Abstract
Purpose
Injection of intra-articular medicaments is an accepted therapy for temporomandibular joint disorders (TMDs). This study compares the efficacy of arthrocentesis followed by platelet-rich plasma (PRP) as compared to hyaluronic acid (HA) injections for TMDs unresponsive to conservative therapy. PRP injection following arthrocentesis was hypothesized to be better compared to arthrocentesis alone or when combined with HA injection.
Methods
Forty-seven patients with TMDs enrolled in an RCT were randomly assigned to three groups: Group A—PRP, Group B—HA or Group C—control group of arthrocentesis alone. Pre-operative evaluation and post-operative changes at 1-, 3-, 6-month intervals were assessed for improvement in pain, maximum mouth opening, joint sounds and excursive movements. Statistical significance was set at P value < 0.05.
Results
Post-operative joint sounds were present in three out of 16 patients in Group A; six out of 15 patients in Group B and eight out of 16 patients in Group C at 6-month follow-up. For the remaining outcome variables, no statistical difference between groups was observed.
Conclusion
Both medicaments produced significant clinical improvements when compared to the control group. When comparing PRP against HA, none showed superiority over the other.
Clinical trial registration number: CTRI/2019/01/017076
Keywords: Arthrocentesis, Prolotherapy, Platelet-rich plasma, Hyaluronic acid
Introduction
The lavage and lysis of the upper joint space using an arthroscope lead to the development of a minimally invasive procedure called arthrocentesis. This simple and blind technique of irrigating the upper temporomandibular joint space using lactated Ringer’s lactate solution is highly effective in relieving pain and restoring normal mouth opening [1].
In temporomandibular joint disorders (TMDs), the translation of the disc is restricted. This limitation is due to changes in the upper joint space. Hence, manipulation of the upper joint space allows translation of the disc along the eminence and this explains the efficacy of arthrocentesis.
George S Hackett (1956) used the term ‘Prolotherapy’ to denote the injection of growth factors or its stimulants into the human body for repair or restoration of soft tissues. Proliferative injection therapy has been used for ligament, tendon and joint repair.
Hyaluronic acid is a normal constituent of synovial fluid. It maintains the viscosity of synovial fluid and regulates its flow. It also provides nourishment to the articular cartilage. Platelet-rich plasma (PRP) is a concentrate of platelets suspended in plasma which contains growth factors. These platelets actively secrete protein growth factors which initiates wound healing.
This study aims to prospectively compare the efficacy of intra-articular administration of PRP following arthrocentesis as compared to hyaluronic acid in patients suffering from TMD who were nonresponsive to conservative treatment modalities. PRP injection following arthrocentesis was hypothesized to be better compared to arthrocentesis alone or when combined with HA injection.
Materials and Methods
An RCT was designed prospectively and performed on patients diagnosed with TMDs based on Diagnostic criteria [2], reporting for treatment to the Department of Oral and Maxillofacial Surgery. The study was conducted from August 2016 to April 2018. This trial complies with the Helsinki Declaration, and clearance was obtained from the institutional ethics committee. The study included patients older than 18 years with symptomatic disc disorders categorized as per taxonomic classification into disc displacement with/without reduction. Patients with any previous invasive procedures on TMJ, connective tissue diseases, degenerative joint disorders, bony pathology associated with TMJ, a history of trauma, orthodontic treatment, allergic reaction to local anesthetics and psychiatric disorders were excluded from the study.
