Abstract
Objectives:
Self-medication is increasingly popular among people in developing nations like Nepal where the expense of healthcare is relatively high and over-the-counter) medications are widely and easily accessible. Although this method has certain advantages, it is also clear that it has some drawbacks, including the potential for adverse drug reactions, drug resistance, medication interactions, and increased morbidity and mortality. This study aimed to evaluate the use of self-medication in nine wards of Kathmandu Metropolitan City (ward no. 4, 5, 13, 15, 16, 17, 23, 31, and 32).
Methods:
This cross-sectional descriptive survey was conducted in the chosen wards of Kathmandu Metropolitan city for 3 months from August to October 2021. A semi-structured questionnaire was used to collect data from 372 patients who were seeking self-medication. The participants were chosen randomly.
Results:
Self-medication was common among people (78%). The most frequent ailments for which participants self-medicated were the common cold (17.1%), headache (14.7%), fever (14.5%), and cough (7.6%). Anticold medications (18.2%), non-steroidal anti-inflammatory drugs (17.4%), antipyretics (15.2%), and analgesics (9.1%) were the most popular drug classes used in self-medication. The two most frequent justifications for self-medication were the absence of any major ailment (35%) and self-experience (22.7%). When symptoms started, the majority of patients started taking medication for themselves, and 47.7% of them got their prescriptions directly from the pharmacist by explaining their symptoms. When the symptoms were not relieved by the medication used for self-medication, it was found that the majority of participants (79.7%) stopped using the medication and visit the doctor.
Conclusion:
The prevalence of self-medication in Kathmandu city was ascertained by assessing the practice among residents of the Kathmandu Metropolitan city. The study showed self-medication is common among people and therefore, proper education about drug use and self-medication is needed.
Keywords: Drug use, self-medication, practice, prevalence, Kathmandu
Introduction
Self-medication practice is the use of medication without a prescription from healthcare professionals. According to the World Health Organization, self-medication is treating problems or symptoms that have been self-diagnosed with the help of medications that are intended to be used by patients as part of their initiatives and responsibilities.1,2 For self-care, people are using self-medication, which does not require a prescription.3 People self-identified their illnesses from the experience and select and use the medication that may be herbal and traditional.4 The practice of self-medication is becoming popular as it relieves stress and saves time and money in treating minor illnesses.4,5
In Nepal, allopathic drugs are classified as “a,” “b,” or “c,” with respective subcategories. Category “a” consists of narcotic and poisonous drugs; category “b” consists of antibiotics, hormones, etc. that require a prescription for dispensing from pharmacies; and category “c” usually consists over-the-counter (OTC) drugs.6 The prevalence rates of self-medication in Nepal are much higher in comparison to developed nations due to limited access to appropriate and affordable medication and healthcare facilities.7,8 This encourages people to practice self-medication to manage the majority of diseases. Similarly, increased availability of drug and disease information, particularly on the Internet, along with increased interest in one’s health, has led in the higher demand for more direct involvement of patients in the decision-making.9 The prevalence rate for self-medication was found to be 38.8% and 75.7% in Asia5 and Africa,10 respectively. According to a study from the United States, up to 80% of all drugs are purchased without any prescription in developing countries.7 Different studies conducted in Nepal reported that self-medication prevalence was 59% in the general population at Pokhara,11 50.7% in nursing students at Chitwan,12 35.1% in dental students at Kathmandu,8 and 26.2% in medical students at Pokhara.13 A study at the B. P. Koirala Institute of Health Sciences showed that 90.1% of the health sciences students self-prescribed paracetamol.14
According to studies, the most frequent causes of self-prescribed medication are prior illness experience, a lack of accurate information about the condition, difficulty affording medical care, a lack of time, and easy access to medications.15,16 Self-medication has advantages such as active patient choice in product use, immediate and direct access to self-care and treatment, convenience, and lower hospital visitation costs.17,18 The potential drawbacks of self-medication are delaying treatment or receiving the wrong diagnosis, increasing the risk of abuse, misuse, overdosage, adverse events, or interactions with other drugs.3,19,20
Numerous research has been done in Nepal about the use of self-medication among medical students.8,12–14,21 However, very few studies have focused on the self-medication practice of people in a community setting in Nepal.11,22 This called for more research focusing on how self-medication work in a communal environment. Therefore, this study was carried out in nine wards (4, 5, 13, 15, 16, 17, 23, 31, and 32) of Kathmandu Metropolitan City (KMC) to comprehend the self-medication and drug use by different groups of people.
