Abstract
Background:
Entering neurosurgical training in the United Kingdom demands extensive prior commitment and achievement, despite little to no exposure to the specialty in medical school. Conferences run by student “neuro-societies” offer a means to bridge this gap. This paper describes one student-led neuro-society’s experience of curating a 1-day national neurosurgical conference supported by our neurosurgical department.
Methods:
A pre-and post-conference survey was distributed to attendees to ascertain baseline opinions and conference impact using a five-point Likert Scale, and free text questions explored medical students’ opinions of neurosurgery and neurosurgical training. The conference offered four lectures and three workshops; the latter provided practical skills and networking opportunities. There were also 11 posters displayed throughout the day.
Results:
47 medical students participated in our study. Post-conference, participants were more likely to understand what a neurosurgical career involves and how to secure training. They also reported increased knowledge about neurosurgery research, electives, audits, and project opportunities. Respondents enjoyed the workshops provided and suggested the inclusion of more female speakers in future.
Conclusion:
Neurosurgical conferences organized by student neuro-societies successfully address the gap between a lack of neurosurgery exposure and a competitive training selection. These events give medical students an initial understanding of a neurosurgical career through lectures and practical workshops; attendees also gain insight into attaining relevant achievements and have an opportunity to present research. Student neuro-society-organized conferences have the potential to be adopted internationally and used as a tool to educate on a global level and greatly aid medical students who are aspiring neurosurgeons.
Keywords: Medical education, Medical school, Neuro society, Neurosurgery conference, Undergraduate

INTRODUCTION
Exposure to different clinical specialties is crucial for medical students as they consider their career paths and make informed decisions about their future training and residency.[29,30] This is especially true in the UK, where formal clinical experience is often required for selection into training programs. Medical schools worldwide have adopted a generalist approach, with a theory-based curriculum interspersed with clinical placements.[21] However, the broad scope of medicine makes it challenging for students to rotate through all specialties during their time in medical school. Some universities, such as the University of Glasgow, allocate a limited amount of time for neurosurgery in their mandatory curriculum, with students spending a maximum of 12 days in the neurosurgical department over 5 years. This limited exposure to neurosurgery can be attributed to various factors, including political pressures to address specific healthcare issues within a country, as in the UK, where medical education is evolving to address the shortage of general practitioners. [21] As a result, increasing exposure to neurosurgery within a compacted curriculum can be difficult.[21,32]
Candidates typically apply for neurosurgical training in the middle of the 2nd year of the 2-year UK Foundation program, which is required for all British medical school graduates. This program serves as a bridge between medical school and specialty training and is roughly equivalent to the internship or house job position in North America and Asia. It allows newly qualified doctors to rotate through six specialties, each lasting 4 months. These rotations typically include mandatory time in general medicine and general surgery but also offer some flexibility for elective rotations, such as neurosurgery. During an elective neurosurgery rotation, doctors work at the intern level in a neurosurgical center.
In the United Kingdom, the national neurosurgical recruitment team works closely with the Yorkshire and Humber deanery to select the best candidates for the training positions. The process requires input from many UK consultant The process requires input from many UK consultant neurosurgeons to help score each candidate.
To be shortlisted for an interview, candidates must demonstrate a strong portfolio of achievements.[26] The portfolio is scored using a matrix that includes various domains, including research publications, national and international presentations, and the completion of higher research degrees such as a PhD. Credit is also given for formal teaching roles, audit and quality improvement projects, leadership positions, and postgraduate exams.[26] The top candidates are invited to interview to assess their skills further. Successful candidates are then allocated a “national training number,” which allows them to enter a neurosurgical training program within a particular geographical region.
Deaneries (groups responsible for ensuring the quality of training) representing specific geographical areas and Training Programme Directors oversee the allocation of training positions to hospitals within their jurisdiction. For example, the Scottish deanery is responsible for allocating neurosurgical training positions to the four neurosurgical centers in Scotland (Glasgow, Edinburgh, Dundee, and Aberdeen).[26]
Deaneries may advertise national training numbers (residency spots) yearly via the “national selection” process.[26] All candidates who make it to the interview rank their preferred training centers. The top-scoring candidate gets their first choice, and the second-highest candidate gets their first choice unless it was the first choice of the top-ranking candidate (in which case they get their second-ranked choice) until all residency spots are allocated in this manner.
In 2022, 255 applicants applied for neurosurgical training.[9] Of these, 56 were invited to interview.[9] Only 16 “national training numbers” were advertised; thus, only the top 16 ranking candidates secured a categorical PGY1 neurosurgical training spot in the UK. With a competition ratio of 1–16, neurosurgical training is the second most competitive specialty in the UK, behind cardiothoracic surgery.[9]
Once a national training number has been achieved, trainees are employed in a neurosurgical residency for 8 years until the completion of their training, at which point they are eligible to apply for attending or consultant jobs. Therefore, those interested in neurosurgery are in training for a minimum of 15 years. This comprises 5 years of medical school at the “undergraduate level”, and the vast majority of the medical schools in the UK offer an undergraduate medical curriculum where applicants are typically 17 or 18-year-olds from high school. This is followed by postgraduate training lasting at least 10 years, including the 2-year foundation program and 8 years of neurosurgical training and 8 years of neurosurgical training, excluding any higher degrees (PhD/MD(res)) or post residency subspeciality fellowships.
The number of training applications for neurosurgery has substantially risen in the last few years with a concomitant reduction in the number of training places. The latter was partly to redress the current workforce concerns highlighted by the British Neurosurgical Workforce Report, where there are over 80 neurosurgeons who have completed their residency, but there is no substantive consultant job for them.[33] This problem is estimated to reach a peak of 100 post-residency neurosurgeons by 2028/2029, according to the report, and is expected to decline after that.[33] This issue is alleviated by trainees committing further training years in research and/or subspecialty fellowships (e.g., vascular, complex spine, skull base), after which consultant posts may be available. Fellows are salaried by individual hospitals and generally tend to earn less than residents, as their focus is elective subspecialty operations, and are typically 2nd on call in the on-call rotas. Most UK trainees, after completing residency stay as fellows until a substantive consultant/ attending appointment is available.
