Abstract
Background
Suicidal behaviors, including suicide deaths and attempts, are major public health concerns. However, previous suicide models required a huge amount of input features, resulting in limited applicability in clinical practice.
Objective
We aimed to construct applicable models (ie, with limited features) for short- and long-term suicidal behavior prediction. We further validated these models among individuals with different genetic risks of suicide.
Methods
Based on the prospective cohort of UK Biobank, we included 223 (0.06%) eligible cases of suicide attempts or deaths, according to hospital inpatient or death register data within 1 year from baseline and randomly selected 4460 (1.18%) controls (1:20) without such records. We similarly identified 833 (0.22%) cases of suicidal behaviors 1 to 6 years from baseline and 16,660 (4.42%) corresponding controls. Based on 143 input features, mainly including sociodemographic, environmental, and psychosocial factors; medical history; and polygenic risk scores (PRS) for suicidality, we applied a bagged balanced light gradient-boosting machine (LightGBM) with stratified 10-fold cross-validation and grid-search to construct the full prediction models for suicide attempts or deaths within 1 year or between 1 and 6 years. The Shapley Additive Explanations (SHAP) approach was used to quantify the importance of input features, and the top 20 features with the highest SHAP values were selected to train the applicable models. The external validity of the established models was assessed among 50,310 individuals who participated in UK Biobank repeated assessments both overall and by the level of PRS for suicidality.
Results
Individuals with suicidal behaviors were on average 56 years old, with equal sex distribution. The application of these full models in the external validation data set demonstrated good model performance, with the area under the receiver operating characteristic (AUROC) curves of 0.919 and 0.892 within 1 year and between 1 and 6 years, respectively. Importantly, the applicable models with the top 20 most important features showed comparable external-validated performance (AUROC curves of 0.901 and 0.885) as the full models, based on which we found that individuals in the top quintile of predicted risk accounted for 91.7% (n=11) and 80.7% (n=25) of all suicidality cases within 1 year and during 1 to 6 years, respectively. We further obtained comparable prediction accuracy when applying these models to subpopulations with different genetic susceptibilities to suicidality. For example, for the 1-year risk prediction, the AUROC curves were 0.907 and 0.885 for the high (>2nd tertile of PRS) and low (<1st) genetic susceptibilities groups, respectively.
Conclusions
We established applicable machine learning–based models for predicting both the short- and long-term risk of suicidality with high accuracy across populations of varying genetic risk for suicide, highlighting a cost-effective method of identifying individuals with a high risk of suicidality.
Keywords: suicide, suicidal behaviors, risk prediction, machine learning approach, genetic susceptibility, machine learning, behavior, data, model, sex, risk, cost-effective
Introduction
According to the estimation of the Global Burden of Disease study, approximately 800,000 people die by suicide every year [1], which translates to the astonishing number of 1 person dying by suicide every 40 seconds. In the United Kingdom, there were 5691 deaths by suicide registered in England and Wales in 2019, which corresponded to an age-standardized rate of 11 deaths per 100,000 people [2]. Importantly, behind the number of suicidal deaths, there is a much higher incidence of suicide attempts requiring further research. From 2000 to 2010, a prospective study using data from 5 emergency departments in the United Kingdom identified 38,415 individuals who presented at an emergency department following a suicide attempt [3], among which only 261 (0.7%) died. This finding implies that the population targeted for suicide prevention, such as timely psychological support, is considerably larger. However, only 28% of people who attempt suicide in the United Kingdom have previously received psychiatric services [4]. Therefore, it is urgent to improve the identification of individuals at high risk for suicidality to improve suicide prevention.
The previous research suggests that the mechanisms of suicidality are complex and multifactorial [5], likely involving interactions between genetic, psychological (including traumatic experiences), and socioeconomic or other environmental factors [6,7]. This report might explain the suboptimal accuracy of suicidality prediction based on traditional statistical models, for example, with the area under the receiver operating characteristic (AUROC) curve reported to be 0.58 in a meta-analysis of 367 studies, which was only slightly better than a prediction of chance [8].
Alternatively, as tools that can deal with multidimensional data, artificial intelligence techniques (including machine learning) that have been widely used to uncover predictions of multiple diseases [9-11] might have the potential to improve the prediction of suicidality. Indeed, based on data from electronic medical records and mental health questionnaires, as well as sociodemographic factors, researchers have constructed machine learning models that obtained good performance (AUROC=0.590-0.930) for suicidality prediction in the high-risk population [12]. Likewise, more recent efforts to predict suicide attempts or deaths in the general population using this approach have yielded promising results, showing AUROC curves of 0.80 and 0.88 among men and women, respectively, in a Danish population and an AUROC curve of 0.857 among participants in the National Alcohol Epidemiological Survey in the United States [13,14]. However, prior studies did not consider several important factors, such as genetic background [7] and lifestyle factors (eg, diet, physical activity, and sleep) [15,16]. In addition, all these existing models require many input variables (2554 and 2978 inputted features for the Danish and US study, respectively), which have limited implications for daily practice.
Taking advantage of enriched information about suicidality and environmental factors, as well as the available individual-level genotyping data in UK Biobank, we aimed to construct applicable models using a machine learning approach (ie, with limited features) to predict suicidal behavior over both the short and long term. To test the robustness of our models, we validate them among individuals with different genetic risks of suicide.
Methods
Data Source
A prospective UK Biobank cohort recruited 502,507 participants aged 40 to 69 years across the United Kingdom between 2006 and 2010 [17], which coincides with a high-risk age group of suicide among men and women [18]. At recruitment, all participants filled out questionnaires covering information on sociodemographic, lifestyle, and health–related factors, with a physical examination and collection of biological samples performed during the initial assessment. After recruitment, a proportion was invited several years later to repeat the assessment. In that study, 20,334 participants received a first repeated assessment in 2012 and 2013 and 51,131 received a second repeated assessment visit in 2014.
To track health-related outcomes, UK Biobank data have been linked periodically to multiple national registries with the participants’ consent [17]. The inpatient hospital data were obtained through linked hospital records in England, Scotland, and Wales, which were mapped from the Hospital Episode Statistics in England, the Scottish Morbidity Record, and the Patient Episode Database in Wales [19]. Primary care data were obtained from multiple data suppliers, including the Phoenix Partnership and Egton Medical Information Systems, which cover approximately 45% of UK Biobank participants [20]. The mortality data were obtained from national death registers, such as the National Health Services (NHS) Digital Registry and the NHS Central Registry [21].
