Abstract
Background
Adults with inflammatory bowel disease (IBD) are at increased risk of developing cytomegalovirus (CMV) colitis, which is associated with adverse outcomes. Similar studies in pediatric IBD patients are lacking.
Methods
We analyzed non-overlapping years of National Inpatient Sample (NIS) and Kids Inpatient Database (KID) between 2003 and 2016. We included all patients < 21 years with a diagnosis of Crohn’s disease (CD) or ulcerative colitis (UC). Patients with coexisting CMV infection during that admission were compared with patients without CMV infection for outcome measures such as in-hospital mortality, disease severity, and healthcare resource utilization.
Results
We analyzed a total of 254,839 IBD-related hospitalizations. The overall prevalence rate of CMV infection was 0.3% with an overall increasing prevalence trend, P < 0.001. Approximately two-thirds of patients with CMV infection had UC, which was associated with almost 3.6 times increased risk of CMV infection (confidence interval (CI): 3.11 to 4.31, P < 0.001). IBD patients with CMV had more comorbid conditions. CMV infection was significantly associated with increased odds of in-hospital mortality (odds ratio (OR): 3.58; CI: 1.85 to 6.93, P < 0.001) and severe IBD (OR: 3.31; CI: 2.54 to 4.32, P < 0.001). CMV-related IBD hospitalizations had increased length of stay by 9 days while incurring almost $65,000 higher hospitalization charges, P < 0.001.
Conclusions
The prevalence of CMV infection is increasing in pediatric IBD patients. CMV infections significantly corelated with increased risk of mortality and severity of IBD leading to prolonged hospital stay and higher hospitalization charges. Further prospective studies are needed to better understand the factors leading to this increasing CMV infection.
Keywords: Inflammatory bowel disease, Cytomegalovirus infection, Ulcerative colitis, Crohn’s disease, CMV colitis, Population-based study, Health care utilization, Mortality
Introduction
Cytomegalovirus (CMV) belongs to the family of Herpesviridae. CMV infection in immunocompetent individuals are usually asymptomatic or can cause a mild infection with a self-limited course. However, in immunocompromised individuals, CMV can lead to an invasive disease with manifestations such as retinitis, hepatitis, pneumonia, secondary hemophagocytic lymphohistiocytosis and a disseminated CMV infection [1-3]. Among inflammatory bowel disease (IBD) patients, CMV commonly affects the colon [4-6]. CMV colitis is estimated to affect one-third of steroid-resistant acute severe ulcerative colitis (UC) patients [7]. Recent population-based studies in adults demonstrated an increasing incidence of CMV infection among IBD patients in the USA [8]. CMV colitis has been reported in IBD patients with increased usage of steroids and immunomodulators [9-13]. The prevalence of CMV colitis is largely unknown in pediatric UC and Crohn’s disease (CD), and its impact on the disease process is also poorly understood [10, 14]. Recent American College of Gastroenterology UC guidelines published in 2019 stated that adults with acute severe UC should undergo sigmoidoscopy to evaluate for CMV colitis [15]. Similarly, the European Society of Pediatric Gastroenterology Hepatology and Nutrition consensus statement recommends that children with steroid-resistant IBD should undergo sigmoidoscopy and pathologic evaluation for CMV infection [16]. The seroprevalence of CMV among pediatric IBD patients is 38% in children less than 10 years and between 22% to 25% in children aged 11 to 19 years of age, which is in contrast to adult IBD patients where the seroprevalence reaches close to 90% [12, 13, 17]. This relatively lower seropositivity suggests that CMV infection among the pediatric age group is likely a primary infection, whereas in adults, the manifestations are likely to be due to reactivation of a latent infection [18]. There is paucity of data on the burden and impact of CMV infection among hospitalized pediatric IBD patients. Thus, we decided to evaluate the burden of CMV infection and its implications on IBD-related pediatric hospitalizations in the USA.
Materials and Methods
We analyzed non-overlapping years of two separate databases, National Inpatient Sample (NIS) and Kids Inpatient Database (KID), between 2003 and 2016. Both NIS and KID are part of databases developed for the Health Care Cost and Utilization Project (HCUP). NIS includes 20% stratified data with sample frame representative of more than 97% of the US population. NIS database includes patients of all age groups, and data are reported on an annual basis. The KID is a stratified aggregation of pediatric data from more than 4,200 hospitals across the USA and are sampled at a rate of 80%. The KID includes data on hospitalizations of patients less than 21 years of age and is released every 3 years. Both the NIS and KID contain discharge level data from community hospitals (excluding long-term acute care and rehabilitation centers) across the USA.