Given the extreme competition for neurosurgical training in the UK and the requirement for a substantial extracurricular portfolio, aspiring neurosurgeons need to begin working on their applications from early medical school. However, guidance in this process is lacking due to the limited exposure to the specialty.[21,32]
One valuable platform for interested medical students to bolster their exposure is attending national conferences conducted by student interest groups.[5,13,16] Such events expose the student to neurosurgery from an early stage and provide significant networking opportunities.[5,13,16,34] They can be an invaluable platform to provide targeted advice to complete various domains of the shortlisting portfolio, providing aspiring medical students with much-needed guidance. In addition, they can give a genuine insight into the life of a neurosurgeon (personal and professional), allowing candidates to make an informed decision.[5,13,16]
Despite their benefit, the literature regarding the impact of conferences organized by medical student run neurosurgical interest groups is sparse. This paper aims to describe the impact of one such conference by the Glasgow Neuro Society - a medical student led society based at the University of Glasgow Medical School. This paper describes the structure of such an event, the lessons learned, and the impact of a student-organized conference on the knowledge, attitudes, and perceptions of medical students toward a neurosurgical career. The role and importance of student-run neurosurgical interest groups are highlighted.
MATERIALS AND METHODS
Study setting and conference program
This study was conducted at the 9th annual Glasgow Neuro International Conference. A 1-day, in-person event was held at the Royal College of Physicians and Surgeons of Glasgow in November 2021. This meeting is predominately attended by medical students who are interested in neurosurgery. A focused conference program incorporating a mix of lectures, workshops, and poster presentations was designed to maximize learning opportunities for delegates. Four lectures were delivered by national and international invited speakers across various neurological domains, including artificial intelligence, clinical and basic research, and advancements within the neurosurgical sphere. Speakers are asked to ensure their lectures are pitched appropriately for medical students.
Workshops were delivered by consultant neurosurgeons and neurosurgical residents local to the University of Glasgow’s Medical School neurosurgical department (Institute of Neurological Sciences, Queen Elizabeth University Hospital Glasgow). These comprised of:
A typical day in the life of a neurosurgeon
How to maximize entry into neurosurgical training
Hands-on intracranial pressure monitoring workshop.
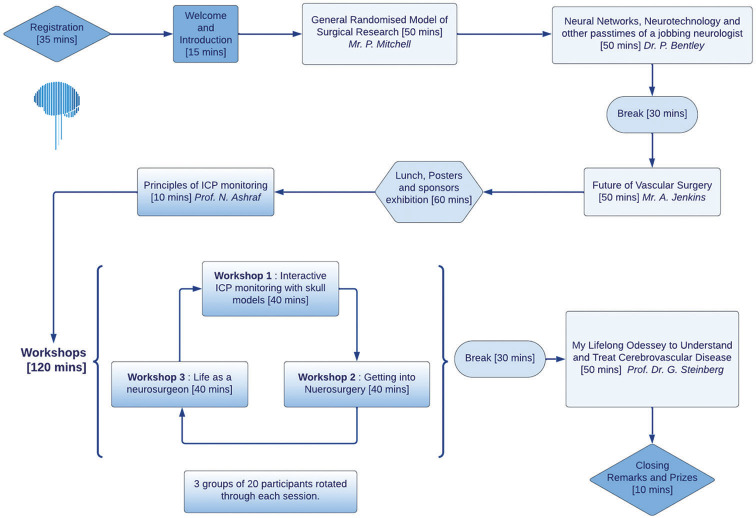
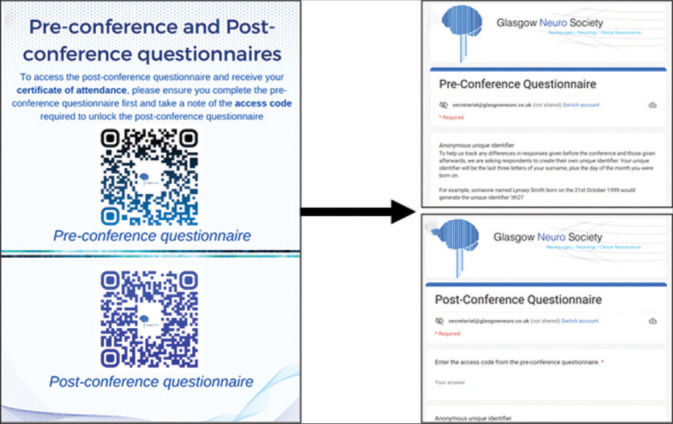
The conference itself was entirely organized by a committee of medical students supported by a consultant neurologist and neurosurgeon. The conference workflow is illustrated in Figure 1.
Figure 1:
Illustrates entire conference workflow and contents and duration of lectures and workshops. Figure design courtesy of coauthor Ameerah Gardee.
In keeping with the primary aim of an in-person conference to promote interpersonal networking, we invited delegates to submit neurosurgical scientific abstracts. From the selection of abstracts submitted for consideration, 11 were selected after blinded peer-reviewed by a consultant neurosurgeon and neurologist. Posters were displayed throughout the day as a conduit to invite conversation between authors, attendees, and trainees/consultants during the break and lunch sessions. Posters were subject to grading by the attending neurosurgical faculty/speakers.
Conference evaluation form
As stipulated by the Federation of the Royal College of Physicians of the United Kingdom, live events, such as this conference, must provide evaluation forms to delegates requesting them to record their rating of the event’s relevance, quality and effectiveness. To meet this requirement, the Glasgow Neuro committee developed a two-part questionnaire to establish delegates’ baseline knowledge and views regarding neurosurgery as a career before the conference and statistically compare with findings after the conference. This was done using an aptly named Pre-Conference questionnaire [Appendix Table A] and Post-conference questionnaire [Appendix Table B] using Google Forms, an open-source platform for creating questionnaires (Google, Mountain View, CA, USA). Both surveys contained identical questions, allowing for direct comparisons of answers for each delegate before and after the event. Questions are shown in Tables 1 and 2. The complete questionnaire is attached as appendixes in supplementary files.
Table 1:
McNamar’s test on pre- and post-conference questions.
