OBJECTIVES:
Tracheal intubation (TI) is a common procedure in critical care, often performed with a Macintosh curved blade used for direct laryngoscopy (DL). Minimal evidence informs the choice between Macintosh blade sizes during TI. We hypothesized that Macintosh 4 blade would have higher first-attempt success than Macintosh 3 blade during DL.
DESIGN:
Retrospective analysis using a propensity score and inverse probability weighting of data from six prior multicenter randomized trials.
SETTING AND PARTICIPANTS:
Adult patients who underwent nonelective TI at participating emergency departments and ICUs. We compared the first-pass success of TI with DL in subjects intubated with a size 4 Macintosh blade on the first TI attempt to subjects with a size 3 Macintosh blade on the first TI attempt.
MAIN RESULTS:
Among 979 subjects, 592 (60.5%) had TI using DL with a Macintosh blade, of whom 362 (37%) were intubated with a size 4 blade and 222 (22.7%) with a size 3 blade. We used inverse probability weighting with a propensity score for analyzing data. We found that patients intubated with a size 4 blade had a worse (higher) Cormack-Lehane grade of glottic view than patients intubated with a size 3 blade (adjusted odds ratio [aOR], 1.458; 95% CI, 1.064–2.003; p = 0.02). Patients intubated with a size 4 blade had a lower first pass success than those with a size 3 blade (71.1% vs 81.2%; aOR, 0.566; 95% CI, 0.372–0.850; p = 0.01).
CONCLUSIONS AND RELEVANCE:
In critically ill adults undergoing TI using DL with a Macintosh blade, patients intubated using a size 4 blade on first attempt had a worse glottic view and a lower first pass success than patients intubated with a size 3 Macintosh blade. Further prospective studies are needed to examine the optimal approach to selecting laryngoscope blade size during TI of critically ill adults.
Keywords: airway management, critical care, laryngoscopesize, laryngoscopy, mechanical ventilation, tracheal intubation
KEY POINTS
Question: Does a Macintosh size 4 laryngoscope have higher first-attempt success than a Macintosh size 3 during tracheal intubation (TI) with direct laryngoscopy (DL)?
Findings: In a post hoc analysis of six clinical trials, using inverse probability weighting, patients intubated with a size 4 blade had a worse (higher) glottic view and a lower first pass success for TI with DL than those who had TI with a size 3 blade. The duration of intubation was similar between the 2 blade sizes.
Meaning: Macintosh size 3 blade performed better than size 4 during TI with DL. Further research is needed to determine the optimal approach to selecting laryngoscope blade size during TI of critically ill adults.
Tracheal intubation (TI) is a lifesaving procedure performed routinely in emergency departments (EDs) and ICUs. TI is associated with a significant risk of complications such as hypoxemia and cardiovascular collapse (1–3). Intubation using a direct laryngoscope (DL) with a Macintosh curved blade remains one of the most common techniques for intubation (3, 4). When it was introduced in 1943, only the current size 3 Macintosh blade existed. Since then, multiple blade sizes have become available, ranging from 0 to 4 (5). The operator typically chooses the blade size based on individual preferences, experience, perceived patient characteristics, and availability. The size of the DL blade has often been left to clinician discretion in clinical trials. Historically, a size 3 blade was considered the standard size for intubation. More recently, however, some experts have suggested using a size 4 blade in all patients due to the longer length with a similar vertical footprint as a size 3. In addition, the added length of the size 4 blade has been hypothesized to better engage a deep vallecula or, if needed, directly lift the epiglottis to facilitate intubation (4). Available studies are limited to specific patient populations (6), simulation environments (7) or small sample sizes (8). In a secondary analysis of six previously reported clinical trials, we aimed to compare size 4 versus size 3 blades with regard to clinical outcomes, including the grade of glottic view, successful intubation on the first attempt, and duration of intubation among critically ill adults undergoing nonelective TI using a DL technique (9). We hypothesized that a Macintosh size 4 would have greater clinical success when compared with a Macintosh size 3 during TI using DL.
