Abstract
Background
Advances have been made to the traditional inlay Grammont Reverse Shoulder Arthroplasty (RSA) design such as the onlay humeral component prosthesis. Currently, there is no agreement in the literature regarding the best option for the humeral component when comparing inlay and onlay designs. This review compares the outcomes and complications between onlay versus inlay humeral components for RSA.
Methods
A literature search was conducted using PubMed and Embase. Only studies reporting outcomes comparing onlay versus inlay RSA humeral components were included.
Results
Four studies with 298 patients (306 shoulders) were included. Onlay humeral components were associated with better external rotation (ER) (p < 0.0001). No significant difference in forward flexion (FF) or abduction was found. Constant scores (CS) and VAS scores did not differ. Increased scapular notching was found in the inlay group (23.18%) versus the onlay group (7.74%) (p = 0.02). Postoperative scapular fractures and acromial fractures did not differ.
Conclusion
Onlay and inlay RSA designs are associated with improved postoperative range of motion (ROM). Onlay humeral designs may be associated with greater ER and lower rate of scapular notching; however, no difference was found in Constant and VAS scores, so further studies are required to assess the clinical significance of these differences.
Keywords: reverse shoulder arthroplasty, inlay, onlay
Introduction
Reverse shoulder arthroplasty (RSA) is an effective treatment option for shoulder pathologies such as cuff tear arthropathy, massive rotator cuff tears, proximal humeral fractures, and revisions arthroplasty requirements.1–8 Numerous technological evolutions in prosthesis designs have allowed for an expansion in indications.4,9–12 With the many new advancements in RSA, pain and functional outcomes have improved.1,3,5,9–14
Humeral prostheses have evolved into two types, the onlay and inlay designs. The inlay humeral prosthesis, which was seen in the original Grammont design, increases bony contact with the proximal component, requiring additional reaming of metaphyseal bone.1,2,5,10,12,15,16 This design has been designated as the gold standard since its development.12,15 Despite its improved outcomes compared to previous designs, it has been associated with an increased risk of scapular notching and a reduction in active external and internal rotation.1,5,7,13,17 The more recently developed onlay design establishes an increased metaphyseal bone preserving technique and facilitates ease of modularity and convertibility for future interventions.10–14 Additionally, recent studies have reported improved external rotation (ER), lower rates of glenoid radiolucency, humeral bone remodeling, and scapular notching in the onlay humeral prosthesis when compared to the traditional inlay design.1,10,12,13,17 This onlay prosthesis results in more lateral displacement of the humerus,2,9,11,12 increasing the tension of the rotator cuff and lengthens the deltoid moment arm.3,10,16,17 However, current discussions over the implant design have included concerns over the possibility of these biomechanical properties leading to increase bony compromise to the scapula.1,2,9,11,12,17
The purpose of this systematic review and meta-analysis is to compare the range of motion (ROM), functional outcomes, and complication rates between onlay and inlay humeral prosthesis designs using currently available comparative literature. We hypothesize that the onlay design is associated with better clinical and functional outcomes with fewer complications than inlay design.
