Abstract
Objective
To emulate a randomized target trial to estimate the association between the antiviral drug molnupiravir and hospital admission or death in adults with SARS-CoV-2 infection in the community during the omicron predominant era who were at high risk of progression to severe covid-19.
Design
Emulation of a randomized target trial using electronic health records.
Setting
US Department of Veterans Affairs.
Participants
85 998 adults with SARS-CoV-2 infection between 5 January and 30 September 2022 and at least one risk factor for progression to severe covid-19: 7818 participants were eligible for and treated with molnupiravir and 78 180 received no treatment.
Main outcomes measure
The primary outcome was a composite of hospital admission or death at 30 days. The clone method with inverse probability of censoring weighting was used to adjust for informative censoring and balance baseline characteristics between the groups. The cumulative incidence function was used to estimate the relative risk and the absolute risk reduction at 30 days.
Results
Molnupiravir was associated with a reduction in hospital admissions or death at 30 days (relative risk 0.72 (95% confidence interval 0.64 to 0.79)) compared with no treatment; the event rates for hospital admission or death at 30 days were 2.7% (95% confidence interval 2.5% to 3.0%) for molnupiravir and 3.8% (3.7% to 3.9%) for no treatment; the absolute risk reduction was 1.1% (95% confidence interval 0.8% to 1.4%). Molnupiravir appeared to be effective in those who had not been vaccinated against covid-19 (relative risk 0.83 (0.70 to 0.97) and absolute risk reduction 0.9% (0.2% to 1.9%)), had received one or two vaccine doses (0.69 (0.56 to 0.83) and 1.3% (0.7% to 1.9%)), and had received a booster dose (0.71 (0.58 to 0.83) and 1.0% (0.5% to 1.4%)); in those infected during the era when the omicron subvariant BA.1 or BA.2 was predominant (0.72 (0.62 to 0.83) and 1.2% (0.7% to 1.6%)) and when BA.5 was predominant (0.75 (0.66 to 0.86) and 0.9% (0.5% to 1.3%)); and in those with no history of SARS-CoV-2 infection (0.72 (0.64 to 0.81) and 1.1% (0.8% to 1.4%)) and with a history of SARS-CoV-2 infection (0.75 (0.58 to 0.97) and 1.1% (0.1% to 1.8%)).
Conclusions
The findings of this emulation of a randomized target trial suggest that molnupiravir might have reduced hospital admission or death at 30 days in adults with SARS-CoV-2 infection in the community during the recent omicron predominant era who were at high risk of progression to severe covid-19 and eligible for treatment with molnupiravir.
Introduction
Randomized evidence from the MOVe-OUT (Efficacy and Safety of Molnupiravir in Non-Hospitalized Adult Participants With COVID-19) trial showed that, compared with placebo, the antiviral drug molnupiravir reduced the composite outcome of hospital admission or death at 29 days in people with covid-19.1 This international trial enrolled unvaccinated adults with mild to moderate, laboratory confirmed SARS-CoV-2 infection and at least one risk factor for severe covid-19; the trial was conducted in the pre-omicron era (between May and early October 2021) when delta was the dominant SARS-CoV-2 variant.1 In late 2021 and early 2022, regulatory agencies in the United Kingdom, United States, Europe, and several other countries issued emergency use authorization for molnupiravir for the treatment of community dwelling individuals with mild or moderate covid-19 at risk of progression to severe disease.2 By the time molnupiravir was authorized for use, omicron had replaced delta and more than four billion people around the globe (including 240 million in the US and 50 million in the UK) had received at least one dose of covid-19 vaccine. Increasingly, more people are experiencing a second SARS-CoV-2 infection.3
A recent pragmatic trial (Platform adaptive trial of novel antivirals for early treatment of COVID-19 in the community (PANORAMIC)) in vaccinated community dwelling people during the early omicron era (when subvariants BA.1 and BA.2 were predominant) at high risk of progression to severe covid-19 found that molnupiravir did not reduce the frequency of covid-19 related hospital admissions or death.4 By design, PANORAMIC excluded people at highest risk of adverse outcomes who had been advised to seek medical care from special covid-19 clinics that provide access to antivirals or monoclonal antibodies outside the trial setting.4 Overall, evidence supporting the effectiveness of molnupiravir is limited. Whether any benefit from the drug can be maintained in people of varying vaccination status is not known and it is unclear whether molnupiravir could have provided protection during periods when the omicron subvariants BA.1 or BA.2 and BA.5 were predominant or in people who experience reinfection with SARS-CoV-2. We used data from healthcare databases of the US Department of Veterans Affairs to emulate a randomized target trial to estimate whether molnupiravir offers any benefit over no treatment in reducing hospital admission or death at 30 days in adults with SARS-CoV-2 infection in the community during the omicron predominant era who have at least one risk factor for progression to severe covid-19. We emulated the trial in the overall cohort and in prespecified cohorts according to covid-19 vaccination status (not vaccinated, one or two vaccine doses, and booster), period of infection (omicron BA.1 or BA.2 predominant era and BA.5 predominant era), history of SARS-CoV-2 infection, age (≤65 years and >65 years), sex, and comorbidities (including cancer, cardiovascular disease, chronic kidney disease, and diabetes).
Methods
Specification of the target trial
We specified a randomized target trial to evaluate the efficacy of oral treatment with molnupiravir started within five days of testing positive for SARS-CoV-2 versus no treatment in reducing hospital admission or death at 30 days in adults. The specified target trial was then emulated using the healthcare databases of the US Department of Veterans Affairs.5 6 Supplementary table S1 presents the key components of the target trial protocol.
The target trial was designed to include participants with confirmed SARS-CoV-2 infection between 5 January and 30 September 2022 and with at least one risk factor for progression to severe covid-19: age >60 years, body mass index (BMI) >30, chronic lung disease, cancer, cardiovascular disease, chronic kidney disease, and diabetes. We excluded participants who received covid-19 antibody treatment, received an antiviral other than molnupiravir, were admitted to hospital at the time of study enrollment, or had end stage kidney disease or an estimated glomerular filtration rate (eGFR) <30 mL/min/1.73m2. In accordance with the US Food and Drug Administration emergency use authorization for molnupiravir, participants in the molnupiravir group were to receive treatment within five days of a covid-19 diagnosis.7 8 Participants were followed from the date of a positive SARS-CoV-2 test result until 20 October 2022. The cumulative incidence function was used to estimate the effect of initiating molnupiravir within five days of testing positive for SARS-CoV-2 (see supplementary table S1 for components of the emulation process).
Setting
The emulation was based on data from the 1293 healthcare facilities of Veterans Affairs (171 Veterans Affairs medical centers and 1112 outpatient sites) across the US. Veterans Affairs operates the largest integrated healthcare system in the US and serves discharged veterans of the US armed forces. Healthcare provided by Veterans Affairs includes preventive and health maintenance, outpatient care, inpatient hospital care, prescriptions, mental health care, home healthcare, primary care, specialty care, geriatric and extended care, medical equipment, and prosthetics.