MATERIALS AND METHODS
Design
We performed a post hoc analysis of prospectively collected data from six previously published randomized trials of airway management conducted by the Pragmatic Critical Care Research Group in the United States (1, 10–14). The trials enrolled 979 patients undergoing nonelective TI in the ED or ICU between February 2014 and May 2018. We analyzed deidentified data in the trial datasets from patients who were intubated using DL with a Macintosh blade size 4 or 3 on the first attempt; we excluded patients intubated with smaller blade sizes or those for whom data on blade size was missing or a video laryngoscope used on first attempt. Individual trials were approved by the institutional review board (IRB) of each respective site with documented waiver of informed consent by respective site IRB (1, 10–14). Studies were carried out per the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975. Details are documented in individual manuscripts. This study was deemed a secondary analysis of a deidentified data set of prior studies and no IRB review was deemed necessary by the IRBs (and thus no number was assigned) as it did not fall under the board’s guidelines as human subjects research.
Dataset and Patient Population
The included trials had similar exclusion criteria, data collection procedures, variables, and outcome definitions. Patients were excluded if they were pregnant, or incarcerated, there was an immediate need to intubate preventing randomization, or the treating provider felt that the trial intervention was either required or contraindicated. The trials examined fluid bolus administration, bag-mask ventilation after induction, apneic oxygenation, use of a checklist for emergent intubation, video laryngoscopy compared with DL, and ramped positioning during TI of critically ill adults, respectively (1, 10–14). In each trial, a trained, independent observer collected data on the outcomes of the procedure, including the time between induction and intubation, peripheral oxygen saturation at induction, the number of intubation attempts, and the lowest oxygen saturation between induction and 2 minutes after TI. Immediately after each intubation, the operator reported the laryngoscope use, the initial Cormack-Lehane grade of glottic view (15), whether the intubation was successful on the first attempt, rescue devices used, the presence of difficult airway characteristics, and the occurrence of complications. Research personnel collected data on baseline characteristics, the initial laryngoscope blade size, management before and after laryngoscopy, and clinical outcomes from the electronic health record.
Outcomes
Outcomes for this secondary analysis included Cormack-Lehane grade glottic view, successful intubation on the first attempt, lowest peripheral oxygen saturation between induction and 2 minutes after TI, severe hypoxemia (defined as peripheral saturation < 80%), and duration of intubation (defined as the time from administration of induction medications to successful placement of the endotracheal tube in the trachea) (15). Exploratory outcomes included additional equipment required, peri-procedural complications, ventilator-free days, ICU length of stay, and death within 1 hour of the procedure. Additional equipment required was defined as the use of any adjunct, video laryngoscopy, or DL as identified by the proceduralist. Procedural complications included esophageal intubation, aspiration, airway trauma, or cardiac arrest, as reported by the proceduralist.
Statistical Analysis
We compared patients intubated with a size 4 Macintosh blade to patients intubated with a size 3 Macintosh blade. Baseline characteristics of the patients and procedure details were compared between groups using Mann-Whitney rank-sum tests, two-sample proportion tests, or permutation simulation tests as appropriate. To account for potential indication bias when comparing outcomes between patients intubated with a size 4 versus size 3 blade, we performed inverse probability weighting (IPW) using propensity score analysis (16). We fitted a logistic regression model for the treatment outcome of being intubated using a size 4 blade with the independent variables of patients’ age, sex, race, height, body mass index, Acute Physiology and Chronic Health Evaluation (APACHE II) score (17), indications for intubation (compromised airway, hypoxia, hypercapnia), limited neck mobility, preoxygenation method, operator experience with intubation, and trial site at which the intubation was performed. From this treatment model, we estimated a patient’s propensity to be treated with a size 4 blade. In place of propensity score matching to address potential covariate imbalances, which can often increase imbalance, model dependence, and bias, the propensity scores were used to generate IPWs (18). The IPWs were then assigned to the full analytical population to promote covariate balance between the two treatments and to measure the average treatment effect of the size 4 blade. We assessed covariate balance pre- and post-IPW using standardized differences in means and ratio of variance for every covariate.
