. The therapeutic interventions and oral medications are highlighted in Table 2 and the assessment of wound healing (with the “Bates-Jensen wound assessment tool”) are shown in Table 3 [10].
Fig. 3.
Ropana ghrita application with Patraadaana(A)(B)(C).
Table 2.
Therapeutic intervention and oral medicine
| Sl No | Plan of care | Procedure | Duration(Days) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 5-10 | 10-15 | 15-20 | 20-25 | Follow up |
|||||
| 25-35 | 35-45 | 45-60 | |||||||
| 01 | Modern medicine | IV Antibiotics like Injection Odicef-S (ceftriaxone with sulbactum) 1.5 grams Intravenous twice daily Intravenous metronidazole 100 millilitre thrice daily Injection Gentamycin 80 milligrams Intravenous twice daily |
✓ ✓ |
✓ | |||||
| 02 | Intravenous (IV) fluids | IV fluids like Dextrose Normal Saline (DNS), Ringer Lactate (RL) -1500 millilitre/day Tab Paracetamol 500 mg SOS |
✓ | ||||||
| Ayurveda management (Internal) | |||||||||
| 01 | Tab.Triphalaguggulu | 250 milligrams two times daily after food | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 02 | Tab.Punarnavamandoora | 250 milligrams two times daily after food | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 03 | Punarnavadi kashaya | 10 millilitre thrice daily after foodwith warm water | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 04 | Tab Chandrakala rasa | 250 milligrams two times daily after food | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 05 | Tab Kamadugha with mukta | 250 milligrams two times daily after food | ✓ | ✓ | ✓ | ||||
| Wound Care (External) | |||||||||
| 06 | a) Wound healing | Ropaha ghrita application followed with tinospora cordifolia leaves bandage twice daily | ✓ ✓ |
✓ ✓ |
✓ ✓ |
✓ ✓ |
✓ | ✓ | ✓ |
| b) Fumigation | Twice daily | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
Table 3.
Assessment of wound healing
| 1st day | 10th day | 20th day | 25th day | 35th day | 45th day | 60th day | ||
|---|---|---|---|---|---|---|---|---|
| Pain (VAS) | 10 | 7 | 4 | 2 | 1 | – | – | |
| Total body surface area (TBSA) RULE | Anterior trunk | 08% | 08% | 6% | 3% | 2% | – | – |
| Posterior trunk | 12% | 12% | 6% | 3% | 2% | – | – | |
| Right upper limb | 8% | 8% | 4% | 3% | 2% | – | – | |
| Right lower limb | 10% | 10% | 5% | 3% | 2% | – | – | |
| Floor | Anterior trunk | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Mild slough with#RGT | #RGT | ∗ES | ∗ES |
| Posterior trunk | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Mild slough with #RGT | #RGT | ∗ES | ∗ES | |
| Right upper limb | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Mild slough with #RGT | #RGT | ∗ES | ∗ES | |
| Right lower limb | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Yellow slough with centralized Eschar | Mild slough with #RGT | #RGT | ∗ES | ∗ES | |
| Discharge | Anterior trunk | Purulent | Serous | Serous | – | – | – | – |
| Posterior trunk | Purulent | Serous | Serous | – | – | – | – | |
| Right upper limb | Purulent | Serous | Serous | – | – | – | – | |
| Right lower limb | Purulent | Serous | Serous | – | – | – | – | |
| Granulation tissue | Anterior trunk | – | No granulation tissue | No granulation tissue | #RGT | #RGT | – | – |
| Posterior trunk | – | No granulation tissue | No granulation tissue | #RGT | #RGT | – | – | |
| Right upper limb | – | No granulation tissue | No granulation tissue | #RGT | #RGT | – | – | |
| Right lower limb | – | No granulation tissue | No granulation tissue | #RGT | #RGT | – | – | |
| Epithelialisation | Anterior trunk | – | – | No epithelialisation | No epithelialisation | No epithelialisation | ∗ES | ∗ES |
| Posterior trunk | – | – | No epithelialisation | No epithelialisation | No epithelialisation | ∗ES | ∗ES | |
| Right upper limb | – | – | No epithelialisation | No epithelialisation | No epithelialisation | ∗ES | ∗ES | |
| Right lower limb | – | – | No epithelialisation | No epithelialisation | No epithelialisation | ∗ES | ∗ES |
VAS- Visual analogue scale, #RGT –Red granulation tissue, ∗ES – Epithelialisation.