Data sources
Data were used from the Veterans Affairs Corporate Data Warehouse (CDW), which are updated daily. Information on healthcare encounters, comorbidities, procedures, and surgeries were collected from the outpatient encounter and inpatient encounter domains; information on prescriptions from the outpatient pharmacy and bar code medication administration domains; laboratory results from the laboratory data domains; and personal information from the patient data domains. We also used the Veterans Affairs covid-19 Shared Data Resource for information on covid-19 test results and vaccination status, and the area deprivation index as a measure of contextual disadvantage at participants’ residential locations.9
Cohort
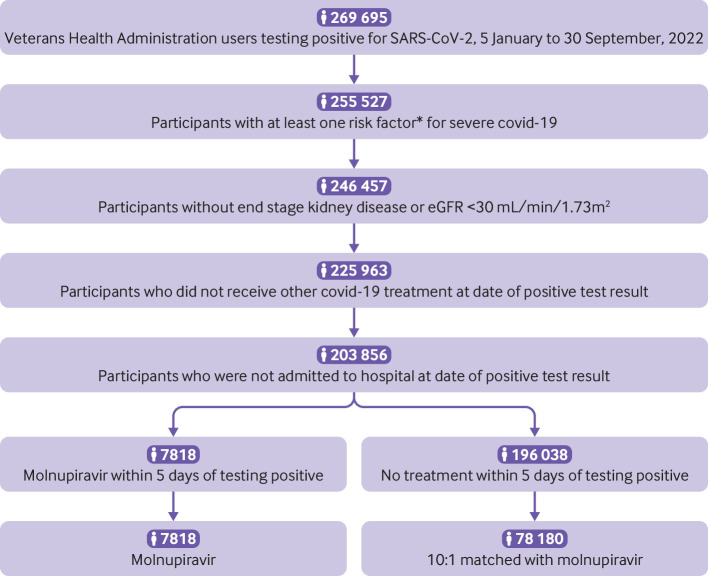
We identified 269 695 participants enrolled in the Veterans Health Administration for more than three years and who tested positive for SARS-CoV-2 between 5 January and 30 September 2022. To align with the FDA emergency use authorization for molnupiravir, we selected 255 527 participants with at least one of the following risk factors for developing severe covid-19; age >60 years, BMI >30, chronic lung disease, cardiovascular disease, chronic kidney disease, and diabetes. We then further selected those without end stage kidney disease or an estimated glomerular filtration rate (eGFR) <30 mL/min/1.73m2, which resulted in 246 457 participants. Of these participants, 225 963 did not receive other covid-19 treatment at the date of testing positive for SARS-CoV-2. After further excluding participants who were admitted to hospital at the time of a positive SARS-CoV-2 test result, the cohort comprised 203 856 participants. Overall, 7818 participants who were eligible for molnupiravir received treatment within five days of testing positive for SARS-CoV-2 and 196 038 participants received no treatment. To enhance comparability, we further restricted the no treatment group to those with a similar probability of receiving molnupiravir by matching every 10 participants in the no treatment group to one molnupiravir user based on the propensity score of receiving molnupiravir conditional on personal characteristics, vital signs, health characteristics, and other covariates (see below). The date of study enrollment was the date of a first positive test result for SARS-CoV-2, and the treatment initiation period was defined as being within five days after study enrollment. The cohort was followed until 20 October 2022.
Outcomes
The primary outcome was a composite of all cause hospital admission based on information from the inpatient database, or death based on patient vital status data. We also examined the outcomes of hospital admission and death separately.
Covariates
To adjust for confounding we specified a set of covariates,10 which were selected on the basis of the probability of a prescription for molnupiravir being issued and also the probability of hospital admission or death from previous research findings; covariates were assessed within three years before study enrollment when we chose the values before and closest to the date of study enrollment.3 11 12 13 14 15 16 17 18 19 20 21 22 A directed acyclic graph guided the selection of covariates10 (see supplementary figure S1). The covariates were age, race (White, Black, and other), sex, deprivation (area deprivation index), BMI, smoking status (current, former, and never), covid-19 vaccination status (not vaccinated, one or two vaccine doses, booster), history of SARS-CoV-2 infection, calendar week of the SARS-CoV-2 infection in 2022, influenza vaccination status, short term use of steroids (<30 days), long term care, eGFR, systolic and diastolic blood pressure, cancer, cardiovascular disease, chronic lung disease, dementia, diabetes, hyperlipidemia, and liver disease. We also considered healthcare utilization variables: number of outpatient and inpatient encounters, number of laboratory encounters and number of drugs received as an outpatient within one year before study enrollment, and number of outpatient and inpatient encounters through Medicare. Because molnupiravir is generally used as an alternative to nirmatrelvir-ritonavir, we also adjusted for covariates based on drugs that would have drug-drug interactions with nirmatrelvir-ritonavir at four levels: require an alternative covid-19 treatment to nirmatrelvir-ritonavir, require a temporary suspension of treatment with concomitant drugs, require adjustment of concomitant drug dosing, and require monitoring for adverse effects. Within our cohort, 2.6% of the eGFR, 0.4% of the systolic and diastolic blood pressure, and 0.5% of the BMI values were missing and were imputed conditional on age, race, sex, and treatment group. We transformed continuous variables into restricted cubic spline functions with four knots (at the 5th, 35th, 65th, and 95th centiles) to account for potential non-linear relationships.23
Statistical analysis
Baseline characteristics of the cohort are presented as mean and standard deviation or as frequency and percentage. Absolute standardized differences were used to evaluate balance between the groups, with an absolute standardized difference in percentage of <10 considered to show good balance.
To estimate the effect of initiating molnupiravir within five days of a positive SARS-CoV-2 test result we applied the clone method.24 25 26 Each participant was assigned (cloned) to both the treatment and the no treatment groups at the date of study enrollment. Participants were considered censored from the cloned no treatment group on the day they received molnupiravir or other covid-19 treatments within the treatment initiation period. Participants were considered censored from the cloned treatment group on the day they received other covid-19 treatments, or at the end of the treatment initiation period if they had not received treatment. Inverse probability of censoring weight at each time point during treatment initiation period was used to account for biases due to such informative censoring. Within each cloned group and within those still at risk at each time point, we used logistic regression to estimate the probability of not being censored conditional on all covariates. The inverse probability of censoring weight was calculated as the cumulative weight from day 1 of the inverse probability of not being censored and stabilized by the observed proportion of participants not being censored.27 The inverse probability of censoring weights had a mean of 1.00 (standard deviation 0.08) and resulted in covariates that were well balanced between groups. As a result, truncation of the weights was not undertaken.
Relative risk was calculated using the cumulative incidence function through the weighted non-parametric estimator.28 29 The cumulative incidence rate at 30 days for each group is reported as a percentage. We report the relative risk as the ratio of incidence rates at 30 days between the molnupiravir group and no treatment group. Absolute risk reduction was calculated as the difference in incidence rate between the molnupiravir group and no treatment group. During the estimation of hospital admission outcome, we considered death as a competing event.