Materials and methods
Search strategy and data extraction
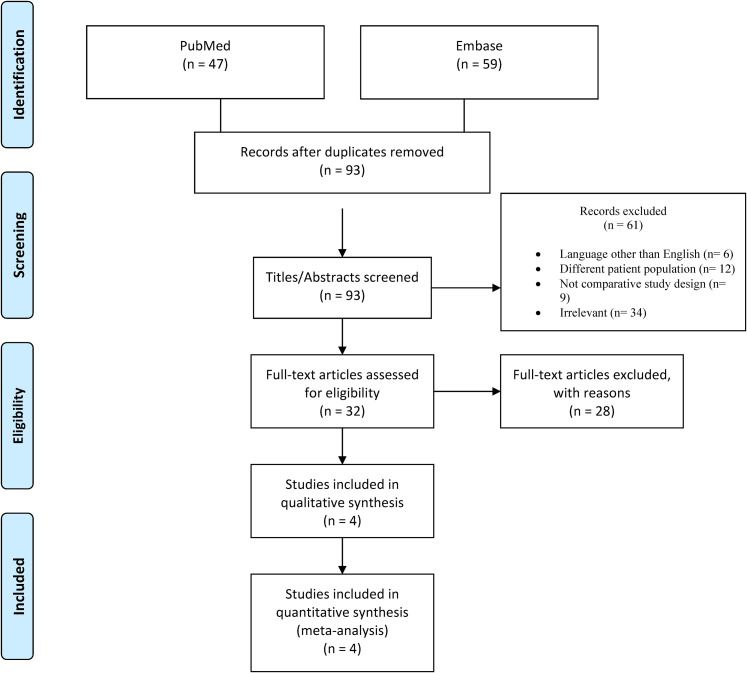
The literature search and data extraction were conducted utilizing the guidelines of the preferred reporting items for systematic review and meta-analysis (PRISMA). In June 2021, a comprehensive database search was performed using PubMed and Embase. The reference lists of the original studies were searched for additional studies. The search criteria included the keywords “Inlay”, “Onlay”, “Reverse Shoulder Arthroplasty”, and “RSA”. 106 articles were initially found. Languages other than English, biomechanical studies, letters to editors, non-full text, case reports, meta-analyses, and review articles were excluded. Once the 13 duplicates were removed, the title and abstract screening included 93 articles, of which 61 were deemed irrelevant because they did not focus on the topic of concern. Only 32 full-text articles were evaluated for eligibility (Figure 1). Following the full-text screening, four papers met our criteria comparing inlay to onlay humeral component prosthesis for RSA. The data was extracted from the results of the included studies and was entered into a Microsoft excel spreadsheet for further analysis. The selected articles were not blinded for the author, affiliation, or source.
Figure 1.
PRISMA flow diagram.
Outcomes measures
The following outcomes measures were analyzed: active range of motion (AROM), Constant Score (CS), Visual Analogue Scale (VAS) for shoulder pain, scapular notching, scapular fractures, and acromial fractures.
Methodological quality assessment
Methodological quality assessment of the selected articles was conducted utilizing the Coleman score, which evaluates the quality of randomized and nonrandomized orthopaedic studies. This score includes a list of 10 criteria, with a final score ranging from 0 to 100. Higher scores indicate the absence of biases while lower scores equate to increased biases. The scores are categorized into excellent (85–100), good (70–84), fair (50–69), and poor (<50). Each selected study was given a calculated score by reviewers.
Data analysis
The meta-analysis software Review Manager 5.4.1 (Cochrane Collaboration, London, UK) was used for the data analysis. Each outcome measure was depicted in a forest plot. The forest plots indicated the standardized mean difference, individual study weights, and the 95% confidence interval for each article. The event outcomes for the postoperative complications were depicted in forest plots indicating the odds ratio, individual study weights, and the 95% confidence interval. To measure the heterogeneity of the included studies, a Chi2 index was used. Due to the presence of a high level of heterogeneity, a random-effects meta-analysis was used due to its ability to weigh studies more equally. To analyze publication bias of the included studies, a funnel plot was used. A P value <0.05 indicated statistical significance.
Results
Four papers5,9,12,14 with a total of 298 patients (306 shoulders) met our search criteria. Of the 306 shoulders, 155 received an onlay humeral component and 151 an inlay humeral component, with a mean patient age of 74.5 ± 5.9 years (125 males, 181 females). The minimum length of follow-up was 12 months for Beltrame et al. 9 and 24 months for the other three studies. One study utilized a 135° neck-shaft angle (NSA) stem for both the inlay and onlay groups. Three studies utilized a 145° curved stem for the onlay group and a 155° straight stem for the inlay group. Table 1 illustrates the characteristics of each study. All the included studies are of level III evidence. No articles in this analysis are randomized controlled trials, three are retrospective and one is prospective. The Coleman score ranged between 58 and 64, indicating a fair quality of evidence.