We included all patients less than 21 years of age during the study period with a primary diagnosis of CD or UC using the International Classification of Diseases, Ninth Revision (ICD-9) and 10th Revision (ICD-10) codes. Patients having a concomitant diagnosis of CMV infection during the same hospitalization were then identified and compared with IBD patients without CMV infection. We also analyzed risk factors of CMV infection such as bone marrow and solid organ transplant status, primary immunodeficiency disorders, human immunodeficiency virus (HIV) infection and common malignancies encountered in children (such as leukemia, lymphoma, central nervous system malignancies, and bone tumors). We also evaluated common IBD-related surgeries and compared between the groups. For hospital resource utilization, we compared the length of hospital stay and total hospitalization charges between the two cohorts.
Using previously described validated methods, we classified the severity of IBD based on the presence or absence of parameters such as anemia, total parenteral nutrition use, malnutrition, requirement of blood transfusion, Clostridium difficile infection [19, 20]. The severity score ranges from 0 to 14 for CD and up to 7 for UC [19, 20]. These risk score predicting the need for surgical intervention among IBD patients and the severity of hospitalization have been used and validated in prior studies evaluating the severity of disease among IBD patients [19-23]. The risk scores and stratification are described here (Supplementary Material 1, www.gastrores.org). This study was approved by the Institutional Review Board (STUDY20220003) and was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Statistical analysis
Categorical variables were described as proportions and percentages. Continuous variables were described as mean and standard deviations. Categorical variables were compared using Chi-squared test and continuous variables using independent Student’s t-test. Multivariate logistic regression model was used to calculate the adjusted odds ratio (OR) and 95% confidence interval (CI) for in-hospital mortality and severity of IBD. Linear regression models were constructed to estimate the effect of CMV infection on length of hospital stay and total charges of IBD-related hospitalization. Multivariate models were adjusted for all the factors associated with CMV infection at a P value < 0.2 on the univariate analysis. Least square regression analysis was used for trend analysis of CMV infection over the years. SPSS 26 was used for statistical analysis.
Results
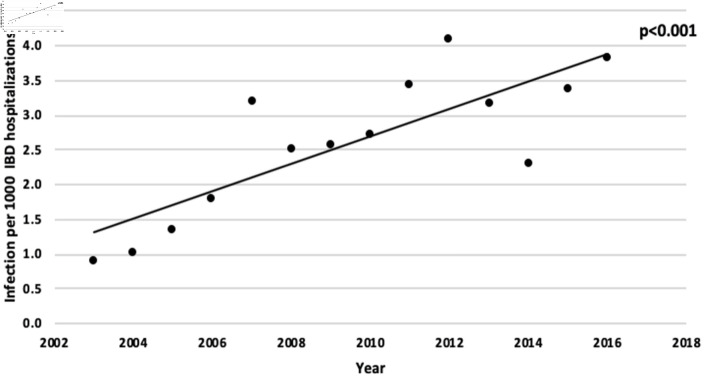
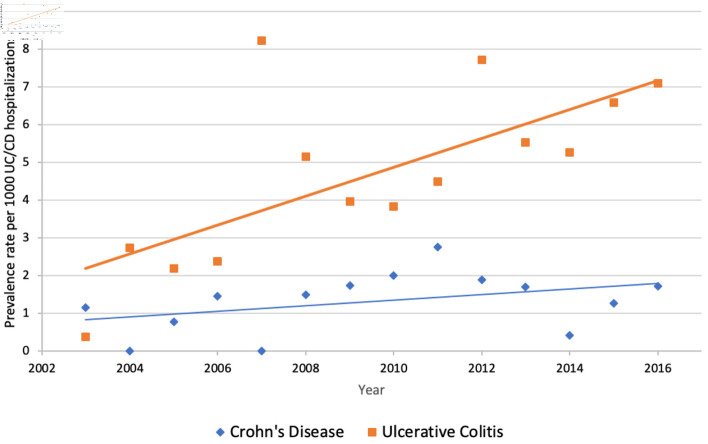
During the study period between 2003 and 2016, there were 254,839 IBD hospitalizations. The overall prevalence rate of CMV infection in IBD patients was 0.3% (680 patients). The prevalence rate of CMV infection increased from 0.89 per 1,000 IBD hospitalizations to 3.8 per 1,000 hospitalizations in 2016, P < 0.001 (Fig. 1). Of the IBD hospitalizations with CMV infection, majority had UC (69%). UC was associated with almost 3.6 times increased risk concomitant CMV infection (OR: 3.66, CI: 3.11 to 4.31, P < 0.001). The prevalence rate of CMV infection among UC increased from 0.3 per 1,000 UC hospitalizations in 2003 to 7.1 per 1,000 UC hospitalizations in 2016, P < 0.001 (Fig. 2). Similar overall uptrend in the prevalence of CMV infection was observed among pediatric patients with CD, P < 0.01 (Fig. 2). IBD hospitalizations with CMV infections corelated with a younger age (14.9 vs. 15.6 years) (Table 1). However, after adjusting for other factors, age was not significantly associated with CMV infection in the IBD population. Female gender had increased risk of