Abstract
Background:
Anterior cruciate ligament rupture represents a career-threatening injury for professional soccer players.
Purpose:
To analyze the pattern of injury, return to play (RTP), and performance of a consecutive series of elite professional soccer players after anterior cruciate ligament reconstruction (ACLR).
Study Design:
Case series; Level of evidence, 4.
Methods:
We evaluated the medical records of 40 consecutive elite soccer players who underwent ACLR by a single surgeon between September 2018 and May 2022. Patient age, height, weight, body mass index, position, injury history, affected side, RTP time, minutes played per season (MPS), and MPS as a percentage of playable minutes before and after ACLR were retrieved from medical records and from publicly available media-based platforms.
Results:
Included were 27 male patients (mean ± SD age at surgery, 23.2 ± 4.3 years; range, 18-34 years). The injury occurred during matches in 24 players (88.9%), with a noncontact mechanism in 22 (91.7%). Meniscal pathology was found in 21 patients (77.8%). Lateral meniscectomy and meniscal repair were performed in 2 (7.4%) and 14 (51.9%) patients, respectively, and medial meniscectomy and meniscal repair were performed in 3 (11.1%) and 13 (48.1%) patients, respectively. A total of 17 players (63.0%) underwent ACLR with bone–patellar tendon–bone autograft and 10 (37.0%) with soft tissue quadriceps tendon. Lateral extra-articular tenodesis was added in 5 patients (18.5%). The overall RTP rate was 92.6% (25 of 27). Two athletes moved to a lower league after surgery. The mean MPS% during the last preinjury season was 56.69% ± 21.71%; this decreased significantly to 29.18% ± 20.6% (P < .001) in the first postoperative season and then increased to 57.76% ± 22.89% and 55.89% ± 25.8% in the second and third postoperative seasons. Two (7.4%) reruptures and 2 (7.4%) failed meniscal repairs were reported.
Conclusion:
ACLR in elite UEFA soccer players was associated with a 92.6% rate of RTP and 7.4% rate of reinjury within 6 months after primary surgery. Moreover, 7.4% of soccer players moved to a lower league during the first season after surgery. Age, graft selection, concomitant treatments, and lateral extra-articular tenodesis were not significantly associated with prolonged RTP.
Keywords: ACL injury, ACL reconstruction, elite athletes, soccer, return to play, associated injuries, LET
Anterior cruciate ligament (ACL) rupture represents one of the most common knee injuries that occurs in professional soccer players. 7,11,18 It is considered a severe threat to the player’s career because of the long rehabilitation process and the risk of further ipsi- and/or contralateral injuries. 1,3,5,23 ACL injuries result in long periods of lost play for athletes, as well as lost productivity and profitability for the clubs. Therefore, an issue that remains largely unresolved is whether elite soccer players return to the levels of play and performance after ACL rupture that they had achieved before injury and, if so, on what timeline. Several studies have pointed out the time to return to play (RTP) as well as RTP rates in elite soccer athletes. 2,27 They reported that RTP times range from 186 to 310 days, with excellent RTP rates from 77% to 95%. These studies were carried out using publicly available information, such as media-based platforms and official websites of teams and players. 10,12,20
A limit of these studies is the lack of intraoperative information, such as surgical technique, concomitant injuries to cartilage and menisci, physical examination findings, and the athlete’s psychological status. Moreover, in these studies, surgical factors and associated injuries that could affect RTP could not be investigated. Considering these limits, the present study was designed to extensively analyze the demographic characteristics, concomitant injuries, and associated surgical treatments of elite soccer players who underwent ACL reconstruction (ACLR) in our center. Our secondary aim was to establish the time to RTP, RTP rates, and player performance after ACLR in high-level soccer players.
Methods
After receiving ethics committee approval for the study protocol, we conducted a retrospective review of consecutive elite United European Football Association (UEFA) professional soccer players with a complete ACL injury who underwent ACLR at our institution. All patients underwent surgery by the senior author (C.F.) between September 2018 and May 2022. Patients with multiligamentous injuries and revision ACLR and those who had not returned to sport at the time of data collection were excluded. All patients had belonged on the first team of elite UEFA leagues (Bundesliga, Serie A, Premier League) during the ACL rupture.
All demographic and anthropometric characteristics—age, height, weight, body mass index, position, injury history, affected side, RTP time, minutes played per season (MPS), and MPS as a percentage of playable minutes—before and after ACLR were retrieved from medical records and publicly available media-based platforms: Transfermarkt (https://www.transfermarkt.com), uefa.com,fifa.com, official team websites, injury reports, official team press releases, personal websites, and professional statistical websites. These methods have commonly been used in similar research. 10,20 Concomitant injuries to menisci, cartilage, and collateral ligaments were extracted from our clinical database.
