Abstract
Objectives
To develop evidence-based points to consider for cost-effective use of biological and targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) in the treatment of inflammatory rheumatic diseases, specifically rheumatoid arthritis, psoriatic arthritis and axial spondyloarthritis.
Methods
Following EULAR procedures, an international task force was formed, consisting of 13 experts in rheumatology, epidemiology and pharmacology from seven European countries. Twelve strategies for cost-effective use of b/tsDMARDs were identified through individual and group discussion. For each strategy, PubMed and Embase were systematically searched for relevant English-language systematic reviews and, for six strategies, additionally for randomised controlled trials (RCTs). Thirty systematic reviews and 21 RCTs were included. Based on the evidence, a set of overarching principles and points to consider was formulated by the task force using a Delphi procedure. Level of evidence (1a–5) and grade (A–D) were determined for each point to consider. Individual voting on the level of agreement (LoA; between 0 (completely disagree) and 10 (completely agree)) was performed anonymously.
Results
The task force agreed on five overarching principles. For 10 of 12 strategies, the evidence was sufficient to formulate one or more points to consider, leading to 20 in total, regarding response prediction, drug formulary use, biosimilars, loading doses, low-dose initial therapy, concomitant conventional synthetic DMARD use, route of administration, medication adherence, disease activity–guided dose optimisation and non-medical drug switching. Ten points to consider (50%) were supported by level 1 or 2 evidence. The mean LoA (SD) varied between 7.9 (1.2) and 9.8 (0.4).
Conclusion
These points to consider can be used in rheumatology practices and complement inflammatory rheumatic disease treatment guidelines to incorporate cost-effectiveness in b/tsDMARD treatment.
Keywords: Biological Therapy; Arthritis, Rheumatoid; Arthritis, Psoriatic; Economics; Spondylitis, Ankylosing
What is already known about this subject
Biological and targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) are effective drugs in the treatment of inflammatory rheumatic diseases but are also associated with side effects and high societal costs.
A systematic overview of the literature and practical points to consider in improving the cost-effective use of these drugs are missing.
What does this study add
In this Delphi study, 12 strategies for the cost-effective use of b/tsDMARDs have been identified. Furthermore, five overarching principles and 20 points to consider have been formulated.
How might this impact clinical practice?
These points to consider help rheumatology healthcare providers to incorporate patient-centred and cost-effective use of b/tsDMARDs in their daily practice.
Introduction
In the last two decades, pharmacological treatment options for inflammatory rheumatic diseases (IRDs), including specifically rheumatoid arthritis (RA), psoriatic arthritis (PsA) and axial spondyloarthritis (axSpA), have vastly expanded. In particular, the biological and targeted synthetic disease-modifying antirheumatic drugs (bDMARDs and tsDMARDs, respectively) have taken an important place in IRD treatment, as they have been shown to reduce disease activity, slow down radiological progression and improve daily functioning.1–3
Although b/tsDMARD therapy is effective, it has disadvantages, such as adverse events, the need for parenteral administration (for bDMARDs) and high costs. Concerning the costs, b/tsDMARDs are substantially more expensive per year than conventional synthetic DMARDs (csDMARDs),4 are used by an increasing number of patients and in principle require chronic use. With the arrival of biosimilars, some bDMARDs have become somewhat less expensive,5 but their impact on a pressured healthcare budget remains.
When following the current disease-specific recommendations, many patients can reach good disease control. Therefore, the current challenge for clinicians is not only controlling the disease but also achieving this in the most cost-effective way, to provide optimal rheumatology care from a societal perspective. This viewpoint has been adopted in the EULAR RA recommendations as follows: ‘RA incurs high individual, medical and societal costs, all of which should be considered in its management by the treating rheumatologist’.6 However, specific recommendations or points to consider on how to optimise cost-effectiveness have not been formulated.
Cost-effectiveness, expressed as the effect on health divided by the costs of an intervention, can be improved by either increasing effectiveness or reducing costs.7 So far, several strategies for improving cost-effectiveness of b/tsDMARDs have been investigated, with dose reduction and biosimilar use being the most systematically studied.8 9 Concerning the use of biosimilars, recommendations for clinical practice have been formulated by Kay et al.9 However, to facilitate that clinicians and rheumatology practices choose the optimal strategy in their specific situation, a systematic overview of all (possible and attempted) strategies to optimise cost-effectiveness with points to consider for all strategies, including less-known options, is needed.
Therefore, the aim of this project was to provide a systematic overview of evidence regarding strategies aimed at improving the cost-effective use and to develop international, consensus-based, interdisciplinary points to consider on cost-effective prescribing of b/tsDMARDs in IRD from a societal perspective.
Methods
These consensus-based and evidence-based points to consider were developed for individual rheumatologists or groups of rheumatologists (eg, in a hospital). They were designed to be applicable across different healthcare systems. For the development of the points to consider, we used the EULAR standardised operating procedure for recommendations10 and the additional EULAR guidance on methodology.11 Of note, where the word ‘rheumatologist’ is used, the task force means any rheumatology healthcare provider prescribing b/tsDMARDs, including among others rheumatology trainees, and in some countries also nurse specialists and physician assistants. For the definition of cost-effectiveness, we used an adapted version of the NICE definition: ‘Guideline recommendations should be based on the estimated costs of the interventions or services in relation to their expected health benefits (that is, their “cost-effectiveness”), rather than on the total cost or resource impact of implementing them’.7
Task force
In September 2020, an international interdisciplinary task force of 13 experts from seven European countries was formed for this study, consisting of 7 rheumatologists (DA, RA, KC, JG, JI, DM and PV), 1 pharmacist (AGV), 1 epidemiologist-health technology assessment expert (PMJW), 1 research fellow (CJTvdT), 1 epidemiologist (LV), 1 pharmacist-clinical pharmacologist (BVdB) and 1 rheumatologist-epidemiologist (AAdB). The steering committee, consisting of CJTvdT, BVdB, LV and AAdB performed the scoping review and hosted the task force meetings. All task force members were involved in formulating the points to consider and voting for the level of agreement (LoA).
Phase I: scope and strategies
In October and November 2020, one-to-one open interviews with all members of the task force were performed by CJTvdT to identify all relevant strategies on the cost-effective use of b/tsDMARDs (figure 1). Thereafter, in November 2020, an online kick-off meeting took place to reach consensus on the included b/tsDMARDs (table 1), the definition of a strategy for cost-effective use, the included strategies with their definitions and the protocol of the scoping review. A study was considered eligible if it included: patients with RA, PsA or axSpA, (planning to be) treated with b/tsDMARDs (Population), comparison of treatment with and without a strategy [Intervention/Comparison] and any of the following outcomes: cost-effectiveness, costs, efficacy, safety or patient-reported outcomes (PROMs) (Outcome). Of note, a formal cost-effectiveness assessment was considered the primary outcome of our review. However, when not available, a more informal approach for assessing costs and resource use in relation to effectiveness outcomes was performed. Only systematic literature reviews (SLRs) and randomised controlled trials (RCTs) were included, to search for available high-quality evidence and to conserve feasibility. Moreover, the panel agreed on two further limitations: (1) publications in English only, as this was the only language understood by every participant in the project and (2) studies published in 2000 or thereafter since we did not expect any relevant publications beforehand.
Figure 1.
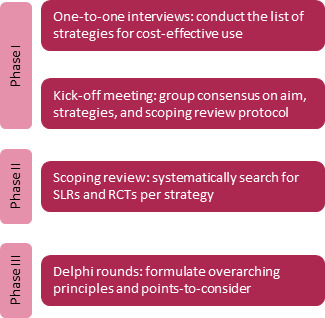
Study phases. RCT, randomised controlled trial; SLR, systematic literature review.
Table 1.