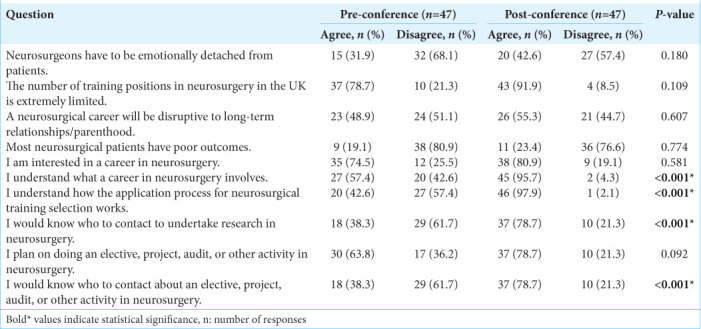
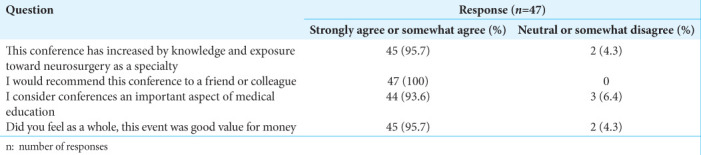
Table 2:
Post-conference questionnaire questions and feedback.
Questions were grouped into three categories:
Questions aimed at collecting demographic information
Questions relating to participants’ perceptions of neurosurgery as a career and the attributes/achievements required for successful application
Questions on participant’s views about the conference.
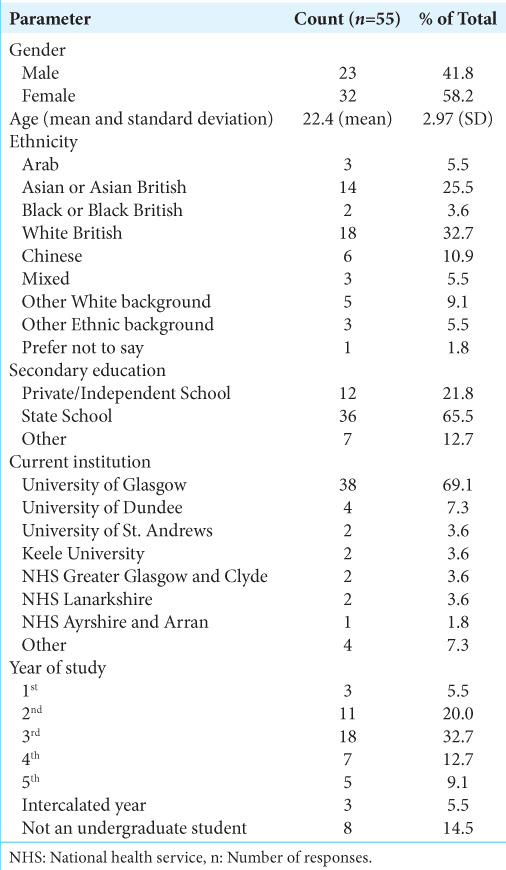
As detailed in Appendix Tables A and B, we utilized a mix of 5-point Likert-type ranking questions (strongly disagree [1], disagree, neither agree nor disagree, agree, strongly agree [5]), and short-text responses within the questionnaire. The reasoning for this was two-fold: using a Likert scale allows for quantitative analysis of answers, whilst free-text questions allow delegates to express opinions freely, which can be qualitatively examined. Before attending the conference, the pre-conference survey was used to determine baseline knowledge, attitudes, and perceptions of neurosurgery. It was distributed as a web link to all delegates through email 1 week before the event. The post-conference survey was advertised using QR codes (a type of barcode which, when scanned by any smartphone, automatically redirects the device to the survey) displayed throughout the conference venue and within the conference brochure distributed to all attendees during the morning registration. This is illustrated in Figure 2.
Figure 2:
QR code system for accessing pre- and post-conference surveys. Scanning the QR code with a smartphone directs the user to the respective survey to complete.
Delegates were sent the survey before the conference and were invited to read an information sheet about this study and indicate their consent to partake. Those who did not complete the survey were invited to do so on the morning of the conference at the registration desk. The survey did not collect any personal information from the delegates, which could be used for identification purposes. To link each delegate’s pre-conference responses with their post-conference answers, a unique identifier consisting of the last three letters of their surname plus the day of the month they were born was the connection between responses.
Statistical analysis
An independent statistician analyzed the results using Statistical Package for Social Science (SPSS) Version 26 developed by IBM (Chicago, IL, USA). To examine any existing relationship between demographics (for example, age, gender, and level of progression through medical school) and opinions/exposure to neurosurgery as a career, information was collected about the attendees, and descriptive data were presented as percentages and means. Likert scale responses were dichotomized such that positive responses (agree and strongly agree) were combined, and neutral or negative responses (disagree and strongly disagree) were combined. Due to the paired nature of the data, McNemar’s test was utilized in SPSS to find statistically significant differences between the pre-and post-conference responses. The results were also stratified by gender to see if there was a difference in the perceptions of male and female medical students. P < 0.05 was considered statistically significant. Thematic analysis was used in the analysis of short-text responses. This method involves identifying, coding, and synthesizing recurring themes within the data, enabling the extraction of meaningful insights. By grouping similar concepts and examining their relationships, key themes were identified that encapsulate the underlying meaning of the responses.
RESULTS
Demographics
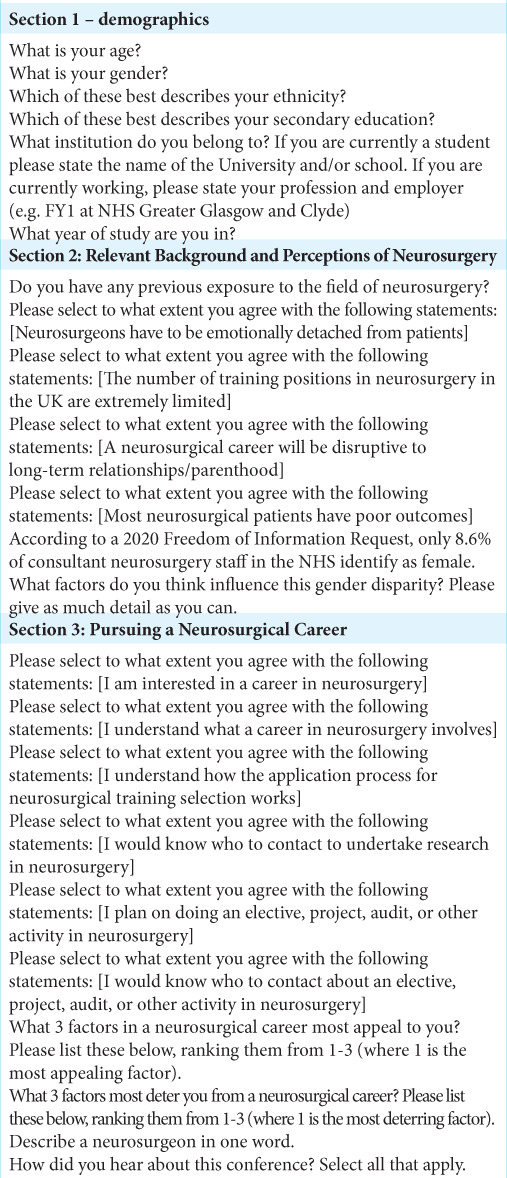
A total of 55 participants completed both the pre-and post-conference surveys, with a 100% response rate. Descriptive statistics are presented in Table 3. The majority of delegates were female (58.2%), identified as White British (32.7%) or Asian/Asian British (25.5%), and attended a state school (65.5%). The mean age of medical student delegates was 22.4 ± 2.97 years. Most participants were from Scottish universities, with 69.1% coming from the University of Glasgow and the remainder coming from the Universities of Dundee, Keele, and St Andrews. Most delegates were in the second (20.0%) or 3rd year (32.7%) of medical school. Eight participants (14.5%) were not undergraduate students and were therefore excluded from further analysis.
