Abstract
Background:
Physical function decline is a major public health concern and can predict later mortality. This study aims to examine the sociodemographic factors associated with physical function decline among U.S. Chinese older adults through a longitudinal population-based study.
Methods:
Data were derived from the Population Study of Chinese Elderly (PINE) at two time points: 2011–2013 and 2013–2015. Physical function was measured by observed physical performance testing, including chair stand, tandem stand, and timed walk. Mixed-effect models were used to analyze the demographic risk factors associated with physical function decline.
Results:
Of the 2,713 participants in waves 1 and 2, their average age was 72.6 years old, 58.4% were female, with 8.7 years of education average, and 85.8% had an annual individual income of less than $10,000. Our findings show subjects of older age, female sex, lower education, lower income, and a greater number of medical comorbidities had lower physical function levels at baseline. Older adults experienced a faster decline in physical function for the overall performance measure (β = −.02, p < .001). Additionally, elderly adults with higher education have a faster decline of physical function in the overall performance measure (β = −.03, p < .01).
Discussion:
As the first to examine physical function decline among U.S. Chinese older adults, our study finds older age and higher education are two factors associated with a faster rate of physical function decline. In future research, long-term follow up and multiple waves of data are needed to investigate risk or resilience factors for disability or recovering from disability.
Keywords: functional performance, epidemiology, minority aging, risk factors
Physical function and its decline among older adults is a major public health concern given its impact on individuals, their caregivers, and the larger society (1,2). Research has shown that physical function status is a predictor of later disability (3,4), morbidity (5,6), and mortality (7). Physical function limitations are most commonly measured through self-reported difficulty with tasks (Activities of Daily Living, Instrumental Activities of Daily Living, etc.) (3), but these measurements may not accurately reflect an individual’s physical function due to reporting bias and environmental influence (8). Performance-based measures have particular advantages compared to self-reported physical function measurements, such as fewer floor or ceiling effects (9), but these measures are often not included in longitudinal studies.
Further, research has shown that minority older adults, especially those with a lower socioeconomic status, experience higher levels of functional disability compared to their white counterparts (10). In addition, common risk factors of faster functional decline like higher levels of disease and lower socioeconomic status (10,11) are disproportionately experienced by minority older adults (12). While a study of older Hispanic immigrants found minimal functional declines after a 5-year follow-up (13), to our knowledge there are no studies which examine the trajectory of physical function involving performance tests and among U.S. Asian immigrants. Older adult Asian immigrants in the United States experience these particular risk factors at high rates (14,15), but many studies examine Asians as an aggregate group, which is unable to tease apart ethnic group differences and diverse experiences (16).
The Chinese community is the oldest and largest Asian American subgroup in the United States (16). Chinese older adults constitute a large segment of the general Chinese population in the United States, of whom 14.4% are aged 60 years or older (17). Chinese older adults may disproportionately experience physical function decline compared with U.S. older adults, resulting from a variety of socioeconomics, culture beliefs, health literacy, and available social services (18). Longitudinal research on Chinese older adults found male sex and younger old age were associated with physical function decline (19,20). For Chinese in the United States, older Chinese immigrants may not utilize preventive care services which may exacerbate environmental conditions that prompt physical function decline. This may be due to lack of linguistic and culturally appropriate health care services or other service barriers such as cost, distrust of Western medicine, and transportation issues (21). Our previous work has found that U.S. Chinese older adults are vulnerable to functional impairment and related issues (22) and experience multiple disease and symptom burden (23), which have been identified as risk factors for functional impairment (10,11). However, there is a paucity of research concerning the physical function trajectory and its rate of change among of Chinese older adults living outside China, especially in the United States (18).
The objectives of this study are to examine: (a) the 2-year decline of observed physical function performance among U.S. Chinese older adults and (b) the sociodemographic, socioeconomic, and health-related variables associated with these physical function trajectories.