Included drugs with abbreviation and their indications, authorised dose, interval and route of administration
| Drug | Abbreviation | Indication for RA, PsA, axSpA? (EMA) | RoA | Authorised dosing scheme (EMA) | Different registration for FDA? | |
| Loading dose | Maintenance dose | |||||
| Abatacept | ABA | RA, PsA | IV | Weight-based infusion at weeks 0, 2, 4 | Weight-based infusion every 4 weeks: <60 kg 500 mg, 60–100 kg 750 mg, >100 kg 1000 mg | No |
| SC | Weight-based infusion | 125 mg/week | No | |||
| Adalimumab | ADA | RA, PsA, axSpA | SC | None | 40 mg/2 weeks | No |
| Apremilast | APR | PsA | Oral | None | 30 mg once daily | No |
| Baricitinib | BARI | RA | Oral | None | 4 mg once daily | Yes, 2 mg once daily |
| Certolizumab pegol | CER | RA, PsA, axSpA | SC | 400 mg at weeks 0, 2, 4 | 200 mg/2 weeks or 400 mg/4 weeks | No |
| Etanercept | ETN | RA, PsA, axSpA | SC | None | 50 mg/week | No |
| Filgotinib | FILG | RA | Oral | None | 200 mg once daily | Not available in the USA |
| Golimumab | GOL | RA, PsA, axSpA | SC | None | 50 mg/month. If weight is >100 kg and response is insufficient: increase to 100 mg/month | No |
| Infliximab | IFX | RA, PsA, axSpA | IV | Disease-based mg/kg infusion at weeks 0, 2, 6 | 3 mg/kg every 8 weeks for RA; 5 mg/kg every 8 weeks for PsA and axSpA | No |
| RA, PsA, axSpA | SC | 120 mg/2 weeks | Not available in the USA | |||
| Ixekizumab | IXE | PsA, axSpA | SC | 160 mg at week 0 | 80 mg every 4 weeks | No |
| Rituximab | RTX | RA | IV | None | 1000 mg/6 months | No |
| Sarilumab | SARI | RA | SC | None | 200 mg/2 weeks | No |
| Secukinumab | SECU | PsA, axSpA | SC | 150 mg at weeks 0, 1, 2, 3, 4 | 150 mg/month | No |
| Tocilizumab | TCZ | RA | IV | None | 8 mg/kg every 4 weeks (max. 800 mg) | Yes, 4 mg/kg |
| SC | None | 162 mg/week | Yes, 162 mg/2 weeks if weight <100 kg | |||
| Tofacitinib | TOFA | RA, PsA, axSpA | Oral | None | 5 mg twice daily or 11 mg XR once daily | No |
| Upadacitinib | UPA | RA, PsA, axSpA | Oral | None | 15 mg once daily | No |
| Ustekinumab | UST | PsA | SC | 45 mg at weeks 0, 4 90 mg if weight >100 kg |
45 mg/12 weeks 90 mg if weight >100 kg |
No |
Abbreviation (as used in this publication and the online supplemental data)
EMA, European Medicines Agency; FDA, Food and Drug Administration; IV, intravenous; PsA, psoriatic arthritis; RA, rheumatoid arthritis; RoA, route of administration; SC, subcutaneous; SpA, spondyloarthritis; XR, extended release.
rmdopen-2022-002898supp001.pdf (2.5MB, pdf)
Phase II: existing evidence
PubMed and Embase were systematically searched for each strategy using a two-step approach: an initial search for SLRs by filtering for systematic reviews in both PubMed and Embase, and a second search for RCTs for the remaining research gaps by adding the Cochrane high-sensitivity RCT search string in both PubMed and Embase.12 In addition, reference lists of included articles were screened for relevant studies. In general, the search string consisted of three parts: (IRDs) AND (drugs) AND (strategy). The first part (IRDs) was identical for all strategies, and the second part (drugs) for every strategy except for the route of administration, of which this part only focused on drugs with multiple administration routes available (abatacept, infliximab, tocilizumab). The outcomes were not included in the search string but checked for in the title/abstract screening. Further information on the search strategies and searches is included in the online supplemental file 1.
Title/abstract screening was performed by two steering committee members separately. Disagreements were discussed by the two reviewers until an agreement was reached, or, if persistent were resolved by the vote of another steering committee member. If more than five SLRs were accepted after title/abstract screening, full-texts of recent SLRs (published in 2019 or thereafter) were screened first. Full-texts of older reviews were only screened in case of research gaps. Full-text screening combined with risk of bias (RoB) assessment was performed by the same reviewers as title/abstract screening independently, using AMSTAR-2 for SLRs13 and the Cochrane RoB tool 2 for RCTs.14 The data extraction form was designed by LV and CJTvdT. CJTvdT performed the data extraction.
Phase III: consensus
The steering committee drafted a first version of the overarching principles and points to consider, the latter including level of evidence (LoE) and grade of recommendation (GR), based on the underlying evidence. Thereafter, a summary of the evidence and the proposed points-to-consider were communicated to all task force members prior to the meetings. In total, five online task force Delphi meetings took place between June and December 2021. In the first meeting, the overarching principles were discussed and accepted with ‘no objection’ during the meeting. In the following meetings, we discussed the content and phrasing of the definitive points to consider. Also, LoE and GR were determined in accordance with the EULAR additional guidance.11 If consensus was reached on the formulation of the point to consider in the group meeting, task force members were asked afterwards by e-mail to vote on its LoA. LoA score ranged from 0 (completely disagree) to 10 (completely agree), based on the 2014 EULAR SOP.10
Results
Phase I: scope and strategies
The task force formulated a definition for strategies of cost-effective b/tsDMARD use (see box 1). Of note, we assumed that the diagnosis of the patients should be sufficiently certain.
Box 1. Definition for strategies of cost-effective b/tsDMARD use.
Strategies on the level of an individual patient or a hospital, concerning cost-effective prescribing1 or use of biological and targeted synthetic DMARDs in the treatment of rheumatoid arthritis, psoriatic arthritis or axial spondyloarthritis.
1Includes the indication, selection, dose, interval, route of administration and monitoring of the drug, and any comedication interfering pharmacokinetically or pharmacodynamically. b/tsDMARD, biological and targeted synthetic disease-modifying antirheumatic drug.
The task force identified four distinct ways for a strategy to increase cost-effectiveness (benefits): (1) a direct reduction of drug price per milligram, (2) a lower drug quantity needed (dose/interval), (3) lower direct additional non-medication costs (eg, day care costs for infusion) and (4) improved efficacy or safety, or reduced patient burden. Furthermore, the task force identified 12 strategies: (1) response prediction, (2) drug formulary policy, (3) biosimilar/generic drug use, (4) avoid dose loading, (5) initial lower dose, (6) optimising pharmacokinetic exposure, (7) combination therapy, (8) route of administration, (9) drug wastage, (10) medication adherence, (11) disease activity–guided dose optimisation (DAGDO) and (12) non-medical drug switching. An overview of the strategies including their definition and potential benefits is displayed in table 2.
Table 2.