Materials and methods
Study setting and population
A community-based cross-sectional descriptive study was conducted from August to October 2021 in nine randomly chosen KMC wards (4, 5, 13, 15, 16, 17, 23, 31, and 32).
Eligibility criteria
Individuals 18 years and older were eligible to participate in this study. We preferentially included young and middle-aged adults; however, older adults were also included in this study. Individuals below 18 years of age, unable to listen or speak, pregnant, and those who were not willing to participate were excluded.
Sample size
The sample size was determined using the following formula with the assumption: the total population of KMC (N), a 5% margin of error (e), a 95% confidence interval, and the prevalence of self-medication in Nepal which is estimated as 59% (p).11
Based on this formula, the final sample size used for this study was 372.
Sampling procedure
Out of 32 wards from KMC, 16 were excluded from the study as the wards have a population of less than 20,000. From the remaining 16 wards, 9 wards were selected randomly. The sample size was allotted based on the population in each ward. Furthermore, the sampling process at each ward was initiated by identifying the center of the catchment area with the help of Google Maps version 10.14.1. The selected ward was divided into five areas (eastern, western, northern, southern, and central). The area for that ward was apportioned based on the sample size for that ward (e.g., the sample size for ward 15 is found to be 48 so 48/5 = 9.6, i.e., 10 individuals were interviewed randomly in that area). All individuals who completed the informed consent process were included in the study. We gathered sociodemographic information from all participants. We asked participants whether they had taken a “medication without a proper prescription during the last 3 months.” If they responded “yes,” we asked for additional information about their self-medication practices, whereas if they responded “no,” they were rejected.
Data collection procedure
A simple random sampling technique was used. A semi-structured interview questionnaire was used for data collection. The questionnaire was self-developed, reviewing the literature. The self-developed questionnaire was given to four experts. The experts were requested to judge the questionnaire in terms of agree or disagree related to relevance, clarity, accuracy, appropriateness, and usefulness to the present study. As per the suggestions and recommendations of the experts, necessary modifications were made to the questionnaire. All the questions were translated into the Nepali language and back-translated into the English language by a language expert to maintain translation validity. The questionnaire translated into Nepali language was pretested among 10% of the total sample, that is, 37 (n = 372), and those individuals were excluded from the main study. Then, pretesting was done to finalize the questionnaire. Eight students studying in different semesters of Bachelor in Pharmacy and Bachelor in Public Health of CiST College were oriented on how to hold an effective interview with the study units using the questionnaire. A semi-structured questionnaire was employed to gather the necessary information.
Study parameters
Sociodemographic variables included age in years and sex of the individual as stated by the respondent, family caste-ethnicity division (Brahmin/Chhetri, Janajati, Dalit, Madhesi, Muslim, and others), religion (Hindu, Buddhist, Christian, and Islamic), marital status (single, married, separated, divorced, and widowed), and education (illiterate, literate, primary level, intermediate level, bachelor level, and above) and enabling variables included types of drug used, knowledge about self-medication practice, symptoms/complains that leads to self-medication, and reason for self-medication) were collected.
Ethical consideration
Before data collection, permission was obtained from the office of KMC and the Institutional Review Committee (IRC-CiST) at the Central Institute of Science and Technology, affiliated with Pokhara University, Nepal (IRC no. 49/076/077).
Informed consent
A written consent form was given to the participants in Nepali and English versions explaining all the details of it and for illiterate subjects inform consent was obtained by their thumb print after verbally delivering all the content written in the inform consent. Only after their agreement their thumb print was obtained. They were informed that participation would be voluntary and that sufficient time was given to read and understand it. The identity of participants was kept confidential. Any type of economic and other benefits are not provided, and any influence was not used to collect the data from patients.
Statistical analysis
Data were entered and analyzed using version 16 of the Statistical Package for the Social Sciences program. Categorical variables were expressed as frequencies and percentages. To test the significance of the association between categorical variables, the chi-square test was used.