We used a Cox proportional hazards model to regress the procedure duration to successful intubation based on the blade size, weighting responses with IPW (19). Binary secondary outcomes were modeled using logistic regression. A cumulative logistic model was used to compare the Cormack-Lehane grade of view. ICU-free days, ventilator-free days, and the lowest blood oxygen saturation were all scaled to the range (0–1) and modeled using zero-one inflated beta regression (20). Poisson and negative binomial generalized linear models were used to compare the average number of attempts and ICU length of stay for each blade size. Sensitivity analyses were conducted using several configurations of the model, including: 1) using the propensity score weights as a covariate instead of as sample weights, 2) inclusion of study site as a covariate, 3) inclusion of trial group as a covariate, 4) using an indicator for the study site with above average use of the larger blade size, and 5) ignoring propensity score weighting. Data were analyzed using the “survival” package in R (Version 4.1.2, Vienna, Austria), and the IPWs were generated using the “weightit” command from the WeightIt package (19, 21, 22). A two-sided α-level of 0.05 was used to establish significance, and to ensure valid inference, we implemented a bootstrap resampling procedure to construct standard errors from 1999 replications. To address missing values in our dataset, we used k-Nearest neighbors imputation to reduce bias relative to listwise deletion or mean substitution. Incomplete variables were imputed using a weighted average of the nearest 10 data points, the default settings in the DMwR2 package (23). Exploratory data analysis was leveraged to determine possible correlations of height, weight, body mass index, gender, and blade size on the procedure duration. Nonparametric locally weighted scatterplot smoothing (LOWESS) curves were fitted to the data to ascertain any potential cutoff points in the covariates to determine the optimal blade size for the operation. No such boundaries were found. The reporting of this study followed the Strengthening the Reporting of Observational Studies in Epidemiology statement (24).
RESULTS
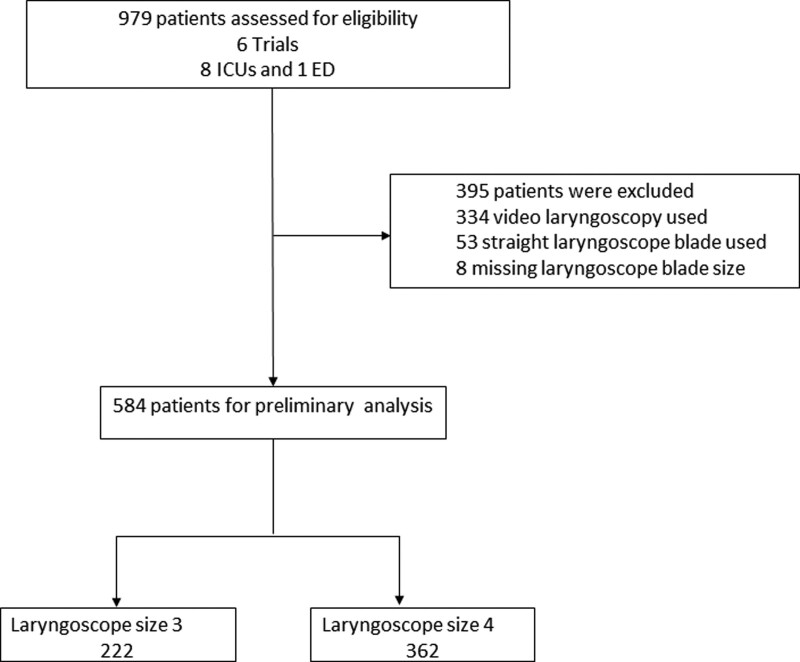
Of 979 patients in the combined dataset, 592 patients (60.5%) were intubated using a DL with a Macintosh blade. Of these, 8 (0.8%) were excluded due to missing blade size or blade size less than size 3. Therefore, we analyzed data on 584 patients (59.7%), with 222 (22.7%) intubated with a size 3 blade and 362 (37%) intubated with a size 4 blade (Fig. 1). The proportion of intubations performed using a size 4 blade showed considerable variation among study sites, ranging from 12.5% to 76.1% of intubations.
Figure 1.
Flow chart of patient selection. ED = emergency department.
