Abstract
There were substantial ethnic disparities in the incidence rates of triple-negative breast cancer, but few studies were conducted on the incidence trend of triple-negative breast cancer by race/ethnicity. This study aimed to address the longer trends in the incidence of triple-negative breast cancer by race/ethnicity in women from 2010 to 2019, examine the incidence trends by patient age, tumor stage and time periods, and explore the changing proportions of three component receptors over time for triple-negative breast cancer. Our study identified 573,168 women with incident breast cancer at age ≥20 years between 2010 and 2019 in 18 SEER (Surveillance, Epidemiology, and End Results) registries. Of them, 62,623 (10.9%) were incident triple-negative breast cancer and 510,545 were non-triple negative breast cancer cases. The denominator of population included 320,117,009 women aged ≥20 in the same SEER areas. The study found that overall age-adjusted incidence rate of triple-negative breast cancer in women aged ≥20 years was 18.3 cases per 100,000 women. Age-adjusted incidence rate of triple-negative breast cancer was the highest in black women (33.8 cases per 100,000 women), followed by white (17.5), American Indian and Alaska Native (AIAN) (14.7), Hispanic (14.7), and Asian women (12.4). The significantly higher age-adjusted incidence of triple-negative breast cancer in black women as compared to white women appeared to be limited in younger women aged 20-44 only. Annual percentage changes in age-adjusted incidence of triple-negative breast cancer slightly decreased insignificantly in white, black and Asian women aged 20-44 and 45-54 years. There was a statistically significant annual percentage increase in age-adjusted incidence of triple-negative breast cancer in Asian and black women aged ≥55 years. In conclusion, there was a significantly higher incidence of triple-negative breast cancer in black women aged 20-44 years. From 2010 to 2019, there were no significant annual percentage changes in age-adjusted incidence of triple-negative breast cancer in all ethnic groups of women aged <55 years, with the exception of a significant decrease among AIAN women aged 45-54 years. However, there was a statistically significant annual percentage increase in age-adjusted incidence of triple-negative breast cancer in Asian and black women aged ≥55 years.
Keywords: Triple-negative breast cancer, cancer incidence, incidence trend, racial disparities, SEER
Introduction
It has been well documented that breast cancer incidence rates varied significantly by race and ethnicity with a higher risk of breast cancer in non-Hispanic (NH) white and black women and a lower risk in women from Hispanics, Asians and Pacific Islanders, and American Indians and Alaska Natives (AIAN) [1-8]. From 2000 to 2018, there was a slightly increasing trend in overall breast cancer incidence for all ethnic women in the United States, except for NH-white women who experienced a decreasing trend [9]. Over the past decade, there have been an increasing number of investigations on the incidence of an aggressive molecular subtype of breast cancer, i.e., triple-negative breast cancer which refers to the fact that estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor-2 (HER2) are all negative [10-19]. Triple-negative breast cancer is more aggressive, tends to grow and spread faster, and currently has fewer options of effective treatment, leading to worse outcomes and higher mortality [15,20]. Triple-negative breast cancer accounts for approximately 10%~15% of all breast cancers in women and appears to be more common in black women [10-19]. A number of studies reported racial and ethnic disparities in the incidence rates of triple-negative breast cancer [21-25]. Only one study specifically examined the incidence trends of molecular subtypes of breast cancer by race/ethnicity over multiple years from 2010 to 2016 [25], which concluded that triple-negative breast cancer incidence rates decreased among midlife non-Hispanic white and black women. This current study aims to 1) address the longer trends in the incidence of triple-negative breast cancer by race/ethnicity in women in the SEER areas from 2010 to 2019, 2) examine the incidence trends stratified by patient age, tumor stage and time periods, and 3) explore the changing proportions of three component receptors over time to see if any factor is the main driver for triple-negative breast cancer incidence trend.
Methods
Data sources
The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Public Use Datasets released in November 2021 were used for this study. Both breast cancer cases (numerator) and population (denominator) from SEER areas from 2010 to 2019 are available for cancer incidence calculation [26]. The year 2010 is the earliest year for triple-negative breast cancer data available in SEER data and the year 2019 is the latest dataset. The SEER program supports 18 population-based tumor registries in 9 areas (San Francisco/Oakland, San Jose-Monterey, Los Angeles, Greater California, Detroit, Seattle, Atlanta, Rural Georgia, and Greater Georgia) and 9 states (Alaska, Connecticut, Iowa, New Mexico, Utah, Hawaii, Louisiana, Kentucky, and New Jersey), accounting for 28% of the U.S. population. The SEER registries ascertain all newly diagnosed (incident) cancer cases from multiple reporting sources. The estimated completeness of cancer case reporting in SEER areas was 97.7% [26]. Cancer-related variables collected in SEER registries include tumor location and size; histologic type and grade of tumor; demographic characteristics such as age, gender, race/ethnicity, and marital status; and type of treatments provided in the first course of therapy after diagnosis. This study was considered exempt for Institutional Review Board (IRB) review because it did not involve any patient contact, only had the analysis of de-identified existing SEER Public Use Data, and had no any health risk to study subjects.
Study population
Our study identified 573,168 women who were diagnosed with incident breast cancer at age ≥20 years between 2010 and 2019 in 18 SEER registries. Of them, 62,623 (10.9%) were incident triple-negative breast cancer and 510,545 (89.1%) were non-triple negative breast cancer cases. Because this study focused on the incidence trend of triple-negative breast cancer [hormone receptor (HR) negative: HR-/HER2-], other three groups of breast cancer (HR+/HER2+, HR+/HER2-, and HR-/HER2+) were considered as non-triple negative breast cancers. The denominator of population data included all 320,117,009 women aged ≥20 years in the same SEER areas that were provided in the SEER*Stat package.
Study variables
Race/ethnicity variable was classified into non-Hispanic white (white), non-Hispanic black (black), non-Hispanic Asians/Pacific Islanders (Asian), Hispanic women, and American Indians and Alaska Natives (AIAN), and others or unknown race. Patients with unknown or missing information on race/ethnicity were included for the incidence calculation for overall population and some sup-total stratified groups, but were not presented as a separate race/ethnicity group because the SEER*Stat software did not provide this incidence information for this group. Patient age was divided into 3 broad groups as young (20-44 years), middle-age (45-54) who were recommended to start for regular screening, and older age (≥55) in order to avoid small number of cases in stratified analyses by race/ethnicity, tumor stage, age group, and year of diagnosis. The other covariates included year of diagnosis (2010 to 2019) and geographic areas (18 SEER registries). Tumor factors included triple-negative vs non-triple negative breast cancer, estrogen receptor status, progesterone receptor status, HER2 receptor status, and tumor stage (in-situ or local, regional, distant stage, or unknown/missing).
Statistical analysis
We utilized the SEER*Stat software (version 8.4.0.1) that was provided by the National Cancer Institute together with the SEER data for analyses in cancer incidence rates and trends. Incidence of breast cancer in women is defined as a ratio of the number of women with a new breast cancer at age ≥20 years over the number of total female population at age ≥20 years in the same SEER areas by year, which is presented as the number of breast cancer cases per 100,000 persons. Because age is a significant risk factor for cancer incidence, the incidence rates of breast cancer in all comparison groups by race/ethnicity or time periods that may consist of different age compositions are standardized by age. The incidence rates in this study are adjusted to the year 2000 U.S. population by age available from the SEER*Stat. The age-adjusted incidence rates, 95% confidence intervals for incidence rates, incidence rate ratios (IRR) and their 95% confidence intervals, and annual percentage change (APC) of incidence rates are calculated from the SEER*Stat software. A p value <0.05 is considered statistically significant.
