Abstract
The SARS-CoV-2 (COVID-19) viral pandemic dramatically affected human health, health care delivery, health care workers, and health care research worldwide. The field of academic neurology was no exception. In this 2022 Presidential Plenary, we discuss the challenges faced by neurologists and neuroscientists professionally and personally. We review the threats posed by the pandemic to neuroscience research activities, materials, productivity, and funding. We then discuss the impact of the pandemic on clinical trials for neurologic diseases. Restrictions to patient enrolment due to limited in-person access to laboratory testing, imaging, and study visits led to delay in both clinical trial enrolment and study completion but also to innovative new means to engage clinical trial participants remotely and to strategies to critically appraise the frequency and design of trial-related patient evaluations. Clinical care was also challenged by initial pandemic prioritization of urgent visit and inpatient care and the rapid pivot to telehealth for most other neurology care encounters. Front-line neurology care teams faced their fears of infection, with the first few months of the pandemic being characterized by uncertainty, inconsistent national health care strategies, limited personal protective equipment, and an alarming rate of human illness and death caused by COVID-19. The personal and societal toll of the pandemic is incalculable. Across research and clinical neurology providers, women and particularly those with young families juggled the impossible balance of career and family care as schools closed and children required home-based education. Shining through this dark time are lessons that should shape a brighter future for our field. We are resilient, and the advances in neuroscience and neurology care continue to advance improved neurologic outcomes. The National Institutes of Health devised multiple support strategies for researchers to help bridge the pandemic. Telehealth, clinical trial designs that are more participant-centric with remote monitoring, and flexible work schedules are strategies to rebalance overworked lives and improve our engagement with our patients. As we re-emerge, we have the chance to reframe our field.
The SARS-CoV-2 pandemic has had a dramatic impact on all aspects of human health and health care worldwide. The impact on the field of neurology has been no less profound. We learned about the neurologic manifestations of COVID-19, both acutely and now with ongoing symptomatology (termed “long-haul COVID”). In addition to the direct neuroinvasive aspects of the SARS-CoV-2 infection, there have been numerous points of impact of the pandemic on the health of patients with neurologic disease and their families. Increased rates of cardiovascular disease, long-term postinfectious respiratory issues, and reduced exercise tolerance are just a few issues that will serve as comorbid contributors to reduced neurologic health. A dramatic rise in anxiety, depression, and suicidality affecting both adults and children has been alarming.1-3 In a meta-analysis of data relating to over 80,000 youth, rates of clinically-elevated depression affected 25% and anxiety 20%, with rates being more than double the prepandemic rates.1 Suicide is the second leading cause of death in adolescents, with increasing rates in minoritized youth.4 Increased rates of depression, anxiety, and burnout among neurology care providers has also been reported, and many presentations at the American Academy of Neurology Meeting held in April 2022 addressed these pivotal health issues faced by our patients, colleagues, and communities.
The Presidential Plenary lecture focused on the impact of the COVID-19 pandemic on the neurology academic community and more specifically on the impact of the pandemic because it relates to neurologic research, basic, translational, and clinical trials. We review the critical challenges and the resilience that emerged. Lessons learned and importantly lessons not to be forgotten will be shared. Broader issues, including national guidelines for informed health decisions, effective communication strategies that not only disseminate critical information during a pandemic but also directly address fears, misinformation, cultural beliefs, and the disproportionate impact of the pandemic on persons of color, on communities living with food insecurity and health care inequity are beyond our neurology-focused presentation but are pivotal issues that warrant serious and ongoing focus.
Pandemic: A Long-term Threat to Basic Science
In February 2021, the Office of Extramural Research of the National Institutes of Health (NIH) published the results of a survey distributed to 234,254 NIH-funded investigators, of whom 45,348 responded. Approximately half of investigators involved in all kinds of biomedical research indicated that the COVID-19 pandemic would negatively affect their career.5 Those engaged in laboratory-based research seemed to be most frequently and those in epidemiologic and public health research, least frequently affected (Figure 1). The challenges of the pandemic to laboratory-based basic science can be divided into 5 interrelated categories: people, animals, supplies and equipment, spaces, and time.
Figure 1. Percentage of NIH Principal Investigators Performing Research of Different Types Who Noted in a February 2021 Survey That They Would Experience Negative Effects on Their Careers Because of the COVID-19 Pandemic.