Methods
Population and Settings
The Population Study of Chinese Elderly (PINE) is a population-based epidemiological study of U.S. Chinese older adults in the greater Chicago area. Its purpose is to collect community-level data of U.S. Chinese older adults to examine key determinants of health and well-being. The project was initiated by a community-academic collaboration between Rush Institute for Healthy Aging, Northwestern University, and many community-based social service organizations throughout the greater Chicago area. Detailed descriptions of the first wave of PINE data collection are published elsewhere (24), which were collected from 2011 to 2013. The second wave of data collection for the PINE Study occurred from 2013 to 2015. Of 3,157 wave 1 participants, follow-up interviews were conducted with 2,713 individuals. The Institutional Review Boards of the Rush University Medical Center has approved the PINE study.
Measurements
Sociodemographic characteristics and health status
Sociodemographic characteristics included age, education, annual income, and marital status, which were coded into a dichotomous variable. All analyses involved these characteristics at wave 1 unless otherwise noted. Medical comorbidities were assessed by the presence of nine diseases, such as heart disease, stroke, and diabetes (23).
Observed physical performance testing was measured through the (a) chair stand—ability to rise to a standing position from a chair; (b) tandem stand—a lead-in performance test (semi-tandem), which then followed by either full tandem, or side-by-side, depending on participant’s performance on semi-tandem; and (c) timed walk—an 8-foot timed walk (22). Each item was evaluated with a score ranging from 0 to 5. The three tests were summed for a composite score ranging from 0 to 15 (10), with a higher score indicating better physical function performance. Internal consistency and reliability of these performance tests were proved in the Chicago Health and Aging Project (25,26), with a Cronbach’s α of .69. Time was measured as years from baseline. Time at wave 1 was 0; the mean time at wave 2 was 1.92 years (SD = .30).
Data Analysis
Univariate statistics were used to summarize physical function at two time points, along with the change between time points. Spearman correlations were calculated to determine the relationship between wave 1 sociodemographic variables and change in physical function assessments. Mixed-effect models, which models individual change over time, were used to analyze the demographic risk factors associated with the annual rate of decline in physical function. The total score, walk, and chair used a mixed-effect model using an identity link and normal error distribution. As tandem stand has a nonnormal distribution, reversed coded it and then fit mixed-effect models using a log link with a negative binominal error distribution. We included age, sex, education, income, marital status, and medical conditions in the model. For plots, representative values were chosen to stratify cognitive change. Young–old, middle–old, and old–old age were defined as 65, 75, and 85, respectively. For income, low, middle, high, were defined as $0–4,999, $5,000–$9,999, and $10,000–$14,999. Around 95% of participants had incomes in these three groups; the remaining 5% had an income above $15,000. Education low, middle, and high were defined as completing 8, 12, or 16 years of school. All statistical analyses were undertaken using SAS, version 9.2 (SAS Institute Inc., Cary, NC).
Results
Descriptive Statistics of Wave 1, Wave 2, and Change in Physical Function Measurements
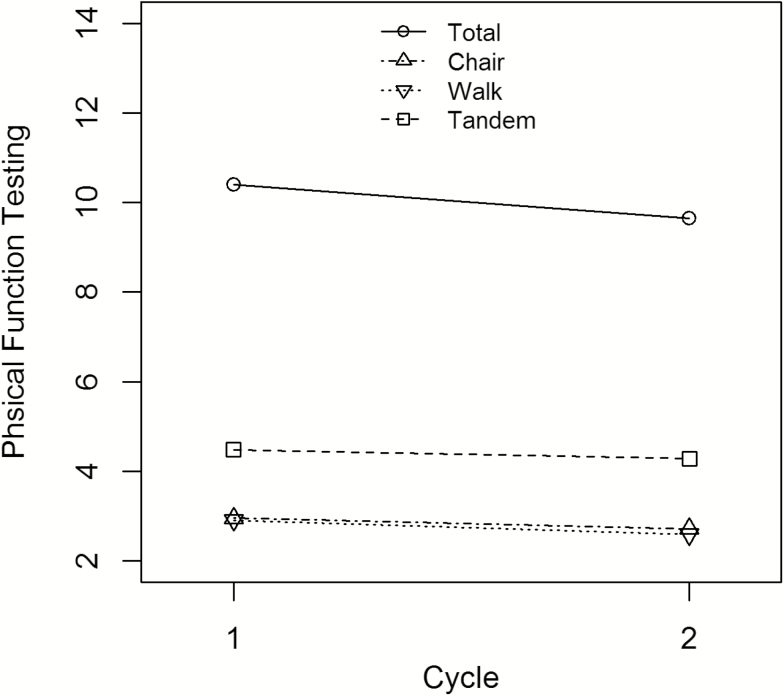
Of the 2,713 participants who were interviewed in waves 1 and 2, the average age was 72.6 years old and 58.4% were female. They had an average of 8.7 years of education, and 85.8% had income of less than $10,000. At wave 1, 70.9% were married. On average, they had 2.1 chronic conditions. Table 1 presents a description of observed physical function measurements. Overall, observed physical performance declined between waves 1 and 2. Figure 1 presents the raw changes of physical function as plotted data between waves 1 and 2.