Results
Sociodemographic characteristics
Out of 372 participants, 53.0% were men and 47.0% were women. Regarding ethnicity, most of the participants were Brahmin/Chhetri (51.1%), followed by Janatati (40.3%). Similarly, 36.6% of the respondents were among the age group of 26–35, followed by the age group 36–45, which covered 26.1% of the total respondents. The majority of the respondents were Hindu (84.7%) and unmarried (32.0%). Similarly, 56.5% had a university degree and 3.0% were illiterate (Table 1).
Table 1.
Sociodemographic characteristics of the participants (n = 372).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 197 | 53 |
| Female | 175 | 47 |
| Ethnicity | ||
| Brahmin/Chhetri | 190 | 51.1 |
| Janajati | 150 | 40.3 |
| Dalit | 6 | 1.6 |
| Madhesi | 16 | 4.3 |
| Muslim | 4 | 1.1 |
| Others | 6 | 1.6 |
| Age group (years) | ||
| 18–25 | 63 | 16.9 |
| 26–35 | 136 | 36.6 |
| 36–45 | 97 | 26.1 |
| 46–55 | 51 | 13.7 |
| 56–65 | 22 | 5.9 |
| 66+ | 3 | 0.8 |
| Religion | ||
| Hindu | 315 | 84.7 |
| Buddhist | 42 | 11.3 |
| Christian | 11 | 3.0 |
| Islamic | 4 | 1.1 |
| Marital status | ||
| Single | 119 | 32.0 |
| Married | 239 | 64.2 |
| Separated | 3 | 0.8 |
| Divorced | 2 | 0.5 |
| Widowed | 9 | 2.4 |
| Education | ||
| Illiterate | 11 | 3.0 |
| Literate | 39 | 10.5 |
| Primary level | 32 | 8.6 |
| Intermediate level | 80 | 21.5 |
| Bachelor level and above | 210 | 56.5 |
Knowledge and practice of self-medication
Prevalence of self-medication (n = 372)
Self-medication was found to be prevalent in 78.0% of cases (Table 2). Out of 82 participants who did not self-medicate, 44.9% claimed that they did not do so because they were healthy during the 3 months. Thirty-one percent of them admitted to being concerned about the medications’ negative effects.
Table 2.
Prevalence of self-medication.
| Taken medications without prescription in the last 3 months | Frequency | Percentage (%) |
|---|---|---|
| Yes | 290 | 78 |
| No | 82 | 22 |
Symptoms/complaints (n = 290)
Out of 290 individuals, the most common symptom demanding self-medication was common cold 90 (31%), followed by headache 77 (26.5%), fever 75 (25.8%), gastritis 63 (21.7%), cough 40 (13.8%), and menstrual pain 20 (6.9%). Other signs that prompted self-medication included bodily aches, sore throats, diarrhea, constipation, and skin issues, among others (Figure 1).
Figure 1.
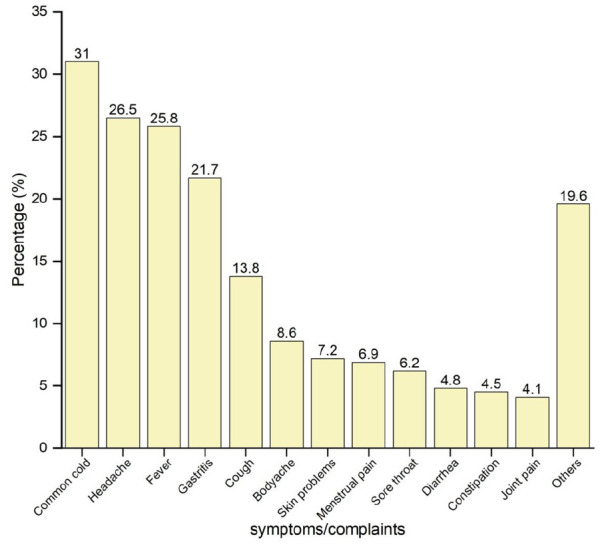
Common symptoms/ complaints for self-medications.
Reasons for self-medication (n = 290)
Out of 290 participants, 120 (41.4%) of them reported that they used self-medication because the illness was mild and 78 (26.9%) of them used it from their previous experience/prescription. Similarly, 46 (15.9%) of people who did not have time to see a doctor turned to self-medicate (Figure 2).
Figure 2.