Table 1.
Study characteristics.
| Author | Study, LoE | CS | Participants | Mean age (range), yr | Gender (M/F) | Mean Follow-up | Humeral Prothetic Design | Glenoid Sided Construct | Outcomes | Statistically Significant Outcomes | Complications (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beltrame et al. 9 | Prospective, III | 64 | Onlay: 21 Inlay: 21 Total: 42 (42 shoulders) |
Onlay: 77 ± 3.8 (68–85) Inlay: 73 ± 8.2 (55–88) |
Onlay: 6/15 Inlay: 6/15 |
Onlay: 12 months Inlay: 12 months |
Onlay: 145° curved stem (Ascend Flex) Inlay: 155° straight stem (Modular Shoulder System) |
Active Range of Motion (AROM) (abduction, adduction, forward flexion, extension, external rotation, internal rotation), CS. | Onlay: None Inlay: inferior scapular notching (3) |
||
| Polisetty et al. 14 | Retrospective, III | 58 | Onlay: 46 Inlay: 46 Total: 92 (92 shoulders) |
Onlay: 74.8 ± 3.6 Inlay: 73.2 ± 5.9 |
Onlay: 22/24 Inlay: 18/28 |
Onlay: 31 months Inlay: 29 months |
Both used a 135° neck-shaft angle stem | Both used lateral | ASES, SST, VAS, AROM (external rotation, forward flexion, internal rotation) | ER: Increased in the Onlay group
(P < 0.001) FF: Increased in the Onlay group (P < 0.001) Greater tuborosity and calcar resorption: Increased in the Onlay group (P < 0.0001) |
Onlay: Scapular notching (4), greater tuberosity resorption
(34), calcar resorption (18), acromial fracture
(6) Inlay: Scapular notching (4), greater tuberosity resorption (13), calcar resorption (1), acromial fracture (4) |
| Franceschetti et al. 5 | Retrospective, III | 62 | Onlay: 49 (50 shoulders) Inlay: 47 (48 shoulders) Total: 96 (98 shoulders) |
Onlay: 73 ± 6 Inlay: 75 ± 4 |
Onlay: 24/26 Inlay: 26/22 |
Onlay: 25 months Inlay: 32 months |
Onlay: 145° curved stem (Ascend flex) Inlay: 155° straight stem (Aequalis reversed II) |
CS, VAS, AROM (Forward flexion, abduction, external rotation, internal rotation, strength (forward flexion, abduction, external rotation, internal rotation) | Onlay: Scapular notching (6), postoperative infections (2),
scapular spine fracture (1) Inlay: Scapular fractures (1), scapular notching (14), dislocations (1), postoperative infections (2) |
||
| Merolla et al. 12 | Retrospective, III | 64 | Onlay: 38 shoulders Inlay: 36 shoulders Total: 68 (74 shoulders) |
Onlay: 74.7 ± 9 (55–91) Inlay: 75.8 ± 8 (55–88) |
Onlay: 13/25 Inlay: 10/26 |
Onlay: 29.1 months Inlay: 35.1 months |
Onlay: 145° curved stem (Ascend Flex) Inlay: 155° straight stem (Aequalis II) |
CS, AROM (forward flexion, abduction, external rotation, external rotation, internal rotation), VAS | ER: Increased in the Onlay group
(P = 0.016) Scapular notching: Increased in the Inlay group (P = 0.0003) |
Onlay: Scapular spine fractures (2), scapular notching (2),
acromial fracture (1). Postoperative infections (3),
dislocations (1) Inlay: dislocation (2), scapular notching (14) |
LoE, Level of evidence; CS, Coleman score; ASES, American shoulder and elbow score; VAS, Visual analogue scale; AROM, Active range of motion; SST, Simple shoulder; ER, External Rotation; FF, Forward Flexion.