Table 1.
Descriptive Statistics of Wave 1, Wave 2, and Change in Observed Physical Function Assessment Tests
| Wave 1 | Wave 2 | Change | ||||
|---|---|---|---|---|---|---|
| Physical Function Tests | Total Number | Mean (SD) | Total Number | Mean (SD) | Total Number | Mean (SD) |
| Chair | 2,679 | 2.96 (1.50) | 2,661 | 2.72 (1.56) | 2,628 | −0.23 (1.59) |
| Tandem | 2,682 | 4.48 (1.10) | 2,662 | 4.28 (1.44) | 2,632 | −0.19 (1.27) |
| Walk | 2,713 | 2.91 (1.44) | 2,713 | 2.59 (1.50) | 2,713 | −0.32 (1.75) |
| Total | 2,675 | 10.40 (3.11) | 2,655 | 9.66 (3.58) | 2,618 | −0.72 (3.05) |
Note: Chair = chair stand; Tandem = tandem stand; Walk = measured walk; Total = physical performance tests summary score.
Figure 1.
Plotted data on the raw change of physical performance testing between waves 1 and 2.
Spearman Correlations of Sociodemographic Variables and Change in Physical Function
Table 2 presents sociodemographic variables associated with (waves 1 and 2) changes in physical function assessment. For physical performance testing, older age (r = −.05, p < .05), lower education (r = .06, p < .01), and higher income (r = −.05, p < .01) were associated with performance decline in the chair stand. Older age (r = −.12, p < .001) and more medical comorbidities (r = −.06, p < .01) were associated with performance decline in the tandem stand. Higher education (r = −.20, p < .001) and being married (r = −.05, p < .05) were associated with performance decline in the walk test. Last, older age (r = −.07, p < .001) and higher education (r = −.07, p < .01) were associated with overall performance decline in the physical performance tests.
Table 2.
Spearman Correlations Between Changes in Physical Function Assessments and Sociodemographic Variables
| Age | Sex | Edu | Income | Married | Medical Conditions | |
|---|---|---|---|---|---|---|
| Chair | −.05* | −.02 | .06+ | −.05+ | .04* | .00 |
| Tandem | −.12# | −.03 | .01 | −.02 | .06+ | −.06+ |
| Walk | .03 | .02 | −.20# | .02 | −.05* | .00 |
| Total | −.08# | −.00 | −.07# | −.02 | .01 | −.02 |
Notes: Edu = education; Children = number of children; Chair = chair stand; Tandem = tandem stand; Walk = measured walk; Total = physical performance tests summary score.
*p < .05, +p < .01, #p < .001.
Estimations of Mixed-Effect Models
The unadjusted annual rate of change showed a significant decrease for overall physical performance (β = −.38, p ≤ .001), chair stand (β = −.12, p ≤ .001), tandem stand (β = .17, p < .001), and the walk test (β = −.17, p < .001). Table 3 shows results from a fully adjusted model of sociodemographic and socioeconomic characteristics. Our findings show older age (β = −.15, p < .001), female sex (β = .42, p < .001), lower education (β = .11, p < .001), lower income (β = .10, p < .05), and a greater number of medical comorbidities (β = −.53, p < .001) were associated with lower level of physical function at baseline.