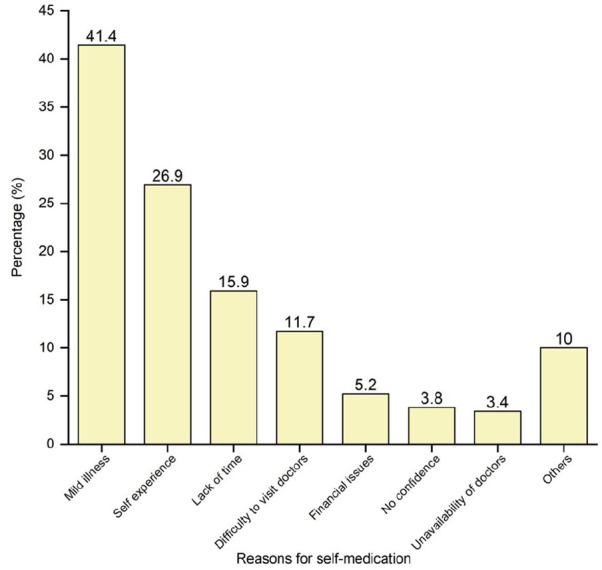
Reasons for self-medication.
Means for receiving medicines for self-medication (n = 290) and methods adopted for procuring medicines (n = 201)
Out of 290 individuals, 223 (76.9%) of them received the medicines directly from a pharmacy outlet without a prescription, followed by 63 (21.7%) who got the medicines with the help of previous prescriptions and 26 (8.9%) who received the medicines from leftover medicines at home (Table 3).
Table 3.
Means and method adopted for receiving medicine, routes, and dosage forms of drug and participants’ anticipated behavior if symptoms do not resolve at Kathmandu Metropolitan City.
| Frequency | Percentage (%) | ||
|---|---|---|---|
| Means for receiving medicines (n = 290) | Pharmacy outlet without prescription | 223 | 76.9 |
| Pharmacy outlet with previous prescription | 63 | 21.7 | |
| Left-over medicines | 26 | 8.9 | |
| Others | 9 | 3.1 | |
| Method adopted to get medicines (n = 223) | By mentioning the symptoms/complaints | 122 | 54.7 |
| By mentioning name of medicines | 113 | 50.7 | |
| By showing the paper with the name of medicines written | 12 | 5.4 | |
| By showing the medicine package | 9 | 4 | |
| Routes of drugs (n = 229) | Oral | 224 | 97.8 |
| Topical | 5 | 2.2 | |
| Ophthalmic/otic | 4 | 1.7 | |
| Nasal | 1 | 0.4 | |
| Inhalation | 1 | 0.4 | |
| Dosage forms of drugs (n = 229) | Tablet | 214 | 93.4 |
| Syrup | 34 | 14.8 | |
| Powder/granules | 17 | 7.4 | |
| Capsule | 10 | 4.4 | |
| Suspension | 9 | 3.9 | |
| Solution | 8 | 3.5 | |
| Ointment | 4 | 1.7 | |
| Participants’ anticipated behavior if symptoms do not resolve (n = 290) | Stop medicine and consult doctors | 256 | 88.3 |
| Stop medicine and consult pharmacist | 62 | 21.4 | |
| Use of alternative drug | 36 | 12.4 | |
| Increase the dose of drug | 27 | 9.3 | |
| Others | 19 | 6.5 |
Likewise, out of 223 individuals who received the medicines directly from the pharmacy without a prescription, 122 (54.7%) people got their medicines by mentioning their symptoms/complaints, followed by 113 (50.7%) by mentioning the name of the medicines and 12 (5.4%) and 9 (4%) of people received it by showing the paper with the name of medicine written and medicine package, respectively (Table 4).
Table 4.
Association between sociodemographic characteristics and self-medication.