Populations were then defined with different baseline characteristics and several additional trials separately emulated to estimate effectiveness of molnupiravir versus no treatment in prespecified population groups: covid-19 vaccination status (not vaccinated, one or two vaccine doses, booster), subvariant predominant during period of infection (BA.1 or BA.2 between 5 January and 22 June 2022 and BA.5 between 23 June and 30 September 20224), history of SARS-CoV-2 infection, age group (≤65 years and >65 years), sex (men and women), and the presence of comorbidities (cancer, cardiovascular disease, and chronic kidney disease) at the start of enrollment. Before using the clone method, inverse probability weighting was performed to weight all populations towards the overall cohort. The clone method, including inverse probability of censoring weight, was conducted independently within each emulated trial, and the balance of characteristics between groups was assessed for each trial based on absolute standardized differences.
We conducted sensitivity analyses to test the robustness of our results to challenge in model specification. First, we analyzed those participants without any events within the treatment initiation period, instead of the primary approach where we included those who experienced events during the treatment initiation period. Second, we defined the treatment initiation period as three days instead of five days in the primary approach. Finally, we defined the outcome as covid-19 related hospital admission or death instead of all cause hospital admission or death used in the primary approach.
Findings were considered to be statistically significant when the 95% confidence intervals for risk on a relative scale did not cross 1 or when the 95% confidence interval for risk difference on an absolute scale did not cross zero. We performed 500 iterations of non-parametric bootstrapping and considered the 2.5th and 97.5 centiles of the bootstrapped results to be the upper and lower limits of the 95% confidence interval. All analyses were performed in SAS Enterprise Guide, version 8.2 (SAS Institute).
Patient and public involvement
No patients or members of the public were directly involved in developing the study’s research question, design, and implementation. Drafts of this manuscript were, however, shared with members of the public to obtain feedback, including the informing of factors that may affect initiation of treatment in the real world, which has been incorporated in the revisions.
Results
Figure 1 shows the flow of the cohort through the study. Overall, 85 998 adults were enrolled: 7818 were eligible for and treated with molnupiravir and 78 180 received no treatment. Table 1 provides the personal and health characteristics of the overall cohort and by treatment group before weighting. Before weighting, the study cohort had a mean age of 67.3 (standard deviation 12.7), 75.7% (n=65 079) were white, and 89.5% (n=77 014) were men. Standardized mean differences of personal and health characteristics between the molnupiravir group and no treatment group at each day during the treatment initiation period (days 1 to 5) suggested good balance (see supplementary figure S2). Supplementary table S2 shows the weighted characteristics in both study groups at the end of the treatment initiation period (day 5) and supplementary table S3 the distribution of the inverse probability of censoring weight.
Fig 1.
Flow of cohort through study. *Older than 60 years, body mass index >30, chronic lung disease, cancer, cardiovascular disease, chronic kidney disease, and diabetes
Table 1.
Personal and health characteristics of the overall cohort, and both study groups before weighting in adults with SARS-CoV-2 infection in the omicron era at high risk of progression to severe covid-19 and eligible for treatment with molnupiravir. Values are number (percentage) unless stated otherwise
| Characteristics | Overall cohort (n=85 998) | Molnupiravir group (n=7818) | No treatment group (n=78 180) | Absolute SMD (%) |
|---|---|---|---|---|
| Mean (SD) age (years) | 67.3 (12.7) | 69.2 (12.0) | 67.1 (12.7) | 17.0 |
| Race: | ||||
| White | 65 079 (75.7) | 6216 (79.5) | 58 863 (75.3) | 10.1 |
| Black | 16 452 (19.1) | 1262 (16.1) | 15 190 (19.4) | 8.6 |
| Other | 4467 (5.2) | 340 (4.4) | 4127 (5.3) | 4.3 |
| Sex: | ||||
| Men | 77 014 (89.5) | 7129 (91.2) | 69 885 (89.4) | 6.1 |
| Women | 8984 (10.5) | 689 (8.8) | 8295 (10.6) | 6.1 |
| Smoking status: | ||||
| Never | 34 869 (40.5) | 3001 (38.4) | 31 868 (40.8) | 4.8 |
| Former | 36 167 (42.1) | 3544 (45.3) | 32 623 (41.7) | 7.3 |
| Current | 14 962 (17.4) | 1273 (16.3) | 13 689 (17.5) | 3.3 |
| Mean (SD) area deprivation index* | 54.4 (19.2) | 55.2 (18.8) | 54.3 (19.3) | 4.7 |
| Long term care | 918 (1.1) | 85 (1.1) | 833 (1.1) | 0.2 |
| Covid-19 vaccination status: | ||||
| None | 14 805 (17.2) | 1107 (14.2) | 13 698 (17.5) | 9.2 |
| 1 vaccine dose | 3193 (3.7) | 242 (3.1) | 2951 (3.8) | 3.7 |
| 2 vaccine doses | 22 125 (25.7) | 1838 (23.5) | 20 287 (26.0) | 5.7 |
| Booster | 45 875 (53.3) | 4631 (59.2) | 41 244 (52.8) | 13.1 |
| Mean (SD) BMI† | 30.8 (5.5) | 30.9 (5.5) | 30.8 (5.4) | 1.4 |
| Mean (SD) eGFR (mL/min/1.73m2)‡ | 77.1 (18.9) | 74.8 (19.1) | 77.3 (18.9) | 13.1 |
| Mean (SD) systolic blood pressure (mm Hg)§ | 134.0 (11.5) | 134.2 (11.5) | 133.9 (11.5) | 2.8 |
| Mean (SD) diastolic blood pressure (mm Hg)§ | 77.9 (7.0) | 77.3 (6.9) | 78 (7.0) | 9.4 |
| History of SARS-CoV-2 infection | 11 987 (13.9) | 1279 (16.4) | 10 708 (13.7) | 7.4 |
| Use of steroid | 6396 (7.4) | 664 (8.5) | 5732 (7.3) | 4.3 |
| Drugs that would have drug-drug interaction with nirmatrelvir-ritonavir: | ||||
| Require an alternative covid-19 treatment to nirmatrelvir-ritonavir | 3959 (4.6) | 751 (9.6) | 3208 (4.1) | 21.9 |
| Require temporary suspension of concomitant drug | 44 088 (51.3) | 4822 (61.7) | 39 266 (50.2) | 23.2 |
| Require adjustment of concomitant drug dosing | 36 666 (42.6) | 4033 (51.6) | 32 633 (41.7) | 19.8 |
| Require monitoring for adverse effects | 34 736 (40.4) | 3869 (49.5) | 30 867 (39.5) | 20.2 |
| Comorbidities: | ||||
| Cancer | 18 145 (21.1) | 1873 (24.0) | 16 272 (20.8) | 7.6 |
| Chronic lung disease | 25 136 (29.2) | 2649 (33.9) | 22 487 (28.8) | 11.1 |
| Dementia | 8783 (10.2) | 923 (11.8) | 7860 (10.1) | 5.6 |
| Diabetes | 35 097 (40.8) | 3521 (45.0) | 31 576 (40.4) | 9.4 |
| Cardiovascular disease | 34 948 (40.6) | 3811 (48.8) | 31 137 (39.8) | 18.0 |
| Hyperlipidemia | 37 288 (43.4) | 3650 (46.7) | 33 638 (43.0) | 7.4 |
| Liver disease | 658 (0.8) | 67 (0.9) | 591 (0.8) | 1.1 |
| Immune dysfunction | 4627 (5.4) | 461 (5.9) | 4166 (5.3) | 2.5 |
| Mean (SD No of hospital admissions¶ | 0.2 (0.8) | 0.3 (0.9) | 0.2 (0.8) | 9.2 |
| Mean (SD) No of outpatient visits¶ | 3.4 (1.4) | 3.6 (1.4) | 3.3 (1.4) | 18.6 |
| Mean (SD) No of blood tests¶ | 9.1 (10.1) | 10.7 (12.1) | 8.9 (9.9) | 16.5 |
| Mean (SD) No of drugs¶ | 12 (7.9) | 13.8 (8.4) | 11.8 (7.8) | 24.9 |
| Mean (SD) No of hospital admissions from Medicare | 0 (0.3) | 0.1 (0.3) | 0 (0.3) | 2.6 |
| Mean (SD) No of outpatient visits from Medicare | 0.2 (0.7) | 0.2 (0.7) | 0.2 (0.7) | 2.6 |
| Influenza vaccine | 62 589 (72.8) | 5993 (76.7) | 56 596 (72.4) | 9.8 |
| Mean (SD) calendar week of SARS-CoV-2 infection in 2022 | 23.7 (9.3) | 26.1 (8.8) | 23.5 (9.3) | 28.2 |
BMI=body mass index; eGFR=estimated glomerular filtration rate; SD=standard deviation; SMD=standardized mean difference.