CMV infections (adjusted odds ratio (aOR): 1.28, CI: 1.1 to 1.5, P < 0.001). Similarly, Hispanic ethnicity had significant association (aOR: 1.85, CI: 1.46 to 2.34, P < 0.001) with CMV infection when compared to Caucasians, P < 0.001. Univariate analysis (Table 1) showed that IBD patients with a CMV infection had more hospitalizations with comorbid conditions. There was no significant difference in IBD-related abdominal surgeries between the groups, P = 0.24. After adjusting for various comorbid conditions and severity of IBD, hospitalizations with concomitant CMV infection were associated with 3.5 times increased odds of in-hospital mortality. Similarly, CMV infection positively correlated with an increasing degree of severity of IBD (Table 2). When compared to IBD with low severity, severe IBD and intermediate severity had 3.3 times and 2.4 times increased risk of CMV infection respectively (Table.2). On sub-analysis based on the disease type (UC and CD), we found a similar significant association with mortality and disease severity (Table 3). CMV-related IBD hospitalizations had increased length of stay by 9 days while incurring almost $65,000 higher hospitalization charges (Table 2). On sub-analysis, the risk of CMV associated in-hospital mortality was higher for CD patients than for UC patients (aOR: 4.26 vs. 2.87). Further, UC patients with CMV infection had prolonged hospitalization stay over CD patients (11 days vs. 4 days), described in Table 3. Full model of multivariate regression analyses was included here (Supplementary Materials 2-4, www.gastrores.org).
Figure 1.
Prevalence of cytomegalovirus (CMV) infection-related hospitalization among inflammatory bowel disease (IBD) patients between 2003 and 2016. IBD: inflammatory bowel disease; CMV: cytomegalovirus.
Figure 2.
Prevalence of cytomegalovirus (CMV) infection among ulcerative colitis and Crohn’s disease patients between 2003 and 2016. CD: Crohn’s disease; UC: ulcerative colitis.
Table 1. Univariate Analysis Comparing Demographics, Associated Diseases, and Severity of Disease Between IBD Patients With and Without CMV Infection.
| Parameters | IBD with CMV infection | IBD without CMV infection | P value |
|---|---|---|---|
| Age | 14.92 ± 4.5 | 15.6 ± 3.9 | < 0.001 |
| Gender | |||
| Male | 309 (45.5%) | 127,643 (50.3%) | 0.01 |
| Female | 370 (54.5%) | 126,363 (49.7%) | |
| Race | |||
| Caucasian | 341 (50.1%) | 148,564 (58.3%) | < 0.001 |
| Black | 79 (11.6%) | 29,880 (11.7%) | |
| Hispanics | 99 (14.6%) | 21,109 (8.3%) | |
| Others | 161 (23.7%) | 55,287 (21.7%) | |
| Insurance | |||
| Public | 197 (29%) | 67,000 (26.3%) | 0.01 |
| Private | 411 (60.4%) | 166,347 (65.3%) | |
| Self-Pay/uninsured/others | 72 (10.6%) | 21,492 (8.4%) | |
| Hospital bed size | |||
| Small | 74 (11.1%) | 28,435 (11.3%) | < 0.001 |
| Medium | 97 (14.5%) | 59,505 (23.6%) | |
| Large | 497 (74.4%) | 164,056 (65.1%) | |
| Admission type | |||
| Elective | 94 (13.9%) | 50,835 (20%) | < 0.001 |
| Nonelective | 584 (86.1%) | 202,882 (80%) | |
| Primary immunodeficiency disorders | 24 (3.5%) | 1,640 (0.6%) | < 0.001 |
| Human immunodeficiency virus infection | 11 (1.6%) | 78 (< 0.1%) | < 0.001 |
| Malignancy | 40 (5.9%) | 2,265 (0.9%) | < 0.001 |
| Transplant status | 102 (15%) | 2,006 (0.8%) | < 0.001 |
| IBD surgeries | 62 (9.1%) | 26,906 (10.6%) | 0.24 |
| IBD severity | |||
| Low | 293 (43.1%) | 174,597 (68.5%) | < 0.001 |
| Intermediate | 316 (46.5%) | 68,101 (26.7%) | |
| Severe | 71 (10.4%) | 12,141 (4.8%) | |
| Mortality | 12 (1.8%) | 335 (0.1%) | < 0.001 |
| Length of stay | 17.8 ± 1.2 | 5.8 ± 0.01 | < 0.001 |
| Total hospitalization charges | 125,701 ± 7,239 | 37,405 ± 137 | < 0.001 |
IBD: inflammatory bowel disease; CMV: cytomegalovirus.