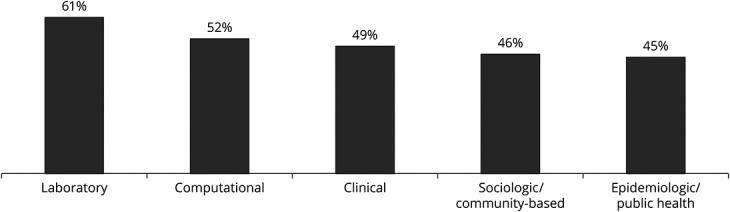
n = 45,348 respondents of 234,254 NIH-funded invitees; National Institutes of Health Office of Extramural Research, 2021.
Impact on Personnel
The direct effects of the COVID-19 pandemic on the basic science research workforce and those who support their work include the illness, SARS-CoV-2 test positivity, and exposure to ill and/or SARS-CoV-2–positive people of sizable fractions of this workforce. Absences from work pervaded the scientific, facilities, security, food service, and other communities for over 2 years.6
Increased responsibilities for home care of children, elderly relatives, and those with disabilities also kept large segments of the research and support workforce away from the workplace. Closure of schools and daycare centers disproportionately affected women and young scientists.7 In addition, those who do basic research that depends on obtaining specimens of body fluids from or interacting with normal human subjects were negatively affected by closure of hospitals and clinics to research subjects who would not directly benefit medically from study participation.
Graduate students and postdoctoral fellows were particularly affected by initial shutdowns of laboratory facilities and by the needs of their often-young families. Although academic and government institutions generally extended deadlines and term limits, anxiety around interruption of career time lines and income streams remain an enormous challenge. On the other hand, social media, podcasts, and cloud-based analytic tools kept many students and fellows connected to their peers and mentors and able to continue with aspects of their work that, because of technology, no longer required physical presence in the laboratory or on the university campus.
This personnel shortage affected nonscientists as well. For example, at the NIH, security was insufficiently staffed to respond to calls from staff who locked themselves out of their offices; there were repeated calls for additional personnel to staff the COVID-19 testing service; and at one point, there was a critical shortage of people staffing the power station on campus.
Impact on Animal Research
While some of the work of many who support biomedical research can be performed remotely, those who work in laboratory animal research facilities must be on site during their shifts. They are like health care workers in a hospital or clinic. For this reason, animal research facilities were disproportionately affected by workforce shortages during the pandemic.8 As such, priorities had to be set, with essential activities first and foremost and research-related activities postponed or canceled. Breeding colonies were lost; large cohort surgeries were cancelled; routine task performance protocols were changed to make them doable with limited staff; and suppliers of animals were unable to accommodate the demand.9 In many institutions, on-site animal research staff numbers were below critical levels for much of the winter of 2021–2022.
Impact on Supplies and Equipment
As in many industries and disciplines, supply chain issues continue to curtail access to supplies for basic biomedical research.9 Plasticware, as is used in tissue culture research, is particularly difficult to obtain. In addition, equipment acquisition, delivery, installation, and maintenance have been curtailed. This is particularly challenging for new investigators, most of whom are hoping to establish and equip their laboratories in the setting of limited time windows of eligibility for career development funding. A 2022 survey of principal investigators in the Division of Intramural Research at the National Institute of Neurologic Disorders and Stroke demonstrated that 84% of these scientists experienced delays in supply receipt and 68% reported having to find an alternate vendor for supplies that were often not optimal for performance of planned studies.
Impact on Space
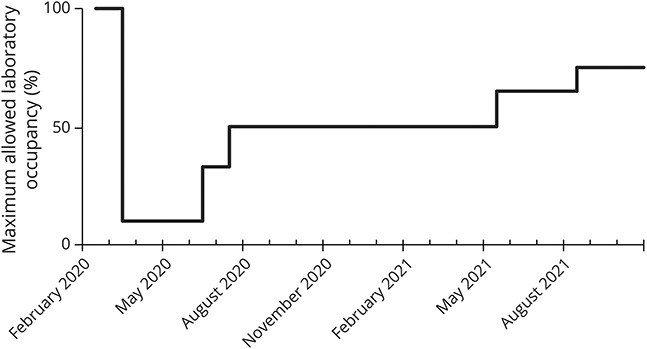
In many institutions, the density of people in laboratory, conference, and office space was tightly regulated. At the NIH, in March 2020, only essential personnel (i.e., those involved in caring for patients or animals, performing COVID-19-related research, or maintaining mission-critical facilities or functions) were allowed on campus. Between then and the following Fall, allowable “people density” increased only gradually (Figure 2), requiring scientists and those who support them to work in shifts and often to perform what were normally team activities singly for a large fraction of that year. Indoor people density restrictions also limited construction, renovation, and equipment installation once again, especially impeding the progress of new investigators who are most likely to be setting up new laboratories.