Definition of strategies and how cost-effectiveness can be optimised
| Strategy | Definition | Benefit(s)* |
| Response prediction | To use a predictor for optimising any drug use intervention, such as drug selection, drug dose reduction or drug discontinuation | 4 |
| Drug formulary policy | To prescribe b/tsDMARDs in a preferential order for the rheumatology practice, primarily based on effectiveness and safety but in case of equality also on cost-effectiveness | 1 |
| Biosimilar/generic drug use | To (allow the) start of or transition to the best value drug variant (biosimilar/generic or originator) of a b/tsDMARD | 1 |
| Avoid dose loading | To avoid the loading dose (initial higher dose than maintenance dose) that is part of an authorised dosing | 2, 4 |
| Initial lower dose | To use a lower dose than the authorised dose in the maintenance phase | 2, 4 |
| Optimising pharmacokinetic exposure | To improve exposure to the b/tsDMARD by influencing pharmacokinetic parameters | 2, 4 |
| Combination therapy | To choose for either combined treatment of a b/tsDMARD with a csDMARD or monotherapy of a specific b/tsDMARD | 2, 3, 4 |
| Route of administration | To start with or to transition to the most cost-effective route of administration for bDMARDs of which multiple routes are available | 2, 3, 4 |
| Drug wastage | To reduce wastage of the b/tsDMARD to reduce total amount of drug needed | 2, 3 |
| Medication adherence | To improve the extent to which a person’s medication intake corresponds with agreed treatment decisions with the healthcare provider | 3, 4 |
| Disease activity–guided dose optimisation | To gradually reduce drug dosage or lengthen the interval of the b/tsDMARD to the minimal effective dose or discontinuation guided by the disease activity | 2, 4 |
| Non-medical drug switching | To switch patients to another more cost-effective b/tsDMARD (within or between classes), excluding biosimilars, to reduce drug costs | 1 |
*1. A direct reduction of drug price per milligram. 2. A lower needed drug quantity (dose/interval). 3. Lower direct additional drug costs. 4. Improved efficacy or safety, or reduced patient burden.
b/tsDMARD, biological and targeted synthetic disease-modifying antirheumatic drug; csDMARD, conventional synthetic disease-modifying antirheumatic drug.
Phase II: existing evidence
The SLR searches, performed on 24 February 2021 and 1 November 2021 (initial lower dose), identified 1104 publications. Of those, 57 were accepted after title-abstract screening. After full-text screening, 30 SLRs in total could be included. For five strategies, no systematic reviews could be included. Except for the strategy biosimilar/generic drug use, additional RCT searches were performed for the other 11 strategies between 22 March 2021 and 17 November 2021, identifying 4804 publications. Of those, 25 were accepted after title-abstract screening and eventually 21 full-text publications were included for six strategies. For the four strategies, no articles could be accepted, including drug formulary policy, optimising pharmacokinetic exposure, reducing drug wastage and non-medical drug switching (excluding biosimilar transitioning). The searches, output flowcharts per strategy and extracted data are included in the online supplemental file 1.
Phase III: consensus
In the Delphi meetings, the task force agreed on five overarching principles and 20 points to consider (see table 3), which are explained in the following paragraphs. The overall mean LoA was 8.9 (range 7.9–9.7). Of the 240 votes received, four times a 5 was voted (2%), five times a 6 (2%) and nine times a 7 (4%). All other votes were ≥8. Except for the strategy ‘avoid dose loading’, all other strategies required only one Delphi meeting to agree with the completeness of the search and to reach consensus on the phrasing of the recommendation. Regarding the strategy ‘avoid dose loading’, the task force requested for an additional search in the ‘summary of the product characteristics’ of the included drugs but no additional information was found.
Table 3.
Overarching principles and consensus-based points to consider
| Overarching principles | |||
| A. Treatment choices must be based on shared decision-making between the patient and the rheumatologist. | |||
| B. Treat-to-target is the cornerstone of b/tsDMARD-based treatment in RA, PsA and axSpA. | |||
| C. Cost-effectiveness considerations are an important aspect of treatment, and rheumatologists should have a leading role regarding this. | |||
| D. Reimbursement policies should cover cost-effective use of pharmacological treatments, both on-label and off-label, when it is evidence based and supported by (inter)national guidelines. | |||
| E. Bio-originators and biosimilars are considered similar, and thus all recommendations apply equally to bio-originators and biosimilars. | |||
| Points to consider | LoE | GR | LoA |
| Response prediction | |||
| 1. Therapeutic drug monitoring* of b/tsDMARDs in patients with RA, PsA and axSpA is not advised because of the absence of evidence† on efficacy and safety. | 5 | D | 8.3±1.4 (6–10) |
| 2. Using other predictors for either choosing or tapering a particular b/tsDMARD is not advised because none have demonstrated superiority to standard care. | 5 | D | 8.3±1.0 (7–10) |
| Drug formulary policy‡ | |||
| 3. Rheumatologists might consider to adopt and use a drug formulary for their practice, primarily based on effectiveness and safety, and cost-effectiveness thereafter. | 5 | D | 9.1±1.0 (7–10) |
| Biosimilar/generic drug use | |||
| 4. A biosimilar, if approved by a drug-regulating authority in a highly regulated area, should be preferred if it is the most cost-effective version of the drug. | 1b | A | 9.8±0.39 (9–10) |
| 5. A single transition from a bio-originator to one of its biosimilars should be considered if it contributes to the cost-effectiveness of the treatment. | 1b | A | 9.4±0.51 (9–10) |
| Avoid dose loading | |||
| 6. When initiating abatacept or certolizumab in RA, or secukinumab in PsA or axSpA, rheumatologists might consider to initiate treatment using the maintenance dose, as dose loading has not shown superior efficacy. | 1b | B | 8.5±1.5 (5–10) |
| 7. For the other b/tsDMARDs, there is no information on the effect of dose loading. Therefore, these drugs should be used as authorised. | 5 | D | 9.4±1.0 (7–10) |
| Initial lower dose | |||
| 8. In RA, low-dose rituximab (1*1000 mg or 2*500 mg per cycle) has similar efficacy and less toxicity compared with authorised-dose rituximab (2*1000 mg) and should thus be preferred over the authorised dose. | 1a | A | 9.3±1.3 (6–10) |
| 9. In patients with RA, rheumatologists might start with the lower dose§ of baricitinib or tocilizumab because of a more favourable safety and/or cost-effectiveness profile. | 4 | D | 7.9±1.2 (5–10) |
| Combination therapy | |||
| 10. In patients with RA, rheumatologists should combine the b/tsDMARD with methotrexate to maximise efficacy; in patients who cannot use methotrexate as comedication, IL-6 pathway inhibitors and JAK-inhibitors¶ might be preferred over other bDMARDs. | 1a 2a¶ |
A | 9.5±0.78 (8–10) |
| 11. For patients with PsA or axSpA, combination therapy of a TNF inhibitor with methotrexate cannot be advised, because increased efficacy compared with TNF inhibitor monotherapy is not shown. | 1a | A | 8.4±1.3 (5–10) |
| 12. For patients with PsA or axSpA, combination therapy of non-TNF inhibitors with methotrexate cannot be advised because of the absence of evidence on efficacy and safety. | 5 | D | 8.7±1.2 (6–10) |
| Route of administration | |||
| 13. For patients with RA, non-inferiority of subcutaneous versus intravenous treatment of abatacept, infliximab and tocilizumab has been shown, and thus rheumatologists can choose the most cost-effective route of administration when initiating one of those drugs. | 1b | A | 9.5±0.52 (9–10) |
| 14. For patients with RA, a single switch from subcutaneous to intravenous tocilizumab or vice versa did not affect efficacy or safety, and thus rheumatologists might consider this for cost-effectiveness reasons. | 2b | C | 8.9±1.0 (7–10) |
| Medication adherence | |||
| 15. Rheumatologists should take adherence into account in the management of their patients by using the current points to consider** to manage non-adherence of b/tsDMARDs. | 5 | D | 9.5±0.52 (9–10) |
| Disease activity–guided dose optimisation | |||
| 16. For patients with RA in whom the treatment target is reached and sustained, rheumatologists should consider disease activity–guided dose optimisation of anti-TNF drugs. | 1 | A | 9.6±0.90 (7–10) |
| 17. For patients with RA in whom the treatment target is reached and sustained, rheumatologists might consider disease activity–guided dose optimisation of IL-6 inhibitors, rituximab, baricitinib or abatacept. | 1b | B | 8.8±0.87 (7–10) |
| 18. For patients with axSpA†† and PsA†† in whom the treatment target is reached and sustained, rheumatologists might consider disease activity–guided dose optimisation of anti-TNF drugs. | 1a†† 5†† |
B†† D†† |
8.2±1.1 (6–10) |
| 19. Rheumatologists can use any disease activity–guided dose optimisation scheme, as none is preferential based on the evidence. | 5 | D | 8.9±1.4 (5–10) |
| Non-medical drug switching‡ | |||
| 20. Non-medical switching within or between b/tsDMARD classes is not advised because of the absence of evidence on efficacy and safety. | 5 | D | 9.7±0.65 (8–10) |
*Adjustments of dose and/or interval based on drug serum levels and/or antidrug antibodies.