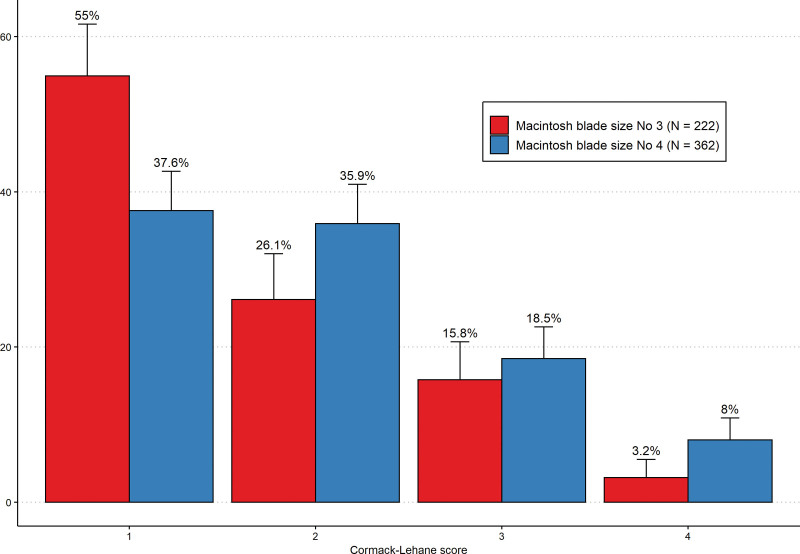
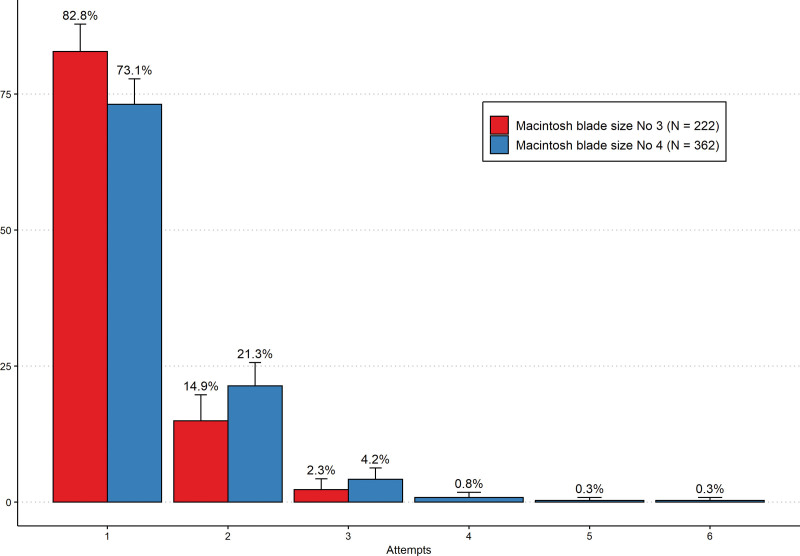
The unadjusted and adjusted baseline characteristics of the two groups are recorded in Table 1. The median patient age was 59 years, with a median APACHE II score of 21. Hypoxic respiratory failure was the most common reason for intubation (44.5%), and 46.2% of patients had at least one difficult airway characteristic. Prior to adjustment, there was a significant difference in height, weight, and sex between the two blade sizes. After IPW with a propensity score, the baseline characteristics between those intubated using a size 4 Macintosh blade to a size 3 were similar (Table 1). In an analysis using IPW with a propensity score, the Cormack-Lehane grade of glottic view was significantly higher (worse) with a size 4 blade compared with a size 3 blade (adjusted odds ratio [aOR],1.458; 95% CI, 1.064–2.003) (Table 2 and Fig. 2). First-pass success for endotracheal intubation was significantly lower for patients with TI using a size 4 blade than a size 3 blade (aOR, 0.566; 95% CI, 0.372–0.850; Fig. 3). The number of attempts for a size 4 blade was approximately 13% more than the number of attempts for a size 3 blade (adjusted incidence rate ratio [aIRR], 1.13, 95% CI, 1.04–1.23). The lowest oxygen saturation between induction and 2 minutes after intubation was similar between a size 4 blade and a size 3 blade (aOR, 1.00; 95% CI, 0.778–1.27). The percentage of subjects with of severe hypoxemia did not differ significantly between a size 4 blade and a size 3 blade (aOR, 0.772; 95% CI, 0.362–1.643). Duration of intubation also did not significantly differ between patients intubated using a size 4 blade compared with a size 3 blade 142.0 seconds versus 125.0 seconds (adjusted hazard ratio, 0.883; 95% CI, 0.718–1.086) (Supplemental Table 1 and Supplemental Figs. 1 and 2, http://links.lww.com/CCX/B137). The use of additional equipment during subsequent intubation attempts, such as DL, video laryngoscope, or repositioning, was similar between the two groups (Supplemental Table 2, http://links.lww.com/CCX/B137).
TABLE 1.
