Abstract
Background
This study aimed to evaluate the feasibility and acceptability of engaging unhoused peer ambassadors (PAs) in coronavirus disease 2019 (COVID-19) vaccination efforts to reach people experiencing unsheltered homelessness in Los Angeles County.
Methods
From August to December 2021, vaccinated PAs aged ≥18 years who could provide informed consent were recruited during vaccination events for same-day participation. Events were held at encampments, service providers (eg, housing agencies, food lines, and mobile showers), and roving locations around Los Angeles. PAs were asked to join outreach alongside community health workers and shared their experience getting vaccinated, receiving a $25 gift card for each hour they participated. Postevent surveys evaluated how many PAs enrolled and how long they participated. In October 2021, we added a preliminary effectiveness evaluation of how many additional vaccinations were attributable to PAs. Staff who enrolled the PAs estimated the number of additional people vaccinated because of talking with the PA.
Results
A total of 117 PAs were enrolled at 103 events, participating for an average of 2 hours. At events with the effectiveness evaluation, 197 additional people were vaccinated over 167 PA hours ($21.19 gift card cost per additional person vaccinated), accounting for >25% of all vaccines given at these events.
Discussion
Recruiting same-day unhoused PAs is a feasible, acceptable, and preliminarily effective technique to increase COVID-19 vaccination in unsheltered settings. The findings can inform delivery of other health services for people experiencing homelessness.
Keywords: COVID-19, Vaccination, Homelessness, Peer education
People experiencing homelessness are at elevated risk of disease and death associated with coronavirus disease 2019 (COVID-19), as a higher burden of comorbid conditions intersects with socioeconomic risk factors [1–4]. Lack of permanent housing may make it more difficult to mitigate COVID-19 exposure through recommended behaviors, such as social distancing, mask wearing, and regular handwashing [5–7]. In Los Angeles County, the most recent estimates (from January 2020) suggest that ≥66 000 residents are unhoused, the majority unsheltered, with only a quarter of the unhoused population staying in shelters at a given time [8]. Beyond challenges faced by all individuals experiencing homelessness, people living in unsheltered settings, such as encampments, face additional, unique challenges in accessing medical care [9].
In addition, although early in the pandemic there was evidence of reduced COVID-19 acquisition among people experiencing homelessness staying in open air environments [10, 11], more recent outbreak data from the Los Angeles County Department of Public Health provides evidence that crowded encampments may facilitate disease transmission comparably to indoor congregate shelters [12]. Regardless, people experiencing homelessness who acquired COVID-19 experienced an estimated 30% higher case fatality rate than the general population, as shown in an analysis of publicly available data by Leifheit et al [1].
Immunization against COVID-19 is the most effective means to prevent infection, severe illness, and death [13]. However, limited access to routine healthcare services and concerns about the COVID-19 vaccine are barriers to achieving sufficient coverage among people experiencing homelessness [2–4]. We conducted a field survey during vaccine clinics and outreach in May and June 2021 and nearly 600 people experiencing homelessness responded. We found that 36% reported already being vaccinated, 34% wanted to get the vaccine that day, and 30% declined at the time of the survey [14]. Of the unvaccinated people who declined vaccination that day, 56% reported they were “not yet” ready to be vaccinated, rather than “never” wanting the vaccine [14]. A more in-depth survey of 90 people experiencing homelessness in Los Angeles County revealed that 48% of respondents reported some degree of vaccine hesitancy, citing safety concerns owing to rapid development of the vaccines, belief that vaccination is unnecessary because of low perceived risk, lack of trust in government, and negative past experiences in clinical settings due to the stigma of homelessness [2].
