Abstract
Background
Parafunctional forces are a potential risk factor for implant-related complications. This study aimed to evaluate the possible relationship of bruxism with implant-related complications and marginal bone loss (MBL).
Methods
In this prospective cohort study, patients were divided into two groups with and without bruxism, and received single-tooth implants in the posterior mandible. Patients in the bruxer group were requested to use a customized fabricated night guard. Bone quality was also assessed based on CBCT scans. The MBL, crown detachment, and porcelain fracture were evaluated, and clinical assessments were made at the 12-month follow-up.
Results
Seventy patients were studied in two groups (n = 35 in each group). None of the implants in any of the two groups showed pain, sensitivity, suppuration, exudation, clinically detectable mobility, or peri-implant radiolucency. No significant difference was observed between the two groups in the mean MBL at the 12-month follow-up (p = 0.60). Regarding bone quality, there was no significant difference in the mean MBL among different types of bone qualities (p = 0.66). There were no significant differences regarding crown detachment and porcelain fracture between the two groups either (p = 0.32 and p = 0.30, respectively).
Conclusion
According to the results of this study, dental implant treatment according to the suggested protocol in bruxers yielded promising outcomes.
Keywords: Bruxism, Dental implants, Marginal bone loss
Introduction
Dental implants are the gold standard for replacement of the missing teeth in partially and completely edentulous patients. Despite their increasing application and popularity, complications and failures are still common. Only two-thirds of patients undergoing dental implant treatment are entirely free from any complications [1, 2]. Complications that occur following dental implant treatment can be divided into two main groups of biological and mechanical. These complications are related to several risk factors. Inappropriate occlusal forces are among the main factors contributing to excessive stress applied to the implant and the bone-implant interference, leading to both mechanical and biological complications due to implant overload, and failure [3]. Bruxism, as a movement disorder of the masticatory system, can generate and apply parafunctional forces to dental implants. It is usually characterized by tooth grinding or clenching and thrusting of the mandible that lead to nonfunctional contacts between the mandibular and maxillary teeth, causing damage to the stomatognathic structures. The prevalence of bruxism in the adult population is about 10%. Considering its relatively high prevalence in the general population, use of implant-supported restorations is inevitable in patients with parafunctional habits [2, 4, 5]. According to some recent studies, bruxism is a potential risk factor for both mechanical and biological implant-related complications. However, the role of bruxism in development of implant complications or failure remains controversial. To the best of our knowledge, most of the causal relationships suggested between bruxism and implant failure, or its consideration as a contraindication for dental implantation are based on expert opinions and clinical experiences [6–8].
Considering the most acceptable guidelines regarding implant treatment in patients with bruxism, this study aimed to evaluate the possible relationship of bruxism with implant-related complications and marginal bone loss (MBL). Moreover, this study aimed to suggest a safe protocol regarding implant-supported prosthetic rehabilitation in bruxers to prevent the potential risk factors for implant overload and failure.
Materials and Methods
This prospective cohort study evaluated patients referred to the Department of Oral and Maxillofacial Surgery of Shahid Beheshti University of Medical Sciences between September 1, 2017 and December 28, 2019 for implant treatment. All treatments were carried out by the same practitioner. Patients aged > 18 years with good oral hygiene and no systemic disease (ASA I and ASA II) who required single tooth implants in the posterior mandible (at the site of first and second molars) to achieve occlusal contacts were included in this study. The exclusion criteria were concomitant TMJ disorders, systemic diseases such as uncontrolled diabetes mellitus and autoimmune disorders, poor oral hygiene, active periodontal infection, requiring or having a history of bone augmentation procedures, use of medications affecting the bone metabolism, cyclobenzaprine or benzodiazepine muscle relaxants, and tricyclic antidepressants, smoking, not showing up for the follow-ups, or unwillingness for participation in the study. The patients were divided into two groups of bruxers (group 1) and non-bruxers (group 2). Patients with clenching or grinding of the teeth and/or bracing or thrusting of the mandible and tooth surface abrasion or abfraction were diagnosed as bruxers. Demographic information, including age and gender of patients, was collected. The study design and objectives were explained to all participants, and written informed consent was obtained from them. This study was performed according to the principles outlined by the World Medical Association’s Declaration of Helsinki on experimentation involving human subjects, as revised in 2000. The protocol of the study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (code: IR.SBMU.DRC.REC.1398.009).