In this study, among the 502,507 UK Biobank participants, we excluded 48 individuals who had withdrawn from the UK Biobank. To ensure the measurement of genetic susceptibility for suicidality, 376,878 individuals with White ancestry and eligible genotyping data were included in the analysis (Figure 1A). Specifically, the polygenic risk score (PRS) was used as an index of genetic susceptibility, which was generated based on the genome-wide association study (GWAS) summary statistics (ie, effect sizes and standard errors for the variants) from an independent sample of 50,264 Danish residents involving 6,024 cases with an incidence of suicide attempt and 44,240 controls [22]. In addition to removing individuals with nonhomogenous European ancestry, this GWAS study applied principal components of genetic ancestry to take into account the effect of population stratification. We computed the PRS using LDPred2, a method of PRS calculation based on a matrix of correlations between genetic variants, which is faster, more accurate, and more robust than the LDPred14 [23]. In a validation step, the calculated PRS showed a high consistency with the studied phenotype (ie, suicidal behaviors) in our study population, yielding a mean area under the curve of 0.550 and an odds ratio of 2.34 (95% CI 1.66-3.29) by a unit increase in the PRS. During the analysis, we defined the genetic risk levels of suicidality as low (<1st tertile of the PRS), moderate (1st-2nd tertile), and high (>2nd tertile).
Figure 1.
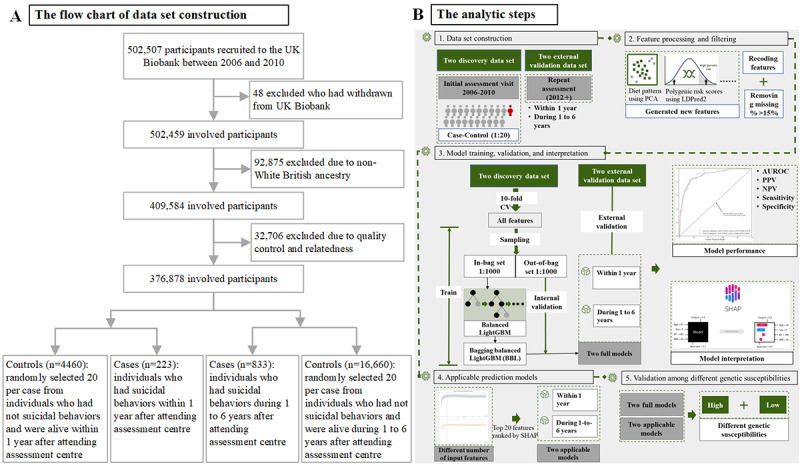
Flowchart of the study. AUROC: area under the receiver operator curve; CV: corss validation; LightGBM: light gradient-boosting machine; NPV: negative predictive value; PCA: principal component analysis; PPV: positive predictive value.
Ethics Approval
UK Biobank has full ethical approval from the NHS National Research Ethics Service (16/NW/0274), and informed consent was obtained before data collection from each participant. This study was also approved by the biomedical research ethics committee of West China Hospital (2019-1171).
Ascertainment of Suicidal Behaviors
To expand the application of our models to suicide prevention, both suicide attempts and deaths identified during the study period were considered suicidal behaviors of interest, which is consistent with previous studies [24,25]. Specifically, death by suicide was defined as death with suicide as the underlying cause of death and documented by its correspondence to the International Classification of Diseases 9th revision (ICD-9) and 10th revision (ICD-10) codes (ie, ICD-10: X60-84 and Y10-34; ICD-9: E950-958) [24,25] in the death register. Suicide attempts were considered as hospital admissions with a diagnosis of intentional self-harm (ICD 10: X60-84 and ICD-9: E950-958) or self-harm of undetermined intent (ICD-10: Y10-34) [24,25]. With relatively stable age- and sex-standardized incidence rates, the absolute number of suicide attempts and deaths was high within the first year of enrollment and dropped gradually to half that number in 6th year (Figure S1 of Multimedia Appendix 1 [26-28]). Thus, the outcomes of interest were suicidal behaviors occurring within 1 year (ie, short term) and 1 to 6 years (ie, long term) after the recruitment. We considered individuals with suicide attempts before the recruitment as those having a history of suicide attempts.
Data Set Construction
We constructed separate data sets for predicting suicidal behaviors within 1 year and 1 to 6 years. For the short-term risk prediction, we identified cases of suicide attempts or deaths at least 1 time within 1 year after recruitment (n=223). Controls (n=4460) were randomly selected (1:20 allocation ratio) from the remaining participants who were eligible, alive, and free of suicidal behaviors 1 year after the recruitment, resulting in a data set consisting of 4683 participants (Figure 1A). The same strategies were applied to constructing data sets for long-term (ie, 1 to 6 years) suicide risk prediction, yielding a full data set of 17,493 participants, with 833 (4.8%) and 16,660 (95.2%) cases and controls, respectively.
The 2 aforementioned data sets were then used as discovery data sets for model training and the assessment of internal validity. We additionally used a subsample comprising 50,310 participants of White ancestry from UK Biobank who participated in the repeat assessments. Among this subsample, there were 12 (0.02%) and 31 (0.06%) individuals who attempted or died by suicide within 1 year or during 1 to 6 years after their repeat measurements, respectively, as the validation data set for assessing external validity.
Feature Processing and Filtering
Taking full advantage of the diversity of variables in UK Biobank, we generated a feature list involving multidimensional factors. Due to difficulties obtaining individual genetic data in the real world, we did not involve the PRS in the construction of the prediction models, but we subsequently validated the suicide prediction models with the subgroups of varying (ie, high and low) genetic susceptibility to suicidality to demonstrate their robustness. Information regarding sociodemographic, environmental, and psychosocial factors was derived from the data collected at recruitment using the touchscreen or face-to-face interview questionnaires. For categorical variables (eg, “In general, how would you rate your overall health?”), UK Biobank assigns negative values to categories denoting missingness (ie, −1 refers to “Prefer not to answer,” and −3 refers to “Do not know”). Therefore, we recorded those negative values as “NA.” Specifically, instead of directly using variables collected through a generic diet questionnaire, we identified dietary patterns based on the results of principal component analysis with varimax rotation (Figure S2 of Multimedia Appendix 1). They were referred to as the prudent, western, and open-sandwich patterns [26], yielding variables with top factor loadings in each component (Table S1 in Multimedia Appendix 1). Medical data included the physical examinations (eg, pulse rate, blood pressure, and grip strength of both hands) conducted during the initial medical center visit, and we calculated mean values when multiple records existed. Additionally, a history of psychiatric disorders was defined as any previous diagnosis of psychiatric disorders before baseline (ICD-10: any F), which was identified through self-reported, hospital inpatient, and primary care data. To consider the influence of somatic fitness, we generated time-varying (0 to 1 and 1 to 4 years before the recruitment) dichotomous variables for each subtype of severe somatic diseases [29]. For the analyses of the total study population, the level of genetic susceptibility to suicidality (low, moderate, or high) was also considered a candidate feature.