The erosion of trust in government and health officials, fueled in part by misinformation campaigns and historical injustices, requires leveraging of social networks to allay fears, provide vaccine education, and promote COVID-19 vaccine uptake among people experiencing homelessness [3, 4]. Sociobehavioral research demonstrates the influence of social context, in-group identities, and observational learning prompts behavior change in individuals [15–18]. Engaging peers and people with relevant lived experience has been shown to play a key role in promoting immunization [19]. Community health workers (CHWs) with lived experience of homelessness have been instrumental in behavioral interventions focused on substance use disorder recovery, cancer care, and infectious disease [20–22]. The US Department of Housing and Urban Development recommends using peer ambassadors (PAs) as a strategy to promote vaccine education and uptake among people experiencing homelessness [23]. Peers are an important influence on health behaviors and can serve as trusted sources of information to persuade hesitant individuals to accept COVID-19 vaccines [24, 25].
In this academic and community partnership, we conducted a demonstration project to recruit vaccinated individuals with lived experience of homelessness to serve as same-day PAs during COVID-19 vaccination clinics in unsheltered settings in Los Angeles County, California. Crucially, we also trained and built capacity for full-time CHWs (many with lived experience of homelessness themselves) to recruit, consent, and supervise PAs. We conducted a hybrid feasibility-evaluation study on this demonstration project.
METHODS
Study Rationale
This project was developed as a demonstration project in partnership between academic and government partners in Los Angeles County. Housing for Health is a division of the Los Angeles County Department of Health Services that provides health services and housing opportunities to people experiencing homeless. Housing for Health was funded by the Los Angeles County Department of Public Health to create COVID-19 response teams to provide onsite testing and later vaccination in highly mobile teams across the county, with the guiding principle of meeting people experiencing homelessness where they were. Housing for Health began holding vaccination events in January 2021. A PA program was envisioned as one part of the vaccine educational strategy, but feasibility and best practices in unsheltered settings were unknown. A partnership with academic medical faculty presented an opportunity to undertake this demonstration project.
Ethical Considerations
The UCLA Institutional Review Board approved all study procedures (protocol no. 21-000951). Participants provided written consent to participate. Training in research ethics, including conducting informed consent conversation, was provided to Housing for Health staff in 3 stages. Each person who would act as research staff for the purposes of this study was required to complete all 3 in sequence before being certified by the principal investigator (PI) (C. L. S.) to conduct informed consent with participants. These stages included (1) completing online training from the Collaborative Institutional Training Initiative (“Basic Course—Human Subjects Research”), (2) viewing a 1-hour live or prerecorded consent and safety training session led by the PI, and (3) individual, in-field observation with the PI or UCLA research staff, including mock consent (with a coworker playing the role of potential research participant) or mentored consent (with the trainee staff member leading the consent conversation with a participant, while UCLA staff observed and gave feedback as needed). Step 3 was repeated over days or weeks as needed, until the staff member was confident, comfortable, and competent to conduct the informed consent process with participants. Training in managing and reporting gift cards was provided by Housing for Health staff concurrently with the research training.
Setting
Housing for Health had 4 regional COVID-19 response teams that conducted vaccination events in unsheltered settings in all regions of Los Angeles County. At vaccination events, CHWs—full-time outreach staff with experience in homeless services and/or lived experience of homelessness—talked to potential clients about vaccination and distributed supplies, including food, water, hygiene supplies, and harm reduction kits (eg, naloxone, clean needles, and pipes), as well as prepaid mobile phones to facilitate follow-up for second doses for clients receiving messenger RNA vaccines. Clinical staff were available to administer vaccines, and street medicine clinical partners provided other medical care (eg, blood pressure checks, wound care, rapid COVID-19 testing). Vaccination events were held 6 days a week at rotating locations, with each team holding as many as 2 events per day on weekdays and fewer on weekends. To build relationships over time, CHWs also conducted outreach and education in advance of vaccination events. Moreover, repeated visits to sites over time (eg, for second doses and to engage with people who were not present during earlier visits) helped build rapport.