Complete clinical examination of oral soft and hard tissues was performed for all patients. Panoramic radiographs were obtained for primary radiographic examination. A cone-beam computed tomography (CBCT) scan of the implant region was also requested to assess the bone width and bone quality at the implant site and ridge angulation. NewTom VGi CBCT unit (QR SRL Company, Verona, Italy) was used for all CBCT scans. Scans analysis were done using NewTom NNT viewer version 5.3 software (Quantitative Radiology, Verona, Italy). CBCT scan’s parameters were 8 × 12 cm field of view (FOV) and 200 µm voxel size. An oral and maxillofacial surgeon and a radiologist determined the bone quality in each implant area according to the Lekholm and Zarb classification [9].
Implant Placement
All patients received prophylactic antibiotics (2 g amoxicillin) 1 h before surgery and rinsed their mouth with 0.2% chlorhexidine mouthwash. All dental implants were placed by elevating a full-thickness flap through a crestal incision. Two short releasing incisions were made at the mesial and distal aspects of the crestal incision. The implant sites were prepared using twisting drills with increasing diameter. Next, 4-mm and 4.8-mm diameter implants with 10 mm length (Straumann® fixture, RN) were placed for all patients. All implants were placed with good primary stability. Finally, the flap was sutured with 4–0 Vicryl sutures (Ethicon Inc., Johnson & Johnson Company, Somerville, NJ, USA). Postoperative antibiotics were not administered for the patients, and the patients were only instructed to use 0.2% chlorhexidine mouthwash for 7 days.
Implant Loading
All implants were loaded 3 months after placement. All restorations were metal-ceramic single crowns. The crowns were cemented with temporary cement (Temp-Bond ®; Kerr, Orange, CA, USA). Optimal occlusion was carefully ensured on an articulator and intraorally for all restorations. Customized night guards were fabricated for each patient individually in the bruxer group. They were instructed to use the splint, at least eight hours a day, especially overnight.
Clinical, Radiographic and Prosthetic Evaluations
The implants were evaluated for presence or absence of pain or sensitivity, suppuration or exudation, clinically detectable mobility, and peri-implant radiolucency on periapical radiographs. Intraoral periapical radiographs were obtained immediately after implant loading (T0), and 12 months (T1) later in the recall sessions. A long-cone paralleling technique was used to evaluate the bone resorption and MBL at the mesial and distal surfaces of the implants. Radiographs were taken in a reproducible manner using an individual Rinn alignment system (Rinn ®; Dentsply, Elgin, IL, USA) and a customized positioner, which was fabricated with polyvinyl siloxane impression material (Polyvinylsiloxane, Kerr, Germany) for each patient. The same exposure settings (70 kV, 8 mA, and 0.08 s time) were applied for both imaging sessions. Radiographs were obtained using Digora-fmx scanner with blue plates (Soredex, Helsinki, Finland). The distance from the tube to the tooth was 32 cm while the distance between the tooth and receptor was 2 cm. Digora® for windows version 2.8 was used for image processing. An oral and maxillofacial radiologist interpreted the images. To assess the MBL over time, the vertical distance between the implant shoulder and the alveolar crest was measured at the mesial and distal surfaces of each implant (Fig. 1), and the mean value was calculated for each radiograph. The bone level at the time of implant loading was considered as the baseline value for evaluation of MBL. Dimensional distortion was considered in measurements and corrected by comparing the true implant length and the apparent length of the implant on radiographs using the following equation:
Fig.1.