The overall RTP rate was defined as the percentage of players, among all the injured players in the study, who were able to play in at least 1 game at a professional level after ACLR. RTP time was defined as the number of days from ACL injury to the first match appearance. The mean MPS and MPS% were calculated for the preinjury season as well as the first 3 postoperative seasons for all applicable players. The first season after ACLR, with a minimum of 4 months of competition, was defined as the first season of return to sport. The second and third seasons after ACLR, regardless of the amount of time played, represented the seasons after the first season post-ACLR. Players were noted who moved to a lower league according to UEFA country ranking during the same seasons or stopped their careers for any reason during the observation period. Complications after ACLR were documented.
The RTP times were compared with respect to player age (<25 vs ≥25 years), field position, absence of cartilage and meniscal tears, lateral and medial meniscal repair, type of graft, and presence of lateral extra-articular tenodesis (LET).
Surgical Technique
All ACLR procedures were performed within 20 days from the injury. As a result of a previous study concerning graft rerupture rates, 24 hamstring tendon grafts are no longer used as our primary option for professional athletes, and soft tissue quadriceps tendon (QT) or bone–patellar tendon–bone (BTPB) grafts are the current choices for elite soccer players in our clinical practice. QT graft is the first choice in case of patellar tendinitis (ipsi- or contralateral), patella baja, patellofemoral pain, chondromalacia of the patellofemoral joint, and history of Osgood-Schlatter disease or Sinding-Larsen-Johansson syndrome. A BTPB graft is preferred in case of quadriceps tendinitis (ipsi- or contralateral) and history of rectus femur injuries.
For all players in the present study, regardless of graft type, a rectangular femoral tunnel was used as described by Fink et al. 9 A rectangular tunnel is able to cover the footprint area more efficiently with the same cross-sectional area (graft size) as compared with the round reamer. 9,25,26 For femoral graft fixation, an extracortical flip button was utilized in all grafts. The tibial tunnel was created with a conventional tibial guide and standard round reamers. For soft tissue QT grafts, a fully threaded, cannulated bioabsorbable interference screw matching the tunnel diameter was used with the suture ends tied over a cortical bone bridge. 9 Patellar tendon grafts were fixed with titanium interference screws. Concomitant meniscal tears and chondral injuries were treated considering several factors. The time from injury to surgery and the location, size, and stability of meniscal tear were considered in the choice between meniscal repair and meniscectomy. Microfractures were indicated in case of chondral lesions of ICRS grade 3 or 4 (International Cartilage Repair Society) no larger than 2 to 4 cm2. Chondroplasty was performed in case of chondral lesion of ICRS grade 1 or 2 with an unstable part. 15
LET, specifically a modified Ellison technique, 13 was added in patients considered at high risk of reinjury. Age, generalized ligamentous laxity, high-grade pivot shift, presence of Segond fracture, posterior tibial slope >12°, or history of ipsi- or contralateral ACL injuries are all factors that are taken into account during the decision process. 29 After satisfactory review at 6 months postoperatively, the progression of rehabilitation and fitness to RTP was supervised by the teams’ medical staff.
Statistical Analysis
Data were collected and analyzed using XLSTAT statistics software (Addinsoft). Normal distribution was assessed by the Shapiro-Wilk test. The study variables were recorded as mean and standard deviations or medians and IQRs (first quartile–third quartile) according to their own distribution.
The distributions of age, RTP, and MPS were asymmetric; hence, a nonparametric approach was chosen. Height and weight showed normal distribution. The Student t test or Wilcoxon rank sum test was used according to variable distributions. Statistical significance was set at P < .05.
Results
During the study period, 40 consecutive elite soccer players who underwent ACLR were assessed for eligibility. Two patients were excluded for multiligament injuries; 3 underwent revision ACL surgery; and 8 were excluded because they had ACL surgery after November 2021 and had therefore not returned to field because of the rehabilitation program. Thus, 27 male patients were included in the present study. Patient characteristics are reported in Table 1. The median age at the time of injury was 23 years (IQR, 19.5-26.5 years). The injury occurred during matches in 24 (88.9%) cases, with a noncontact mechanism in 22 (91.7%) cases. No predominant position on the field was observed. Five (18.5%) players had an ACL injury on the contralateral knee in their histories.
Table 1.