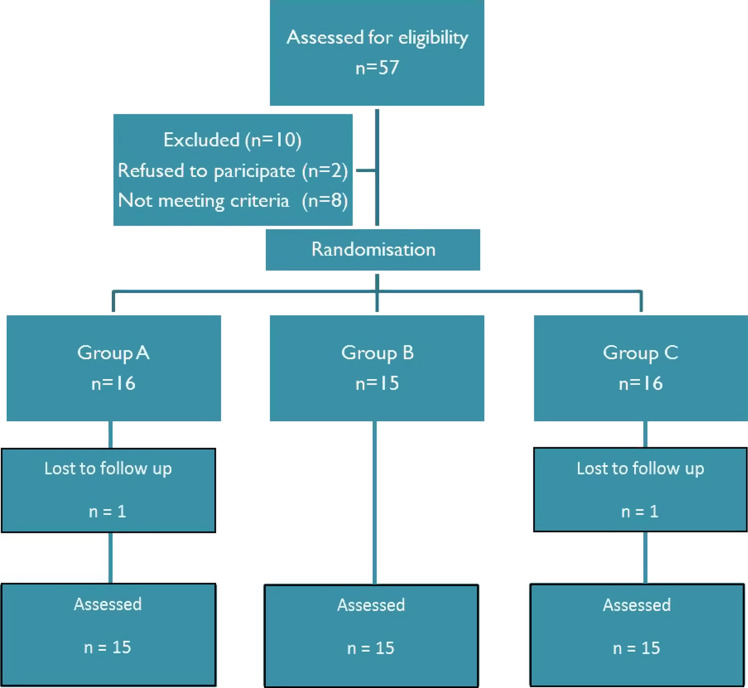
‘Maximal mouth opening’ (MMO), laterotrusive and protrusive movements were measured in millimetres with the help of a metallic scale. The pain level was self-assessed by the patient using the Visual Analogue Scale (VAS) ranging from 0 (zero) to 10 (ten). Temporomandibular joint sounds on palpation/auscultation were rated clinically as present or absent. Radiological evaluation was done pre-operatively using an Orthopantomogram (OPG) to rule out any bony pathology associated with TMJ. Magnetic resonance imaging (MRI), T1-weighted images of the affected joint in open and closed mouth positions were performed to assess the position of the mandibular condyle to the articular disc (Fig. 1).
Fig. 1.
T1-weighted MR image of right TMJ in open mouth position showing anteriorly trapped articular disc
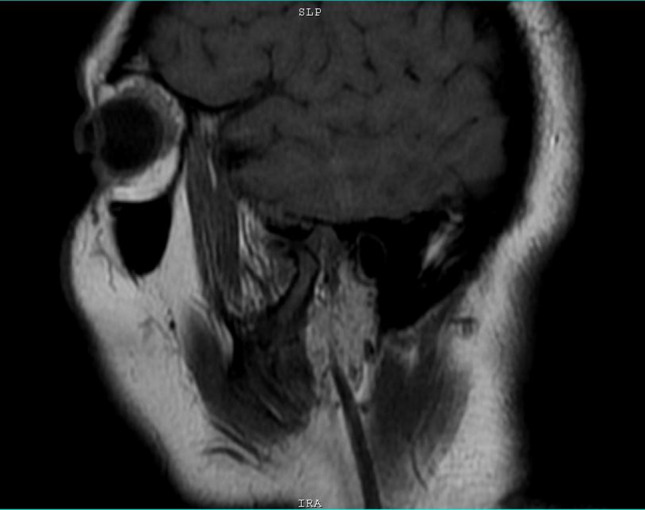
A total of 47 consenting patients with unilateral temporomandibular joint internal derangement were taken up for management. Power of the study was set at 80%, and a significance level of 95% was used to calculate the required sample size. Based on this analysis, each study group required assessment of minimum 15 joints. The patients were assigned randomly to any of the three groups by the lottery method. Group A underwent arthrocentesis followed by a single injection of 1 ml PRP; Group B underwent arthrocentesis followed by a single injection of 1 ml HA, while Group C underwent arthrocentesis alone (Fig. 2).
Fig. 2.
Flowchart of patients enrolled in the study
In the present study, the double-needle technique of arthrocentesis proposed by Nitzan was performed using 21 gauge needles at a depth of 20–25 mm (Fig. 3). The auriculotemporal nerve block using 2% lignocaine with 1:80,000 adrenaline was administered. Ringer's lactate solution (100 ml) was used to perform arthrocentesis procedure by conventional technique (Fig. 4). One millilitre of either PRP or HA (Inj. Hyalosyn 10 mg; Mol wt 2.4–3.6 million Daltons) was injected into the upper joint space using the needle through the entry port. The second needle in the exit port was withdrawn before injection. PRP was prepared using a single-step centrifugation method as proposed by Anitua et al. [3]. One millilitre of PRP thus obtained was then injected into the upper joint space without activating since nonactivated PRP can promote chondrogenic differentiation, mesenchymal stem cell (MSC) proliferation and osteoinductivity more than activated PRP [4].