Measure of socioeconomic disadvantage, ranging from low (0) to high (100).
0.5% of BMI values were missing and were imputed based on age, race, sex, and treatment groups.
2.6% of eGFR values were missing and were imputed based on age, race, sex, and treatment groups.
0.4% of systolic and diastolic blood pressure values were missing and were imputed based on age, race, sex, and treatment groups.
Data collected within one year before study enrollment.
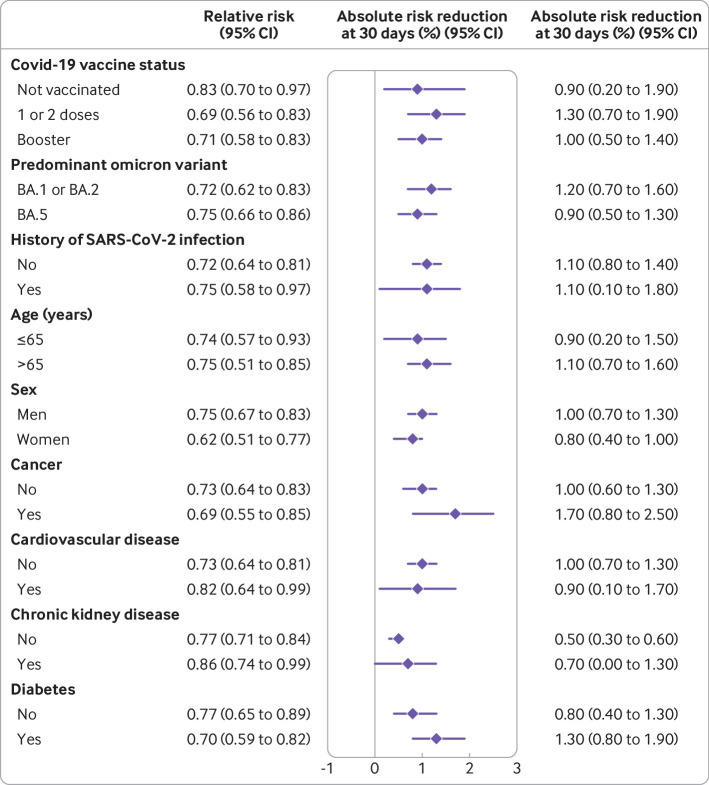
Two estimates are provided for the comparison between molnupiravir and no treatment—the relative risk of admission to hospital or death at 30 days, which represents the risk ratio of the molnupiravir arm versus no treatment arm, and the absolute risk reduction at 30 days—this estimate was based on the difference in incidence event rate between the molnupiravir and no treatment group at 30 days.
Compared with no treatment, molnupiravir was associated with a reduction in hospital admission or death at 30 days (relative risk 0.72 (95% confidence interval 0.64 to 0.79). The rate of hospital admission or death at 30 days was 2.7% (2.5% to 3.0%) for the molnupiravir group and 3.8% (3.7% to 3.9%) for the no treatment group, with an absolute risk reduction of 1.1% (95% confidence interval 0.8% to 1.4%) (fig 2 and table 2). Analyses of the individual components of the composite outcome suggested that molnupiravir was effective in reducing hospital admissions (relative risk 0.80 (0.71 to 0.90) and absolute risk reduction 0.6% (0.3% to 0.9%)) and deaths (0.35 (0.24 to 0.49) and 0.5% (0.4% to 0.6%)) (fig 3, fig 4, and table 2).
Fig 2.
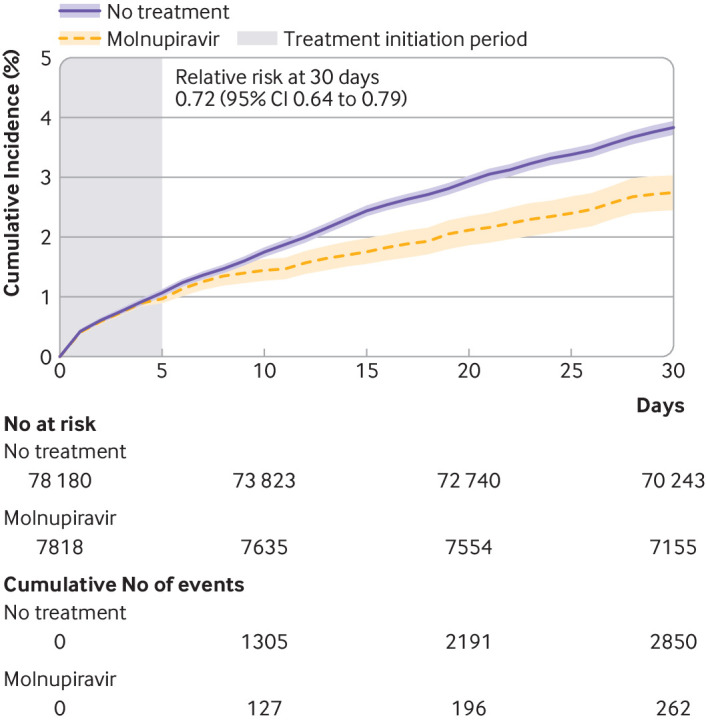
Cumulative incidence of hospital admission or death in molnupiravir (purple) and no treatment (orange) groups. Shaded area denotes treatment initiation period. Light colored bands represent 95% confidence intervals
Table 2.