After excluding variables with over 15% of missing or irrelevant data (eg, device ID, seated boxing height, and hair color), we included a total of 143 features. The coding book of the included features is shown in Table S2 of Multimedia Appendix 1.
Model Training and Validation
We constructed prediction models using all eligible features. The balanced bagging algorithm is proven to have good performance for classification models with class-imbalanced data [14]. Moreover, the light gradient-boosting machine (LightGBM) [30], as a gradient-boosting algorithm, has been widely applied in machine learning research due to its fast computational speed, high accuracy, and ability to handle missing values [11]. Therefore, considering the data imbalance and the existence of missing values, we used the balanced bagging LightGBM approach to achieve high classification accuracy and fast computation speed, which bagged 1000 balanced LightGBM classifiers (ie, using “class_weight” =“balanced”) after random downsampling [31]. We tuned the parameters by using stratified 10-fold cross-validation and grid-search, with the best combination of hyperparameters shown in the Methods section of Multimedia Appendix 1. Each of the 1000 balanced LightGBM classifiers randomly selected subsamples from the group of the minority class (ie, those who had suicidal behavior) and matched samples with the same size from the group of the majority class (ie, those who had no suicidal behavior) to construct case-control samples (ie, the in-bag set). The randomly selected case-control samples were applied to train balanced LightGBM classifiers, and the remaining sample, referred to as the out-of-bag (OOB) set, was used to estimate the prediction of the suicide risk score of the OOB set.
We defined the OOB set as the internal validation set. Specifically, we aggregated the predicted suicide risk scores of the OOB set from the 1000 balanced LightGBM classifiers to estimate the internal validated predicted error [32], and we regarded the models with the highest OOB AUROCs as optimal. Then, we computed the predicted suicide risk scores of the externally validated data sets from the repeated assessments for the optimal model. Due to the lack of agreement regarding which of the risk thresholds of classification provides the most sufficient clinical utility, we computed the AUROC [13,24], sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) at different suicide risk score thresholds.
Model Explanation
Interpretations of the models were measured using the Shapley Additive Explanations (SHAP) approach, which quantifies the relationship of the input features with the outcome [33]. Specifically, we computed the contribution of all the features to the studied suicidal behaviors for each participant and assigned each feature an importance score (ie, a SHAP value) after considering its interactions with the remaining features. The absolute values of the average SHAP values were presented as a bar plot illustrating the relative importance of these input features for the models’ predictions at the population level.
Applicable Prediction Models
To facilitate the application of the prediction models, we conducted feature reduction by illustrating the changes in the prediction accuracy of the models with different numbers of input features (ie, those with top 10, 20, 50, and 100 SHAP values) [34,35]. As shown in Figure S3 of Multimedia Appendix 1, the models for predicting suicidal behaviors within 1 year and from 1 to 6 years both achieved overall good performance when the input feature dimension with the highest SHAP value was increased to 20, so we considered the models with 20 input features as the applicable prediction models which might facilitate the future implication.
Model Validation Among Individuals With Different Genetic Susceptibilities
To illustrate the robustness of the suicide prediction models, we validated both full and applicable models in the whole population as well as subgroups of varying (ie, high and low) genetic susceptibility to suicidality by computing the OOB performance of these models.
We performed the data set construction and calculation of the PRS using R software version 3.6.1 (Lucent Technologies Co). The machine learning model development was achieved using Python software version 3.6 (Software Foundation), imbalanced-learn 0.9.0, and lightgbm version 3.2.1. We conducted the model interpretation analysis using SHAP version 0.38.1. We then analyzed the models’ performance and plot creation using scikit-learn version 1.0.2 and matplotlib version 3.3.2, respectively.
Results
Study Population Characteristics
The data sets for the prediction of suicidal behavior prediction within 1 year and for 1 to 6 years showed largely comparable characteristics at baseline (Table 1). We obtained similar ages, with mean ages of 56.75 (SD 8.03) and 56.65 (SD 7.99) years, respectively, and female-to-male sex distributions of 1:1.13 and 1:1.20, respectively. However, the characteristics of the validation sample for external validity (ie, individuals involved in the repeat assessments) were different from the discovery sample (ie, individuals recruited in the initial assessment visit), characterized by older age, more likely to have a history of psychiatric disorders, and lived in their own accommodation at time of data collection (Table 1).
Table 1.
Basic characteristics of analytic samples for the construction of prediction models for 1 year and 1 to 6 years.