Results
Table 1 presents the number of total female population, number of incident triple-negative breast cancer cases, number of incident non-triple-negative breast cancer cases, unadjusted and age-adjusted breast cancer incidence rates, and incidence rate ratio by race/ethnicity. The overall age-adjusted incidence rate of triple-negative breast cancer in women aged ≥20 years was 18.3 cases per 100,000 women. The age-adjusted incidence rate of triple-negative breast cancer was the highest in black women (33.8 cases per 100,000 women), followed by white (17.5), AIAN (14.7), Hispanic (14.7), and Asian women (12.4). When compared to white women, the incidence rate ratio was statistically significantly higher in black women (incidence rate ratio: 1.93, 95% CI: 1.88-1.97) and significantly lower in AIAN (0.84, 0.75-0.93), Hispanic (0.84, 0.82-0.86), and Asian women (0.71, 0.68-0.73). However, the patterns of age-adjusted incidence rates of non-triple-negative breast cancer cases by race/ethnicity were different. The age-adjusted non-triple-negative breast cancer incidence rate ratio was statistically significantly lower in black women (0.83, 0.83-0.84) and in all other ethnic women as compared to white women (Table 1).
Table 1.
Number of population, number of triple-negative breast cancer cases and non-triple negative breast cancer, and incidence rates of breast cancer in all SEER areas, 2010-2019, by race/ethnicity
| Race/Ethnicity | Number of population | Number of breast cancer cases | Unadjusted Incidence rates (N of cases per 100,000) (95% CI) | Age-adjusted* incidence rates (N of cases per 100,000) (95% CI) | Rate ratio (between age-adjusted incidence rates) (95% CI) |
|---|---|---|---|---|---|
| Triple-negative breast cancer | |||||
| Non-Hispanic white | 178,531,435 | 36,695 | 20.6 (20.3-20.8) | 17.5 (17.4-17.7) | 1.00 (reference) |
| Non-Hispanic Asians and Pacific Islanders | 37,051,694 | 4,727 | 12.8 (12.4-13.1) | 12.4 (12.0-12.7) | 0.71* (0.68-0.73) |
| Non-Hispanic black | 2,608,851 | 12,102 | 33.9 (33.3-34.5) | 33.8 (33.2-34.4) | 1.93* (1.88-1.97) |
| American Indians and Alaska Natives | 2,608,851 | 371 | 14.2 (12.8-15.7) | 14.7 (13.2-16.3) | 0.84* (0.75-0.93) |
| Hispanics | 66,191,520 | 8,494 | 12.8 (12.6-13.1) | 14.7 (14.4-15.1) | 0.84* (0.82-0.86) |
| Sub-Total | 320,117,009 | 62,623 | 19.6 (19.4-19.7) | 18.3 (18.1-18.4) | 1.04* (1.03-1.06) |
| Non-Triple-negative breast cancer | |||||
| Non-Hispanic white | 178,531,435 | 349,087 | 195.5 (194.9-196.2) | 159.4 (158.9-160.0) | 1.00 (reference) |
| Non-Hispanic Asians and Pacific Islanders | 37,051,694 | 48,061 | 129.7 (128.6-130.9) | 125.8 (124.7-127.0) | 0.79* (0.78-0.80) |
| Non-Hispanic black | 2,608,851 | 47,156 | 132.0 (130.8-133.2) | 133.0 (131.7-134.2) | 0.83* (0.83-0.84) |
| American Indians and Alaska Natives | 2,608,851 | 3,057 | 117.2 (113.1-121.4) | 116.7 (112.5-121.0) | 0.73* (0.71-0.76) |
| Hispanics | 66,191,520 | 60,528 | 91.4 (90.7-92.2) | 109.4 (108.5-110.3) | 0.69* (0.68-0.69) |
| Sub-Total | 320,117,009 | 510,545 | 159.5 (159-159.9) | 145.8 (145.4-146.2) | 0.91* (0.91-0.92) |
Incidence rates were adjusted to the 2000 US population by age.
Breast cancer cases with unknown or missing information on race/ethnicity were included in the total or sub-total incidence calculation.
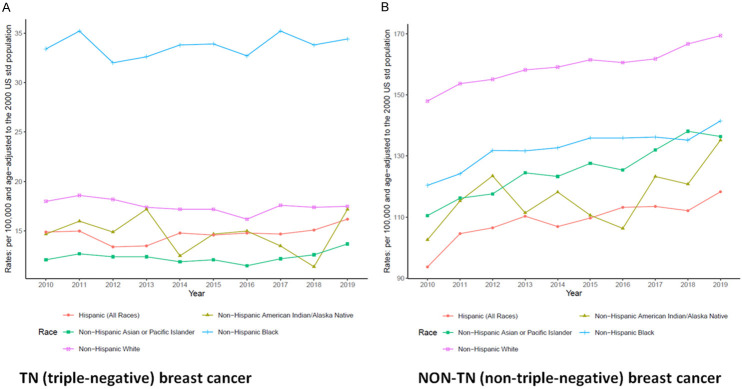
Figure 1 presents the age-adjusted incidence trends over time from 2010 to 2019 for both triple-negative breast cancer (Figure 1A) and non-triple-negative breast cancer cases (Figure 1B) by race/ethnicity. The age-adjusted incidence rate of triple-negative breast cancer was much higher in black women than other ethnic women and increased slightly over time from 2010 to 2019, whereas the age-adjusted incidence rate of non-triple-negative breast cancer was much higher in white women than other ethnic women and increased more sharply over time.
Figure 1.
Trends in age-adjusted incidence rates of triple-negative (TN) breast cancer versus incidence trends in age-adjusted non-triple-negative (Non-TN) breast cancer (number of breast cancer cases per 100,000 population) among women in SEER areas from 2010 to 2019, by race/ethnicity.
Annual percentage change (APC) in age-adjusted incidence of triple-negative breast cancer in the total population aged ≥20 years from 2010 to 2019 slightly increased in Hispanic, black, and Asian women, and slightly decreased in white and AIAN women, but none of these trends was statistically significant (Table 2). In the stratified analyses by the 3 age groups (20-44, 45-54, and ≥55), annual percentage changes in age-adjusted incidence of triple-negative breast cancer slightly decreased but not significantly in white, black and Asian women aged 20-44 and 45-54 years. In AIAN and Hispanic women, there were no significant annual percentage changes in age-adjusted incidence of triple-negative breast cancer except a significant decrease in AIAN women aged 45-54 years. Interestingly, there was a statistically significant annual percentage increase in age-adjusted incidence of triple-negative breast cancer in Asian and black women aged 55 years or older. However, annual percentage change in age-adjusted incidence of non-triple-negative breast cancer from 2010 to 2019 increased significantly in all ethnic women except in AIAN and black women aged 45-54 years.
Table 2.