†Except for (1) proactive TDM (drug doses and timing of doses are based on serum drug levels) of infliximab in RA, PsA and axSpA and (2) dose increase of infliximab based on baseline TNF-alpha for RA, this has not shown superiority (both LoE 1b, strength B).
‡No evidence (SLR or RCT) found for this strategy.
§2 mg once daily for baricitinib and 4 mg/kg (intravenously)* or 162 mg every 2 weeks (subcutaneously)* for tocilizumab, all three authorised doses in the USA. *Only for patients with a body weight <100 kg
¶Lower LoE for baricitinib
**Ritschl V, et al. Ann Rheum Dis. 2020.47
††Different LoE and GR for PsA and axSpA.
axSpA, axial spondyloarthritis; b/tsDMARD, biological and targeted synthetic disease-modifying antirheumatic drug; GR, grade of point to consider; IL-6, interleukin 6; JAK, Janus kinase; LoA, level of agreement on a numeric rating scale from 0 (completely disagree) to 10 (completely agree), displayed as mean±SD (range); LoE, level of evidence; LoE, level of evidence; PsA, psoriatic arthritis; RA, rheumatoid arthritis; RCT, randomised controlled trial; SLR, systematic literature review; TDM, therapeutic drug monitoring; TNF, tumour necrosis factor.
Overarching principles
A. Treatment choices must be based on shared decision-making between the patient and the rheumatologist
RA, PsA and axSpA are diseases with a chronic course and require chronic treatment in the vast majority of patients. Shared decision-making can enhance medication adherence by adapting treatment to a patient’s personal life/preferences, leading to increased satisfaction and control of treatment.
B. Treat-to-target (T2T) is the cornerstone of b/tsDMARD-based treatment in RA, PsA and axSpA
The T2T approach comprises tight monitoring of disease activity for the evaluation of treatment. This approach is recommended for RA, PsA and axSpA.15–17 T2T should be the standard background strategy for b/tsDMARD treatment.
C. Cost-effectiveness considerations are an important aspect of treatment, and rheumatologists should have a leading role regarding this
Currently, there are many drugs available for inflammatory arthritis. As most of these drugs are comparable in efficacy and safety, we believe that cost-effectiveness should be an additional selection criterium. Antirheumatic treatment has a significant impact on the rheumatology healthcare budget and as explained further in this paper, multiple strategies for more cost-effective use are available. Moreover, we believe that rheumatologists should have a leading role in this because of their knowledge, training, experience and direct involvement in b/tsDMARD prescription and the hospital’s drug formulary.
D. Reimbursement policies should cover cost-effective use of pharmacological treatments, both on-label and off-label, when it is evidence based and supported by (inter)national guidelines
Some of these points to consider require off-label use of b/tsDMARDs, for example, a reduced dose, a prolonged interval or removal of a loading dose. We acknowledge that off-label use of medication is sometimes not included in reimbursement policies or not financially beneficial for the hospital while this could have multiple advantages regarding outcomes and/or costs at a societal level. We believe that every opportunity for healthcare cost reduction (without significant impact on the quality of care) should be taken advantage of for the preservation of affordable healthcare. We therefore advocate that reimbursement policies, either from governments or healthcare insurance companies, include off-label medication use in case of proven added value. We consider these points to consider a first step towards removing barriers for providing cost-effective care.
E. Bio-originators and approved biosimilars are considered similar, and thus all recommendations apply equally to bio-originators and biosimilars
As further explained in the online supplemental file 1 of the fourth point to consider (on biosimilar/generic drug use), we consider bio-originators and approved biosimilars clinically similar, in agreement with the American College of Rheumatology RA guideline.17 Therefore, all points to consider apply equally to biosimilars.
Consensus recommendations
Response prediction
1. Therapeutic drug monitoring of b/tsDMARDs in patients with RA, PSA and axSpA is not advised because of the absence of evidence on efficacy and safety.
Therapeutic drug monitoring (TDM) is a clinical practice in which adjustments of dose and/or interval are made based on drug serum levels and/or antidrug antibodies (ADAb).18 One can distinguish ‘proactive TDM’ in which drug levels and/or ADAb are measured with the aim to proactively adjust treatment, regardless of the clinical response, and ‘reactive TDM’ in which drug levels and/or ADAb are measured in case of loss of efficacy or side effects.18 A recent systematic review on the clinical effectiveness of TDM of anti-tumour necrosis factor (anti-TNF) in RA found one clinical study on this subject but could not draw conclusions because of the serious RoB of this study.19 We found another RCT (NORDRUM I), which compared proactive TDM of induction of infliximab treatment to standard care and did not find a difference in clinical remission at week 30.20 Based on the available evidence, the task force concluded that TDM can currently not be advised because of the absence of evidence on superiority.
2. Using other predictors for either choosing or tapering a particular b/tsDMARD is not advised because none have demonstrated superiority to standard care.
Other predictors could include either biomarkers, genetic markers or clinical markers. Disease activity was not included as a clinical marker because T2T is already incorporated in the overarching principles and disease activity–based tapering in the DAGDO section. Four systematic reviews found no clinical test–treatment trials with these markers.21–24 An RCT on circulating TNF-alpha levels as a predictor for increasing infliximab dosage in RA found no differences in sustained remission.25 Therefore, using other predictors for selecting or tapering a b/tsDMARD is not advised.
Drug formulary policy
3. Rheumatologists might consider to adopt and use a drug formulary for their practice, primarily based on effectiveness and safety, and cost-effectiveness thereafter.
A drug formulary is a preferred order of b/tsDMARDs, established for a hospital, region or country. Formularies provide a structure for safe, rational and cost-effective drug use. As formularies uniformalise and prioritise drug therapy strategies, they are also an important instrument for the cost-conscious procurement of medication. We found no supporting SLRs or RCTs on this topic. However, as these points to consider aim to inform rheumatologists on incorporating cost-effectiveness in their practice, and drug formulary policy was seen as an important strategy, the task force agreed on a point to consider based on expert opinion only.
Biosimilar/generic drug use
4. A biosimilar, if approved by a drug regulating authority in a highly regulated area, should be preferred if it is the most cost-effective version of the drug.
Biosimilars are available for an increasing number of bDMARDs, and from 2027 on, generic drug variants of tsDMARDs can also be expected. We found two systematic reviews supporting the use of biosimilars but both are of low quality.26 27 As mentioned in the introduction, the expert group of Kay et al has formulated consensus-based recommendations for biosimilar use in clinical care.9 The current point to consider is directly adapted from one of their overarching principles, which states that approved biosimilars in highly regulated areas are neither better nor worse in efficacy and non-inferior in safety to bio-originators. Our task force agreed on this principle and the addition that initiating therapy with a biosimilar can contribute to cost-effectiveness.
5. A single transition from a bio-originator to one of its biosimilars should be considered if it contributes to the cost-effectiveness of the treatment.
There is high-quality evidence available for the efficacy and safety of a single transition from bio-originator to biosimilar. Twelve RCTs regarding transitioning of infliximab (6), adalimumab (5) and etanercept (1) were included in three systematic reviews, which demonstrated the efficacy and safety of a single switch.28–30 Furthermore, transitioning is also supported by the recommendations of Kay et al.9 Regarding multiple switching, there was no evidence available at the time of the systematic search. Therefore, only a single transition is included in the second point to consider.