| Characteristics | Discovery | External validation (n=50,310) | |||||
|
|
Within 1 year (n=4683) | 1 to 6 years (n=17,493) |
|
||||
| Age (years), mean (SD) | 56.75 (8.03) | 56.65 (7.99) | 63.24 (7.49) | ||||
| Gender, n (%) | |||||||
|
|
Female | 2480 (53) | 9537 (54.5) | 25,675 (51) | |||
|
|
Male | 2203 (47) | 7956 (45.5) | 24,635 (49) | |||
| History of psychiatric disorders, n (%) | |||||||
|
|
No | 3760 (80.3) | 14,371 (82.2) | 39,226 (78) | |||
|
|
Yes | 923 (19.7) | 3122 (17.8) | 11,084 (22) | |||
| History of suicide attempt n (%) | |||||||
|
|
No | 4574 (97.7) | 17,270 (98.7) | 50,108 (99.6) | |||
|
|
Yes | 109 (2.3) | 223 (1.3) | 202 (0.4) | |||
| Have you ever seen a psychiatrist for nerves, anxiety, tension, or depression? n (%) | |||||||
|
|
No | 3999 (85.4) | 15,188 (86.8) | 45,372 (90.2) | |||
|
|
Yes | 660 (14.1) | 2248 (12.9) | 4556 (9.1) | |||
|
|
Missing | 24 (0.5) | 57 (0.3) | 382 (0.8) | |||
| Have you ever seen a general practitioner for nerves, anxiety, tension, or depression? n (%) | |||||||
|
|
No | 2882 (61.5) | 11,181 (63.9) | 34,168 (67.9) | |||
|
|
Yes | 1768 (37.8) | 6215 (35.5) | 15,685 (31.2) | |||
|
|
Missing | 33 (0.7) | 97 (0.6) | 457 (0.9) | |||
| In the past, how often have you smoked tobacco? n (%) | |||||||
|
|
Smoked on most or all days | 1212 (25.9) | 4237 (24.2) | 11,900 (23.7) | |||
|
|
Smoked occasionally | 573 (12.2) | 2231 (12.8) | 6061 (12) | |||
|
|
Just tried once or twice | 685 (14.6) | 2634 (15.1) | 7983 (15.9) | |||
|
|
I have never smoked | 1806 (38.6) | 6897 (39.4) | 22,789 (45.3) | |||
|
|
Missing | 407 (8.7) | 1494 (8.5) | 1577 (3.1) | |||
| Do you live in your own accommodation? n (%) | |||||||
|
|
No | 2194 (46.9) | 8136 (46.5) | 11,670 (23.2) | |||
|
|
Yes | 2414 (51.5) | 9155 (52.3) | 38,114 (75.8) | |||
|
|
Missing | 75 (1.6) | 202 (1.2) | 526 (1) | |||
| Average annual total household income before taxa, n (%) | |||||||
|
|
Less than £18,000 (US $16,676) | 945 (20.2) | 3410 (19.5) | 6502 (12.9) | |||
|
|
£18,000 to £30,999 (US $16,676 to $28,718) | 1045 (22.3) | 3802 (21.7) | 13,250 (26.3) | |||
|
|
£31,000 to £51,999 (US $28,719 to $48,173) | 1073 (22.9) | 3958 (22.6) | 13,577 (27) | |||
|
|
£52,000 to £100,000 (US $48,174 to $92,642) | 816 (17.4) | 3113 (17.8) | 9529 (18.9) | |||
|
|
Greater than £100,000 (US $92,642) | 194 (4.1) | 797 (4.6) | 2614 (5.2) | |||
|
|
Missing | 610 (13) | 2413 (13.8) | 4838 (9.6) | |||
| Cases, n (%) | 223 (47.62) | 833 (47.62) | 12 (0.02)b and 31 (0.06)c | ||||
aNote that income data were collected between 2008 and 2010. Income was converted to US dollars according to the current exchange range.
bRefers to the number of cases of suicidal behaviors within 1 year.
cRefers to the number of cases of suicidal behaviors for 1 to 6 years.
Prediction Models Involving All Features
The internal validated AUROC of the prediction models involving all features was 0.888 (95% CI 0.863-0.914) for the prediction of suicidal behaviors within 1 year and 0.852 (95% CI 0.838-0.867) for 1 to 6 years (Figure 2). Figure 2 shows values of sensitivity, specificity, and predictive indices over a series of risk thresholds. For instance, at the 0.70 risk threshold, the short- and long-term sensitivities were, respectively, 57.85% and 54.74%, the specificities were 95.11% and 94.05%, the PPVs were 37.18% and 31.49%, and the NPVs were 97.83% and 97.65%. Furthermore, the externally validated AUROC curves were 0.919 (95% CI 0.852-0.985) for the model predicting suicidal behaviors within 1 year and 0.892 (95% CI 0.844-0.940) for the model predicting suicidal behaviors between 1 and 6 years, indicating the robustness of the prediction models.
Figure 2.
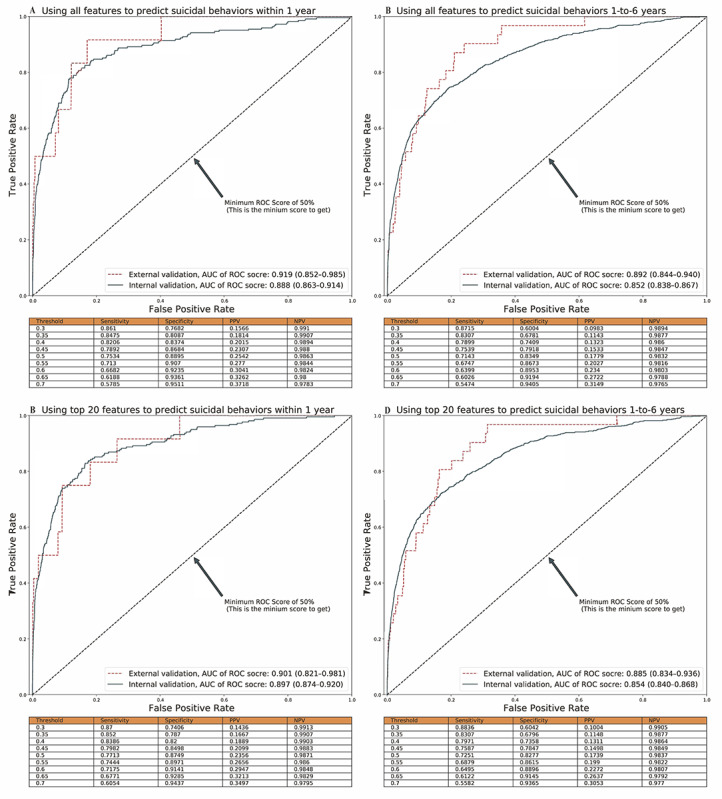
The performance of prediction models using all input features and top 20 features. The area under the receiver operating characteristic (AUROC) curve. The tables showed the internal validation performance (ie, sensitivity, specificity, positive predictive value [PPV], and negative predictive value [NPV]) of suicide prediction models at different classified thresholds.
Regarding the importance of features measured using SHAP values, similar to age, family income, and body fat percentage, mental health–related factors (eg, history of psychiatric disorders, history of suicide attempt, etc) were top ranked in both models within 1 year (7 among the top 20 features) and during 1 to 6 years (8 among the top 20 features). However, notable differences were observed with respect to some lifestyle and social factors (eg, “How many years of using a mobile phone at least once per week to make or receive calls?” and “Age you first had sexual intercourse”), as these seemed to have greater importance for only the prediction models within 1 year but not 1 to 6 years (Figure 3). In contrast, some general health–related factors (ie, “In general how would you rate your overall health?” and “Compared with 1 year ago, has your weight changed?”) seemed only important for the 1-to-6 years prediction model. Detailed information on the included features is shown in Table S2 of Multimedia Appendix 1.
Figure 3.