Table 3.
Mixed Models Testing the Associations Between Sociodemographic, SES Variables, and Change in Physical Function Assessments
| β Estimate (Standard Deviation), p value | ||||
|---|---|---|---|---|
| Physical Performance Testing | ||||
| Model Term | Chair | Tandem × | Walk | Total |
| Time | −.07 (.05) | .18 (.09)* | −.22 (.05)# | −.35 (.09)# |
| Age | −.05 (.00)# | .09 (.01)# | −.05 (.00)# | −.15 (.01)# |
| Age × Time | −.01 (.00)* | .00 (.00) | .00 (.00) | −.02 (.00)# |
| Sex | .26 (.06)# | −.25 (.10)* | .06 (.05) | .42 (.11)# |
| Sex × Time | −.01 (.04) | .00 (.06) | .04 (.04) | .07 (.07) |
| Education | .02 (.01)+ | −.04 (.01)# | .07 (.01)# | .11 (.01)# |
| Education × Time | .01 (.00)+ | .00 (.01) | −.04 (.00)# | −.03 (.01)# |
| Income | .09 (.03)# | −.05 (.05) | .01 (.02) | .10 (.05)* |
| Income × Time | −.03 (.01) | .02 (.03) | .00 (.02) | −.03 (.03) |
| Marital Status | −.03 (.07) | −.11 (.10) | −.13 (.06)* | −.13 (.13) |
| Marital Status × Time | −.02 (.05) | .03 (.06) | .04 (.04) | .01 (.08) |
| Medical Conditions | −.24 (.02)# | .33 (.04)# | −.15 (.02)# | −.53 (.05)# |
| Medical Conditions × Time | .01 (.02) | −.03 (.03) | .00 (.02) | .00 (.03) |
*p < .05, +p < .01, #p < .001.
× Reversed coded.
On average, total physical performance is declining at an annual rate of 0.35 units. Older age significantly increased the rate of physical performance decline among the overall physical performance tests (β = −.02, p < .001) and chair stand (β = −.01, p < .01). Higher education increased the rate of physical performance decline in the walk test (β = −.04, p < .001) and the overall physical performance measure (β = −.03, p < .01). Income and number of medical conditions were not significantly associated with rate of physical performance decline.
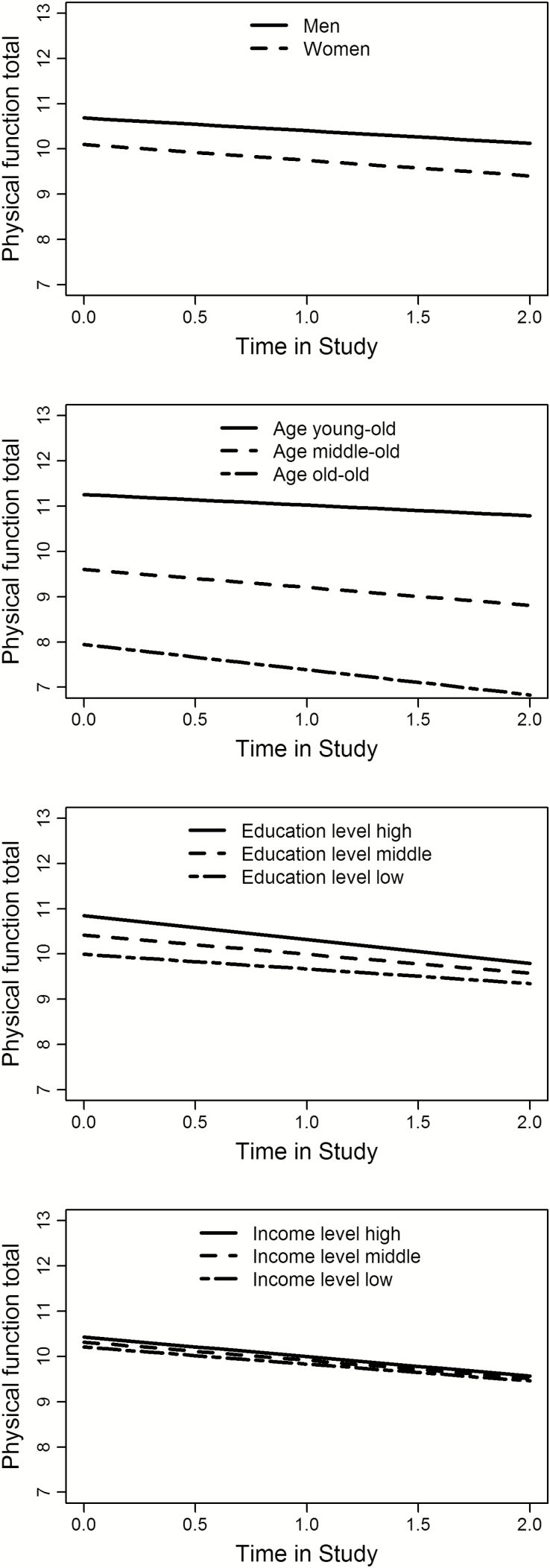
Figure 2 shows the plotted data on the change of each physical function decline with regard to gender, age, education, and income. From these stratified plots, the largest differences in physical function change correspond to age in both level and rate of change.
Figure 2.
Plotted data on the change in direct physical function testing scores by age, sex, education, and income levels.
Discussion
To our knowledge, this is the first longitudinal study regarding observed physical function performance among community-dwelling U.S. Chinese older adults, which extends prior studies by using directly observed measures to assess physical function and investigates physical function decline in 2 years. Our findings suggest that with respect to age, older individuals experience a faster decline in physical performance in the overall performance measure and the chair stand testing. Individuals with higher education experience a faster decline of physical performance with the overall performance measure and the walk test.