Baseline Characteristics of Patients Intubated With Macintosh Size Three Versus Size Four
| Patient Characteristics | Before IPW | p | After IPW | p | ||
|---|---|---|---|---|---|---|
| Mac 3 | Mac 4 | Mac 3 | Mac 4 | |||
| Number of Pts | 222 | 362 | ||||
| Age | 59.0 (47.0–67.0) | 59.0 (46.3–68.0) | 0.91 | 57.6 (46.6–68.4) | 56.8 (46.0–67.2) | 0.52 |
| Weight (kg)a | 71.7 (60.8–86.2) | 83.0 (71.2–98.9) | 0.00 | 83.1 (64.2–94.6) | 83.1 (66.0–97.5) | 0.99 |
| Height (cm)a | 168.8 (160.0–175.3) | 173 (166.9–180.3) | 0.00 | 171.5 (162.6–177.8) | 171.5 (164.8–180.1) | 0.83 |
| Body mass indexa | 26.1 (22.0–30.7) | 27.2 (23.8–32.8) | 0.01 | 28.6 (23.4–31.9) | 28.1 (22.5–32.6) | 0.5 |
| Gender (male) | 103 (46%) | 230 (64%) | 0.00 | 59% | 59% | 0.89 |
| Whitea | 153 (69%) | 267 (74%) | 0.24 | 72% | 71% | 0.77 |
| Acute Physiology and Chronic Health Evaluation II | 21.0 (16.0–27.0) | 22.0 (16.0–27.0) | 0.92 | 22.1 (15.3–26.3) | 22.3 (15.4–26.8) | 0.8 |
| Reason for intubation: | ||||||
| Hypoxemia | 102 (46%) | 158 (44%) | 0.64 | 45.3% | 48.4% | 0.47 |
| Hypoxemia and hypercapnia | 22 (10%) | 50 (14%) | 0.21 | 15.2% | 12.2% | 0.3 |
| Airway compromise | 12 (5%) | 13 (4%) | 0.40 | 3.4% | 3.8% | 0.78 |
| Any difficult airway characteristicsa | 96 (43%) | 174 (48%) | 0.29 | 50.0% | 48.8% | 0.77 |
| Limited neck mobility | 6 (3%) | 8 (2%) | 0.92 | 1.9% | 2.5% | 0.66 |
| Limited mouth opening | 4 (2%) | 11 (3%) | 0.52 | 2.8 (1.3%) | 2.3% | 0.36 |
| Methods of preoxygenation | ||||||
| Bag-mask ventilation | 54 (24%) | 85 (23%) | 0.89 | 26.6% | 26.5% | 0.97 |
| Noninvasive ventilation | 43 (19%) | 96 (27%) | 0.06 | 20.3% | 23.7% | 0.34 |
| High-flow nasal cannula | 21 (9%) | 29 (8%) | 0.65 | 17.3 (7.8%) | 8.1% | 0.88 |
| Nonrebreather | 95 (43%) | 134 (37%) | 0.19 | 41.3% | 37.1% | 0.31 |
| Baseline saturationa | 100.0 (96.0–100.0) | 99.0 (95.0–100.0) | 0.08 | 96.9 (95.5–99.8) | 96.8 (95.0–99.5) | 0.95 |
| Baseline SBPa | 121.9 (106.0–138.0) | 122.1 (107.3–138.0) | 0.71 | 126.2 (105.9–139.3) | 125.8 (106.4–139.7) | 0.86 |
| Any neuromuscular blockade | 209 (94%) | 352 (97%) | 0.1 | 96.7% | 97.0% | 0.81 |
IPW = inverse probability weighting, Mac 3 = Macintosh size 3 blade, Mac 4 = Macintosh size 4 blade, SBP = systolic blood pressure.
Imputation method used for missing values.
See Text for details of all difficult airway characteristics.
Interquartile range or percentage of the total.
TABLE 2.