Avoid dose loading
6. When initiating abatacept or certolizumab in RA or secukinumab in PsA or axSpA, rheumatologists might consider to initiate treatment using the maintenance dose, as dose loading has not shown superior efficacy.
7. For the other b/tsDMARDs, there is no information on the effect of dose loading. Therefore, these drugs should be used as authorised.
A loading dose is a higher initial dose given at the beginning of a treatment course with the aim to achieve steady-state concentrations of a drug earlier in time, especially when a drug has a long half-life. For six bDMARDs, a loading dose is advised (table 1). The task force advocates that a loading dose should not be used when superiority on effectiveness has not been demonstrated in a head-to-head study. A systematic review on this subject found comparative studies with/without loading doses for abatacept and certolizumab in RA and secukinumab in both PsA and axSpA.31 The authors concluded that there is insufficient evidence on the superiority of dose loading for these drugs. For the other drugs authorised with a loading dose, no comparative studies were found. Thus, the task force concluded that for the aforementioned drugs, a regimen without loading dose could optimise cost-effectiveness. However, these drugs were studied and authorised with loading dose, and therefore the decision should be made carefully and with a shared decision to the patient. For the other drugs, more research is required to evaluate the additional value of the loading dose.
Initial lower dose
8. In RA, low-dose rituximab (1*1000 mg or 2*500 mg per cycle) has similar efficacy and less toxicity compared with authorised-dose rituximab (2*1000 mg) and should thus be preferred over the authorised dose.
For some b/tsDMARDs, an initial dose lower than the authorised dose may be as efficacious. The authorised dose of rituximab is two infusions of 1000 mg (14 days apart) every 6 months (2*1000 mg). An updated systematic review of Bredemeier et al based on three RCTs concluded that there were no significant differences between 2*1000 mg and 1*1000 mg rituximab in the primary efficacy outcomes.32 Moreover, 1*1000 mg rituximab was associated with a lower incidence of first infusion reactions. Based on this systematic review, 1*1000 mg could be advised over 2*1000 mg for the treatment of RA.
9. In patients with RA, rheumatologists might start with the lower dose of baricitinib or tocilizumab because of a more favourable safety and/or cost-effectiveness profile
For both tocilizumab and baricitinib, the authorised doses in the European Union (EU) and the USA are different. Baricitinib is dosed as 2 mg daily for RA in the USA, in contrast to 4 mg daily in the EU, and tocilizumab as 162 mg every 2 weeks (subcutaneous) or 4 mg/kg (intravenous) in the USA, in contrast to 162 mg weekly (subcutaneous) or 8 mg/kg (intravenous) in the EU. Although no formal cost–benefit study has been performed between the two regimens, the task force suggests that, based on the evidence,33–36 these lower doses could also be used as initial doses in European clinical practice. The use of baricitinib 2 mg might not lead to lower drug costs due to the flat pricing of 2 and 4 mg tablets. As lower-dosed tocilizumab was associated with numerically lower infection rates, and fewer cases of hypercholesterolaemia and neutropaenia,34 this regimen could especially be suitable for patients with safety concerns.
Combination therapy
Combining a b/tsDMARD with a csDMARD is known to increase the effectiveness of therapy and drug survival, and therefore cost-effectiveness. For this strategy, we specifically looked for evidence on starting a b/tsDMARD with or without concomitant csDMARD.
10. In patients with RA, rheumatologists should combine the b/tsDMARD with methotrexate (MTX) to maximise efficacy; in patients who cannot use MTX as comedication, interleukin 6 (IL-6) pathway inhibitors and Janus kinase (JAK) inhibitors might be preferred over other bDMARDs.
For RA, there is high-quality evidence supporting combination therapy. A meta-analysis investigated studies comparing b/tsDMARD treatment with and without MTX and found significantly better efficacy outcomes (ACR20/ACR50 response) for combination therapy for all bDMARDs.37 For tsDMARDs, this effect was not significant. Two other reviews specifically investigated tocilizumab and found comparable ACR20 responses38 and effectiveness measured with PROMs.39 Regarding sarilumab, no specific evidence was found. In the 2019 EULAR recommendations, combination therapy is advised for all b/tsDMARDs, and therapy with an IL-6 inhibitor or a JAK-inhibitor alone, if combination therapy is not possible.6 We formulated the point to consider in line with the EULAR RA recommendation but with a specific focus on MTX instead of csDMARDs, based on the available evidence. In addition, a dose of 10 mg MTX weekly may be sufficient for the effect.40
11. For patients with PsA or axSpA, combination therapy of a TNF-inhibitor (TNFi) with MTX cannot be advised, because increased efficacy compared with TNFi monotherapy is not shown.
For PsA and axSpA, two systematic reviews on combination therapy of TNFi41 42 found no additional effect of combination therapy on efficacy outcomes. However, the drug survival of TNFi, specifically infliximab, seemed somewhat better when combined with MTX in PsA according to registry data.41 The current EULAR guideline on the management of PsA therefore advises to continue MTX but to reduce the dose in good responders. We advise, in the light of cost-effectiveness, to taper the csDMARD to full discontinuation when the bDMARD is efficacious, although stopping the csDMARD when starting the bDMARD is an alternative possibility.
12. For patients with PsA or axSpA, combination therapy of non-TNFis with MTX cannot be advised because of the absence of evidence on efficacy and safety.
We found no systematic reviews or RCTs on combination therapy for non-TNFi in PsA or axSpA. Therefore, an expert opinion point to consider was formed in which combination therapy for non-TNFi in these diseases was not advised.
Route of administration
13. For patients with RA, non-inferiority of subcutaneous versus intravenous treatment of abatacept, infliximab and tocilizumab has been shown, and thus rheumatologists can choose the most cost-effective route of administration when initiating one of those drugs.
For abatacept, infliximab and tocilizumab, both intravenous and subcutaneous formulations are available which may differ in yearly medication costs. However, intravenous administration of the medication comes with additional costs for day care treatment. Both routes of administration for those three drugs have shown to be non-inferior regarding efficacy and without differences in safety.43–45 Therefore, we advise that a rheumatologist chooses the most cost-effective route of administration, whenever possible.
14. For patients with RA, a single switch from subcutaneous to intravenous tocilizumab or vice versa did not affect efficacy or safety, and thus rheumatologists might consider this for cost-effectiveness reasons.
The extension of the SUMMACTA study investigated switching from intravenous to subcutaneous tocilizumab or vice versa in a subpopulation and found maintained efficacy and similar safety profiles.46 For abatacept and infliximab, this has not yet been investigated. Therefore, the current point to consider is that a switch in the route of administration might be advised for tocilizumab to increase cost-effectiveness.
Medication adherence
15. Rheumatologists should take adherence into account in the management of their patients by using the current points to consider to manage non-adherence of b/tsDMARDs.
Even the most perfectly prescribed drug cannot have its desired effect in the case of non-adherence. Therefore, medication adherence should be included in points to consider for cost-effectiveness. We did not find any supporting systematic reviews or RCTs on this topic but refer to the current EULAR points to consider on non-adherence,47 which can help rheumatologists to manage non-adherence.
Disease activity–guided dose optimisation
DAGDO (also known as tapering) is a strategy that includes a stepwise dose reduction (often by interval lengthening between injections) with or without complete discontinuation as final step. According to the task force, DAGDO should also fulfil the following criteria: (1) following the T2T principle with regular visits (every 1–3 months or up to every 6 months if there is sustained remission), (2) measurement of disease activity with a valid tool, (3) agreement on treatment target (remission or low disease activity) and (4) switching/intensifying treatment if treatment target is not reached. DAGDO should only be performed when the treatment target is sustained, defined as ≥3 months on target with two or more formal disease activity measurements.
16. For patients with RA in whom the treatment target is reached and sustained, rheumatologists should consider DAGDO of anti-TNF drugs.