PAs were the focal participants of this analysis. They were recruited during vaccination events for same-day participation. As CHWs conducted outreach in the vicinity of the clinic, typically on foot, they could recruit PAs from nearby areas even if the prospective PA had not yet visited the vaccination clinic that day. Eligibility criteria for PAs included lived experience of homelessness, receipt of ≥1 dose of a COVID-19 vaccine, age ≥18 years, ability to speak English or Spanish fluently, and ability to provide informed consent. PAs completed informed consent in English or Spanish by trained study staff fluent in the participant’s chosen language. PAs were eligible to participate up to 4 hours per day, 20 hours in total, with up to 2 PAs per event at a time. Participants were compensated with a $25 gift card for each hour they participated.
The vaccination status of PAs was verified by directly observing the receipt of a dose, locating the participant’s COVID-19 vaccination record on the California Immunization Registry, or viewing the participant’s vaccination card. To reduce barriers to PA participation, study staff collected only limited personal data needed to verify vaccination status (first name, last name, and date of birth) and optional contact information for those who wanted to participate in future events. PAs were asked to share their experience of being vaccinated and participating in outreach alongside Housing for Health staff. Participant information was collected on paper forms in the field and then submitted electronically as a postevent survey. On these forms, research staff could enter additional notes about the event or PA’s experience, which we have included in Supplementary Table 1.
Initially, the program was piloted at a subset of Housing for Health’s vaccination events, approximately 40 per week, in unsheltered settings including encampments, safe parking sites, parks, recycling centers, and service providers. For the first 8 weeks (from 5 August to 30 September 2021), UCLA research staff primarily recruited and consented PA participants. Concurrently, UCLA research staff conducted the research trainings described above to build capacity for CHWs, who did not have prior research experience, to recruit and consent participants, holding the first in-field consent training on 8 September 2021. We examined the experience of CHWs in research participation in a qualitative study [26]. After increased study capacity to enroll PAs, we conducted an informal evaluation of the PA program for an additional 7 weeks.
Measures and Statistical Methods
The primary outcomes of the demonstration project were feasibility, measured by the number of PAs who were enrolled, and acceptability, measured by the average number of hours PAs participated (collected from 5 August to 3 December 2021). Early anecdotal success prompted the team to add a more detailed evaluation alongside these original outcomes. At 10 weeks into the study, we added an evaluation question to the postevent survey: “How many clients got vaccinated as a result of talking to the PA?” Research staff (including CHWs) were instructed to estimate the number of clients the PA recruited to be vaccinated, clients whom the staff determined were unlikely to been vaccinated that day without the PA’s involvement (collected from 13 October to 3 December 2021 only for events during that period).
Drawing on the epidemiology concept of “person-time,” we used the postevent survey responses to this question to calculate the number of additional clients vaccinated per hour of PA participation [27]. We used these metrics to calculate the additional cost (in PA hourly compensation) associated with an additional person vaccinated, averaged across all PAs who participated during the evaluation period. Based on this postevent survey question, we also calculated the proportion of all doses administered at the event that were attributed to the PA. We obtained the denominator for this proportion, the total number of vaccines administered at each event, using Housing for Health’s administrative records, which were kept separately from the study data.
The staff notes in the postevent survey provided descriptive data on implementation questions that emerged as the project started. Because we did not set out to collect these notes for a formal qualitative analysis, we simply provide them in Supplementary Table 1. Three authors (C. L. S., A. F., and R. R.) grouped the comments thematically for readability but no further systematic analysis was performed on the notes.
RESULTS
Between 5 August and 3 December 2021, a total of 117 unique PAs were enrolled at 103 unsheltered vaccination events. They participated for an average of 2 hours (range, 1–10 hours) in total, with 8 participating on 2 days, 1 participating on 3 days, and 1 participating on 4 days. The average age of PAs was 48.6 years, with an age range of 20–73 years. Nine participants completed the informed consent process in Spanish, and a larger number conducted outreach in both English and Spanish.