Previous literature has suggested that age and education play significant roles in the aging process, especially with respect to physical function decline. Our findings support claims that physical function is more likely to decline at a faster rate if an individual is older. Studies conducted among older adults in the United States also report physical function declines as age increases (11,27). In addition, the potential protective effect of higher education in relationship to physical performance may diminish. This adds to existing research which supports the idea that individuals with higher levels of education initially have a slow rate of health decline, which then accelerates in older age, also known as the “age-as-leveler” hypothesis (28). The mechanisms of this phenomenon warrant further exploration. Future research should examine the possibility of mortality selection or cohort effect in influencing the relationship between level of education and physical performance trajectory.
Of note, our study finds that individual yearly income and number of medical conditions were not associated with the rate of physical performance decline over time. In contrast, previous research on Chinese older adults using cross-sectional data reported lower income was associated with lower level of physical function (18). A longitudinal study found medical conditions differentially affect physical function decline (11). In our population, individual income may not fully capture an individual’s socioeconomic status, as researchers have indicated that household income or wealth may elucidate relationships between socioeconomic status and physical function (29). Further, there is significant socioeconomic variability within the category of Asian Americans (30), which may obfuscate the association between SES and physical function decline. In our study, education and income are negatively correlated, which may help to explain the differences in their respective relationships to physical function decline. Future research should examine SES through household and individual income or wealth to fully explore this relationship.
This study’s findings should be interpreted with limitations. First, all participants reside in the Greater Chicago area; therefore, the findings of this study may not be generalizable to other Chinese populations. Second, we did not collect information about individual or household wealth, which may have a disparate effect on health outcomes compared to individual yearly income. Third, physical function decline was recorded by two waves data, which may be unable to capture certain changing directions such as impairment followed by recovery. Fourth, based on the two time points of data, raw change of observed physical functioning was computed, which is beneficial to investigate physical function decline despite the potential loss of information and specification errors.