17. For patients with RA in whom the treatment target is reached and sustained, rheumatologists might consider DAGDO of IL-6 inhibitors, rituximab, baricitinib or abatacept.
DAGDO of TNFis in RA is supported by two systematic reviews8 48 and should therefore be considered in patients in which the treatment target is reached and sustained. DAGDO of abatacept and tocilizumab is also supported by two reviews48 49 but with less evidence compared with TNFis. Dose reduction of rituximab (to 1*500 or 1*200 mg every 6 months) was investigated in a double-blinded RCT and advised by the authors, although formal non-inferiority criteria were not met.50 A study investigating the dose reduction of baricitinib to 2 mg found that many patients could maintain control of disease activity, and if not, disease control could be recaptured with return to 4 mg.51
18. For patients with axSpA and PsA in whom the treatment target is reached and sustained, rheumatologists might consider DAGDO of anti-TNF drugs.
Evidence on DAGDO of TNFi in axSpA has been included in two low-quality reviews, supporting stepwise tapering of these drugs.49 52 One review also looked into DAGDO of PsA but was not able to draw conclusions because of the absence of evidence.49 Therefore, the point to consider for PsA is expert opinion level only.
19. Rheumatologists can use any DAGDO scheme, as none is preferential based on the evidence.
An expert opinion point to consider was formulated on the dose reduction scheme. Although no scheme is preferential, the task force advises dose reduction by interval lengthening in 1–4 steps with or without complete discontinuation, for example, 100%–50%–0% or 100%–66%–50%–33%−0%. Whenever a flare or loss of disease control occurs, it is advised to return to last effective dose.
Non-medical drug switching
20. Non-medical switching within or between b/tsDMARD classes is not advised because of the absence of evidence on efficacy and safety.
Non-medical drug switching is drug switching for other reasons than (loss of) efficacy, side effects or adherence, for example, to reduce drug costs.53 For these recommendations, this includes switching within or between a drug class but excludes non-medical biosimilar transitioning (which is addressed as a separate strategy). We found no supporting evidence on this topic. Therefore, non-medical drug switching is not advised and should be further investigated. Of note, when a drug is not available temporarily or definitively, which was the case, for example for tocilizumab, sarilumab and abatacept in COVID times, non-medical switching cannot be avoided and should be offered of course.
Discussion
In this study, we were able to identify 12 strategies for cost-effective use of b/tsDMARDs in IRD: response prediction, drug formulary policy, biosimilar/generic drug use, avoid dose loading, initial lower dose, optimising pharmacokinetic exposure, combination therapy, route of administration, drug wastage, medication adherence, DAGDO and non-medical drug switching. Moreover, we formulated high-quality clinical points to consider for the majority of those strategies, based on an extensive literature review and stakeholder engagement. These points to consider can be used in addition to the recommendations for the management of RA, PsA or axSpA and are broadly applicable across many healthcare environments.
Our points to consider have some limitations. First, we did not include patient representatives to our task force, but we would fully recommend this for an updated version. Second, because of feasibility, we only included systematic reviews and RCTs as a consequence of which we could have missed some important non-randomised clinical studies. For the strategy of initial lower dose specifically, we planned to look in the registration data of all b/tsDMARDs to check for lower effective doses tested in phase 1 and 2 trials, but this was deemed not feasible. Third, most included systematic reviews were of low or critically low AMSTAR-2 quality. Nevertheless, we were able to combine multiple reviews with high-quality RCTs to form high-quality points to consider. Four, we mainly focused on drug costs as the main cost component of cost-effectiveness and might have missed other important costs which can influence cost-effectiveness of therapy. Also, net drug costs fluctuate over time which may affect the points to consider. Last, because of contextual differences in healthcare systems and reimbursement policies across countries, the generalisability of these points-to-consider may be limited in certain contexts.
Although we could form points to consider for most strategies, some research gaps have been identified through the scoping review. An important one is less overall evidence for PsA and axSpA compared with RA at the time of our search, for example, for DAGDO and combination therapy. Moreover, for the four strategies, there was no SLR or RCT evidence available. A research agenda is included in the supplementary online supplemental box 1. Of note, important studies have been published after our search which could not be included when formulating the points to consider, such as the NOR-DRUM B study and a DAGDO RCT in PsA and axSpA.54 55
Changes in b/tsDMARD prices require these points to consider to be kept under review and, if necessary, updated. As an increasing number of b/tsDMARDs will lose their patent and thus the possibility for biosimilar or generic drug variants becomes available, this might lead to increased competition and lower drug prices. However, the drug losing patent protection does not equate to direct availability of a biosimilar, for example, rituximab (4 years after patent expiry), and tocilizumab and abatacept (no biosimilars available yet). Also, new b/tsDMARDs are still entering the market, leading to an increased number to choose from and more price competition. Finally, some points to consider are of value to the patient also when leaving costs out of the equation, for example, lower-dosed rituximab for the same effect but with less infusion time and side effects. Therefore, we think that these points to consider on cost-effectiveness will remain of value and require an update in the future.
In conclusion, healthcare costs are spiralling up, and yet we have a finite financial envelope. For clinicians to provide the best care to the greatest number, it is our responsibility to be cognisant of costs and use high-cost medications wisely. This framework of strategies and corresponding points to consider for cost-effective use of b/tsDMARDs in IRD can be a starting point to incorporate cost-effectiveness into clinical care.
Footnotes
Contributors: All authors were involved in defining the strategies with their definitions, formulating the overarching principles and recommendations, and voting for the recommendations. The scoping review was performed by CJTvdT under the supervision of BVdB, LV and AAdB. RoB assessment was performed by CJTvdT, BVdB, LV and AAdB. The analyses were performed by CJTvdT. The manuscript was drafted by CJTvdT and AAdB, and all other authors critically revised the manuscript. AAdB is the guarantor of the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: BvdB: speakers bureau for UCB, Pfizer, Sanofi-Aventis, Galapagos, Amgen and Eli Lilly. DA: speakers bureau for Abbvie, Amgen, Lilly, Janssen, Merck, Novartis, Pfizer, Roche and Sandoz; consultant of Abbvie, Amgen, Lilly, Janssen, Merck, Novartis, Pfizer, Roche and Sandoz; research support from: Abbvie, Amgen, Lilly, Novartis, Roche, SoBi and Sanofi. RA: speakers bureau for Abbvie, BMS, Celltrion, Galapagos, Gilead, Janssen, Lilly, Novartis, Pfize and Roche; paid instructor for Abbvie, BMS, Celltrion, Galapagos, Gilead, Janssen, Lilly, Novartis, Pfizer and Roche; consultant of Abbvie, BMS, Celltrion, Galapagos, Gilead, Janssen, Lilly, Novartis, Pfizer and Roche; research support from Abbvie, BMS, Celltrion, Galapagos, Gilead, Janssen, Lilly, Novartis, Pfizer and Roche. KC: consultant of Eli Lilly, AbbVie and Pfizer. JI: speakers bureau for AbbVie, Gilead, Roche and UCB; research support from GSK, Janssen and Pfizer. DM: invitation to attend congress: Celltrion Healthcare and GSK. PV: speakers bureau for Eli Lilly, MSD, Galapagos and Roularta; consultant of Galapagos, Gilead, Pfizer, Sidekick Health, Eli Lilly, Nordic Pharma, Abbvie, Celltrion, BMS and UCB; research support from Pfizer. AGV: speakers bureau for Amgen, Biogen Idec, Bristol Meyers Squibb, Effik Benelux, F. Hoffmann-La Roche, Eli Lilly, Febelgen/Medaxes, Medicines for Europe AISBL, Mundipharma, Pfizer/Hospira and Hexal/Sandoz; paid instructor for Effik Benelux, Fresenius/Kabi, Amgen and Sandoz/Novartis; consultant of Biogen Idec, Effik Benelux, Fresenius/Kabi, Pfizer/Hospira, Sandoz/Novartis and Samsung Bioepis. AAdB: research support from Abbvie, Galapagos, Pfizer, Novartis, Lilly, Sanofi and Gilead. CJTvdT, JG, PMJW and LV have no competing interests to declare.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
References
- 1.Kerschbaumer A, Sepriano A, Smolen JS, et al. Efficacy of pharmacological treatment in rheumatoid arthritis: a systematic literature research Informing the 2019 update of the EULAR recommendations for management of rheumatoid arthritis. Ann Rheum Dis 2020;79:744–59. 10.1136/annrheumdis-2019-216656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kerschbaumer A, Smolen JS, Dougados M, et al. Pharmacological treatment of psoriatic arthritis: a systematic literature research for the 2019 update of the EULAR recommendations for the management of psoriatic arthritis. Ann Rheum Dis 2020;79:778–86. 10.1136/annrheumdis-2020-217163 [DOI] [PubMed] [Google Scholar]
- 3.Cruz-Machado AR, Rodrigues-Manica S, Silva JL, et al. Effect of biologic disease-modifying anti-rheumatic drugs targeting remission in axial spondyloarthritis: systematic review and meta-analysis. Rheumatology (Oxford) 2020;59:3158–71. 10.1093/rheumatology/keaa268 [DOI] [PubMed] [Google Scholar]
- 4.John M. n.d. Eisenberg center for clinical decisions and communications science. medicines for rheumatoid arthritis: A review of the research for adults.