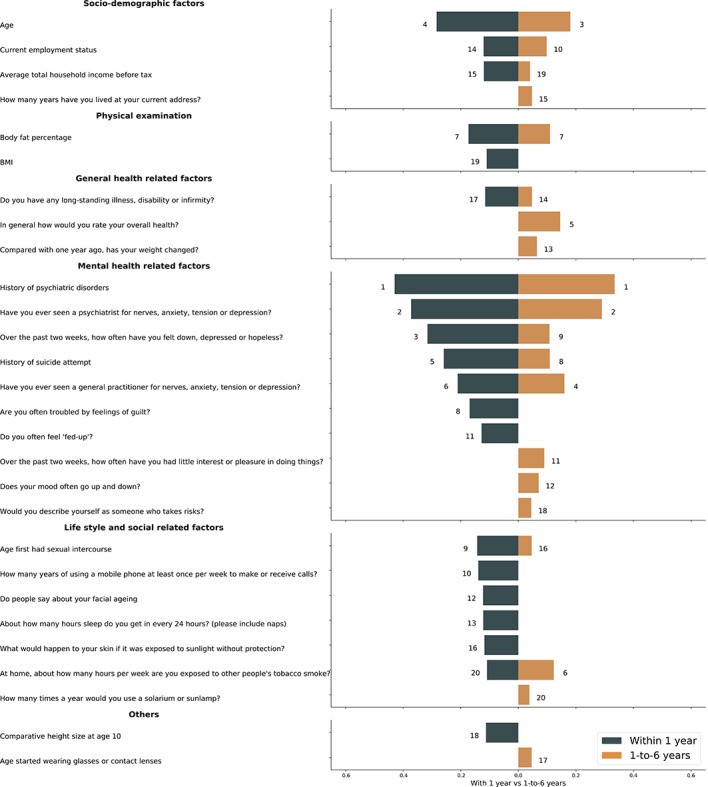
The comparison of top 20 features identified in suicide risk prediction full models for within 1 year and 1-to-6 years. The dark blue and yellow bar represent the relatively importance of these input features for the prediction, respectively. And the numbers next to the bars are corresponding to the ranking of top 20 features. The detailed information of the included features is shown in Table S2 in Multimedia Appendix 1.
Prediction Models Involving the Top 20 Features
Figure S3 of Multimedia Appendix 1 displays the indices of model performance for the models involving different numbers of the top features (ie, top 20, 40, 60, and 100). Accordingly, the 2 models with the top 20 input features were considered optimal (Figure 2). The AUROC curves for their internal and external validations for the within 1-year suicide prediction were 0.897 (95% CI 0.874-0.920) and 0.901 (95% CI 0.821-0.981), respectively. For the 1-to-6 years prediction, the corresponding estimate was 0.854 (95% CI 0.840-0.868) and 0.885 (95% CI 0.834-0.936), respectively. Based on the applicable models, we found individuals in the top quintile of predicted risk accounting for 91.7% (n=11) and 80.7% (n=25) of all cases of suicide attempts or deaths within 1 year and during 1 to 6 years, respectively.
Models for Individuals With Different Genetic Susceptibilities
Using both full and simplified prediction models, we obtained a comparable prediction accuracy for individuals with low and high genetic susceptibilities to suicidality (Figures S4 and S5 of Multimedia Appendix 1). For instance, for short-term risk prediction, the AUROC curves for models with the top 20 involved features were 0.907 and 0.885 for the high and low genetic susceptibility groups, respectively. The corresponding numbers for the long-term risk prediction were 0.869 and 0.822, respectively.
Discussion
Principal Findings
In this study on a community-based UK Biobank cohort of over 0.5 million UK residents aged 40 to 69 years (covering the age group with a high risk of suicide [18]), we established machine learning–based models to accurately predict both short- and long-term risks of suicide attempts and deaths (AUROC=0.892-0.919). Importantly, our applicable models achieved high predictive accuracy across populations with varying genetic susceptibility to suicide with a limited number (ie, 20) of phenotypic features that could be accessed easily through practice. Specifically, we found that individuals with the top 20% of predicted risks comprised over 80% of real cases of suicide attempts or deaths, suggesting that our approach may be a cost-effective way to identify high-risk middle-aged individuals who should be targeted for suicide prevention. In addition, besides some well-known suicide risk factors (ie, mental health–related conditions), these established models provide novel insights into factors driving suicidal behaviors, revealing that some lifestyle and social factors (eg, cell phone use frequency, etc) may be risk factors for suicidal behaviors in the short-term, while self-reported general health ratings are more important for the prediction of long-term suicidal risk.
In line with 2 previous studies focusing on machine learning–based suicide risk prediction in the general population using data from Danish health registers [13] and the National Alcohol Epidemiological Survey of the United States [14], our results identified mental health–related factors (ie, prior suicide attempt, history of psychiatric disorders, and past emotion) and sociodemographic factors (ie, age and family income) as top features for suicide risk prediction. However, benefiting from the enriched data in UK Biobank, particularly items related to neuroticism, lifestyle, social contacts, and self-rated general health, our prediction models achieved improved performance. In addition, the comparison of features that matter for short- versus longer-term suicide risk was not addressed in prior investigations. Similar efforts have been made in some specific populations (eg, patients receiving psychiatric [24] or other medical care [36] and soldiers [37]), though with only comparable predictive accuracy (ie, the AUROC curves ranged between 0.77 and 0.93) with more homogeneous clinical populations.
Consistent with our findings, neuroticism was reported as a risk factor for suicidal behaviors in a previous study, with plausible mechanisms of shared genetic components [38]. Likewise, severe somatic diseases, disabilities, or physical weakness have consistently been reported to be associated with higher suicide risk, which is possibly due to the chronic stress associated with these diagnoses and living with these diseases [7]. Previous efforts exploring the association between BMI and suicidality have led to inconsistent results [39], and the association between body fat and suicidality has remained largely unexplored. Nevertheless, our findings of the association between body fat percentage and suicidality gain support from a Mendelian randomization analysis, which revealed a causal link between a high percentage of body fat and depression [40].
Our attempts to construct separate models for the prediction of both short- and long-term suicide risks indicated that the models generally achieved better prediction accuracy for the more immediate period before the suicide attempt or death, which is in line with the findings of prior studies concerning time-varying suicide risk assessments [24,41]. While factors directly reflecting mental health impairment show consistent importance for both short- and long-term suicidal risk prediction, the significance of lifestyle and social factors (eg, the frequency of using a cell phone to make or receive calls) was mainly observed for short-term risk (ie, within 1 year), indicating the role of lower social support and social relations among individuals with suicide risk [7]. Additionally, our findings on the association between self-reported health ratings and long-term suicide risk are in line with the results of the Danish study, which also found that medical diagnoses and medications related to some somatic illnesses (eg, infection and respiratory diseases) measured 48 months before suicide were more important indicators of suicide risk than those measured 6 months earlier [13].