Annual percentage change (APC) in age-adjusted incidence rates (number of breast cancer cases per 100,000 population) in women in 2010-2019 by triple-negative breast cancer status, race/ethnicity and age groups
| Race/Ethnicity | Triple-negative breast cancer | Non-Triple-negative breast cancer | Total breast cancer (triple-negative and non-triple-negative breast cancer) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2010 to 2019 | P value | N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2010 to 2019 | P value | N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2010 to 2019 | P value | |
| All breast cancer cases aged 20 or older | ||||||||||||
| Non-Hispanic white | 36,695 | 17.5 (17.4-17.7) | -0.7 (-1.5-0.1) | 0.1 | 349,087 | 159.4 (158.9-160.0) | 1.2 (1.0-1.5) | <0.001 | 385,782 | 176.9 (176.4-177.5) | 1.1 (0.8-1.3) | <0.001 |
| Non-Hispanic Asians and Pacific Islanders | 4,727 | 12.4 (12.0-12.7) | 0.6 (-0.6-1.9) | 0.3 | 48,061 | 125.8 (124.7-127.0) | 2.3 (1.8-2.8) | <0.001 | 52,788 | 138.2 (137.0-139.4) | 2.1 (1.6-2.6) | <0.001 |
| Non-Hispanic black | 12,102 | 33.8 (33.2-34.4) | 0.3 (-0.5-1.1) | 0.4 | 47,156 | 133.0 (131.7-134.2) | 1.4 (0.8-1.9) | <0.001 | 59,258 | 166.7 (165.4-168.1) | 1.2 (0.8-1.5) | <0.001 |
| American Indians and Alaska Natives | 371 | 14.7 (13.2-16.3) | -0.7 (-4-2.7) | 0.7 | 3,057 | 116.7 (112.5-121.0) | 1.7 (-0.1-3.5) | 0.1 | 3,428 | 131.4 (126.9-136.0) | 1.4 (-0.3-3.1) | 0.1 |
| Hispanics | 8,494 | 14.7 (14.4-15.1) | 1.0 (-0.2-2.2) | 0.1 | 60,528 | 109.4 (108.5-110.3) | 1.7 (0.9-2.5) | <0.001 | 69,022 | 124.2 (123.2-125.1) | 1.7 (1.0-2.3) | <0.001 |
| Total | 62,623 | 18.3 (18.1-18.4) | -0.2 (-1-0.6) | 0.5 | 510,545 | 145.8 (145.4-146.2) | 1.3 (1.0-1.6) | <0.001 | 573,168 | 164.1 (163.7-164.5) | 1.1 (0.8-1.4) | <0.001 |
| Breast cancer cases aged 20-44 years | ||||||||||||
| Non-Hispanic white | 4,590 | 7.3 (7.1-7.5) | -0.7 (-3.0-1.7) | 0.2 | 26,465 | 42.5 (42.0-43.0) | 1.7 (0.7-2.7) | <0.001 | 31,055 | 49.8 (49.2-50.3) | 1.3 (0.2-2.5) | <0.001 |
| Non-Hispanic Asians and Pacific Islanders | 855 | 4.9 (4.6-5.2) | -1.3 (-7.5-5.3) | 0.3 | 7,214 | 42.1 (41.2-43.1) | 2.4 (0.2-4.7) | <0.001 | 8,069 | 47.0 (46.0-48.1) | 2.0 (-0.2-4.3) | <0.001 |
| Non-Hispanic black | 1,904 | 12.3 (11.8-12.9) | -0.7 (-6.0-4.9) | 0.5 | 6,045 | 39.3 (38.3-40.3) | 1.5 (-0.3-3.4) | <0.001 | 7,949 | 51.7 (50.5-52.8) | 1.0 (-0.6-2.6) | <0.001 |
| American Indians and Alaska Natives | 80 | 7.4 (5.9-9.3) | 1.7 (-14.4-20.8) | 0.6 | 373 | 35.7 (32.1-39.5) | 4.5 (-4.1-13.8) | <0.001 | 453 | 43.1 (39.2-47.3) | 4.1 (-3.5-12.3) | <0.001 |
| Hispanics | 2,239 | 6.6 (6.3-6.9) | 1.1 (-1.9-4.1) | 0.1 | 10,110 | 30.4 (29.8-31.0) | 2.9 (0.1-5.8) | <0.001 | 12,349 | 37.0 (36.3-37.7) | 2.6 (0.3-4.9) | <0.001 |
| Sub-Total | 9,710 | 7.4 (7.3-7.6) | -0.4 (-2.1-1.4) | 0.3 | 50,548 | 39.2 (38.8-39.5) | 2.0 (1.1-2.9) | <0.001 | 60,258 | 46.6 (46.2-47.0) | 1.6 (0.7-2.6) | <0.001 |
| Breast cancer cases aged 45-54 years | ||||||||||||
| Non-Hispanic white | 7,060 | 21.7 (21.2-22.2) | -0.7 (-2.4-1.1) | 0.1 | 61,500 | 189.2 (187.7-190.7) | 1.7 (0.7-2.7) | <0.001 | 68,560 | 210.9 (209.3-212.5) | 1.4 (0.5-2.4) | <0.001 |
| Non-Hispanic Asians and Pacific Islanders | 1,033 | 15.3 (14.4-16.3) | -0.4 (-8.0-7.7) | 0.8 | 12,143 | 180.4 (177.2-183.6) | 2.7 (1.4-4.0) | <0.001 | 13,176 | 195.7 (192.4-199.1) | 2.5 (0.8-4.1) | <0.001 |
| Non-Hispanic black | 3,100 | 45.5 (43.9-47.1) | -0.2 (-4.0-3.8) | 0.8 | 10,175 | 149.8 (146.9-152.8) | 1.2 (-1.6-4.1) | 0.1 | 13,275 | 195.4 (192-198.7) | 0.9 (-1.4-3.2) | 0.1 |
| American Indians and Alaska Natives | 89 | 18.1 (14.5-22.3) | -6.0 (-16.7-6.0) | <0.001 | 642 | 130.6 (120.6-141.2) | 2.7 (-6.8-13.2) | 0.2 | 731 | 148.7 (138-159.9) | 1.5 (-6.4-10.1) | 0.4 |
| Hispanics | 2,338 | 19.8 (19.0-20.6) | -0.5 (-5.7-5.0) | 0.7 | 15,762 | 133.5 (131.4-135.6) | 1.8 (-0.6-4.2) | <0.001 | 18,100 | 153.3 (151.1-155.6) | 1.5 (-0.6-3.6) | <0.001 |
| Sub-Total | 13,688 | 23.4 (23.0-23.8) | -0.6 (-3.1-2.0) | 0.3 | 100,804 | 172.7 (171.7-173.8) | 1.6 (0.6-2.6) | <0.001 | 114,492 | 196.2 (195-197.3) | 1.3 (0.4-2.3) | <0.001 |
| Breast cancer cases aged 55 years or older | ||||||||||||
| Non-Hispanic white | 25,045 | 32.4 (32.0-32.9) | -0.7 (-2.8-1.6) | 0.2 | 261,122 | 340.2 (338.9-341.5) | 1.0 (0.4-1.6) | <0.001 | 286,167 | 372.6 (371.3-374) | 0.9 (0.3-1.4) | <0.001 |
| Non-Hispanic Asians and Pacific Islanders | 2,839 | 23.3 (22.4-24.1) | 1.7 (-1.7-5.2) | <0.001 | 28,704 | 234.3 (231.6-237.1) | 2.0 (0.5-3.5) | <0.001 | 31,543 | 257.6 (254.7-260.5) | 2.0 (0.7-3.3) | <0.001 |
| Non-Hispanic black | 7,098 | 62.9 (61.4-64.5) | 0.8 (-0.1-1.8) | <0.001 | 30,936 | 282.1 (278.9-285.4) | 1.4 (0.1-2.7) | <0.001 | 38,034 | 345.1 (341.5-348.7) | 1.3 (0.3-2.3) | <0.001 |
| American Indians and Alaska Natives | 202 | 25.0 (21.6-28.9) | 0.6 (-8.8-10.9) | 0.8 | 2,042 | 246.2 (235.2-257.5) | 0.6 (-5.3-6.7) | 0.7 | 2,244 | 271.2 (259.7-283.1) | 0.6 (-5.2-6.7) | 0.6 |
| Hispanics | 3,917 | 25.5 (24.7-26.3) | 1.7 (-2.2-5.8) | 0.1 | 34,656 | 229.1 (226.6-231.6) | 1.5 (-0.1-3.1) | <0.001 | 38,573 | 254.6 (252-257.2) | 1.5 (0.2-2.8) | <0.001 |
| Sub-Total | 39,225 | 33.6 (33.3-34.0) | 0.0 (-1.7-1.8) | 0.9 | 359,193 | 310.8 (309.8-311.9) | 1.0 (0.4-1.6) | <0.001 | 398,418 | 344.5 (343.4-345.5) | 0.9 (0.4-1.5) | <0.001 |
Table 3 presents the age-adjusted incidence of triple-negative breast cancer and non-triple-negative breast cancer by 3 time periods (2010-2013, 2014-2016, and 2017-2019) and race/ethnicity. The age-adjusted incidence of triple-negative breast cancer marginally increased during these time periods among Hispanic, black and Asian women. For example, the age-adjusted incidence of triple-negative breast cancer in black women was 33.3 cases per 100,000 women for 2010-2013, 33.5 cases for 2014-2016, and 34.5 cases for 2017-2019. The age-adjusted incidence of non-triple-negative breast cancer increased in white, black, Asian and Hispanic women by these 3 time periods, while the age-adjusted incidence of non-triple-negative breast cancer among AIAN women was lower in 2014-2016 than in 2010-2013 but was higher in 2017-2019.
Table 3.