Table 2. Multivariate Analysis Evaluating the Impact of CMV Infection on the Outcomes of Severe Disease, Mortality, Length of Stay and Total Hospitalization Charges Among All Patients With IBD.
| Parameters | Adjusted odds ratio | 95% CI | P value |
|---|---|---|---|
| In-hospital mortalitya | 3.58 | 1.85 - 6.93 | < 0.001 |
| IBD severitya | |||
| Low | Reference | ||
| Intermediate | 2.48 | 2.11 - 2.93 | < 0.001 |
| Severe | 3.31 | 2.54 - 4.32 | < 0.001 |
| Average difference | 95% CI | P value | |
| Length of stay (in days)b | 9.57 | 9.01 - 10.14 | < 0.001 |
| Total hospitalization costsc | $64,972 | $59794 - $70,150 | < 0.001 |
| Parameters | Average difference | 95% CI | P value |
|---|---|---|---|
| Length of stay (in days)b | 9.57 | 9.01 - 10.14 | < 0.001 |
| Total hospitalization costsc | $64,972 | $59794 - $70,150 | < 0.001 |
aRefer to Supplementary Material 2 (www.gastrores.org) for a full model of multivariate logistic regression analysis. bRefer to Supplementary Material 3 (www.gastrores.org) for a full model of multivariate linear regression analysis. cRefer to Supplementary Material 4 (www.gastrores.org) for a full model of multivariate linear regression analysis. IBD: inflammatory bowel disease; CMV: cytomegalovirus; CI: confidence interval.
Table 3. Multivariate Analysis Evaluating the Impact of CMV Infection on the Outcomes of Severe Disease, Mortality, Length of Stay and Total Hospitalization Charges Among All Patients With Ulcerative Colitis and Crohn’s Disease.
| Parameters | Ulcerative colitis |
Crohn’s disease |
||
|---|---|---|---|---|
| Adjusted odds ratio (95% CI) | P value | Adjusted odds ratio (95% CI) | P value | |
| In-hospital mortality | 2.87 (1.36 - 6.06) | 0.005 | 4.26 (1.14 - 15.86) | 0.03 |
| IBD severity | ||||
| Low | Reference | Reference | ||
| Intermediate | 2.27 (1.86 - 2.76) | < 0.001 | 2.35 (1.77 - 3.10) | P < 0.001 |
| Severe | 3.38 (2.49 - 4.60) | < 0.001 | 2.08 (1.20 - 3.60) | P < 0.01 |
| Average difference | P value | Average difference | P value | |
| Length of stay (in days) | 11.71 (10.96 - 12.45) | < 0.001 | 3.97 (3.04 - 4.89) | < 0.001 |
| Total hospitalization costs | $61,304 (54,397 - 68,211) | < 0.001 | $64,157 (55,499 - 72,815) | < 0.001 |
IBD: inflammatory bowel disease; CMV: cytomegalovirus; CI: confidence interval.
Discussion
Our large database study demonstrates an increasing prevalence of CMV infection among pediatric patients with IBD. Our investigation validated the significant association of CMV infection with increasing severity of the disease leading to prolonged hospital stay and incurring higher hospitalization charges among pediatric IBD patients.
CMV infection can manifest in three different ways in patients with IBD: 1) CMV disease without intestinal involvement, which can occur as a primary infection as well as in reactivation; 2) CMV colitis with or without systemic signs; and 3) intestinal CMV infection with only histologic stigmata of local CMV reactivation without any local or systemic signs [4]. The prevalence rate of CMV infection among IBD-related hospitalizations is 0.89 to 3.2 per 1,000 IBD among pediatric patients. Among UC-related hospitalizations, the increase in prevalence rate is even more profound, increasing from 0.38 to 7.1 per 1,000 hospitalizations. A similar increasing trend of CMV infection was noted among adult UC patients in the USA, with the prevalence rate increasing from 1.4 to 6.3 per 1,000 hospitalizations and 0.3 to 1.8 per 1,000 CD-related hospitalizations between 1998 and 2014 [8]. There are very limited data on the prevalence of CMV infection among pediatric IBD patients. Most data on pediatric patients are case series or studies limited by smaller sample sizes and involving only severe colitis patients [24-27]. Whether this increased prevalence of CMV infection in both adult and pediatric patients is related to increased awareness and testing for CMV by physicians or due to an actual increase in CMV infection rate secondary to use of various immunomodulators and/or biologics is unclear.