Estimated relative risk, event rate, and absolute risk reduction for composite of hospital admission or death and for hospital admission and death separately at 30 days in adults with SARS-CoV-2 infection in the omicron era at high risk of progression to severe covid-19 and eligible for treatment with molnupiravir
| Outcome | Relative risk (95% CI) | Event rate (%) (95% CI) | Absolute risk reduction* (%) (95% CI) | |
|---|---|---|---|---|
| Molnupiravir group | No treatment group | |||
| Hospital admission or death | 0.72 (0.64 to 0.79) | 2.7 (2.5 to 3.0) | 3.8 (3.7 to 3.9) | 1.1 (0.8 to 1.4) |
| Hospital admission | 0.80 (0.71 to 0.90) | 2.5 (2.2 to 2.8) | 3.1 (3.0 to 3.3) | 0.6 (0.3 to 0.9) |
| Death | 0.35 (0.24 to 0.49) | 0.3 (0.2 to 0.4) | 0.8 (0.7 to 0.9) | 0.5 (0.4 to 0.6) |
CI=confidence interval.
Models adjusted for age, race, smoking status, area deprivation index, long term care use, covid-19 vaccination status, body mass index, estimated glomerular filtration rate, systolic and diastolic blood pressure, history of SARS-CoV-2 infection, steroid use, drug with drug-drug interaction with nirmatrelvir-ritonavir, cancer, chronic lung disease, dementia, diabetes, cardiovascular disease, hyperlipidemia, liver disease, immune dysfunction, healthcare utilization (number of hospital admissions, outpatient visits, blood tests, drugs), number of hospital admissions and outpatient visits from Medicare, influenza vaccine, and calendar week of SARS-CoV-2 infection in 2022 through inverse probability of censoring weight.
Difference in incident event rate between molnupiravir group and no treatment group.
Fig 3.
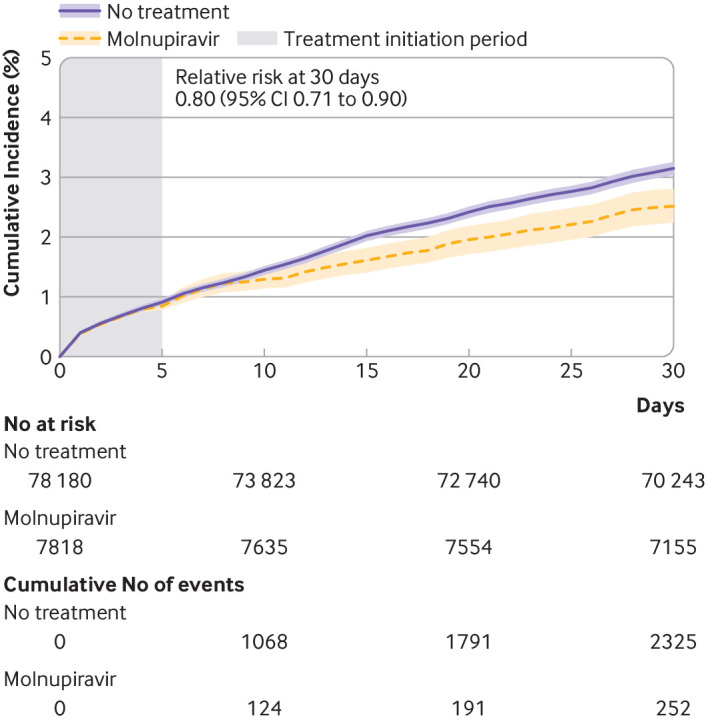
Cumulative incidence of hospital admission in molnupiravir (purple) and no treatment (orange) groups. Shaded area denotes treatment initiation period. Light colored bands represent 95% confidence intervals
Fig 4.
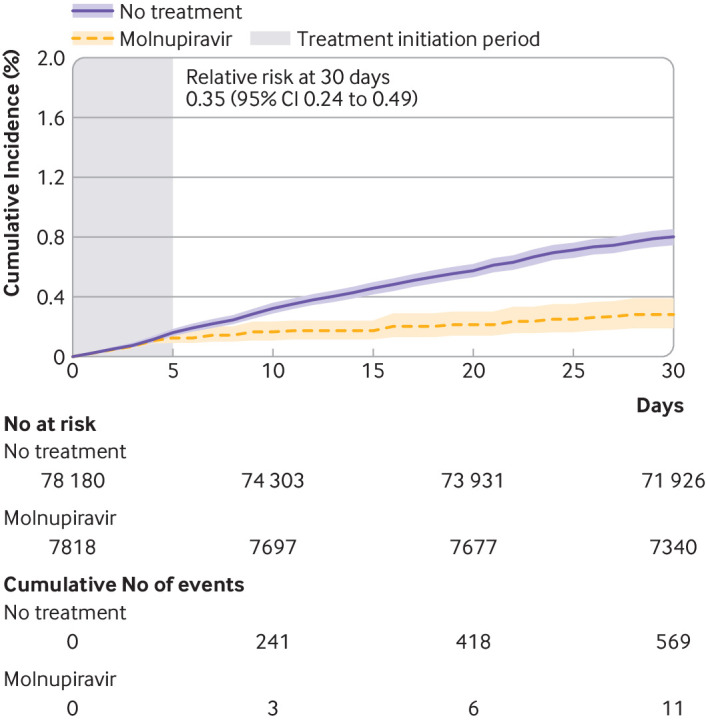
Cumulative incidence of death in molnupiravir (purple) and no treatment (orange) groups. Shaded area denotes treatment initiation period. Light colored bands represent 95% confidence intervals
Separately emulated trials in prespecified population groups suggested that molnupiravir was effective against hospital admission or death at 30 days in those who had not been vaccinated against covid-19 (relative risk 0.83 (0.70 to 0.97) and absolute risk reduction 0.9% (0.2% to 1.9%)), had received one or two vaccine doses (0.69 (0.56 to 0.83) and 1.3% (0.7% to 1.9%)), and had received a booster dose (0.71 (0.58 to 0.83) and 1.0% (0.5% to 1.4%)); those infected during the omicron BA.1 or BA.2 predominant era (0.72 (0.62 to 0.83) and 1.2% (0.7% to 1.6%) and BA.5 predominant era (0.75 (0.66 to 0.86) and 0.9% (0.5% to 1.3%); those with no history of SARS-CoV-2 infection (0.72 (0.64 to 0.81) and 1.1% (0.8% to 1.4%)) and with a history of SARS-CoV-2 infection (0.75 (0.58 to 0.97) and 1.1% (0.1% to 1.8%)); those 65 years or younger and those older than 65 years; men and women; and those with and without comorbidities, such as cancer, cardiovascular disease, chronic kidney disease, and diabetes (fig 5, table 3, and supplementary figure S3).
Fig 5.
Relative risk and absolute risk reduction for composite outcome of hospital admission or death at 30 days after testing positive for SARS-CoV-2 in prespecified populations. A separate trial was emulated for each group. CI=confidence interval
Table 3.