Annual percentage change (APC) in age-adjusted incidence rates* of triple-negative breast cancer (number of breast cancer cases per 100,000 population) in women by time period and race/ethnicity
| Race/Ethnicity | 2010-2013 | 2014-2016 | 2017-2019 | APC (95% CI) | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| N. Population | N. Cases | Incidence rate (95% CI) | N. Population | N. Cases | Incidence rate (95% CI) | N. Population | N. Cases | Incidence rate (95% CI) | |||
| Triple-negative breast cancer | |||||||||||
| NH-white | 71,255,586 | 14,871 | 18.1 (17.8-18.4) | 53,725,401 | 10,615 | 16.9 (16.5-17.2) | 53,550,448 | 11,209 | 17.5 (17.2-17.9) | -0.7 (-1.5-0.1) | 0.1 |
| NH-Asians and P. Islanders | 13,667,498 | 1,696 | 12.4 (11.8-13.0) | 11,287,880 | 1,387 | 11.8 (11.2-12.4) | 12,096,316 | 1,644 | 12.8 (12.2-13.5) | 0.6 (-0.6-1.9) | 0.3 |
| NH-black | 13,649,493 | 4,502 | 33.3 (32.3-34.3) | 10,818,753 | 3,637 | 33.5 (32.4-34.6) | 11,265,263 | 3,963 | 34.5 (33.4-35.6) | 0.3 (-0.5-1.1) | 0.4 |
| American Indians and AN | 1,008,653 | 149 | 15.7 (13.2-18.5) | 789,737 | 108 | 14.1 (11.5-17.1) | 810,461 | 114 | 14.0 (11.5-17.0) | -0.7 (-4-2.7) | 0.7 |
| Hispanics | 24,791,947 | 2,997 | 14.2 (13.7-14.7) | 20,108,413 | 2,574 | 14.7 (14.1-15.3) | 21,291,160 | 2,923 | 15.3 (14.8-15.9) | 1.0 (-0.2-2.2) | 0.1 |
| Total | 124,373,177 | 24,283 | 18.5 (18.3-18.8) | 96,730,184 | 18,387 | 17.7 (17.5-18.0) | 99,013,648 | 19,953 | 18.5 (18.2-18.8) | -0.2 (-1-0.6) | 0.5 |
| Non-Triple-negative breast cancer | |||||||||||
| NH-white | 71,255,586 | 131,546 | 153.8 (152.9-154.6) | 53,725,401 | 106,100 | 160.4 (159.4-161.4) | 53,550,448 | 111,441 | 165.9 (164.9-167.0) | 1.2 (1-1.5) | <0.001 |
| NH-Asians and P. Islanders | 13,667,498 | 16,194 | 117.4 (115.6-119.2) | 11,287,880 | 14,640 | 125.5 (123.4-127.5) | 12,096,316 | 17,227 | 135.5 (133.4-137.5) | 2.3 (1.8-2.8) | <0.001 |
| NH-black | 13,649,493 | 16,773 | 127.2 (125.2-129.1) | 10,818,753 | 14,531 | 134.9 (132.6-137.1) | 11,265,263 | 15,852 | 137.7 (135.5-139.9) | 1.4 (0.8-1.9) | <0.001 |
| American Indians and AN | 1,008,653 | 1,108 | 113.5 (106.7-120.6) | 789,737 | 892 | 111.6 (104.2-119.4) | 810,461 | 1,057 | 126.6 (118.8-134.8) | 1.7 (-0.1-3.5) | 0.1 |
| Hispanics | 24,791,947 | 20,567 | 104.0 (102.6-105.5) | 20,108,413 | 18,607 | 110.0 (108.4-111.7) | 21,291,160 | 21,354 | 114.7 (113.1-116.3) | 1.7 (0.9-2.5) | <0.001 |
| Total | 124,373,177 | 186,874 | 140.4 (139.8-141.1) | 96,730,184 | 155,540 | 146.6 (145.8-147.3) | 99,013,648 | 168,131 | 151.7 (151.0-152.5) | 1.3 (1.0-1.6) | <0.001 |
Incidence rates were age adjusted to the 2000 US population.
Table 4 presents the age-adjusted incidence of triple-negative breast cancer and incidence rate ratio by age groups (20-44, 45-54, and ≥55), 3 time periods (2010-2013, 2014-2016, and 2017-2019) and race/ethnicity. The significantly higher age-adjusted incidence of triple-negative breast cancer in black women as compared to white women appeared to be limited in younger women aged 20-44 only (incidence rate ratio: 1.04, 95% CI: 1.00-1.08 for 2010-2013; 1.03, 1.00-1.09 for 2014-2016, and 1.03, 0.98-1.07 for 2017-2019). There were significantly lower age-adjusted incidence rates of triple-negative breast cancer in black women than in white women in other 2 age groups (44-54 and 55 or older). The age-adjusted incidence rates of triple-negative breast cancer were generally lower in the 3 age groups among Asian, AIAN and Hispanic women than white women.
Table 4.
Age-adjusted incidence rates of triple-negative breast cancer (number of breast cancer cases per 100,000 women) by age groups, race/ethnicity, and time period
| Race/Ethnicity | Age 20-44 yrs | Age 45-54 yrs | Age ≥55 yrs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| N. Population | N. Cases | Incidence rate* (95% CI) | Rate ratio (95% CI) | N. Population | N. Cases | Incidence rate* (95% CI) | Rate ratio (95% CI) | N. Population | N. Cases | Incidence rate* (95% CI) | Rate ratio (95% CI) | |
| 2010-2013 | ||||||||||||
| NH-white | 27,673,809 | 12,411 | 47.9 (47.1-48.8) | 1.00 (ref) | 13,849,991 | 28,442 | 203.6 (201.2-205.9) | 1.00 (ref) | 29,731,786 | 105,564 | 363.3 (361.1-365.6) | 1.00 (ref) |
| NH-Asians and P. Islanders | 6,822,173 | 2,875 | 44.3 (42.7-46.0) | 0.92 (0.89-0.96) | 2,550,269 | 4,667 | 182.4 (177.2-187.7) | 0.90 (0.87-0.92) | 4,295,056 | 10,348 | 242.4 (237.7-247.2) | 0.67 (0.65-0.68) |
| NH-black | 6,865,584 | 3,040 | 49.9 (48.2-51.7) | 1.04 (1.00-1.08) | 2,736,798 | 5,212 | 189.5 (184.3-194.7) | 0.93 (0.90-0.96) | 4,047,111 | 13,023 | 330.9 (325.1-336.8) | 0.91 (0.89-0.93) |
| American Indians and AN | 501,604 | 163 | 38.6 (32.9-45.0) | 0.81 (0.69-0.94) | 206,716 | 290 | 139.1 (123.5-156.1) | 0.68 (0.61-0.77) | 300,333 | 804 | 277.6 (257.9-298.4) | 0.76 (0.71-0.82) |
| Hispanics | 15,051,841 | 4,442 | 34.3 (33.3-35.3) | 0.72 (0.69-0.74) | 4,408,238 | 6,460 | 146.7 (143.1-150.3) | 0.72 (0.70-0.74) | 5,331,868 | 12,662 | 243.5 (239.1-247.9) | 0.67 (0.66-0.68) |
| Sub-Total (2010-2013) | 56,915,011 | 23,044 | 44.5 (43.9-45.1) | 23,752,012 | 45,266 | 189.3 (187.6-191.1) | 43,706,154 | 142,847 | 335.2 (333.4-336.9) | |||
| 2014-2016 | ||||||||||||
| NH-white | 20,443,406 | 9,217 | 50.1 (49.0-51.1) | 1.00 (ref) | 9,587,313 | 20,423 | 210.5 (207.6-213.4) | 1.00 (ref) | 23,694,682 | 87,075 | 373.4 (370.9-376) | 1.00 (ref) |
| NH-Asians and P. Islanders | 5,491,452 | 2,452 | 46.9 (45.0-48.8) | 0.94 (0.9-0.98) | 2,027,709 | 3,953 | 194.5 (188.5-200.7) | 0.92 (0.89-0.96) | 3,768,719 | 9,622 | 255.4 (250.3-260.7) | 0.68 (0.67-0.70) |
| NH-black | 5,333,868 | 2,387 | 52.2 (50.1-54.3) | 1.04 (1.00-1.09) | 2,025,818 | 4,084 | 199.3 (193.2-205.5) | 0.95 (0.92-0.98) | 3,459,067 | 11,697 | 347.1 (340.6-353.6) | 0.93 (0.91-0.95) |
| American Indians and AN | 384,892 | 130 | 41.3 (34.4-49.0) | 0.83 (0.69-0.98) | 145,382 | 218 | 149.1 (129.8-170.5) | 0.71 (0.62-0.81) | 259,463 | 652 | 254.9 (235-276.1) | 0.68 (0.63-0.74) |