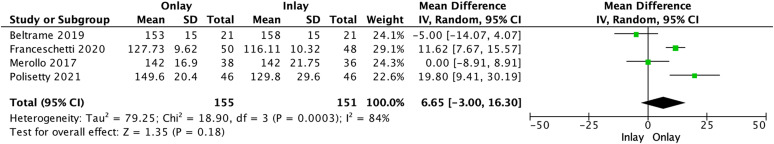
Forward flexion
Forward flexion (FF) was reported in four studies (Figure 2).5,9,12,14 The onlay humeral component prosthesis (155 shoulders) showed improved discrete postoperative results (142.36° ± 15.13) versus the inlay humeral component prosthesis (151 shoulders; 135.71° ± 18.59), which was not statistically significant. (Mean difference, 6.65°; p = 0.18).
Figure 2.
Forward flexion.
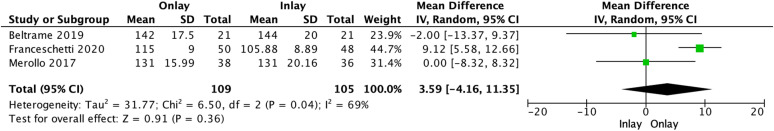
Abduction
In three studies5,9,12 that reported abduction (Figure 3), onlay humeral component (109 shoulders) showed increased discrete postoperative results (126.48° ± 13.23) versus the inlay humeral component (105 shoulders; 122.88° ± 15.08), which was not statistically significant. (Mean difference, 3.59°; p = 0.36).
Figure 3.
Abduction.
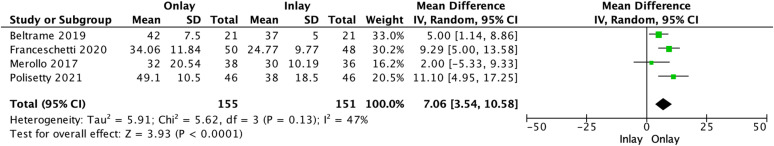
External rotation
Four studies5,9,12,14 reported ER (Figure 4) which reported a statistically significant difference in favor of onlay humeral component (155 shoulders) when compared to inlay humeral component (151 shoulders). (Mean difference, 7.06°; p < 0.0001). The onlay group had a mean postoperative ER of 39.40° ± 11.53 versus the 32.34° ± 10.04 performed by the inlay group.
Figure 4.
External rotation.
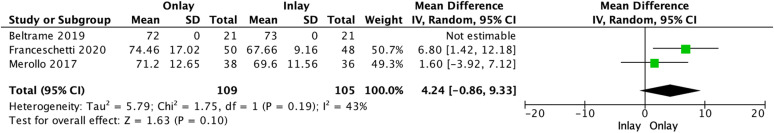
Constant score
In the three studies5,9,12 that reported CS (Figure 5), onlay humeral component (109 shoulders) showed improved results (72.85 ± 12.33) above inlay humeral component (105 shoulders; 69.62 ± 10.34), however, the results are not statistically significant. (Mean difference, 4.24; p = 0.10).
Figure 5.
Constant score.
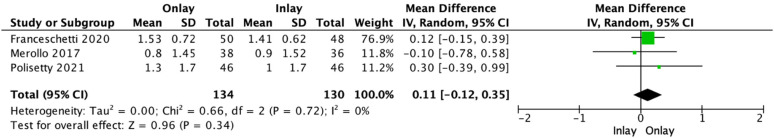
Visual analogue scale (VAS) for anterior shoulder pain
VAS was reported in three studies1,5,12,14 (Figure 6), inlay humeral component (130 shoulders) showed improved results (1.42 ± 0.92) above onlay humeral component (134 shoulders; 1.30 ± 0.85), which was not statistically significant. (Mean difference, 0.11; p = 0.34).
Figure 6.
Visual analogue scale.