| Variables | Categories (n = 372) | Self-medication | p-Value | |
|---|---|---|---|---|
| Yes, n (%) | No, n (%) | |||
| Gender | Male | 153 (77.7) | 44 (22.3) | 0.885 |
| Female | 137 (78.3) | 38 (21.7) | ||
| Age group | 18–25 | 47 (74.6) | 16 (25.4) | 0.629 |
| 26–35 | 103 (75.7) | 33 (24.3) | ||
| 36–45 | 77 (79.4) | 20 (20.6) | ||
| 46–55 | 41 (80.4) | 10 (19.6) | ||
| 56–65 | 20 (90.9) | 2 (9.1) | ||
| 66+ | 2 (66.7) | 1 (33.3) | ||
| Marital status | Single | 91 (76.5) | 28 (23.5) | 0.533 |
| Married | 186 (77.8) | 53 (22.2) | ||
| Separated/divorced | 5 (100) | 0 (0) | ||
| Widowed | 8 (88.9) | 1 (11.1) | ||
| Education level | Illiterate | 10 (90.9) | 1 (9.1) | 0.043* |
| Literate | 27 (69.2) | 12 (30.8) | ||
| Primary level | 24 (75) | 8 (25) | ||
| High school level | 55 (68.8) | 25 (31.2) | ||
| Bachelor level and above | 174 (82.8) | 36 (17.2) | ||
All p-values from a chi-square test. *p-Value significance at <0.05.
Categories, routes, and dosage forms of drugs used in self-medication (n = 290)
Out of 290 individuals, the majority of individuals 91 (31.4%) used anticold medications, followed by non-steroidal anti-inflammatory drugs (NSAIDs) 73 (25.2%), antipyretics 68 (23.5%), and antiulcer medications (PPIs, H2 blockers, and antacids) 45 (15.5%). Antiemetics, cough syrups, vitamin supplements, antihistamines, and laxatives were also consumed by fewer numbers of participants (Figure 3). The most common routes for self-medication are oral 224 (97.8%) and were in tablet (93.4%). The majority of respondents stopped taking medication and visit doctors when symptoms were not relieved 256 (88.3%). Others, stopped taking medication and seeking advice from local pharmacists 62 (21.4%) and 27 (9.3%) increased the dosage. Our study also showed that 19 (6.5%) switched to alternative medicine after self-medication failed to reduce their symptoms (Table 3).
Figure 3.
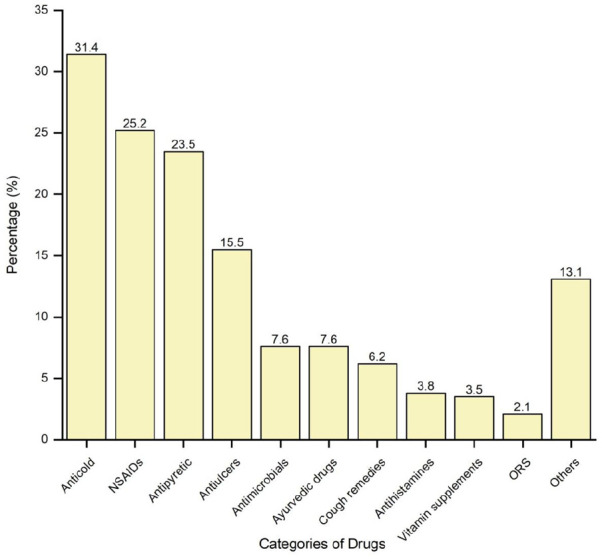
Categories of drugs used in self-medication.
NSAID: non-steroidal anti-inflammatory drug; ORS: oral rehydration solution.
Association between sociodemographic characteristics and self-medication
The study revealed that self-medication was a common practice among different age groups, gender, marital status, and education levels. Education level was found to be significantly associated with self-medication use (p-value: 0.043), which means that individuals with a bachelor’s level and above education reported more frequent self-medication use (82.8%) than those with less education (n = 116/16, 71.6%). Age groups, gender, and marital status were not found to be associated with self-medication use (Table 4).
Discussions
Self-medication was a common practice among people of all ages, genders, socioeconomic backgrounds, and educational levels. According to the results of this research, there was no difference in frequency of self-medication practice based on gender. This result is contradictory to the research done in Nepal where females are higher22 and in India where males are in higher proportion than females.23,24 In the present study, individuals who were 56–65 years were most likely to report taking a self-medication (90.9%) followed by those 46–55 years (80.4%). An increased pattern of self-medication practice was found with increasing age which may be because adults are becoming more money conscious as well as more aware of their own health needs. This study showed that 90.9% of individuals who were illiterate self-medicated followed by 82.8% of people with bachelor’s degrees and then 75% of people with a primary level education. Probably this may be due to that educated people are more likely to adhere to reading the patient information leaflet, label instructions, and expiry date hence do not hesitate to self-medicate. Similarly, illiterate people are less aware of potential side effects associated with concurrent use of medication, and they are also less likely to inquire whether they are receiving proper treatment.