Table 3:
Demographic characteristics of delegates.
Impact of the conference
After attending the conference, participants were significantly more likely to agree that they understood what a career in neurosurgery entails compared to before the conference [95.7% vs. 57.4%; P < 0.001; Table 1]. They were also significantly more likely to agree that they understood how the application process for neurosurgical training selection works after attending the conference [97.9% vs. 42.6%; P < 0.001; Table 1]. A significantly greater number of participants also reported that they would know who to contact to undertake research in neurosurgery [78.7% vs. 38.3%; P < 0.001; Table 1] and would be aware of opportunities for electives, projects, audits, or other activities in neurosurgery [78.7% vs. 38.3%; P < 0.001; Table 1] after the conference compared to before the conference. In addition, more students reported that they planned to participate in electives, projects, audits, or other activities in neurosurgery after the conference than before [78.7% vs. 63.8%; P = 0.09; Table 1].
When stratified by gender, males were significantly more likely to agree that a neurosurgical career will be disruptive to long-term relationships/parenthood after attending the conference (77.8%) compared to before the conference (44.4%). Conversely, fewer females agreed to this statement after the conference (41.4%) than before the conference (51.7%); however, this difference was not significant (P = 0.05). These results suggest that females may have a different perception of the potential impact of a career in neurosurgery on personal relationships than males.
Opinions and feedback about the conference
About 95.7% of attendees indicated that the conference increased their knowledge and perception of neurosurgery, with 100% stating that they would recommend such a conference to friends or colleagues. In addition, 93.6% of attendees considered conferences an important aspect of medical education, and 95.7% felt that the event was a good value for money [Table 2].
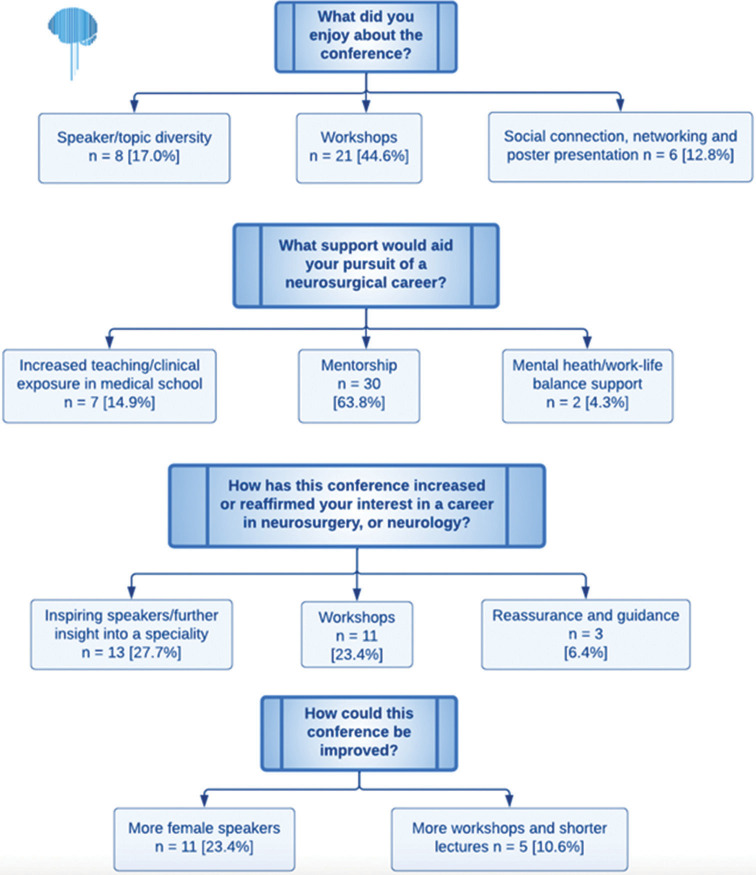
Thematic analysis was performed on the following questions, with the results depicted in Figure 3:
What aspects of the conference did attendees enjoy?
How did the conference increase, strengthen, or reinforce attendees’ interest in neurology or neurosurgery as a future career?
What support do attendees feel they may benefit from in pursuing a neurosurgical career?
Are there any improvements that could be made to future conferences?
Figure 3:
Thematic analysis for the question “what did you enjoy about the conference” in our delegates. Figure design courtesy of coauthor Ameerah Gardee.
Mentorship was identified as the most critical form of support desired by participants in pursuing a neurosurgical career, with 30 attendees citing it as their primary need. Increased clinical exposure and formal teaching on neurosurgery in medical school were also identified as important forms of support (n = 7). Most attendees identified the workshop experience and diversity of speakers and topics as positive aspects (n = 21 and n = 8, respectively). A small number of participants appreciated the poster presentations (n = 3) and the interactive nature of the conference, which facilitated socialization (n = 3). Several attendees suggested the inclusion of more female speakers at future conferences (n = 11), while a few also recommended incorporating additional workshops (n = 3). The inclusion of practical workshops was a novel feature of this conference and will be considered for inclusion in future events.