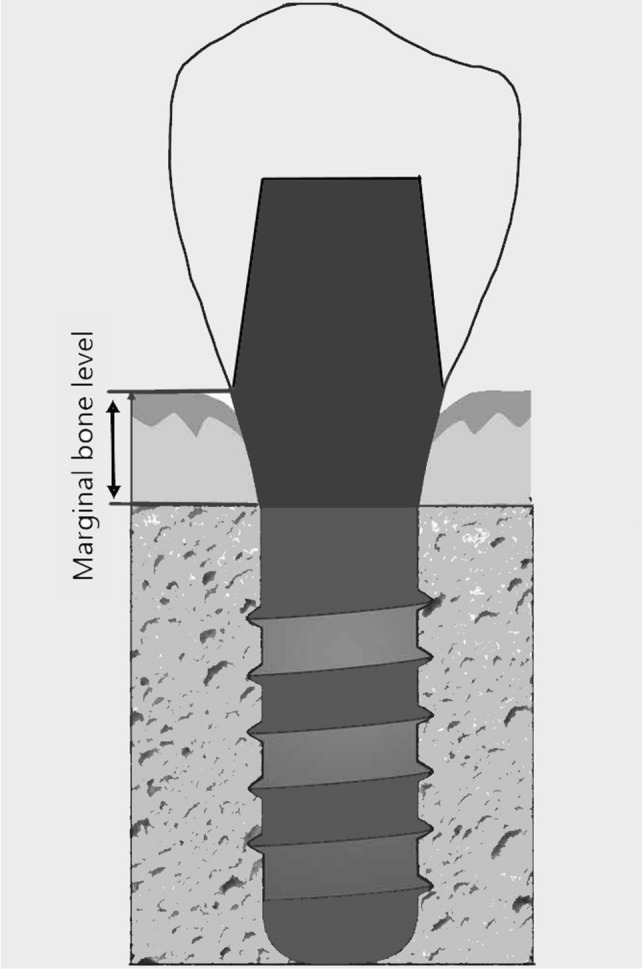
Measuring marginal bone level (MBL) in periapical radiographs
Statistical Analysis
The statistical analyses were performed using SPSS version 23 (SPSS Inc., IL, USA). The independent t-test was used to compare the mean age and MBL between the two groups. The mean MBL was also compared between types of bone qualities using the independent t-test. The Chi-square test was applied to compare gender distribution, location, bone quality, frequency of crown detachment, and porcelain fracture between the two groups. P-value < 0.05 was considered statistically significant.
Results
Thirty-five patients in the bruxer group (group 1) and 35 patients in the non-bruxer group (group 2) were evaluated. There were 21 males and 14 females in each of the two groups. The mean age of patients was 40.60 ± 8.79 years in the bruxer group and 38.22 ± 9.06 years in the non-bruxer group. The analysis showed no significant difference between the two groups (p = 0.86). In the first group, 23 implants were placed in the first molar region and 12 implants in the second molar region while in the second group, 22 implants were placed in the first molar region and 13 implants in the second molar region. Among four types of bone quality according to the Lekholm and Zarb classification, 16 implants were loaded in D2 bone quality and 19 implants were loaded in D3 bone in the first group, where as in the second group, 15 implants were loaded in D2 and 20 implants were loaded in D3 bone. No significant differences were observed between the two groups regarding implant location (p = 0.80) and bone quality (p = 0.81).
None of the implants in any of the two groups showed pain, sensitivity, suppuration, exudation, or clinically detectable mobility. No peri-implant radiolucency was detected on periapical radiographs.
The mean MBL at 12 months after implant loading was 0.86 ± 0.18 mm in group 1 and 0.79 ± 0.22 mm in group 2. No significant difference was observed between the two groups in the mean MBL during this time period (p = 0.60, Table 1).
Table 1.