- 5.Brkic A, Diamantopoulos AP, Haavardsholm EA, et al. Exploring drug cost and disease outcome in rheumatoid arthritis patients treated with biologic and targeted synthetic dmards in Norway in 2010-2019-a country with a national tender system for prescription of costly drugs. BMC Health Serv Res 2022;22:48. 10.1186/s12913-021-07425-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 2020;79:685–99. 10.1136/annrheumdis-2019-216655 [DOI] [PubMed] [Google Scholar]
- 7.National institute for health and care excellence (NICE) . Process and methods: 7 assessing cost effectiveness. Available: https://www.nice.org.uk/process/pmg6/chapter/assessing-cost-effectiveness [Accessed 25 Jul 2022].
- 8.Verhoef LM, van den Bemt BJ, van der Maas A, et al. Down-titration and discontinuation strategies of tumour necrosis factor-blocking agents for rheumatoid arthritis in patients with low disease activity. Cochrane Database Syst Rev 2019;5:CD010455. 10.1002/14651858.CD010455.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kay J, Schoels MM, Dörner T, et al. Consensus-Based recommendations for the use of biosimilars to treat rheumatological diseases. Ann Rheum Dis 2018;77:165–74. 10.1136/annrheumdis-2017-211937 [DOI] [PubMed] [Google Scholar]
- 10.van der Heijde D, Aletaha D, Carmona L, et al. 2014 update of the EULAR standardised operating procedures for EULAR-endorsed recommendations. Ann Rheum Dis 2015;74:8–13. 10.1136/annrheumdis-2014-206350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van der Heijde D, De Thurah A. Additional guidance on the methodology for the development/update of EULAR recommendations. Available: https://www.eular.org/myUploadData/files/additional_guidance_sop_eular_endorsed_recommendations_v2_june2018.pdf [Accessed 25 Jul 2022].
- 12.The cochrane collaboration. the cochrane highly sensitive search strategies for identifying randomized trials in pubmed. n.d. Available: https://work.cochrane.org/pubmed
- 13.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smolen JS, Breedveld FC, Burmester GR, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international Task force. Ann Rheum Dis 2016;75:3–15. 10.1136/annrheumdis-2015-207524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smolen JS, Schöls M, Braun J, et al. Treating axial spondyloarthritis and peripheral spondyloarthritis, especially psoriatic arthritis, to target: 2017 update of recommendations by an international Task force. Ann Rheum Dis 2018;77:3–17. 10.1136/annrheumdis-2017-211734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fraenkel L, Bathon JM, England BR, et al. 2021 American College of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 2021;73:924–39. 10.1002/acr.24596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shmais M, Regueiro M, Hashash JG. Proactive versus reactive therapeutic drug monitoring: why, when, and how? Inflamm Intest Dis 2022;7:50–8. 10.1159/000518755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tikhonova IA, Yang H, Bello S, et al. Enzyme-Linked immunosorbent assays for monitoring TNF-alpha inhibitors and antibody levels in people with rheumatoid arthritis: a systematic review and economic evaluation. Health Technol Assess 2021;25:1–248. 10.3310/hta25080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Syversen SW, Goll GL, Jørgensen KK, et al. Effect of therapeutic drug monitoring vs standard therapy during infliximab induction on disease remission in patients with chronic immune-mediated inflammatory diseases: a randomized clinical trial. JAMA 2021;325:1744–54. 10.1001/jama.2021.4172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pouw J, Leijten E, Radstake T, et al. Emerging molecular biomarkers for predicting therapy response in psoriatic arthritis: a review of literature. Clin Immunol 2020;211:108318.:S1521-6616(19)30607-2. 10.1016/j.clim.2019.108318 [DOI] [PubMed] [Google Scholar]
- 22.Schlager L, Loiskandl M, Aletaha D, et al. Predictors of successful discontinuation of biologic and targeted synthetic dmards in patients with rheumatoid arthritis in remission or low disease activity: a systematic literature review. Rheumatology (Oxford) 2020;59:324–34. 10.1093/rheumatology/kez278 [DOI] [PubMed] [Google Scholar]
- 23.Tweehuysen L, van den Ende CH, Beeren FMM, et al. Little evidence for usefulness of biomarkers for predicting successful dose reduction or discontinuation of a biologic agent in rheumatoid arthritis: a systematic review. Arthritis Rheumatol 2017;69:301–8. 10.1002/art.39946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ingegnoli F, Favalli EG, Meroni PL. Does polymorphysm of genes coding for pro-inflammatory mediators predict the clinical response to TNF alpha blocking agents? A review analysis of the literature. Autoimmun Rev 2011;10:460–3. 10.1016/j.autrev.2011.01.010 [DOI] [PubMed] [Google Scholar]
- 25.Tanaka Y, Oba K, Koike T, et al. Sustained discontinuation of infliximab with a raising-dose strategy after obtaining remission in patients with rheumatoid arthritis: the RRRR study, a randomised controlled trial. Ann Rheum Dis 2020;79:94–102. 10.1136/annrheumdis-2019-216169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim JW, Jung JY, Suh CH. Real-World observational study of biosimilars in inflammatory arthritis treatment: a systematic literature review. Expert Opin Biol Ther 2021;21:57–73. 10.1080/14712598.2020.1812575 [DOI] [PubMed] [Google Scholar]
- 27.Cantini F, Benucci M, Li Gobbi F, et al. Biosimilars for the treatment of psoriatic arthritis. Expert Rev Clin Immunol 2019;15:1195–203. 10.1080/1744666X.2020.1682553 [DOI] [PubMed] [Google Scholar]
- 28.Numan S, Faccin F. Non-Medical switching from originator tumor necrosis factor inhibitors to their biosimilars: systematic review of randomized controlled trials and real-world studies. Adv Ther 2018;35:1295–332. 10.1007/s12325-018-0742-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feagan BG, Lam G, Ma C, et al. Systematic review: efficacy and safety of switching patients between reference and biosimilar infliximab. Aliment Pharmacol Ther 2019;49:31–40. 10.1111/apt.14997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mezones-Holguin E, Gamboa-Cardenas RV, Sanchez-Felix G, et al. Efficacy and safety in the continued treatment with a biosimilar drug in patients receiving infliximab: a systematic review in the context of decision-making from a latin-american country. Front Pharmacol 2019;10:1010. 10.3389/fphar.2019.01010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geurts-Voerman GE, Verhoef LM, van den Bemt BJF, et al. The pharmacological and clinical aspects behind dose loading of biological disease modifying anti-rheumatic drugs (bdmards) in auto-immune rheumatic diseases (airds): rationale and systematic narrative review of clinical evidence. BMC Rheumatol 2020;4:37. 10.1186/s41927-020-00130-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bredemeier M, Campos GG, de Oliveira FK. Updated systematic review and meta-analysis of randomized controlled trials comparing low- versus high-dose rituximab for rheumatoid arthritis. Clin Rheumatol 2015;34:1801–5. 10.1007/s10067-015-2977-z [DOI] [PubMed] [Google Scholar]