A qualitative analysis of student perceptions of neurosurgeons revealed that respondents hold a favorable view of neurosurgeons, using terms such as “dedicated,” “driven,” “hero,” “determined,” “meticulous,” and “hardworking” to describe this professional group. These are depicted in Figure 3. Most medical students (68.1%) disagreed with the statement that neurosurgeons must be emotionally detached from their patients, and an even larger proportion (80.9%) rejected the notion that most neurosurgical patients have poor outcomes. Approximately half of the participants (51.1%) agreed that a neurosurgical career might potentially disrupt long-term relationships or parenthood, although this percentage decreased to 44.7% in the post-conference survey.
DISCUSSION
For those seeking to enter neurosurgical training, engaging with the specialty at the medical school level is becoming increasingly important for achieving the subsequent milestones required to secure training, as stipulated by the national selection criteria.[26] This study suggests that neurosurgical conferences may be a useful platform for providing early exposure to neurosurgery. When asked about the support that would benefit them in their journey to obtain a neurosurgical residency, the second most common response was the need for increased neurosurgical clinical exposure and formal teaching at medical school, with the desire for a neurosurgical mentor ranking first. These findings are consistent with contemporary literature but are not being addressed by policymakers and relevant authorities.[5,13,16,34]
As competition for training places increases and the number of available positions decreases, the question becomes how exposure and guidance about neurosurgery and the completion of relevant achievements can be made accessible without formal teaching by medical schools. Medical student-led conferences may serve as a conduit for this. This study shows that delegate understanding of neurosurgery as a career and the application process significantly increased following the conference (57–97.5% and 42.6–97.7%, respectively). While the event program is key to this, it is clear that such events may offer guidance to medical students not available through their medical school programs. However, the importance of a varied itinerary is likely important as well. Glasgow Neuro was fortunate to offer delegates speakers from the UK, the United States, and Asia, representing several subspecialties within neurosurgery. This program facilitated an understanding of the wide scope of neurosurgical practice, despite its increasingly subspecialized nature. In addition, our “Life as a Neurosurgeon” workshop outlined the scope of consultant practice within Scotland and the UK [Figure 1], covering the various roles a neurosurgeon may take on (clinical and administrative), the demands and sacrifices required, and an insight into how the specialty has evolved to become more accommodating. This workshop was beneficial as the advice came from an individual in a position and location where delegates hoped to practice.
Contemporary literature has demonstrated the effectiveness of student-led neurological conferences in enhancing student knowledge of neurosurgical careers. A study by Horan et al.[16] found that a 1-day student-led neurosurgical conference in Ireland resulted in a significant increase in participant knowledge about a career in neurosurgery, from 34% (baseline) to 94% (post-conference).[16] A similar study conducted in London also reported a significant increase in participant understanding, from 38.6% (baseline) to 92.1% (post-conference).[13] These findings suggest that even a short lecture can give delegates a useful baseline understanding of neurosurgery as a career. The literature also suggests that this may also have the secondary effect of fostering further curiosity, although this was not assessed in our survey.[13]
Neurosurgical research also constitutes an integral part of the trainee portfolio. The previous studies, such as that conducted by Horan et al.,[16] have shown that while conferences may increase medical students’ understanding of a neurosurgical career, only a minority of attendees (35%) leave the event confident in their ability to approach someone to pursue neurosurgical research. (source) In contrast, our study found a significant increase in confidence among delegates from baseline to post-conference (38% vs. 79%, respectively). In addition, more delegates (n = 37) reported an intention to complete a neurosurgical elective, project, or audit after the conference compared to before (n = 30), although this did not reach statistical significance. Conference feedback indicated that students rated the “How to Maximize Entry into Neurosurgical Training” workshop highly in providing direction on completing relevant portfolio activities and where to pursue them. This workshop was conducted by a neurosurgical resident who had recently undergone the national selection process. Evidence from the literature supports the benefits of near-peer teaching and mentoring in enhancing student understanding in less formal contexts.[12] Therefore, this paper advocates for a portfolio/resume workshop conducted by recently appointed neurosurgical trainees, as it is believed that students benefit from both the tutor’s recent experience and the reciprocal teaching from a near-peer through the provision of current, practical, and relatable advice.[12]
Student conferences are gaining increasing recognition in the literature as a platform to develop an early researcher’s presentation skills.[5] Presenting at neurosurgical conferences has also been shown to enhance the quality of future research projects and output.[10,20,25] Delegates had the opportunity to have their abstracts published in Surgical Neurology International as part of the conference proceedings.[4] The other advantage of student-run conferences is that they generally operate on a nonprofit model and increase the opportunity for students to present scientific work. Compared to student conferences and training courses, postgraduate conferences often charge hundreds of US$ to attend. A recent UK study highlighted that the average postgraduate will spend between £2735 and £20,780 attending such conferences/courses.[27] When considering factors such as commute and accommodation, traditional postgraduate meetings can reach a cost many medical students may not afford. The conference organized in this paper was a non-profit event, charging GB£25 (US$33) with no further costs to attend the hands-on workshop session. However, the workshops were delivered at a similar level as some basic neurosurgical skills courses at lower costs. For example, the high cost of Rowena heads (realistic models used for teaching in neurosurgical simulation courses) was circumvented by producing low-cost alternative models. This was done using anatomical calvariums, children’s play slime, and waste bags to mimic brain parenchyma and dural puncture, allowing for a relatively accurate simulation of important neurosurgical skills.[3] This was reflected by delegate feedback, with 95.7% of delegates reporting that the conference was good value for money.
In the United Kingdom, it is not uncommon for doctors to work in non-training posts in National Health Service Hospitals for an extended period after completing their foundation program because they could not secure neurosurgical training on their first attempt. These positions are usually at the FY2 (intern) level and do not generally have career progression. Applicants must then apply for a training number/PGY1/ST1 (first year of residency) position in the subsequent year which has inadvertently placed 1st-time applicants at a disadvantage, as they are competing against more experienced candidates who have undertaken these non-training posts for PGY1 positions. Ideally, all aspiring applicants would be able to secure competitive entry into training on their first attempt, but many medical students do not have sufficient exposure to neurosurgery during medical school to prepare them for the national selection process. This study and contemporary literature highlight the important role that student interest groups and student-organized conferences can play in addressing this lack of exposure by providing aspiring applicants with early guidance and the foundation necessary to meet the milestones required for securing a neurosurgical training position.[5,13,16]
A key finding of this paper was medical students’ desire for mentorship in their journey toward a neurosurgical career. Literature suggests mentors can be crucial for professional success, increasing satisfaction, productivity, diversity, and inclusivity.[2,8,11,14,15,17,24] This is not surprising, as many milestones required for obtaining a neurosurgical training number, such as conducting research, often require mentorship. Whilst numerous barriers are identified to successful mentorship,[8,11,14,15,24] Glasgow Neuro Society has informally linked medical students with neurosurgical registrars, often in the context of the latter’s need for human resources to complete research projects. These experiences have been positive for both parties, with the students often gaining authorship on a peer-reviewed publication or conference presentation.