Strengths and Weaknesses
The major merits of our study include the use of multidimensional data (including individual-level genotyping data) from a large community-based cohort of UK Biobank. The application of the machine learning approach, together with the use of SHAP values for feature interpretation, enabled us to identify the most informative variables that maximized the efficiency of the data for an accurate prediction of suicide risk. The imbalance in the sample sizes of the cases and the controls was mitigated by randomly downsampling and setting class weights for imbalanced classes in LightGBM during the training step [30,42]. Further, we improved the feasibility of our prediction models by using the feature reduction process, where accurate classification was achieved with only 20 features. Although no similar data from independent samples could be used for external validation, the validity of our models was demonstrated in a subgroup of UK Biobank participants who repeated surveys many years after the baseline measurement (showing different basic characteristics compared to the discovery data set), as well as the subpopulations stratified by their level of genetic susceptibility to suicidality.
A notable limitation of this study is the absence of data from emergency care departments, which were the main source for suicide case identification in previous studies [13,43]. Therefore, our study focused on suicidal behaviors resulting in hospitalization or death, and those with less severe consequences require further investigation. In addition, it is difficult to distinguish suicide attempts from nonsuicidal intentional self-harm based on ICD codes, as clinical diagnoses tended to be consequence oriented (ie, leading to life-threatening harm or not) or dependent on self-reported reasoning on intent. Moreover, such outcome ascertainment strategies have been demonstrated to suffer from poor sensitivity, resulting in a risk of underestimation of suicidal cases, as well as attenuated associations between studied exposures and suicidal outcomes [44]. Nevertheless, as this is the most feasible method to identify suicidal behavior, similar definitions and ascertainment of suicidal behaviors have been widely used in other large community- or population-based studies with a similar focus [24,25]. Furthermore, we only used the LightGBM as the base estimator for bagging, mainly due to its capability to handle missing values and achieve high discrimination accuracy [30]. It is possible that other machine learning approaches (eg, deep neural network), with some common methods of feature engineering (eg, standardization, one-hot encoding), might obtain better performance at the price of model interpretability. Finally, the UK Biobank study recruited only 5.5% of the invited individuals in the age range of 40 to 69 years, leading to a selection bias of the study population compared to the entirety of the population in the United Kingdom [45]. Consequently, the generalization of our findings to the total UK population and other populations cannot be made.
Conclusions
In conclusion, based on a UK Biobank cohort, we established clinically applicable machine learning–based models for accurately predicting both short- and long-term risks of suicidal behaviors. The good performance of the models for subgroups with different genetic susceptibilities to suicidality highlights the possibility of applying these models to high-risk individual identification in the general middle-aged population, which may facilitate the development of cost-effective suicide prevention.
Acknowledgments
This research was conducted using UK Biobank (application 54803). This work uses data provided by patients and collected by the National Health Services (NHS) as part of their care and support. This research used data assets made available by National Safe Haven as part of the Data and Connectivity National Core Study, led by Health Data Research UK in partnership with the Office for National Statistics and funded by UK Research and Innovation. We thank the team members of the West China Biomedical Big Data Center for Disease Control and Prevention for their support.
This work was supported by the 1.3.5 Project for Disciplines of Excellence of the West China Hospital at Sichuan University (ZYYC21005) and by the National Natural Science Foundation of China (81971262) to author HS.
Abbreviations
- AUROC
area under the receiver operating characteristic
- GWAS
genome-wide association study
- ICD-9/ICD-10
International Classification of Diseases 9th revision/10th revision
- LightGBM
light gradient-boosting machine
- NHS
National Health Services
- NPV
negative predictive value
- OOB
out of bag
- PPV
positive predictive value
- PRS
polygenic risk score
- SHAP
Shapley Additive Explanations
Supplementary methods, tables, and figures.
Data Availability
Data from the UK Biobank are available to all researchers upon submitted application. All codes associated with the current submission are available and can be requested by contacting the corresponding authors.
Footnotes
Authors' Contributions: HS and JW were responsible for the study’s concept and design. JW, HY, and YQ were responsible for data and project management. JW, YZ, and HY performed the data cleaning and analysis. JW, JQ, TZ, UAV, and HS interpreted the data. JW, JQ, TZ, YZ, HY, YS, JY, UAV, and HS drafted and revised the manuscript. All the authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Conflicts of Interest: None declared.
References
- 1.Roth GA. Global, regional, and national age–sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 Jan;385(9963):117–171. doi: 10.1016/s0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suicides in England and Wales. Office for National Statistics. [2022-06-01]. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/suicidesintheunitedkingdomreferencetables .