The study revealed that the prevalence of self-medication practice among the participants was found to be 78%, which was comparable with the 75.5% prevalent rate reported by the study conducted in the neighborhood of Addis Abeba25 and 76.6% of MBBS students in Kathmandu.26 However, our study findings were higher than the prevalence reported among various types of research on self-medication conducted in Western Nepal (59%),11 medical students in Eastern Nepal (48.3%)27 and nursing students in Kathmandu (50.7%).12 This difference in the prevalence of self-medication practice may be due to different sample sizes, the population, cultural differences, healthcare systems, infrastructures, and sociodemographic characteristics. On the other hand, the finding of this study was lower than those studies carried out on medical students from Pokhara (81.35%)13 and India (88.18%28 and 92%29). This difference might be due to the variation in sociodemographic and economic characteristics, the different research locations, study time variation, the accessibility of OTC medications, and another possible justification might be because these studies were conducted among medical students rather than the broader population who might know the risk of self-medication.
According to the study, common cold 90 (31%), headaches 77 (26.5%), fever 75 (25.8%), and gastritis 63 (21.7%) were the most common symptoms of self-medication, which is consistent with research from Nepal11,26,30,31 and India28 who reported these to be the frequent health complaints. The present study showed that the most common reason for self-medication was mild illness 120 (41.4%) followed by previous self-experience 78 (26.9%) and lack of time to visit doctors 46 (15.9%), which is similar to the study conducted in Pokhara, Nepal11 showed the common reason was mild illness followed by previous experience of treating similar illness. However, the study conducted in Dhankuta, Nepal31 showed the most common reason was saving time visiting doctors (37.87%), which is contradictory to our study. The means of receiving self-medication was pharmacy outlets without prescription 223 (76.9%) in the study. The main reasons for choosing pharmacy outlets might be convenience, time limitation, and no consultation charges for receiving medication for the participants. The methods adopted for procuring the medicines without prescription in the present study were by mentioning the symptoms/complaints 122 (54.7%) and by mentioning the name of the medicines 113 (50.7%).
In this study, anticold drugs 91 (31.4%) were the most often used drug for self-medication over the previous 3 months, followed by NSAIDs 73 (25.6%), antipyretic (paracetamol) 68 (23.5%), and antiulcer drugs 45 (15.5%), which was skewed from the studies conducted in Pokhara11 and Dhankuta.31 This may be because the study was carried out immediately following the COVID pandemic period. Antimicrobial usage was found to be low 22 (7.6%), which was consistent with earlier investigations conducted in Nepal.11,31 However, research from Karachi32 and Abu Dhabi33 indicates an increased tendency for antimicrobial self-medication. Similarly, stopping taking medicine and preceding doctor consultations 256 (88.3%) would be their possible steps if their symptoms do not relieved. This demonstrates the sincere attitude of the participants toward rational self-medication practice.
This study showed that education level was significantly associated with self-medication which demonstrates that the practice of self-medication is influenced by education level. Other sociodemographic factors like age groups, gender, and marital status were not found to be associated with self-medication.
Limitation of the study
We are aware that our study had several limitations. First, assessed the selection and use of medicines in the last 3 months before the data collection period; therefore, recall bias could have affected the results. The insufficient number of patients recruited may be another limitation. Much larger studies are required to adequately determine the practice of self-medication.
Conclusion
Self-medication is common in KMC. The most frequent justifications for self-medication were lack of serious symptoms, prior drug use, and difficulty in getting to a doctor. Drugs, especially antimicrobials were also used as self-medication without seeking medical advice. A more specific and larger-scale study is required in the general population to evaluate the impact, role, and burden of self-medication in our country. Furthermore, national guidelines on medicine access should be reinforced to avoid the widespread harmful implications of self-medication practice among the general population.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121231158966 for Self-medication practice in Kathmandu Metropolitan City: A cross-sectional study by Prayas Ghimire, Poonam Pant, Sujata Khatiwada, Swechchha Ranjit, Sharad Malla and Sudip Pandey in SAGE Open Medicine
Acknowledgments
The authors would like to express their gratitude to the University Grant Commission for the fund. The authors would also like to thank all respondents for their willingness to participate in the study.