This conference was designed with three main purposes: First, to inspire medical students aspiring to become neurosurgeons, second, to provide them with a knowledge foundation of the reality of life as a neurosurgeon and insight into the specialty and neurosurgical training, and finally, to provide them with targeted advice on preparing early for the neurosurgical training program application with emphasis on research projects, audits, and elective placements, as these make up a large chunk of portfolio points. Overall, the conference was well received, with 94% of delegates believing such conferences are an important part of medical education, and 98% of delegates stated they would recommend our conference to friends or colleagues.
This study has limitations. First, the sample size was relatively small, which may have influenced the statistical significance of some responses. This may be partly due to the restrictions on in-person events imposed by the COVID-19 pandemic. It is worth noting that this conference typically attracts between 100 and 150 delegates annually, indicating its popularity among medical students. Another limitation is that student-led neurosurgical societies and conferences, while providing valuable resources and support for aspiring neurosurgeons, may be influenced by a self-selection bias due to their reliance on funding, support from local medical schools, and the presence of a neurosurgical department. Furthermore, the scope of these societies is limited to addressing gaps in delegate exposure and understanding rather than studying the impact of curricula-based interventions on student interest in neurosurgery. Finally, it is worth acknowledging that the results of this study may be influenced by various factors, such as personal experiences and individual expectations, and should be interpreted with caution.
Whilst conferences appear to be a good solution to promote early exposure to neurosurgery, it is important to acknowledge that alternative avenues exist for increasing student awareness and interest in neurosurgical careers. These include e-modules, student-selected components (self-proposed study blocks in UK medical schools), increased inclusion of neurosurgical teaching/access to the neurosurgical theatre during medical school, and elective clinical or research placements.[6,7,22,23,31] These are long-term initiatives that span the entire duration of medical school, and their role and impact should be further studied.
Finally, we wanted to acknowledge one important and novel education measure form, SNIDigital.[19,28] This platform pioneered by Ausman is the first major neurosurgical journal that has extended its empowerment to medical students through hosting lectures that are not one-way dialogues and panel talks.[19,28] In addition, their “Let’s Talk” series, which is in development, aims to foster cross-generational communication between educators, policymakers, neurosurgeons, and medical students.[28] It is in the process of having its impact evaluated as Ashraf and Ismahel developed the first ‘Lets Talk’- an initiative led by medical students.[28] Similarly, SNIDigital also includes work by Ausman and Hoz, where they already demonstrated the potential of such an initiative and its role in inspiring the next generation of neurosurgeons amongst medical students based on work from Ausman and Hoz involving medical students and Iraq.[1,17-19,28] Initiatives like SNIDigital may then be the ideal solution to our experience [Figure 3] where students are generally less interested in didactic lectures and more desirous of workshops and discussions which are interactive experiences.
CONCLUSION
Medical student-led neurosurgical societies can provide a valuable foundation for students interested in pursuing a career in neurosurgery, helping them to develop the knowledge and skills needed to succeed in this specialized field. Student conferences can also be useful in gathering insights into medical students’ perceptions of neurosurgery and identifying areas where additional support may be needed. Given the importance of early engagement with neurosurgery in preparing for a career, we encourage all interested medical students to consider forming a neurosurgical society at their institution. These societies can serve as a platform for promoting neurosurgery, filling gaps in the curriculum, and attracting motivated and qualified members.
Acknowledgments
Glasgow Neuro Society was set up in 2010 at the University of Glasgow Medical School by then medical student Mr. Allan Hall - a current neurosurgical resident at the Institute of Neurological Science, Queen Elizabeth University Hospital, Glasgow, United Kingdom. The society was fortunate to have the legendary neurosurgeon Sir Professor Graham Teasdale, as its patron-in-chief. Over the last 10 years, the society has extensively grown to be one of the largest organizations representing junior members of the medical profession in the UK, interested in neurology, neurosurgery, and clinical neuroscience. For that, we are grateful to the previous committees for their hard work and dedication to growing Glasgow Neuro. Glasgow Neuro Society would also like to acknowledge the strong support from the neurology and neurosurgery faculty at the Institute of Neurological Sciences in Glasgow and the University of Glasgow Medical School, who have provided guidance and support for our events over the years.
For the 2021 annual conference, we would like to acknowledge the following individuals and organizations without whom our conference would not be possible.
Mr Tony Poutney- Territory Manager for Delta Surgical in Scotland and Northern Ireland. Delta surgical kindly sponsored the intracranial pressure monitoring (ICP) monitoring workshop, providing cranial access kits and ICP bolts.