2.3. Follow up and outcome
The patient was admitted for a period of 25 days and advised to continue the same oral medications after discharge, along with the Ropana ghrita application. The drugs for fumigation were given to the patient and she was instructed to continue at home. The patient was advised to perform the movements of affected joints in order to prevent contracture and asked to visit the hospital every 10th day for assessing the changes in the wound. The wound healed completely (Fig. 4) with mild contracture (at the wrist joint, elbow joint, and axilla, where the second-degree partial-thickness burns were present) after 60 days of treatment. The patient is now able to perform her routine activities without any discomfort.
Fig. 4.
60 th day after treatment(A)(B)(C).
3. Discussion
Burn injury management is a difficult task as it causes significant pain and disability to the victims. These injuries requires proper wound care as they are more susceptible to infection. Long-term heat/temperature exposure causes tissue damage and protein denaturation, resulting in the release of toxic metabolites that cause localized oedema and a systemic inflammatory response [11]. The prime concern in burn injury management is late complications like scarring, pigmentation, contractures, and keloid formation, so the process of wound healing and the final outcome of this process are entirely dependent on how it is managed throughout the stages of wound healing.
The treatment principles are designed by analyzing the degree of burn and its systemic effect on the body. Initially, the case was managed with standard treatment protocol, i.e., intravenous fluid resuscitation, broad-spectrum antibiotics, anti-inflammatory drugs, and analgesics.
The present case was treated as per the Plushta and Durdagdha lines of management, which highlights, external treatment modalities like application of medicated ghee, Covering the wound area with Tinospora cordifilia leaves, wound fumigation, andoral medications. The medicines used for topical application should possess properties like good tissue penetration, debridement property, antimicrobial, anti-inflammatory, and provide a moist environment for faster wound healing [12].
Ropana ghrita was used as an external application in the wound management because it contains ingredients like Madhuchista (beeswax), Madhuka (Madhuca indica Linn), Lodhra (Symplocos racemosa Linn), Sarjarasa (Vateria indica Linn), Manjistha (Rubia cordifolia Linn), Chandana (Santalum album Linn), Murva (Morus alba Linn), Go-Ghrita (Cow's ghee) [13]. The formulation possess properties like wound healing, increase complexion, Twachya (good for skin), Raktaprasadana (blood nourishment), Sheeta (cold potency), Lekhana (scraping), Jantughna (antimicrobial), etc which helps in the wound healing process. The Go ghrita possesses Rakshoghna (anti-microbial and anti-fungal), Vranashodhana (wound cleansing), Vranaropana, and Vata pitta shamaka (pacifies Vata and pitta dosha) properties with its madhura vipaka. This also helps in lubricating the wound surface and prevents eschar formation, as well as insensible loss of fluid from the burn site [14]. Manjishta is another content, which has active phytochemicals like amino acids, saponin, carbohydrates, alkaloids, glycosides, phenolic compounds, and tannins. It functions as an antitoxic, blood detoxifying, antiseptic, and antioxidant agent [15].
Patraadaana has been the subject of numerous studies, including lotus leaves as an alternative dressing material [16], banana leaves in secondary burn wounds, etc [17]. These studies show that the non-adherent, waxy, and cool properties of the leaves provide a healthy platform for proper and faster-wound healing [16,17]. Guduchi (T. cordifolia, Linn) leaves are used in a wound indicated in Pitta and Rakta dosha predominant condition. The application of leaves for wound covering helps in the reduction of burning sensation and accelerates wound healing. In this study, the Guduchi leaves were applied over burn wounds after the application of Ropanaghrita. The waxy surface of the leaves has non-adherent properties, doesn't interfere with the intact epithelial tissue bed, and a provide moist wound environment thus facilitating wound healing [18].
The Triphala guggulu possesses the properties like scraping, anti-inflammatory and wound healing properties. Active phytochemicals in this formulation include glycosides, amino acids, flavonoids, tannin, steroids, protein, carbohydrates, and saponin [19]. Triphala inhibits both gram-positive and gram-negative bacteria growth [20]. Study on Triphala showed a decrease in the bacterial count in granulation tissue and an increase in collagen [21]. Increased epigallocate chingallate interaction with collagen contributes to increased tissue regeneration and hastens wound closure[22].
Kamadugha with Mukta was administered due to its properties like Jantughna, raktaprasadana, kandugna, raktasthambaka (coagulative), and rasayana (rejuvinative). Kamadugharasa is a kharaliya preparation (classical method of drug preparation) with Kshara nature (alkaline nature), which contains the ingredients like Pravala (coral calx) and Mukta (pearl calcium). These ingredients possess Deepana (appetizer) and Pachana (digestive) properties which helps in Vranaropana. The preparation contains mostly the Sheeta (cold) Virya (potency) drugs, thus doing the Pitta-shamana, and helps in wound healing. Kamadugha rasa contains elements like sodium, iron, aluminum, potassium, and other essential minerals for a healthy body [23].