Adjusted Outcomes Comparing Macintosh Curved Blades 3 and 4
| Adjusted Outcomes | Macintosh Size 3 Blade | Macintosh Size 4 Blade | p | Adjusted OR (CI) |
|---|---|---|---|---|
| Duration of intubation (s)a | 125.0 (90–200.3) | 142.0 (88–218.8) | 0.249 | 0.883 (0.718–1.086) |
| Median lowest o2 saturation (%)a | 93.5 (84.1–99.0) | 93.5 (81.6–97.8) | 0.97 | 1 (0.778–1.27) |
| Severe hypoxemiaa | 33.1 (15.2%) | 42.8 (12.2%) | 0.501 | 0.772 (0.362–1.643) |
| First-pass successa | 177.0 (81.2%) | 249.0 (71.1%) | 0.007 | 0.566 (0.372–0.850) |
| Cormack-Lehane grade view | 0.019 | 1.458 (1.064–2.003) | ||
| I | 105.6 (48.4%) | 135.7 (38.8%) | ||
| II | 65.4 (30.0%) | 116.4 (33.2%) | ||
| III | 35.4 (16.2%) | 72.0 (20.6%) | ||
| IV | 11.6 (5.3%) | 26.0 (7.4%) | ||
| Additional equipment: | 35.9 (16.4%) | 57.8 (16.4%) | 0.988 | 1.003 (0.638–1.594) |
| Direct laryngoscopy | 8.0 (3.6%) | 7.9 (2.2%) | 0.334 | 0.611 (0.221–1.691) |
| Video laryngoscopy | 27.9 (12.8%) | 49.8 (14.2%) | 0.629 | 1.131 (0.692–1.880) |
| Repositiona | 4.8 (7.9%) | 5.2 (4.6%) | 0.323 | 0.522 (0.140–1.987) |
| Complications | ||||
| Aspiration | 8.7 (4.0%) | 10.0 (2.8%) | 0.47 | 0.71 (0.280–1.839) |
| Esophageal intubation | 5.8 (2.7%) | 9.8 (2.8%) | 0.917 | 1.057 (0.382–3.204) |
| Airway trauma | 0.9 (0.0%) | 0.9 (0.0%) | 0.739 | 0.597 (0.015–21.87) |
| Cardiac arrest | 2.8 (1.3%) | 5.4 (1.5%) | 0.803 | 1.203 (0.295–6.195) |
| Outcomes | ||||
| 1-hr mortality | 5.2 (2.3%) | 2.2 (0.6%) | 0.091 | 0.252 (0.039–1.13) |
| Ventilator-free days, median | 15.0 (0.0–25.0) | 17.0 (0.0–25.0) | 0.504 | 0.767 (0.530–1.064) |
| ICU length of stay, mediana | 6.0 (3.0–9.0) | 6.0 (3.0–10.0) | 0.307 | 1.072 (0.936–1.228) |
OR = odds ratio.
Imputation method used for missing values.
Outcomes adjusted for age, sex, race, height, body mass index, Acute Physiology and Chronic Health Evaluation II score, indications for intubation (compromised airway, hypoxia, hypercapnia), limited neck mobility, preoxygenation method, operator experience with intubation, and trial site.
Interquartile range or percentage of total.
Figure 2.
Percentage of Cormack-Lehane grade view obtained by Macintosh (Mac) blade on the initial attempt. Mac 4 was associated with a worse view compared with Mac 3. Adjusted odds ratio 1.45 (1.06–2.00) size.
Figure 3.
Number of attempts by Macintosh (Mac) blade size. Mac 4 associated with lower first pass success and higher number of attempts in comparison to size 3 Mac blade.
DISCUSSION
We used a propensity score analysis of data from six randomized trials of nonelective TI in critical care settings to test the hypothesis that Macintosh 4 blades would have higher first-pass success than Macintosh 3 blades for DL. We found that contrary to our assumption, a size 3 blade was associated with a better (lower) grade of glottic view and higher first-pass success with fewer intubation attempts. The total duration of intubation, lowest oxygen saturation, and presence of severe hypoxemia were similar between the two Macintosh sizes. Otherwise, there was no difference in exploratory outcomes including 1-hour mortality, ventilator-free days, or length of stay.
Our data are consistent with other studies that have evaluated laryngoscope blade size (6–8, 25). In a randomized trial of simulated intubations by physician trainees in South Korea, Kim et al (7) reported a higher incidence of successful intubation on the first attempt with a size 3 blade compared with a size 4 blade. Similarly, in a cross-over study of a select population of edentulous patients undergoing TI for elective surgery, Kim et al (8) reported an improved visualization of glottic opening with the smaller blade size. Tripathi and Pandey (6), in a study from India, suggested fewer intubation failures with smaller size blades in patients with shorter thyromental distances. Most recently, Godet et al (25) published in 2022 a multicenter observational study in French ICUs demonstrating higher first-pass success with Macintosh size 3 compared with size 4. Our results are in line with these prior studies and provide evidence against an approach of routinely using a size 4 blade during TI of critically ill adults.