Patient Characteristics (N = 27)
| Characteristic | Mean ± SD (Range) or No. (%) |
|---|---|
| Age, y | 23.15 ± 4.3 (18-34) |
| Height, cm | 185 ± 5.2 (175-196) |
| Body mass, kg | 79.1 ± 7.3 (70-90) |
| Body mass index, kg/m2 | 23.1 ± 1.4 (20.8-25.8) |
| Position | |
| Goalkeeper | 0 (0) |
| Defender | 10 (37) |
| Midfielder | 9 (33.3) |
| Forward | 8 (29.6) |
| Foot dominance | |
| Right | 21 (77.8) |
| Left | 6 (22.2) |
| Side affected | |
| Right | 17 (63.0) |
| Left | 10 (37.0) |
| Injury occurrence | |
| Match | 24 (88.9) |
| Training | 3 (11.1) |
| Injury mechanism | |
| Contact | 5 (8.3) |
| Noncontact | 22 (91.7) |
Of the 27 patients, 17 (63.0%) underwent ACLR with BTPB autograft and 10 (37.0%) with soft tissue QT. There were 6 (22.2%) patients who underwent to isolated ACLR; the remaining 21 (77.8%) had ACLR with concomitant procedures, such as meniscal and/or cartilage procedures. A modified Ellison technique was added in 5 patients (18.5%).
Injury Patterns
Meniscal pathology was found in 21 patients (77.8%), with the lateral meniscus affected in 16 (59.3%) and the medial meniscus affected 16 (59.3%). In 11 (40.7%) players, both the medial and lateral menisci were injured. On the medial side, ramp lesion and longitudinal tears represented 31.3% and 43.8% of injuries, respectively. The most common tear on the lateral meniscus was longitudinal (62.5%), followed by posterior root avulsion (25%) (Table 2). Lateral meniscectomy and meniscal repair were performed in 2 (7.4%) and 14 (51.9%) patients, respectively. Medial meniscectomy and meniscal repair were performed in 3 (11.1%) and 13 (48.1%) patients. Seven athletes (25.9%) had chondral lesions—specifically, 5 had ICRS grade 1 or 2 injuries and 2 had ICRS grade 3 or 4 injuries. All cartilage lesions were <2 cm2.
Table 2.
Meniscal Injuries Pattern in Elite Soccer Players a
| Lesion Type | Medial | Lateral |
|---|---|---|
| Overall | 16 (59.3) | 16 (59.3) |
| Ramp | 5 (31.3) | 4 (25) |
| Bucket handle | 3 (18.8) | 1 (6.3) |
| Radial tear | 1 (6.3) | 1 (6.3) |
| Longitudinal | 7 (43.8) | 10 (62.5) |
a Data are reported as No. (%).
Five (71.4%) patients had medial or lateral femoral condyle lesions, 1 (14.3%) had patellar lesions, and 1 (14.3%) had lateral tibial plateau lesions. Microfractures and chondroplasty were performed in 1 (3.7%) and 4 (14.8%) players, respectively. Table 3 illustrates all concomitant injuries and treatments.
Table 3.
Concomitant Injuries and Procedures (N = 27) a
| Procedure or Injury | No. (%) |
|---|---|
| Graft | |
| BPTB | 17 (63.0) |
| Soft tissue QT | 10 (27.0) |
| Isolated ACLR | 6 (22.2) |
| Concomitant procedures | 21 (77.8) |
| Meniscectomy | |
| Medial | 3 (11.1) b |
| Lateral | 2 (7.4) c |
| Meniscal repair | |
| Medial | 13 (48.1) d |
| Lateral | 14 (51.9) e |
| Cartilage lesions | 7 (25.9) f |
| Patella | 1 (14.3) |
| MFC/LFC | 5 (71.4) |
| Tibial plateau | 1 (14.3) |
| Chondroplasty | 4 of 7 (57.1) |
| Nanofractures | 1 of 7 (14.3) |
| Lateral extra-articular tenodesis | 5 (18.5) |
a ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; LFC, lateral femoral condyle; MFC, medial femoral condyle; QT, quadriceps tendon.
b Two patients: lateral meniscal repair.
c One patient: medial meniscal repair.
d Eight patients: concomitant lateral repair; 1 patient with lateral meniscectomy.
e Eight patients: concomitant medial repair; 2 patients with medial meniscectomy.
f All patients with cartilage lesions had associated meniscal injuries.