Punarnava Mandura contains mainly Pippali, which has Agni Deepaka, Pachana, Vataanulomaka (pacifies Vata), and Rasayana properties [24]. Mandura Bhasma (calx of iron rust) is raktavridhikara (improves hemoglobin). Amalaki (Emblica officinalis) is another ingredient that helps in the absorption of iron, thus helping in blood circulation. Punarnavamandoora is the best choice for oral iron therapy [25].
Chandrakala rasa contains vangabhasma, lauhabhasma, rasa sindhoora, and abhrakabhasmawhich acts on Baahya-abhyantaradaha (internal and external burning sensation), Brama (giddiness), Murcha (unconsciousness), Raktapitta (bleeding disorder), etc [26].
Punarnavadi Kashaya possesses Laghu guna (lightness), Katu rasa (spicy), and Ushna virya (hot potency) which does Amapachana (improves indigestion), Kledaghana (reduces putrefaction) and reduces shotha (inflammation) [27]. The Punarnava (Boerhavia diffusa Linn) acts as an excellent anti-inflammatory and diuretic [28].
Wound fumigation is explained in the classics as Rakshognavidhi (anti-microbial/anti-fungal etc.) in Janapadodhwamsa vyadhis (communicable diseases), and Vranachikitsa (wound management) [29]. Direct reference in the classics regarding use of fumigation in burn injuries are not available, but cross-references to protect wounded from various entities are available. Various treatments are advised to protect the wounded person and the wound, among which fumigation is one. In this case, the Dhoopana karma was done with Nimba (Azadirachta indica), Guggulu (Commiphora wightii), Ushira (Vitiveria zizanioides), Vacha (Acorus calamus), Sarsapa (Brassica campestris), and cow ghee [29]. Neem has a very high sensitivity towards Streptococcus pyogenes and Staphylococcus aureus. The Krimighna, Kandughna and kushtagna properties of the drugs helped in wound healing and also prevented secondary infections [30].
Burn care demands extended hospitalization, which might be the major source of secondary infections [31]. This integrated approach accelerated wound healing and thereby shortened hospital stay; further research in this approach is necessary to provide evidence based results.
4. Conclusion
Burn management is a challenging task; even after complete recovery complications such as contractures, discoloration and keloid formation occur invariably. The present case was successfully treated with an integrated approach, i.e. Ayurveda and Modern medicine. The wound healed completely within 60 days of the treatment. The integrated approach minimized the hospital stay, contracture and enhanced the wound healing process with minimal discoloration. Ayurvedic procedures such as fumigation, medicated ghee application, and Tinospora leaves bandaging has given promising results in the burn wound healing. It was a single case study; further research in this field is essential with inclusion of larger samples.
Informed consent
The informed consent regarding documentation and publication of the case was obtained from the patient.
Patient perspectives
The patient was satisfied and pleased with the care which was provided in the hospital. She is now able to perform her routine activities without discomfort.
Funding
Nil.
Authors contribution statement
Dr Pradeep S Shindhe, Dr Ramesh S Killedar carried out the clinical study and treated the patient. Data acquisition, documentation was done by Dr Priyanka K, Dr. Dhrushnu Prasannan, Dr Kirthi A. Manuscript was drafted by Dr Pradeep S Shindhe, Dr Ramesh Killedar, DrPriyanka. Manuscript editing and reviewing was done by Dr Pradeep S Shindhe, Dr Ramesh Killedar. All the authors are guarantors for the publication and data integrity.
Declaration of Competing Interest
Nil.