- 3.Kapur N, Steeg S, Turnbull P, Webb R, Bergen H, Hawton K, Geulayov G, Townsend E, Ness J, Waters K, Cooper J. Hospital management of suicidal behaviour and subsequent mortality: a prospective cohort study. Lancet Psychiatry. 2015 Sep;2(9):809–816. doi: 10.1016/s2215-0366(15)00169-8. [DOI] [PubMed] [Google Scholar]
- 4.Houston K, Haw C, Townsend E, Hawton K. General practitioner contacts with patients before and after deliberate self harm. Br J Gen Pract. 2003 May;53(490):365–70. https://bjgp.org/lookup/pmidlookup?view=long&pmid=12830563 . [PMC free article] [PubMed] [Google Scholar]
- 5.Turecki G. The molecular bases of the suicidal brain. Nat Rev Neurosci. 2014 Dec;15(12):802–16. doi: 10.1038/nrn3839. https://europepmc.org/abstract/MED/25354482 .nrn3839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, de Girolamo G, Gluzman S, de Graaf R, Gureje O, Haro JM, Huang Y, Karam E, Kessler RC, Lepine JP, Levinson D, Medina-Mora ME, Ono Y, Posada-Villa J, Williams D. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008 Mar 02;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. https://europepmc.org/abstract/MED/18245022 .S0007125000233886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turecki G, Brent DA, Gunnell D, O'Connor RC, Oquendo MA, Pirkis J, Stanley BH. Suicide and suicide risk. Nat Rev Dis Primers. 2019 Oct 24;5(1):74. doi: 10.1038/s41572-019-0121-0.10.1038/s41572-019-0121-0 [DOI] [PubMed] [Google Scholar]
- 8.Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 2017 Mar;143(2):187–232. doi: 10.1037/bul0000084.2016-54856-001 [DOI] [PubMed] [Google Scholar]
- 9.Qiu J, Yin J, Qian W, Liu J, Huang Z, Yu H, Ji L, Zeng X. A novel multiresolution-statistical texture analysis architecture: radiomics-aided diagnosis of PDAC based on plain CT images. IEEE Trans Med Imaging. 2021 Jan;40(1):12–25. doi: 10.1109/tmi.2020.3021254. [DOI] [PubMed] [Google Scholar]
- 10.Mi X, Zou B, Zou F, Hu J. Permutation-based identification of important biomarkers for complex diseases via machine learning models. Nat Commun. 2021 May 21;12(1) doi: 10.1038/s41467-021-22756-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Artzi NS, Shilo S, Hadar E, Rossman H, Barbash-Hazan S, Ben-Haroush A, Balicer RD, Feldman B, Wiznitzer A, Segal E. Prediction of gestational diabetes based on nationwide electronic health records. Nat Med. 2020 Jan 13;26(1):71–76. doi: 10.1038/s41591-019-0724-8.10.1038/s41591-019-0724-8 [DOI] [PubMed] [Google Scholar]
- 12.Belsher BE, Smolenski DJ, Pruitt LD, Bush NE, Beech EH, Workman DE, Morgan RL, Evatt DP, Tucker J, Skopp NA. Prediction models for suicide attempts and deaths: a systematic review and simulation. JAMA Psychiatry. 2019 Jun 01;76(6):642–651. doi: 10.1001/jamapsychiatry.2019.0174.2727387 [DOI] [PubMed] [Google Scholar]
- 13.Gradus JL, Rosellini AJ, Horváth-Puhó E, Street AE, Galatzer-Levy I, Jiang T, Lash TL, Sørensen HT. Prediction of sex-specific suicide risk using machine learning and single-payer health care registry data from Denmark. JAMA Psychiatry. 2020 Jan 01;77(1):25–34. doi: 10.1001/jamapsychiatry.2019.2905. https://europepmc.org/abstract/MED/31642880 .2753014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.García de la Garza Á, Blanco C, Olfson M, Wall MM. Identification of suicide attempt risk factors in a national US survey using machine learning. JAMA Psychiatry. 2021 Apr 01;78(4):398–406. doi: 10.1001/jamapsychiatry.2020.4165. https://europepmc.org/abstract/MED/33404590 .2774348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berardelli I, Corigliano V, Hawkins M, Comparelli A, Erbuto D, Pompili M. Lifestyle interventions and prevention of suicide. Front Psychiatry. 2018 Nov 6;9:567. doi: 10.3389/fpsyt.2018.00567. https://europepmc.org/abstract/MED/30459660 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bernert RA, Turvey CL, Conwell Y, Joiner TE. Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: a longitudinal, population-based study of late life. JAMA Psychiatry. 2014 Oct 01;71(10):1129–37. doi: 10.1001/jamapsychiatry.2014.1126. https://europepmc.org/abstract/MED/25133759 .1895670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, Motyer A, Vukcevic D, Delaneau O, O'Connell J, Cortes A, Welsh S, Young A, Effingham M, McVean G, Leslie S, Allen N, Donnelly P, Marchini J. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018 Oct 10;562(7726):203–209. doi: 10.1038/s41586-018-0579-z. https://europepmc.org/abstract/MED/30305743 .10.1038/s41586-018-0579-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iacobucci G. Suicide rates continue to rise in England and Wales. BMJ. 2020 Sep 03;370:m3431. doi: 10.1136/bmj.m3431. [DOI] [PubMed] [Google Scholar]
- 19.Mapping inpatient hospital data across England, Scotland and Wales. UK Biobank. [2020-10-01]. http://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/inpatient_mapping.pdf .
- 20.Data providers and dates of data availability. UK Biobank. [2021-03-01]. https://biobank.ndph.ox.ac.uk/showcase/exinfo.cgi?src=Data_providers_and_dates .
- 21.Mortality data: linkage to death registries. UK Biobank. [2020-10-01]. https://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/DeathLinkage.pdf .
- 22.Erlangsen A, Appadurai V, Wang Y, Turecki G, Mors O, Werge T, Mortensen PB, Starnawska A, Børglum AD, Schork A, Nudel R, Bækvad-Hansen M, Bybjerg-Grauholm J, Hougaard DM, Thompson WK, Nordentoft M, Agerbo E. Genetics of suicide attempts in individuals with and without mental disorders: a population-based genome-wide association study. Mol Psychiatry. 2020 Oct 16;25(10):2410–2421. doi: 10.1038/s41380-018-0218-y. https://europepmc.org/abstract/MED/30116032 .10.1038/s41380-018-0218-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Privé F, Arbel J, Vilhjálmsson BJ. LDpred2: better, faster, stronger. Bioinformatics. 2020 Dec 16;36(22-23):5424–31. doi: 10.1093/bioinformatics/btaa1029. https://europepmc.org/abstract/MED/33326037 .6039173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Q, Zhang-James Y, Barnett EJ, Lichtenstein P, Jokinen J, D'Onofrio BM, Faraone SV, Larsson H, Fazel S. Predicting suicide attempt or suicide death following a visit to psychiatric specialty care: A machine learning study using Swedish national registry data. PLoS Med. 2020 Nov 6;17(11):e1003416. doi: 10.1371/journal.pmed.1003416. https://dx.plos.org/10.1371/journal.pmed.1003416 .PMEDICINE-D-20-00084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simon GE, Johnson E, Lawrence JM, Rossom RC, Ahmedani B, Lynch FL, Beck A, Waitzfelder B, Ziebell R, Penfold RB, Shortreed SM. Predicting suicide attempts and suicide deaths following outpatient visits using electronic health records. Am J Psychiatry. 2018 Oct 01;175(10):951–960. doi: 10.1176/appi.ajp.2018.17101167. https://europepmc.org/abstract/MED/29792051 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei X, Zhu C, Ji M, Fan J, Xie J, Huang Y, Jiang X, Xu J, Yin R, Du L, Wang Y, Dai J, Jin G, Xu L, Hu Z, Shen H, Zhu M, Ma H. Diet and risk of incident lung cancer: a large prospective cohort study in UK Biobank. Am J Clin Nutr. 2021 Dec 01;114(6):2043–2051. doi: 10.1093/ajcn/nqab298.6377471 [DOI] [PubMed] [Google Scholar]