Fig. 3.

Nitzan’s technique—surface marking
Fig. 4.

Arthrocentesis using 100 ml Ringer’s lactate
The study subjects were followed up at 1 week, 1, 3 and 6 months, and data were recorded concerning the reduction in pain, improvement in maximum mouth opening, excursive movements and reduction in joint sounds. The individuals evaluating the post-treatment outcomes and the statistician were blinded in this study to prevent bias.
Results
The recorded data were analysed statistically, and the results were tabulated. Statistical analysis was performed using SPSS (version 21.0) software, and p < 0.05 was considered statistically significant. A nonparametric test of significance was used because of the relatively small sample size. The pre-procedural and post-procedural change in data recorded was used for intergroup comparisons using the Kruskal–Wallis test and intragroup comparisons using Friedman, Mann–Whitney and Wilcoxon signed-rank tests.
The mean age of the study sample was 46.19 ± 14.72 years (median: 46 years; range: 18–79 years). Females accounted for 63.8% (30), and 36.2% (17) were males. Group A included 16 patients, Group B comprised 15 patients and Group C had 16 patients. One patient each in Group A and Group C was lost to follow-up.
The pain was the only complaint in 28 patients (59.6%). Pain with clicking sounds was the complaint in 11 patients (23.4%), while pain and decreased mouth opening in eight patients (17%). Joint sounds were present in all patients pre-operatively. The mean VAS score pre-operatively was 7.19 ± 1.28 in Group A, 7.27 ± 1.39 in Group B and 7.44 ± 0.81 in Group C (p > 0.05). Based on the disease severity, 61.7% of the study population (29 patients) had disc displacement with reduction, while 38.3% (18 patients) had disc displacement without reduction. Pre-operative baseline comparative values for study and outcome variables are tabulated (Table 1). Pre-operatively, no significant difference existed between the groups for any of the study variables.
Table 1.
Pre-operative intergroup baseline comparison between the study and predictor variables; mean ± SD
| Study variables | Group A (n = 16) | Group B (n = 15) | Group C (n = 16) | p value |
|---|---|---|---|---|
| Age (years) | 40.56 ± 9.72 | 46.53 ± 19.15 | 51.50 ± 12.80 | p > 0.05* |
| Female n (%) | 12 (70.59%) | 09 (60.00%) | 09 (56.25%) | p > 0.05* |
| VAS | 7.19 ± 1.28 | 7.27 ± 1.39 | 7.44 ± 0.81 | p > 0.05* |
| MMO | 34.88 ± 8.62 | 28.93 ± 3.63 | 40.00 ± 10.71 | p > 0.05* |
| (Rt) Laterotrusion | 7.00 ± 2.07 | 6.20 ± 1.90 | 7.31 ± 2.02 | p > 0.05* |
| (Lt) Laterotrusion | 7.38 ± 2.58 | 7.53 ± 1.69 | 7.00 ± 1.71 | p > 0.05* |
| Protrusion | 6.31 ± 1.58 | 6.27 ± 1.44 | 6.00 ± 1.75 | p > 0.05* |
SD standard deviation, VAS visual analogue scale, MMO maximum mouth opening, Rt Right, Lt Left
*p value is calculated using Kruskal–Wallis Test (one-way nonparametric)
Post-operative comparative values for the outcome variables at 6 months follow-up are tabulated (Table 2). Post-operative joint sounds at 6 months were present in only three patients in Group A, six patients in Group B; however, in Group C, eight patients had joint sounds. For the remaining outcome variables, no statistical significance was noted between groups at 6-month follow-up. However, a significant increase in mouth opening following the intervention was noted in Group A and B at 3- and 6-month follow up (p < 0.05). Pain and joint sounds decreased while maximum mouth opening without pain increased in all three groups. Patients belonging to Group A presented with swelling and tenderness over the TMJ on the first post-operative day. One patient of Group A reported with port site infection two weeks after the procedure which subsided with antibiotic therapy. Two patients (one each from Group A and Group C) who had disc displacement without reduction did not show any improvement at 6-month follow-up visit and hence were taken up subsequently for open joint surgery. One patient experienced a brief episode of vertigo following arthrocentesis that regressed spontaneously in a few seconds.