Guarantors of Brain
BBraun
Oss Designs
Brainlab
Codman/Integra
Wesleyan
Digby Brown Solicitors, Glasgow
John Smith’s Student Store, Glasgow
WILEY Publishers
Renishaw
The Royal College of Surgeons of England
Wolfson School of Medicine, University of Glasgow
APPENDIX TABLE
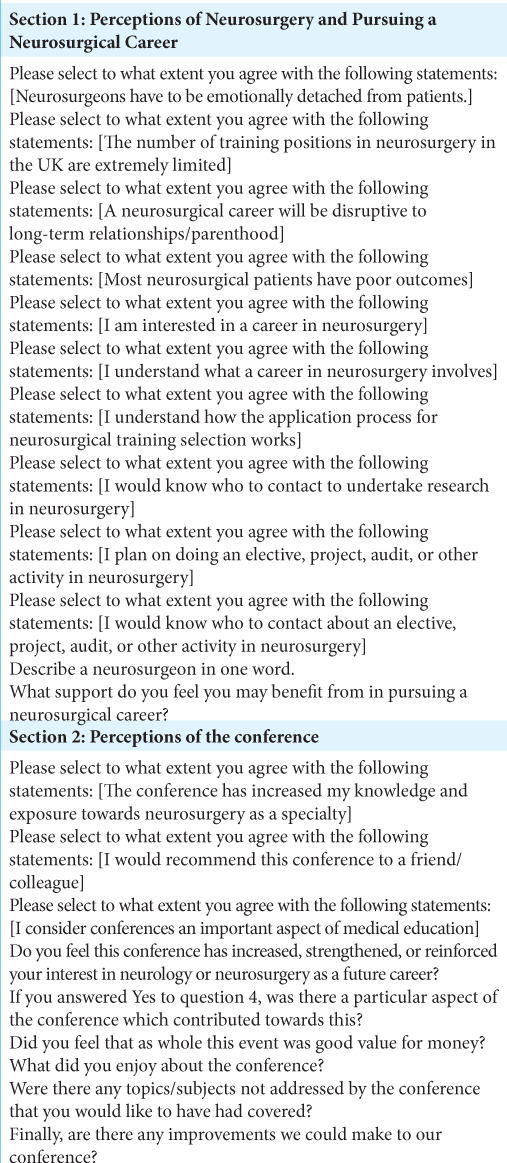
Appendix Table A:
Pre-conference survey. This survey was divided into 3 sections: demographics, relevant background and perceptions of neurosurgery, and pursuing a neurosurgical career. The survey is a combination of free-text questions and Likert-scale questions. Likert scale questions are denoted by [] brackets.
Appendix Table B:
Post-conference survey with two sections. The first section includes questions about perceptions of neurosurgery and pursuing a neurosurgical career, which are identical to those in the pre-conference survey to allow for comparison of responses before and after the conference. The second section explores delegates’ attitudes towards the conference through a combination of free-text and Likert scale questions (denoted by [] brackets)
Footnotes
How to cite this article: Ashraf M, Ismahel H, Lub S, Gardee A, Evans VE, Middleton EE, et al. Role of a medical student neuro-society organized neurosurgical conference: The Glasgow neuro experience. Surg Neurol Int 2023;14:70.
Contributor Information
Mohammad Ashraf, Email: mohammad_5676@hotmail.com.
Hassan Ismahel, Email: hassan.ismahel@gmail.com.
Sytske Lub, Email: sytskelub@hotmail.com.
Ameerah Gardee, Email: ameerah@icloud.com.
Vivienne Eloise Evans, Email: vivienne.evans2@nhs.net.
Eilidh Elizabeth Stewart Middleton, Email: eilidh.middleton@hotmail.co.uk.
Attika Chaudhary, Email: attikachaudhary@gmail.com.
Huzaifa Ahmad Cheema, Email: huzaifaahmadcheema@gmail.com.
Abia Shahid, Email: abiashahid126@gmail.com.
Laulwa Al Salloum, Email: laulwaalsalloum@hotmail.com.
Eva Szilagyi-Nagy, Email: szilnagyeva@gmail.com.
Samia Omar, Email: samiaomar@outlook.com.
Calan Mathieson, Email: calan.mathieson@ggc.scot.nhs.uk.
Tracey Anne Baird, Email: tracey.baird@ggc.scot.nhs.uk.
Roddy O’Kane, Email: roddy.o'kane@ggc.scot.nhs.uk.
Naveed Ashraf, Email: drnashraf@yahoo.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.AbdulWahid J, Ismail M, Al-Mosawy MS, Abdulsada AM, AlAgeely TA, Hoz SS. Ins and outs in deciding a future career in neurosurgery: A medical student’s perspective. Surg Neurol Int. 2022;13:530. doi: 10.25259/SNI_884_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agarwal N, Norrmen-Smith IO, Tomei KL, Prestigiacomo CJ, Gandhi CD. Improving medical student recruitment into neurological surgery: A single institution’s experience. World Neurosurg. 2013;80:745–50. doi: 10.1016/j.wneu.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 3.Ashraf M, Ashraf N. Affordable low-cost home-made skull model for interactive neurosurgical workshops: Experience with hands-on intracranial pressure monitoring at 2 international neurosurgical conferences. World Neurosurg. 2022;161:34–8. doi: 10.1016/j.wneu.2022.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Ashraf M, Ismahel H, Lub S, Middleton E, Chaudhary A, Gardee A, et al. Glasgow neuro society 2021 conference proceedings. Surg Neurol Int. 2022;13:173. doi: 10.25259/SNI_268_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrios-Anderson A, Liu DD, Snead J, Wu E, Lee DJ, Robbins J, et al. The national student neurosurgical research conference: A research conference for medical students. World Neurosurg. 2021;146:e398–404. doi: 10.1016/j.wneu.2020.10.108. [DOI] [PubMed] [Google Scholar]
- 6.Burford C, Guni A, Rajan K, Hanrahan J, Armitage M, Driscoll A, et al. Designing undergraduate neurosurgical e-learning: Medical students’ perspective. Br J Neurosurg. 2019;33:79. doi: 10.1080/02688697.2018.1520806. [DOI] [PubMed] [Google Scholar]
- 7.Clark DJ, Kolias AG, Garnett MR, Trivedi RA, Price SJ, Hutchinson PJ. Student-selected components in neurosurgery. Br J Neurosurg. 2016;30:4–6. doi: 10.3109/02688697.2015.1114590. [DOI] [PubMed] [Google Scholar]
- 8.Cochran A, Paukert JL, Scales EM, Neumayer LA. How medical students define surgical mentors. Am J Surg. 2004;187:698–701. doi: 10.1016/j.amjsurg.2003.12.053. [DOI] [PubMed] [Google Scholar]
- 9.Competition Ratios Higher Education England. 2022. Available from: https://medical.hee.nhs.uk/medical-training-recruitment/medical-specialty-training/competition-ratios/2022-competition-ratios [Last accessed on 2023 Feb 01]
- 10.Czorlich P, Regelsberger J, Meixensberger J, Westphal M, Eicker SO. From abstract to publication in a peer-reviewed journal: Evaluation of the 63rd annual meeting of the German society of neurosurgery. J Neurol Surg A Cent Eur Neurosurg. 2016;77:46–51. doi: 10.1055/s-0035-1558822. [DOI] [PubMed] [Google Scholar]
- 11.Entezami P, Franzblau LE, Chung KC. Mentorship in surgical training: A systematic review. Hand (N Y) 2012;7:30–6. doi: 10.1007/s11552-011-9379-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haggins A, Sandhu G, Ross PT. Value of near-peer mentorship from protégé and mentor perspectives: A strategy to increase physician workforce diversity. J Natl Med Assoc. 2018;110:399–406. doi: 10.1016/j.jnma.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Hanrahan J, Burford C, Ansaripour A, Smith B, Sysum K, Rajwani KM, et al. Undergraduate neurosurgical conferences-what role do they play? Br J Neurosurg. 2019;33:76–8. doi: 10.1080/02688697.2018.1527288. [DOI] [PubMed] [Google Scholar]