Acknowledgement
Dr Suhaskumar Shetty, Principal and Medical director, KAHER's Shri B. M K. Ayurveda Mahavidyalaya and Hospital, Belagavi.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Das S. SD publications; 13,old mayor’s court Kolkata: 2020. A concise textbook of surgery Burns; p. 61. [Google Scholar]
- 2.Park J. 24th ed. M/S Banarasidas Bhanot; India: 2017. Park's Text book of preventive and social medicine; p. 428. [Google Scholar]
- 3.Gupta J.L., Makhija L.K., Bajaj S.P. National programme for prevention of burn injuries. Indian J Plast Surg. 2010 Sep;43(Suppl):S6–S10. doi: 10.4103/0970-0358.70716. PMID: 21321659; PMCID: PMC3038407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schaefer Timothy j, Szymanski Kiran D. Stat pearls. Stat Pearls Publishing; Treasure Island (FL): 2021 Aug 11. Burn evaluation and management.https://pubmed.ncbi.nlm.nih.gov/28613492/ [Internet] 2022 Jan–. PMID: 28613492. [Google Scholar]
- 5.Jeschke M.G., van Baar M.E., Choudhry M.A., Chung K.K., Gibran N.S., Logsetty S. Burn injury. Nat Rev Dis Prim. 2020 Feb 13;6(1):11. doi: 10.1038/s41572-020-0145-5. PMID: 32054846; PMCID: PMC7224101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajgopalshenoy K., Shenoy Anita. CBS publishers and distributors; New delhi: 2020. Manipal manual of surgery; pp. 210–217. [Google Scholar]
- 7.Vaidya Jadavji Trikamji Acharya and Narayan Ram Acharya Kavyatirtha. Susrut samhita of susruta. Varanasi. Choukhambha Sanskrit Sansthan. 2012. sutrasthana12/16–26 P.52-53.
- 8.Vaidya JadavjiTrikamji Acharya and Narayan Ram Acharya Kavyatirtha. Susrutsamhita of Susruta. Varanasi. Choukhambha Sanskrit Sansthan. 2012.Chikitsa sthana 1/8 p. 397.
- 9.Castera M.R., Borhade M.B. StatPearls. StatPearls Publishing; Treasure Island (FL): 2022 Jan. Fluid Management. [Updated 2021 Sep 8]https://www.ncbi.nlm.nih.gov/books/NBK532305 [Internet] Available from: [PubMed] [Google Scholar]
- 10.Bates-Jensen B.M., McCreath H.E., Harputlu D., Patlan A. Reliability of the Bates-Jensen wound assessment tool for pressure injury assessment: the pressure ulcer detection study. Wound Repair Regen. 2019 Jul;27(4):386–395. doi: 10.1111/wrr.12714. Epub 2019 Mar 18. PMID: 30828890; PMCID: PMC6693585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laycock H., Valente J., Bantel, Nagy I. Peripheral mechanisms of burn injury- associated pain. Eur J Pharmacol. 2013;716(1–3):169–178. doi: 10.1016/j.ejphar.2013.01.071. Epub 2013 Mar 13. PMID: 23500208. [DOI] [PubMed] [Google Scholar]
- 12.Dai T., Huang Y.Y., Sharma S.K., Hashmi J.T., Kurup D.B., Hamblin M.R. Topical antimicrobials for burn wound infections. Recent Pat Anti-Infect Drug Discov. 2010 Jun;5(2):124–151. doi: 10.2174/157489110791233522. PMID: 20429870; PMCID: PMC2935806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vaidya Jadavji Trikamji Acharya and Narayan Ram Acharya Kavyatirtha. Susrut samhita of susruta. Varanasi. Choukhambha Sanskrit Sansthan. 2012.sutrasthana12/27, Pg.54.
- 14.Udwadia T.E. Ghee and honey dressing for infected wounds. Indian J Surg. 2011 Aug;73(4):278–283. doi: 10.1007/s12262-011-0240-7. Epub 2011 Apr 6. PMID: 22851841; PMCID: PMC3144338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chandrashekar B.S., Prabhakara S., Mohan T., Shabeer D., Bhandare B., Nalini M., et al. Characterization of Rubia cordifolia L. root extract and its evaluation of cardioprotective effect in Wistar rat model. Indian J Pharmacol. 2018 Jan-Feb;50(1):12–21. doi: 10.4103/ijp.IJP_418_17. doi: 10.4103/ijp.IJP_418_17. PMID: 29861523; PMCID: PMC5954628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okur M.E., Karantas I.D., Şenyiğit Z., Üstündağ Okur N., Siafaka P.I. Recent trends on wound management: new therapeutic choices based on polymeric carriers. Asian J Pharm Sci. 2020 Nov;15(6):661–684. doi: 10.1016/j.ajps.2019.11.008. Epub 2020 Jan 23. PMID: 33363624; PMCID: PMC7750807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gore Madhuri A., Akolekar Deepika. Evaluation of banana leaf dressing for partial thickness burn wounds. Burns. 2003;29(5):487–492. doi: 10.1016/s0305-4179(03)00050-0. PMID: 12880731. [DOI] [PubMed] [Google Scholar]
- 18.Vaidya Jadavji Trikamji Acharya and Narayan Ram Acharya Kavyatirtha. Susrutsamhita of susruta. Varanasi. Choukhambha Sanskrit Sansthan. 2012.chikitsasthana 1/112–118,pg 406.