Mean marginal bone loss (MBL) at the 12-month follow-up in the bruxer and non-bruxer groups (n = 35)
| Group | Mean MBL1 ± SD2 | Independent t-test |
|---|---|---|
| Bruxer group | 0.86 ± 0.18 | p = 0.60 |
| Non-bruxer group | 0.79 ± 0.22 |
1MBL Marginal bone loss, 2SD Standard deviation
Regarding bone quality, implants loaded in the D2 group showed 0.84 ± 0.22 mm MBL at 12 months after implant loading and in the D3 group, 0.82 ± 19 mm MBL was observed. There was no significant difference in the mean MBL among different types of bone qualities (p = 0.66).
Table 2 presents the frequency of crown detachment and porcelain fracture. There were no significant differences regarding these two variables between the two groups (p > 0.05, Table 2, Fig. 2).
Table 2.
Frequency of crown detachment and porcelain fracture at the 12-month follow-up in the bruxer and non-bruxer groups
| Bruxer group | Non- bruxer group | p value | ||
|---|---|---|---|---|
| Crown detachment | Yes | 7 | 4 | 0.32 |
| No | 28 | 31 | ||
| Porcelain fracture | Yes | 3 | 1 | 0.30 |
| No | 32 | 34 | ||
Fig. 2.
Clinical image of the patient who had crown fracture, a before loading, b immediately after loading, c 12 months after loading
Discussion
Parafunctional stresses applied to teeth in bruxers may cause various complications such as occlusal wear, dental fractures, temporomandibular disorders and pain. Application of excessive or abnormal occlusal forces to implants may lead to both biological and mechanical complications. In some clinical experiences, bruxism is even considered as a contraindication for implant placement. Due to the limited number of published studies and the gap of information about the effects of bruxism on dental implants, guidelines for the management of bruxer patients are mainly based on clinical experience and expert opinion with insufficient level of evidence [2, 6, 7, 10]. Thus, the effect of parafunctional forces on dental implants remains a controversial topic. Mangano et al. [11] reported an actual cumulative implant success rate in patients with and without parafunctional habits following placement of short implants supporting single crowns in the posterior regions after 10 years of follow-up. In contrast to their findings and ours, Chrcanovic et al., [12] in their retrospective study on 2670 patients suggested that bruxism significantly increased both implant failure and mechanical complications of implant-supported restorations. Another study reported a higher implant failure rate associated with a positive dental history of bruxism in the maxillary and mandibular implant-supported fixed complete dentures [13].
Systematic reviews and meta-analyses regarding the effect of bruxism on implants mostly did not suggest any causative relationship [2, 3, 6]. Two other systematic reviews by Yi Zhou et al. [8] and Manfredini et al. [7] reported a positive relationship between bruxism and mechanical complications and prosthesis failure rate following dental implant treatments.
Despite the controversial results, practical guidelines are required for management of bruxer patients to help surgeons make an informed decision about a reliable treatment plan. Recent studies by including experimental articles about the effect of different types of occlusal forces on MBL and other data about the intensity of forces applied to teeth during bruxism suggested some clinical protocols to decrease the risk of implant failure in patients with bruxism [6, 14, 15]. Manfredini et al. [14] suggested adherence to some practical points to minimize the risk of implant treatment in bruxer patients, which included use of as many implants as possible with the largest possible diameters, splinting of implants together for better force distribution, avoiding implant placement in low-density bone quality, following the regular time of implant loading, not using a cantilever design for occlusal rehabilitation, axial loading of implants, considering sufficient freedom of movement in maximum intercuspation, designing a flat cuspidal plane to better tolerate lateral movements, and fabrication of customized occlusal splints (night guards).
The prosthetic components in bruxer patients should be designed such that they minimize inappropriate occlusal forces [16]. The frameworks are more passive in cement-retained restorations. The cement space allows for passivity, since the cement serves as a shock absorber and decreases the level of stress applied to implants and the bone interface [17]. Excessive occlusal forces may cause crown detachment or porcelain fracture in bruxer patients. However, in screw-type restorations, excessive forces could lead to screw fracture or even fixture fracture [18].