Nevertheless, this study has specific strengths which have wide implications for research, practice, and policy. As the first study to our knowledge which examines the physical function decline of U.S. Chinese older adults, we demonstrated some of the complexities regarding physical function decline. First, by using a short battery of physical performance tests versus self-reported physical function, we were able to reduce respondent bias from our main outcome of interest. Second, our findings indicate that physical function decline among U.S. Chinese older adult is experienced differently than among other populations, due to the nonsignificant associations between income, medical conditions, and the rate of physical performance change. Therefore, it may be advantageous to identify at-risk Chinese older adults through other metrics, such as age and education, rather than income and medical comorbidities. Culturally relevant health interventions for U.S. Chinese older adults must adjust their targeted populations accordingly. Third, our study points to some preliminary differences between Chinese in the United States versus in China. For example, compared to longitudinal studies in China (19,20), we did not find male gender or younger age to be associated with physical function decline. Our findings may speak to how the immigrant experience impacts aging and health for U.S. Chinese.
In future research, long-term follow-up and multiple waves data are needed to investigate different facets of physical function trajectory. Future research should examine both disability and recovery in physical function during late life. Research focusing on older adults who develop significant impairment can examine the risk factors for their physical function decline, while examining older adults who recover from physical impairment would be beneficial to identify factors contributing to physical resilience. Future studies are needed to elucidate additional risk/protective factors and potential adverse health consequences of physical function decline in Chinese populations.
Conclusion
This study is the first to show physical function decline among U.S. Chinese older adults. As age increases, older adults experience a faster decline in physical performance for the overall performance measure and the chair stand. Older adults with higher education have a faster decline of physical performance in the overall performance measure and the walk test. Future research may focus on the trajectory of developing significant impairment and recovering from physical impairment of older adults to identify the risk and resilience factors by multiple waves data.
Contributor Information
XinQi Dong, Chinese Health, Aging, and Policy Program, Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, Illinois..
Stephanie M. Bergren, Chinese Health, Aging, and Policy Program, Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, Illinois.
Melissa A. Simon, Feinberg School of Medicine, Northwestern University, Chicago, Illinois.
References
- 1. Trupin L, Rice DP, Max W. Medical Expenditures for People with Disabilities it the United States, 1987. Washington, DC: U.S. Department of Education, National Institute on Disability and Rehabilitation Research; 1995. [Google Scholar]
- 2. Ettner SL. The opportunity costs of elder care. J Hum Resour. 1996;31:189–205. doi:10.2307/146047 [Google Scholar]
- 3. Freedman VA Martin LG Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002;288:3137–3146. doi:10.1001/jama.288.24.3137 [DOI] [PubMed] [Google Scholar]
- 4. Guralnik JM Fried LP Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health. 1996;17:25–46. doi: 10.1146/annurev.pu.17.050196.000325 [DOI] [PubMed] [Google Scholar]
- 5. Wallman T Wedel H Johansson S et al. The prognosis for individuals on disability retirement An 18-year mortality follow-up study of 6887 men and women sampled from the general population. BMC Public Health. 2006;6:1. doi: 10.1186/1471-2458-6-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guralnik JM Simonsick EM Ferrucci L et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi:https://doi.org/10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- 7. Johnson NE. The racial crossover in comorbidity, disability, and mortality. Demography. 2000;37:267–283. doi:10.2307/2648041 [PubMed] [Google Scholar]
- 8. Crimmins EM. Mixed trends in population health among older adults. J Gerontol B Psychol Sci Soc Sci. 1996;51:S223–S225. doi:https://doi.org/10.1093/geronb/51B.5.S223 [DOI] [PubMed] [Google Scholar]