Figure 2. Maximum Allowed Laboratory and Office Occupancy on the Campuses of the National Institutes of Health as a Percentage of Their Prepandemic Occupancy.
Impact on Time
Perhaps the most challenging aspect of the effects of the pandemic on basic research involves the loss of time in the laboratories, conference rooms, and offices in which basic research is planned, performed, and discussed. The loss in productivity of research teams during lockdown followed by restrictions has directly delayed the creation of new knowledge and its translation into preventive, treatment, and curative approaches that will ease the burden of neurologic disorders. By interfering with animal husbandry and breeding, development of nonanimal approaches to research, and availability of supplies and equipment, it has further delayed research beyond the time frame of access to laboratory spaces and personnel. Tools for research now need to be remade and reacquired. This indirect delay will be felt for years.
Furthermore, many research grant mechanisms for those just developing their careers have eligibility windows that are jeopardized by COVID-19 pandemic-related delays.10 Garnering necessary preliminary data, publishing scientific papers, and writing grants were made near impossible for those affected by limited access to space and materials, caring for young children at home, facilitating schooling online, and caring for elders displaced by closed long-term care facilities. Many institutions instituted hiring freezes, canceling offers made, and preventing compensation and progression to the next career step for dozens of young scientists and trainees. It is feared by many that if we are not careful and proactive with solutions, we will have lost much of a generation of biomedical scientists to the pandemic.
COVID-19 and Clinical Trials
As the pandemic took hold, all nonessential activities in health care were suspended. In most institutions, clinical trials were halted unless the trial was directly offering life-supporting or essential therapeutic potential benefit or if sudden cessation of exposure to a particular agent could result in harm. Very few new clinical trials were commenced. Studies that involved imaging as a primary or key secondary outcome measure were disproportionally affected because many centers could not bring in participants for research MRI scans. Many clinical trials pivoted when possible to remote visits including for obtaining informed consent and for follow-up visits. For example, the Healey ALS Platform Trial11 modified the protocol to require only the baseline and final visits in person and to allow the visits in between to be conducted virtually. NeuroNext, a NIH-supported phase 2 network, modified all active protocols in a similar manner and allowed virtual remote monitoring because most institutions would not allow in-person monitoring visits.
As the pandemic continued, clinical trial supplies became scarce because of supply chain issues, with national shortages of pipettes, sample tubes, and other core supplies. In a survey performed at the Massachusetts General Hospital, 75% of clinical investigators reported delays or lack of access to key supplies (M. Cudkowicz, personal communication). Just as mentioned in the discussion regarding basic clinical research, clinical trial staff also departed the workforce and new hires were largely placed on hold. Even now, there remains a shortage of nurses, including those who serve as essential members of a clinical trial team.
Important insights, however, have been gained in the ability to perform electronic consenting and patient-centric evaluations performed remotely and in the ability to reduce patient on-site testing and instead enable laboratory visits closer to home or even in home. It is now beholden to clinical trial networks to leverage these insights into long-term sustainable new “alternative trial participation” trial designs akin to the “alternative work arrangements” embraced during the pandemic. Remote training for study staff, sponsored meetings performed remotely instead of on site, and electronic signature options have all enabled startup of clinical trials.
New research is now required to validate digital outcome measures, hopefully with engaged input from clinical trial participants themselves. Studies are required to determine whether “alternative trial participation” models improve representation of diverse communities in clinical trials or whether an untoward outcome of such models might be to reduce engagement of persons less comfortable with home-based study visits or those without robust access to digital health.