- 33.Maini RN, Taylor PC, Szechinski J, et al. Double-Blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate. Arthritis Rheum 2006;54:2817–29. 10.1002/art.22033 [DOI] [PubMed] [Google Scholar]
- 34.Smolen JS, Beaulieu A, Rubbert-Roth A, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (option study): a double-blind, placebo-controlled, randomised trial. Lancet 2008;371:987–97. 10.1016/S0140-6736(08)60453-5 [DOI] [PubMed] [Google Scholar]
- 35.Ogata A, Atsumi T, Fukuda T, et al. Sustainable efficacy of switching from intravenous to subcutaneous tocilizumab monotherapy in patients with rheumatoid arthritis. Arthritis Care Res (Hoboken) 2015;67:1354–62. 10.1002/acr.22598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weng C, Xue L, Wang Q, et al. Comparative efficacy and safety of Janus kinase inhibitors and biological disease-modifying antirheumatic drugs in rheumatoid arthritis: a systematic review and network meta-analysis. Ther Adv Musculoskelet Dis 2021;13:1759720X21999564. 10.1177/1759720X21999564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tarp S, Jørgensen TS, Furst DE, et al. Added value of combining methotrexate with a biological agent compared to biological monotherapy in rheumatoid arthritis patients: a systematic review and meta-analysis of randomised trials. Semin Arthritis Rheum 2019;48:958–66. 10.1016/j.semarthrit.2018.10.002 [DOI] [PubMed] [Google Scholar]
- 38.Teitsma XM, Marijnissen AKA, Bijlsma JWJ, et al. Tocilizumab as monotherapy or combination therapy for treating active rheumatoid arthritis: a meta-analysis of efficacy and safety reported in randomized controlled trials. Arthritis Res Ther 2016;18:211. 10.1186/s13075-016-1108-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jansen JP, Buckley F, Dejonckheere F, et al. Comparative efficacy of biologics as monotherapy and in combination with methotrexate on patient reported outcomes (pros) in rheumatoid arthritis patients with an inadequate response to conventional dmards -- a systematic review and network meta-analysis. Health Qual Life Outcomes 2014;12:102. 10.1186/1477-7525-12-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burmester G-R, Kivitz AJ, Kupper H, et al. Efficacy and safety of ascending methotrexate dose in combination with adalimumab: the randomised concerto trial. Ann Rheum Dis 2015;74:1037–44. 10.1136/annrheumdis-2013-204769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Behrens F, Cañete JD, Olivieri I, et al. Tumour necrosis factor inhibitor monotherapy vs combination with MTX in the treatment of PSA: a systematic review of the literature. Rheumatology (Oxford) 2015;54:915–26. 10.1093/rheumatology/keu415 [DOI] [PubMed] [Google Scholar]
- 42.Lin S, He M, Chen J. Tumor necrosis factor-alpha inhibitor combined with methotrexate for ankylosing spondylitis: a systematic review and meta-analysis. Rheumatol Rep 2014;6:6–11. 10.4081/rr.2014.5127 [DOI] [Google Scholar]
- 43.Burmester GR, Rubbert-Roth A, Cantagrel A, et al. A randomised, double-blind, parallel-group study of the safety and efficacy of subcutaneous tocilizumab versus intravenous tocilizumab in combination with traditional disease-modifying antirheumatic drugs in patients with moderate to severe rheumatoid arthritis (SUMMACTA study). Ann Rheum Dis 2014;73:69–74. 10.1136/annrheumdis-2013-203523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Westhovens R, Wiland P, Zawadzki M, et al. Efficacy, pharmacokinetics and safety of subcutaneous versus intravenous CT-P13 in rheumatoid arthritis: a randomized phase I/III trial. Rheumatology (Oxford) 2021;60:2277–87. 10.1093/rheumatology/keaa580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Genovese MC, Covarrubias A, Leon G, et al. Subcutaneous abatacept versus intravenous abatacept: a phase IIIB noninferiority study in patients with an inadequate response to methotrexate. Arthritis Rheum 2011;63:2854–64. 10.1002/art.30463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Burmester GR, Rubbert-Roth A, Cantagrel A, et al. Efficacy and safety of subcutaneous tocilizumab versus intravenous tocilizumab in combination with traditional dmards in patients with RA at week 97 (SUMMACTA). Ann Rheum Dis 2016;75:68–74. 10.1136/annrheumdis-2015-207281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ritschl V, Stamm TA, Aletaha D, et al. 2020 EULAR points to consider for the prevention, screening, assessment and management of non-adherence to treatment in people with rheumatic and musculoskeletal diseases for use in clinical practice. Ann Rheum Dis 2021;80:707–13. 10.1136/annrheumdis-2020-218986 [DOI] [PubMed] [Google Scholar]
- 48.Vasconcelos LB, Silva MT, Galvao TF. Reduction of biologics in rheumatoid arthritis: a systematic review and meta-analysis. Rheumatol Int 2020;40:1949–59. 10.1007/s00296-020-04651-z [DOI] [PubMed] [Google Scholar]
- 49.Edwards CJ, Fautrel B, Schulze-Koops H, et al. Dosing down with biologic therapies: a systematic review and clinicians’ perspective. Rheumatology (Oxford) 2017;56:1847–56. 10.1093/rheumatology/kew464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Verhoef LM, den Broeder N, Thurlings RM, et al. Ultra-Low doses of rituximab for continued treatment of rheumatoid arthritis (REDO study): a randomised controlled non-inferiority trial. The Lancet Rheumatology 2019;1:e145–53. 10.1016/S2665-9913(19)30066-9 [DOI] [PubMed] [Google Scholar]
- 51.Takeuchi T, Genovese MC, Haraoui B, et al. Dose reduction of baricitinib in patients with rheumatoid arthritis achieving sustained disease control: results of a prospective study. Ann Rheum Dis 2019;78:171–8. 10.1136/annrheumdis-2018-213271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Navarro-Compán V, Plasencia-Rodríguez C, de Miguel E, et al. Anti-Tnf discontinuation and tapering strategies in patients with axial spondyloarthritis: a systematic literature review. Rheumatology (Oxford) 2016;55:1188–94. 10.1093/rheumatology/kew033 [DOI] [PubMed] [Google Scholar]
- 53.Dolinar R, Kohn CG, Lavernia F, et al. The non-medical switching of prescription medications. Postgrad Med 2019;131:335–41. 10.1080/00325481.2019.1618195 [DOI] [PubMed] [Google Scholar]
- 54.Syversen SW, Jørgensen KK, Goll GL, et al. Effect of therapeutic drug monitoring vs standard therapy during maintenance infliximab therapy on disease control in patients with immune-mediated inflammatory diseases: a randomized clinical trial. JAMA 2021;326:2375–84. 10.1001/jama.2021.21316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Michielsens CA, den Broeder N, van den Hoogen FH, et al. Treat-to-target dose reduction and withdrawal strategy of TNF inhibitors in psoriatic arthritis and axial spondyloarthritis: a randomised controlled non-inferiority trial. Ann Rheum Dis 2022;81:1392–9. 10.1136/annrheumdis-2022-222260 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2022-002898supp001.pdf (2.5MB, pdf)
Data Availability Statement
Data are available on reasonable request.