Return to Play
The overall RTP rate of the 27 athletes was 92.6% (n = 25). RTP was delayed in 2 athletes (7.4%) for graft failure, with both occurring within 6 months postoperatively. Thus, 25 soccer players were included in the analysis of performance in the first season after ACLR. Of these players, 16 patients had at least 2 years of follow-up and were included in the analysis of performance in the second season after ACLR. Last, 5 patients with at least 3 years of follow-up were included for the analysis of performance in the third season after ACLR.
Specifically, 23 (85.0%) soccer players returned to the same level of professional soccer (first team of elite UEFA leagues), and 2 (7.4%) moved to a lower league (second division of professional soccer) and during the first season after ACLR. The RTP times of the athletes who moved to a lower league were 408 and 352 days. Both athletes had ACLR with medial meniscal repair. The median RTP time of all athletes was 256 days (IQR, 222.5-288 days) (Figure 1). From our analysis, we did not find any factors that significantly increased RTP time (Table 4). Concerning demographic data, the median RTP was 256 days (IQR, 227-294 days) for players <25 years old and 251.5 days (IQR, 223.8-276 days) for players ≥25 years old.
Figure 1.
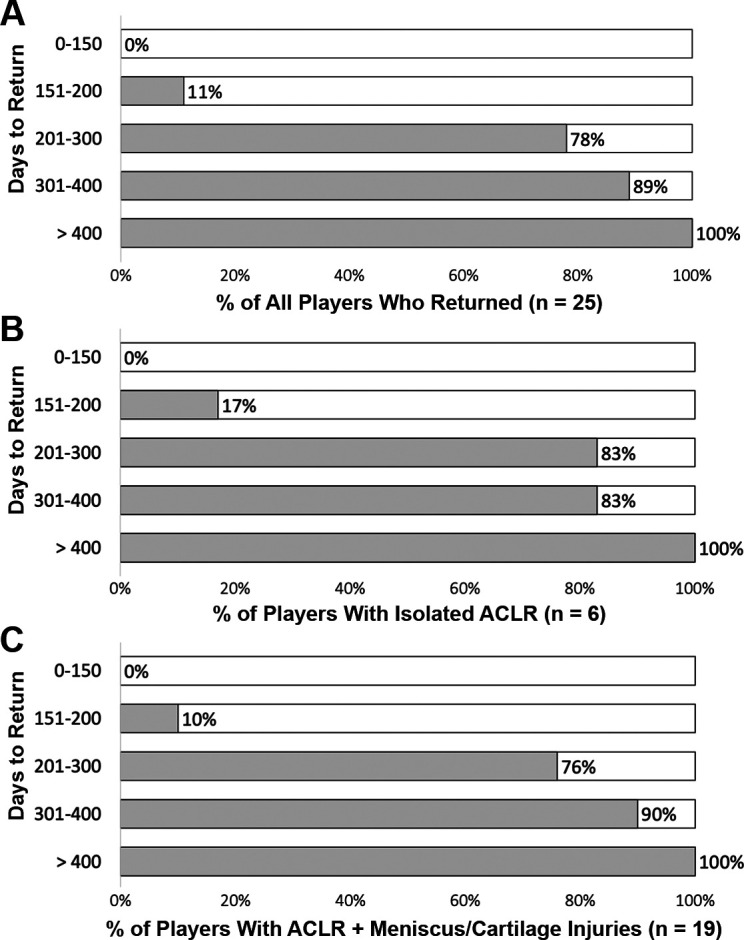
Progression of the percentage of elite soccer players who returned to play (A) overall, (B) after isolated ACLR, and (C) after ACLR with meniscal/cartilage injuries. ACLR, anterior cruciate ligament reconstruction.
Table 4.
Effect of Demographic, Pre-, Intra-, and Postoperative Factors on RTP Time in Elite Professional Soccer Players (n = 25) a
| Variable | RTP Time, d b |
|---|---|
| Overall | 267.6 ± 66.9 (173-410) |
| Age, y | |
| <25 (n = 18) | 273.3 ± 74.6 (173-410) |
| ≥25 (n = 7) | 254.1 ± 44.9 (202-339) |
| Field position | |
| Defender (n = 10) | 268.2 ± 68.2 (173-406) |
| Midfielder (n = 8) | 262.6 ± 64.6 (182-410) |
| Forward (n = 7) | 264.0 ± 66.0 (210-339) |
| Cartilage and/or meniscal injuries | |
| No chondral or meniscal tears (n = 6) | 249 ± 82.9 (173-406) |
| Meniscal injuries (n = 19) | |
| Lateral meniscal repair (n = 13) | 260.2 ± 60.4 (182-410) |
| Medial meniscal repair (n = 12) | 283.6 ± 69.1 (182-410) |
| Graft type | |
| BPTB (n = 16) | 266.6 ± 68.8 (173-410) |
| Soft tissue QT (n = 9) | 269.2 ± 67.3 (184-406) |
| LET (all grafts) | |
| ACLR with LET (n = 5) | 278.0 ± 75.3 (210-406) |
| ACLR without LET (n = 20) | 265.2 ± 66.6 (173-410) |
a Data are reported as mean ± SD (range). ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; LET, lateral extra-articular tenodesis; RTP, return to play.
b All comparisons within variables were not significant (P > .05).