- 19.Savarikar S.S., Barbhind M.M., Halde U.K., Kulkarni A.P. Pharmaceutical and analytical evaluation of triphalaguggulkalpa tablets. J Ayurveda Integr Med. 2011 Jan;2(1):21–25. doi: 10.4103/0975-9476.78187. PMID: 21731383; PMCID: PMC3121249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Biradar Y.S., Jagatap S., Khandelwal K.R., Singhania S.S. Exploring of antimicrobial activity of triphala mashi-an ayurvedic formulation. Evid Based Complement Alternat Med. 2008;5(1):107–113. doi: 10.1093/ecam/nem002. PMID: 18317557; PMCID: PMC2249739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar M.S., Kirubanandan S., Sripriya R., Sehgal P.K. Triphala promotes healing of infected full-thickness dermal wound. J Surg Res. 2008 Jan;144(1):94–101. doi: 10.1016/j.jss.2007.02.049. Epub 2007 Jul 27. PMID: 17662304. [DOI] [PubMed] [Google Scholar]
- 22.Kumar M.S., Kirubanandan S., Sripriya R., Sehgal P.K. Triphala incorporated collagen sponge--a smart biomaterial for infected dermal wound healing. J Surg Res. 2010 Jan;158(1):162–170. doi: 10.1016/j.jss.2008.07.006. PMID: 19118845. [DOI] [PubMed] [Google Scholar]
- 23.Meenakshi K., Vinteshwari N., Minaxi J., Vartika S. Effectiveness of Ayurveda treatment in urdhwaga amlapitta: a clinical evaluation. J Ayurveda Integr Med. 2021 Jan-Mar;12(1):87–92. doi: 10.1016/j.jaim.2020.12.004. Epub 2021 Feb 3. PMID: 33546994; PMCID: PMC8039346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pandya M.G., Dave A.R. A clinical study of Punarnava Mandura in the management of Pandu Roga in old age (geriatric anemia) Ayu. 2014 Jul-Sep;35(3):252–260. doi: 10.4103/0974-8520.153735. PMID: 26664234; PMCID: PMC4649575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rasheed A., Naik M., Mohammed-Haneefa K.P., Arun-Kumar R.P., Azeem A.K. Formulation, characterization and comparative evaluation of Trivangabhasma: a herbo-mineral Indian traditional medicine. Pak J Pharm Sci. 2014 Jul;27(4):793–800. PMID: 25015442. [PubMed] [Google Scholar]
- 26.Vaidya yadavji trikamjiacharya, sidhayogasangraha. Chaukamba publications; New Delhi: 2008. p. 96. [Google Scholar]
- 27.Sharma S. Meherchand Lachmidas Publications; New Delhi: 2000. Chakradatta of chakrapani, shotha chikitsa; p. 254. Ch. 43. vol. 10. [Google Scholar]
- 28.Mishra S., Aeri V., Gaur P.K., Jachak S.M. Phytochemical, therapeutic, and ethnopharmacological overview for a traditionally important herb: boerhavia diffusa Linn. BioMed Res Int. 2014;2014 doi: 10.1155/2014/808302. Epub 2014 May 14. PMID: 24949473; PMCID: PMC4053255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaidya Jadavji Trikamji Acharya, Narayan Ram Acharya Kavyatirtha. Commentary nibandhasangraha of sri dalhanacharya on susrutasamhita of susruta, Sutrasthana: [Chapter 5], verse19-32. Chikitsasthana: [Chapter 1],verse 80, Susruta samhita sutrasthana19/28, Varanasi:Chaukhamba Surbharati Prakashan, 2012, 21.
- 30.Balkrishna A., Yagyadev S., Vipradev S., Singh K., Varshney Y., Rastogi S., et al. Vishaghn dhoop, nano-scale particles with detoxifying medicinal fume, exhibits robust anti-microbial activities: implications of disinfection potentials of a traditional ayurvedic air sterilization technique. J Evid Based Integr Med. 2022 Jan-Dec doi: 10.1177/2515690X211068832. 27:2515690X211068832. PMID: 34985370; PMCID: PMC8744077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Onah C.N., Allmendinger R., Handl J., Dunn K.W. Surviving burn injury: drivers of length of hospital stay. Int J Environ Res Publ Health. 2021 Jan 18;18(2):761. doi: 10.3390/ijerph18020761. PMID: 33477442; PMCID: PMC7829802. [DOI] [PMC free article] [PubMed] [Google Scholar]