Relative risk, event rate, and absolute risk reduction for composite of hospital admission or death at 30 days in prespecified population groups in the omicron era at high risk of progression to severe covid-19 and eligible for treatment with molnupiravir
| Population groups | Relative risk (95% CI) | Event rate (%) (95% CI) | Absolute risk reduction* (%) (95% CI) | |
|---|---|---|---|---|
| Molnupiravir group | No treatment group | |||
| Vaccination status: | ||||
| None | 0.83 (0.70 to 0.97) | 4.7 (4.0 to 5.5) | 5.7 (5.2 to 6.1) | 0.9 (0.2 to 1.9) |
| 1 or 2 vaccine doses | 0.69 (0.56 to 0.83) | 2.9 (2.3 to 3.4) | 4.2 (3.9 to 4.4) | 1.3 (0.7 to 1.9) |
| Booster dose | 0.71 (0.58 to 0.83) | 2.4 (2.0 to 2.8) | 3.3 (3.2 to 3.5) | 1.0 (0.5 to 1.4) |
| Predominant omicron subvariant: | ||||
| BA.1 or BA.2 | 0.72 (0.62 to 0.83) | 3.0 (2.6 to 3.5) | 4.2 (4.0 to 4.4) | 1.2 (0.7 to 1.6) |
| BA.5 | 0.75 (0.66 to 0.86) | 2.7 (2.3 to 3.0) | 3.6 (3.4 to 3.8) | 0.9 (0.5 to 1.3) |
| History of SARS-CoV-2 infection: | ||||
| No | 0.72 (0.64 to 0.81) | 2.8 (2.5 to 3.2) | 4.0 (3.8 to 4.1) | 1.1 (0.8 to 1.4) |
| Yes | 0.75 (0.58 to 0.97) | 3.1 (2.4 to 3.4) | 4.1 (3.7 to 4.6) | 1.1 (0.1 to 1.8) |
| Age (years): | ||||
| ≤65 | 0.74 (0.57 to 0.93) | 2.5 (1.9 to 3.1) | 3.3 (3.0 to 3.7) | 0.9 (0.2 to 1.5) |
| >65 | 0.75 (0.65 to 0.85) | 3.3 (2.9 to 3.8) | 4.4 (4.2 to 4.6) | 1.1 (0.7 to 1.6) |
| Sex: | ||||
| Men | 0.75 (0.67 to 0.83) | 2.9 (2.7 to 3.3) | 3.9 (3.8 to 4.1) | 1.0 (0.7 to 1.3) |
| Women | 0.62 (0.51 to 0.77) | 1.2 (1.0 to 1.6) | 2.0 (1.7 to 2.3) | 0.8 (0.4 to 1.0) |
| Cancer: | ||||
| No | 0.73 (0.64 to 0.83) | 2.6 (2.3 to 2.9) | 3.5 (3.4 to 3.7) | 1.0 (0.6 to 1.3) |
| Yes | 0.69 (0.55 to 0.85) | 3.8 (3.0 to 4.6) | 5.5 (5.1 to 5.9) | 1.7 (0.8 to 2.5) |
| Cardiovascular disease: | ||||
| No | 0.77 (0.71 to 0.84) | 1.7 (1.5 to 1.9) | 2.2 (2.0 to 2.3) | 0.5 (0.3 to 0.6) |
| Yes | 0.86 (0.74 to 0.99) | 4.3 (3.7 to 4.9) | 4.9 (4.7 to 5.2) | 0.7 (0 to 1.3) |
| Chronic kidney disease: | ||||
| No | 0.73 (0.64 to 0.81) | 2.7 (2.4 to 3.0) | 3.7 (3.6 to 3.8) | 1.0 (0.7 to 1.3) |
| Yes | 0.82 (0.64 to 0.99) | 3.9 (3.1 to 4.7) | 4.8 (4.4 to 5.2) | 0.9 (0.1 to 1.7) |
| Diabetes: | ||||
| No | 0.77 (0.65 to 0.89) | 2.8 (2.4 to 3.2) | 3.6 (3.4 to 3.8) | 0.8 (0.4 to 1.3) |
| Yes | 0.70 (0.59 to 0.82) | 3.2 (2.7 to 3.7) | 4.5 (4.2 to 4.8) | 1.3 (0.8 to 1.9) |
CI=confidence interval.
Models adjusted for age, race, smoking status, area deprivation index, long term care use, covid-19 vaccination status, body mass index, estimated glomerular filtration rate, systolic and diastolic blood pressure, history of SARS-CoV-2 infection, steroid use, drug with drug-drug interaction with nirmatrelvir-ritonavir, cancer, chronic lung disease, dementia, diabetes, cardiovascular disease, hyperlipidemia, liver disease, immune dysfunction, healthcare utilization (number of hospital admissions, outpatient visits, blood tests, drugs), number of hospital admissions and outpatient visits from Medicare, influenza vaccine, and calendar week of SARS-CoV-2 infection in 2022 through inverse probability of censoring weight.
Difference in incident event rate between molnupiravir group and no treatment group.
Sensitivity analyses
We conducted sensitivity analyses to test the robustness of results. First, we conducted analyses only in participants with no events during the treatment initiation period (in the primary approach we included participants with events during this period). Second, we conducted a separate trial emulation process in which the treatment initiation period was three days from a positive SARS-CoV-2 test result (in the primary approach this period was five days after a positive result). Finally, we evaluated the effectiveness of molnupiravir in reducing the risk of covid-19 related hospital admission or death (in the primary approach the outcome was all cause hospital admission or death). All sensitivity analyses yielded results consistent with the primary approach, suggesting that molnupiravir was effective in reducing hospital admission or death at 30 days compared with no treatment (see supplementary table S4).
Discussion
The findings of this study emulating a randomized target trial suggest that molnupiravir is effective in reducing hospital admission or death at 30 days and is effective in those who have not been vaccinated against covid-19, have received one or two vaccine doses, and have received a booster dose; those infected during the omicron predominant era (BA.1 or BA.2 and BA.5); those with no history of SARS-CoV-2 infection and with a history of SARS-CoV-2 infection; in those 65 years and younger and older than 65 years; men and women; and those with and without cancer, cardiovascular disease, chronic kidney disease, and diabetes.
Findings in relation to other studies
Until recently, the only randomized trial to evaluate the efficacy of oral molnupiravir in adults was performed in unvaccinated participants in the pre-omicron era.1 This study did not, however, represent the many people worldwide who have been vaccinated against covid-19 (eg, as of 17 February 2023 69.5% of the world’s population has received at least one vaccine dose) and who may be exposed to a subvariant of omicron. Our study extends this evidence base to the eras when three subvariants of omicron predominated in the US—BA.1 and BA.2 from 5 January (beginning of study enrollment) to 22 June 2022, and BA.5 from 23 June to 30 September 2022 (end of study enrollment)). The results suggest that molnupiravir was effective in both these periods and that the magnitude of effectiveness was similar.
The number of people reinfected with SARS-CoV-2 globally is increasing.3 Reinfection is associated with increased risk of mortality and with serious adverse health outcomes in the acute and post-acute phase.3 Based on current evidence, it is unclear whether molnupiravir continues to show effectiveness in reducing the risk of hospital admission or death during the acute phase of reinfection. Our analyses supplement the evidence base and suggest that molnupiravir might retain similar effectiveness in people with and without previous SARS-CoV-2 infection.