Player position did not affect RTP time after ACLR. Meniscectomy and meniscal repair associated with ACLR were not associated with an increase in RTP time. Similarly, there were no significant differences in RTP with regard to graft type or addition of LET.
Player Performance
During the last season before ACL injury, the mean MPS% was 56.69% ± 21.71% (range, 21%-91%). This decreased significantly to 29.18% ± 20.6% in the first season after ACLR (P < .001 vs preinjury); however, it increased to 57.75% ± 22.89% (not significant) in the second season after ACLR and to 55.89% ± 25.8% (not significant) in the third season after ACLR (Table 5). From our analysis, 3 athletes retired after ACL injury—specifically, 1 patient stopped 4 weeks after RTP and 1 after the first postoperative season, while the third retired after the second postoperative season. The mean age of the retired players was 23 years.
Table 5.
Player Performance After RTP a
| Season | Mean ± SD or No. of Players |
|---|---|
| Last season before ACL injury | |
| MPS% | 56.69 ± 21.71 |
| First season after ACLR (n = 25) b | |
| Retired | 1 |
| Lower league | 2 |
| MPS (24 players after 1 retirement) | 1108.0 ± 868.4 |
| MPS% c | 29.18 ± 20.6 |
| Second season after ACLR (n = 16) | |
| Retired | 1 (after 1 season of play) |
| Lower league | 0 |
| MPS (15 players after 1 retirement) | 2160.1 ± 841 |
| MPS% c | 57.76 ± 22.89 |
| Third season after ACLR (n = 5) | |
| Retired | 1 (after 2 seasons of play) |
| Lower league | 0 |
| MPS (4 players after 1 retirement) | 1625.6 ± 852.5 |
| MPS% | 55.89 ± 25.8 |
a ACLR, anterior cruciate ligament reconstruction; MPS, minutes played per season; MPS%, percentage of minutes played divided by the total playable minutes during the season; RTP, return to play.
b Two players were excluded for graft failure.
Two players (19 and 20 years old) moved to a lower league after RTP and within the first season after ACLR. These athletes had a preinjury MPS% of 56.6% and 70.9%, which respectively decreased to 6.5% (owing to failure of the meniscal repair and later surgery) and 41.5% in the first postoperative season.
Complications
There were 2 (7.4%) graft reruptures, which occurred within 6 months from initial ACLR. One of these patients previously presented with a deep infection (4 weeks) after the primary ACLR after having received 2 steroid injections attributed to persistent postoperative swelling at 2 and 3 weeks after surgery. He was then treated by recurrent arthroscopic lavage and parental antibiotics. The infection resolved, and although he went on to uneventful rehabilitation, he subsequently had a reinjury during a training game 5.5 months after the initial ACL surgery. The second patient had a graft rerupture after an uncontrolled fall that was due to activities unrelated to soccer at 6 months from ACL surgery. Both players had undergone complex initial ACLR with medial and lateral meniscal repair. In 1 patient a BPTB graft was used; in the other, a soft tissue QT was used. No LET has been performed in either player. Both players went on to revision surgery (ipsi- and contralateral BPTB as well as a modified Lemaire procedure). They both returned at the field at 6.5 and 7.5 months after their revision procedures. Two (7.4%) patients had meniscal repairs that failed within 1 year from ACL surgery. Both patients had undergone medial meniscal repair with all-inside sutures for longitudinal tears. Both were addressed by arthroscopic partial meniscal resection. One (3.7%) patient was affected by a loose body from a cartilage injury of the patella, which occurred within 6 months from ACLR and was corrected by arthroscopic removal.
Discussion
The main finding of the present study was that 92.6% of professional soccer players were able to return to a professional level after ACLR. Two ACLR procedures (7.4%) failed because of graft reruptures within 6 months from surgery, and 2 athletes (7.4%) moved to a lower league. In our series, the median RTP time was 256 days (IQR, 222.5-288 days). Most of our athletes (78%) returned to professional sport within 300 days (10 months) postoperatively (Figure 1).