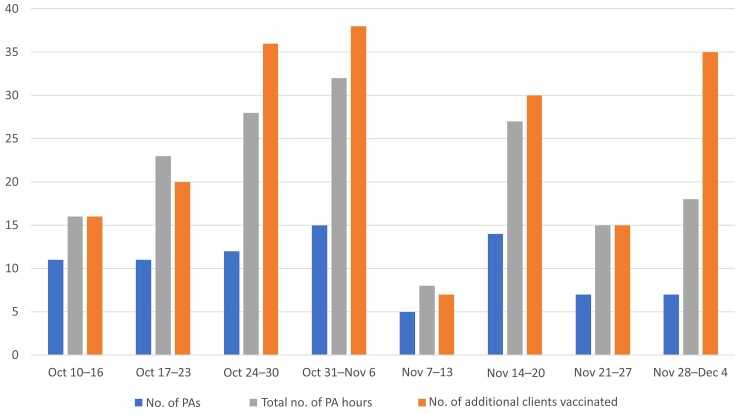
At 63 events (from 13 October to 3 December 2021) for which data were available for the number of additional clients vaccinated as a result of talking to a PA, 197 additional people were vaccinated over 167 PA hours. This corresponds to a gift card cost of $21.19 per additional person vaccinated. The number of additional vaccinations attributed to a PA on a single day of participation ranged from 0 to 15. Figure 1 shows the weekly number of PAs, PA hours, and people vaccinated as a result of talking with a PA based on the postevent survey. Denominators (total number of vaccines given) were not available for 2 events hosted by external clinical partners of Housing for Health). At the events for which the total number of vaccines was available, the 197 additional vaccinations attributed to the PAs accounted for 28% of the 678 doses given across these 61 unique events.
Figure 1.
Vaccinations attributable to peer ambassadors (PAs) by week. Bars represent the number of PAs for the given week (first bar, left to right), the total number of PA hours for that week (second bar), and the number of additional clients vaccinated (third bar).
Four categorical themes emerged from the staff notes: characteristics of a PA, techniques that a PA used, future outreach (eg, whether or not the staff recommended engaging the PA at a later event), and barriers the PA faced. Staff notes conveyed that the personal connection of the program was often key, with PAs engaging people who had previously been hesitant to engage with Housing for Health staff in the past (Supplementary Table 1). Comments on techniques revealed that PAs sharing their own story was often central to persuading others to take the COVID-19 vaccine.
DISCUSSION
This project demonstrated that it is feasible to recruit same-day peer vaccine PAs in unsheltered settings, and this program is acceptable to participants. Furthermore, preliminary evaluation data suggest that the PAs are effective at increasing vaccination uptake among people experiencing homelessness. We estimated that on average during our demonstration project, for each hour that a PA participated, 1 additional person was vaccinated. Because this evaluation was based on observations by research staff, rather than directly asking the people who were vaccinated why they did so, this should be interpreted as plausible rather than definitive evidence.
The low-barrier method of inviting people to join outreach for as little as an hour illustrates a promising way to involve and empower community members to participate in public health work. The fact that during the pilot most PAs only participated once and for a relatively short duration (average, 2 hours) underscores the strength of this “foot in the door” approach in this setting rather than starting with an intervention with more expectations of participants [28]. Because PAs are residents of the settings where they conduct outreach, there is additional benefit to them in community immunity if more of their neighbors get vaccinated. Compensating people to share their vaccine story and positively encourage their peers honors the education many are already doing in their communities.
From the focus group discussions with CHWs, one salient concern was finding ways to make a more lasting improvements in the lives of PAs after this brief participation, to avoid exploiting the valuable trust they have with their communities [26]. This is an extremely important area for follow-up research: in the setting of unsheltered homelessness, how can we design programs to empower people to get involved with whatever ability they have in the moment, and also create avenues for sustained impact? Further research investigating the potential long-term effects on PAs is also warranted, given the prior research finding that without proper support, the impact on peer health workers who participate in similar interventions can be negative or even traumatic [29].