In the MOVe-OUT trial, which included unvaccinated adults at high risk of progression to severe covid-19, molnupiravir reduced the risk of hospital admission or death at 29 days (relative risk 0.70, v 0.72 in our study, and absolute risk reduction 3.0%, v 1.1% in our study).1 In our study the absolute risk reduction was more modest, possibly because of the lower baseline risk in our cohort (event rates were 3.8% in the control arm in our study v 9.7% in MOVe-OUT). A recent pragmatic trial (PANORAMIC) during the BA.1 and BA.2 predominant era that included vaccinated participants at high risk of progression to severe covid-19 found that molnupiravir did not reduce the risk of hospital admission or death (adjusted odds ratio 1.06 (95% bayesian credible interval 0.81 to 1.41)).4 The difference between our results and those of PANORAMIC could be explained by variations in study setting, recruitment strategy, and definition of the intervention (see supplementary table S5). Because patients at the highest risk of adverse outcomes with covid-19 in the UK were advised to seek medical advice from special regional covid-19 specialist clinics with access to antivirals or monoclonal antibodies, they were not the target population of PANORAMIC.4 Consequently, PANORAMIC’s findings might be less applicable to patients in this highest risk category.4 In PANORAMIC’s control groups, the 28 day event rates were 1% for hospital admission or death and 0.04% for death compared with 30 day event rates in our control group of 3.8% for hospital admission or death and 0.8% for death. The difference in baseline risk between PANORAMIC and our study also supported by the comparison of baseline characteristics where the PANORAMIC trial included a relatively younger (average age 56.7, v 67.3 years in our study) and healthier population (eg, in PANORAMIC 8% had cardiovascular disease and 12% had diabetes v 40.6% and 40.8%, respectively, in our study). In addition, PANORAMIC allowed outpatient treatment of covid-19 in the control group (molnupiravir, monoclonal antibodies, remdesivir or nirmatrelvir) and outpatient treatment of covid-19 other than molnupiravir in the treatment group during usual care, whereas in our emulated trial we estimated the effectiveness of using only molnupiravir as outpatient treatment compared with no treatment. Taken together, the results from MOVe-OUT, PANORAMIC, and our analysis suggest the possibility of graded erosion in effectiveness of molnupiravir as the baseline risk (risk in the control group) of the target population decreases—suggesting that those at the highest risk of progression to severe covid-19 are likely to derive most benefit.
We provided risk estimates on both a relative scale and an absolute scale. The relative risk provides estimates of effectiveness independent of baseline risk, whereas the absolute risk reduction additionally reflects the baseline risk in the studied population; and both these effect estimates should be interpreted along with their uncertainty intervals (confidence intervals). For example, Although the absolute rates in both the molnupiravir and the no treatment arms appeared to be reduced in those who had received a covid-19 booster dose compared with unvaccinated people, both the relative risk and the absolute risk reduction are maintained.
Strengths and limitations of this study
This study has several strengths. We used data from healthcare databases of the US Department of Veterans Affairs, which operates the largest nationally integrated healthcare system in the US, to emulate a target trial to estimate the real world effectiveness of molnupiravir. To comprehensively capture information of the cohort from the three years before study enrollment, we used data from multiple domains: covid-19 data repository, vaccination records, drug prescription records, diagnosis codes, laboratory records, hospital admission records, and death records. We leveraged advances in causal inference methodologies and applied the clone method to adjust for bias because of the time difference between treatment initiation and infection. Relative risk was estimated in clinically meaningful population groups by vaccination status, period of infection (eras when the omicron subvariants BA.1 or BA.2 and BA.5 were predominant), previous SARS-CoV-2 infection, age, sex, and clinical comorbidities. Such an approach may be useful in informing clinical decision making. To test the robustness of our approach to changes in specification, we conducted sensitivity analyses.
This study also has several limitations. Most of the participants were White and men, which limits generalizability of the findings. Although we emulated a randomized target trial, leveraging the breadth of Veterans Affairs data, and advanced causal inference methodologies, we cannot completely rule out residual confounding or misclassification bias. Those eligible for and treated with molnupiravir had a higher baseline health burden, such as older age and higher prevalence of risk factors for progression to severe covid-19 than those who received no treatment; residual confounding, if present, may have resulted in underestimation of the findings for molnupiravir. Misclassification of drug use is possible if people obtained prescriptions for molnupiravir from outside the Veterans Affairs system. Although such prescribing is rare, if present in large numbers the findings for molnupiravir would have been underestimated. Misclassification of covariates, such as history of SARS-CoV-2 infection, if present, would have occurred to a similar degree across treatment arms after adjusting for healthcare utilization and health seeking behaviors. Misclassification of outcomes (ie, undercounting hospital admission or death) is unlikely; if present, misclassification would most probably be similar across treatment arms and therefore the relative risk is unlikely to be biased but the absolute risk reduction would be underestimated. We did not examine adverse events. We also did not evaluate the risk of post-acute outcomes—an area of intense interest that should be investigated in future research.30 31 Finally, the covid-19 pandemic is still evolving dynamically, and the effectiveness of therapeutics may change as the virus mutates and as other characteristics of the pandemic develop over time.
Conclusions
Emulation of a randomized target trial in adults with SARS-CoV-2 infection in the community at high risk of progression to severe covid-19 suggested that molnupiravir might reduce hospital admission or death at 30 days in those who have not been vaccinated against covid-19, have received one or two vaccine doses, and have received a booster dose; were infected during the era when the omicron subvariants BA.1 or BA.2 and BA.5 were predominant; and have a history of or no history of SARS-CoV-2 infection; and in subgroups based on age, sex, and comorbidities.
What is already known on this topic
In a randomized placebo controlled trial (MOVe-OUT) in unvaccinated people with SARS-CoV-2 infection in the pre-omicron era, molnupiravir reduced the composite outcome of hospital admission or death at 29 days
In a pragmatic trial (PANORAMIC) that enrolled participants during the early omicron era (BA.1 and BA.2) and included vaccinated participants at risk of progression to severe covid-19 but not people at the highest risk who would otherwise qualify for molnupiravir through standard care, molnupiravir did not reduce the risk of hospital admission or death
What this study adds
This emulation of a randomized target trial in adults with SARS-CoV-2 infection in the community during the omicron predominant era at high risk of progression to severe covid-19 and eligible for treatment with molnupiravir, suggested that molnupiravir reduced hospital admission or death at 30 days compared with no treatment
Molnupiravir appeared to be effective in those who were not vaccinated against covid-19, had received one dose or two vaccine doses, and had received a booster dose; those infected during the omicron era when subvariants BA.1 or BA.2 and BA.5 were predominant; and in those with no history or a history of SARS-CoV-2 infection
Web extra.
Extra material supplied by authors
Supplementary information: Figures S1-S3 and tables S1-S5
Contributors: ZAA and YX conceived and designed the study, analyzed the data and interpreted the results, and drafted the manuscript. ZAA, YX, and BB critically revised the manuscript. ZAA provided administrative, technical, and material support, as well as supervision and mentorship. Each author contributed important intellectual content during drafting or revision of the manuscript and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. All authors approved the final version of the report. ZAA is the guarantor. The contents do not represent the views of the US Department of Veterans Affairs or the US government. The corresponding author attests that all the listed authors meet the authorship criteria and that no others meeting the criteria have been omitted.