Erickson et al 8 and Balendra et al 1 respectively reported RTP times of 10 and 10.6 months on professional soccer players, which are similar to our results. Conversely, Niederer et al 22 cited a shorter RTP of 209 ± 93 days. However, it should be considered that only 59.4% of the patients in that study returned to their preinjury levels. Several studies revealed that choice of graft and meniscal and cartilage pathology had no statistically significant effect on RTP rate. 4,16 To the best of our knowledge, Balendra et al published the unique and original study aimed to analyze the effect of associate injuries on RTP time. They stated that graft choice, meniscal repair, and LET did not affect RTP time after ACLR. The present study showed similar results, yet the limited sample size made the research unpowered for multivariate analysis (type II error).
Most of the patients (77.8%) had meniscal injuries with subsequent associated procedures, such as ramp repair (18.9%) (Figure 2) and root repair (14.8%). This is consistent with the published literature in which the incidence of ramp lesion ranges from 9% to 34% in patients with ACL tears. 6,17,19,21,30 Regarding elite athletes, Willinger et al 30 cited a 16% incidence of ramp lesion in 100 professional soccer players. Indeed, the forceful forward displacement of the tibia that occurs during ACL rupture determines a subsequent stress on the posteromedial capsule that can result in posteromedial meniscocapsular injury. 17 Concerning lateral meniscus root tears, previous studies reported an approximate incidence of 8% in nonprofessional athletes. 14 In our cohort, we observed a posterior lateral root tear in 14.8% of elite soccer players. This difference could be due to different patient population: Elite athletes might be involved in high-energy trauma with subsequent greater risk of meniscal injuries.
Figure 2.
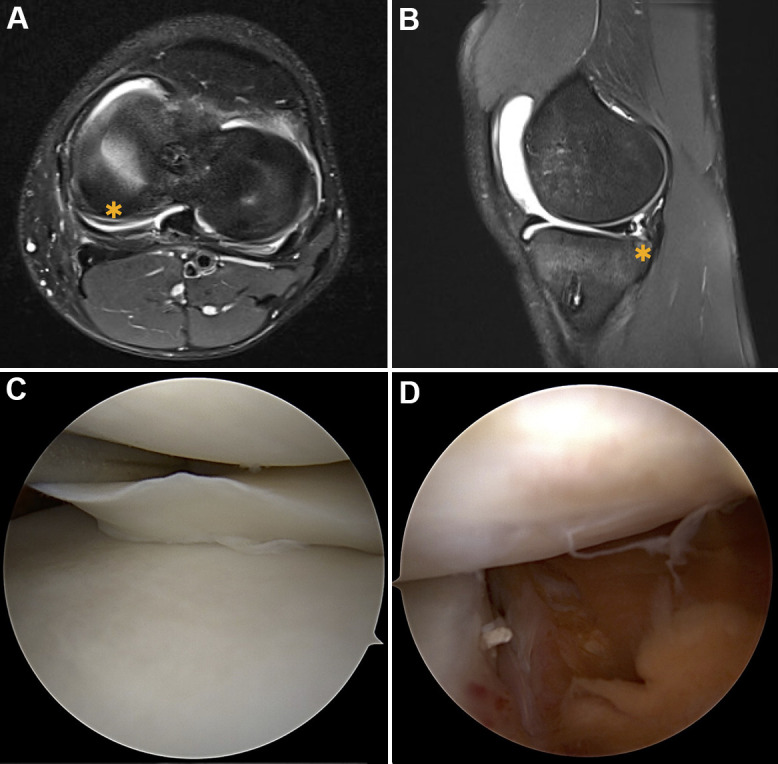
Ramp lesion (*) detected on (A) axial and (B) sagittal T2-weighted 3-T magnetic resonance imaging. Intraoperative findings from the (C) anterolateral portal and (D) transnotch views.
With respect to complications, we reported a lower rate of graft failure (7.4%; 2 of 27 elite soccer players) than the current literature. Additionally, both reruptures were not “classic” reinjury cases. One patient was complicated by postoperative infection but nevertheless joined into a training match at 5.5 months after surgery. The second soccer player had a reinjury at 6 months after surgery that was due to activities unrelated to soccer and rehabilitation. The published rate for ACL failure in elite athletes range from 3% to 22%. 3,5,28 Previous studies about elite soccer players cited consistent rates of failure in the UEFA Elite Club Injury Study (9.5%, 10%, and 9.3%). 1,5,8 The limited number of athletes in the present study could underestimate the failure rate. However, it has been demonstrated that 4% of ruptures occur before the RTP, with an additional 3% in the 3 months after RTP. 28 To confirm this, both graft failures occurred within 6 months after ACL surgery, and 27 athletes had at least 1 year of follow-up.