| Hispanics | 11,764,741 | 3,811 | 37.7 (36.5-38.9) | 0.75 (0.73-0.78) | 3,596,453 | 5,541 | 154.0 (149.9-158.1) | 0.73 (0.71-0.75) | 4,747,219 | 11,829 | 254.9 (250.2-259.7) | 0.68 (0.67-0.70) |
| Sub-Total (2014-2016) | 43,418,359 | 18,108 | 46.9 (46.2-47.6) | 17,382,675 | 34,411 | 196.2 (194.1-198.3) | 35,929,150 | 121,408 | 344.6 (342.7-346.6) | |||
| 2017-2019 | ||||||||||||
| NH-white | 20,200,529 | 9,427 | 52.1 (51.0-53.2) | 1.00 (ref) | 8,766,150 | 19,695 | 222.9 (219.7-226) | 1.00 (ref) | 24,583,769 | 93,528 | 382.7 (380.3-385.2) | 1.00 (ref) |
| NH-Asians and P. Islanders | 5,732,601 | 2,742 | 50.5 (48.6-52.4) | 0.97 (0.93-1.01) | 2,144,483 | 4,556 | 212.4 (206.3-218.7) | 0.95 (0.92-0.98) | 4,219,232 | 11,573 | 274.9 (269.9-280.1) | 0.72 (0.70-0.73) |
| NH-black | 5,470,780 | 2,522 | 53.5 (51.4-55.6) | 1.03 (0.98-1.07) | 1,980,094 | 3,979 | 199.4 (193.2-205.7) | 0.89 (0.86-0.93) | 3,814,389 | 13,314 | 357.7 (351.5-364) | 0.93 (0.92-0.95) |
| American Indians and AN | 389,128 | 160 | 51.2 (43.5-59.8) | 0.98 (0.83-1.15) | 134,852 | 223 | 163.1 (142.3-186.1) | 0.73 (0.64-0.84) | 286,481 | 788 | 279.1 (259.4-299.9) | 0.73 (0.68-0.78) |
| Hispanics | 12,067,250 | 4,096 | 39.7 (38.5-40.9) | 0.76 (0.73-0.79) | 3,801,546 | 6,099 | 160.4 (156.4-164.4) | 0.72 (0.70-0.74) | 5,422,364 | 14,082 | 265.1 (260.6-269.6) | 0.69 (0.68-0.71) |
| Sub-Total (2017-2019) | 43,860,288 | 19,106 | 49.2 (48.5-49.9) | 16,827,125 | 34,815 | 205.7 (203.6-207.9) | 38,326,235 | 134,163 | 354.5 (352.6-356.4) | |||
| Total (2010-2019) | 144,193,65 | 60,258 | 46.6 (46.2-47.0) | 57,961,812 | 114,492 | 196.2 (195.0-197.3) | 117,961,539 | 398,418 | 344.5 (343.4-345.5) | |||
Incidence rates were age adjusted to the 2000 US population in each of the 3 age groups.
Table 5 presents the annual percentage change in age-adjusted incidence of triple-negative breast cancer and non-triple-negative breast cancer by tumor stage (in-situ/local, regional, distant stage, or unknown stage) and race/ethnicity. Among patients with local stage breast cancer, annual percentage change in age-adjusted incidence of triple-negative breast cancer from 2010 to 2019 slightly decreased in white women but increased in Hispanic, black, Asian, and AIAN women (P>0.05). Among patients with regional stage breast cancer, annual percentage change in age-adjusted incidence of triple-negative breast cancer from 2010 to 2019 decreased in all ethnic women but only statistically significantly decreased in white women. In contrast, annual percentage change in age-adjusted incidence of triple-negative breast cancer from 2010 to 2019 increased significantly in white and Hispanic women with distant stage and in white women with unknown stage breast cancer, but not significantly increased in black and Asian women. Annual percentage change in age-adjusted incidence of non-triple-negative breast cancer from 2010 to 2019 increased significantly in almost all ethnic women with local or distant stage breast cancer and slightly increased in those with regional stage breast cancer. In those with unknown stage breast cancer, annual percentage change in age-adjusted incidence of non-triple-negative breast cancer from 2010 to 2019 increased for white, Asian and Hispanic women, but decreased for black and AIAN women.
Table 5.
Annual percentage change (APC) in age-adjusted incidence rates (number of breast cancer cases per 100,000 population) in women in 2010-2019 by tumor stage, triple-negative breast cancer status and race/ethnicity
| Race/Ethnicity | Triple-negative breast cancer | Non-Triple-negative breast cancer | Total breast cancer (triple-negative and non-triple-negative breast cancer) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2010 to 2019 | N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2010 to 2019 | N. Cases | Incidence rate (95% CI) | APC (95% CI) from 2010 to 2019 | |
| Local stage Breast Cancer | |||||||||
| Non-Hispanic white | 11.0 (10.9-11.2) | -0.5 (-2.5-1.5) | 238,689 | 107 (106.6-107.4) | 1.8*** (1.0-2.5) | 262,038 | 118.0 (117.6-118.5) | 1.5*** (0.8-2.3) | |
| Non-Hispanic Asians and Pacific Islanders | 2,893 | 7.5 (7.3-7.8) | 1.1 (-2.4-4.7) | 31,778 | 83.0 (82-83.9) | 2.4*** (1.3-3.5) | 34,671 | 90.5 (89.5-91.5) | 2.3*** (1.2-3.3) |
| Non-Hispanic black | 6,689 | 18.6 (18.1-19.1) | 0.4 (-1.7-2.6) | 27,340 | 77.2 (76.3-78.2) | 2.1*** (0.4-3.8) | 34,029 | 95.8 (94.8-96.9) | 1.7*** (0.3-3.2) |
| American Indians and Alaska Natives | 215 | 8.4 (7.3-9.6) | 0.5 (-10.8-13.3) | 1,909 | 72.4 (69.1-75.8) | 1.9 (-3.4-7.4) | 2,124 | 80.8 (77.3-84.4) | 1.7 (-3.7-7.5) |
| Hispanics | 4,739 | 8.3 (8.1-8.5) | 1 (-3-5.1) | 36,253 | 66.8 (66.1-67.5) | 2.4*** (0.6-4.3) | 40,992 | 75.1 (74.4-75.9) | 2.3*** (0.8-3.8) |
| Sub-Total | 38,016 | 11.0 (10.9-11.1) | -0.2 (-2.1-1.8) | 337,626 | 95.4 (95.1-95.8) | 1.7*** (1.0-2.5) | 375,642 | 106.5 (106.1-106.8) | 1.5*** (0.8-2.3) |
| Regional Stage Breast Cancer | |||||||||
| Non-Hispanic white | 10,616 | 5.2 (5.1-5.4) | -1.8** (-4.3-0.7) | 91,171 | 43.7 (43.4-44.0) | -0.2 (-0.9-0.6) | 101,787 | 48.9 (48.6-49.3) | -0.4 (-1.0-0.2) |
| Non-Hispanic Asians and Pacific Islanders | 1,504 | 4.0 (3.8-4.2) | -0.7 (-6.0-5.0) | 13,706 | 36.2 (35.6-36.8) | 1.7* (-0.5-3.9) | 15,210 | 40.1 (39.5-40.8) | 1.5* (-0.8-3.8) |
| Non-Hispanic black | 4,310 | 12.1 (11.7-12.5) | -0.1 (-3.1-3.0) | 15,763 | 44.4 (43.7-45.1) | 0.4 (-1.2-2.1) | 20,073 | 56.5 (55.7-57.3) | 0.3 (-1.2-1.8) |
| American Indians and Alaska Natives | 119 | 4.9 (4.1-5.9) | -2.1 (-18.9-18) | 944 | 36.2 (33.9-38.7) | 0.0 (-5.9-6.2) | 1,063 | 41.1 (38.6-43.8) | -0.3 (-5.5-5.1) |
| Hispanics | 3,058 | 5.2 (5-5.4) | 0.0 (-2.8-3.0) | 20,575 | 35.9 (35.4-36.4) | 0.3 (-1.6-2.3) | 23,633 | 41.1 (40.6-41.7) | 0.3 (-1.2-1.8) |
| Sub-Total | 19,678 | 5.9 (5.8-5.9) | -1.0* (-2.8-0.8) | 142,801 | 41.8 (41.6-42) | 0.1 (-0.7-1.0) | 162,479 | 47.6 (47.4-47.9) | 0.0 (-0.8-0.8) |