Funding: This research was funded by the US Department of Veterans Affairs (ZAA). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from the US Department of Veterans Affairs for the submitted work. BB reports receiving consultation fees from AstraZeneca. ZAA reports receiving consultation fees from Gilead Sciences and receipt of funding (unrelated to this work) from Tonix pharmaceuticals. ZAA reports consulting (uncompensated) for Pfizer.
The lead author (ZAA) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Dissemination to participants and related patient and public communities: The authors have no specific plans to disseminate the findings to study participants. However, study results will be disseminated via a press release with mainstream media and will also be promoted on twitter (via the corresponding senior author’s account @zalaly). We will also share the findings with public health agencies and our contacts in the US government (the US covid-19 task force), British government, and the Canadian government (the Office of the Chief Science Advisor of Canada). The results will be shared with advocacy groups and will be presented in scientific meetings and at academic institutions.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
This study was approved by the institutional review board of the VA Saint Louis Health Care System (protocol No 1606333).
Data availability statement
The data that support the findings of this study are available from the US Department of Veterans Affairs. Veterans Affairs data are made freely available to researchers behind a firewall with an approved Veterans Affairs study protocol. For more information, please visit https://www.virec.research.va.gov or contact VIReC@va.gov.
References
- 1. Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. MOVe-OUT Study Group . Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients. N Engl J Med 2022;386:509-20. 10.1056/NEJMoa2116044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Extance A. Covid-19: What is the evidence for the antiviral molnupiravir? BMJ 2022;377:o926. 10.1136/bmj.o926. [DOI] [PubMed] [Google Scholar]
- 3. Bowe B, Xie Y, Al-Aly Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat Med 2022;28:2398-405. 10.1038/s41591-022-02051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Butler CC, Hobbs FDR, Gbinigie OA, et al. PANORAMIC Trial Collaborative Group . Molnupiravir Plus Usual Care Versus Usual Care Alone as Early Treatment for Adults with COVID-19 at Increased Risk of Adverse Outcomes (PANORAMIC): Preliminary Analysis from the United Kingdom Randomised, Controlled Open-Label, Platform Adaptive Trial. Lancet 2023;401:281-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hernán MA, Robins JM. Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available. Am J Epidemiol 2016;183:758-64. 10.1093/aje/kwv254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dickerman BA, García-Albéniz X, Logan RW, Denaxas S, Hernán MA. Avoidable flaws in observational analyses: an application to statins and cancer. Nat Med 2019;25:1601-6. 10.1038/s41591-019-0597-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. MOVe-OUT Study Group . Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients. N Engl J Med 2022;386:509-20. 10.1056/NEJMoa2116044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Food and Drug Administration. Emergency Use Authorization 108. 2022.
- 9. Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med 2018;378:2456-8. 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Matthews AA, Danaei G, Islam N, Kurth T. Target trial emulation: applying principles of randomised trials to observational studies. BMJ 2022;378:e071108. 10.1136/bmj-2022-071108. [DOI] [PubMed] [Google Scholar]
- 11. Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 2021;594:259-64. 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]
- 12. Xie Y, Bowe B, Maddukuri G, Al-Aly Z. Comparative evaluation of clinical manifestations and risk of death in patients admitted to hospital with covid-19 and seasonal influenza: cohort study. BMJ 2020;371:m4677. 10.1136/bmj.m4677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bowe B, Cai M, Xie Y, Gibson AK, Maddukuri G, Al-Aly Z. Acute Kidney Injury in a National Cohort of Hospitalized US Veterans with COVID-19. Clin J Am Soc Nephrol 2020;16:14-25. 10.2215/CJN.09610620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bowe B, Xie Y, Xu E, Al-Aly Z. Kidney Outcomes in Long COVID. J Am Soc Nephrol 2021;32:2851-62. 10.1681/ASN.2021060734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med 2022;28:583-90. 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ 2022;376:e068993. 10.1136/bmj-2021-068993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med 2022;28:1461-7. 10.1038/s41591-022-01840-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol 2022;10:311-21. 10.1016/S2213-8587(22)00044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xu E, Xie Y, Al-Aly Z. Long-term neurologic outcomes of COVID-19. Nat Med 2022;28:2406-15. 10.1038/s41591-022-02001-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xie Y, Bowe B, Al-Aly Z. Burdens of post-acute sequelae of COVID-19 by severity of acute infection, demographics and health status. Nat Commun 2021;12:6571. 10.1038/s41467-021-26513-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Xu E, Xie Y, Al-Aly Z. Risks and burdens of incident dyslipidaemia in long COVID: a cohort study. Lancet Diabetes Endocrinol 2023;11:120-8. 10.1016/S2213-8587(22)00355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Xu E, Xie Y, Al-Aly Z. Long-term gastrointestinal outcomes of COVID-19. Nat Commun 2023;(In press). 10.1038/s41467-023-36223-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrell Jr FE. Regression Modeling Strategies With Applications To Linear Models, Logistic And Ordinal Regression, And Survival Analysis. pdf.
- 24. Hernán MA, Sauer BC, Hernández-Díaz S, Platt R, Shrier I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol 2016;79:70-5. 10.1016/j.jclinepi.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hernán MA, Robins JM. Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available. Am J Epidemiol 2016;183:758-64. 10.1093/aje/kwv254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Maringe C, Benitez Majano S, Exarchakou A, et al. Reflection on modern methods: trial emulation in the presence of immortal-time bias. Assessing the benefit of major surgery for elderly lung cancer patients using observational data. Int J Epidemiol 2020;49:1719-29. 10.1093/ije/dyaa057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models [published Online First: 2008/08/07]. Am J Epidemiol 2008;168:656-64. 10.1093/aje/kwn164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Austin PC, Lee DS, Fine JP. Introduction to the Analysis of Survival Data in the Presence of Competing Risks. Circulation 2016;133:601-9. 10.1161/CIRCULATIONAHA.115.017719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Willems S, Schat A, van Noorden MS, Fiocco M. Correcting for dependent censoring in routine outcome monitoring data by applying the inverse probability censoring weighted estimator. Stat Methods Med Res 2018;27:323-35. 10.1177/0962280216628900. [DOI] [PubMed] [Google Scholar]
- 30. Al-Aly Z, Agarwal A, Alwan N, et al. Long COVID: long-term health outcomes and implications for policy and research. Nat Rev Nephrol 2022;1-2. 10.1038/s41581-022-00652-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Al-Aly Z. Diabetes after SARS-CoV-2 infection. Lancet Diabetes Endocrinol 2023;11:11-3. 10.1016/S2213-8587(22)00324-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information: Figures S1-S3 and tables S1-S5
Data Availability Statement
The data that support the findings of this study are available from the US Department of Veterans Affairs. Veterans Affairs data are made freely available to researchers behind a firewall with an approved Veterans Affairs study protocol. For more information, please visit https://www.virec.research.va.gov or contact VIReC@va.gov.