An overall 18.5% of soccer players had an ACL injury on the opposite side according to their history. These results are in line with the current literature. Indeed, it has been reported that almost 20% of elite soccer players sustained a second ACL injury after ACLR and return to field. 28
Limitations
The present study has several limitations. Given its retrospective design, the various surgical factors were decided by the senior author on the basis of history, clinical examination, and personal experience and not as part of a randomization process. The sample size, even though similar to other studies 3 on professional athletes, was still small, which leads to limited and underpowered statistical analysis (type II errors), and the duration of follow-up was also short. Finally, we acknowledge the limitation of online data sources. However, the publicly available sources used in the present research are the best that currently exist.
Conclusion
ACLR in elite UEFA soccer players using soft tissue QT and BPTB grafts was associated with a 92.6% rate of RTP and 7.4% rate of reinjury. Moreover, 7.4% of soccer players moved down a league during the first season after surgery. Because of the high probability of associated injuries, a systematic and careful inspection of cartilage and menisci must be performed during ACLR. Age, graft selection, concomitant treatments, and LET were not significantly associated with prolonged RTP. However, the design of the study and the sample size made the study underpowered for the multivariate analysis.
Acknowledgment
The authors thank all of the study participants for their participation and effort.
Footnotes
Final revision submitted October 18, 2022; accepted November 9, 2022.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Medical University Innsbruck (AN2015-0050).
References
- 1. Balendra G, Jones M, Borque KA, Willinger L, Pinheiro VH, Williams A. Factors affecting return to play and graft re-rupture after primary ACL reconstruction in professional footballers. Knee Surg Sports Traumatol Arthrosc. 2022;30(7):2200–2208. [DOI] [PubMed] [Google Scholar]
- 2. Barth KA, Lawton CD, Touhey DC, et al. The negative impact of anterior cruciate ligament reconstruction in professional male footballers. Knee. 2019;26(1):142–148. [DOI] [PubMed] [Google Scholar]
- 3. Bonanzinga T, Grassi A, Altomare D, et al. High return to sport rate and few re-ruptures at long term in professional footballers after anterior cruciate ligament reconstruction with hamstrings. Knee Surg Sports Traumatol Arthrosc. 2022;30(11):3681–3688. [DOI] [PubMed] [Google Scholar]
- 4. Daruwalla JH, Greis PE, Hancock R, Xerogeanes JW. Rates and determinants of return to play after anterior cruciate ligament reconstruction in NCAA Division 1 college football athletes: a study of the ACC, SEC, and PAC-12 conferences. Orthop J Sports Med. 2014;2(8):2325967114543901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Della Villa F, Hägglund M, Della Villa S, Ekstrand J, Waldén M. High rate of second ACL injury following ACL reconstruction in male professional footballers: an updated longitudinal analysis from 118 players in the UEFA Elite Club Injury Study. Br J Sports Med. 2021;55(23):1350–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(10):2233–2237. [DOI] [PubMed] [Google Scholar]
- 7. Ekstrand J, Krutsch W, Spreco A, et al. Time before return to play for the most common injuries in professional football: a 16-year follow-up of the UEFA Elite Club Injury Study. Br J Sports Med. 2020;54(7):421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male Major League Soccer players. Orthop J Sport Med. 2013;1(2):2325967113497189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fink C, Lawton R, Förschner F, Gföller P, Herbort M, Hoser C. Minimally invasive quadriceps tendon single-bundle, arthroscopic, anatomic anterior cruciate ligament reconstruction with rectangular bone tunnels. Arthrosc Tech. 2018;7(10):e1045–e1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Forsythe B, Lavoie-Gagne OZ, Forlenza EM, Diaz CC, Mascarenhas R. Return-to-play times and player performance after ACL reconstruction in elite UEFA professional soccer players: a matched-cohort analysis from 1999 to 2019. Orthop J Sport Med. 2021;9(5):23259671211008892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grassi A, Macchiarola L, Filippini M, Lucidi GA, Della Villa F, Zaffagnini S. Epidemiology of anterior cruciate ligament injury in Italian first division soccer players. Sports Health. 2020;12(3):279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grassi A, Rossi G, D’Hooghe P, et al. Eighty-two per cent of male professional football (soccer) players return to play at the previous level two seasons after Achilles tendon rupture treated with surgical repair. Br J Sports Med. 2020;54(8):480–486. [DOI] [PubMed] [Google Scholar]