This work builds on the literature of peer support to show how these principles can be applied in a rapid and brief way. Although the model of COVID-19 vaccine ambassadors in unsheltered settings is novel, there is substantial precedent for involving peer navigators and peer support workers to deliver homeless services [30, 31]. Descriptive notes from our study demonstrate how PAs were uniquely able to influence their neighbors to get vaccinated, at times engaging and succeeding among individuals who had previously declined vaccination when approached by outreach staff. The ability of PAs to connect with these individuals is especially important because they would otherwise likely go unreached and unvaccinated. This model may be applicable to other communities of hardly reached people and is worth exploring in other settings. Moreover, it is likely that a PA model would also work for other vaccination efforts for people experiencing homelessness. Demonstrating success with COVID-19 vaccination, a vaccine with a high degree of mistrust surrounding it, suggests the PA approach may work as well or better for other vaccine-preventable diseases, such as hepatitis A, hepatitis B, measles, mumps, rubella, influenza, and cervical cancer.
A study of US Medicare beneficiaries found that the average cost per COVID-19–related hospital stay was >$21 752, which rose to $49 441 for those who needed a ventilator and $32 015 for those who died [32]. Our estimated $21.19 in gift card costs per additional person vaccinated suggests that the PA program has the potential to be a cost effective addition to vaccination efforts, even at high thresholds for the number of vaccinated persons to prevent a single hospitalization [33]. The findings from this demonstration project may be useful to parameterize future cost-effectiveness models examining the roles of peer outreach workers in vaccine strategies.
One key limitation of the current study is the lack of certainty in attributing vaccinations to PAs specifically. Asking research staff to report how many additional people were vaccinated because they talked with PAs may be subject to social desirability bias, which would also have been a concern had we directly interviewed the PAs or the people who were vaccinated. The PA program was implemented alongside other efforts to increase vaccination, including monetary incentives for being vaccinated, messaging about the Delta variant, and vaccine requirements by the city and county for some sectors and settings. Any of these factors, alone or in combination, may account for individual decisions to be vaccinated. In addition, PAs were not recruited at all vaccination events. Vaccination events varied in location, size, duration, and subjective factors such as community engagement that made comparison between PA and non-PA events not feasible within the scope of this pilot study. Our evaluation findings should therefore be understood as preliminary and establish the plausibility of success by such a PA program. Further research describing the benefits of this program compared with other vaccine promotions and control vaccination events is warranted.
Despite these limitations, our study demonstrates large potential for same-day PA programs, particularly on those for COVID-19 vaccination. Via quantitative and descriptive data, our study suggests that the PA program added value for the community served, program staff, and funders. Given these promising results, organizations involved in COVID-19 response and other vaccination efforts should consider whether same-day PAs could benefit their work. The 2 lessons learned from our study have potential implications for other public health programs in hardly reached communities. The first lesson is that the “foot in the door” approach to engaging participation might be key, particularly with people who may struggle with long commitments owing to the instability of their lives and the mental health challenges common among those who are unhoused [28]. The second and most important lesson is that peer contact seems critical in this community. This same-day PA model may be applied to deliver other programs or services. Future work may test it in delivering addiction treatment, preventive medicine, or social services. The PA model may also present an avenue to scale up to longer-term employment for PAs, and implementation studies examining that outcome are warranted.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Acknowledgments. The authors thank all the peer ambassadors who participated in this study. You have taught us so much by modeling peer-to-peer vaccine education. The authors also thank the coronavirus disease 2019 (COVID-19) response team staff of Housing for Health, without whom this project would not have been possible.