The pandemic also highlighted disparities in clinical trial participation and opportunities to improve. The importance of ensuring access to virtual care and virtual trials in diverse populations was paramount from the start of the COVID-19 pandemic. This includes access to internet, different virtual platforms, and information on research opportunities. A recent COVID-19 trial reported on the power of social media and digital technology to increase participation of diverse populations in clinical trials.12 There is a critical positive opportunity here to leverage for future trials where more patient-centered trials can increase participation by diverse communities because of the ability to have visits while at home; at work; on nonwork hours; and without the added expense, time and stress to travel to a center.
COVID-19 and Neurology Care Teams
The COVID-19 pandemic revealed major deficits in pandemic readiness at the local and national levels in the United States and internationally. In the first months (March–June 2020), as cases of SARS-CoV-2 infection rapidly multiplied and patients developed mild to severe COVID-19 illness, health care providers responded to the crisis with limited data. In a survey of over 400 US-based neurologists (56% of whom work in academic centers), personal protective equipment (PPE) was not available to all and the definition of PPE (type of mask, surgical gowns) varied, and 45% stated that they were required to reuse PPE.13 Testing for COVID-19 was also not uniform, and 44% stated that they had seen patients without wearing PPE only to learn later that the patient subsequently was confirmed to be COVID-19–positive.
Administrative leaders of hospital-based neurology services and hospital leadership broadly made daily decisions regarding deployment of front-line staff. Attempts to minimize risk to employees while maintaining patient care led to rapid adoption of new strategies. Telehealth rose rapidly as a means to offer comprehensive patient histories, patient and family-facilitated witnessed neurologic assessment, and dissemination of care plans to patients in their own homes. Many neurology departments closed all ambulatory clinics, offering only emergent in-person care and converting all other care to telehealth. In an analysis of over 2,500 telehealth encounters performed by a large pediatric neurology division, 93% of faculty were satisfied by the quality of care provided, and only 5% of all encounters led to an urgent in-person evaluation.14 Of 200 parents interviewed, 86% endorsed telehealth as a positive experience. Techniques through which to optimize a video-witnessed neurologic examination were published by the AAN online (aan.com/telehealth). “Telephone-only” consultations were also offered in some regions. In a study performed in the United Kingdom, of 430 respondents, 78% of clinicians and 78% of patients stated that telephone-based consultations met their care needs.15
Telehealth not only offered a means for safe neurology care in the height of the pandemic but also liberalized work hours for many providers. Telehealth clinic days, performed from home, eliminated commute times. Telehealth clinics can occur at hours more convenient for both providers and patients, including early morning preregular workday or in the evenings. As one provider shared, “I have now been home for dinner and bedtime stories many nights over the past 2 years. This is invaluable time that I would have frequently missed were it not for telehealth options.” Many providers also felt that telehealth visits were more efficient, with no delays due to waiting room lineups and with patients and families being more mindful of the duration of the visit. The requirement to sign off from a call to sign into the next visit provided clear time limits that were respected more frequently than in-person visits. Limitations included poor internet literacy and inadequate connectivity for some families—a source of health disparity. Conveyance of difficult diagnostic news through video differs from the in-person empathetic experience. Patients may communicate their concerns differently through telehealth, influenced in part by whether they have a private space in their home from which to conduct a telehealth visit.
While being home more frequently was a source of wellness for some, it posed major challenges for others. In a survey regarding the impact of the COVID-19 pandemic on physicians in MA, female physicians significantly reduced their professional duties and increased their child care responsibilities.16 School and daycare closures were nearly universal across the United States early in the pandemic, and they occurred with variable and often unpredictable frequency as the pandemic time progressed. Virtually enabled home schooling became a parental responsibility. “Impossible is the one word that comes to mind when you ask for my thoughts. What COVID has required of people like me, junior physician researchers with young children, is tasking us with the impossible. It already felt like swimming upstream pre-pandemic. Trying to be productive clinically and with research while being present for my children felt like swimming up a gushing waterfall.”