| Distant Stage Breast Cancer | |||||||||
| Non-Hispanic white | 2,458 | 1.1 (1.1-1.2) | 2.0** (-0.8-5) | 17,047 | 7.8 (7.7-7.9) | 1.9** (0.0-3.8) | 19,505 | 8.9 (8.8-9.0) | 1.9*** (0.3-3.5) |
| Non-Hispanic Asians and Pacific Islanders | 277 | 0.7 (0.6-0.8) | 1.7 (-10.7-15.8) | 2,224 | 5.8 (5.6-6.0) | 3.6** (-0.4-7.8) | 2,501 | 6.5 (6.3-6.8) | 3.4*** (0.3-6.7) |
| Non-Hispanic black | 1,004 | 2.8 (2.6-3.0) | 0.8 (-3.2-4.9) | 3,677 | 10.3 (10.0-10.6) | 0.7 (-1.9-3.4) | 4,681 | 13.1 (12.7-13.5) | 0.7 (-1.5-3.1) |
| American Indians and Alaska Natives | 32 | 1.2 (0.8-1.7) | -8.5 (-29.9-19.4) | 179 | 7.0 (5.9-8.1) | 8.1*** (1.5-15.2) | 211 | 8.2 (7.1-9.4) | 5.4 (-3.8-15.4) |
| Hispanics | 593 | 1.1 (1.0-1.2) | 5.4** (0.1-11.0) | 3,205 | 5.7 (5.5-5.9) | 2.1* (-1.1-5.3) | 3,798 | 6.8 (6.0.6-7) | 2.6** (-0.1-5.3) |
| Sub-Total | 4,371 | 1.3 (1.2-1.3) | 2.1 (-1.4-5.7) | 26,421 | 7.6 (7.5-7.6) | 1.8*** (0.4-3.1) | 30,792 | 8.8 (8.7-8.9) | 1.8*** (0.7-2.9) |
| Unknown stage or missing/not coded | |||||||||
| Non-Hispanic white | 272 | 0.1 (0.1-0.1) | 10.0* (-5.3-27.7) | 2,180 | 0.9 (0.9-1.0) | 4.9* (-5.0-15.9) | 2,452 | 1.1 (1.0-1.1) | 5.5* (-4.7-16.8) |
| Non-Hispanic Asians and Pacific Islanders | 53 | 0.1 (0.1-0.2) | 3.3 (-19.2-32.1) | 353 | 0.9 (0.0.8-1.0) | 3.8 (-11.1-21.3) | 406 | 1.1 (1-1.2) | 4.1 (-10.6-21.2) |
| Non-Hispanic black | 99 | 0.3 (0.2-0.3) | 1.9 (-16.6-24.6) | 376 | 1.1 (1.0-1.2) | -0.4 (-8.0-7.8) | 475 | 1.4 (1.2-1.5) | 0.2 (-8.0-9.0) |
| American Indians and Alaska Natives | 104 | 0.2 (0.1-0.5) | ~ (~-~)$ | 25 | 1.1 (0.7-1.7) | -0.1 (-25.4-33.9) | 30 | 1.3 (0.9-1.9) | 1.9 (-19.3-28.6) |
| Hispanics | 5 | 0.2 (0.1-0.2) | 7.7 (-22.2-48.9) | 495 | 0.9 (0.8-1.0) | 6.1 (-16.0-34.1) | 599 | 1.1 (1.0-1.2) | 6.2 (-16.5-35.1) |
| Sub-Total | 558 | 0.2 (0.1-0.2) | 7.7* (-7.2-25.1) | 3,697 | 1.0 (1.0-1.1) | 4.9 (-6.5-17.7) | 4,255 | 1.2 (1.2-1.2) | 5.3 (-6.4-18.5) |
P<0.05, indicating the incidence rate other ethnic groups is significantly different than the rate for Non-Hispanic White;
P<0.01, indicating the incidence rate other ethnic groups is significantly different than the rate for Non-Hispanic White;
P<0.001, indicating the incidence rate other ethnic groups is significantly different than the rate for Non-Hispanic White.
APC was not obtainable from the SEER*Stat.
Table 6 presents the changes in the proportion of estrogen receptor, progesterone receptor and HER2 receptor status from 2010 to 2019 to determine if the changing trends in the incidence of triple-negative breast cancer was affected more or less by the changing proportions of the 3 individual receptors over time. Of all incident (triple-negative and non-triple-negative) breast cancer cases in 2010-2019, the proportion of patients with estrogen receptor negative slightly decreased from 17.7% in 2010 to 15.3% in 2019; the proportion of patients with progesterone receptor negative also slightly decreased from 29.2% in 2010 to 26.0% in 2019; and the proportion of patients with HER2 receptor negative slightly increased from 85.1% to 86.7%.
Table 6.
Proportion of breast cancer cases having hormone-receptor negative and HER2-negative tumors by year
| Year | Total N | Number by estrogen receptor status negative | Row % by estrogen receptor status negative | Number by progesterone receptor status negative | Row % by progesterone receptor negative | Number by HER2-receptor status negative | Row % by HER2-receptor negative |
|---|---|---|---|---|---|---|---|
| 2010 | 49,404 | 8,740 | 17.70% | 14,410 | 29.20% | 42,036 | 85.10% |
| 2011 | 52,452 | 9,131 | 17.40% | 14,845 | 28.30% | 44,894 | 85.60% |
| 2012 | 53,808 | 9,099 | 16.90% | 14,919 | 27.70% | 45,877 | 85.30% |
| 2013 | 55,493 | 9,001 | 16.20% | 14,785 | 26.60% | 47,335 | 85.30% |
| 2014 | 56,482 | 9,342 | 16.50% | 15,084 | 26.70% | 47,538 | 84.20% |
| 2015 | 58,491 | 9,583 | 16.40% | 15,714 | 26.90% | 49,071 | 83.90% |
| 2016 | 58,954 | 9,241 | 15.70% | 15,704 | 26.60% | 49,594 | 84.10% |
| 2017 | 60,770 | 9,810 | 16.10% | 16,077 | 26.50% | 51,379 | 84.50% |
| 2018 | 62,709 | 9,731 | 15.50% | 16,517 | 26.30% | 53,865 | 85.90% |
| 2019 | 64,605 | 9,870 | 15.30% | 16,769 | 26.00% | 55,999 | 86.70% |
| Total | 573,168 | 93,548 | 16.30% | 154,824 | 27.00% | 487,588 | 85.10% |
Discussion
This study examined the age-adjusted incidence rates and trends by race/ethnicity for both triple-negative breast cancer and non-triple-negative breast cancer. The age-adjusted incidence rate of triple-negative breast cancer was the highest in black women, followed by white, AIAN, Hispanic, and Asian women. The incidence rate ratio was statistically significantly higher in black women and significantly lower in AIAN, Hispanic, and Asian women as compared to white women. The significantly higher age-adjusted incidence of triple-negative breast cancer in black women as compared to white women appeared to be limited in younger women aged 20-44 only. There was no significant difference in age-adjusted incidence of triple-negative breast cancer among women aged 44-54 and ≥55 years. The study found that there were no significant annual percentage changes in age-adjusted incidence of triple-negative breast cancer from 2010 to 2019 in all ethnic groups of women aged 20-44 and 45-54 years, with the exception of a significant decrease in AIAN women aged 45-54 years. However, there was a statistically significant annual percentage increase in age-adjusted incidence of triple-negative breast cancer in Asian and black women aged ≥55 years. All ethnic women, with the exception of AIAN women, experienced a significant annual percentage increase in age-adjusted incidence of non-triple-negative breast cancer from 2010 to 2019. The trends in age-adjusted incidences of triple-negative breast cancer were not affected by dramatical changes in proportions in any of the 3 receptors.