Table 2.
Intergroup comparison of outcome variables at the 6th post-operative month; mean ± SD
| Study variables | Group A (n = 15) | Group B (n = 15) | Group C (n = 15) | p value |
|---|---|---|---|---|
| VAS | 3.40 ± 1.81 | 3.93 ± 2.19 | 4.27 ± 1.67 | p > 0.05* |
| MMO | 41.40 ± 8.22 | 40.53 ± 6.11 | 43.67 ± 8.25 | p > 0.05* |
| (Rt) Laterotrusion | 9.20 ± 1.57 | 9.27 ± 1.58 | 8.87 ± 1.81 | p > 0.05* |
| (Lt) Laterotrusion | 9.07 ± 1.03 | 8.60 ± 1.35 | 9.13 ± 0.92 | p > 0.05* |
| Protrusion | 6.80 ± 1.61 | 6.53 ± 1.30 | 6.93 ± 0.80 | p > 0.05* |
SD standard deviation, VAS visual analogue scale, MMO maximum mouth opening, Rt Right, Lt Left
*p value is calculated using Kruskal–Wallis Test (one-way nonparametric)
Discussion
TMDs are a common cause for orofacial pain, and the diagnosis and treatment of this are quite challenging. Pre-operative orthopantomogram is a useful modality for screening in TMDs. It helps to assess the osseous components of the TMJ as most of the bony abnormalities occur in the lateral third of the condylar head [5]. Alterations in the condylar height and inclination are a frequent finding in internal derangements of the TMJ. Since the 1980s, MRI is the investigation of choice to diagnose diseases of the TMJ. Improved diagnostic accuracy with the high spatial resolution has made this modality a gold standard for diagnoses of TMDs [6].
The present study compared the therapeutic efficacy of two different intra-articular medicaments: PRP and HA. Sodium hyaluronate, a component of normal synovial fluid, is a high molecular weight polysaccharide. The half-life (t l/2) of HA is only 13.2 h in other joint spaces, and thus the administered exogenous hyaluronate is unlikely to be present in bulk within the joint space for the entire 6-month period. It was proposed that the short-term lubricating action prevents damage to the articular disc and synovial surfaces in acute discal obstruction [7].
PRP contains seven protein growth factors which include the three subtypes of platelet-derived growth factor, vascular endothelial growth factor (VEGF), two subtypes of transforming growth factors (TGF1 and TGF2), and epithelial growth factor (EGF). It also contains the three proteins—fibrin, fibronectin and vitronectin. These proteins promote osteoconduction and also play a role in connective tissue and epithelial migration [8].
In terms of secondary outcomes, significant clinical improvements for VAS parameters were noted in all three groups. The mean change in VAS scores was 3.79 for the PRP group, 3.34 for the HA group and 3.17 for the control group of arthrocentesis alone (Table 3). These findings were less when compared to the study done by Kilic et al. who found a mean change of 4.68 for the PRP group and 5.17 for HA group [9]. Hanci et al. showed that the mean change in the VAS score was 6.62 for the PRP group and 3.77 for a group of arthrocentesis alone [10].
Table 3.