In our study, the majority proportion of CMV infection occurred in patients with underlying UC in contrast to CD (69% vs. 31%). This increased prevalence of CMV among UC patients has been well documented in adult studies [8, 28-31]. Increased levels of tumor necrosis factor (TNF)-alpha has been believed to play a crucial role in the reactivation of latent CMV infection and thought to help in the macrophage and other permissive cells such as mucosal epithelial cells, dendritic cells, vascular endothelial cells leading to increased CMV replication in these cells. By contrast, CD elicits a type 1 hypersensitivity reaction leading to increased interferon (IFN)-gamma expression, which could suppress CMV reactivation, leading to decreased prevalence of CMV reactivation in patients with CD [32]. Unlike in adults, most patients in pediatrics are likely to have primary CMV infection rather than reactivation of latent infection, which makes the argument about a possible a different immune interaction that could make UC patients more prone for CMV infection.
The mortality rate among children is very low in our study with an overall in-hospital mortality among IBD-related hospitalizations of 0.13% (347 deaths). After adjusting for various risk factors of CMV infection and severity of IBD, we found that CMV infection is associated with 3.5 times increased odds of associated in-hospital mortality (OR: 3.58; CI: 1.85 to 6.93, P < 0.001). Our results are in agreement with similar adult studies demonstrating IBD patients with CMV have a 2.5 to 7 times increased odds of in-hospital mortality [12, 20]. We also report a significant association of CMV infection with severity of IBD, length of hospital stay, and total hospitalization charges. Our results showed increasing odds of associated CMV infection with a worsening degree of IBD. IBD-related hospitalizations associated with severe disease are 3 times more likely to have CMV infection than those hospitalized with IBD of lower severity. Our results are consistent with those studies in children and adults demonstrating an increased prevalence of CMV infection in patients with acute, severe as well as steroid-resistant colitis [6, 8, 21, 26, 33]. Despite these strong associations, there is still an ongoing debate about the causality of severe colitis by CMV infection or if CMV is an innocent bystander in the severely inflamed colonic mucosa. A meta-analysis in adult patients with IBD showed no significant association of antiviral treatment with improved outcomes among patients with CMV-positive UC [34]. On the contrary, some studies have suggested that antivirals may be of benefit in patients with CMV infection associated with steroid-resistant UC [35-38]. Thus, CMV associated severe colitis continues to be a management dilemma regarding the use of antiviral therapies.
In our study, we did not find any significant association between CMV and IBD-related surgeries during the same hospitalizations (P = 0.24). A recent multicenter European study evaluating the effect of CMV on pediatric IBD demonstrated no difference in the requirement for colectomy during the initial hospitalization between CMV-positive and -negative patients admitted with severe acute colitis (P = 0.17) [27]. Although they had a smaller sample size, during their 12-month follow-up period, CMV-positive patients required more colectomy than their counterparts (P = 0.049) [27]. A similar population-based study in adults showed that CMV infection was associated with 2.5 times increased risk of colectomy among UC patients, but no significant association was noted in CD patients (P = 0.60) [8].
Our study has various limitations which are inherent to large retrospective database analyses. We rely on the diagnostic codes to categorize IBD and CMV infections, and manual coding errors need to be considered while interpreting the results. ICD-9 has only one code for CMV disease or infection and does not classify the different systems involved. Although CMV typically affects the gastrointestinal tract and causes colitis in IBD patients, the lack of a specific ICD code is a limitation. Further, we performed a subanalysis of last quarter of 2015 and 2016 both of which employed ICD-10 and had specific ICD codes for organ-specific CMV infection. We did not find any patients with CMV pneumonitis, hepatitis or pancreatitis, thus indirectly suggesting that majority of infections are likely related to the gastrointestinal system in IBD patients as suggested in prior studies [4-6]. Here, we cannot ascertain the causal relationship between IBD and CMV infection. Our study does not answer the questions whether severe colitis predisposed to CMV infection or CMV infection resulted in severe colitis in IBD patients. The modalities used for diagnosis of CMV infection such as polymerase chain reaction (PCR) (quantitative or qualitative) or immunohistochemistry staining, are not coded and hence not available for analysis and interpretation. Similarly, we do not have data on pharmacological interventions of IBD such as the dosage and duration of corticosteroids, immunomodulators, and biologic therapies which could potentially alter the predisposition and course of CMV infection. Further, the treatment of CMV with antivirals and its impact on clinical outcomes were not analyzed due to lack of data. Although the lack of medication data precluded us from doing predictive analysis, our results are still valid as they rely on the coding for CMV infection. Longitudinal data on patients with CMV and the requirement of surgery were not analyzed due to lack of data on follow-up and readmissions. Despite these limitations, our study highlights various important facts. To our knowledge, this is the largest population-based study evaluating the risk of CMV infection among pediatric IBD patients. Both the NIS and KID provide a large number of pediatric patients with IBD and CMV infection, which is otherwise difficult to achieve from single or multicenter studies and allowed us to control for other risk factors of CMV infection in pediatric IBD patients.