Several previous studies examined the incidence rates of triple-negative breast cancer by race/ethnicity [21-25], of which only one study examined the incidence trends of triple-negative breast cancer among various racial and ethnic women [25]. Clarke and colleagues examined a large cohort of women with invasive breast cancer in California in 2006-2009 and found that black women had statistically significantly higher incidence rates of triple-negative breast cancer than white women at all ages [21]. Howlader and colleagues examined the incidence of triple-negative breast cancer in 2010, which was the first year for HER2-receptor status to be available in the complete SEER data [22]. They found that non-Hispanic black women had the highest incidence rates of triple-negative breast cancer across all age groups and non-Hispanic black women were much more likely to be diagnosed with this subtype of breast cancer than were the three other racial/ethnic groups [22]. Kohler and colleagues specifically examined the incidence of triple-negative breast cancer in 2011 by race/ethnicity in SEER areas and found that the incidence rate of triple-negative breast cancer was highest among non-Hispanic black women with an aged-adjusted rate of 27.2 cases per 100,000 women, as compared with all other racial/ethnic women [23]. Acheampong and colleagues reported the trends in triple-negative breast cancer incidence rates from 2010 to 2016 in SEER areas and found that triple-negative breast cancer incidence decreased in non-Hispanic white women aged 40-54 and 55-69 years as well as in non-Hispanic Black women aged 55-69 years [25]. Our study examined the incidence trends in more recent years from 2010 to 2019 and also addressed the incidence rates and trends among various racial/ethnic women, stratified by age groups and tumor stage. Our study found that there were no significant annual percentage changes in age-adjusted incidence of triple-negative breast cancer in all ethnic women aged 20-44 and 45-54 years except a significant decrease in AIAN women aged 45-54 years. However, there was a statistically significant annual percentage increase in age-adjusted incidence of triple-negative breast cancer from 2010 to 2019 in Asian and black women aged ≥55 years. Some of these findings appeared to differ from a previous study reporting breast cancer cases in 2010-2016 [25]. These differences in age-adjusted incidence rates of triple-negative breast cancer for some older ethnic women may have been resulted from more breast cancer cases in recent years (2017-2019).
Because triple-negative breast cancer is a more aggressive subtype of cancer, spreads much faster than other subtypes of cancer, and has limited effective treatment options, patients with triple-negative breast cancer often have much poorer clinical outcomes and lower survival [10-20]. A higher risk of developing triple-negative breast cancer in black women with limited treatment choices may be one of the reasons why black women with breast cancer were reported to have a significantly higher risk of mortality [10-20]. Apparent racial and ethnic disparities in triple-negative breast cancer incidence and outcomes could be explained by a number of factors according to previous studies [10-20]. These include both biologic factors (such as genetic factors, early menarche, high parity, lack of breastfeeding, and obesity in promoting this subtype of disease biology) and non-biologic factors (such as unsafe neighborhoods, poverty, unmarried household, social stress, and toxic-waste dumping) [12-17,27-34]. Once triple-negative breast cancer can be detectable clinically, it would be critical to have access to medical care in order to improve outcomes. Health insurance, transportation, timely treatment, compliance, and regular follow-up care are some of the factors that have been shown to have an impact on racial/ethnic disparities in breast cancer outcomes [35-40].
There are several limitations in this study. First, because triple-negative breast cancer was based on the coding of estrogen receptor, progesterone receptor, and HER2 receptor status, there were some concerns about completeness and accuracy of information on these receptors and about the number of breast cancer cases with missing or unknown status on these receptors, which could significantly affect the estimates of incidence of triple-negative breast cancer. Second, women aged ≥20 years in SEER areas as dynamic populations and denominators for the incidence rates may change over time due to migration, hence affecting the incidence rates. Third, women were grouped into broader categories of non-Hispanic whites, blacks, Asians, and Hispanics. Variations by sub-Saharan African women, subgroups of Hispanic population (Cuban or Mexico), and subgroups of Asian and Pacific Islanders were not considered in the analyses. Therefore, it should require a caution at interpreting and generalizing the study findings to sub-groups of various racial/ethnic populations.
In conclusion, age-adjusted incidence rates of triple-negative breast cancer was statistically significantly higher in black women and significantly lower in AIAN, Hispanic, and Asian women as compared to white women. The significantly higher age-adjusted incidence of triple-negative breast cancer in black women than white women were observed only in younger women aged 20-44. There were no significant annual percentage changes in age-adjusted incidence of triple-negative breast cancer from 2010 to 2019 in all ethnic women age 20-44 and 45-54 years except a significant decrease in AIAN aged 45-54 years. However, there was a statistically significant annual percentage increase in age-adjusted incidence of triple-negative breast cancer in Asian and black women aged ≥55 years. More research may be needed to explore why there is a significantly higher incidence of triple-negative breast cancer only in younger women aged 20-44 years and why there is significant annual percentage increase in age-adjusted incidence of triple-negative breast cancer in Asian and black women aged ≥55 years.
Acknowledgements
Research reported in this publication was supported in part by the National Institute on Aging of the National Institutes of Health under Award Number R01AG058971 and R01AG067498. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure of conflict of interest
None.
References
- 1.Bray F, McCarron P, Parkin DM. The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res. 2004;6:229–239. doi: 10.1186/bcr932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ravdin PM, Cronin KA, Howlader N, Berg CD, Chlebowski RT, Feuer EJ, Edwards BK, Berry DA. The decrease in breast cancer incidence in 2003 in the United States. N Engl J Med. 2007;356:1670–1674. doi: 10.1056/NEJMsr070105. [DOI] [PubMed] [Google Scholar]
- 3.Porter P. “Westernizing” women’s risks? Breast cancer in lower-income countries. N Engl J Med. 2008;358:213–216. doi: 10.1056/NEJMp0708307. [DOI] [PubMed] [Google Scholar]
- 4.Shin HR, Joubert C, Boniol M, Hery C, Ahn SH, Won YJ, Nishino Y, Sobue T, Chen CJ, You SL, Mirasol-Lumague MR, Law SC, Mang O, Xiang YB, Chia KS, Rattanamongkolgul S, Chen JG, Curado MP, Autier P. Recent trends and patterns in breast cancer incidence among Eastern and Southeastern Asian women. Cancer Causes Control. 2010;21:1777–1785. doi: 10.1007/s10552-010-9604-8. [DOI] [PubMed] [Google Scholar]
- 5.Zbuk K, Anand SS. Declining incidence of breast cancer after decreased use of hormone-replacement therapy: magnitude and time lags in different countries. J Epidemiol Community Health. 2012;66:1–7. doi: 10.1136/jech.2008.083774. [DOI] [PubMed] [Google Scholar]
- 6.DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A. International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2015;24:1495–1506. doi: 10.1158/1055-9965.EPI-15-0535. [DOI] [PubMed] [Google Scholar]
- 7.DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin. 2016;66:31–42. doi: 10.3322/caac.21320. [DOI] [PubMed] [Google Scholar]
- 8.DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 9.Du XL, Song L. Breast cancer incidence trends in Asian women aged 20 or older as compared to other ethnic women in the United States from 2000 to 2018 by time period, age and tumor stage. Cancer Epidemiol. 2022;76:102076. doi: 10.1016/j.canep.2021.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010;363:1938–1948. doi: 10.1056/NEJMra1001389. [DOI] [PubMed] [Google Scholar]