Our observation of better procedural outcomes among patients intubated with a smaller blade size has several potential explanations. First, the longer length of a size 4 blade may make it more challenging to control its tip, leading to worse views than a size 3 blade. The increase in width by a few millimeters may contribute to poor visualization. In addition, as previously suggested by Kim et al (7), proceduralists may insert the size 4 laryngoscope too deeply, leading to poor visualization and esophageal intubations. However, while we did have worse views in our study with a size 4 blade, the number of esophageal intubations was similar between the two groups.
Our study has several limitations. First, our study is a retrospective analysis of prospectively collected data, which may lead to potential unidentified confounders. We have attempted to limit the effect of confounding by indication using propensity scoring. Propensity scoring allowed us to create a weighted sample of patients intubated with different-sized blades but similar in their baseline characteristics, minimizing the selection bias. For example, individuals intubated with size 4 Macintosh were heavier, taller, and more likely to be male before adjusting with propensity scoring. However, as with any observational analysis, the potential for residual confounding from unmeasured factors remains. Second, this analysis is limited to TI with a DL and does not inform the question of blade size or angulation during video laryngoscopy. Further research is needed to examine whether these findings on blade size translate to video laryngoscopy with a Macintosh blade. Third, our data set did not capture additional techniques such as glottic manipulation or patient positioning (except for a limited set of patients enrolled in the trial that investigated positioning) that may improve success rates. Finally, while we captured some difficult airway characteristics, we did not have an organized approach to characterizing difficult airway characteristics such as the MACHOCHA score (26).
Despite these limitations, our analysis represents a significant cohort of critically ill adults undergoing TI in the United States and allows us to understand the role of blade size in emergent TI. Our study extends the observations of the prior literature regarding the potential for better outcomes with a size 3 Macintosh blade. In addition, the variation of blade size usage amongst different study sites highlights the variation in practice due to the lack of evidence.
In conclusion, among critically ill adults undergoing TI, the duration of intubation was similar while using a size 3 Macintosh blade rather than a size 4 Macintosh blade. However, a size 3 Macintosh blade was associated with a higher incidence of successful intubation on the first attempt and better glottic visualization, with similar rates of complications. Our data suggest that laryngoscope blade size selection is an easily implementable intervention in emergent TI with the potential to impact clinical outcomes. Future prospective research should compare approaches to selecting blade size during TI of critically ill adults to definitively determine the effect of blade size on outcomes. This should include operator surveys examining preferences and difficult airway characteristics contributing to blade selection using validated scales such as the MACHOCHA score.
ACKNOWLEDGMENTS
Dr. James Dargin was the site PI for the Pragmatic Critical Care Research Group at Lahey Hospital & Medical Center in Burlington, MA, from the inception of Lahey’s participation in the network until his tragic passing (October 31, 2021) and was integral to the collection and quality of data included in this work.
APPENDIX 1. EXECUTIVE COMMITTEE MEMBERS PRAGMATIC CRITICAL CARE RESEARCH GROUP
Adit A. Ginde, MD, MPH, University of Colorado; Sheetal Gandotra, MD, University of Alabama at Birmingham Medical Center; Brian E. Driver, MD, Hennepin County Medical Center; Matthew E. Prekker, MD MPH, Hennepin County Medical Center; Stacy Trent, MD, Denver Health Medical Center; David R. Janz, MD, MSc, Louisiana State University School of Medicine; Derek W. Russell, MD, University of Alabama at Birmingham Medical Center; Todd W. Rice, MD, MSc Vanderbilt University Medical Center; Wesley H. Self, MD, Vanderbilt University Medical Center; and Kevin Gibbs, MD, Atrium Health, Wake Forest Baptist (https://www.pragmaticcriticalcare.org/about/leadership/).
Footnotes
Dr. Khan has received research funding from Eli Lilly, AstraZeneca, Regeneron pharmaceuticals, United Therapeutics, Johnson & Johnson, Dompe Pharmaceuticals, and 4D Medical, as site Principal Investigator for research enrollment, and consulting fees from Dompe Pharmaceuticals for clinical trial design. The remaining authors have disclosed that they do not have any potential conflicts of interest.