Conclusions
In the past two decades, the prevalence of CMV infection has been increasing among pediatric IBD-related hospitalizations. CMV infection is associated with higher mortality, increased severity of IBD leading to accruing health care resource utilization. Our study findings strengthen the evidence-based recommendations to evaluate for CMV colitis in all pediatric IBD patients hospitalized with severe disease. The increasing prevalence of IBD may put patients at increased risk of CMV infection. Further studies are required to understand better understand the factors influencing this rising trend.
Learning points
CMV infection is associated with severe colitis in pediatric IBD patients. Prevalence of CMV infection is increasing in both pediatric UC and CD patients. CMV infection is associated with increased risk of mortality and severity of the disease. CMV infection significantly corelated with prolonged hospital stay and increased hospitalization charges.
Supplementary Material
Factors used for determining severity and stratification scores.
Multivariate logistic regression analysis of various factors associated with CMV infection in IBD-related hospitalizations.
Multivariate linear regression analysis for length of stay in IBD patients with CMV infection.
Multivariate linear regression analysis for total hospitalization charges in IBD patients with CMV infection.
Acknowledgments
None to declare.
Financial Disclosure
No funding was obtained for this study.
Conflict of Interest
Aravind Thavamani, Krishna Kishore Umapathi and Senthilkumar Sankararaman declare no conflict of interest. Thomas J. Sferra is a consultant for Best Doctors INC.
Informed Consent
Not applicable for this study as this is a database study using deidentified patient information.
Author Contributions
Aravind Thavamani (AT) conceptualization of the idea, data collection, analysis, interpretation, manuscript drafting and revision. Krishna Kishore Umapathi (KKU): data collection, analysis, interpretation of results, and drafting manuscript. Thomas J. Sferra (TJS): supervision of manuscript, data interpretation of results, and revision of manuscript. Senthilkumar Sankararaman (SS): conceptualization of the idea and methodology, interpretation of results, manuscript drafting and revision. All authors approved the final version of the draft for submission.
Data Availability
We have used publicly available database for this analysis. Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
References
- 1.Sager K, Alam S, Bond A, Chinnappan L, Probert CS. Review article: cytomegalovirus and inflammatory bowel disease. Aliment Pharmacol Ther. 2015;41(8):725–733. doi: 10.1111/apt.13124. [DOI] [PubMed] [Google Scholar]
- 2.Dieterich DT, Rahmin M. Cytomegalovirus colitis in AIDS: presentation in 44 patients and a review of the literature. J Acquir Immune Defic Syndr. 1991;(Suppl 1):S29–S35. [PubMed] [Google Scholar]
- 3.Yoshikawa T. Significance of human herpesviruses to transplant recipients. Curr Opin Infect Dis. 2003;16(6):601–606. doi: 10.1097/00001432-200312000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Pillet S, Pozzetto B, Jarlot C, Paul S, Roblin X. Management of cytomegalovirus infection in inflammatory bowel diseases. Dig Liver Dis. 2012;44(7):541–548. doi: 10.1016/j.dld.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 5.Hommes DW, Sterringa G, van Deventer SJ, Tytgat GN, Weel J. The pathogenicity of cytomegalovirus in inflammatory bowel disease: a systematic review and evidence-based recommendations for future research. Inflamm Bowel Dis. 2004;10(3):245–250. doi: 10.1097/00054725-200405000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Garrido E, Carrera E, Manzano R, Lopez-Sanroman A. Clinical significance of cytomegalovirus infection in patients with inflammatory bowel disease. World J Gastroenterol. 2013;19(1):17–25. doi: 10.3748/wjg.v19.i1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayre K, Warren BF, Jeffery K, Travis SP. The role of CMV in steroid-resistant ulcerative colitis: A systematic review. J Crohns Colitis. 2009;3(3):141–148. doi: 10.1016/j.crohns.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Hendler SA, Barber GE, Okafor PN, Chang MS, Limsui D, Limketkai BN. Cytomegalovirus infection is associated with worse outcomes in inflammatory bowel disease hospitalizations nationwide. Int J Colorectal Dis. 2020;35(5):897–903. doi: 10.1007/s00384-020-03536-8. [DOI] [PubMed] [Google Scholar]