- 13. Herbort M, Abermann E, Feller JA, Fink C. Anterolateral stabilization using the modified Ellison technique—treatment of anterolateral instability and reduction of ACL re-rupture risk. Article in German. Oper Orthop Traumatol. 2022;34(3):231–238. [DOI] [PubMed] [Google Scholar]
- 14. Herbst E, Hoser C, Tecklenburg K, et al. The lateral femoral notch sign following ACL injury: frequency, morphology and relation to meniscal injury and sports activity. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2250–2258. [DOI] [PubMed] [Google Scholar]
- 15. Hinckel BB, Thomas D, Vellios EE, et al. Algorithm for treatment of focal cartilage defects of the knee: classic and new procedures. Cartilage. 2021;13(1):473S–495S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Howard JS, Lembach ML, Metzler A V, Johnson DL. Rates and determinants of return to play after anterior cruciate ligament reconstruction in National Collegiate Athletic Association Division I soccer athletes: a study of the Southeastern Conference. Am J Sports Med. 2016;44(2):433–439. [DOI] [PubMed] [Google Scholar]
- 17. Kim SH, Seo HJ, Seo DW, Kim KI, Lee SH. Analysis of risk factors for ramp lesions associated with anterior cruciate ligament injury. Am J Sports Med. 2020;48(7):1673–1681. [DOI] [PubMed] [Google Scholar]
- 18. Koch M, Klügl M, Frankewycz B, et al. Football-related injuries are the major reason for the career end of professional male football players. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3560–3568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–837. [DOI] [PubMed] [Google Scholar]
- 20. Mazza D, Viglietta E, Monaco E, et al. Impact of anterior cruciate ligament injury on European professional soccer players. Orthop J Sport Med. 2022;10(2):23259671221076865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mouton C, Magosch A, Pape D, Hoffmann A, Nührenbörger C, Seil R. Ramp lesions of the medial meniscus are associated with a higher grade of dynamic rotatory laxity in ACL-injured patients in comparison to patients with an isolated injury. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1023–1028. [DOI] [PubMed] [Google Scholar]
- 22. Niederer D, Engeroff T, Wilke J, Vogt L, Banzer W. Return to play, performance, and career duration after anterior cruciate ligament rupture: a case-control study in the five biggest football nations in Europe. Scand J Med Sci Sports. 2018;28(10):2226–2233. [DOI] [PubMed] [Google Scholar]
- 23. Petersen W, Fink C, Kopf S. Return to sports after ACL reconstruction: a paradigm shift from time to function. Knee Surgery, Sport Traumatol Arthrosc. 2017;25(5):1353–1355. [DOI] [PubMed] [Google Scholar]
- 24. Runer A, Csapo R, Hepperger C, Herbort M, Hoser C, Fink C. Anterior cruciate ligament reconstructions with quadriceps tendon autograft result in lower graft rupture rates but similar patient-reported outcomes as compared with hamstring tendon autograft: a comparison of 875 patients. Am J Sports Med. 2020;48(9):2195–2204. [DOI] [PubMed] [Google Scholar]
- 25. Siebold R, Schuhmacher P, Fernandez F, et al. Flat midsubstance of the anterior cruciate ligament with tibial “C”-shaped insertion site. Knee Surgery, Sport Traumatol Arthrosc. 2015;23(11):3136–3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Śmigielski R, Zdanowicz U, Drwięga M, Ciszek B, Ciszkowska-Łysoń B, Siebold R. Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3143–3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Melick N, van Rijn L, Nijhuis-van der Sanden MWG, Hoogeboom TJ, van Cingel REH. Fatigue affects quality of movement more in ACL-reconstructed soccer players than in healthy soccer players. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):549–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50(12):744–750. [DOI] [PubMed] [Google Scholar]
- 29. Williams A, Ball S, Stephen J, White N, Jones M, Amis A. The scientific rationale for lateral tenodesis augmentation of intra-articular ACL reconstruction using a modified “Lemaire” procedure. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1339–1344. [DOI] [PubMed] [Google Scholar]
- 30. Willinger L, Balendra G, Pai V, et al. Medial meniscal ramp lesions in ACL-injured elite athletes are strongly associated with medial collateral ligament injuries and medial tibial bone bruising on MRI. Knee Surg Sports Traumatol Arthrosc. 2022;30(5):1502–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]