Individuals living with neurologic disability also shared their views regarding the impact of the pandemic. “It took a pandemic, during which time CEOs and their teams were afraid to come to work, to develop strategies and policy shifts that empowered and embraced alternative work arrangements. For the first time, my contributions to the work force are on equal footing.” Telehealth visits also empowered neurology patients, as such visits obviated the need for public transport and access services, greatly reduced the effort required to prepare for a visit and offered options for clinicians to visualize how their patients cope in the home environment. Recent studies support the value of teleneurology visits, with 94% of neurologists reporting in a recent study that they felt the virtual visit provided requisite clinical information and observed neurologic examination data to inform care over 95% of the time,17 findings that were also found in a study evaluating over 1,000 patient encounters.18 Advocacy for teleneurology reimbursement will be a key step to sustain virtual visits, as well as including patient perspectives in the improved access and reduced burden afforded by this model of neurology care delivery.
An important aspect of the pandemic has been the increase in mental health among our peers. In a study of physicians, a significant increase in depression was reported by female physicians in particular.19 The more selective increase in depression among female physicians adds to the already recognized increased rate of burnout in female neurologists reported even before the pandemic.20 In a study of 181 female neurologists, 45% endorsed burnout, and of those with three or more children, 66% stated that if they could choose their career over again, they would not select becoming a neurologist.20 Strategies to support our neurology colleagues will be critical, and institutions are implementing counseling and emotional support programs.21
Resilience, Hope, and Solutions
The pandemic is not yet over, and we continue to face ongoing challenges with COVID-19–related illness (both acute and “long-haul” residua from prior COVID-19 infection) among our patients, peers, families, and communities. Ready access to vaccines that have proven to be highly effective at presenting serious COVID-19 infection and hospitalization has been the direct result of urgently prioritized research and development. As medical professionals, we are part of a community that is now more informed about pandemic readiness and hopefully will serve as ongoing advocates for improved pandemic planning, communication, and preparedness. As neurologists, we continue to learn about the neurologic complications of acute and convalescent COVID-19 infection.
We have learned valuable lessons regarding our ability to rapidly adopt new models of neurologic care, clinical trials, and clinical and basic research. We have the opportunity to celebrate this new flexibility. The question perhaps should not be “will teleneurology continue” but rather “how can we optimize neurologic assessments and communications” to best serve our patients. Teleneurology offers a measure of health equity to persons with disabilities that otherwise limit their access to in-person visits. Alternative working arrangements, such as teleneurology and virtual meetings, have the potential to improve work-life balance for us as neurology care providers, and we can serve as advocates for such arrangements for our neurology patients. Despite the pandemic-learned lessons, many institutions have already scaled back teleneurology care provision, and many states have reinstated barriers to teleneurology care provision across state lines. Directed research with active patient-reported and provider-reported data regarding quality of care, care satisfaction, and care facilitation is needed to avoid abandonment of an enabling form of health care delivery.
The pandemic also enabled online learning with webinars virtual conferences and hybrid learning options. The AAN's annual meeting was one such example, with a fully online meeting in 2020 and a hybrid meeting in 2021. Asynchronous learning offers flexibility, which may permit busy neurologists to self-select learning times that best align with their work and home life and allows neurologists to avail themselves of current data presented by worldwide experts. The very low cost of virtual lectures facilitates faculty invitations from outside institutions and have the potential to foster the academic careers of junior faculty given that outside lecture invitations are weighted heavily by many schools of medicine promotion committees. This enhanced invitational potential could help address the academic promotional barriers facing young women with children, who might not otherwise be able to travel to give an invited lecture. Visiting professorship days also include engagement with both faculty and trainees and future potential neurologists. Virtual visiting professorships, typically full-day events with a formal lecture and then individual faculty and group trainee meetings, open doors for underrepresented minority in medicine (URM) faculty across the country, who not only can share their clinical expertise and research but also inspire URM medical students, trainees, and staff. As an illustrative example, the Training in Research for Academic Neurologists to Sustain Careers and Enhance the Numbers of Diverse Scholars (TRANSCENDS) AAN program uses online connectivity as a core part of the program,22,23 and the results of the first cycle show a high degree of scholar endorsement. Mentorship is a deliberate and active process that we all have the opportunity to engage in. Enhanced cross-institutional virtual meetings provide visibility that can bring mentees and mentors who would otherwise never have connected in the prepandemic, in-person meeting culture.