The effect of occlusal overload on MBL or total loss of osseointegration is unclear when excessive occlusal loads exceed the biologically acceptable threshold [19]. It is a challenging topic whether traumatic occlusal forces result in peri-implant bone loss, and little evidence is available to support a cause-and-effect relationship in implant dentistry [20]. Despite the poor reports on the effect of occlusal overload on MBL, prevention of occlusal overload needs a comprehensive examination, precise surgical and prosthetic treatments, regular maintenance in bruxer patients, and use of occlusal splints to minimize the generation of excessive occlusal loads by parafunctional habits [17, 18, 21].
Because of the nature of studies regarding implant treatment in patients with bruxism, it was difficult to assess whether the suggested guidelines had been applied in studies or not. Moreover, the outcomes of the review studies are controversial due to the heterogeneous treatment protocols of the included articles. Adherence to the most recent clinical suggestions (as our study methodology) can lead to promising outcomes with regard to mechanical and biological implant factors in patients with bruxism undergoing dental implant treatment. Considering the limited number of published studies on this topic with limited study populations, further investigations regarding the accuracy and efficacy of the suggested protocols about implant treatment in bruxer patients and their effect on implant survival are warranted.
Conclusion
According to the current results, dental implant treatment in bruxer patients, according to the suggested protocol, showed promising outcomes. There were no significant differences between the bruxer and non-bruxer groups in terms of MBL, crown detachment and porcelain fracture at the 12-month follow-up after implant loading.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declarations
Conflict of interest
All authors have no conflict of interest to declare.
Ethical Approval
This study was performed according to the principles outlined by the World Medical Association’s Declaration of Helsinki on experimentation involving human subjects, as revised in 2000. The protocol of the study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (code: IR.SBMU.DRC.REC.1398.009).
Informed Consent
The study design and objectives were explained to all participants, and written informed consent was obtained from them.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References:
- 1.Albrektsson T, Donos N, 1 WG. (2012) Implant survival and complications. The Third EAO consensus conference 2012. Clin Oral Implants Res 23(Suppl 6) 63-5. [DOI] [PubMed]
- 2.Chrcanovic BR, Albrektsson T, Wennerberg A. Bruxism and dental implants: a meta-analysis. Implant Dent. 2015;24(5):505–516. doi: 10.1097/ID.0000000000000298. [DOI] [PubMed] [Google Scholar]
- 3.Komiyama O, Lobbezoo F, De Laat A, Iida T, Kitagawa T, Murakami H, et al. (2012) Clinical management of implant prostheses in patients with bruxism. Int J Biomater. 2012. [DOI] [PMC free article] [PubMed]
- 4.Lobbezoo F, Van der Zaag J, Visscher C, Naeije M. Oral kinesiology a new postgraduate programme in the Netherlands. J Oral Rehabil. 2004;31(3):192–8. doi: 10.1046/j.0305-182X.2003.01244.x. [DOI] [PubMed] [Google Scholar]
- 5.Manfredini D, Winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F. Epidemiology of bruxism in adults: a systematic review of the literature. J Orofac Pain. 2013;27(2):99–110. doi: 10.11607/jop.921. [DOI] [PubMed] [Google Scholar]
- 6.Lobbezoo F, Brouwers J, Cune M, Naeije M. Dental implants in patients with bruxing habits. J Oral Rehabil. 2006;33(2):152–159. doi: 10.1111/j.1365-2842.2006.01542.x. [DOI] [PubMed] [Google Scholar]
- 7.Manfredini D, Poggio CE, Lobbezoo F. Is bruxism a risk factor for dental implants? a systematic review of the literature. Clin Implant Dent Relat Res. 2014;16(3):460–469. doi: 10.1111/cid.12015. [DOI] [PubMed] [Google Scholar]
- 8.Zhou Y, Gao J, Luo L, Wang Y. Does bruxism contribute to dental implant failure? a systematic review and meta-analysis. Clin Implant Dent Relat Res. 2016;18(2):410–420. doi: 10.1111/cid.12300. [DOI] [PubMed] [Google Scholar]
- 9.Zarb GA, Albrektsson T. 1985 Patient selection and preparation. In: Branemark PI, Zarb G, T A, editors. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence 199–209.