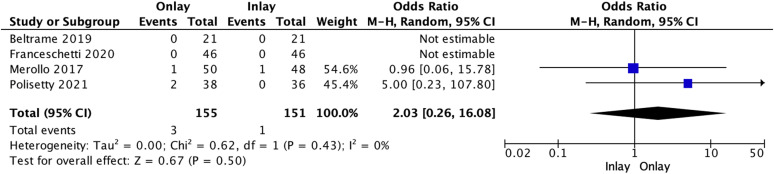
Scapular and acromial fractures
Scapular fractures were reported in four studies (Figure 7).5,9,12,14 Onlay humeral component reported an increased number of scapular fractures (3 of 155 shoulders; 1.94%) when compared to inlay humeral component (1 of 151 shoulders; 0.66%), which was not statistically significant (Odds ratio, 2.03; p = 0.50).
Figure 7.
Scapular fractures.
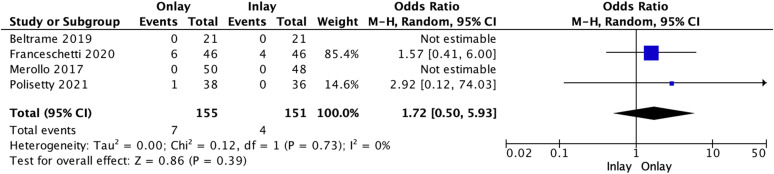
Acromial fractures were reported in four studies (Figure 8).5,9,12,14 Onlay humeral component (155 shoulders) showed increased acromial fractures (7 of 155 shoulders; 4.52%) versus inlay humeral component (4 of 151 shoulders; 2.65%), which was found not to be statistically significant (Odds ratio, 1.72; p = 0.39).
Figure 8.
Acromial fractures.
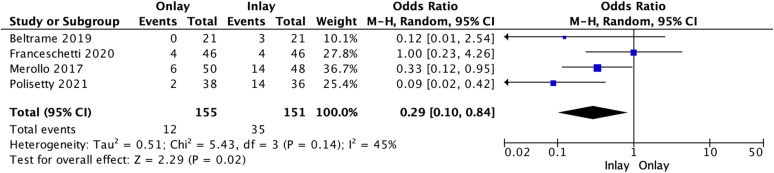
Scapular notching
In four studies5,9,12,14 that reported scapular notching (Figure 9), inlay humeral component (35 of 151 shoulders; 23.18%) showed an increased number of scapular notching versus onlay humeral component (12 of 155 shoulders; 7.74%), which was statistically significant (Odds ratio, 0.29; p = 0.02).
Figure 9.
Scapular notching.
Discussion
This meta-analysis aimed to compare outcomes and complications between onlay and inlay humeral prosthesis designs. This study found that onlay humeral prostheses appear to have greater ER and lower rates of scapular notching compared to the inlay designs evaluated in the literature. No statistically significant differences in FF, abduction, CS, VAS, scapular fractures, or acromial fractures were observed between the two designs.