- 9.Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R. et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–2778. doi: 10.1016/S0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- 10.Coward S, Clement F, Benchimol EI, Bernstein CN, Avina-Zubieta JA, Bitton A, Carroll MW. et al. Past and future burden of inflammatory bowel diseases based on modeling of population-based data. Gastroenterology. 2019;156(5):1345–1353.e1344. doi: 10.1053/j.gastro.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Mourad FH, Hashash JG, Kariyawasam VC, Leong RW. Ulcerative Colitis and Cytomegalovirus Infection: From A to Z. J Crohns Colitis. 2020;14(8):1162–1171. doi: 10.1093/ecco-jcc/jjaa036. [DOI] [PubMed] [Google Scholar]
- 12.Hradsky O, Copova I, Zarubova K, Durilova M, Nevoral J, Maminak M, Hubacek P. et al. Seroprevalence of Epstein-Barr virus, cytomegalovirus, and polyomaviruses in children with inflammatory bowel disease. Dig Dis Sci. 2015;60(11):3399–3407. doi: 10.1007/s10620-015-3764-z. [DOI] [PubMed] [Google Scholar]
- 13.Domenech E, Vega R, Ojanguren I, Hernandez A, Garcia-Planella E, Bernal I, Rosinach M. et al. Cytomegalovirus infection in ulcerative colitis: a prospective, comparative study on prevalence and diagnostic strategy. Inflamm Bowel Dis. 2008;14(10):1373–1379. doi: 10.1002/ibd.20498. [DOI] [PubMed] [Google Scholar]
- 14.Yerushalmy-Feler A, Kern-Isaacs S, Cohen S. CMV infection in pediatric IBD. Curr Gastroenterol Rep. 2018;20(4):13. doi: 10.1007/s11894-018-0617-x. [DOI] [PubMed] [Google Scholar]
- 15.Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019;114(3):384–413. doi: 10.14309/ajg.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 16.Turner D, Travis SP, Griffiths AM, Ruemmele FM, Levine A, Benchimol EI, Dubinsky M. et al. Consensus for managing acute severe ulcerative colitis in children: a systematic review and joint statement from ECCO, ESPGHAN, and the Porto IBD Working Group of ESPGHAN. Am J Gastroenterol. 2011;106(4):574–588. doi: 10.1038/ajg.2010.481. [DOI] [PubMed] [Google Scholar]
- 17.Yi F, Zhao J, Luckheeram RV, Lei Y, Wang C, Huang S, Song L. et al. The prevalence and risk factors of cytomegalovirus infection in inflammatory bowel disease in Wuhan, Central China. Virol J. 2013;10:43. doi: 10.1186/1743-422X-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ardura MI, Toussi SS, Siegel JD, Lu Y, Bousvaros A, Crandall W. NASPGHAN clinical report: surveillance, diagnosis, and prevention of infectious diseases in pediatric patients with inflammatory bowel disease receiving tumor necrosis factor-alpha inhibitors. J Pediatr Gastroenterol Nutr. 2016;63(1):130–155. doi: 10.1097/MPG.0000000000001188. [DOI] [PubMed] [Google Scholar]
- 19.Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A novel risk score to stratify severity of Crohn's disease hospitalizations. Am J Gastroenterol. 2010;105(8):1799–1807. doi: 10.1038/ajg.2010.105. [DOI] [PubMed] [Google Scholar]
- 20.Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. Simple score to identify colectomy risk in ulcerative colitis hospitalizations. Inflamm Bowel Dis. 2010;16(9):1532–1540. doi: 10.1002/ibd.21225. [DOI] [PubMed] [Google Scholar]
- 21.Zhang C, Krishna SG, Hinton A, Arsenescu R, Levine EJ, Conwell DL. Cytomegalovirus-related hospitalization is associated with adverse outcomes and increased health-care resource utilization in inflammatory bowel Disease. Clin Transl Gastroenterol. 2016;7(3):e150. doi: 10.1038/ctg.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg. 2011;15(2):267–276. doi: 10.1007/s11605-010-1396-3. [DOI] [PubMed] [Google Scholar]
- 23.Ananthakrishnan AN, McGinley EL, Saeian K, Binion DG. Temporal trends in disease outcomes related to Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17(4):976–983. doi: 10.1002/ibd.21457. [DOI] [PubMed] [Google Scholar]