- 27.Tyrrell Jessica, Wood Andrew R, Ames Ryan M, Yaghootkar Hanieh, Beaumont Robin N, Jones Samuel E, Tuke Marcus A, Ruth Katherine S, Freathy Rachel M, Davey Smith George, Joost Stéphane, Guessous Idris, Murray Anna, Strachan David P, Kutalik Zoltán, Weedon Michael N, Frayling Timothy M. Gene-obesogenic environment interactions in the UK Biobank study. Int J Epidemiol. 2017 Apr 01;46(2):559–575. doi: 10.1093/ije/dyw337. https://europepmc.org/abstract/MED/28073954 .dyw337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Niarchou Maria, Byrne Enda M, Trzaskowski Maciej, Sidorenko Julia, Kemper Kathryn E, McGrath John J, O' Donovan Michael C, Owen Michael J, Wray Naomi R. Genome-wide association study of dietary intake in the UK biobank study and its associations with schizophrenia and other traits. Transl Psychiatry. 2020 Feb 03;10(1):51–171. doi: 10.1038/s41398-020-0688-y. doi: 10.1038/s41398-020-0688-y.10.1038/s41398-020-0688-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morgan C, Webb RT, Carr MJ, Kontopantelis E, Chew-Graham CA, Kapur N, Ashcroft DM. Self-harm in a primary care cohort of older people: incidence, clinical management, and risk of suicide and other causes of death. Lancet Psychiatry. 2018 Nov;5(11):905–912. doi: 10.1016/s2215-0366(18)30348-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ke G, Meng Q, Finley T, Wang T, Chen W, Ma W. Lightgbm: A highly efficient gradient boosting decision tree. 31st Conference on Neural Information Processing Systems; December 8; Long Beach, CA. 2017. p. A. [Google Scholar]
- 31.Xia H, Wei X, Gao Y, Lv H. Traffic prediction based on ensemble machine learning strategies with bagging and LightGBM. 53rd IEEE International Conference on Communications Workshops (ICC Workshops); May 20-24; Shanghai, China. 2019. [DOI] [Google Scholar]
- 32.Breiman L. Out-of-bag estimation. University of California Berkeley. [2021-11-01]. https://www.stat.berkeley.edu/~breiman/OOBestimation.pdf .
- 33.Lundberg S. A unified approach to interpreting model predictions. 31st Conference on Neural Information Processing Systems; December 8; Long Beach, CA. 2017. [Google Scholar]
- 34.Bugaj M, Wrobel K, Iwaniec J. Model explainability using SHAP values for LightGBM predictions. 2021 IEEE XVIIth International Conference on the Perspective Technologies and Methods in MEMS Design (MEMSTECH); May 12-16; Polyana, Ukraine. 2021. [DOI] [Google Scholar]
- 35.Bi Y, Xiang D, Ge Z, Li F, Jia C, Song J. An interpretable prediction model for identifying N-Methylguanosine sites based on XGBoost and SHAP. Mol Ther Nucleic Acids. 2020 Dec 04;22:362–372. doi: 10.1016/j.omtn.2020.08.022. https://linkinghub.elsevier.com/retrieve/pii/S2162-2531(20)30251-1 .S2162-2531(20)30251-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barak-Corren Y, Castro VM, Javitt S, Hoffnagle AG, Dai Y, Perlis RH, Nock MK, Smoller JW, Reis BY. Predicting suicidal behavior from longitudinal electronic health records. Am J Psychiatry. 2017 Mar 01;174(2):154–162. doi: 10.1176/appi.ajp.2016.16010077. [DOI] [PubMed] [Google Scholar]
- 37.Nock MK, Millner AJ, Joiner TE, Gutierrez PM, Han G, Hwang I, King A, Naifeh JA, Sampson NA, Zaslavsky AM, Stein MB, Ursano RJ, Kessler RC. Risk factors for the transition from suicide ideation to suicide attempt: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) J Abnorm Psychol. 2018 Mar;127(2):139–149. doi: 10.1037/abn0000317. https://europepmc.org/abstract/MED/29528668 .2018-09964-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peters EM, John A, Bowen R, Baetz M, Balbuena L. Neuroticism and suicide in a general population cohort: results from the UK Biobank Project. BJPsych Open. 2018 Mar 16;4(2):62–68. doi: 10.1192/bjo.2017.12. https://europepmc.org/abstract/MED/29971148 .S2056472417000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perera S, Eisen RB, Dennis BB, Bawor M, Bhatt M, Bhatnagar N, Thabane L, de Souza R, Samaan Z. Body Mass Index is an important predictor for suicide: results from a systematic review and meta-analysis. Suicide Life Threat Behav. 2016 Dec 20;46(6):697–736. doi: 10.1111/sltb.12244. [DOI] [PubMed] [Google Scholar]
- 40.Speed MS, Jefsen OH, Børglum AD, Speed D, Østergaard SD. Investigating the association between body fat and depression via Mendelian randomization. Transl Psychiatry. 2019 Aug 05;9(1):184. doi: 10.1038/s41398-019-0516-4. doi: 10.1038/s41398-019-0516-4.10.1038/s41398-019-0516-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clin Psychol Sci. 2017 Apr 11;5(3):457–469. doi: 10.1177/2167702617691560. [DOI] [Google Scholar]
- 42.Galar M, Fernandez A, Barrenechea E, Bustince H, Herrera F. A review on ensembles for the class imbalance problem: bagging-, boosting-, and hybrid-based approaches. IEEE Trans Syst, Man, Cybern C. 2012 Jul;42(4):463–484. doi: 10.1109/tsmcc.2011.2161285. [DOI] [Google Scholar]
- 43.Sanderson M, Bulloch AG, Wang J, Williams KG, Williamson T, Patten SB. Predicting death by suicide following an emergency department visit for parasuicide with administrative health care system data and machine learning. EClinicalMedicine. 2020 Mar;20:100281. doi: 10.1016/j.eclinm.2020.100281. https://linkinghub.elsevier.com/retrieve/pii/S2589-5370(20)30025-0 .S2589-5370(20)30025-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Swain RS, Taylor LG, Braver ER, Liu W, Pinheiro SP, Mosholder AD. A systematic review of validated suicide outcome classification in observational studies. Int J Epidemiol. 2019 Oct 01;48(5):1636–1649. doi: 10.1093/ije/dyz038.5419291 [DOI] [PubMed] [Google Scholar]
- 45.Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, Collins R, Allen NE. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017 Nov 01;186(9):1026–1034. doi: 10.1093/aje/kwx246. https://europepmc.org/abstract/MED/28641372 .3883629 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary methods, tables, and figures.
Data Availability Statement
Data from the UK Biobank are available to all researchers upon submitted application. All codes associated with the current submission are available and can be requested by contacting the corresponding authors.