Regardless of whether the humeral prosthesis was an onlay or inlay design, the overall average ROM of patients in this analysis improved postoperatively. When comparing ROM ER, the onlay humeral prosthesis showed a significant increase of 7.06 ± 4.8° compared to the inlay humeral prosthesis. This finding is consistent with multiple comparative studies that analyzed ROM.5,9–11,18 Utilizing a three-dimensional computer model, Lädermann et al. 11 demonstrated a significant improvement in adduction, extension, and ER in a short curved onlay stem when compared to the traditional inlay Grammont stem with the same inclinations (135°, 145°, 155°). Additionally, in a more recent study of 42 patient's, Beltrame et al. 9 reported a significant difference in adduction, ER, and extension when comparing onlay versus inlay humeral prosthesis designs. However, the authors reported no significant differences in FF and abduction, supporting our findings in this analysis. 9
The increased ROM in the onlay design has been described to be a result of the humeral offset, as well as the increased arm lengthening that is provided by the onlay humeral prosthetic design.5,11,12,19 In a biomechanical study performed by Hamilton et al., 20 the authors analyzed the increased ER seen in the onlay design versus the traditional inlay design. The authors discovered that the increased lateralization seen in the onlay design increases the rotation moment arm of the posterior deltoid, the primary external rotator muscle in RSA patients with torn or absent rotator cuff tendons. Due to the medialization of the inlay humeral component, the posterior deltoid moment arm was decreased, resulting in lower recruitment of the muscle as an external rotator.5,20
The traditional inlay humeral component for RSA is not only known for its relatively limited ER but also its increased risk for scapular notching.3,5,9,12,14 In our analysis, we reported a 15.44% increase in scapular notching within the inlay group when compared to the onlay group. Scapular notching has been discovered to be directly related to polyethylene wear, creating an osteolytic process known to be a concern for patients with the inlay design.1,2,9,11,17,19 Although studies have shown that increased scapular notching results in worse postoperative outcomes,1–3,5,12,21 a more recent study found that it did not correlate with worsened functional outcomes. 9 Acromial and scapular spine fractures are also among the most common postoperative complications following an RSA.1,2,14,22 These fractures have been discovered to worsen recovery as well as functional outcomes.1,2,14,22 In a recent meta-analysis of 4393 patients, acromial and scapular spine fractures were found to be the most common postoperative complication in the onlay humeral component (1.75%). 2 In our analyses, the onlay humeral component resulted in an increased number of acromial and scapular spine fractures, which was not statistically significant (p = 0.50, P = 0.39).
Several limitations have been identified in this analysis. Firstly, there were no randomized control trials included in our analyses. One study was of a prospective design, while the other three were of retrospective design. All these studies corresponded to a level III of evidence with the Coleman scores ranging from 58 to 64, indicating a fair quality of evidence. Secondly, multiple factors have been established to further influence the clinical outcomes and complications that were not well controlled in these articles. These include the type of glenosphere, postoperative rehabilitation, prior interventions, humeral version, and length of follow-up. The greatest limitation of this study is that is it did not control for NSA, which can influence ROM and rate of scapular notching.
Multiple articles have reported larger NSA to have increased scapular notching.23–26 Within our analysis, 109 of 155 shoulders within the onlay group utilized 145° NSA while 105 of 151 shoulders within the inlay group utilized 155° NSA. A systematic review of 2222 shoulders performed by Erickson et al., 23 compared 155° NSA versus 135° NSA and its effects on scapular notching. The authors reported that patients with the 155° NSA resulted in a 14.0% increased rate of scapular notching compared to the 135° NSA. A more recent randomized controlled trial of 100 patients demonstrated significantly higher rates of scapular notching in patients with 155° NSA compared to a 135° NSA; however, there was no significant difference found in ER, FF, or functional outcomes. 24 Therefore, although our analysis reports an increased scapular notching with the inlay humeral component, due to the uncontrolled NSA, it remains unclear whether these results are due to onlay versus inlay humeral components, or the increased NSA seen in the inlay group.
In addition to the humeral component for RSA, many studies have demonstrated the glenosphere to play an important role in scapular notching.27–31 Biomechanical studies have found that a more lateralized glenoid offset improves rotational movement and avoids scapular notching.31,32 In a recent study of 147 RSA's, scapular notching has been found to directly correlate with glenosphere inclination and inferiorization. 30 Despite these findings, scapular notching and its effect on clinical outcomes continues to be a controversial discussion in current literature. While some authors report no impact on postoperative outcomes, others found scapular notching to have worse outcomes and increased complication rate.27–29
Conclusion
This meta-analysis provides evidence that both onlay and inlay RSA designs are associated with improved postoperative ROM. Onlay humeral prosthesis designs in RSA may be associated with greater ER and lower rate of scapular notching postoperatively; however, no difference was found in Constant and VAS scores between designs, so further studies are required to assess the clinical significance of these differences.
Acknowledgements
None.
Footnotes
SS receives consultant payments from Lima USA, MEdacta, and Wright Medical Technology, INC. NH receives consultant payments from Stryker.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Ethical approval (include full name of committee approving the research and if available mention reference number of that approval): Ethical approval was not sought for the present study because this study is a review.