Footnotes
Author contributions: PG and PP developed the study concept; SK, SR, and SM conducted the data mining and analysis; and PP, PG, and SP wrote the manuscript, which was reviewed and edited by all authors.
Data sharing statements: All the data supporting the findings are within the manuscript. Additional detailed information and raw data are available from the corresponding author upon reasonable request.
Data availability: The raw data used to support the findings of this study are made available from the corresponding author upon reasonable request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: University Grant Commission (UGC) (UGC Award No.: SRDIG-76/77-HS-6), Sanothimi, Bhaktapur, Bagmati Province, Nepal.
Ethical approval: Before data collection, permission was obtained from the office of Kathmandu Metropolitan City and the Institutional Review Committee (IRC-CiST) at the Central Institute of Science and Technology, affiliated with Pokhara University, Nepal (IRC no. 49/076/077).
Informed consent: A written consent form was given to the participants in Nepali and English versions explaining all the details of it, and for illiterate subjects, informed consent was obtained by their thumb print after verbally delivering all the content written in the informed consent. Only after their agreement, their thumb print was obtained. They were informed that participation would be voluntary, and sufficient time was given to read and understand it. The identity of participants was kept confidential. Any type of economic and other benefits are not provided, and any influence was not used to collect the data from patients.
ORCID iD: Poonam Pant  https://orcid.org/0000-0002-9822-3215
https://orcid.org/0000-0002-9822-3215
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Self-Medication Industry (WSMI). The story of self-care and self-medication: 40 Years of Progress, 1970-2010. Ferney-Voltaire. [Google Scholar]
- 2. Pokharel R, Chapagain K. Prevalence of self medication among patients visiting outpatient services of ear nose and throat department of government hospital of eastern nepal and nepalese Journal of Ent Head & Neck Surgery 2016; 7: 1, https://www.njehns.org.np/index.php/njehns/article/view/158 (accessed 5 September 2022). [Google Scholar]
- 3. Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self medication. Drug Saf 2001; 24: 1027–1037. [DOI] [PubMed] [Google Scholar]
- 4. Pokharel R, Chapagain K. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Nepal J ENT Head Neck Surg 2016; 7: 1. [Google Scholar]
- 5. Ocan M, Obuku EA, Bwanga F, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health 2015; 15: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Department of Drug Administration. Drug Standard Regulation 2043 (1986). Nepal Gazette, https://www.dda.gov.np/content/drug-standard-regulation-2043 (accessed 6 November 2022).
- 7. Gore PR, Madhavan S. Consumers’ preference and willingness to pay for pharmacist counselling for non-prescription medicines. J Clin Pharm Ther 1994; 19: 17–25. [DOI] [PubMed] [Google Scholar]
- 8. Pant N, Sagtani RA, Pradhan N, et al. Self-medication with antibiotics among dental students of Kathmandu-prevalence and practice. Orig Artic Nepal Med Coll J 2015; 17: 47–53. [Google Scholar]
- 9. Horvat OJ, Tomas AD, Kusturica MMP, et al. Is the level of knowledge a predictor of rational antibiotic use in Serbia? PLoS One 2017; 12. Epub ahead of print 1 July 2017. DOI: 10.1371/JOURNAL.PONE.0180799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ocan M, Bwanga F, Bbosa GS, et al. Patterns and predictors of self-medication in Northern Uganda. PLoS One 2014; 9: e92323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shankar PR, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: a questionnaire-based study. BMC Fam Pract 2002; 3: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sah AK, Jha RK, Shah DK. Self-medication with antibiotics among nursing students of Nepal. Int J Pharma Sci Res. Epub ahead of print 2016. DOI: 10.1186/1471-2296-11-58. [DOI] [Google Scholar]
- 13. Banerjee I, Sathian B, Gupta RK, et al. Self-medication practice among preclinical university students in a medical school from the city of Pokhara, Nepal. Nepal J Epidemiol 2016; 6: 574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yadav AK, Rai BK, Budhathoki SS, et al. Self-prescription of paracetamol by undergraduate students in BP Koirala Institution of Health Sciences. JNMA 2016; 55: 11–15. [PubMed] [Google Scholar]
- 15. Abdi A, Faraji A, Dehghan F, et al. Prevalence of self-medication practice among health sciences students in Kermanshah, Iran. BMC Pharmacol Toxicol 2018; 19: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hossain S, Sikdar S, Asif MM, et al. A survey on awareness, practice and consequence of self-medication in Chittagong City, http://ilab-australia.org/ (accessed 5 September 2022).