We also learned to adapt as a research community. As is often the case in challenging circumstances, the scientific community rose in many ways to the occasion to enable those developing their careers to work and advance and to keep the biomedical pipeline alive for those dealing with neurologic disorders. Senior investigators worked and mentored from home, so trainees and junior faculty could come into the laboratory without violating occupancy restrictions. NIH and other funding agencies created mechanisms to extend eligibility windows for training and early career grants. Institutions extended the time between internal reviews of research faculty and adjusted expectations and time lines for tenure determinations. The NIH funded an extra year of postdoctoral research for scientists whose faculty position was rescinded in the face of institutional hiring freezes. Up to $2,500 per year was made available to principal investigators of NIH mentored grants for child and elder care. NIH also made supplementary funds available for replacement of colonies and cell lines lost due to the pandemic. Bridge funding for those who could not work toward imminent grant renewal and supplementary funding for those who pivoted to perform research of relevance to efforts against SARS-CoV-2 and COVID-19 were made available to investigators by the institutes of NIH.24
In addition to enabling continuity of clinical care and research during the pandemic, the neurology and neuroscience communities contributed in innovative ways to the need for protective equipment, natural history of COVID-19–related disease information, and biologic samples for research25-27 Despite unprecedented challenges, the clinical and biomedical neurology community has remained committed to neurologic care and neuroscience for the benefit of humankind, to education and career development for the workforce of tomorrow, and to ease the burden of neurologic disorders for all our communities.
Glossary
- NIH
National Institutes of Health
- PPE
personal protective equipment
- TRANSCENDS
Training in Research for Academic Neurologists to Sustain Careers and Enhance the Numbers of Diverse Scholars
- URM
under-represented minority
Appendix. Authors
Footnotes
COVID-19 Resources: NPub.org/COVID19
Study Funding
The authors report no targeted funding.
Disclosure
N. Schor is an employee of the Federal Government. M. Cudkowicz has no relevant disclosures. B. Banwell has no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1142-1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samji H, Wu J, Ladak A, et al. Review: mental health impacts of the COVID-19 pandemic on children and youth - a systematic review. Child Adolesc Ment Health. 2022;27(2):173-189. doi: 10.1111/camh.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harvey SB, Epstein RM, Glozier N, et al. Mental illness and suicide among physicians. Lancet. 2021;398(10303):920-930. doi: 10.1016/S0140-6736(21)01596-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benton TD. Suicide and suicidal behaviors among minoritized youth. Child Adolesc Psychiatr Clin N Am. 2022;31(2):211-221. doi: 10.1016/j.chc.2022.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Bernard MA, Lauer M. The impact of the Covid-19 pandemic on the extramural scientific workforce - outcomes from an NIH-led survery. Extramur Nexus. Published online 2021. nexus.od.nih.gov/all/2021/03/25/the-impact-of-the-covid-19-pandemic-on-the-extramural-scientific-workforce-outcomes-from-an-nih-led-survey/ [Google Scholar]
- 6.Lyttleton T, Zang E. Occupations and sickness-related absences during the COVID-19 pandemic. J Health Soc Behav. 2022;(63):19-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van der Feltz-Cornelis C, Varley D, Allgar V, de Beurs E. Workplace stress, presenteeism, absenteeism, and resilience amongst university staff and students in the COVID-19 lockdown. Front Psychiatry. 2020;11(588803). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petervary N, Pritchard C, Esparza-Trujillo J, Gopee N. Veterinary staffing shortages and potential solutions during the COVID-19 pandemic. Lab Anim Sci Profess. Published nline November 2020:24-26.