- 11.Kurian AW, Fish K, Shema SJ, Clarke CA. Lifetime risks of specific breast cancer subtypes among women in four racial/ethnic groups. Breast Cancer Res. 2010;12:R99. doi: 10.1186/bcr2780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newman LA, Kaljee LM. Health disparities and triple-negative breast cancer in African American women: a review. JAMA Surg. 2017;152:485–493. doi: 10.1001/jamasurg.2017.0005. [DOI] [PubMed] [Google Scholar]
- 13.Siddharth S, Sharma D. Racial disparity and triple-negative breast cancer in African-American women: a multifaceted affair between obesity, biology, and socioeconomic determinants. Cancers (Basel) 2018;10:514. doi: 10.3390/cancers10120514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garlapati C, Joshi S, Sahoo B, Kapoor S, Aneja R. The persisting puzzle of racial disparity in triple-negative breast cancer: looking through a new lens. Front Biosci (Schol Ed) 2019;11:75–88. doi: 10.2741/S527. [DOI] [PubMed] [Google Scholar]
- 15.Tao L, Gomez SL, Keegan TH, Kurian AW, Clarke CA. Breast cancer mortality in African-American and non-Hispanic white women by molecular subtype and stage at diagnosis: a population-based study. Cancer Epidemiol Biomarkers Prev. 2015;24:1039–1045. doi: 10.1158/1055-9965.EPI-15-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brinton LA, Figueroa JD, Awuah B, Yarney J, Wiafe S, Wood SN, Ansong D, Nyarko K, Wiafe-Addai B, Clegg-Lamptey JN. Breast cancer in Sub-Saharan Africa: opportunities for prevention. Breast Cancer Res Treat. 2014;144:467–478. doi: 10.1007/s10549-014-2868-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dietze EC, Sistrunk C, Miranda-Carboni G, O’Regan R, Seewaldt VL. Triple-negative breast cancer in African-American women: disparities versus biology. Nat Rev Cancer. 2015;15:248–254. doi: 10.1038/nrc3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zahnd WE, Sherman RL, Klonoff-Cohen H, McLafferty SL, Farner S, Rosenblatt KA. Disparities in breast cancer subtypes among women in the lower Mississippi Delta Region states. Cancer Causes Control. 2019;30:591–601. doi: 10.1007/s10552-019-01168-0. [DOI] [PubMed] [Google Scholar]
- 19.Scott LC, Mobley LR, Kuo TM, Il’yasova D. Update on triple-negative breast cancer disparities for the United States: a population-based study from the United States Cancer Statistics database, 2010 through 2014. Cancer. 2019;125:3412–3417. doi: 10.1002/cncr.32207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du X. Racial disparities in health insurance, triple-negative breast cancer diagnosis, tumor stage, treatment and survival in a large nationwide SEER cohort in the United States. Mol Clin Oncol. 2022;16:95. doi: 10.3892/mco.2022.2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clarke CA, Keegan TH, Yang J, Press DJ, Kurian AW, Patel AH, Lacey JV Jr. Age-specific incidence of breast cancer subtypes: understanding the black-white crossover. J Natl Cancer Inst. 2012;104:1094–1101. doi: 10.1093/jnci/djs264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LA, Cronin KA. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106:dju055. doi: 10.1093/jnci/dju055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kohler BA, Sherman RL, Howlader N, Jemal A, Ryerson AB, Henry KA, Boscoe FP, Cronin KA, Lake A, Noone AM, Henley SJ, Eheman CR, Anderson RN, Penberthy L. Annual report to the nation on the status of cancer, 1975-2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107:djv048. doi: 10.1093/jnci/djv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kong X, Liu Z, Cheng R, Sun L, Huang S, Fang Y, Wang J. Variation in breast cancer subtype incidence and distribution by race/ethnicity in the United States from 2010 to 2015. JAMA Netw Open. 2020;3:e2020303. doi: 10.1001/jamanetworkopen.2020.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Acheampong T, Kehm RD, Terry MB, Argov EL, Tehranifar P. Incidence trends of breast cancer molecular subtypes by age and race/ethnicity in the US from 2010 to 2016. JAMA Netw Open. 2020;3:e2013226. doi: 10.1001/jamanetworkopen.2020.13226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER Research Data, 18 Registries, Nov 2020 Sub (2000-2019) - National Cancer Institute, DCCPS, Surveillance Research Program, released April 2022, based on the November 2021 submission.
- 27.Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS, Thorsen T, Quist H, Matese JC, Brown PO, Botstein D, Lønning PE, Børresen-Dale AL. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001;98:10869–10874. doi: 10.1073/pnas.191367098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pierobon M, Frankenfeld CL. Obesity as a risk factor for triple-negative breast cancers: a systematic review and meta-analysis. Breast Cancer Res Treat. 2013;137:307–314. doi: 10.1007/s10549-012-2339-3. [DOI] [PubMed] [Google Scholar]
- 29.Jiralerspong S, Goodwin PJ. Obesity and breast cancer prognosis: evidence, challenges, and opportunities. J. Clin. Oncol. 2016;34:4203–4216. doi: 10.1200/JCO.2016.68.4480. [DOI] [PubMed] [Google Scholar]
- 30.Plasilova ML, Hayse B, Killelea BK, Horowitz NR, Chagpar AB, Lannin DR. Features of triple-negative breast cancer: analysis of 38,813 cases from the national cancer database. Medicine (Baltimore) 2016;95:e4614. doi: 10.1097/MD.0000000000004614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gershuni V, Li YR, Williams AD, So A, Steel L, Carrigan E, Tchou J. Breast cancer subtype distribution is different in normal weight, overweight, and obese women. Breast Cancer Res Treat. 2017;163:375–81. doi: 10.1007/s10549-017-4192-x. [DOI] [PubMed] [Google Scholar]
- 32.Prakash O, Hossain F, Danos D, Lassak A, Scribner R, Miele L. Racial disparities in triple-negative breast cancer: a review of the role of biologic and non-biologic factors. Front Public Health. 2020;8:576964. doi: 10.3389/fpubh.2020.576964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moss JL, Tatalovich Z, Zhu L, Morgan C, Cronin KA. Triple-negative breast cancer incidence in the United States: ecological correlations with area-level sociodemographics, healthcare, and health behaviors. Breast Cancer. 2021;28:82–91. doi: 10.1007/s12282-020-01132-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siegel SD, Brooks MM, Lynch SM, Sims-Mourtada J, Schug ZT, Curriero FC. Racial disparities in triple negative breast cancer: toward a causal architecture approach. Breast Cancer Res. 2022;24:37. doi: 10.1186/s13058-022-01533-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCarthy AM, Friebel-Klingner T, Ehsan S, He W, Welch M, Chen J, Kontos D, Domchek SM, Conant EF, Semine A, Hughes K, Bardia A, Lehman C, Armstrong K. Relationship of established risk factors with breast cancer subtypes. Cancer Med. 2021;10:6456–6467. doi: 10.1002/cam4.4158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aoki RF, Uong SP, Gomez SL, Alexeeff SE, Caan BJ, Kushi LH, Torres JM, Guan A, Canchola AJ, Morey BN, Lin K, Kroenke CH. Individual- and neighborhood-level socioeconomic status and risk of aggressive breast cancer subtypes in a pooled cohort of women from Kaiser Permanente Northern California. Cancer. 2021;127:4602–4612. doi: 10.1002/cncr.33861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luo J, Kroenke CH, Hendryx M, Shadyab AH, Liu N, Chen X, Wang F, Thomas F, Saquib N, Qi L, Cheng TD, Arthur R, Wactawski-Wende J. Mediation analysis of racial disparities in triple-negative breast cancer incidence among postmenopausal women. Breast Cancer Res Treat. 2021;188:283–293. doi: 10.1007/s10549-021-06158-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Michaels EK, Canchola AJ, Beyer KMM, Zhou Y, Shariff-Marco S, Gomez SL. Home mortgage discrimination and incidence of triple-negative and Luminal A breast cancer among non-Hispanic Black and non-Hispanic White females in California, 2006-2015. Cancer Causes Control. 2022;33:727–735. doi: 10.1007/s10552-022-01557-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sinha S, Bhatia R, Narasimamurthy M, Rayne S, Grover S. Epidemiology of breast cancer presentation in Botswana, South Africa, and the United States. J Surg Res. 2022;279:533–539. doi: 10.1016/j.jss.2022.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siegel SD, Brooks MM, Sims-Mourtada J, Schug ZT, Leonard DJ, Petrelli N, Curriero FC. A population health assessment in a community cancer center catchment area: triple-negative breast cancer, alcohol use, and obesity in New Castle County, Delaware. Cancer Epidemiol Biomarkers Prev. 2022;31:108–116. doi: 10.1158/1055-9965.EPI-21-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]