- 9. Sherman SE Reuben D. Measures of functional status in community-dwelling elders. J Gen Intern Med. 1998;13:817–823. doi:10.1046/j.1525-1497.1998.00245.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mendes de Leon CF Barnes LL Bienias JL Skarupski KA Evans DA. Racial disparities in disability: recent evidence from self-reported and performance-based disability measures in a population-based study of older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60:S263–S271. doi:https://doi.org/10.1093/geronb/60.5.S263 [DOI] [PubMed] [Google Scholar]
- 11. Stuck AE Walthert JM Nikolaus T Büla CJ Hohmann C Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–469. doi:http://dx.doi.org/10.1016/S0277-9536(98)00370-0 [DOI] [PubMed] [Google Scholar]
- 12. Fuller-Thomson E Nuru-Jeter A Minkler M Guralnik JM. Black-White disparities in disability among older Americans: further untangling the role of race and socioeconomic status. J Aging Health. 2009;21:677–698. doi: 10.1177/0898264309338296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ailinger RL Dear MR Holley-Wilcox P. Predictors of function among older Hispanic immigrants: a five-year follow-up. Nurs Res. 1993;42:240–244. [PubMed] [Google Scholar]
- 14. A Statistical Profile of Older Asian Americans. Adminstration for Community Living. Washington, DC: Administration for Community Living; 2015. [Google Scholar]
- 15. Asian Pacific American Legal Center; Asian American Justice Center. A Community of Contrasts: Asian Americans in the United States, 2011. San Fransisco, CA: Asian Americans Advancing Justice; 2011. [Google Scholar]
- 16. Holland AT Palaniappan LP. Problems with the collection and interpretation of Asian-American health data: omission, aggregation, and extrapolation. Ann Epidemiol. 2012;22:397–405. doi: 10.1016/j.annepidem.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. American fact finder [Internet]. United States Census Bureau. 2010. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed January 1, 2017.
- 18. Dong X Su D. Epidemiology of physical function impairment in global Chinese aging population: a systematic review. J Geriatrics Palliative Care. 2016;4:23. [Google Scholar]
- 19. Feng Q Zhen Z Gu D Wu B Duncan PW Purser JL. Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998-2008. J Gerontol B Psychol Sci Soc Sci. 2013;68:476–485. doi: 10.1093/geronb/gbt012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liang Y Song A Du S Guralnik JM Qiu C. Trends in disability in activities of daily living among Chinese older adults, 1997–2006: the China Health and Nutrition Survey. J Gerontol A Biol Sci Med Sci. 2014;70:glu204. doi:https://doi.org/10.1093/gerona/glu204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Aroian KJ Wu B Tran TV. Health care and social service use among Chinese immigrant elders. Res Nurs Health. 2005;28:95–105. doi: 10.1002/nur.20069 [DOI] [PubMed] [Google Scholar]
- 22. Dong X Chang ES Simon MA. Physical function assessment in a community-dwelling population of U.S. Chinese older adults. J Gerontol A Biol Sci Med Sci. 2014;69(suppl 2):S31–S38. doi: 10.1093/gerona/glu205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dong X Chen R Simon MA. The prevalence of medical conditions among U.S. Chinese community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2014;69(suppl 2):S15–S22. doi: 10.1093/gerona/glu151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dong X Wong E Simon MA. Study design and implementation of the PINE study. J Aging Health. 2014;26:1085–1099. doi:10.1177/0898264314526620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dong X Simon M Fulmer T de Leon CFM Rajan B Evans DA. Physical function decline and the risk of elder self-neglect in a community-dwelling population. Gerontologist. 2010;50:316–326. doi:https://doi.org/10.1093/geront/gnp164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dong X Simon M Evans D. Decline in physical function and risk of elder abuse reported to social services in a community-dwelling population of older adults. J Am Geriatr Soc. 2012;60:1922–1928. doi: 10.1111/j.1532-5415.2012.04147.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Penninx BW Guralnik JM Ferrucci L Simonsick EM Deeg DJ Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. JAMA. 1998;279:1720–1726. doi:10.1001/jama.279.21.1720 [DOI] [PubMed] [Google Scholar]
- 28. Herd P. Do functional health inequalities decrease in old age? Educational status and functional decline among the 1931–1941 birth cohort. Res Aging. 2006;28:375–392. doi:10.1177/0164027505285845 [Google Scholar]
- 29. Braveman PA Cubbin C Egerter S et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879 [DOI] [PubMed] [Google Scholar]
- 30. Sakamoto A Goyette KA Kim CH. Socioeconomic attainments of Asian Americans. Annu Rev Sociol. 2009;35:255–76. doi:10.1146/annurev-soc-070308-115958 [Google Scholar]