The Executive Committee members for the Pragmatic Critical Care Research Group are listed in Appendix 1.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Supplementary Material
REFERENCES
- 1.Casey JD, Janz DR, Russell DW, et al. : Bag-mask ventilation during tracheal intubation of critically ill adults. N Engl J Med 2019; 380:811–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Russell DW, Casey JD, Gibbs KW, et al. : Effect of fluid bolus administration on cardiovascular collapse among critically ill patients undergoing tracheal intubation: A randomized clinical trial. JAMA 2022; 328:270–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Russotto V, Myatra SN, Laffey JG, et al. : Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. JAMA 2021; 325:1164–1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walls R, Murphy M. (Eds): Manual of Emergency Airway Management. Fourth Edition. Philadelphia, PA, Lippincott Williams & Wilkins, 2012 [Google Scholar]
- 5.Macintosh RR: A new laryngoscope. Lancet 1943; 1:205 [Google Scholar]
- 6.Tripathi M, Pandey M: Short thyromental distance: A predictor of difficult intubation or an indicator for small blade selection?. Anesthesiology 2006; 104:1131–1136 [DOI] [PubMed] [Google Scholar]
- 7.Kim JH, Kim SW, Kim YM, et al. : Effect of the curved blade size on the outcomes of tracheal intubation performed by incoming interns: A randomized controlled manikin study. Medicine (Baltim) 2018; 97:e11984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim H, Chang JE, Han SH, et al. : Effect of the Macintosh curved blade size on direct laryngoscopic view in edentulous patients. Am J Emerg Med 2018; 36:120–123 [DOI] [PubMed] [Google Scholar]
- 9.Sakles JC, Chiu S, Mosier J, et al. : The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med 2013; 20:71–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janz DR, Semler MW, Lentz RJ, et al. : Randomized trial of video laryngoscopy for endotracheal intubation of critically ill adults. Crit Care Med 2016; 44:1980–1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Semler MW, Janz DR, Lentz RJ, et al. : Randomized trial of apneic oxygenation during endotracheal intubation of the critically ill. Am J Respir Crit Care Med 2016; 193:273–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Semler MW, Janz DR, Russell DW, et al. : A multicenter, randomized trial of ramped position vs sniffing position during endotracheal intubation of critically ill adults. Chest 2017; 152:712–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janz DR, Semler MW, Joffe AM, et al. : A multicenter randomized trial of a checklist for endotracheal intubation of critically ill adults. Chest 2018; 153:816–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Janz DR, Casey JD, Semler MW, et al. : Effect of a fluid bolus on cardiovascular collapse among critically ill adults undergoing tracheal intubation (PrePARE): A randomised controlled trial. Lancet Respir Med 2019; 7:1039–1047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cormack RS, Lehane J: Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39:1105–1111 [PubMed] [Google Scholar]
- 16.Rubin DB: The design versus the analysis of observational studies for causal effects: Parallels with the design of randomized trials. Stat Med 2007; 26:20–36 [DOI] [PubMed] [Google Scholar]
- 17.Knaus WA, Draper EA, Wagner DP, et al. : APACHE II: A severity of disease classification system. Crit Care Med 1985; 13:818–829 [PubMed] [Google Scholar]
- 18.King G, Nielsen R: Why propensity scores should not be used for matching. Political Anal 2019; 27:435–454 [Google Scholar]
- 19.Therneau TM: A Package for Survival Analysis in R. 2022. Available at: https://CRAN.R-project.org/package=survival. Accessed January 9, 2022
- 20.Rigby RA, Stasinopoulos DM: Generalized additive models for location, scale and shape. J R Stat Soc Ser C (Appl Stat) 2005; 54:507–554 [Google Scholar]
- 21.R Core Team: A language and environment for statistical computing. MSOR Connect 2014; 1 [Google Scholar]
- 22.Greifer N: Weighting for Covariate Balance in Observational Studies [R package WeightIt version 0.10.2]. 2020. Available at: https://cran.r-project.org/web/packages/WeightIt/WeightIt.pdf. Accessed January 9, 2022
- 23.Torgo L: Data Mining With R: Learning With Case Studies. Second Edition. Boca Raton, FL, CRC Press, Taylor & Francis Group, 2017 [Google Scholar]
- 24.von Elm E, Altman DG, Egger M, et al. : The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007; 370:1453–1457 [DOI] [PubMed] [Google Scholar]
- 25.Godet T, De Jong A, Garin C, et al. : Impact of Macintosh blade size on endotracheal intubation success in intensive care units: A retrospective multicenter observational MacSize-ICU study. Intensive Care Med 2022; 48:1176–1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Jong A, Molinari N, Terzi N, et al. : Early identification of patients at risk for difficult intubation in the intensive care unit: Development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med 2013; 187:832–839 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.