- 10.Misch C. The effect of bruxism on treatment planning for dental implants. Dent Today. 2002;21(9):76–81. [PubMed] [Google Scholar]
- 11.Mangano FG, Shibli JA, Sammons RL, Iaculli F, Piattelli A, Mangano C. Short (8-mm) locking-taper implants supporting single crowns in posterior region: a prospective clinical study with 1-to 10-years of follow-up. Clin Oral Implants Res. 2014;25(8):933–940. doi: 10.1111/clr.12181. [DOI] [PubMed] [Google Scholar]
- 12.Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Bruxism and dental implant treatment complications: a retrospective comparative study of 98 bruxer patients and a matched group. Clin Oral Implants Res. 2017;28(7):e1–e9. doi: 10.1111/clr.12844. [DOI] [PubMed] [Google Scholar]
- 13.Ji T-J, Kan JY, Rungcharassaeng K, Roe P, Lozada JL. Immediate loading of maxillary and mandibular implant-supported fixed complete dentures: a 1-to 10-year retrospective study. J Oral Implantol. 2012;38(S1):469–477. doi: 10.1563/AAID-JOI-D-11-00027. [DOI] [PubMed] [Google Scholar]
- 14.Manfredini D, Bucci MB, Sabattini VB, Lobbezoo F. 2011 Bruxism: overview of current knowledge and suggestions for dental implants planning. CRANIO®. 29 (4) 304–12. [DOI] [PubMed]
- 15.Kim Y, Oh TJ, Misch CE, Wang HL. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants Res. 2005;16(1):26–35. doi: 10.1111/j.1600-0501.2004.01067.x. [DOI] [PubMed] [Google Scholar]
- 16.Lemos CA, de Souza Batista VE, Almeida DA, Santiago Junior JF, Verri FR, Pellizzer EP. Evaluation of cement-retained versus screw-retained implant-supported restorations for marginal bone loss: a systematic review and meta-analysis. J Prosthet Dent. 2016;115(4):419–427. doi: 10.1016/j.prosdent.2015.08.026. [DOI] [PubMed] [Google Scholar]
- 17.Jivraj S. Screw versus cemented implant restorations: The decision-making process. J Dent Implant. 2018;8(1):9–19. doi: 10.4103/jdi.jdi_7_17. [DOI] [Google Scholar]
- 18.Tabrizi R, Behnia H, Taherian S, Hesami N. What are the incidence and factors associated with implant fracture? J Oral Maxillofac Surg. 2017;75(9):1866–1872. doi: 10.1016/j.joms.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Chang M, Chronopoulos V, Mattheos N. Impact of excessive occlusal load on successfully-osseointegrated dental implants: a literature review. J Investig Clin Dent. 2013;4(3):142–150. doi: 10.1111/jicd.12036. [DOI] [PubMed] [Google Scholar]
- 20.Bertolini MM, Del Bel Cury AA, Pizzoloto L, Acapa IRH, Shibli JA, Bordin D. Does traumatic occlusal forces lead to peri-implant bone loss? A systematic review. Braz Oral Res. 2019;33:e069. doi: 10.1590/1807-3107bor-2019.vol33.0069. [DOI] [PubMed] [Google Scholar]
- 21.Fu JH, Hsu YT, Wang HL. Identifying occlusal overload and how to deal with it to avoid marginal bone loss around implants. Eur J Oral Implantol. 2012;5(Suppl):S91–103. [PubMed] [Google Scholar]