- 17. Jember E, Feleke A, Debie A, et al. Self-medication practices and associated factors among households at Gondar town, Northwest Ethiopia: a cross-sectional study. BMC Res Notes 2019; 12: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Noone J, Blanchette CM. The value of self-medication: summary of existing evidence. J Med Econ 2018; 21: 201–211. [DOI] [PubMed] [Google Scholar]
- 19. Nusair MB, Al-azzam S, Alhamad H, et al. The prevalence and patterns of self-medication with antibiotics in Jordan: a community-based study. Int J Clin Pract 2021; 75. Epub ahead of print 1 January 2021. DOI: 10.1111/IJCP.13665. [DOI] [PubMed] [Google Scholar]
- 20. Owusu-Ofori AK, Darko E, Danquah CA, et al. Self-medication and antimicrobial resistance: a survey of students studying healthcare programmes at a Tertiary Institution in Ghana. Front public Heal 2021; 9. Epub ahead of print 8 October 2021. DOI: 10.3389/FPUBH.2021.706290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sharma HB, Gautam RP, Sisir V. District development profile of Nepal : a development database for Nepal and WorldCat.org, 2001, https://www.worldcat.org/title/district-development-profile-of-nepal-a-development-database-for-nepal/oclc/47965006 (accessed 5 September 2022).
- 22. Parajuli SB, Mishra A, Heera KC, et al. Self-medication practices in surrounding communities of Birat Medical College and Teaching Hospital of Eastern Nepal. J Coll Med Sci 2019; 15: 45–52. [Google Scholar]
- 23. Sridevi DK, Subbaiah MV, Surekha M, et al. Assessment of self medication practices among community people. IOSR J Dent Med Sci 2017; 16: 75–82. [Google Scholar]
- 24. Divya M, Bharatesh S, Vasudeva G, et al. Self-medication among adults in Urban Udupi Taluk, Southern India. Int J Med Public Heal 2016; 6: 126–129. [Google Scholar]
- 25. Shafie M, Eyasu M, Muzeyin K, et al. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One 2018; 13. Epub ahead of print 1 March 2018. DOI: 10.1371/JOURNAL.PONE.0194122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Khadka A, Kafle KK. Prevalence of self-medication among MBBS students of a medical college in Kathmandu. JNMA J Nepal Med Assoc 2020; 58: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sarraf DP, Karna G, Dhungana P, et al. Pattern of self-medication in undergraduate students at BP Koirala Institute of Health Sciences – PubMed. Kathmandu Univ Med J 2017; 15: 14–18. [PubMed] [Google Scholar]
- 28. Patil SB, Vardhamane SH, Patil BV, et al. Self-medication practice and perceptions among undergraduate medical students: a cross-sectional study. J Clin Diagn Res 2014; 8: HC20–HC23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Badiger S, Kundapur R, Jain A, et al. Self-medication patterns among medical students in South India. Australas Med J 2012; 5: 217–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bhattarai N, Basyal D, Bhattarai N. Self medication practice among undergraduate pharmacy students in Kathmandu Valley, Nepal. Int J Pharma Sci Res 2014; 5: 737–746. [Google Scholar]
- 31. Kumar Yadav B, Shrestha G, Bhattarai B, et al. Prevalence of self-medication and its associated factors in a Hilly Community of Eastern Nepal: a cross-sectional study from Dhankuta. Res Pharm Heal Sci 2020; 4: 148–153. [Google Scholar]
- 32. Shah JJ, Ahmad H, Rehan BB, et al. Self-medication with antibiotics among non-medical university students of Karachi: a cross-sectional study. BMC Pharmacol Toxicol 2014; 15: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Abasaeed A, Vlcek J, Abuelkhair M, et al. Self-medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries 2009; 3: 491–497. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121231158966 for Self-medication practice in Kathmandu Metropolitan City: A cross-sectional study by Prayas Ghimire, Poonam Pant, Sujata Khatiwada, Swechchha Ranjit, Sharad Malla and Sudip Pandey in SAGE Open Medicine