Informed consent: Informed consent was not sought for the present study because it is a review.
ORCID iDs: Garrett R Jackson https://orcid.org/0000-0002-7018-8382
Bryan M Saltzman https://orcid.org/0000-0003-3984-4246
Trial registration (where applicable): Not applicable because this study is a review.
Guarantor: *BS.
Contributorship: All authors contributed in Design/data interpretation, manuscript revision, final approval, and accountable for all aspects of work.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Ascione F, Kilian CM, Laughlin MS, et al. Increased scapular spine fractures after reverse shoulder arthroplasty with a humeral onlay short stem: an analysis of 485 consecutive cases. J Shoulder Elbow Surg 2018; 27: 2183–2190. [DOI] [PubMed] [Google Scholar]
- 2.Ascione F, Schiavone Panni A, Braile A, et al. Problems, complications, and reinterventions in 4893 onlay humeral lateralized reverse shoulder arthroplasties: a systematic review (part I-complications). J Orthop Traumatol 2021; 22: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boileau P, Watkinson D, Hatzidakis AMet al. et al. Neer award 2005: the grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006; 15: 527–540. [DOI] [PubMed] [Google Scholar]
- 4.Flatow EL, Harrison AK. A history of reverse total shoulder arthroplasty. Clin Orthop Relat Res 2011; 469: 2432–2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franceschetti E, Ranieri R, Giovanetti de Sanctis Eet al. et al. Clinical results of bony increased-offset reverse shoulder arthroplasty (BIO-RSA) associated with an onlay 145° curved stem in patients with cuff tear arthropathy: a comparative study. J Shoulder Elbow Surg 2020; 29: 58–67. [DOI] [PubMed] [Google Scholar]
- 6.Jones KJ, Dines DM, Gulotta Let al. et al. Management of proximal humerus fractures utilizing reverse total shoulder arthroplasty. Curr Rev Musculoskelet Med 2013; 6: 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wall B, Nové-Josserand L, O’Connor DPet al. et al. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 2007; 89: 1476–1485. [DOI] [PubMed] [Google Scholar]
- 8.Werner CM, Steinmann PA, Gilbart Met al. et al. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005; 87: 1476–1486. [DOI] [PubMed] [Google Scholar]
- 9.Beltrame A, Di Benedetto P, Cicuto Cet al. et al. Onlay versus inlay humeral steam in reverse shoulder arthroplasty (RSA): clinical and biomechanical study. Acta Biomed 2019; 90: 54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kozak T, Bauer S, Walch Get al. et al. An update on reverse total shoulder arthroplasty: current indications, new designs, same old problems. EFORT Open Rev 2021; 6: 189–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lädermann A, Denard PJ, Boileau P, et al. Effect of humeral stem design on humeral position and range of motion in reverse shoulder arthroplasty. Int Orthop 2015; 39: 2205–2213. [DOI] [PubMed] [Google Scholar]
- 12.Merolla G, Walch G, Ascione F, et al. Grammont humeral design versus onlay curved-stem reverse shoulder arthroplasty: comparison of clinical and radiographic outcomes with minimum 2-year follow-up. J Shoulder Elbow Surg 2018; 27: 701–710. [DOI] [PubMed] [Google Scholar]
- 13.Costantini O, Choi DS, Kontaxis Aet al. et al. The effects of progressive lateralization of the joint center of rotation of reverse total shoulder implants. J Shoulder Elbow Surg 2015; 24: 1120–1128. [DOI] [PubMed] [Google Scholar]
- 14.Polisetty TS, Baessler AM, Levy JCet al. et al. Onlay versus inlay reverse total shoulder arthroplasty: a retrospective comparison of radiographic and clinical outcomes. Semin Arthroplasty: JSES 2021; 31: 202–208. [Google Scholar]