Mean changes in outcome variables among the three groups at the 6th post-operative month; mean ± SD
| Study variables | Group A (n = 15) | Group B (n = 15) | Group C (n = 15) | p value |
|---|---|---|---|---|
| VAS | 3.80 ± 1.52 | 3.33 ± 1.29 | 3.13 ± 1.88 | p > 0.05 |
| MMO | 6.07 ± 3.63 | 11.60 ± 4.39 | 3.40 ± 4.45 | p > 0.05 |
| (Rt) Laterotrusion | 2.27 ± 2.55 | 3.07 ± 1.67 | 1.47 ± 1.13 | p > 0.05 |
| (Lt) Laterotrusion | 1.47 ± 1.88 | 1.07 ± 1.75 | 2.20 ± 1.42 | p > 0.05 |
| Protrusion | 0.53 ± 1.06 | 0.27 ± 1.22 | 1.07 ± 1.67 | p > 0.05 |
SD standard deviation, VAS visual analogue scale, MMO maximum mouth opening, Rt Right, Lt Left
p value is calculated using Kruskal–Wallis Test (one-way nonparametric)
The mean change in maximal mouth opening (MMO) in this study was 6.52 mm for the PRP group, 11.6 mm for HA the group and only 3.67 mm for the control group of arthrocentesis alone which is not significant. Hanci et al. demonstrated better results for the PRP group which showed a mean change in MMO of 7.7 mm at and 6.1 mm for the group of arthrocentesis alone [10]. Alpaslan et al. in his study demonstrated a mean change in MMO for the HA group to be 7.82 which is significantly less than the result obtained in this study [11]. The mean change in protrusive movements pre-operatively and at 6 months in this study was 0.49 mm for the PRP group, 0.26 mm for the HA group and 0.93 mm for the control group of arthrocentesis alone. In the study by Kilic et al., the mean changes in protrusion were higher 0.89 mm in the PRP group and 1 mm in arthrocentesis-alone group [9].
In this study, joint sounds were present in all patients pre-operatively. Joint sounds were persisting in only three out of 15 joints postoperatively at 6 months for the PRP group (80% reduction), while eight out of 15 joints in the group of arthrocentesis alone (46.7% reduction) had joint sounds. Hanci et al. in his study reported a reduction in joint sounds in ten out of 12 joints for the PRP group, while arthrocentesis alone reduced joint sounds in seven out of 12 joints [10].
The primary and secondary outcomes of this study show that the intra-articular injection of PRP or HA after arthrocentesis resulted in significant improvement in function for patients with TMD, although neither proved to be better than the other. Arthrocentesis alone is still used for the treatment for TMDs but its effect is short-lived. It does not restore the internal joint anatomy. Kilic et al. hypothesized that the injection of an intra-articular agent with regenerative capacity may inhibit degenerative changes and stimulate cartilage regeneration [9].
Pihut et al. in their study found that PRP positively reduced the intensity of pain in TMD patients [12]. Hanci et al. also reported a significant improvement of pain, TMJ sounds and MMO which are consistent with the findings of this study [10]. Bertolami et al. showed that a single intra-articular injection of HA provided relief of symptoms for at least 6 months in cases of disc displacement with reduction [7]. The findings of this study pertaining to the HA group are consistent with the study done by Manfredini et al [13].
TMJ visco-supplementation consists of intra-articular injection of HA which decreases pain and improves joint function. Based on its molecular weight, exogenous HA may increase the production of endogenous HA by synoviocytes. High molecular weight HA (between 1 and 6 × 106 Da) does not pass from the intra-articular to the intercellular medium. Thus, they are unable to act on synoviocytes and chondrocytes, which are required to decrease synovitis and restore the normal fluid properties of the synovium. This property is called ‘visco-induction’. HA with a molecular weight between 0.5 and 1 × 106 Da would provide better effects in vivo and could promote endogenous HA synthesis by synoviocytes [14, 15].
The findings of this study revealed a significant increase in MMO, lateral movements and a reduction in TMJ pain. This indicates the potential utility of prolotherapy agents in the management of TMDs which will allow an earlier return to function for the patient and improved quality of life.
To conclude, arthrocentesis plus PRP injection has no added clinical advantage over arthrocentesis plus HA injection in the short term; thus, PRP need not be considered as the first line of treatment. The present study is in concurrence with the study done by Kilic et al. for TMJ osteoarthritis [9]. It is also hypothesized that intra-articular injection of medication after arthrocentesis is superior to the direct injection of these medicaments into the TMJ without arthrocentesis. Also, arthrocentesis will reduce the frequency of intra-articular medicaments.
The limitations of this study include the relatively small sample size and follow-up period which needs to be longer. Further research is suggested to compare the advantage of arthrocentesis before prolotherapy against direct injection of the agent. Also, extensive work needs to be done in regenerative therapies and the role of stem cells in TMDs.