- 24.Cakir M, Ersoz S, Akbulut UE. Disseminated cytomegalovirus infection and protein losing enteropathy as presenting feature of pediatric patient with Crohn's disease. Pediatr Gastroenterol Hepatol Nutr. 2015;18(1):60–65. doi: 10.5223/pghn.2015.18.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drouin E, Seidman E, Russo P, Deslandres C. Gastrointestinal cytomegalovirus infection complicating Crohn's disease in an adolescent without AIDS. J Pediatr Gastroenterol Nutr. 1997;25(2):210–213. doi: 10.1097/00005176-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Ghidini B, Bellaiche M, Berrebi D, Viala J, Hugot JP, Mougenot JF, Munck A. et al. Cytomegalovirus colitis in children with inflammatory bowel disease. Gut. 2006;55(4):582–583. doi: 10.1136/gut.2005.086736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen S, Martinez-Vinson C, Aloi M, Turner D, Assa A, de Ridder L, Wolters VM. et al. Cytomegalovirus infection in pediatric severe ulcerative colitis-a multicenter study from the pediatric inflammatory bowel disease Porto group of the European society of pediatric gastroenterology, Hepatology and Nutrition. Pediatr Infect Dis J. 2018;37(3):197–201. doi: 10.1097/INF.0000000000001724. [DOI] [PubMed] [Google Scholar]
- 28.Nakase H, Yoshino T, Honzawa Y, Chiba T. Low prevalence of CMV infection in patients with Crohn's disease in comparison with ulcerative colitis: effect of different immune response on prevalence of CMV infection. Dig Dis Sci. 2010;55(5):1498–1499. doi: 10.1007/s10620-010-1162-0. [DOI] [PubMed] [Google Scholar]
- 29.Cottone M, Pietrosi G, Martorana G, Casa A, Pecoraro G, Oliva L, Orlando A. et al. Prevalence of cytomegalovirus infection in severe refractory ulcerative and Crohn's colitis. Am J Gastroenterol. 2001;96(3):773–775. doi: 10.1111/j.1572-0241.2001.03620.x. [DOI] [PubMed] [Google Scholar]
- 30.Roblin X, Pillet S, Berthelot P, Del Tedesco E, Phelip JM, Chambonniere ML, Peyrin-Biroulet L. et al. Prevalence of cytomegalovirus infection in steroid-refractory Crohn's disease. Inflamm Bowel Dis. 2012;18(7):E1396–1397. doi: 10.1002/ibd.21907. [DOI] [PubMed] [Google Scholar]
- 31.Siegmund B. Cytomegalovirus infection associated with inflammatory bowel disease. Lancet Gastroenterol Hepatol. 2017;2(5):369–376. doi: 10.1016/S2468-1253(16)30159-5. [DOI] [PubMed] [Google Scholar]
- 32.Nakase H, Chiba T. TNF-alpha is an important pathogenic factor contributing to reactivation of cytomegalovirus in inflamed mucosa of colon in patients with ulcerative colitis: lesson from clinical experience. Inflamm Bowel Dis. 2010;16(4):550–551. doi: 10.1002/ibd.21047. [DOI] [PubMed] [Google Scholar]
- 33.Papadakis KA, Tung JK, Binder SW, Kam LY, Abreu MT, Targan SR, Vasiliauskas EA. Outcome of cytomegalovirus infections in patients with inflammatory bowel disease. Am J Gastroenterol. 2001;96(7):2137–2142. doi: 10.1111/j.1572-0241.2001.03949.x. [DOI] [PubMed] [Google Scholar]
- 34.Kopylov U, Eliakim-Raz N, Szilagy A, Seidman E, Ben-Horin S, Katz L. Antiviral therapy in cytomegalovirus-positive ulcerative colitis: a systematic review and meta-analysis. World J Gastroenterol. 2014;20(10):2695–2703. doi: 10.3748/wjg.v20.i10.2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones A, McCurdy JD, Loftus EV Jr, Bruining DH, Enders FT, Killian JM, Smyrk TC. Effects of antiviral therapy for patients with inflammatory bowel disease and a positive intestinal biopsy for cytomegalovirus. Clin Gastroenterol Hepatol. 2015;13(5):949–955. doi: 10.1016/j.cgh.2014.09.042. [DOI] [PubMed] [Google Scholar]
- 36.Maconi G, Lombardini M, Furfaro F, Bezzio C, Zerbi P, Ardizzone S. Long-term outcome of inflammatory bowel diseases with cytomegalovirus colitis: effect of antiviral treatment. Eur J Gastroenterol Hepatol. 2014;26(10):1146–1151. doi: 10.1097/MEG.0000000000000175. [DOI] [PubMed] [Google Scholar]
- 37.Pillet S, Pozzetto B, Roblin X. Cytomegalovirus and ulcerative colitis: Place of antiviral therapy. World J Gastroenterol. 2016;22(6):2030–2045. doi: 10.3748/wjg.v22.i6.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shukla T, Singh S, Loftus EV Jr, Bruining DH, McCurdy JD. Antiviral therapy in steroid-refractory ulcerative colitis with cytomegalovirus: systematic review and meta-analysis. Inflamm Bowel Dis. 2015;21(11):2718–2725. doi: 10.1097/MIB.0000000000000489. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Factors used for determining severity and stratification scores.
Multivariate logistic regression analysis of various factors associated with CMV infection in IBD-related hospitalizations.
Multivariate linear regression analysis for length of stay in IBD patients with CMV infection.
Multivariate linear regression analysis for total hospitalization charges in IBD patients with CMV infection.
Data Availability Statement
We have used publicly available database for this analysis. Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.