Author contributions. Conceptualized the study and obtained funding: C. L. S., A. Bratcher, A. H. C., K. R. C., S. S., E. B., L. G., P. M. G., A. W. R., and E. H. T. Recruiting and obtaining consent from participants, data collection, and crucial intellectual contributions to the field-based implementation protocol: C. L. S., J. M., B. R., J. A., A. F., R. R., J. B., A. Bratcher, K. R. C., C. G., P. G., L. R., G. S., A. Baez, A. C., S. H., S. J., C. L., J. Swan, K. T., M. M., A. Rice, M. R., and J. Spoliansky. Programmatic oversight and direction of the project within the Los Angeles County Department of Health Services: J. M., B. R., E. U. K., A. N., and E. H. T. Supervision of the research project as principal investigator: C. L. S. Data analyses: C. L. S. and A. Rosen. Lead writer for the first draft: C. L. S. Contributions to the first draft: J. A., A. F., R. R., and J. B. All authors read and approved the final manuscript.
Financial support. This work was supported by the UCLA David Geffen School of Medicine COVID-19 Research Fund (grant HE-0025); the Centers for Disease Control and Prevention (funding for Housing for Health COVID-19 response teams, through the Los Angeles County Department of Public Health [grants for Covid Response and Relief: ELC Enhancing Detection–6 NU50CK000498-01-09 and ELC Enhancing Detection Expansion–6 NU50CK000498-02-04]; the UCLA David Geffen School of Medicine COVID-19 Research Fund (grant HE-025 the National Institute on Drug Abuse (career development support grant K01-DA050771 to C. L. S.); the Agency for Healthcare Research and Quality (K12 career development support to K. R. C.); and the Patient-Centered Outcomes Research Institute (grant K12HS26407-01 to K. R. C.)
Supplement sponsorship. This article appears as part of the supplement “Homelessness and Infectious Diseases: Understanding the Gaps and Defining a Public Health Approach,” sponsored by the Centers for Disease Control and Prevention.
Supplementary Material
Contributor Information
Chelsea L Shover, Division of General Internal Medicine and Health Services Research, UCLA David Geffen School of Medicine, Los Angeles, California, USA.
Allison Rosen, Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, California, USA; Los Angeles County Department of Health Services, Los Angeles, California, USA.
José Mata, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Brooke Robie, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Julissa Alvarado, Department of Environmental Health Sciences, UCLA Fielding School of Public Health, Los Angeles, California, USA.
Ashley Frederes, Department of Community Health Sciences, UCLA Fielding School of Public Health, Los Angeles, California, USA.
Ruby Romero, Division of General Internal Medicine and Health Services Research, UCLA David Geffen School of Medicine, Los Angeles, California, USA.
Jacqueline Beltran, Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, California, USA.
Anna Bratcher, Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, California, USA.
Alicia H Chang, Los Angeles County Department of Public Health, Los Angeles, California, USA.
Kristen R Choi, Department of Health Policy and Management, UCLA Fielding School of Public Health, Los Angeles, California, USA; UCLA School of Nursing,, Los Angeles, California, USA.
Candelaria Garcia, Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, California, USA.
Steven Shoptaw, Department of Family Medicine, UCLA David Geffen School of Medicine, Los Angeles, California, USA.
Priyanka Guha, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Lindsey Richard, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Gunner Sixx, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Angel Baez, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Anthony Coleman, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Sarah Harvell, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Shirnae Jackson, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Caroline Lee, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Joanna Swan, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Kenny Torres, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Emily Uyeda Kantrim, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Maya McKeever, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Anh Nguyen, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Adam Rice, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Marisol Rosales, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Jordan Spoliansky, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Elizabeth Bromley, Psychiatry and Biobehavioral Sciences, UCLA David Geffen School of Medicine, Los Angeles, California, USA.
Heidi Behforouz, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Lillian Gelberg, Department of Health Policy and Management, UCLA Fielding School of Public Health, Los Angeles, California, USA; Department of Family Medicine, UCLA David Geffen School of Medicine, Los Angeles, California, USA.
Pamina M Gorbach, Division of General Internal Medicine and Health Services Research, UCLA David Geffen School of Medicine, Los Angeles, California, USA; Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, California, USA.