Funding
No funding was received for this study.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral MaxillofacSurg. 1991;49:1163–1167. doi: 10.1016/0278-2391(91)90409-F. [DOI] [PubMed] [Google Scholar]
- 2.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache. 2014;28(1):6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anitua E, Aguirre JJ, Algorta J, et al. Effectiveness of autologous preparation rich in growth factors for the treatment of chronic cutaneous ulcers. J Biomed Mater Res B ApplBiomater. 2008;84:515–521. doi: 10.1002/jbm.b.30886. [DOI] [PubMed] [Google Scholar]
- 4.Mishra A, Tummala P, King A, et al. Buffered platelet-rich plasma enhances mesenchymal stem cell proliferation and chondrogenic differentiation. Tissue Eng Part C Methods. 2009;15(3):431–435. doi: 10.1089/ten.tec.2008.0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahn S-J, Kim T-W, Lee D-Y, et al. Evaluation of internal derangement of the temporomandibular joint by panoramic radiographs compared with magnetic resonance imaging. Am J OrthodDentofacialOrthop. 2006;129:479–485. doi: 10.1016/j.ajodo.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Shan YZ, Chi Y, Min JC, et al. Magnetic resonance imaging in the diagnosis of intra-articular adhesions of the temporomandibular joint. Br J Oral MaxillofacSurg. 2009;47:389–392. doi: 10.1016/j.bjoms.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Charles NB, Thomas G, Glenn TC, et al. Use of sodium hyaluronate in treating temporomandibular joint disorders: a randomized, double-blind placebo-controlled clinical trial. J Oral MaxillofacSurg. 1993;51:232–242. doi: 10.1016/S0278-2391(10)80163-6. [DOI] [PubMed] [Google Scholar]
- 8.Marx RE. Platelet-rich plasma: evidence to support its use. J Oral MaxillofacSurg. 2004;62:489–49610. doi: 10.1016/j.joms.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 9.ComertKilic S, Gungormus M. Is arthrocentesis plus platelet-rich plasma superior to arthrocentesis plus hyaluronic acid for the treatment of temporomandibular joint osteoarthritis: a randomized clinical trial. Int J Oral MaxillofacSurg. 2016;45(12):1538–1544. doi: 10.1016/j.ijom.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 10.Hancı M, Karamese M, Tosun Z, et al. Intra-articular platelet-rich plasma injection for the treatment of temporomandibular disorders and a comparison with arthrocentesis. J CraniomaxillofacSurg. 2015;43:162–166. doi: 10.1016/j.jcms.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Alpaslan GH, Alpaslan C. Efficacy of temporomandibular joint arthrocentesis with or without injection of sodium hyaluronate in treatment of internal derangements. J Oral MaxillofacSurg. 2001;59:613–618. doi: 10.1053/joms.2001.23368. [DOI] [PubMed] [Google Scholar]
- 12.Pihut M, Szuta M, Ferendiuk E, et al. (2014) Evaluation of pain regression in patients with temporomandibular dysfunction treated by intra-articular platelet-rich plasma injections: a preliminary report. Biomed Res Int 132369 PMID:25157351 [DOI] [PMC free article] [PubMed]
- 13.Manfredini D, Bonnini S, Arboretti R, et al. Temporomandibular joint osteoarthritis: an open label trial of 76 patients treated with arthrocentesis plus hyaluronic acid injections. Int J Oral MaxillofacSurg. 2009;38:827–834. doi: 10.1016/j.ijom.2009.03.715. [DOI] [PubMed] [Google Scholar]
- 14.Smith MM, Ghosh P. The synthesis of hyaluronic acid by human synovial fibroblasts is influenced by the nature of the hyaluronate in the extracellular environment. RheumatolInt. 1987;7(3):113–122. doi: 10.1007/BF00270463. [DOI] [PubMed] [Google Scholar]
- 15.Asari A, Miyauchi S, Matsuzaka S, et al. Molecular weight-dependent effects of hyaluronate on the arthritic synovium. Arch HistolCytol. 1998;61(2):125–135. doi: 10.1679/aohc.61.125. [DOI] [PubMed] [Google Scholar]