- 15.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 1993; 16: 65–68. [DOI] [PubMed] [Google Scholar]
- 16.Roche CP, Diep P, Hamilton M, et al. Impact of inferior glenoid tilt, humeral retroversion, bone grafting, and design parameters on muscle length and deltoid wrapping in reverse shoulder arthroplasty. Bull Hosp Jt Dis 2013; 71: 284–293. [PubMed] [Google Scholar]
- 17.Giles JW, Langohr GD, Johnson JAet al. et al. Implant design variations in reverse total shoulder arthroplasty influence the required deltoid force and resultant joint load. Clin Orthop Relat Res 2015; 473: 3615–3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sellers TR, Abdelfattah A, Frankle MA. Massive rotator cuff tear: when to consider reverse shoulder arthroplasty. Curr Rev Musculoskelet Med 2018; 11: 131–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Langohr GD, Giles JW, Athwal GSet al. et al. The effect of glenosphere diameter in reverse shoulder arthroplasty on muscle force, joint load, and range of motion. J Shoulder Elbow Surg 2015; 24: 972–979. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton MA, Diep P, Roche C, et al. Effect of reverse shoulder design philosophy on muscle moment arms. J Orthop Res 2015; 33: 605–613. [DOI] [PubMed] [Google Scholar]
- 21.Zumstein MA, Pinedo M, Old Jet al. et al. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 2011; 20: 146–157. [DOI] [PubMed] [Google Scholar]
- 22.Kennon JC, Lu C, McGee-Lawrence MEet al. et al. Scapula fracture incidence in reverse total shoulder arthroplasty using screws above or below metaglene central cage: clinical and biomechanical outcomes. J Shoulder Elbow Surg 2017; 26: 1023–1030. [DOI] [PubMed] [Google Scholar]
- 23.Erickson BJ, Frank RM, Harris JDet al. et al. The influence of humeral head inclination in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 2015; 24: 988–993. [DOI] [PubMed] [Google Scholar]
- 24.Gobezie R, Shishani Y, Lederman Eet al. et al. Can a functional difference be detected in reverse arthroplasty with 135° versus 155° prosthesis for the treatment of rotator cuff arthropathy: a prospective randomized study. J Shoulder Elbow Surg 2019; 28: 813–818. [DOI] [PubMed] [Google Scholar]
- 25.Gutiérrez S, Levy JC, Frankle MA, et al. Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elbow Surg 2008; 17: 608–615. [DOI] [PubMed] [Google Scholar]
- 26.Pashuck TD, Hirahara AM, Cook JLet al. et al. Superior capsular reconstruction using dermal allograft Is a safe and effective treatment for massive irreparable rotator cuff tears: 2-year clinical outcomes. Arthroscopy 2021; 37: 489–496. e1. [DOI] [PubMed] [Google Scholar]
- 27.Boileau P, Watkinson DJ, Hatzidakis AMet al. et al. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 2005; 14(Suppl S): 147S–161S. [DOI] [PubMed] [Google Scholar]
- 28.Simovitch RW, Zumstein MA, Lohri Eet al. et al. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am 2007; 89: 588–600. [DOI] [PubMed] [Google Scholar]
- 29.Sirveaux F, Favard L, Oudet Det al. et al. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 2004; 86: 388–395. [DOI] [PubMed] [Google Scholar]
- 30.Duethman NC, Aibinder WR, Nguyen NTVet al. et al. The influence of glenoid component position on scapular notching: a detailed radiographic analysis at midterm follow-up. JSES Int 2020; 4: 144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Werner BS, Chaoui J, Walch G. The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26: 1726–1731. [DOI] [PubMed] [Google Scholar]
- 32.Gutiérrez S, Comiskey CA, Luo ZPet al. et al. Range of impingement-free abduction and adduction deficit after reverse shoulder arthroplasty. Hierarchy of surgical and implant-design-related factors. J Bone Joint Surg Am 2008; 90: 2606–2615. [DOI] [PubMed] [Google Scholar]