Anne W Rimoin, Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, California, USA.
Emily H Thomas, Los Angeles County Department of Health Services, Los Angeles, California, USA.
Data Availability
Data are available to the research team only, according to the terms of consent provided by participants.
References
- 1. Leifheit KM, Chaisson LH, Medina JA, Wahbi RN, Shover CL. Elevated mortality among people experiencing homelessness with COVID-19. Open Forum Infect Dis 2021; 8:ofab301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kuhn R, Henwood B, Lawton A, et al. COVID-19 vaccine access and attitudes among people experiencing homelessness from pilot mobile phone survey in Los Angeles, CA. PLoS One 2021; 16:e0255246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kushel M, DiPietro B, Watts B. Bringing covid-19 vaccines to high risk populations—like those who are homeless—requires a tailored approach. 2021. https://blogs.bmj.com/bmj/2021/03/22/bringing-covid-19-vaccines-to-high-risk-populations-like-those-who-are-homeless-requires-a-tailored-approach/. Accessed 18 July 2022.
- 4. Castillo G, O’Gorman CM, Crawshaw J, et al. Factors affecting COVID-19 vaccination among people experiencing homelessness and precarious housing in Canada: a behavioural analysis. 2021. https://www.mcmasterforum.org/docs/default-source/product-documents/living-evidence-syntheses/covid-19-living-evidence-synthesis-4.5---vaccine-confidence-among-homeless-and-housing-precarious-populations.pdf?sfvrsn=3034ef6b_5. Accessed 18 July 2022.
- 5. Montgomery MP, Carry MG, Garcia-Williams AG, et al. Hand hygiene during the COVID-19 pandemic among people experiencing homelessness—Atlanta, Georgia, 2020. J Community Psychol 2021; 49:2441–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Henwood BF, Redline B, Lahey J. Surveying tenants of permanent supportive housing in skid row about COVID-19. J Health Care Poor Underserved 2020; 31:1587–94. [DOI] [PubMed] [Google Scholar]
- 7. Karb R, Samuels E, Vanjani R, Trimbur C, Napoli A. Homeless shelter characteristics and prevalence of SARS-CoV-2. West J Emerg Med 2020; 21:1048–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Los Angeles Homeless Services Authority . 2020 Greater Los Angeles homeless count results. 2020. https://www.lahsa.org/news?article=726-2020-greater-los-angeles-homeless-count-results. Accessed 18 July 2022.
- 9. Roncarati JS, Baggett TP, O’Connell JJ, et al. Mortality among unsheltered homeless adults in Boston. Massachusetts 2000–2009. JAMA Intern Med 2018; 178:1242–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yoon JC, Montgomery MP, Buff AM, et al. Coronavirus disease 2019 (COVID-19) prevalences among people experiencing homelessness and homelessness service staff during early community transmission in Atlanta, Georgia, April–May 2020. Clin Infect Dis 2021; 73:e2978–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Owens T, Ewing D, Devera M, et al. Housing for health in the VA greater Los Angeles tent community. Ann Fam Med 2022; 20:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gokhale S, Shover CL, Blake J, et al. Novel coronavirus outbreaks in homeless encampments and shelters in Los Angeles. Council on State and Territorial Epidemiologists. California: Virtual; 2020. [Google Scholar]
- 13. Centers for Disease Control and Prevention . Benefits of getting vaccinated. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html. Accessed 18 July 2022.