- 9.Woolston C. ‘Does anyone have any of these?’: lab-supply shortages strike amid global pandemic. Nat. Published online March 9, 2021. doi: 10.1038/d41586-021-00613-y. [DOI] [PubMed]
- 10.Bansal A, Abruzzese GA, Hewawasam E, et al. Impact of COVID-19 pandemic on research and careers of early career researchers: a DOHaD perspective. J Dev Orig Health Dis. Published online March 4, 2022:1-6. doi: 10.1017/S2040174422000071. [DOI] [PubMed]
- 11.Paganoni S, Berry JD, Quintana M, et al. Adaptive platform trials to transform amyotrophic lateral sclerosis therapy development. Ann Neurol. 2022;91(2):165-175. doi: 10.1002/ana.26285. [DOI] [PubMed] [Google Scholar]
- 12.Stewart J, Krows ML, Schaafsma TT, et al. Comparison of racial, ethnic, and geographic location diversity of participants enrolled in clinic-based vs 2 remote COVID-19 clinical trials. JAMA Netw Open. 2022;5(2). doi: 10.1001/jamanetworkopen.2021.48325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma A, Maxwell CR, Farmer J, Greene-Chandos D, LaFaver K, Benameur K. Initial experiences of US neurologists in practice during the COVID-19 pandemic via survey. Neurology. 2020;95(5):215-220. doi: 10.1212/WNL.0000000000009844. [DOI] [PubMed] [Google Scholar]
- 14.Rametta SC, Fridinger SE, Gonzalez AK, et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. 2020;95(9):e1257-e1266. doi: 10.1212/WNL.0000000000010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakornchai T, Conci E, Hensiek A, Brown JWL. Clinician and patient experience of neurology telephone consultations during the COVID-19 pandemic. Postgrad Med J. 2022;98(1161):533-538. doi: 10.1136/postgradmedj-2021-141234. [DOI] [PubMed] [Google Scholar]
- 16.Miller KA, Mannix R, Schmitz G, Monuteaux MC, Lee LK. Impact of COVID-19 on professional and personal responsibilities of Massachusetts physicians. Am J Emerg Med. 2020;38(11):2365-2367. doi: 10.1016/j.ajem.2020.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thawani SP, Minen MT, Stainman RS, et al. Neurologists' evaluations of experience and effectiveness of teleneurology encounters. Telemed J E Health. Published online July 14, 2022. doi: 10.1089/tmj.2021.0551. [DOI] [PubMed]
- 18.Tropea TF, Fuentes A, Roberts Z, et al. Provider experience with teleneurology in an academic neurology department. Telemed J E Health. 2022;28(3):374-383. doi: 10.1089/tmj.2021.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frank E, Zhao Z, Fang Y, Rotenstein LS, Sen S, Guille C. Experiences of work-family conflict and mental health symptoms by gender among physician parents during the COVID-19 pandemic. JAMA Netw Open. 2021;4(11):e2134315. doi: 10.1001/jamanetworkopen.2021.34315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore LR, Ziegler C, Hessler A, Singhal D, LaFaver K. Burnout and career satisfaction in women neurologists in the United States. J Womens Health (Larchmt). 2019;28(4):515-525. doi: 10.1089/jwh.2017.6888. [DOI] [PubMed] [Google Scholar]
- 21.Croll L, Kurzweil A, Hasanaj L, Serrano L, Balcer LJ, Galetta SL. The psychosocial implications of COVID-19 for a neurology program in a pandemic epicenter. J Neurol Sci. 2020;416:117034. doi: 10.1016/j.jns.2020.117034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tagge R, Lackland DT, Ovbiagele B. The TRANSCENDS program: rationale and overview. J Neurol Sci. 2021;420:117218. doi: 10.1016/j.jns.2020.117218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tagge R, Lackland DT, Gorelick PB, et al. TRANSCENDS: a career development program for underrepresented in medicine scholars in academic neurology. Neurology. Published online April 23, 2021. doi: 10.1212/WNL.0000000000012058 [DOI] [PMC free article] [PubMed]
- 24.Lauer M. Reminder of COVID-19-related flexibilities for NIH grants. Extramur Nexus. Published online 2021. nexus.od.nih.gov/all/2021/09/24/reminder-of-covid19-related-flexibilities-for-nih-grants/#:∼:text=Nocostextensions.,extensionwithoutNIHpriorapproval [Google Scholar]
- 25.Avitzur O. Not enough N95 masks? This neurology fellow is spearheading development of a new prototype. Neurol Today. Published online 2020. journals.lww.com/neurotodayonline/blog/breakingnews/pages/post.aspx?PostID=936 [Google Scholar]
- 26.Avitzur O. With 3D design know-how, this neurologist is working to produce face shields, gowns, sanitizers for COVID-19. Neurol Today. Published online 2020. journals.lww.com/neurotodayonline/blog/breakingnews/pages/post.aspx?PostID=937 [Google Scholar]
- 27.NeuroCOVID Database. National institute of neurological disorders and Stroke. Coronavirus Resources. 2021. ninds.nih.gov/current-research/coronavirus-and-ninds/resources [Google Scholar]