- 14.Healy NA, Cantillon P, Malone C, Kerin MJ. Role models and mentors in surgery. Am J Surg. 2012;204:256–61. doi: 10.1016/j.amjsurg.2011.09.031. [DOI] [PubMed] [Google Scholar]
- 15.Healy NA, Glynn RW, Malone C, Cantillon P, Kerin MJ. Surgical mentors and role models: Prevalence, importance and associated traits. J Surg Educ. 2012;69:633–7. doi: 10.1016/j.jsurg.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Horan J, Murphy S, O’Brien D. Neurosurgical education in Ireland; a conference and medical student experiences. Surgeon. 2020;18:159–64. doi: 10.1016/j.surge.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Hoz SS, Ismail M, Almufadhal MH, Al-Ageely TA, Aljuboori Z. Reinvigorating medical student mentorships in neurosurgery during the pandemic: Lessons learned from Iraq. Surg Neurol Int. 2022;13:357. doi: 10.25259/SNI_670_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ismail M, Ahmed FO, Abdulsada AM, Al-Khafaji AO, Hoz SS, Lazareff JA, et al. The most inspiring and mind-blowing meetings ever: Highlights of the 15(th) SNI Baghdad neurosurgery online meeting, from participants’ perspectives. Surg Neurol Int. 2022;13:353. doi: 10.25259/SNI_662_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ismail M, Al-Ageely TA, Abdualmurtafie ZI, Daily SK, Ayad F, Al Khafaji AO, et al. SNI/SNI Digital-Baghdad neurosurgery educational series. Surg Neurol Int. 2022;13:485. doi: 10.25259/SNI_697_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Janssen T, Bartels R, Lind B, Villas Tome C, VleggeertLankamp CL. Publication rate of paper and podium presentations from the European section of the cervical spine research society annual meeting. Eur Spine J. 2016;25:2311–6. doi: 10.1007/s00586-016-4404-9. [DOI] [PubMed] [Google Scholar]
- 21.Lee KS, Zhang JJY, Alamri A, Chari A. Neurosurgery education in the medical school curriculum: A scoping review. World Neurosurg. 2020;144:e631–42. doi: 10.1016/j.wneu.2020.09.015. [DOI] [PubMed] [Google Scholar]
- 22.Myers MA, Hall SR, Waters RJ. United Kingdom: MedEdPublish; 2017. Twelve Tips for Medical Students to Get the most Out of an Undergraduate Neurosurgery Placement; p. 6. [Google Scholar]
- 23.Myers MA, Shkanov Y, Rae S, Mahoney D, Hall S. The benefits of a local neurosurgery careers day. Br J Neurosurg. 2017;31:569–70. doi: 10.1080/02688697.2017.1334042. [DOI] [PubMed] [Google Scholar]
- 24.Myers PL, Amalfi AN, Ramanadham SR. Mentorship in plastic surgery: A critical appraisal of where we stand and what we can do better. Plast Reconstr Surg. 2021;148:667–77. doi: 10.1097/PRS.0000000000008295. [DOI] [PubMed] [Google Scholar]
- 25.Narain AS, Hijji FY, Kudaravalli KT, Yom KH, Singh K. Publication rates of abstracts accepted to the 2010-2012 annual meetings of the North American Spine society. Spine (Phila Pa 1976) 2017;42:1723–9. doi: 10.1097/BRS.0000000000002203. [DOI] [PubMed] [Google Scholar]
- 26.National Neurosurgery ST1 & ST2 Recruitment. Health Education Yorkshire and Humber. 2022. Available from: https://www.yorksandhumberdeanery.nhs.uk/recruitment/national_recruitment/national_neurosurgery_st1__st3_recruitment [Last accessed on 2023 Jan 01]
- 27.O’Callaghan J, Mohan HM, Sharrock A, Gokani V, Fitzgerald JE, Williams AP, et al. Cross-sectional study of the financial cost of training to the surgical trainee in the UK and Ireland. BMJ Open. 2017;7:e018086. doi: 10.1136/bmjopen-2017-018086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.SNIDigital Available from: https://www.snidigital.org/Published2023 [Last accessed on 2013 Feb 10]
- 29.Stumpo V, Latour K, Traylor JI, Staartjes VE, Giordano M, Caccavella VM, et al. Medical student interest and recruitment in neurosurgery. World Neurosurg. 2020;141:448–6. doi: 10.1016/j.wneu.2020.04.248. [DOI] [PubMed] [Google Scholar]
- 30.Tayade MC, Latti RG. Effectiveness of early clinical exposure in medical education: Settings and scientific theories-review. J Educ Health Promot. 2021;10:117. doi: 10.4103/jehp.jehp_988_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tiefenbach J, Kaliaperumal C, Demetriades AK. Increasing medical student exposure to neurosurgery: The educational value of special study modules, student selected components, and other undergraduate student projects. Front Surg. 2022;9:840523. doi: 10.3389/fsurg.2022.840523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitehouse KJ, Moore AJ. Undergraduate teaching of neurosurgery-what is the current practice in the UK and is there a need for improvement? Br J Neurosurg. 2015;29:753–7. doi: 10.3109/02688697.2015.1054361. [DOI] [PubMed] [Google Scholar]
- 33.Whitehouse SS, Thomson S, Jenkins UK. London: Society of British Neurological Surgeons; 2020. Neurosurgery Workforce Report 2020. [Google Scholar]
- 34.Yoon JD, Ham SA, Reddy ST, Curlin FA. Role models’ influence on specialty choice for residency training: A national longitudinal study. J Grad Med Educ. 2018;10:149–54. doi: 10.4300/JGME-D-17-00063.1. [DOI] [PMC free article] [PubMed] [Google Scholar]