- 14. Rosen AD, Beltran J, Thomas E, et al. COVID-19 Vaccine acceptability and financial incentives among unhoused people in Los Angeles county: a three-stage field survey. J Urban Health 2022; 99:594–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rossen I, Hurlstone MJ, Lawrence C. Going with the grain of cognition: applying insights from psychology to build support for childhood vaccination. Front Psychol 2016; 7:1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Daas C D, Hubbard G, Johnston M, Dixon D. Protocol of the COVID-19 health and adherence research in Scotland (CHARIS) study: understanding changes in adherence to transmission-reducing behaviours, mental and general health, in repeated cross-sectional representative survey of the Scottish population. BMJ Open 2021; 11:e044135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. AlSaeed AA, Rabbani U. Explaining COVID-19 vaccine rejection using social cognitive theory in Qassim, Saudi Arabia. Vaccines (Basel) 2021; 9:1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bandura A. Self-efficacy: the foundation of agency. In: Perrig WJ, Grob A, eds. Control of human behavior, mental processes, and consciousness: essays in honor of the 60th birthday of August Flammer. Mahwah, NJ: Lawrence Erlbaum Associates Publishers, 2000:17–33. [Google Scholar]
- 19. Holloway IW, Bednarczyk R, Fenimore VL, et al. Factors associated with immunization opinion leadership among men who have sex with men in Los Angeles, California. Int J Environ Res Public Health 2018; 15:939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Corrigan PW, Pickett S, Batia K, Michaels PJ. Peer navigators and integrated care to address ethnic health disparities of people with serious mental illness. Soc Work Public Health 2014; 29:581–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Corrigan PW, Pickett S, Schmidt A, et al. Peer navigators to promote engagement of homeless African Americans with serious mental illness in primary care. Psychiatry Res 2017; 255:101–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Corrigan PW, Kraus DJ, Pickett SA, et al. Using peer navigators to address the integrated health care needs of homeless African Americans with serious mental illness. Psychiatr Serv 2017; 68:264–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Housing and Urban Development . COVID-19 vaccine distribution: HUD message. 2021. https://www.hud.gov/sites/dfiles/CPD/documents/COVID-19-Vaccination-HUD-Message-2021-01-28-QC.pdf. Accessed 18 July 2022.
- 24. Wood S, Schulman K. When vaccine apathy, not hesitancy, drives vaccine disinterest. JAMA 2021; 325:2435–6. [DOI] [PubMed] [Google Scholar]
- 25. Hsu H-T, Petering R, Onasch-Vera L. Implications of COVID-19 vaccine uptake among young adults experiencing homelessness: a brief report. J Soc Distress Homeless 2021; 30:1–6. [Google Scholar]
- 26. Choi K, Romero R, Guha P, et al. Community health worker perspectives on engaging unhoused peer ambassadors for COVID-19 vaccine outreach in homeless encampments and shelters. J Gen Intern Med 2022; 37:2026–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Boslaugh S, McNutt L. Encyclopedia of epidemiology. Thousand Oaks, California: SAGE Publications, 2008. [Google Scholar]
- 28. Grov C, Bux D, Parsons JT, Morgenstern J. Recruiting hard-to-reach drug-using men who have sex with men into an intervention study: lessons learned and implications for applied research. Subst Use Misuse 2009; 44:1855–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Magwood O, Leki VY, Kpade V, et al. Common trust and personal safety issues: a systematic review on the acceptability of health and social interventions for persons with lived experience of homelessness. PLoS One 2019; 14:e0226306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Barker SL, Maguire N. Experts by experience: peer support and its use with the homeless. Community Ment Health J 2017; 53:598–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Miler JA, Carver H, Foster R, Parkes T. Provision of peer support at the intersection of homelessness and problem substance use services: a systematic ‘state of the art’ review. BMC Public Health 2020; 20:641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tsai Y, Vogt TM, Zhou F. Patient characteristics and costs associated with COVID-19–related medical care among Medicare fee-for-service beneficiaries. Ann Intern Med 2021; 174:1101–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kohli M, Maschio M, Becker D, Weinstein MC. The potential public health and economic value of a hypothetical COVID-19 vaccine in the United States: use of cost-effectiveness modeling to inform vaccination prioritization. Vaccine 2021; 39:1157–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available to the research team only, according to the terms of consent provided by participants.